User login
BETHESDA, MD. – The Food and Drug Administration has designated stool for transplant as a biologic drug, necessitating that any gastroenterologist performing fecal microbiota transplants obtain an Investigational New Drug permit.
By designating stool for transplant as a biologic drug, anyone who performs fecal microbiota transplants (FMTs) – whether they perform a single transplant for one patient or recruit dozens for a study – needs to have an IND permit.
The announcement was made at a 2-day public workshop convened by the National Institutes of Health and the Food and Drug Administration to sift through some of the evidence surrounding FMTs.
The intent of the IND requirement, said Dr. Jay Slater, director of FDA’s Division of Bacterial, Parasitic, and Allergenic Products, is not to stamp out the care that patients can now receive, but to make sure it’s safe, effective, and data driven.
"This is a low-tech procedure that already has a CPT code. A ‘how-to’ guide recently appeared online, and it walks you right through how to do the procedure. There are a very large number of people doing this off the grid. What we need are long-term controlled trials on this that will enhance our understanding of its safety and efficacy."
Although neither the biologic designation nor the IND requirement is brand new, they have not been well publicized, according to one of the innovators of FMT, Dr. Lawrence Brandt, of Albert Einstein Medical Center in New York.
"I am struck by the fact that FDA wants these INDs and yet FDA has never publicly set forth any message on it. So from this moment on, all of us who continue to do this without an IND are violating FDA’s policy," he said at the meeting.
One of the primary concerns now, according to Dr. Brandt, is a burgeoning public interest in FMTs, even to the point of do-it-yourself treatments. With online instructions for self-treatment, and a procedure that is rife with variations, regulators can no longer tacitly ignore the issue.
There’s no standardization of how the stool is prepared and filtered – it could be blended in a kitchen blender or by hand with a tongue depressor, or strained through gauze or a coffee filter, he said. Dosing is all over the place, listed as spoonfuls, grams, and milliliters. Different institutions screen donors in different ways. Some patients get a bowel prep, which can be mild or aggressive, and some don’t get one at all. Should the stool be fresh, and if so, how fresh? Is frozen okay? These are all issues that need to be examined from a safety and efficacy perspective and standardized.
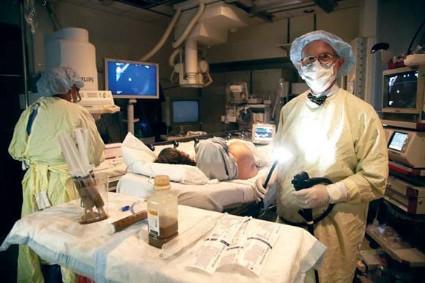
Even the method of delivery varies. The transplant can be administered via nasogastric tube or colonoscope, or by enema. There’s no standardization of data collection either. Some large institutions keep records of everything from the first workup to the last visit. Doctors who perform transplants occasionally may not be as conscientious. And no one knows anything about the do-it-yourselfers, at home with a family member’s donation and a squeeze enema.
Dr. Brandt – and a number of clinicians at the meeting – agreed that answers must be found for all these questions. And they agree that well-conducted clinical trials are the best way to go forward.
Dr. Colleen Kelly, one of the gastroenterologists launching one of 22 currently recruiting studies on FMT, started doing the procedure 5 years ago. Her first patient was a 26-year-old medical student with recurrent bouts of a Clostridium difficile infection.
"I’d heard of [FMT], but never, ever thought of doing one," said Dr. Kelly, of Brown University Medical Center, Providence, R.I. "I thought it was something at the far fringes of medicine."
At her patient’s insistence, Dr. Kelly contacted Dr. Brandt and learned about his process for performing FMT. The following year, she performed 10 FMTs. She is now undertaking a study with Dr. Brandt to recruit about 48 patients with relapsing C. difficile to be randomized to FMT or to a sham treatment with their own stool. Patients who have clinical failure in the sham group will be offered FMT; patients in the active arm who fail on initial FMT will get another FMT from a different donor.
While most trials are examining the utility of FMT in patients with recurrent C. difficile, a few are investigating FMT for use in patients with Crohn’s disease and inflammatory bowel disease. Some clinicians and individual patients are now using FMTs for this condition outside a clinical trial, with no understanding of how a compromised intestinal mucosa might react to transplanted stool.
