User login
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
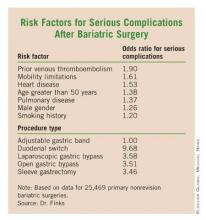
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION