User login
Should hospitalist compensation increase automatically based on how long the physician has been in the practice (i.e., tenure)? Should hospitalist compensation have a cost-of-living provision, in which compensation goes up based on some external measure, such as the consumer price index?
I’m in favor of ever-increasing hospitalist incomes, including mine. And, fortunately, surveys done by SHM and others show hospitalist incomes have been increasing much faster than the cost of living. A portion of this increase can be explained by inflation and the fact that the average productivity for a full-time hospitalist has been increasing. We’re either working harder or more efficiently, but either way, the average full-time hospitalist is seeing more billable encounters than ever before.
But inflation and workload account for only a portion of the historical increase in hospitalist salaries. Market forces—principally, the demand for hospitalists exceeding the supply—probably are the biggest factors leading to rising salaries.
When Is a Hospitalist Most Valuable?
In this column, I’m going to discuss compensation philosophy for standard work as a staff hospitalist. That is mostly direct patient care, with the typical amount of such additional work as committee participation, protocol development, etc. A hospitalist who takes on a new role, such as group leader, medical director of the quality department, chief medical officer, etc., should expect his or her salary to change as a result of the promotion, and I’m excluding that situation from this article.
So back to my original question. If surveys demonstrate hospitalist salaries are increasing, then it is reasonable for your practice to ensure your hospitalist salaries keep up with established market rates. But independent of changes in the market, should hospitalist salaries in your group go up based on years of service in the group or years of experience as a hospitalist, even if some of that time was in another practice?
There are a number of ways to approach this question, but for me the key question is, at what point in an HM career is the hospitalist most valuable to the practice? Is it the first year out of residency? What about five years into your practice as a hospitalist? Maybe 10 years? Longer? I think it makes the most sense for salary to increase as long as the hospitalist’s value to the practice is increasing, but routine increases beyond that probably don’t make sense.
A hospitalist straight out of residency is almost always less valuable than someone with experience in your practice. But one point of view is that the new residency grad usually catches up to experienced hospitalists within six to 18 months. This is often followed by a long plateau phase, and, eventually, some of the more “senior” physicians become a little less valuable than those with just a few years of experience. One orthopedist told me, “New hospitalists are so eager to help and are flexible and are committed to the success of the team. But after a while, a lot of them tend to ossify and become more difficult to work with.”
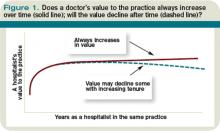
For very understandable reasons, physicians who are more established in their careers could have less scheduling flexibility and might be less willing to adjust their scope of practice to take on new roles. Some senior hospitalists—like doctors in any specialty—lose value if they don’t adequately keep up with advances in medicine. Offsetting this potential decline in value with tenure are the increase in institutional knowledge as well as relationships that a hospitalist develops by staying in the same practice for years (see Figure 1).
This point of view matches a compensation structure that might have a new residency grad start at a lower salary that increases to the “mature” level after 12 to 18 months, and remains there without future tenure-based increases—that is, a single step up in salary based on tenure. I think this makes sense for most practices.
Exceptions to the Rule
I can think of two reasonably common situations in which a group might deviate from a single tenure-based salary increase. The first is private groups in which the physicians are the contractual owners of their practice (i.e., they’re employed by a corporation they own, and not employed by the hospital or another large entity). In this structure, new physicians typically have a lower salary until they become a partner, usually after a year or two with the group. Becoming partner could require buying into the practice with tens of thousands of dollars, and might include the opportunity to share in future profit distributions. (Although buying into physician practices has been a common and appropriate model for decades, I think a new hospitalist should think carefully about whether what they will own after buying in is really worth the cost of the buy-in.)
Another exception is when hospitalists are part of a large multi-specialty physician group that offers multiple tenure-based salary increases for all physicians in all specialties. It probably makes sense to structure the hospitalist compensation plan the same way. But remember, it might take several years for primary-care physicians and surgeons to build robust patient populations and referral streams, and annual increases in salary for the first five years might mirror the pace by which a typical doctor builds his or her practice.
A new hospitalist, even one just out of residency, has an essentially mature referral stream within days of starting. So a five-year, tenure-based increase in salary could look more like the practice is simply underpaying the hospitalist until their fifth anniversary with the practice.
Automatic Increases
Some hospitalists have automatic cost-of-living salary increases. In some cases, the increases are tied to an external benchmark (e.g., the consumer price index), but it is probably more common that the future increase is simply estimated and compensation is contractually assured of increasing by a few percentage points annually.