It will take years to accumulate the data necessary to fully understand FMT and all its implications, Dr. Kelly said. In the interim, the IND requirement will likely shrink the already-small pool of gastroenterologists performing FMTs. "Some will be motivated to get an IND, but the average person in practice won’t," she predicted. "You need to put hours and hours of work into it, and then you’re still under FDA’s oversight because this is not an approved therapy. So that means you have to submit adverse events reports, keep records, and report annually on your program. And at any time, without any warning, [the FDA] can come and inspect your facility."
Dr. Brandt agreed. "It’s a huge amount of paperwork documentation, record-keeping, and follow-up that the average practitioner is simply not going to do." The requirement for an IND means there are simply going to be fewer and fewer physicians who do them, he said.
Admittedly, though, the risks of no regulation can endanger patients, Dr. Kelly said. "If things go on completely unregulated, stupid things will happen," including the spread of infectious diseases like hepatitis C and parasitic infestations.
Indeed, Dr. Alexander Khoruts of the University of Minnesota, Minneapolis, who spoke at the workshop, described the case of an FMT "do-it-yourselfer" who called for some advice on improving her outcomes. Specifically, she had mixed stool from a neighbor and her son’s mother-in-law and administered it to herself without results. "She wanted to know if maybe the chlorine in the water killed off everything. ... Six months later she called me back and said her C. diff was gone, but now she had parasites."
"There are already predatory practices out there [performing FMTs]," Dr. Khoruts said. "I got an e-mail from someone who couldn’t make the drive up to see me, but she found someone near her who would do it for $10,000."
Well-designed and well-executed studies would not only address these immediate safety questions, but would also examine the more nebulous concerns about the long-term effects of tampering with an individual’s unique ecosystem of gut microbes. In recent years, research has begun to document how the balance and proportion of microbial species in the gut can either protect from – or predispose to – metabolic syndrome, obesity, diabetes, cardiovascular disease, arthritis, and even cognitive disorders.
An engrafting microbial transplant could predispose the recipient to develop illnesses that would otherwise never have been destined to occur, Dr. Slater said. "All of the evidence we have suggests that manipulating the gut microbiome is a powerful act that may have long-reaching and subtle effects."
The move toward a standardized FMT product and process is inevitable, Dr. Brandt said. "We’re not going to be doing fecal transplants much longer. This is a temporary situation. We’re already developing compounds that will do the same thing."
Researchers at the University of Guelph, Ontario, have developed a machine that distills and cultures microbes from human feces, producing a kind of super-probiotic that can be used in place of fresh stool.
Also, the Canadian biotech company Rebiotix is working on a similar product, which it intends to test in a phase II randomized controlled trial.
But until those machine-made products are available, physicians and patients with have to stay with the man-made version. "We have access to a substance that is free and has a virtually unlimited supply," Dr. Kelly said. "We cannot deny this effective therapy to these patients who’ve failed all other available treatments."
None of the sources quoted in this article had any financial declarations.
BETHESDA, MD. – The Food and Drug Administration has designated stool for transplant as a biologic drug, necessitating that any gastroenterologist performing fecal microbiota transplants obtain an Investigational New Drug permit.
By designating stool for transplant as a biologic drug, anyone who performs fecal microbiota transplants (FMTs) – whether they perform a single transplant for one patient or recruit dozens for a study – needs to have an IND permit.
The announcement was made at a 2-day public workshop convened by the National Institutes of Health and the Food and Drug Administration to sift through some of the evidence surrounding FMTs.
The intent of the IND requirement, said Dr. Jay Slater, director of FDA’s Division of Bacterial, Parasitic, and Allergenic Products, is not to stamp out the care that patients can now receive, but to make sure it’s safe, effective, and data driven.
"This is a low-tech procedure that already has a CPT code. A ‘how-to’ guide recently appeared online, and it walks you right through how to do the procedure. There are a very large number of people doing this off the grid. What we need are long-term controlled trials on this that will enhance our understanding of its safety and efficacy."
