User login
CDC Issues Advisory About First Mcr-1 Gene in E Coli Found in a Human in the United States
BY JEFF BAUER
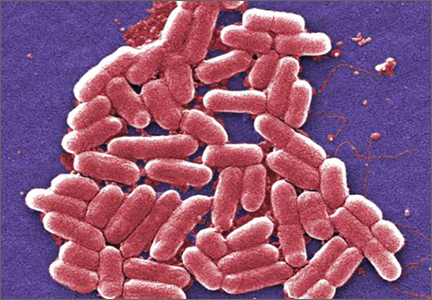
The Centers for Disease Control and Prevention (CDC) issued a health advisory to emphasize the importance of taking measures to prevent the transmission of antibiotic-resistant bacteria after a Pennsylvania woman with no recent travel outside of the United States was found to have Escherichia coli (E coli) bacteria carrying the mcr-1 gene. The mcr-1 gene makes bacteria resistant to colistin, which is used as a last-resort antibiotic to treat patients who have multidrug-resistant infections, including carbapenem-resistant Enterobacteriaceae (CRE). The mcr-1 gene exists on a small piece of DNA that is capable of moving from one bacterium to another, which would allow it to spread antibiotic resistance among species. The CDC has been on alert for this gene in the United States ever since its emergence in China in 2015.
The patient in Pennsylvania, who was being treated for a urinary tract infection (UTI), is believed to be the first human case of mcr-1 E coli in the United States. Although the E coli isolate from the patient was also resistant to antibiotics in five additional antibiotic classes (cephalosporins, fluoroquinolones, sulfonamides, aminoglycosides, and tetracyclines), the woman did not have CRE and the bacteria identified were not resistant to all antibiotics. However, the presence of the mcr-1 gene and its ability to share its colistin resistance with other bacteria increases the risk that pan-resistant bacteria could develop. The CDC’s laboratories have developed protocols for testing microorganisms for the mcr-1 gene and the CDC was performing screening tests to see if people in contact with the patient with mcr-1 might be colonized with this organism.
The CDC recommends that clinicians follow Standard and Contact Precautions for any patients colonized or infected with antibiotic-resistant bacteria, including patients found to have mcr-1-mediated resistant organisms. If a patient is found to have Enterobacteriaceae with mcr-1, healthcare facilities and laboratories should immediately notify local or state public health authorities, and inform all clinicians who are caring for the patient. Any room in which a patient with an antibiotic-resistant infection has been placed should receive thorough daily and terminal cleaning.
1. Centers for Disease Control and Prevention. Alert to U.S. healthcare facilities: first mcr-1 gene in E. coli bacteria found in a human in the United States. https://emergency.cdc.gov/han/han00390.asp. Accessed June 23, 2016.
Emergency Medicine Associate Editor Named as Chair of EM at Rutgers
Lewis S. Nelson, MD, has been appointed as the Chair of the Department of Emergency Medicine at Rutgers New Jersey Medical School and Chief of Service of the Emergency Department at University Hospital in Newark. For many years, Dr Nelson has been serving as associate editor, toxicology, for Emergency Medicine, overseeing the journal’s Case Studies in Toxicology department.
HIV Rapid Tests Miss 1 in 7 Infections
BY RICHARD PIZZI
FROM AIDS
apid human immunodeficiency virus (HIV) tests in high-income countries miss about one in seven infections and should be used in combination with fourth-generation enzyme immunoassays (EIA) or nucleic acid amplification tests (NAAT) in clinical settings whenever possible, according to a study in the journal AIDS.
“These infections are likely to be particularly transmissible due to the high HIV viral load in early infection...in high-income countries, rapid tests should be used in combination with fourth-generation EIA or NAAT, except in special circumstances,” the Australian researchers said.
Researchers performed a systematic review and meta-analysis of 18 studies involving 110,122 HIV rapid test results. The primary outcome was the test’s sensitivity for detecting acute or established HIV infections. Sensitivity was calculated by dividing the number of confirmed positive rapid tests by the number of confirmed positive comparator tests. Specificity was calculated by dividing the number of confirmed negative rapid tests by the number of negative comparator tests.
Compared with EIA, the estimated sensitivity of rapid tests was 94.5% (95% confidence interval [CI], 87.4-97.7). Compared with NAAT, the sensitivity of rapid tests was 93.7% (95% CI, 88.7-96.5). The sensitivity of rapid tests in high-income countries was 85.7% (95% CI, 81.9-88.9), and in low-income countries it was 97.7% (95% CI, 95.2-98.9), compared with either EIA or NAAT (P < .01 for difference between settings). Proportions of antibody-negative acute infections were 13.6% (95% CI, 10.1-18.0) and 4.7% (95% CI, 2.8-7.7) in studies from high- and low-income countries, respectively (P < .01).
Rapid tests were less sensitive when used in clinical settings in high-income countries, regardless of whether they were compared with a NAAT or fourth-generation EIA. However, the researchers noted that the discrepancy between high- and low-income countries could be attributed to the higher proportion of acute HIV infections (antibody-negative NAAT positive) in populations tested in high-income countries, which might reflect higher background testing rates or a higher incidence of HIV in men who have sex with men.
1. Tan WS, Chow EP, Fairley CK, Chen MY, Bradshaw CS, Read TR. Sensitivity of HIV rapid tests compared to fourth generation enzyme immunoassays or HIV RNA tests - a systematic review and meta-analysis. AIDS. 2016 Apr 27. [Epub ahead of print]
Two-Step ED Urinary Tract Infection Screening Cuts Catheterization Rate in Half
BY TARA HAELLE
FROM PEDIATRICS
fter implementation of a quality improvement initiative to more effectively screen febrile children for UTIs in the ED, catheterization rates dropped from 63% to 30% over a 6-month period, a study found.
The sustained drop prevented more than 350 young children from catheterization without increasing revisit rates or missing UTIs in the 39% of children who were followed in the care network. This was in a study that compared catheterization rates in 1,520 children aged 6 to 24 months in the year before the intervention and 828 children in the 6 months during the intervention.
“Although urine catheterization remains the gold standard in diagnosing UTIs, it is an invasive procedure that may be avoided in most patients who are being screened,” wrote Dr Jane M. Lavelle of Children’s Hospital of Philadelphia (CHOP) and her associates. Screening for UTIs by this method can be “painful, time consuming, and costly,” they added.
An alternative method to automatic catheterization is a two-step process already included as an option in the American Academy of Pediatrics guidelines: instead of collecting urine through catheterization just once for screening and culture, an ED first noninvasively collects urine with a urine bag for screening in those indicated with evidence-based risk factors, and then catheterizes only those who screen positive.
“Due to the predictive models’ higher sensitivity than specificity for screening, most urine samples will have a negative screen for pyuria or bacteriuria by urine dipstick or microscopy,” the authors wrote.
At baseline, CHOP’s ED was screening 63% of febrile children under age 24 months using catheterization, but screens were most commonly negative and only 4.3% had positive cultures. The authors therefore initiated a switch to the two-step method as a pilot run in one ED area before educating all ED personnel and expanding to the full department in the second month.
Children aged 6 to 24 months comprised approximately 20% of the ED’s more than 90,000 annual patients, and about 22% of these children presented with fever as the primary concern. Children with a history of genitourinary problems or immune deficiency were excluded.
The pilot ran in an “urgent care section of ED where there are typically more children with less complex medical histories and where ‘fever’ is a common complaint,” the investigators said. The staff completed a learning module with assessment and then received in-person and visual reminders of the procedure.
While 69% of 828 febrile young children still underwent screening during the 6-month intervention period, only 16% still underwent urethral catheterization as the initial screening step, typically because of strong clinical indications for a UTI. Another 14% underwent catheterization only after a positive urine screen from an initial noninvasive urine collection or because of an inability to get an adequate urine specimen with the bag. The reduction in catheterization dropped to 55% within 2 weeks of the intervention’s start and spread to other hospital departments. The drop to a 30% catheterization rate remained throughout 18 additional months of monitoring.
