User login
COLORADO SPRINGS – Implementation of a comprehensive blood conservation algorithm in a community hospital cardiac surgery program led to a 41% reduction in total blood product usage with no adverse impact on safety, a study has shown.
The blood conservation strategy included lowering the postoperative hemoglobin threshold for transfusion to less than 7 g/dL, utilizing a miniature low prime perfusion circuit in patients on cardiopulmonary bypass, intraoperative point-of-care testing to avoid inappropriate RBC and component transfusion, and routine blood withdrawal and storage before bypass and transfusion after protamine administration, Dr. Steve Xydas explained at the annual meeting of the Western Thoracic Surgical Association.
Blood transfusions in patients undergoing cardiac surgery use 15%-20% of the nation’s blood supply.
At present the indications for transfusion aren’t standardized, and there is wide disparity in transfusion rates among cardiac surgery patients, noted Dr. Xydas of Morristown (N.J.) Medical Center (formerly Morristown Memorial Hospital).
For these reasons, he and the other three cardiac surgeons at the hospital decided to push for implementation of a comprehensive blood conservation program.
They prospectively collected data on 481 patients who underwent cardiac surgery during the 6 months prior to introduction of the program. Then, following a 3-month introductory program implementation period, they collected data for 6 months on the 557 patients whose surgery was performed under the new blood transfusion strategy.
Fifty-seven percent of the 1,038 patients underwent isolated coronary artery bypass grafting, 25% had isolated valve surgery, and 18% had both.
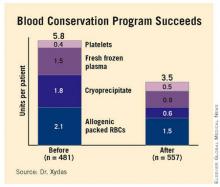
Total blood product usage (defined as the sum of blood, platelets, cryoprecipitate or fresh frozen plasma units) dropped from an average of 5.8 U per patient during the baseline period to 3.5 U per patient following introduction of the program.
Overall 30-day mortality was 1.3%, with no significant difference between the two groups. Nor were there differences in any major morbidity end points, including stroke, reoperation for bleeding, new-onset atrial fibrillation, acute MI, renal failure, or sternal wound infection. Length of stay was similar in the two groups as well.
Discussant Dr. James M. Maxwell of the International Heart Institute of Montana in Missoula observed that so much evidence has accumulated regarding the multiple harmful effects of transfusion that the current thrust is a search for meaningful evidence to support transfusion in the absence of life-threatening hemorrhage.
Because of transfusion’s harmful effects, he’d have expected to see significantly better outcomes in the group operated on under the blood conservation strategy. Dr. Maxwell attributed the lack of a significant difference in outcome between the two groups to the excellent surgical results the Morristown group obtained even before introducing the strategy.
In order to overcome the natural tendency to slide back into old habits, Dr. Xydas said he and his surgical colleagues make a point of sharing their updated results on a quarterly basis with staff cardiologists, pulmonologists, intensivists, and nurses.
Were there any barriers to implementation of the blood conservation program? he was asked. Dr. Xydas replied that this was a cardiac surgeon–led project; he and his surgical colleagues laid the groundwork by leading grand rounds for nonsurgeons in order to convince them the program was a good idea. There was occasional early resistance based on a physician’s anecdotal experience – for example, having encountered a single case of ischemic optic neuritis several decades earlier – but such reservations were easily overcome by presenting hard data on the harmful effects of transfusion, he said.
Dr. Xydas said he had no relevant financial disclosures.
COLORADO SPRINGS – Implementation of a comprehensive blood conservation algorithm in a community hospital cardiac surgery program led to a 41% reduction in total blood product usage with no adverse impact on safety, a study has shown.
The blood conservation strategy included lowering the postoperative hemoglobin threshold for transfusion to less than 7 g/dL, utilizing a miniature low prime perfusion circuit in patients on cardiopulmonary bypass, intraoperative point-of-care testing to avoid inappropriate RBC and component transfusion, and routine blood withdrawal and storage before bypass and transfusion after protamine administration, Dr. Steve Xydas explained at the annual meeting of the Western Thoracic Surgical Association.
Blood transfusions in patients undergoing cardiac surgery use 15%-20% of the nation’s blood supply.
At present the indications for transfusion aren’t standardized, and there is wide disparity in transfusion rates among cardiac surgery patients, noted Dr. Xydas of Morristown (N.J.) Medical Center (formerly Morristown Memorial Hospital).
For these reasons, he and the other three cardiac surgeons at the hospital decided to push for implementation of a comprehensive blood conservation program.
They prospectively collected data on 481 patients who underwent cardiac surgery during the 6 months prior to introduction of the program. Then, following a 3-month introductory program implementation period, they collected data for 6 months on the 557 patients whose surgery was performed under the new blood transfusion strategy.
Fifty-seven percent of the 1,038 patients underwent isolated coronary artery bypass grafting, 25% had isolated valve surgery, and 18% had both.
Total blood product usage (defined as the sum of blood, platelets, cryoprecipitate or fresh frozen plasma units) dropped from an average of 5.8 U per patient during the baseline period to 3.5 U per patient following introduction of the program.