Although neither the biologic designation nor the IND requirement is brand new, they have not been well publicized, according to one of the innovators of FMT, Dr. Lawrence Brandt, of Albert Einstein Medical Center in New York.
"I am struck by the fact that FDA wants these INDs and yet FDA has never publicly set forth any message on it. So from this moment on, all of us who continue to do this without an IND are violating FDA’s policy," he said at the meeting.
One of the primary concerns now, according to Dr. Brandt, is a burgeoning public interest in FMTs, even to the point of do-it-yourself treatments. With online instructions for self-treatment, and a procedure that is rife with variations, regulators can no longer tacitly ignore the issue.
There’s no standardization of how the stool is prepared and filtered – it could be blended in a kitchen blender or by hand with a tongue depressor, or strained through gauze or a coffee filter, he said. Dosing is all over the place, listed as spoonfuls, grams, and milliliters. Different institutions screen donors in different ways. Some patients get a bowel prep, which can be mild or aggressive, and some don’t get one at all. Should the stool be fresh, and if so, how fresh? Is frozen okay? These are all issues that need to be examined from a safety and efficacy perspective and standardized.
Even the method of delivery varies. The transplant can be administered via nasogastric tube or colonoscope, or by enema. There’s no standardization of data collection either. Some large institutions keep records of everything from the first workup to the last visit. Doctors who perform transplants occasionally may not be as conscientious. And no one knows anything about the do-it-yourselfers, at home with a family member’s donation and a squeeze enema.
Dr. Brandt – and a number of clinicians at the meeting – agreed that answers must be found for all these questions. And they agree that well-conducted clinical trials are the best way to go forward.
Dr. Colleen Kelly, one of the gastroenterologists launching one of 22 currently recruiting studies on FMT, started doing the procedure 5 years ago. Her first patient was a 26-year-old medical student with recurrent bouts of a Clostridium difficile infection.
"I’d heard of [FMT], but never, ever thought of doing one," said Dr. Kelly, of Brown University Medical Center, Providence, R.I. "I thought it was something at the far fringes of medicine."
At her patient’s insistence, Dr. Kelly contacted Dr. Brandt and learned about his process for performing FMT. The following year, she performed 10 FMTs. She is now undertaking a study with Dr. Brandt to recruit about 48 patients with relapsing C. difficile to be randomized to FMT or to a sham treatment with their own stool. Patients who have clinical failure in the sham group will be offered FMT; patients in the active arm who fail on initial FMT will get another FMT from a different donor.
While most trials are examining the utility of FMT in patients with recurrent C. difficile, a few are investigating FMT for use in patients with Crohn’s disease and inflammatory bowel disease. Some clinicians and individual patients are now using FMTs for this condition outside a clinical trial, with no understanding of how a compromised intestinal mucosa might react to transplanted stool.
It will take years to accumulate the data necessary to fully understand FMT and all its implications, Dr. Kelly said. In the interim, the IND requirement will likely shrink the already-small pool of gastroenterologists performing FMTs. "Some will be motivated to get an IND, but the average person in practice won’t," she predicted. "You need to put hours and hours of work into it, and then you’re still under FDA’s oversight because this is not an approved therapy. So that means you have to submit adverse events reports, keep records, and report annually on your program. And at any time, without any warning, [the FDA] can come and inspect your facility."
Dr. Brandt agreed. "It’s a huge amount of paperwork documentation, record-keeping, and follow-up that the average practitioner is simply not going to do." The requirement for an IND means there are simply going to be fewer and fewer physicians who do them, he said.
Admittedly, though, the risks of no regulation can endanger patients, Dr. Kelly said. "If things go on completely unregulated, stupid things will happen," including the spread of infectious diseases like hepatitis C and parasitic infestations.
Indeed, Dr. Alexander Khoruts of the University of Minnesota, Minneapolis, who spoke at the workshop, described the case of an FMT "do-it-yourselfer" who called for some advice on improving her outcomes. Specifically, she had mixed stool from a neighbor and her son’s mother-in-law and administered it to herself without results. "She wanted to know if maybe the chlorine in the water killed off everything. ... Six months later she called me back and said her C. diff was gone, but now she had parasites."
