User login
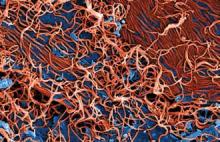
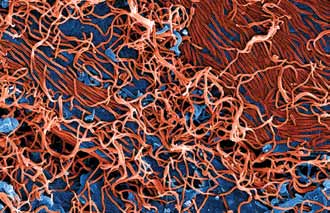
CDC updates guidance on protecting health care workers from Ebola
By: Jennie Smith
The new guidance, issued Oct. 20, closely mirrors the Ebola personal protective equipment (PPE) guidance issued by Médecins Sans Frontières (Doctors Without Borders).
The CDC’s recommendations update the PPE guidance that was issued Aug. 1 and is now widely considered to be inadequate. The new recommendations advise that health care workers have no skin exposed, that they be supervised while donning and removing PPE, and that rigorous training and practice accompany any use of PPE in the treatment of patients with Ebola infections.
Specific equipment recommendations include double gloves, waterproof boot covers to mid-calf or higher, and a disposable fluid-resistant or impermeable gown that extends to at least mid-calf, or an coverall without a hood. The agency also recommends the use of respirators (N95 or powered air purifying), disposable single-use full-face shields in lieu of goggles, surgical hoods for complete coverage of the head and neck, and a waterproof apron extending from torso to mid-calf if patients have vomiting or diarrhea.
The guidance specifies that hospitals must have designated areas for putting on and taking off PPE and that trained observers monitor all donning and removal. The guidance also contains instructions for disinfecting PPE prior to its removal.
The agency emphasized that training, not merely having the correct equipment in place, was key to the successful use of PPE. “Focusing only on PPE gives a false sense of security of safe care and worker safety,” the CDC stated. “Training is a critical aspect of ensuring infection control.”
Facilities must make sure all health care providers practice “numerous times” until they understand how to properly and safely use the equipment, the CDC advised.
Malpractice reform failed to curb defensive medicine in the ED
By: Mary Ann Moon
Vitals Key clinical point: Changing the liability standard for emergency care did not reduce the practice of defensive medicine. Major finding: Malpractice reform failed to decrease intensity of practice in the ED, so eight of nine expected benefits never materialized. Data source: An analysis of all 3,868,110 ED visits to 1,166 hospitals from 1997 through 2011 in three states where malpractice reform was enacted. Disclosures: This study was supported by the Veterans Affairs Office of Academic Affiliations, RAND Health, and the RAND Institute for Civil Justice. Dr Waxman reported having no financial conflicts of interest; one of his associates reported receiving grant support unrelated to this study from The Doctors Company, CAP-MPT, Norcal, Physicians Insurance, and COPIC. |
Malpractice reforms enacted in three states approximately 10 years ago failed to reduce defensive medicine in the emergency department, according to a report published Oct. 16 in the New England Journal of Medicine.
The reforms changed the liability standard for emergency care from ordinary negligence to gross negligence, providing exceptionally broad protection to emergency physicians so they could feel safe from litigation if they stopped ordering unnecessary (and expensive) tests and stopped admitting patients who didn’t truly need inpatient care. The legal community in the three reform states – Texas, Georgia, and South Carolina – “characterizes the gross negligence standard as providing ‘virtual immunity’ to emergency physicians,” said Dr Daniel A. Waxman of RAND Health and the University of California, Los Angeles, and his associates.
“Our findings suggest that physicians are less motivated by legal risk than they believe themselves to be. Although a practice culture of abundant caution clearly exists, it seems likely than aversion to legal risk exists in parallel with a more general risk aversion and with other behavioral, cultural, and economic motivations that might affect decision making. “When legal risk decreases, the ‘path of least resistance’ may still favor resource-intensive care. Our results suggest that malpractice reform may have less effect on costs than has been projected,” they noted.
The researchers examined database information on 3,868,110 emergency department (ED) visits by Medicare patients to 1,166 hospitals across the 3 reform states, as well as to 10 neighboring control states, from 1997 through 2011. They found that the proportion of patients who underwent CT or MRI increased each year in both the reform states and the control states, and per-visit costs increased as well.
In a regression analysis, malpractice reform was not associated with a decline in CT or MRI use in any of the reform states. And in an analysis of ED costs, per-visit ED charges were not reduced after malpractice reform was enacted in either Texas or South Carolina; in Georgia, reforms were associated with a 3.6% reduction.
In addition, the rate of hospital admissions from the ED did not decrease in any of the reform states.
Data regarding the number of malpractice claims during the study period that were specifically related to ED care are not available. But the malpractice reforms in Texas were associated with a 60% reduction in malpractice claims and a 70% reduction in malpractice payments, the investigators noted.
Nevertheless, “we did not find evidence that these reforms decreased practice intensity, as measured by the rate of the use of advanced imaging, by the rate of hospital admission, or in two of three cases, by average charges. Although there was a small [3.6%] reduction in charges in one of the three sites, our results in aggregate suggest that these strongly protective laws caused little if any change in practice intensity among physicians caring for Medicare patients in emergency departments,” Dr Waxman and his associates said (N. Engl. J. Med. 2014 October 16 [doi:10.1056/NEJMsa1313308]).
