Display Headline
Clinical Challenges - February 2017
What's Your Diagnosis?
The Diagnosis
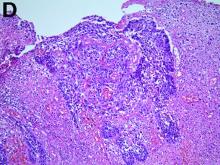
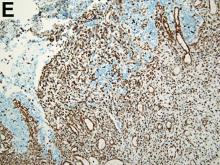
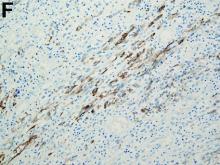
The operative specimen microscopically harbors moderately differentiated squamous carcinomatous (the central nest) as well as sarcomatous (the remainder of the field) components with a transitional zone (Figure D). This composite feature is compatible with that of carcinosarcoma of the esophagus. Immune staining with vimentin is strongly and diffusely positive only in the mesenchymal element (Figure E), whereas staining with cytokeratin AE1/AE3 is positive not only for the epithelial component, but also for spindle-shaped cells (Figure F), suggesting evidence for gradual dedifferentiation of squamous carcinomatous cells into sarcomatous cells.
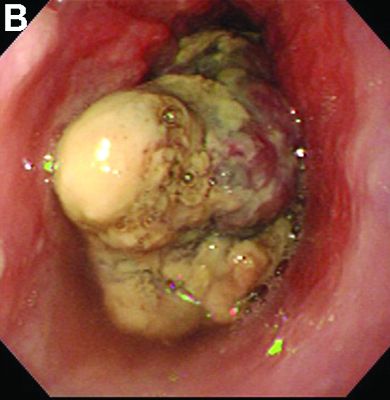
Carcinosarcoma is a rare malignant entity, representing less than 2% of all esophageal neoplasms. It usually shows a bulky appearance of an intraluminal polypoid lesion owing to predominant sarcomatous development with little stromal proliferation.
The exophytic intramurally growing tumors should include this disease in the differential diagnosis. Recent studies have supported the metaplastic theory regarding oncogenesis, whereas the collision concept has fallen out of favor; therefore, most esophageal carcinosarcomas are classified into so-called carcinosarcoma.1 It has such short doubling time that it can clinically contribute to rapid growth and give early symptoms. This allows for earlier detection and treatment; therefore, this tumor was previously believed to carry a favorable prognosis despite its size, as in the case reported herein. However, current reports have shown the converse result that this earlier detection may not translate to a better outcome.2 The sarcomatous component may accompany late metastasis targeting the liver as well as peritoneal and pleural surfaces. Treatment of this disease does not differ from that of other malignancies in the esophagus. Early detection and diagnosis, followed by operative resection, remains the mainstay for this entity to produce significant long-term survival.
References
1. Hung J.J., Li A.F., Liu J.S., et al. Esophageal carcinosarcoma with basaloid squamous cell carcinoma and osteosarcoma. Ann Thorac Surg. 2008;85[3]:1102-4.
2. Madan A.K., Long A.E., Weldon C.B., et al. Esophageal carcinosarcoma. J Gastrointest Surg. 2001;5[4]:414-7.
The Diagnosis
The operative specimen microscopically harbors moderately differentiated squamous carcinomatous (the central nest) as well as sarcomatous (the remainder of the field) components with a transitional zone (Figure D). This composite feature is compatible with that of carcinosarcoma of the esophagus. Immune staining with vimentin is strongly and diffusely positive only in the mesenchymal element (Figure E), whereas staining with cytokeratin AE1/AE3 is positive not only for the epithelial component, but also for spindle-shaped cells (Figure F), suggesting evidence for gradual dedifferentiation of squamous carcinomatous cells into sarcomatous cells.
Carcinosarcoma is a rare malignant entity, representing less than 2% of all esophageal neoplasms. It usually shows a bulky appearance of an intraluminal polypoid lesion owing to predominant sarcomatous development with little stromal proliferation.
The exophytic intramurally growing tumors should include this disease in the differential diagnosis. Recent studies have supported the metaplastic theory regarding oncogenesis, whereas the collision concept has fallen out of favor; therefore, most esophageal carcinosarcomas are classified into so-called carcinosarcoma.1 It has such short doubling time that it can clinically contribute to rapid growth and give early symptoms. This allows for earlier detection and treatment; therefore, this tumor was previously believed to carry a favorable prognosis despite its size, as in the case reported herein. However, current reports have shown the converse result that this earlier detection may not translate to a better outcome.2 The sarcomatous component may accompany late metastasis targeting the liver as well as peritoneal and pleural surfaces. Treatment of this disease does not differ from that of other malignancies in the esophagus. Early detection and diagnosis, followed by operative resection, remains the mainstay for this entity to produce significant long-term survival.
References
1. Hung J.J., Li A.F., Liu J.S., et al. Esophageal carcinosarcoma with basaloid squamous cell carcinoma and osteosarcoma. Ann Thorac Surg. 2008;85[3]:1102-4.
2. Madan A.K., Long A.E., Weldon C.B., et al. Esophageal carcinosarcoma. J Gastrointest Surg. 2001;5[4]:414-7.
The Diagnosis
The operative specimen microscopically harbors moderately differentiated squamous carcinomatous (the central nest) as well as sarcomatous (the remainder of the field) components with a transitional zone (Figure D). This composite feature is compatible with that of carcinosarcoma of the esophagus. Immune staining with vimentin is strongly and diffusely positive only in the mesenchymal element (Figure E), whereas staining with cytokeratin AE1/AE3 is positive not only for the epithelial component, but also for spindle-shaped cells (Figure F), suggesting evidence for gradual dedifferentiation of squamous carcinomatous cells into sarcomatous cells.
Carcinosarcoma is a rare malignant entity, representing less than 2% of all esophageal neoplasms. It usually shows a bulky appearance of an intraluminal polypoid lesion owing to predominant sarcomatous development with little stromal proliferation.
The exophytic intramurally growing tumors should include this disease in the differential diagnosis. Recent studies have supported the metaplastic theory regarding oncogenesis, whereas the collision concept has fallen out of favor; therefore, most esophageal carcinosarcomas are classified into so-called carcinosarcoma.1 It has such short doubling time that it can clinically contribute to rapid growth and give early symptoms. This allows for earlier detection and treatment; therefore, this tumor was previously believed to carry a favorable prognosis despite its size, as in the case reported herein. However, current reports have shown the converse result that this earlier detection may not translate to a better outcome.2 The sarcomatous component may accompany late metastasis targeting the liver as well as peritoneal and pleural surfaces. Treatment of this disease does not differ from that of other malignancies in the esophagus. Early detection and diagnosis, followed by operative resection, remains the mainstay for this entity to produce significant long-term survival.
References
1. Hung J.J., Li A.F., Liu J.S., et al. Esophageal carcinosarcoma with basaloid squamous cell carcinoma and osteosarcoma. Ann Thorac Surg. 2008;85[3]:1102-4.
2. Madan A.K., Long A.E., Weldon C.B., et al. Esophageal carcinosarcoma. J Gastrointest Surg. 2001;5[4]:414-7.
Display Headline
Clinical Challenges - February 2017
What's Your Diagnosis?
Display Headline
Clinical Challenges - February 2017
What's Your Diagnosis?
Content Gating
No Gating (article Unlocked/Free)