User login
It’s been one of those days. It all started at 4:30 this morning, when my 3-year-old son crawled into our bed, naked except for the diarrhea dripping down his leg. Turns out, this was his way—quite effective, I might add—of telling my wife and me that he had had an “accident.” After an hour of carrying soiled sheets to the washer, child-bathing, and Weimaraner coat-scrubbing, we relaxed to the sound of our 1-year-old daughter’s blood-curdling screams.
Upon examination, we found that the night had mysteriously transformed our precious little button-nosed bundle of joy into a tangle-haired, snot-nosed bundle of melancholy. Where her face used to be, there now hung something approximating the mask from that Scream movie. Additionally, her throat was raw, olive-sized lymph nodes populated her neck, and her nose had taken to perpetual booger-manufacturing. A rapid strep swab would later reveal the culprit, but at the moment, our differential tilted toward demonic possession.
That Dripping Feeling
Moments later, my wife and I picked 6:15 a.m. as the time to discover that we both had 7 a.m. meetings and no time to drop the kids off at daycare, especially when factoring in the 10-minute “discussion” we had about who was going to drop the kids off at daycare. All of this preceded my 7:10 a.m. arrival time for the 7 o’clock meeting with a hospital executive team to discuss our HM group funding for the next year—an encounter that left me feeling as my son must have just prior to crawling into bed with us that morning.
Now 8 a.m., I had to meet with a surgeon eager to unveil his “great idea” for our hospitalists to admit all of his patients. “It solves our problem of no interns, and allows you to play a meaningful role in the hospital!” he exclaimed.
“The meaningful role of intern?” I replied. Again, I had that dripping feeling.
It was 8:30 a.m. and I was ready to round on my patients. The first patient, a lovely woman, was stricken with un-insure-ia and a deep-seated belief that the inequitable health system that rendered her unable to get her surgery was clearly the result of some moral failing on my part. Next up was a spectacularly intoxicated male who welcomed my caring touch by belching a bit of breakfast burrito onto my cheek. Then it was a floridly bipolar patient whose apparent life mission was to drop her pants to show me her new mesh thong.
Burnout, Respect, Satisfaction
And so it continued until 1 p.m., when I had a meeting with a resident mentee of mine. It turns out that he wanted to tell me that despite his desire to be a hospitalist since his fourth year of medical school, he instead was going to apply to a rheumatology fellowship. After talking to several practicing hospitalists, he’d decided it just wasn’t for him—discussions he summarized as too much burnout, too little respect, and not enough satisfaction. Again, that dripping feeling.
Stuffing my face with a vending-machine carb-load that doubled as both breakfast and lunch, I sat down for a few minutes of e-mail. First up, a journal rejection of a research paper we’d recently submitted. Oh, the fulfillment of academics. Next were two e-mails that enzymatically trebled my “to do” list for the day. Sandwiched between those e-mails and one from a friend reminding me not to be late for a dinner that night that I was clearly going to be late for was an e-mail from a nice-appearing Nigerian man wanting to give me millions of dollars; at last, my day was turning around.
Alas, this was not the case. Checking my voicemail, I found out that my uncle was in the hospital, my dog’s lab tests were abnormal, my mom was angry about something, and I had missed a dentist appointment that morning. Finally, our group assistant came with a message that our prized hospitalist recruit had accepted a job at another institution. Drip … drip … drip…
Self-Reflection
Now 2:30 p.m., I took stock of my day and reflected on what my resident mentee had said about hospitalists. Trying to balance the rigors of patient care, academic requirements, life, friends, family, and being a boss, I was most definitely feeling a bit downtrodden, unsated, and crispy around the edges. What, exactly, did I like about this job? Was this what I wanted professionally? Would I ever find balance? Perhaps, too, a rheumatology application could salve my problems.
It was at that point that the notice for the SHM annual meeting appeared, oracle-like, on my desk. Picking it up, I realized this, not a two-year sojourn through the world of creaky joints, was the tonic to my problems.
Meeting Hierarchy
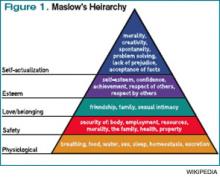
Every year since I began going to the SHM annual meeting in 2003, the meeting has helped me rejuvenate and grow. Much like Maslow’s Hierarchy of Needs, which posits that humans develop in stages that build on each other, I’ve found stepwise growth in the annual meeting.
Before my first meeting, I had been wandering nomadically through a hospitalist job for three years, wondering what, exactly, I was doing. I was the only hospitalist in my group, had few days off, with no support system around me. I had just agreed to take a job at another institution to build a new 10-person hospitalist group and had no idea how to do this. In Maslow terms, I was trying to satisfy my “physiologic needs” to survive. I needed to find, metaphorically, “food, water, clothes, and shelter.”