Many previous studies, including anonymous surveys of ED physicians, have reported that most practice defensive medicine; up to 30% of CT scans and 19% of MRIs were ordered “for defensive purposes” in one study, and as many as 70% of respondents in another study said they often ordered imaging studies or hospital admissions simply to protect themselves.
New test will speed enterovirus D68 case confirmation from weeks to days
By: Lucas Franki
A new lab test for enterovirus D68 is expected to speed up testing and confirmation of cases, according to a press release from the Centers for Disease Control and Prevention.
The new test is a “real-time” reverse transcription polymerase chain reaction and can identify all strains of EV-D68. The previous test could be used to detect almost any enterovirus, but was labor intensive to perform and not conducive to large-scale testing.
Of the 1,200 samples from 45 states sent to the CDC for EV-D68 testing between Aug. 1 to Oct. 10, less than 200 have been tested and about half have tested positive. The CDC now expects to be able to test around 180 samples a day and complete in 7-10 days the testing on samples received since mid-September, The new method will “reduce what would normally take several weeks to get results to a Dr Anne Schuchat few days,” Dr Anne Schuchat, assistant surgeon general and director of the CDC’s National Center for Immunization and Respiratory Diseases, said in the press release.
As with other enteroviruses, the CDC expects new cases of EV-D68 will decrease in the fall, but faster testing will more accurately show trends of the disease and will help to monitor changes in the outbreak as it winds down, according to the CDC press release. [email protected]
ED visits by young patients trended up in California
By: Mary Ann Moon
Vitals Key clinical point: Children’s and adolescents’ use of emergency departments increased markedly across all payer categories between 2005 and 2010 in California. Major finding: Youths’ use of EDs statewide rose 11% overall, 23% among the uninsured, 15% among the privately insured, and 7% among those covered by Medicaid in the late 2000s. Data source: A retrospective analysis of all 2-3 million annual visits to California EDs by children up to age 18 in 2005-2010. Disclosures: This study was primarily supported by the California HealthCare Foundation, with additional support from the National Center for Advancing Translational Sciences, the National Institutes of Health, the University of California, and the Robert Wood Johnson Foundation. Dr Hsia and her associates reported having no financial disclosures. |
Children’s and adolescents’ use of emergency departments rose markedly in the late 2000s, a sharp contrast from their steady or decreasing rates of ED use throughout the 1990s and early 2000s, according to a Research Letter to the Editor published online Oct. 14 in JAMA.
The recent uptick in pediatric ED visits also contrasts with a notable decline in adult ED use during the same time period. “These findings suggest that the drivers for ED use differ significantly between youths and adults, and that policies regarding insurance expansion” – that is, coverage through the Affordable Care Act – “may also have varying effects,” said Dr Renee Y. Hsia of the department of emergency medicine, University of California, San Francisco, and San Francisco General Hospital, and her associates.
They performed a retrospective analysis using a database recording all ED visits by children and adolescents up to 18 years of age to general hospitals across California
“The divergence from older trends in ED use among youths may also reflect the increasingly central role of the ED in the US health care system, especially during a period of severe economic recession, and could signal an overall deterioration in access to primary care across payer groups, or that even privately insured youths with greater access to primary care physicians are being directed to the ED for care,” Dr Hsia and her associates said.
Pit bull bites are worse by several measures
By: Amy Karon
Vitals Key clinical point: Bites by pit bulls and other large dog breeds remain a serious threat to young children. Major finding: Pit bulls caused 42.4% of dog bites that required hospitalization. Data source: A retrospective chart review of 223 children presenting to an emergency department with dog bites. Disclosures: Dr Yeung did not report external funding sources and declared no financial conflicts. |
SAN DIEGO – Pit bulls caused 42% of dog bites for which children were hospitalized, a 4-year retrospective study showed.
Bites by pit bulls had a 40% greater odds of a full trauma team response, and were linked to a 3-day longer mean hospital stay, compared with bites by other dogs [4.2 days vs. 1.3 days], reported lead author Dr Claudia Yeung of Arizona Children’s Center and Maricopa Integrated Health System in Phoenix.
Of about 885,000 dog bites that need medical attention in the United States every year, half affect children, according to the Centers for Disease Control and Prevention. Dr Yeung and her colleagues reviewed the medical charts of 223 children and adolescents who presented with dog bites to the emergency department at Arizona Children’s Center from March 2010 through March 2014. Of the children who presented, 33 (15%) were hospitalized and 12 (5%) required the response of a full trauma team.
Hospitalized children in the study averaged 6 years of age, and almost 82% needed surgical intervention in the operating room. Children younger than age 5 years were more likely to sustain injuries to the face or neck than were older children (51% vs. 21%), she reported.
Besides pit bulls, the most commonly reported breeds associated with bites were German shepherds, Rottweilers, and Labrador retrievers, Dr Yeung said. A limitation of the study was that some medical records lacked data on the breed of the dog.
Doubling of US heroin deaths spurs call for increased naloxone access
By: M. Alexander Otto
Vitals Key clinical point: Heroin overdoses can be reduced by public education about the risks of prescription opioid abuse and by the distribution of intranasal naloxone kits to at-risk populations. Major finding: In a representative sample of 28 states from 2010 to 2012, heroin deaths climbed from 1,779 to 3,635, a rate increase from 1.0 to 2.1 per 100,000 population. Data source: Statistical analysis of state health records. Disclosures: The MMWR is published by the Centers for Disease Control and Prevention. |
Fatal heroin overdoses doubled in the United States from 2010 to 2012, according to a report in the Morbidity and Mortality Weekly Report, a publication of the Centers for Disease Control and Prevention.
