User login
The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor (PPI) therapy, according to an updated international consensus statement published in the October issue of Gastroenterology.
“An initial rationale for the PPI trial was to distinguish eosinophilic esophagitis from gastroesophageal reflux disease, but it is now known that these conditions have a complex relationship and are not necessarily mutually exclusive,” wrote Evan S. Dellon, MD, of the University of North Carolina at Chapel Hill, and his associates. According to current evidence, “PPIs are better classified as a treatment for esophageal eosinophilia that may be due to eosinophilic esophagitis than as a diagnostic criterion,” they said.
Diagnostic guidelines for eosinophilic esophagitis were published first in 2007 and were updated in 2011. The guideline authors recommended either pH monitoring or an 8-week trial of high-dose PPI therapy to rule out inflammation from gastroesophageal reflux disease (GERD).
But subsequent publications described patients with symptomatic esophageal eosinophilia who responded to PPIs and lacked classic GERD symptoms. Guidelines called this condition “PPI-responsive esophageal eosinophilia” and considered it a separate entity from GERD.
However, an “evolving body of research” shows that eosinophilic esophagitis can overlap with GERD, Dr. Dellon and his associates wrote. Furthermore, each of these conditions can trigger the other. Eosinophilic esophagitis can decrease esophageal compliance, leading to secondary reflux, while gastroesophageal reflux can erode the esophageal epithelium, triggering antigen exposure and eosinophilia.
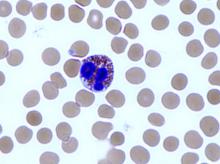
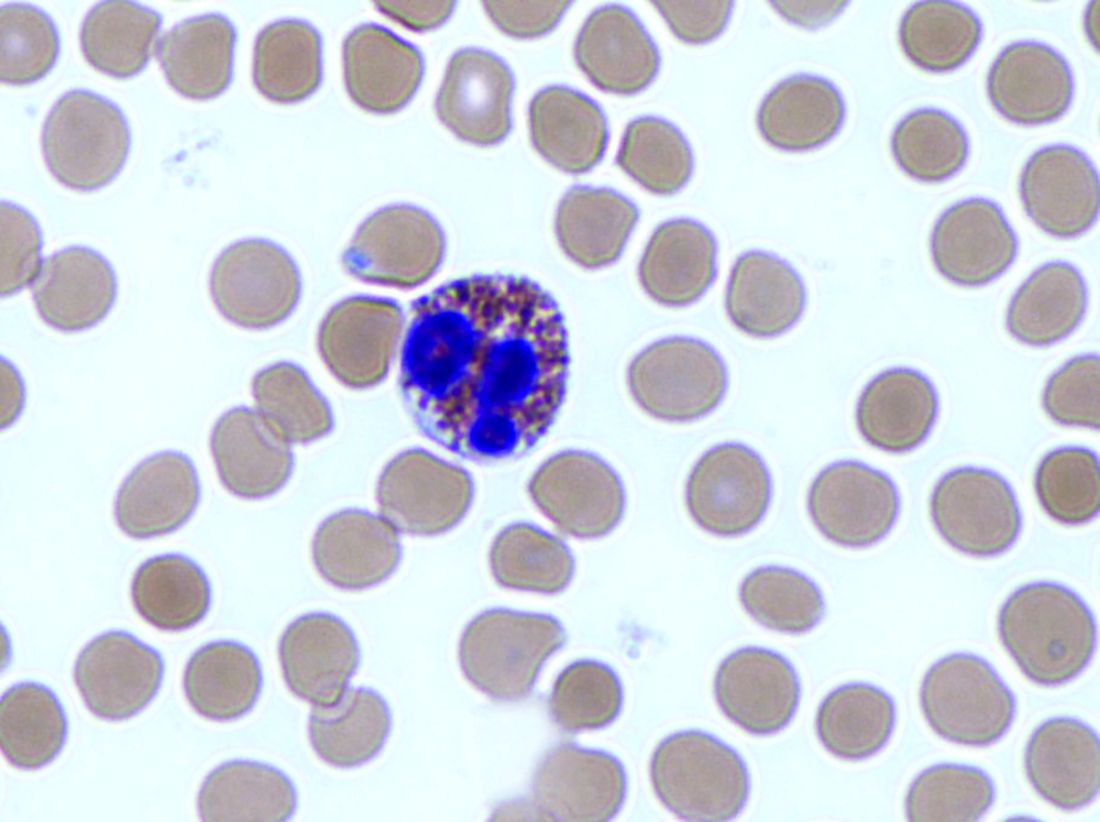
Therefore, Dr. Dellon and his associates recommended defining eosinophilic esophagitis as signs and symptoms of esophageal dysfunction and an esophageal biopsy showing at least 15 eosinophils per high-power field, or approximately 60 eosinophils per millimeter, with infiltration limited to the esophagus. They stressed the importance of esophageal biopsy even if endoscopy shows normal mucosa. “As per prior guidelines, multiple biopsies from two or more esophageal levels, targeting areas of apparent inflammation, are recommended to increase the diagnostic yield,” they added. “Gastric and duodenal biopsies should be obtained as clinically indicated by symptoms, endoscopic findings in the stomach or duodenum, or high index of suspicion for a mucosal process.”
Physicians should increase their suspicion of eosinophilic esophagitis if patients have other types of atopy or endoscopic findings of “rings, furrows, exudates, edema, stricture, narrowing, and crepe-paper mucosa,” they added. In addition to GERD, they recommended looking carefully for other conditions that can trigger esophageal eosinophilia, such as pemphigus, drug hypersensitivity reactions, achalasia, and Crohn’s disease with esophageal involvement.
To create the guideline, Dr. Dellon and his associates searched PubMed for studies of all designs and sizes published from 1966 through December 2016. Teams of experts on specific topics then reviewed and discussed relevant literature. In May 2017, 43 reviewers met for 8 hours to present and discuss conclusions. There was 100% agreement to remove the PPI trial from the diagnostic criteria, the experts noted.
The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, and the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships and receiving research funding from Adare, Celgene/Receptos, Regeneron, and Shire among others. The majority of his coauthors also disclosed relationships with numerous medical companies.
SOURCE: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.
Studies in the 1980s linked the presence of esophageal mucosal eosinophils with increased acid exposure on pH monitoring. For the next 2 decades, clinicians viewed eosinophils on esophageal biopsies as diagnostic for GERD such that the initial description of EoE by Attwood in 1993 distinguished EoE from GERD by the presence of esophageal eosinophilia in the absence of either reflux esophagitis or abnormal acid exposure on pH testing. Consequently, the initial diagnostic criteria for EoE in 2007 included a lack of response to PPI and/or normal pH testing to establish the diagnosis of EoE. Reflecting growing uncertainty regarding the ability of PPI therapy to differentiate acid-induced from allergic inflammatory mechanisms, an updated consensus in 2011 introduced the terminology “PPI responsive esophageal eosinophilia (PPIREE)” to describe an increasingly recognized subset of patients with suspected EoE that resolved with PPI. Now, supported by scientific evidence accumulated over the past decade, AGREE has taken a step back by removing the PPI trial from the diagnosis of EoE, thereby abandoning the PPIREE terminology. This step simplifies the diagnosis of EoE and acknowledges that a histologic response to PPI does not “rule in” GERD or “rule out” EoE. It is important to emphasize that the updated criteria still advocate careful consideration of secondary causes of esophageal eosinophilia prior to the diagnosis of EoE.
Ramifications of the updated diagnostic criteria include the opportunities for clinicians to consider use of topical corticosteroids and diet therapies, rather than mandate an up-front PPI trial, in patients with EoE. On a practical level, based on their effectiveness, safety, and ease of administration, PPIs remain positioned as a favorable initial intervention for EoE. Conceptually, however, the paradigm shift highlights the ability of research to improve our understanding of disease pathogenesis and thereby impact clinical management.
Ikuo Hirano, MD, AGAF, is in the division of gastroenterology, Northwestern University, Chicago. He has received grant support from the NIH Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR, U54 AI117804), which is part of the Rare Disease Clinical Research Network. He has received research funding and consulting fees from Celgene, Regeneron, Shire, and others.
Studies in the 1980s linked the presence of esophageal mucosal eosinophils with increased acid exposure on pH monitoring. For the next 2 decades, clinicians viewed eosinophils on esophageal biopsies as diagnostic for GERD such that the initial description of EoE by Attwood in 1993 distinguished EoE from GERD by the presence of esophageal eosinophilia in the absence of either reflux esophagitis or abnormal acid exposure on pH testing. Consequently, the initial diagnostic criteria for EoE in 2007 included a lack of response to PPI and/or normal pH testing to establish the diagnosis of EoE. Reflecting growing uncertainty regarding the ability of PPI therapy to differentiate acid-induced from allergic inflammatory mechanisms, an updated consensus in 2011 introduced the terminology “PPI responsive esophageal eosinophilia (PPIREE)” to describe an increasingly recognized subset of patients with suspected EoE that resolved with PPI. Now, supported by scientific evidence accumulated over the past decade, AGREE has taken a step back by removing the PPI trial from the diagnosis of EoE, thereby abandoning the PPIREE terminology. This step simplifies the diagnosis of EoE and acknowledges that a histologic response to PPI does not “rule in” GERD or “rule out” EoE. It is important to emphasize that the updated criteria still advocate careful consideration of secondary causes of esophageal eosinophilia prior to the diagnosis of EoE.
Ramifications of the updated diagnostic criteria include the opportunities for clinicians to consider use of topical corticosteroids and diet therapies, rather than mandate an up-front PPI trial, in patients with EoE. On a practical level, based on their effectiveness, safety, and ease of administration, PPIs remain positioned as a favorable initial intervention for EoE. Conceptually, however, the paradigm shift highlights the ability of research to improve our understanding of disease pathogenesis and thereby impact clinical management.
Ikuo Hirano, MD, AGAF, is in the division of gastroenterology, Northwestern University, Chicago. He has received grant support from the NIH Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR, U54 AI117804), which is part of the Rare Disease Clinical Research Network. He has received research funding and consulting fees from Celgene, Regeneron, Shire, and others.
Studies in the 1980s linked the presence of esophageal mucosal eosinophils with increased acid exposure on pH monitoring. For the next 2 decades, clinicians viewed eosinophils on esophageal biopsies as diagnostic for GERD such that the initial description of EoE by Attwood in 1993 distinguished EoE from GERD by the presence of esophageal eosinophilia in the absence of either reflux esophagitis or abnormal acid exposure on pH testing. Consequently, the initial diagnostic criteria for EoE in 2007 included a lack of response to PPI and/or normal pH testing to establish the diagnosis of EoE. Reflecting growing uncertainty regarding the ability of PPI therapy to differentiate acid-induced from allergic inflammatory mechanisms, an updated consensus in 2011 introduced the terminology “PPI responsive esophageal eosinophilia (PPIREE)” to describe an increasingly recognized subset of patients with suspected EoE that resolved with PPI. Now, supported by scientific evidence accumulated over the past decade, AGREE has taken a step back by removing the PPI trial from the diagnosis of EoE, thereby abandoning the PPIREE terminology. This step simplifies the diagnosis of EoE and acknowledges that a histologic response to PPI does not “rule in” GERD or “rule out” EoE. It is important to emphasize that the updated criteria still advocate careful consideration of secondary causes of esophageal eosinophilia prior to the diagnosis of EoE.
