User login
Years ago, I struggled with a difficult decision. Given the fact that the military disallowed dual training tracks, such as internal medicine/pediatrics (med/peds), I had to choose from internal medicine (IM), pediatrics (Peds), or family practice (FP) residencies. My personal history and experiential data remained incomplete and the view ahead blurry; still, the choice remained.
Over time, I’ve embraced the uncertainty inherent in most analyses. Such is the case with the current composition of specialties that make up hospital medicine nationwide. Available data remains in flux, yet I see apparent trends.
A new question in the 2014 State of Hospital Medicine (SOHM) report asked, “Did your hospital medicine group employ hospitalist physicians trained and certified in the following specialties…?” Strikingly, a full 59% of groups serving adult patients only reported having at least one family medicine-trained provider in their midst! And in these adult-only practices, 98% of groups utilized at least one internal medicine physician, 24% reported a med/peds doc, and none reported pediatricians.
Meanwhile, of 40 groups caring for children only, 95% reported using pediatrics, 2.5% internal medicine (huh?), 22.5% med/peds, and zero FPs. The 19 groups serving both adults and children revealed participation from all four nonsurgical hospitalist specialties (IM, peds, FP, med/peds).
So what is the specialty distribution of medical hospitalists overall? There’s no good data about this.
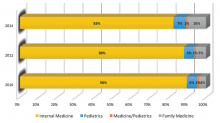
The 2014 Medical Group Management Association (MGMA) sample, licensed for use in SOHM, reported data for roughly 4,200 community hospital medicine providers: 82% were internal medicine, 10% family medicine, 7% pediatrics, and <1% med/peds. MGMA, however, cautions against assuming that this represents the entire population of hospitalists and their training. Although representative of the groups who participated in the survey, it may not be representative of groups that didn’t participate, and thus it would be misleading to suggest that this distribution holds true nationally.
In an effort to corroborate the MGMA distribution, I reviewed other compensation and productivity surveys; one such survey, conducted by the American Medical Group Association, reported hospitalists by training program. It contained over 3,700 community hospital providers—89% internal medicine, 6% family medicine, 5% pediatrics—but did not inquire about medicine/pediatrics.
Finally, if one combines the academic and community provider samples from MGMA (n=4,867), the distribution is 80% IM, 8.5% FP, 10% peds, and <1% med/peds.
Which of these, if any, is the actual distribution of nonprocedural hospitalists? Although we cannot know exactly, I believe something close to the following to be current state: internal medicine 80%, family medicine 10%, pediatrics 10%, and medicine/pediatrics <1%.
It is clear from survey trends that the proportion of family medicine providers is growing, while the internal medicine super-majority is shrinking somewhat. Pediatrics appears to remain stable as a proportion of the total, as does med/peds, with the latter unable to grow in numbers proportionally given the small number of providers nationally compared to the other three fields.
The growth of family medicine-trained hospitalists relates to the continued high demand for the profession, with such residents comprising the largest pool of available providers, second only to internal medicine.
Based on the SHM survey, family medicine hospitalists seem to practice similarly to IM; they generally see adults only. It appears that they are accepted into traditional adult hospitalist practices, readily contrasting with groups serving children, which report no FP participation. Meanwhile, med/peds hospitalists provide care across the spectrum of hospitalist groups, though they often report splitting their duties between adults-only services and pediatric services.
As for me, a generation removed from my election of a family practice internship and subsequent transition to internal medicine residency, I should not have worried so. Both paths can lead to hospital medicine.
Dr. Ahlstrom is a hospitalist at Indigo Health Partners in Traverse City, Mich., and a member of SHM’s Practice Analysis Committee.
Years ago, I struggled with a difficult decision. Given the fact that the military disallowed dual training tracks, such as internal medicine/pediatrics (med/peds), I had to choose from internal medicine (IM), pediatrics (Peds), or family practice (FP) residencies. My personal history and experiential data remained incomplete and the view ahead blurry; still, the choice remained.
Over time, I’ve embraced the uncertainty inherent in most analyses. Such is the case with the current composition of specialties that make up hospital medicine nationwide. Available data remains in flux, yet I see apparent trends.
A new question in the 2014 State of Hospital Medicine (SOHM) report asked, “Did your hospital medicine group employ hospitalist physicians trained and certified in the following specialties…?” Strikingly, a full 59% of groups serving adult patients only reported having at least one family medicine-trained provider in their midst! And in these adult-only practices, 98% of groups utilized at least one internal medicine physician, 24% reported a med/peds doc, and none reported pediatricians.
Meanwhile, of 40 groups caring for children only, 95% reported using pediatrics, 2.5% internal medicine (huh?), 22.5% med/peds, and zero FPs. The 19 groups serving both adults and children revealed participation from all four nonsurgical hospitalist specialties (IM, peds, FP, med/peds).
So what is the specialty distribution of medical hospitalists overall? There’s no good data about this.
The 2014 Medical Group Management Association (MGMA) sample, licensed for use in SOHM, reported data for roughly 4,200 community hospital medicine providers: 82% were internal medicine, 10% family medicine, 7% pediatrics, and <1% med/peds. MGMA, however, cautions against assuming that this represents the entire population of hospitalists and their training. Although representative of the groups who participated in the survey, it may not be representative of groups that didn’t participate, and thus it would be misleading to suggest that this distribution holds true nationally.