The research did not use external funding, and the researchers reported they had no financial disclosures.
1. Lavelle JM, Blackstone MM, Funari MK, et al. Two-step process for ED UTI screening in febrile young children: reducing catheterization rates. Pediatrics. 2016 Jun 2. pii: e20153023. [Epub ahead of print].
CDC Issues Advisory About First Mcr-1 Gene in E Coli Found in a Human in the United States
BY JEFF BAUER
The Centers for Disease Control and Prevention (CDC) issued a health advisory to emphasize the importance of taking measures to prevent the transmission of antibiotic-resistant bacteria after a Pennsylvania woman with no recent travel outside of the United States was found to have Escherichia coli (E coli) bacteria carrying the mcr-1 gene. The mcr-1 gene makes bacteria resistant to colistin, which is used as a last-resort antibiotic to treat patients who have multidrug-resistant infections, including carbapenem-resistant Enterobacteriaceae (CRE). The mcr-1 gene exists on a small piece of DNA that is capable of moving from one bacterium to another, which would allow it to spread antibiotic resistance among species. The CDC has been on alert for this gene in the United States ever since its emergence in China in 2015.
The patient in Pennsylvania, who was being treated for a urinary tract infection (UTI), is believed to be the first human case of mcr-1 E coli in the United States. Although the E coli isolate from the patient was also resistant to antibiotics in five additional antibiotic classes (cephalosporins, fluoroquinolones, sulfonamides, aminoglycosides, and tetracyclines), the woman did not have CRE and the bacteria identified were not resistant to all antibiotics. However, the presence of the mcr-1 gene and its ability to share its colistin resistance with other bacteria increases the risk that pan-resistant bacteria could develop. The CDC’s laboratories have developed protocols for testing microorganisms for the mcr-1 gene and the CDC was performing screening tests to see if people in contact with the patient with mcr-1 might be colonized with this organism.
The CDC recommends that clinicians follow Standard and Contact Precautions for any patients colonized or infected with antibiotic-resistant bacteria, including patients found to have mcr-1-mediated resistant organisms. If a patient is found to have Enterobacteriaceae with mcr-1, healthcare facilities and laboratories should immediately notify local or state public health authorities, and inform all clinicians who are caring for the patient. Any room in which a patient with an antibiotic-resistant infection has been placed should receive thorough daily and terminal cleaning.
1. Centers for Disease Control and Prevention. Alert to U.S. healthcare facilities: first mcr-1 gene in E. coli bacteria found in a human in the United States. https://emergency.cdc.gov/han/han00390.asp. Accessed June 23, 2016.
Emergency Medicine Associate Editor Named as Chair of EM at Rutgers
Lewis S. Nelson, MD, has been appointed as the Chair of the Department of Emergency Medicine at Rutgers New Jersey Medical School and Chief of Service of the Emergency Department at University Hospital in Newark. For many years, Dr Nelson has been serving as associate editor, toxicology, for Emergency Medicine, overseeing the journal’s Case Studies in Toxicology department.
HIV Rapid Tests Miss 1 in 7 Infections
BY RICHARD PIZZI
FROM AIDS
apid human immunodeficiency virus (HIV) tests in high-income countries miss about one in seven infections and should be used in combination with fourth-generation enzyme immunoassays (EIA) or nucleic acid amplification tests (NAAT) in clinical settings whenever possible, according to a study in the journal AIDS.
“These infections are likely to be particularly transmissible due to the high HIV viral load in early infection...in high-income countries, rapid tests should be used in combination with fourth-generation EIA or NAAT, except in special circumstances,” the Australian researchers said.
Researchers performed a systematic review and meta-analysis of 18 studies involving 110,122 HIV rapid test results. The primary outcome was the test’s sensitivity for detecting acute or established HIV infections. Sensitivity was calculated by dividing the number of confirmed positive rapid tests by the number of confirmed positive comparator tests. Specificity was calculated by dividing the number of confirmed negative rapid tests by the number of negative comparator tests.