I found them at the annual meeting. The practice-management pre-course taught me how to build a hospitalist group, the mentorship breakfast introduced me to a veteran I still turn to, and the educational offerings helped improve my patient-care skills. I had conquered the base of Maslow’s pyramid.
The next year, I became involved in an SHM committee, and our gathering at the annual meeting helped set the course for our group’s future endeavors. I also met up with many friends I hadn’t seen since medical school and even recruited a person to my new group. In Maslow-speak, the meeting was helping me achieve my “safety needs” by providing control, well-being, and predictability.
By the third year, I was beginning to look forward to meeting up with national colleagues I had met at prior annual meetings, fulfilling Maslow’s third-stage need of “belonging.” During the ensuing years, I presented research projects, gave talks, and helped develop and lead forums and summits, thus quenching Maslow’s “self-esteem” need.
I wonder, as I leave my office to go back to see my afternoon complement of new patients, what my ninth annual meeting will bring. I’m not sure if I’ll ever achieve Maslow’s final phase of “self-actualization,” mostly because I’m not entirely sure what that means. However, I do know this: This job can be tough. We all feel it regardless of our age, gender, or practice setting. It is easy to get knocked out of balance, to get beaten down, to lose our focus. It is at those times that we all need a mariner to right the course. To remind us why we do this, to allow us to recharge, to facilitate our growth, to fulfill our needs.
For me, that mariner is the annual meeting. I look forward to seeing you all in Dallas next month. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s been one of those days. It all started at 4:30 this morning, when my 3-year-old son crawled into our bed, naked except for the diarrhea dripping down his leg. Turns out, this was his way—quite effective, I might add—of telling my wife and me that he had had an “accident.” After an hour of carrying soiled sheets to the washer, child-bathing, and Weimaraner coat-scrubbing, we relaxed to the sound of our 1-year-old daughter’s blood-curdling screams.
Upon examination, we found that the night had mysteriously transformed our precious little button-nosed bundle of joy into a tangle-haired, snot-nosed bundle of melancholy. Where her face used to be, there now hung something approximating the mask from that Scream movie. Additionally, her throat was raw, olive-sized lymph nodes populated her neck, and her nose had taken to perpetual booger-manufacturing. A rapid strep swab would later reveal the culprit, but at the moment, our differential tilted toward demonic possession.
That Dripping Feeling
Moments later, my wife and I picked 6:15 a.m. as the time to discover that we both had 7 a.m. meetings and no time to drop the kids off at daycare, especially when factoring in the 10-minute “discussion” we had about who was going to drop the kids off at daycare. All of this preceded my 7:10 a.m. arrival time for the 7 o’clock meeting with a hospital executive team to discuss our HM group funding for the next year—an encounter that left me feeling as my son must have just prior to crawling into bed with us that morning.
Now 8 a.m., I had to meet with a surgeon eager to unveil his “great idea” for our hospitalists to admit all of his patients. “It solves our problem of no interns, and allows you to play a meaningful role in the hospital!” he exclaimed.
“The meaningful role of intern?” I replied. Again, I had that dripping feeling.
It was 8:30 a.m. and I was ready to round on my patients. The first patient, a lovely woman, was stricken with un-insure-ia and a deep-seated belief that the inequitable health system that rendered her unable to get her surgery was clearly the result of some moral failing on my part. Next up was a spectacularly intoxicated male who welcomed my caring touch by belching a bit of breakfast burrito onto my cheek. Then it was a floridly bipolar patient whose apparent life mission was to drop her pants to show me her new mesh thong.
Burnout, Respect, Satisfaction
And so it continued until 1 p.m., when I had a meeting with a resident mentee of mine. It turns out that he wanted to tell me that despite his desire to be a hospitalist since his fourth year of medical school, he instead was going to apply to a rheumatology fellowship. After talking to several practicing hospitalists, he’d decided it just wasn’t for him—discussions he summarized as too much burnout, too little respect, and not enough satisfaction. Again, that dripping feeling.
Stuffing my face with a vending-machine carb-load that doubled as both breakfast and lunch, I sat down for a few minutes of e-mail. First up, a journal rejection of a research paper we’d recently submitted. Oh, the fulfillment of academics. Next were two e-mails that enzymatically trebled my “to do” list for the day. Sandwiched between those e-mails and one from a friend reminding me not to be late for a dinner that night that I was clearly going to be late for was an e-mail from a nice-appearing Nigerian man wanting to give me millions of dollars; at last, my day was turning around.