In a representative sample of 28 states, heroin deaths climbed from 1,779 to 3,635, a rate increase from 1.0 to 2.1 per 100,000 people. At the same time, deaths from prescription opioids fell from 10,427 to 9,869, a decrease from 6.0 to 5.6 per 100,000 people (MMWR2014;63:849-54).
In Northeastern states, fatal heroin overdoses increased 211%. Southern states had an increase of 181%, Midwestern states an increase of 62%, and Western states an increase of 91%, based on state health department data.
The report did not give numbers for individual states, only regions, but it did note that Kentucky reported a 279% increase in heroin deaths from 2010 to 2012, and Ohio had an increase of approximately 300% from 2007 to 2012.
The investigators found no statistically significant relationship between the increase in heroin deaths and the decrease in prescription opioid fatalities. However, they noted that about 75% of heroin users report using prescription opioids first, then switching to heroin, a cheaper, more readily available alternative that gives a more potent high.
Young adults are sometimes unaware that prescription pain pills are opioids and that their abuse can slip into heroin use. Particularly hard hit communities have reduced opioid fatalities by getting that message out through education campaigns, and also by distributing intranasal naloxone kits to the people most likely to need them: first responders, family members, and opioid abusers who might need to rescue a friend.
“State policies that increase access to naloxone, a drug that can reverse potentially fatal respiratory depression in persons who have overdosed from either OPRs [opioid pain relievers] or heroin, or policies that reduce or eliminate penalties when someone reports an overdose, are potentially useful strategies” to counter the problem, said the researchers, led by CDC statistician Rose A. Rudd.
Also, “efforts to prevent expansion of the number of OPR users who might use heroin when it is available should continue [including] screening for substance abuse, urine testing for drug use, and referral to substance abuse treatment. The use of prescription drug monitoring programs can address inappropriate opioid prescribing and further prevent OPR abuse,” they said.
In 2012, 25- to 34-year-olds had the highest heroin fatality rate; OPR fatalities were highest in those aged 45-54 years. Non-Hispanic whites had the highest rates for both. Men were four times more likely than women to die from a heroin overdose, but only slightly more likely to die from prescription pain pills.
“Heroin overdose death rates increased significantly for both sexes, all age groups, all census regions, and all racial/ethnic groups other than American Indians/Alaska Natives,” the researchers noted.
Meanwhile, from 2010 to 2012, pain pill overdoses declined significantly in men, people under 45 years old, those who live in the South, and non-Hispanic whites. They increased in people aged 55-64 years. [email protected]
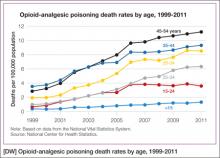
Opioid-poisoning deaths rose fastest in 55- to 64-year-olds
By: Lucas Franki
In 1999, the death rate for opioid analgesics was 1 per 100,000 people for adults aged 55-64 years. By 2011, this rate had increased to 6.3 per 100,000 people, the NCHS reported.
Non-Hispanic white adults had the largest increase in the rate of opioid-analgesic poisoning deaths among measured ethnicities, rising from 1.6 per 100,000 in 1999 to 7.3 in 2011. The death rate for non-Hispanic black adults increased from 0.9 per 100,000 in 1999 to 2.3 in 2011. Hispanic adults did not see a large rate increase, with 1.7 per 100,000 deaths in 1999 and 2 per 100,000 deaths in 2011 attributed to opioid-analgesic poisoning, according to data from the National Vital Statistics System.
[email protected]
Dr Lappin is an assistant professor and an attending physician, department of emergency medicine, New York-Presbyterian Hospital/ Weill Cornell Medical College, New York.
CDC updates guidance on protecting health care workers from Ebola
By: Jennie Smith
The new guidance, issued Oct. 20, closely mirrors the Ebola personal protective equipment (PPE) guidance issued by Médecins Sans Frontières (Doctors Without Borders).
The CDC’s recommendations update the PPE guidance that was issued Aug. 1 and is now widely considered to be inadequate. The new recommendations advise that health care workers have no skin exposed, that they be supervised while donning and removing PPE, and that rigorous training and practice accompany any use of PPE in the treatment of patients with Ebola infections.
Specific equipment recommendations include double gloves, waterproof boot covers to mid-calf or higher, and a disposable fluid-resistant or impermeable gown that extends to at least mid-calf, or an coverall without a hood. The agency also recommends the use of respirators (N95 or powered air purifying), disposable single-use full-face shields in lieu of goggles, surgical hoods for complete coverage of the head and neck, and a waterproof apron extending from torso to mid-calf if patients have vomiting or diarrhea.
The guidance specifies that hospitals must have designated areas for putting on and taking off PPE and that trained observers monitor all donning and removal. The guidance also contains instructions for disinfecting PPE prior to its removal.
The agency emphasized that training, not merely having the correct equipment in place, was key to the successful use of PPE. “Focusing only on PPE gives a false sense of security of safe care and worker safety,” the CDC stated. “Training is a critical aspect of ensuring infection control.”
Facilities must make sure all health care providers practice “numerous times” until they understand how to properly and safely use the equipment, the CDC advised.
Malpractice reform failed to curb defensive medicine in the ED
By: Mary Ann Moon
Vitals Key clinical point: Changing the liability standard for emergency care did not reduce the practice of defensive medicine. Major finding: Malpractice reform failed to decrease intensity of practice in the ED, so eight of nine expected benefits never materialized. Data source: An analysis of all 3,868,110 ED visits to 1,166 hospitals from 1997 through 2011 in three states where malpractice reform was enacted. Disclosures: This study was supported by the Veterans Affairs Office of Academic Affiliations, RAND Health, and the RAND Institute for Civil Justice. Dr Waxman reported having no financial conflicts of interest; one of his associates reported receiving grant support unrelated to this study from The Doctors Company, CAP-MPT, Norcal, Physicians Insurance, and COPIC. |
Malpractice reforms enacted in three states approximately 10 years ago failed to reduce defensive medicine in the emergency department, according to a report published Oct. 16 in the New England Journal of Medicine.
The reforms changed the liability standard for emergency care from ordinary negligence to gross negligence, providing exceptionally broad protection to emergency physicians so they could feel safe from litigation if they stopped ordering unnecessary (and expensive) tests and stopped admitting patients who didn’t truly need inpatient care. The legal community in the three reform states – Texas, Georgia, and South Carolina – “characterizes the gross negligence standard as providing ‘virtual immunity’ to emergency physicians,” said Dr Daniel A. Waxman of RAND Health and the University of California, Los Angeles, and his associates.
“Our findings suggest that physicians are less motivated by legal risk than they believe themselves to be. Although a practice culture of abundant caution clearly exists, it seems likely than aversion to legal risk exists in parallel with a more general risk aversion and with other behavioral, cultural, and economic motivations that might affect decision making. “When legal risk decreases, the ‘path of least resistance’ may still favor resource-intensive care. Our results suggest that malpractice reform may have less effect on costs than has been projected,” they noted.
The researchers examined database information on 3,868,110 emergency department (ED) visits by Medicare patients to 1,166 hospitals across the 3 reform states, as well as to 10 neighboring control states, from 1997 through 2011. They found that the proportion of patients who underwent CT or MRI increased each year in both the reform states and the control states, and per-visit costs increased as well.
In a regression analysis, malpractice reform was not associated with a decline in CT or MRI use in any of the reform states. And in an analysis of ED costs, per-visit ED charges were not reduced after malpractice reform was enacted in either Texas or South Carolina; in Georgia, reforms were associated with a 3.6% reduction.
In addition, the rate of hospital admissions from the ED did not decrease in any of the reform states.
Data regarding the number of malpractice claims during the study period that were specifically related to ED care are not available. But the malpractice reforms in Texas were associated with a 60% reduction in malpractice claims and a 70% reduction in malpractice payments, the investigators noted.
Nevertheless, “we did not find evidence that these reforms decreased practice intensity, as measured by the rate of the use of advanced imaging, by the rate of hospital admission, or in two of three cases, by average charges. Although there was a small [3.6%] reduction in charges in one of the three sites, our results in aggregate suggest that these strongly protective laws caused little if any change in practice intensity among physicians caring for Medicare patients in emergency departments,” Dr Waxman and his associates said (N. Engl. J. Med. 2014 October 16 [doi:10.1056/NEJMsa1313308]).
Many previous studies, including anonymous surveys of ED physicians, have reported that most practice defensive medicine; up to 30% of CT scans and 19% of MRIs were ordered “for defensive purposes” in one study, and as many as 70% of respondents in another study said they often ordered imaging studies or hospital admissions simply to protect themselves.
New test will speed enterovirus D68 case confirmation from weeks to days
By: Lucas Franki
A new lab test for enterovirus D68 is expected to speed up testing and confirmation of cases, according to a press release from the Centers for Disease Control and Prevention.
The new test is a “real-time” reverse transcription polymerase chain reaction and can identify all strains of EV-D68. The previous test could be used to detect almost any enterovirus, but was labor intensive to perform and not conducive to large-scale testing.
Of the 1,200 samples from 45 states sent to the CDC for EV-D68 testing between Aug. 1 to Oct. 10, less than 200 have been tested and about half have tested positive. The CDC now expects to be able to test around 180 samples a day and complete in 7-10 days the testing on samples received since mid-September, The new method will “reduce what would normally take several weeks to get results to a Dr Anne Schuchat few days,” Dr Anne Schuchat, assistant surgeon general and director of the CDC’s National Center for Immunization and Respiratory Diseases, said in the press release.
As with other enteroviruses, the CDC expects new cases of EV-D68 will decrease in the fall, but faster testing will more accurately show trends of the disease and will help to monitor changes in the outbreak as it winds down, according to the CDC press release. [email protected]
ED visits by young patients trended up in California
By: Mary Ann Moon
Vitals Key clinical point: Children’s and adolescents’ use of emergency departments increased markedly across all payer categories between 2005 and 2010 in California. Major finding: Youths’ use of EDs statewide rose 11% overall, 23% among the uninsured, 15% among the privately insured, and 7% among those covered by Medicaid in the late 2000s. Data source: A retrospective analysis of all 2-3 million annual visits to California EDs by children up to age 18 in 2005-2010. Disclosures: This study was primarily supported by the California HealthCare Foundation, with additional support from the National Center for Advancing Translational Sciences, the National Institutes of Health, the University of California, and the Robert Wood Johnson Foundation. Dr Hsia and her associates reported having no financial disclosures. |
Children’s and adolescents’ use of emergency departments rose markedly in the late 2000s, a sharp contrast from their steady or decreasing rates of ED use throughout the 1990s and early 2000s, according to a Research Letter to the Editor published online Oct. 14 in JAMA.