Overall 30-day mortality was 1.3%, with no significant difference between the two groups. Nor were there differences in any major morbidity end points, including stroke, reoperation for bleeding, new-onset atrial fibrillation, acute MI, renal failure, or sternal wound infection. Length of stay was similar in the two groups as well.
Discussant Dr. James M. Maxwell of the International Heart Institute of Montana in Missoula observed that so much evidence has accumulated regarding the multiple harmful effects of transfusion that the current thrust is a search for meaningful evidence to support transfusion in the absence of life-threatening hemorrhage.
Because of transfusion’s harmful effects, he’d have expected to see significantly better outcomes in the group operated on under the blood conservation strategy. Dr. Maxwell attributed the lack of a significant difference in outcome between the two groups to the excellent surgical results the Morristown group obtained even before introducing the strategy.
In order to overcome the natural tendency to slide back into old habits, Dr. Xydas said he and his surgical colleagues make a point of sharing their updated results on a quarterly basis with staff cardiologists, pulmonologists, intensivists, and nurses.
Were there any barriers to implementation of the blood conservation program? he was asked. Dr. Xydas replied that this was a cardiac surgeon–led project; he and his surgical colleagues laid the groundwork by leading grand rounds for nonsurgeons in order to convince them the program was a good idea. There was occasional early resistance based on a physician’s anecdotal experience – for example, having encountered a single case of ischemic optic neuritis several decades earlier – but such reservations were easily overcome by presenting hard data on the harmful effects of transfusion, he said.
Dr. Xydas said he had no relevant financial disclosures.
COLORADO SPRINGS – Implementation of a comprehensive blood conservation algorithm in a community hospital cardiac surgery program led to a 41% reduction in total blood product usage with no adverse impact on safety, a study has shown.
The blood conservation strategy included lowering the postoperative hemoglobin threshold for transfusion to less than 7 g/dL, utilizing a miniature low prime perfusion circuit in patients on cardiopulmonary bypass, intraoperative point-of-care testing to avoid inappropriate RBC and component transfusion, and routine blood withdrawal and storage before bypass and transfusion after protamine administration, Dr. Steve Xydas explained at the annual meeting of the Western Thoracic Surgical Association.
Blood transfusions in patients undergoing cardiac surgery use 15%-20% of the nation’s blood supply.
At present the indications for transfusion aren’t standardized, and there is wide disparity in transfusion rates among cardiac surgery patients, noted Dr. Xydas of Morristown (N.J.) Medical Center (formerly Morristown Memorial Hospital).
For these reasons, he and the other three cardiac surgeons at the hospital decided to push for implementation of a comprehensive blood conservation program.
They prospectively collected data on 481 patients who underwent cardiac surgery during the 6 months prior to introduction of the program. Then, following a 3-month introductory program implementation period, they collected data for 6 months on the 557 patients whose surgery was performed under the new blood transfusion strategy.
Fifty-seven percent of the 1,038 patients underwent isolated coronary artery bypass grafting, 25% had isolated valve surgery, and 18% had both.
Total blood product usage (defined as the sum of blood, platelets, cryoprecipitate or fresh frozen plasma units) dropped from an average of 5.8 U per patient during the baseline period to 3.5 U per patient following introduction of the program.
Overall 30-day mortality was 1.3%, with no significant difference between the two groups. Nor were there differences in any major morbidity end points, including stroke, reoperation for bleeding, new-onset atrial fibrillation, acute MI, renal failure, or sternal wound infection. Length of stay was similar in the two groups as well.
Discussant Dr. James M. Maxwell of the International Heart Institute of Montana in Missoula observed that so much evidence has accumulated regarding the multiple harmful effects of transfusion that the current thrust is a search for meaningful evidence to support transfusion in the absence of life-threatening hemorrhage.
Because of transfusion’s harmful effects, he’d have expected to see significantly better outcomes in the group operated on under the blood conservation strategy. Dr. Maxwell attributed the lack of a significant difference in outcome between the two groups to the excellent surgical results the Morristown group obtained even before introducing the strategy.
In order to overcome the natural tendency to slide back into old habits, Dr. Xydas said he and his surgical colleagues make a point of sharing their updated results on a quarterly basis with staff cardiologists, pulmonologists, intensivists, and nurses.
Were there any barriers to implementation of the blood conservation program? he was asked. Dr. Xydas replied that this was a cardiac surgeon–led project; he and his surgical colleagues laid the groundwork by leading grand rounds for nonsurgeons in order to convince them the program was a good idea. There was occasional early resistance based on a physician’s anecdotal experience – for example, having encountered a single case of ischemic optic neuritis several decades earlier – but such reservations were easily overcome by presenting hard data on the harmful effects of transfusion, he said.
Dr. Xydas said he had no relevant financial disclosures.
Major Finding: Use of a blood conservation algorithm reduced total blood product usage from an average of 5.8 U per patient at baseline to 3.5 U per patient, without compromising safety.
Data Source: Prospective study of 1,038 patients undergoing isolated coronary artery bypass grafting.
Disclosures: Dr. Xydas said he had no relevant financial disclosures.