Alas, this was not the case. Checking my voicemail, I found out that my uncle was in the hospital, my dog’s lab tests were abnormal, my mom was angry about something, and I had missed a dentist appointment that morning. Finally, our group assistant came with a message that our prized hospitalist recruit had accepted a job at another institution. Drip … drip … drip…
Self-Reflection
Now 2:30 p.m., I took stock of my day and reflected on what my resident mentee had said about hospitalists. Trying to balance the rigors of patient care, academic requirements, life, friends, family, and being a boss, I was most definitely feeling a bit downtrodden, unsated, and crispy around the edges. What, exactly, did I like about this job? Was this what I wanted professionally? Would I ever find balance? Perhaps, too, a rheumatology application could salve my problems.
It was at that point that the notice for the SHM annual meeting appeared, oracle-like, on my desk. Picking it up, I realized this, not a two-year sojourn through the world of creaky joints, was the tonic to my problems.
Meeting Hierarchy
Every year since I began going to the SHM annual meeting in 2003, the meeting has helped me rejuvenate and grow. Much like Maslow’s Hierarchy of Needs, which posits that humans develop in stages that build on each other, I’ve found stepwise growth in the annual meeting.
Before my first meeting, I had been wandering nomadically through a hospitalist job for three years, wondering what, exactly, I was doing. I was the only hospitalist in my group, had few days off, with no support system around me. I had just agreed to take a job at another institution to build a new 10-person hospitalist group and had no idea how to do this. In Maslow terms, I was trying to satisfy my “physiologic needs” to survive. I needed to find, metaphorically, “food, water, clothes, and shelter.”
I found them at the annual meeting. The practice-management pre-course taught me how to build a hospitalist group, the mentorship breakfast introduced me to a veteran I still turn to, and the educational offerings helped improve my patient-care skills. I had conquered the base of Maslow’s pyramid.
The next year, I became involved in an SHM committee, and our gathering at the annual meeting helped set the course for our group’s future endeavors. I also met up with many friends I hadn’t seen since medical school and even recruited a person to my new group. In Maslow-speak, the meeting was helping me achieve my “safety needs” by providing control, well-being, and predictability.
By the third year, I was beginning to look forward to meeting up with national colleagues I had met at prior annual meetings, fulfilling Maslow’s third-stage need of “belonging.” During the ensuing years, I presented research projects, gave talks, and helped develop and lead forums and summits, thus quenching Maslow’s “self-esteem” need.
I wonder, as I leave my office to go back to see my afternoon complement of new patients, what my ninth annual meeting will bring. I’m not sure if I’ll ever achieve Maslow’s final phase of “self-actualization,” mostly because I’m not entirely sure what that means. However, I do know this: This job can be tough. We all feel it regardless of our age, gender, or practice setting. It is easy to get knocked out of balance, to get beaten down, to lose our focus. It is at those times that we all need a mariner to right the course. To remind us why we do this, to allow us to recharge, to facilitate our growth, to fulfill our needs.
For me, that mariner is the annual meeting. I look forward to seeing you all in Dallas next month. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s been one of those days. It all started at 4:30 this morning, when my 3-year-old son crawled into our bed, naked except for the diarrhea dripping down his leg. Turns out, this was his way—quite effective, I might add—of telling my wife and me that he had had an “accident.” After an hour of carrying soiled sheets to the washer, child-bathing, and Weimaraner coat-scrubbing, we relaxed to the sound of our 1-year-old daughter’s blood-curdling screams.
Upon examination, we found that the night had mysteriously transformed our precious little button-nosed bundle of joy into a tangle-haired, snot-nosed bundle of melancholy. Where her face used to be, there now hung something approximating the mask from that Scream movie. Additionally, her throat was raw, olive-sized lymph nodes populated her neck, and her nose had taken to perpetual booger-manufacturing. A rapid strep swab would later reveal the culprit, but at the moment, our differential tilted toward demonic possession.
That Dripping Feeling
Moments later, my wife and I picked 6:15 a.m. as the time to discover that we both had 7 a.m. meetings and no time to drop the kids off at daycare, especially when factoring in the 10-minute “discussion” we had about who was going to drop the kids off at daycare. All of this preceded my 7:10 a.m. arrival time for the 7 o’clock meeting with a hospital executive team to discuss our HM group funding for the next year—an encounter that left me feeling as my son must have just prior to crawling into bed with us that morning.
Now 8 a.m., I had to meet with a surgeon eager to unveil his “great idea” for our hospitalists to admit all of his patients. “It solves our problem of no interns, and allows you to play a meaningful role in the hospital!” he exclaimed.