"There are already predatory practices out there [performing FMTs]," Dr. Khoruts said. "I got an e-mail from someone who couldn’t make the drive up to see me, but she found someone near her who would do it for $10,000."
Well-designed and well-executed studies would not only address these immediate safety questions, but would also examine the more nebulous concerns about the long-term effects of tampering with an individual’s unique ecosystem of gut microbes. In recent years, research has begun to document how the balance and proportion of microbial species in the gut can either protect from – or predispose to – metabolic syndrome, obesity, diabetes, cardiovascular disease, arthritis, and even cognitive disorders.
An engrafting microbial transplant could predispose the recipient to develop illnesses that would otherwise never have been destined to occur, Dr. Slater said. "All of the evidence we have suggests that manipulating the gut microbiome is a powerful act that may have long-reaching and subtle effects."
The move toward a standardized FMT product and process is inevitable, Dr. Brandt said. "We’re not going to be doing fecal transplants much longer. This is a temporary situation. We’re already developing compounds that will do the same thing."
Researchers at the University of Guelph, Ontario, have developed a machine that distills and cultures microbes from human feces, producing a kind of super-probiotic that can be used in place of fresh stool.
Also, the Canadian biotech company Rebiotix is working on a similar product, which it intends to test in a phase II randomized controlled trial.
But until those machine-made products are available, physicians and patients with have to stay with the man-made version. "We have access to a substance that is free and has a virtually unlimited supply," Dr. Kelly said. "We cannot deny this effective therapy to these patients who’ve failed all other available treatments."
None of the sources quoted in this article had any financial declarations.
BETHESDA, MD. – The Food and Drug Administration has designated stool for transplant as a biologic drug, necessitating that any gastroenterologist performing fecal microbiota transplants obtain an Investigational New Drug permit.
By designating stool for transplant as a biologic drug, anyone who performs fecal microbiota transplants (FMTs) – whether they perform a single transplant for one patient or recruit dozens for a study – needs to have an IND permit.
The announcement was made at a 2-day public workshop convened by the National Institutes of Health and the Food and Drug Administration to sift through some of the evidence surrounding FMTs.
The intent of the IND requirement, said Dr. Jay Slater, director of FDA’s Division of Bacterial, Parasitic, and Allergenic Products, is not to stamp out the care that patients can now receive, but to make sure it’s safe, effective, and data driven.
"This is a low-tech procedure that already has a CPT code. A ‘how-to’ guide recently appeared online, and it walks you right through how to do the procedure. There are a very large number of people doing this off the grid. What we need are long-term controlled trials on this that will enhance our understanding of its safety and efficacy."
Although neither the biologic designation nor the IND requirement is brand new, they have not been well publicized, according to one of the innovators of FMT, Dr. Lawrence Brandt, of Albert Einstein Medical Center in New York.
"I am struck by the fact that FDA wants these INDs and yet FDA has never publicly set forth any message on it. So from this moment on, all of us who continue to do this without an IND are violating FDA’s policy," he said at the meeting.
One of the primary concerns now, according to Dr. Brandt, is a burgeoning public interest in FMTs, even to the point of do-it-yourself treatments. With online instructions for self-treatment, and a procedure that is rife with variations, regulators can no longer tacitly ignore the issue.
There’s no standardization of how the stool is prepared and filtered – it could be blended in a kitchen blender or by hand with a tongue depressor, or strained through gauze or a coffee filter, he said. Dosing is all over the place, listed as spoonfuls, grams, and milliliters. Different institutions screen donors in different ways. Some patients get a bowel prep, which can be mild or aggressive, and some don’t get one at all. Should the stool be fresh, and if so, how fresh? Is frozen okay? These are all issues that need to be examined from a safety and efficacy perspective and standardized.
Even the method of delivery varies. The transplant can be administered via nasogastric tube or colonoscope, or by enema. There’s no standardization of data collection either. Some large institutions keep records of everything from the first workup to the last visit. Doctors who perform transplants occasionally may not be as conscientious. And no one knows anything about the do-it-yourselfers, at home with a family member’s donation and a squeeze enema.
Dr. Brandt – and a number of clinicians at the meeting – agreed that answers must be found for all these questions. And they agree that well-conducted clinical trials are the best way to go forward.