Ramifications of the updated diagnostic criteria include the opportunities for clinicians to consider use of topical corticosteroids and diet therapies, rather than mandate an up-front PPI trial, in patients with EoE. On a practical level, based on their effectiveness, safety, and ease of administration, PPIs remain positioned as a favorable initial intervention for EoE. Conceptually, however, the paradigm shift highlights the ability of research to improve our understanding of disease pathogenesis and thereby impact clinical management.
Ikuo Hirano, MD, AGAF, is in the division of gastroenterology, Northwestern University, Chicago. He has received grant support from the NIH Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR, U54 AI117804), which is part of the Rare Disease Clinical Research Network. He has received research funding and consulting fees from Celgene, Regeneron, Shire, and others.
The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor (PPI) therapy, according to an updated international consensus statement published in the October issue of Gastroenterology.
“An initial rationale for the PPI trial was to distinguish eosinophilic esophagitis from gastroesophageal reflux disease, but it is now known that these conditions have a complex relationship and are not necessarily mutually exclusive,” wrote Evan S. Dellon, MD, of the University of North Carolina at Chapel Hill, and his associates. According to current evidence, “PPIs are better classified as a treatment for esophageal eosinophilia that may be due to eosinophilic esophagitis than as a diagnostic criterion,” they said.
Diagnostic guidelines for eosinophilic esophagitis were published first in 2007 and were updated in 2011. The guideline authors recommended either pH monitoring or an 8-week trial of high-dose PPI therapy to rule out inflammation from gastroesophageal reflux disease (GERD).
But subsequent publications described patients with symptomatic esophageal eosinophilia who responded to PPIs and lacked classic GERD symptoms. Guidelines called this condition “PPI-responsive esophageal eosinophilia” and considered it a separate entity from GERD.
However, an “evolving body of research” shows that eosinophilic esophagitis can overlap with GERD, Dr. Dellon and his associates wrote. Furthermore, each of these conditions can trigger the other. Eosinophilic esophagitis can decrease esophageal compliance, leading to secondary reflux, while gastroesophageal reflux can erode the esophageal epithelium, triggering antigen exposure and eosinophilia.
Therefore, Dr. Dellon and his associates recommended defining eosinophilic esophagitis as signs and symptoms of esophageal dysfunction and an esophageal biopsy showing at least 15 eosinophils per high-power field, or approximately 60 eosinophils per millimeter, with infiltration limited to the esophagus. They stressed the importance of esophageal biopsy even if endoscopy shows normal mucosa. “As per prior guidelines, multiple biopsies from two or more esophageal levels, targeting areas of apparent inflammation, are recommended to increase the diagnostic yield,” they added. “Gastric and duodenal biopsies should be obtained as clinically indicated by symptoms, endoscopic findings in the stomach or duodenum, or high index of suspicion for a mucosal process.”
Physicians should increase their suspicion of eosinophilic esophagitis if patients have other types of atopy or endoscopic findings of “rings, furrows, exudates, edema, stricture, narrowing, and crepe-paper mucosa,” they added. In addition to GERD, they recommended looking carefully for other conditions that can trigger esophageal eosinophilia, such as pemphigus, drug hypersensitivity reactions, achalasia, and Crohn’s disease with esophageal involvement.
To create the guideline, Dr. Dellon and his associates searched PubMed for studies of all designs and sizes published from 1966 through December 2016. Teams of experts on specific topics then reviewed and discussed relevant literature. In May 2017, 43 reviewers met for 8 hours to present and discuss conclusions. There was 100% agreement to remove the PPI trial from the diagnostic criteria, the experts noted.
The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, and the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships and receiving research funding from Adare, Celgene/Receptos, Regeneron, and Shire among others. The majority of his coauthors also disclosed relationships with numerous medical companies.
SOURCE: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.
The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor (PPI) therapy, according to an updated international consensus statement published in the October issue of Gastroenterology.