Compared with EIA, the estimated sensitivity of rapid tests was 94.5% (95% confidence interval [CI], 87.4-97.7). Compared with NAAT, the sensitivity of rapid tests was 93.7% (95% CI, 88.7-96.5). The sensitivity of rapid tests in high-income countries was 85.7% (95% CI, 81.9-88.9), and in low-income countries it was 97.7% (95% CI, 95.2-98.9), compared with either EIA or NAAT (P < .01 for difference between settings). Proportions of antibody-negative acute infections were 13.6% (95% CI, 10.1-18.0) and 4.7% (95% CI, 2.8-7.7) in studies from high- and low-income countries, respectively (P < .01).
Rapid tests were less sensitive when used in clinical settings in high-income countries, regardless of whether they were compared with a NAAT or fourth-generation EIA. However, the researchers noted that the discrepancy between high- and low-income countries could be attributed to the higher proportion of acute HIV infections (antibody-negative NAAT positive) in populations tested in high-income countries, which might reflect higher background testing rates or a higher incidence of HIV in men who have sex with men.
1. Tan WS, Chow EP, Fairley CK, Chen MY, Bradshaw CS, Read TR. Sensitivity of HIV rapid tests compared to fourth generation enzyme immunoassays or HIV RNA tests - a systematic review and meta-analysis. AIDS. 2016 Apr 27. [Epub ahead of print]
Two-Step ED Urinary Tract Infection Screening Cuts Catheterization Rate in Half
BY TARA HAELLE
FROM PEDIATRICS
fter implementation of a quality improvement initiative to more effectively screen febrile children for UTIs in the ED, catheterization rates dropped from 63% to 30% over a 6-month period, a study found.
The sustained drop prevented more than 350 young children from catheterization without increasing revisit rates or missing UTIs in the 39% of children who were followed in the care network. This was in a study that compared catheterization rates in 1,520 children aged 6 to 24 months in the year before the intervention and 828 children in the 6 months during the intervention.
“Although urine catheterization remains the gold standard in diagnosing UTIs, it is an invasive procedure that may be avoided in most patients who are being screened,” wrote Dr Jane M. Lavelle of Children’s Hospital of Philadelphia (CHOP) and her associates. Screening for UTIs by this method can be “painful, time consuming, and costly,” they added.
An alternative method to automatic catheterization is a two-step process already included as an option in the American Academy of Pediatrics guidelines: instead of collecting urine through catheterization just once for screening and culture, an ED first noninvasively collects urine with a urine bag for screening in those indicated with evidence-based risk factors, and then catheterizes only those who screen positive.
“Due to the predictive models’ higher sensitivity than specificity for screening, most urine samples will have a negative screen for pyuria or bacteriuria by urine dipstick or microscopy,” the authors wrote.
At baseline, CHOP’s ED was screening 63% of febrile children under age 24 months using catheterization, but screens were most commonly negative and only 4.3% had positive cultures. The authors therefore initiated a switch to the two-step method as a pilot run in one ED area before educating all ED personnel and expanding to the full department in the second month.
Children aged 6 to 24 months comprised approximately 20% of the ED’s more than 90,000 annual patients, and about 22% of these children presented with fever as the primary concern. Children with a history of genitourinary problems or immune deficiency were excluded.
The pilot ran in an “urgent care section of ED where there are typically more children with less complex medical histories and where ‘fever’ is a common complaint,” the investigators said. The staff completed a learning module with assessment and then received in-person and visual reminders of the procedure.
While 69% of 828 febrile young children still underwent screening during the 6-month intervention period, only 16% still underwent urethral catheterization as the initial screening step, typically because of strong clinical indications for a UTI. Another 14% underwent catheterization only after a positive urine screen from an initial noninvasive urine collection or because of an inability to get an adequate urine specimen with the bag. The reduction in catheterization dropped to 55% within 2 weeks of the intervention’s start and spread to other hospital departments. The drop to a 30% catheterization rate remained throughout 18 additional months of monitoring.
The research did not use external funding, and the researchers reported they had no financial disclosures.