Most hospitalists don’t have such a provision in their contracts. Indeed, most working Americans with salaries in the hospitalist range and higher don’t have cost-of-living increases. Instead, future salary adjustments are made based on market data, such as the results of salary surveys. TH
Dr. Nelson has been a hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Should hospitalist compensation increase automatically based on how long the physician has been in the practice (i.e., tenure)? Should hospitalist compensation have a cost-of-living provision, in which compensation goes up based on some external measure, such as the consumer price index?
I’m in favor of ever-increasing hospitalist incomes, including mine. And, fortunately, surveys done by SHM and others show hospitalist incomes have been increasing much faster than the cost of living. A portion of this increase can be explained by inflation and the fact that the average productivity for a full-time hospitalist has been increasing. We’re either working harder or more efficiently, but either way, the average full-time hospitalist is seeing more billable encounters than ever before.
But inflation and workload account for only a portion of the historical increase in hospitalist salaries. Market forces—principally, the demand for hospitalists exceeding the supply—probably are the biggest factors leading to rising salaries.
When Is a Hospitalist Most Valuable?
In this column, I’m going to discuss compensation philosophy for standard work as a staff hospitalist. That is mostly direct patient care, with the typical amount of such additional work as committee participation, protocol development, etc. A hospitalist who takes on a new role, such as group leader, medical director of the quality department, chief medical officer, etc., should expect his or her salary to change as a result of the promotion, and I’m excluding that situation from this article.
So back to my original question. If surveys demonstrate hospitalist salaries are increasing, then it is reasonable for your practice to ensure your hospitalist salaries keep up with established market rates. But independent of changes in the market, should hospitalist salaries in your group go up based on years of service in the group or years of experience as a hospitalist, even if some of that time was in another practice?
There are a number of ways to approach this question, but for me the key question is, at what point in an HM career is the hospitalist most valuable to the practice? Is it the first year out of residency? What about five years into your practice as a hospitalist? Maybe 10 years? Longer? I think it makes the most sense for salary to increase as long as the hospitalist’s value to the practice is increasing, but routine increases beyond that probably don’t make sense.
A hospitalist straight out of residency is almost always less valuable than someone with experience in your practice. But one point of view is that the new residency grad usually catches up to experienced hospitalists within six to 18 months. This is often followed by a long plateau phase, and, eventually, some of the more “senior” physicians become a little less valuable than those with just a few years of experience. One orthopedist told me, “New hospitalists are so eager to help and are flexible and are committed to the success of the team. But after a while, a lot of them tend to ossify and become more difficult to work with.”
For very understandable reasons, physicians who are more established in their careers could have less scheduling flexibility and might be less willing to adjust their scope of practice to take on new roles. Some senior hospitalists—like doctors in any specialty—lose value if they don’t adequately keep up with advances in medicine. Offsetting this potential decline in value with tenure are the increase in institutional knowledge as well as relationships that a hospitalist develops by staying in the same practice for years (see Figure 1).
This point of view matches a compensation structure that might have a new residency grad start at a lower salary that increases to the “mature” level after 12 to 18 months, and remains there without future tenure-based increases—that is, a single step up in salary based on tenure. I think this makes sense for most practices.
Exceptions to the Rule
I can think of two reasonably common situations in which a group might deviate from a single tenure-based salary increase. The first is private groups in which the physicians are the contractual owners of their practice (i.e., they’re employed by a corporation they own, and not employed by the hospital or another large entity). In this structure, new physicians typically have a lower salary until they become a partner, usually after a year or two with the group. Becoming partner could require buying into the practice with tens of thousands of dollars, and might include the opportunity to share in future profit distributions. (Although buying into physician practices has been a common and appropriate model for decades, I think a new hospitalist should think carefully about whether what they will own after buying in is really worth the cost of the buy-in.)
Another exception is when hospitalists are part of a large multi-specialty physician group that offers multiple tenure-based salary increases for all physicians in all specialties. It probably makes sense to structure the hospitalist compensation plan the same way. But remember, it might take several years for primary-care physicians and surgeons to build robust patient populations and referral streams, and annual increases in salary for the first five years might mirror the pace by which a typical doctor builds his or her practice.
A new hospitalist, even one just out of residency, has an essentially mature referral stream within days of starting. So a five-year, tenure-based increase in salary could look more like the practice is simply underpaying the hospitalist until their fifth anniversary with the practice.
Automatic Increases
Some hospitalists have automatic cost-of-living salary increases. In some cases, the increases are tied to an external benchmark (e.g., the consumer price index), but it is probably more common that the future increase is simply estimated and compensation is contractually assured of increasing by a few percentage points annually.
Most hospitalists don’t have such a provision in their contracts. Indeed, most working Americans with salaries in the hospitalist range and higher don’t have cost-of-living increases. Instead, future salary adjustments are made based on market data, such as the results of salary surveys. TH
Dr. Nelson has been a hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Should hospitalist compensation increase automatically based on how long the physician has been in the practice (i.e., tenure)? Should hospitalist compensation have a cost-of-living provision, in which compensation goes up based on some external measure, such as the consumer price index?