Dr. Colleen Kelly, one of the gastroenterologists launching one of 22 currently recruiting studies on FMT, started doing the procedure 5 years ago. Her first patient was a 26-year-old medical student with recurrent bouts of a Clostridium difficile infection.
"I’d heard of [FMT], but never, ever thought of doing one," said Dr. Kelly, of Brown University Medical Center, Providence, R.I. "I thought it was something at the far fringes of medicine."
At her patient’s insistence, Dr. Kelly contacted Dr. Brandt and learned about his process for performing FMT. The following year, she performed 10 FMTs. She is now undertaking a study with Dr. Brandt to recruit about 48 patients with relapsing C. difficile to be randomized to FMT or to a sham treatment with their own stool. Patients who have clinical failure in the sham group will be offered FMT; patients in the active arm who fail on initial FMT will get another FMT from a different donor.
While most trials are examining the utility of FMT in patients with recurrent C. difficile, a few are investigating FMT for use in patients with Crohn’s disease and inflammatory bowel disease. Some clinicians and individual patients are now using FMTs for this condition outside a clinical trial, with no understanding of how a compromised intestinal mucosa might react to transplanted stool.
It will take years to accumulate the data necessary to fully understand FMT and all its implications, Dr. Kelly said. In the interim, the IND requirement will likely shrink the already-small pool of gastroenterologists performing FMTs. "Some will be motivated to get an IND, but the average person in practice won’t," she predicted. "You need to put hours and hours of work into it, and then you’re still under FDA’s oversight because this is not an approved therapy. So that means you have to submit adverse events reports, keep records, and report annually on your program. And at any time, without any warning, [the FDA] can come and inspect your facility."
Dr. Brandt agreed. "It’s a huge amount of paperwork documentation, record-keeping, and follow-up that the average practitioner is simply not going to do." The requirement for an IND means there are simply going to be fewer and fewer physicians who do them, he said.
Admittedly, though, the risks of no regulation can endanger patients, Dr. Kelly said. "If things go on completely unregulated, stupid things will happen," including the spread of infectious diseases like hepatitis C and parasitic infestations.
Indeed, Dr. Alexander Khoruts of the University of Minnesota, Minneapolis, who spoke at the workshop, described the case of an FMT "do-it-yourselfer" who called for some advice on improving her outcomes. Specifically, she had mixed stool from a neighbor and her son’s mother-in-law and administered it to herself without results. "She wanted to know if maybe the chlorine in the water killed off everything. ... Six months later she called me back and said her C. diff was gone, but now she had parasites."
"There are already predatory practices out there [performing FMTs]," Dr. Khoruts said. "I got an e-mail from someone who couldn’t make the drive up to see me, but she found someone near her who would do it for $10,000."
Well-designed and well-executed studies would not only address these immediate safety questions, but would also examine the more nebulous concerns about the long-term effects of tampering with an individual’s unique ecosystem of gut microbes. In recent years, research has begun to document how the balance and proportion of microbial species in the gut can either protect from – or predispose to – metabolic syndrome, obesity, diabetes, cardiovascular disease, arthritis, and even cognitive disorders.
An engrafting microbial transplant could predispose the recipient to develop illnesses that would otherwise never have been destined to occur, Dr. Slater said. "All of the evidence we have suggests that manipulating the gut microbiome is a powerful act that may have long-reaching and subtle effects."
The move toward a standardized FMT product and process is inevitable, Dr. Brandt said. "We’re not going to be doing fecal transplants much longer. This is a temporary situation. We’re already developing compounds that will do the same thing."
Researchers at the University of Guelph, Ontario, have developed a machine that distills and cultures microbes from human feces, producing a kind of super-probiotic that can be used in place of fresh stool.
Also, the Canadian biotech company Rebiotix is working on a similar product, which it intends to test in a phase II randomized controlled trial.
But until those machine-made products are available, physicians and patients with have to stay with the man-made version. "We have access to a substance that is free and has a virtually unlimited supply," Dr. Kelly said. "We cannot deny this effective therapy to these patients who’ve failed all other available treatments."
None of the sources quoted in this article had any financial declarations.