The recent uptick in pediatric ED visits also contrasts with a notable decline in adult ED use during the same time period. “These findings suggest that the drivers for ED use differ significantly between youths and adults, and that policies regarding insurance expansion” – that is, coverage through the Affordable Care Act – “may also have varying effects,” said Dr Renee Y. Hsia of the department of emergency medicine, University of California, San Francisco, and San Francisco General Hospital, and her associates.
They performed a retrospective analysis using a database recording all ED visits by children and adolescents up to 18 years of age to general hospitals across California
“The divergence from older trends in ED use among youths may also reflect the increasingly central role of the ED in the US health care system, especially during a period of severe economic recession, and could signal an overall deterioration in access to primary care across payer groups, or that even privately insured youths with greater access to primary care physicians are being directed to the ED for care,” Dr Hsia and her associates said.
Pit bull bites are worse by several measures
By: Amy Karon
Vitals Key clinical point: Bites by pit bulls and other large dog breeds remain a serious threat to young children. Major finding: Pit bulls caused 42.4% of dog bites that required hospitalization. Data source: A retrospective chart review of 223 children presenting to an emergency department with dog bites. Disclosures: Dr Yeung did not report external funding sources and declared no financial conflicts. |
SAN DIEGO – Pit bulls caused 42% of dog bites for which children were hospitalized, a 4-year retrospective study showed.
Bites by pit bulls had a 40% greater odds of a full trauma team response, and were linked to a 3-day longer mean hospital stay, compared with bites by other dogs [4.2 days vs. 1.3 days], reported lead author Dr Claudia Yeung of Arizona Children’s Center and Maricopa Integrated Health System in Phoenix.
Of about 885,000 dog bites that need medical attention in the United States every year, half affect children, according to the Centers for Disease Control and Prevention. Dr Yeung and her colleagues reviewed the medical charts of 223 children and adolescents who presented with dog bites to the emergency department at Arizona Children’s Center from March 2010 through March 2014. Of the children who presented, 33 (15%) were hospitalized and 12 (5%) required the response of a full trauma team.
Hospitalized children in the study averaged 6 years of age, and almost 82% needed surgical intervention in the operating room. Children younger than age 5 years were more likely to sustain injuries to the face or neck than were older children (51% vs. 21%), she reported.
Besides pit bulls, the most commonly reported breeds associated with bites were German shepherds, Rottweilers, and Labrador retrievers, Dr Yeung said. A limitation of the study was that some medical records lacked data on the breed of the dog.
Doubling of US heroin deaths spurs call for increased naloxone access
By: M. Alexander Otto
Vitals Key clinical point: Heroin overdoses can be reduced by public education about the risks of prescription opioid abuse and by the distribution of intranasal naloxone kits to at-risk populations. Major finding: In a representative sample of 28 states from 2010 to 2012, heroin deaths climbed from 1,779 to 3,635, a rate increase from 1.0 to 2.1 per 100,000 population. Data source: Statistical analysis of state health records. Disclosures: The MMWR is published by the Centers for Disease Control and Prevention. |
Fatal heroin overdoses doubled in the United States from 2010 to 2012, according to a report in the Morbidity and Mortality Weekly Report, a publication of the Centers for Disease Control and Prevention.
In a representative sample of 28 states, heroin deaths climbed from 1,779 to 3,635, a rate increase from 1.0 to 2.1 per 100,000 people. At the same time, deaths from prescription opioids fell from 10,427 to 9,869, a decrease from 6.0 to 5.6 per 100,000 people (MMWR2014;63:849-54).
In Northeastern states, fatal heroin overdoses increased 211%. Southern states had an increase of 181%, Midwestern states an increase of 62%, and Western states an increase of 91%, based on state health department data.
The report did not give numbers for individual states, only regions, but it did note that Kentucky reported a 279% increase in heroin deaths from 2010 to 2012, and Ohio had an increase of approximately 300% from 2007 to 2012.
The investigators found no statistically significant relationship between the increase in heroin deaths and the decrease in prescription opioid fatalities. However, they noted that about 75% of heroin users report using prescription opioids first, then switching to heroin, a cheaper, more readily available alternative that gives a more potent high.
Young adults are sometimes unaware that prescription pain pills are opioids and that their abuse can slip into heroin use. Particularly hard hit communities have reduced opioid fatalities by getting that message out through education campaigns, and also by distributing intranasal naloxone kits to the people most likely to need them: first responders, family members, and opioid abusers who might need to rescue a friend.
“State policies that increase access to naloxone, a drug that can reverse potentially fatal respiratory depression in persons who have overdosed from either OPRs [opioid pain relievers] or heroin, or policies that reduce or eliminate penalties when someone reports an overdose, are potentially useful strategies” to counter the problem, said the researchers, led by CDC statistician Rose A. Rudd.