I’m in favor of ever-increasing hospitalist incomes, including mine. And, fortunately, surveys done by SHM and others show hospitalist incomes have been increasing much faster than the cost of living. A portion of this increase can be explained by inflation and the fact that the average productivity for a full-time hospitalist has been increasing. We’re either working harder or more efficiently, but either way, the average full-time hospitalist is seeing more billable encounters than ever before.
But inflation and workload account for only a portion of the historical increase in hospitalist salaries. Market forces—principally, the demand for hospitalists exceeding the supply—probably are the biggest factors leading to rising salaries.
When Is a Hospitalist Most Valuable?
In this column, I’m going to discuss compensation philosophy for standard work as a staff hospitalist. That is mostly direct patient care, with the typical amount of such additional work as committee participation, protocol development, etc. A hospitalist who takes on a new role, such as group leader, medical director of the quality department, chief medical officer, etc., should expect his or her salary to change as a result of the promotion, and I’m excluding that situation from this article.
So back to my original question. If surveys demonstrate hospitalist salaries are increasing, then it is reasonable for your practice to ensure your hospitalist salaries keep up with established market rates. But independent of changes in the market, should hospitalist salaries in your group go up based on years of service in the group or years of experience as a hospitalist, even if some of that time was in another practice?
There are a number of ways to approach this question, but for me the key question is, at what point in an HM career is the hospitalist most valuable to the practice? Is it the first year out of residency? What about five years into your practice as a hospitalist? Maybe 10 years? Longer? I think it makes the most sense for salary to increase as long as the hospitalist’s value to the practice is increasing, but routine increases beyond that probably don’t make sense.
A hospitalist straight out of residency is almost always less valuable than someone with experience in your practice. But one point of view is that the new residency grad usually catches up to experienced hospitalists within six to 18 months. This is often followed by a long plateau phase, and, eventually, some of the more “senior” physicians become a little less valuable than those with just a few years of experience. One orthopedist told me, “New hospitalists are so eager to help and are flexible and are committed to the success of the team. But after a while, a lot of them tend to ossify and become more difficult to work with.”
For very understandable reasons, physicians who are more established in their careers could have less scheduling flexibility and might be less willing to adjust their scope of practice to take on new roles. Some senior hospitalists—like doctors in any specialty—lose value if they don’t adequately keep up with advances in medicine. Offsetting this potential decline in value with tenure are the increase in institutional knowledge as well as relationships that a hospitalist develops by staying in the same practice for years (see Figure 1).
This point of view matches a compensation structure that might have a new residency grad start at a lower salary that increases to the “mature” level after 12 to 18 months, and remains there without future tenure-based increases—that is, a single step up in salary based on tenure. I think this makes sense for most practices.
Exceptions to the Rule
I can think of two reasonably common situations in which a group might deviate from a single tenure-based salary increase. The first is private groups in which the physicians are the contractual owners of their practice (i.e., they’re employed by a corporation they own, and not employed by the hospital or another large entity). In this structure, new physicians typically have a lower salary until they become a partner, usually after a year or two with the group. Becoming partner could require buying into the practice with tens of thousands of dollars, and might include the opportunity to share in future profit distributions. (Although buying into physician practices has been a common and appropriate model for decades, I think a new hospitalist should think carefully about whether what they will own after buying in is really worth the cost of the buy-in.)
Another exception is when hospitalists are part of a large multi-specialty physician group that offers multiple tenure-based salary increases for all physicians in all specialties. It probably makes sense to structure the hospitalist compensation plan the same way. But remember, it might take several years for primary-care physicians and surgeons to build robust patient populations and referral streams, and annual increases in salary for the first five years might mirror the pace by which a typical doctor builds his or her practice.
A new hospitalist, even one just out of residency, has an essentially mature referral stream within days of starting. So a five-year, tenure-based increase in salary could look more like the practice is simply underpaying the hospitalist until their fifth anniversary with the practice.
Automatic Increases
Some hospitalists have automatic cost-of-living salary increases. In some cases, the increases are tied to an external benchmark (e.g., the consumer price index), but it is probably more common that the future increase is simply estimated and compensation is contractually assured of increasing by a few percentage points annually.
Most hospitalists don’t have such a provision in their contracts. Indeed, most working Americans with salaries in the hospitalist range and higher don’t have cost-of-living increases. Instead, future salary adjustments are made based on market data, such as the results of salary surveys. TH
Dr. Nelson has been a hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson Flores Hospital Medicine Consultants, a national hospitalist practice management consulting firm (www.nelsonflores.com). He is also course co-director and faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.