1. Lavelle JM, Blackstone MM, Funari MK, et al. Two-step process for ED UTI screening in febrile young children: reducing catheterization rates. Pediatrics. 2016 Jun 2. pii: e20153023. [Epub ahead of print].
CDC Issues Advisory About First Mcr-1 Gene in E Coli Found in a Human in the United States
BY JEFF BAUER
The Centers for Disease Control and Prevention (CDC) issued a health advisory to emphasize the importance of taking measures to prevent the transmission of antibiotic-resistant bacteria after a Pennsylvania woman with no recent travel outside of the United States was found to have Escherichia coli (E coli) bacteria carrying the mcr-1 gene. The mcr-1 gene makes bacteria resistant to colistin, which is used as a last-resort antibiotic to treat patients who have multidrug-resistant infections, including carbapenem-resistant Enterobacteriaceae (CRE). The mcr-1 gene exists on a small piece of DNA that is capable of moving from one bacterium to another, which would allow it to spread antibiotic resistance among species. The CDC has been on alert for this gene in the United States ever since its emergence in China in 2015.
The patient in Pennsylvania, who was being treated for a urinary tract infection (UTI), is believed to be the first human case of mcr-1 E coli in the United States. Although the E coli isolate from the patient was also resistant to antibiotics in five additional antibiotic classes (cephalosporins, fluoroquinolones, sulfonamides, aminoglycosides, and tetracyclines), the woman did not have CRE and the bacteria identified were not resistant to all antibiotics. However, the presence of the mcr-1 gene and its ability to share its colistin resistance with other bacteria increases the risk that pan-resistant bacteria could develop. The CDC’s laboratories have developed protocols for testing microorganisms for the mcr-1 gene and the CDC was performing screening tests to see if people in contact with the patient with mcr-1 might be colonized with this organism.
The CDC recommends that clinicians follow Standard and Contact Precautions for any patients colonized or infected with antibiotic-resistant bacteria, including patients found to have mcr-1-mediated resistant organisms. If a patient is found to have Enterobacteriaceae with mcr-1, healthcare facilities and laboratories should immediately notify local or state public health authorities, and inform all clinicians who are caring for the patient. Any room in which a patient with an antibiotic-resistant infection has been placed should receive thorough daily and terminal cleaning.
1. Centers for Disease Control and Prevention. Alert to U.S. healthcare facilities: first mcr-1 gene in E. coli bacteria found in a human in the United States. https://emergency.cdc.gov/han/han00390.asp. Accessed June 23, 2016.
Emergency Medicine Associate Editor Named as Chair of EM at Rutgers
Lewis S. Nelson, MD, has been appointed as the Chair of the Department of Emergency Medicine at Rutgers New Jersey Medical School and Chief of Service of the Emergency Department at University Hospital in Newark. For many years, Dr Nelson has been serving as associate editor, toxicology, for Emergency Medicine, overseeing the journal’s Case Studies in Toxicology department.
HIV Rapid Tests Miss 1 in 7 Infections
BY RICHARD PIZZI
FROM AIDS
apid human immunodeficiency virus (HIV) tests in high-income countries miss about one in seven infections and should be used in combination with fourth-generation enzyme immunoassays (EIA) or nucleic acid amplification tests (NAAT) in clinical settings whenever possible, according to a study in the journal AIDS.
“These infections are likely to be particularly transmissible due to the high HIV viral load in early infection...in high-income countries, rapid tests should be used in combination with fourth-generation EIA or NAAT, except in special circumstances,” the Australian researchers said.
Researchers performed a systematic review and meta-analysis of 18 studies involving 110,122 HIV rapid test results. The primary outcome was the test’s sensitivity for detecting acute or established HIV infections. Sensitivity was calculated by dividing the number of confirmed positive rapid tests by the number of confirmed positive comparator tests. Specificity was calculated by dividing the number of confirmed negative rapid tests by the number of negative comparator tests.