In an effort to corroborate the MGMA distribution, I reviewed other compensation and productivity surveys; one such survey, conducted by the American Medical Group Association, reported hospitalists by training program. It contained over 3,700 community hospital providers—89% internal medicine, 6% family medicine, 5% pediatrics—but did not inquire about medicine/pediatrics.
Finally, if one combines the academic and community provider samples from MGMA (n=4,867), the distribution is 80% IM, 8.5% FP, 10% peds, and <1% med/peds.
Which of these, if any, is the actual distribution of nonprocedural hospitalists? Although we cannot know exactly, I believe something close to the following to be current state: internal medicine 80%, family medicine 10%, pediatrics 10%, and medicine/pediatrics <1%.
It is clear from survey trends that the proportion of family medicine providers is growing, while the internal medicine super-majority is shrinking somewhat. Pediatrics appears to remain stable as a proportion of the total, as does med/peds, with the latter unable to grow in numbers proportionally given the small number of providers nationally compared to the other three fields.
The growth of family medicine-trained hospitalists relates to the continued high demand for the profession, with such residents comprising the largest pool of available providers, second only to internal medicine.
Based on the SHM survey, family medicine hospitalists seem to practice similarly to IM; they generally see adults only. It appears that they are accepted into traditional adult hospitalist practices, readily contrasting with groups serving children, which report no FP participation. Meanwhile, med/peds hospitalists provide care across the spectrum of hospitalist groups, though they often report splitting their duties between adults-only services and pediatric services.
As for me, a generation removed from my election of a family practice internship and subsequent transition to internal medicine residency, I should not have worried so. Both paths can lead to hospital medicine.
Dr. Ahlstrom is a hospitalist at Indigo Health Partners in Traverse City, Mich., and a member of SHM’s Practice Analysis Committee.
Years ago, I struggled with a difficult decision. Given the fact that the military disallowed dual training tracks, such as internal medicine/pediatrics (med/peds), I had to choose from internal medicine (IM), pediatrics (Peds), or family practice (FP) residencies. My personal history and experiential data remained incomplete and the view ahead blurry; still, the choice remained.
Over time, I’ve embraced the uncertainty inherent in most analyses. Such is the case with the current composition of specialties that make up hospital medicine nationwide. Available data remains in flux, yet I see apparent trends.
A new question in the 2014 State of Hospital Medicine (SOHM) report asked, “Did your hospital medicine group employ hospitalist physicians trained and certified in the following specialties…?” Strikingly, a full 59% of groups serving adult patients only reported having at least one family medicine-trained provider in their midst! And in these adult-only practices, 98% of groups utilized at least one internal medicine physician, 24% reported a med/peds doc, and none reported pediatricians.
Meanwhile, of 40 groups caring for children only, 95% reported using pediatrics, 2.5% internal medicine (huh?), 22.5% med/peds, and zero FPs. The 19 groups serving both adults and children revealed participation from all four nonsurgical hospitalist specialties (IM, peds, FP, med/peds).
So what is the specialty distribution of medical hospitalists overall? There’s no good data about this.
The 2014 Medical Group Management Association (MGMA) sample, licensed for use in SOHM, reported data for roughly 4,200 community hospital medicine providers: 82% were internal medicine, 10% family medicine, 7% pediatrics, and <1% med/peds. MGMA, however, cautions against assuming that this represents the entire population of hospitalists and their training. Although representative of the groups who participated in the survey, it may not be representative of groups that didn’t participate, and thus it would be misleading to suggest that this distribution holds true nationally.
In an effort to corroborate the MGMA distribution, I reviewed other compensation and productivity surveys; one such survey, conducted by the American Medical Group Association, reported hospitalists by training program. It contained over 3,700 community hospital providers—89% internal medicine, 6% family medicine, 5% pediatrics—but did not inquire about medicine/pediatrics.
Finally, if one combines the academic and community provider samples from MGMA (n=4,867), the distribution is 80% IM, 8.5% FP, 10% peds, and <1% med/peds.
Which of these, if any, is the actual distribution of nonprocedural hospitalists? Although we cannot know exactly, I believe something close to the following to be current state: internal medicine 80%, family medicine 10%, pediatrics 10%, and medicine/pediatrics <1%.
It is clear from survey trends that the proportion of family medicine providers is growing, while the internal medicine super-majority is shrinking somewhat. Pediatrics appears to remain stable as a proportion of the total, as does med/peds, with the latter unable to grow in numbers proportionally given the small number of providers nationally compared to the other three fields.
The growth of family medicine-trained hospitalists relates to the continued high demand for the profession, with such residents comprising the largest pool of available providers, second only to internal medicine.
Based on the SHM survey, family medicine hospitalists seem to practice similarly to IM; they generally see adults only. It appears that they are accepted into traditional adult hospitalist practices, readily contrasting with groups serving children, which report no FP participation. Meanwhile, med/peds hospitalists provide care across the spectrum of hospitalist groups, though they often report splitting their duties between adults-only services and pediatric services.
As for me, a generation removed from my election of a family practice internship and subsequent transition to internal medicine residency, I should not have worried so. Both paths can lead to hospital medicine.
Dr. Ahlstrom is a hospitalist at Indigo Health Partners in Traverse City, Mich., and a member of SHM’s Practice Analysis Committee.