Also, “efforts to prevent expansion of the number of OPR users who might use heroin when it is available should continue [including] screening for substance abuse, urine testing for drug use, and referral to substance abuse treatment. The use of prescription drug monitoring programs can address inappropriate opioid prescribing and further prevent OPR abuse,” they said.
In 2012, 25- to 34-year-olds had the highest heroin fatality rate; OPR fatalities were highest in those aged 45-54 years. Non-Hispanic whites had the highest rates for both. Men were four times more likely than women to die from a heroin overdose, but only slightly more likely to die from prescription pain pills.
“Heroin overdose death rates increased significantly for both sexes, all age groups, all census regions, and all racial/ethnic groups other than American Indians/Alaska Natives,” the researchers noted.
Meanwhile, from 2010 to 2012, pain pill overdoses declined significantly in men, people under 45 years old, those who live in the South, and non-Hispanic whites. They increased in people aged 55-64 years. [email protected]
Opioid-poisoning deaths rose fastest in 55- to 64-year-olds
By: Lucas Franki
In 1999, the death rate for opioid analgesics was 1 per 100,000 people for adults aged 55-64 years. By 2011, this rate had increased to 6.3 per 100,000 people, the NCHS reported.
Non-Hispanic white adults had the largest increase in the rate of opioid-analgesic poisoning deaths among measured ethnicities, rising from 1.6 per 100,000 in 1999 to 7.3 in 2011. The death rate for non-Hispanic black adults increased from 0.9 per 100,000 in 1999 to 2.3 in 2011. Hispanic adults did not see a large rate increase, with 1.7 per 100,000 deaths in 1999 and 2 per 100,000 deaths in 2011 attributed to opioid-analgesic poisoning, according to data from the National Vital Statistics System.
[email protected]
Dr Lappin is an assistant professor and an attending physician, department of emergency medicine, New York-Presbyterian Hospital/ Weill Cornell Medical College, New York.
CDC updates guidance on protecting health care workers from Ebola
By: Jennie Smith
The new guidance, issued Oct. 20, closely mirrors the Ebola personal protective equipment (PPE) guidance issued by Médecins Sans Frontières (Doctors Without Borders).
The CDC’s recommendations update the PPE guidance that was issued Aug. 1 and is now widely considered to be inadequate. The new recommendations advise that health care workers have no skin exposed, that they be supervised while donning and removing PPE, and that rigorous training and practice accompany any use of PPE in the treatment of patients with Ebola infections.
Specific equipment recommendations include double gloves, waterproof boot covers to mid-calf or higher, and a disposable fluid-resistant or impermeable gown that extends to at least mid-calf, or an coverall without a hood. The agency also recommends the use of respirators (N95 or powered air purifying), disposable single-use full-face shields in lieu of goggles, surgical hoods for complete coverage of the head and neck, and a waterproof apron extending from torso to mid-calf if patients have vomiting or diarrhea.
The guidance specifies that hospitals must have designated areas for putting on and taking off PPE and that trained observers monitor all donning and removal. The guidance also contains instructions for disinfecting PPE prior to its removal.
The agency emphasized that training, not merely having the correct equipment in place, was key to the successful use of PPE. “Focusing only on PPE gives a false sense of security of safe care and worker safety,” the CDC stated. “Training is a critical aspect of ensuring infection control.”
Facilities must make sure all health care providers practice “numerous times” until they understand how to properly and safely use the equipment, the CDC advised.
Malpractice reform failed to curb defensive medicine in the ED
By: Mary Ann Moon
Vitals Key clinical point: Changing the liability standard for emergency care did not reduce the practice of defensive medicine. Major finding: Malpractice reform failed to decrease intensity of practice in the ED, so eight of nine expected benefits never materialized. Data source: An analysis of all 3,868,110 ED visits to 1,166 hospitals from 1997 through 2011 in three states where malpractice reform was enacted. Disclosures: This study was supported by the Veterans Affairs Office of Academic Affiliations, RAND Health, and the RAND Institute for Civil Justice. Dr Waxman reported having no financial conflicts of interest; one of his associates reported receiving grant support unrelated to this study from The Doctors Company, CAP-MPT, Norcal, Physicians Insurance, and COPIC. |
Malpractice reforms enacted in three states approximately 10 years ago failed to reduce defensive medicine in the emergency department, according to a report published Oct. 16 in the New England Journal of Medicine.
The reforms changed the liability standard for emergency care from ordinary negligence to gross negligence, providing exceptionally broad protection to emergency physicians so they could feel safe from litigation if they stopped ordering unnecessary (and expensive) tests and stopped admitting patients who didn’t truly need inpatient care. The legal community in the three reform states – Texas, Georgia, and South Carolina – “characterizes the gross negligence standard as providing ‘virtual immunity’ to emergency physicians,” said Dr Daniel A. Waxman of RAND Health and the University of California, Los Angeles, and his associates.
“Our findings suggest that physicians are less motivated by legal risk than they believe themselves to be. Although a practice culture of abundant caution clearly exists, it seems likely than aversion to legal risk exists in parallel with a more general risk aversion and with other behavioral, cultural, and economic motivations that might affect decision making. “When legal risk decreases, the ‘path of least resistance’ may still favor resource-intensive care. Our results suggest that malpractice reform may have less effect on costs than has been projected,” they noted.