Compared with EIA, the estimated sensitivity of rapid tests was 94.5% (95% confidence interval [CI], 87.4-97.7). Compared with NAAT, the sensitivity of rapid tests was 93.7% (95% CI, 88.7-96.5). The sensitivity of rapid tests in high-income countries was 85.7% (95% CI, 81.9-88.9), and in low-income countries it was 97.7% (95% CI, 95.2-98.9), compared with either EIA or NAAT (P < .01 for difference between settings). Proportions of antibody-negative acute infections were 13.6% (95% CI, 10.1-18.0) and 4.7% (95% CI, 2.8-7.7) in studies from high- and low-income countries, respectively (P < .01).
Rapid tests were less sensitive when used in clinical settings in high-income countries, regardless of whether they were compared with a NAAT or fourth-generation EIA. However, the researchers noted that the discrepancy between high- and low-income countries could be attributed to the higher proportion of acute HIV infections (antibody-negative NAAT positive) in populations tested in high-income countries, which might reflect higher background testing rates or a higher incidence of HIV in men who have sex with men.
1. Tan WS, Chow EP, Fairley CK, Chen MY, Bradshaw CS, Read TR. Sensitivity of HIV rapid tests compared to fourth generation enzyme immunoassays or HIV RNA tests - a systematic review and meta-analysis. AIDS. 2016 Apr 27. [Epub ahead of print]
Two-Step ED Urinary Tract Infection Screening Cuts Catheterization Rate in Half
BY TARA HAELLE
FROM PEDIATRICS
fter implementation of a quality improvement initiative to more effectively screen febrile children for UTIs in the ED, catheterization rates dropped from 63% to 30% over a 6-month period, a study found.
The sustained drop prevented more than 350 young children from catheterization without increasing revisit rates or missing UTIs in the 39% of children who were followed in the care network. This was in a study that compared catheterization rates in 1,520 children aged 6 to 24 months in the year before the intervention and 828 children in the 6 months during the intervention.
“Although urine catheterization remains the gold standard in diagnosing UTIs, it is an invasive procedure that may be avoided in most patients who are being screened,” wrote Dr Jane M. Lavelle of Children’s Hospital of Philadelphia (CHOP) and her associates. Screening for UTIs by this method can be “painful, time consuming, and costly,” they added.
An alternative method to automatic catheterization is a two-step process already included as an option in the American Academy of Pediatrics guidelines: instead of collecting urine through catheterization just once for screening and culture, an ED first noninvasively collects urine with a urine bag for screening in those indicated with evidence-based risk factors, and then catheterizes only those who screen positive.
“Due to the predictive models’ higher sensitivity than specificity for screening, most urine samples will have a negative screen for pyuria or bacteriuria by urine dipstick or microscopy,” the authors wrote.
At baseline, CHOP’s ED was screening 63% of febrile children under age 24 months using catheterization, but screens were most commonly negative and only 4.3% had positive cultures. The authors therefore initiated a switch to the two-step method as a pilot run in one ED area before educating all ED personnel and expanding to the full department in the second month.
Children aged 6 to 24 months comprised approximately 20% of the ED’s more than 90,000 annual patients, and about 22% of these children presented with fever as the primary concern. Children with a history of genitourinary problems or immune deficiency were excluded.
The pilot ran in an “urgent care section of ED where there are typically more children with less complex medical histories and where ‘fever’ is a common complaint,” the investigators said. The staff completed a learning module with assessment and then received in-person and visual reminders of the procedure.
While 69% of 828 febrile young children still underwent screening during the 6-month intervention period, only 16% still underwent urethral catheterization as the initial screening step, typically because of strong clinical indications for a UTI. Another 14% underwent catheterization only after a positive urine screen from an initial noninvasive urine collection or because of an inability to get an adequate urine specimen with the bag. The reduction in catheterization dropped to 55% within 2 weeks of the intervention’s start and spread to other hospital departments. The drop to a 30% catheterization rate remained throughout 18 additional months of monitoring.
The research did not use external funding, and the researchers reported they had no financial disclosures.
1. Lavelle JM, Blackstone MM, Funari MK, et al. Two-step process for ED UTI screening in febrile young children: reducing catheterization rates. Pediatrics. 2016 Jun 2. pii: e20153023. [Epub ahead of print].