“An initial rationale for the PPI trial was to distinguish eosinophilic esophagitis from gastroesophageal reflux disease, but it is now known that these conditions have a complex relationship and are not necessarily mutually exclusive,” wrote Evan S. Dellon, MD, of the University of North Carolina at Chapel Hill, and his associates. According to current evidence, “PPIs are better classified as a treatment for esophageal eosinophilia that may be due to eosinophilic esophagitis than as a diagnostic criterion,” they said.
Diagnostic guidelines for eosinophilic esophagitis were published first in 2007 and were updated in 2011. The guideline authors recommended either pH monitoring or an 8-week trial of high-dose PPI therapy to rule out inflammation from gastroesophageal reflux disease (GERD).
But subsequent publications described patients with symptomatic esophageal eosinophilia who responded to PPIs and lacked classic GERD symptoms. Guidelines called this condition “PPI-responsive esophageal eosinophilia” and considered it a separate entity from GERD.
However, an “evolving body of research” shows that eosinophilic esophagitis can overlap with GERD, Dr. Dellon and his associates wrote. Furthermore, each of these conditions can trigger the other. Eosinophilic esophagitis can decrease esophageal compliance, leading to secondary reflux, while gastroesophageal reflux can erode the esophageal epithelium, triggering antigen exposure and eosinophilia.
Therefore, Dr. Dellon and his associates recommended defining eosinophilic esophagitis as signs and symptoms of esophageal dysfunction and an esophageal biopsy showing at least 15 eosinophils per high-power field, or approximately 60 eosinophils per millimeter, with infiltration limited to the esophagus. They stressed the importance of esophageal biopsy even if endoscopy shows normal mucosa. “As per prior guidelines, multiple biopsies from two or more esophageal levels, targeting areas of apparent inflammation, are recommended to increase the diagnostic yield,” they added. “Gastric and duodenal biopsies should be obtained as clinically indicated by symptoms, endoscopic findings in the stomach or duodenum, or high index of suspicion for a mucosal process.”
Physicians should increase their suspicion of eosinophilic esophagitis if patients have other types of atopy or endoscopic findings of “rings, furrows, exudates, edema, stricture, narrowing, and crepe-paper mucosa,” they added. In addition to GERD, they recommended looking carefully for other conditions that can trigger esophageal eosinophilia, such as pemphigus, drug hypersensitivity reactions, achalasia, and Crohn’s disease with esophageal involvement.
To create the guideline, Dr. Dellon and his associates searched PubMed for studies of all designs and sizes published from 1966 through December 2016. Teams of experts on specific topics then reviewed and discussed relevant literature. In May 2017, 43 reviewers met for 8 hours to present and discuss conclusions. There was 100% agreement to remove the PPI trial from the diagnostic criteria, the experts noted.
The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, and the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships and receiving research funding from Adare, Celgene/Receptos, Regeneron, and Shire among others. The majority of his coauthors also disclosed relationships with numerous medical companies.
SOURCE: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.
FROM GASTROENTEROLOGY
Key clinical point: The diagnosis of eosinophilic esophagitis no longer needs to include a trial of proton pump inhibitor therapy.
Major finding: Eosinophilic esophagitis and gastroesophageal reflux disease are not mutually exclusive.
Study details: Review by an international consensus panel of studies published between 1966 and 2016.
Disclosures: The authors disclosed financial support from the International Gastrointestinal Eosinophilic Diseases Researchers (TIGERS), The David and Denise Bunning Family, the Rare Disease Clinical Research Network. Dr. Dellon disclosed consulting relationships with Adare, Allakos, Alivio, Banner, Celgene/Receptos, Enumeral, GSK, Regeneron, and Shire. He also reported receiving research funding from Adare, Celgene/Receptos, Miraca, Meritage, Nutricia, Regeneron, and Shire and educational grants from Banner and Holoclara. The majority of his coauthors disclosed relationships with numerous medical companies.
Source: Dellon ES et al. Gastroenterology. 2018 Jul 12. doi: 10.1053/j.gastro.2018.07.009.