The researchers examined database information on 3,868,110 emergency department (ED) visits by Medicare patients to 1,166 hospitals across the 3 reform states, as well as to 10 neighboring control states, from 1997 through 2011. They found that the proportion of patients who underwent CT or MRI increased each year in both the reform states and the control states, and per-visit costs increased as well.
In a regression analysis, malpractice reform was not associated with a decline in CT or MRI use in any of the reform states. And in an analysis of ED costs, per-visit ED charges were not reduced after malpractice reform was enacted in either Texas or South Carolina; in Georgia, reforms were associated with a 3.6% reduction.
In addition, the rate of hospital admissions from the ED did not decrease in any of the reform states.
Data regarding the number of malpractice claims during the study period that were specifically related to ED care are not available. But the malpractice reforms in Texas were associated with a 60% reduction in malpractice claims and a 70% reduction in malpractice payments, the investigators noted.
Nevertheless, “we did not find evidence that these reforms decreased practice intensity, as measured by the rate of the use of advanced imaging, by the rate of hospital admission, or in two of three cases, by average charges. Although there was a small [3.6%] reduction in charges in one of the three sites, our results in aggregate suggest that these strongly protective laws caused little if any change in practice intensity among physicians caring for Medicare patients in emergency departments,” Dr Waxman and his associates said (N. Engl. J. Med. 2014 October 16 [doi:10.1056/NEJMsa1313308]).
Many previous studies, including anonymous surveys of ED physicians, have reported that most practice defensive medicine; up to 30% of CT scans and 19% of MRIs were ordered “for defensive purposes” in one study, and as many as 70% of respondents in another study said they often ordered imaging studies or hospital admissions simply to protect themselves.
New test will speed enterovirus D68 case confirmation from weeks to days
By: Lucas Franki
A new lab test for enterovirus D68 is expected to speed up testing and confirmation of cases, according to a press release from the Centers for Disease Control and Prevention.
The new test is a “real-time” reverse transcription polymerase chain reaction and can identify all strains of EV-D68. The previous test could be used to detect almost any enterovirus, but was labor intensive to perform and not conducive to large-scale testing.
Of the 1,200 samples from 45 states sent to the CDC for EV-D68 testing between Aug. 1 to Oct. 10, less than 200 have been tested and about half have tested positive. The CDC now expects to be able to test around 180 samples a day and complete in 7-10 days the testing on samples received since mid-September, The new method will “reduce what would normally take several weeks to get results to a Dr Anne Schuchat few days,” Dr Anne Schuchat, assistant surgeon general and director of the CDC’s National Center for Immunization and Respiratory Diseases, said in the press release.
As with other enteroviruses, the CDC expects new cases of EV-D68 will decrease in the fall, but faster testing will more accurately show trends of the disease and will help to monitor changes in the outbreak as it winds down, according to the CDC press release. [email protected]
ED visits by young patients trended up in California
By: Mary Ann Moon
Vitals Key clinical point: Children’s and adolescents’ use of emergency departments increased markedly across all payer categories between 2005 and 2010 in California. Major finding: Youths’ use of EDs statewide rose 11% overall, 23% among the uninsured, 15% among the privately insured, and 7% among those covered by Medicaid in the late 2000s. Data source: A retrospective analysis of all 2-3 million annual visits to California EDs by children up to age 18 in 2005-2010. Disclosures: This study was primarily supported by the California HealthCare Foundation, with additional support from the National Center for Advancing Translational Sciences, the National Institutes of Health, the University of California, and the Robert Wood Johnson Foundation. Dr Hsia and her associates reported having no financial disclosures. |
Children’s and adolescents’ use of emergency departments rose markedly in the late 2000s, a sharp contrast from their steady or decreasing rates of ED use throughout the 1990s and early 2000s, according to a Research Letter to the Editor published online Oct. 14 in JAMA.
The recent uptick in pediatric ED visits also contrasts with a notable decline in adult ED use during the same time period. “These findings suggest that the drivers for ED use differ significantly between youths and adults, and that policies regarding insurance expansion” – that is, coverage through the Affordable Care Act – “may also have varying effects,” said Dr Renee Y. Hsia of the department of emergency medicine, University of California, San Francisco, and San Francisco General Hospital, and her associates.
They performed a retrospective analysis using a database recording all ED visits by children and adolescents up to 18 years of age to general hospitals across California
“The divergence from older trends in ED use among youths may also reflect the increasingly central role of the ED in the US health care system, especially during a period of severe economic recession, and could signal an overall deterioration in access to primary care across payer groups, or that even privately insured youths with greater access to primary care physicians are being directed to the ED for care,” Dr Hsia and her associates said.
Pit bull bites are worse by several measures
By: Amy Karon
Vitals Key clinical point: Bites by pit bulls and other large dog breeds remain a serious threat to young children. Major finding: Pit bulls caused 42.4% of dog bites that required hospitalization. Data source: A retrospective chart review of 223 children presenting to an emergency department with dog bites. Disclosures: Dr Yeung did not report external funding sources and declared no financial conflicts. |
SAN DIEGO – Pit bulls caused 42% of dog bites for which children were hospitalized, a 4-year retrospective study showed.