“The meaningful role of intern?” I replied. Again, I had that dripping feeling.
It was 8:30 a.m. and I was ready to round on my patients. The first patient, a lovely woman, was stricken with un-insure-ia and a deep-seated belief that the inequitable health system that rendered her unable to get her surgery was clearly the result of some moral failing on my part. Next up was a spectacularly intoxicated male who welcomed my caring touch by belching a bit of breakfast burrito onto my cheek. Then it was a floridly bipolar patient whose apparent life mission was to drop her pants to show me her new mesh thong.
Burnout, Respect, Satisfaction
And so it continued until 1 p.m., when I had a meeting with a resident mentee of mine. It turns out that he wanted to tell me that despite his desire to be a hospitalist since his fourth year of medical school, he instead was going to apply to a rheumatology fellowship. After talking to several practicing hospitalists, he’d decided it just wasn’t for him—discussions he summarized as too much burnout, too little respect, and not enough satisfaction. Again, that dripping feeling.
Stuffing my face with a vending-machine carb-load that doubled as both breakfast and lunch, I sat down for a few minutes of e-mail. First up, a journal rejection of a research paper we’d recently submitted. Oh, the fulfillment of academics. Next were two e-mails that enzymatically trebled my “to do” list for the day. Sandwiched between those e-mails and one from a friend reminding me not to be late for a dinner that night that I was clearly going to be late for was an e-mail from a nice-appearing Nigerian man wanting to give me millions of dollars; at last, my day was turning around.
Alas, this was not the case. Checking my voicemail, I found out that my uncle was in the hospital, my dog’s lab tests were abnormal, my mom was angry about something, and I had missed a dentist appointment that morning. Finally, our group assistant came with a message that our prized hospitalist recruit had accepted a job at another institution. Drip … drip … drip…
Self-Reflection
Now 2:30 p.m., I took stock of my day and reflected on what my resident mentee had said about hospitalists. Trying to balance the rigors of patient care, academic requirements, life, friends, family, and being a boss, I was most definitely feeling a bit downtrodden, unsated, and crispy around the edges. What, exactly, did I like about this job? Was this what I wanted professionally? Would I ever find balance? Perhaps, too, a rheumatology application could salve my problems.
It was at that point that the notice for the SHM annual meeting appeared, oracle-like, on my desk. Picking it up, I realized this, not a two-year sojourn through the world of creaky joints, was the tonic to my problems.
Meeting Hierarchy
Every year since I began going to the SHM annual meeting in 2003, the meeting has helped me rejuvenate and grow. Much like Maslow’s Hierarchy of Needs, which posits that humans develop in stages that build on each other, I’ve found stepwise growth in the annual meeting.
Before my first meeting, I had been wandering nomadically through a hospitalist job for three years, wondering what, exactly, I was doing. I was the only hospitalist in my group, had few days off, with no support system around me. I had just agreed to take a job at another institution to build a new 10-person hospitalist group and had no idea how to do this. In Maslow terms, I was trying to satisfy my “physiologic needs” to survive. I needed to find, metaphorically, “food, water, clothes, and shelter.”
I found them at the annual meeting. The practice-management pre-course taught me how to build a hospitalist group, the mentorship breakfast introduced me to a veteran I still turn to, and the educational offerings helped improve my patient-care skills. I had conquered the base of Maslow’s pyramid.
The next year, I became involved in an SHM committee, and our gathering at the annual meeting helped set the course for our group’s future endeavors. I also met up with many friends I hadn’t seen since medical school and even recruited a person to my new group. In Maslow-speak, the meeting was helping me achieve my “safety needs” by providing control, well-being, and predictability.
By the third year, I was beginning to look forward to meeting up with national colleagues I had met at prior annual meetings, fulfilling Maslow’s third-stage need of “belonging.” During the ensuing years, I presented research projects, gave talks, and helped develop and lead forums and summits, thus quenching Maslow’s “self-esteem” need.
I wonder, as I leave my office to go back to see my afternoon complement of new patients, what my ninth annual meeting will bring. I’m not sure if I’ll ever achieve Maslow’s final phase of “self-actualization,” mostly because I’m not entirely sure what that means. However, I do know this: This job can be tough. We all feel it regardless of our age, gender, or practice setting. It is easy to get knocked out of balance, to get beaten down, to lose our focus. It is at those times that we all need a mariner to right the course. To remind us why we do this, to allow us to recharge, to facilitate our growth, to fulfill our needs.
For me, that mariner is the annual meeting. I look forward to seeing you all in Dallas next month. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.