Bites by pit bulls had a 40% greater odds of a full trauma team response, and were linked to a 3-day longer mean hospital stay, compared with bites by other dogs [4.2 days vs. 1.3 days], reported lead author Dr Claudia Yeung of Arizona Children’s Center and Maricopa Integrated Health System in Phoenix.
Of about 885,000 dog bites that need medical attention in the United States every year, half affect children, according to the Centers for Disease Control and Prevention. Dr Yeung and her colleagues reviewed the medical charts of 223 children and adolescents who presented with dog bites to the emergency department at Arizona Children’s Center from March 2010 through March 2014. Of the children who presented, 33 (15%) were hospitalized and 12 (5%) required the response of a full trauma team.
Hospitalized children in the study averaged 6 years of age, and almost 82% needed surgical intervention in the operating room. Children younger than age 5 years were more likely to sustain injuries to the face or neck than were older children (51% vs. 21%), she reported.
Besides pit bulls, the most commonly reported breeds associated with bites were German shepherds, Rottweilers, and Labrador retrievers, Dr Yeung said. A limitation of the study was that some medical records lacked data on the breed of the dog.
Doubling of US heroin deaths spurs call for increased naloxone access
By: M. Alexander Otto
Vitals Key clinical point: Heroin overdoses can be reduced by public education about the risks of prescription opioid abuse and by the distribution of intranasal naloxone kits to at-risk populations. Major finding: In a representative sample of 28 states from 2010 to 2012, heroin deaths climbed from 1,779 to 3,635, a rate increase from 1.0 to 2.1 per 100,000 population. Data source: Statistical analysis of state health records. Disclosures: The MMWR is published by the Centers for Disease Control and Prevention. |
Fatal heroin overdoses doubled in the United States from 2010 to 2012, according to a report in the Morbidity and Mortality Weekly Report, a publication of the Centers for Disease Control and Prevention.
In a representative sample of 28 states, heroin deaths climbed from 1,779 to 3,635, a rate increase from 1.0 to 2.1 per 100,000 people. At the same time, deaths from prescription opioids fell from 10,427 to 9,869, a decrease from 6.0 to 5.6 per 100,000 people (MMWR2014;63:849-54).
In Northeastern states, fatal heroin overdoses increased 211%. Southern states had an increase of 181%, Midwestern states an increase of 62%, and Western states an increase of 91%, based on state health department data.
The report did not give numbers for individual states, only regions, but it did note that Kentucky reported a 279% increase in heroin deaths from 2010 to 2012, and Ohio had an increase of approximately 300% from 2007 to 2012.
The investigators found no statistically significant relationship between the increase in heroin deaths and the decrease in prescription opioid fatalities. However, they noted that about 75% of heroin users report using prescription opioids first, then switching to heroin, a cheaper, more readily available alternative that gives a more potent high.
Young adults are sometimes unaware that prescription pain pills are opioids and that their abuse can slip into heroin use. Particularly hard hit communities have reduced opioid fatalities by getting that message out through education campaigns, and also by distributing intranasal naloxone kits to the people most likely to need them: first responders, family members, and opioid abusers who might need to rescue a friend.
“State policies that increase access to naloxone, a drug that can reverse potentially fatal respiratory depression in persons who have overdosed from either OPRs [opioid pain relievers] or heroin, or policies that reduce or eliminate penalties when someone reports an overdose, are potentially useful strategies” to counter the problem, said the researchers, led by CDC statistician Rose A. Rudd.
Also, “efforts to prevent expansion of the number of OPR users who might use heroin when it is available should continue [including] screening for substance abuse, urine testing for drug use, and referral to substance abuse treatment. The use of prescription drug monitoring programs can address inappropriate opioid prescribing and further prevent OPR abuse,” they said.
In 2012, 25- to 34-year-olds had the highest heroin fatality rate; OPR fatalities were highest in those aged 45-54 years. Non-Hispanic whites had the highest rates for both. Men were four times more likely than women to die from a heroin overdose, but only slightly more likely to die from prescription pain pills.
“Heroin overdose death rates increased significantly for both sexes, all age groups, all census regions, and all racial/ethnic groups other than American Indians/Alaska Natives,” the researchers noted.
Meanwhile, from 2010 to 2012, pain pill overdoses declined significantly in men, people under 45 years old, those who live in the South, and non-Hispanic whites. They increased in people aged 55-64 years. [email protected]
Opioid-poisoning deaths rose fastest in 55- to 64-year-olds
By: Lucas Franki
In 1999, the death rate for opioid analgesics was 1 per 100,000 people for adults aged 55-64 years. By 2011, this rate had increased to 6.3 per 100,000 people, the NCHS reported.
Non-Hispanic white adults had the largest increase in the rate of opioid-analgesic poisoning deaths among measured ethnicities, rising from 1.6 per 100,000 in 1999 to 7.3 in 2011. The death rate for non-Hispanic black adults increased from 0.9 per 100,000 in 1999 to 2.3 in 2011. Hispanic adults did not see a large rate increase, with 1.7 per 100,000 deaths in 1999 and 2 per 100,000 deaths in 2011 attributed to opioid-analgesic poisoning, according to data from the National Vital Statistics System.
[email protected]
Dr Lappin is an assistant professor and an attending physician, department of emergency medicine, New York-Presbyterian Hospital/ Weill Cornell Medical College, New York.