User login
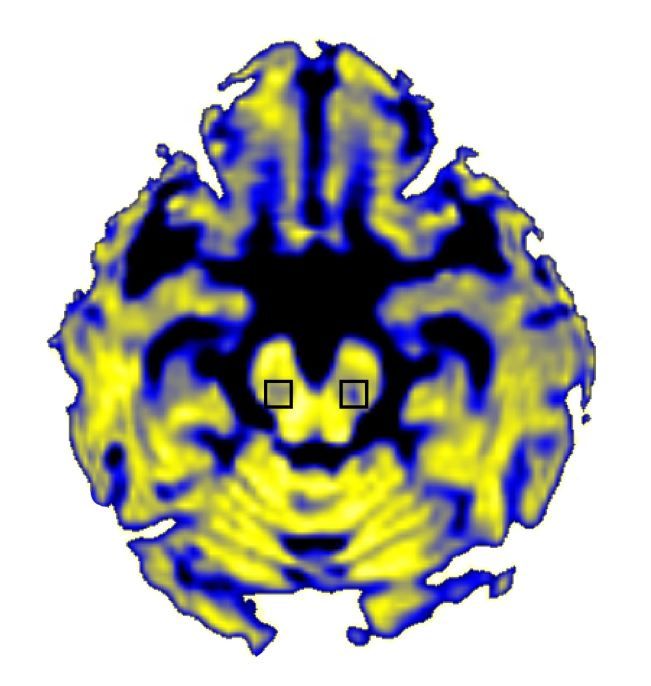
Free water in the posterior substantia nigra brain region increased as clinical Parkinson’s disease progressed in a 4-year longitudinal study of participants in the Parkinson’s Progression Markers Initiative.
Free water in this brain region is measurable via diffusion MRI, and this study – the first to look at free water in Parkinson’s patients across this time frame – suggests it to be a viable biomarker of disease progression that could be used in clinical trials evaluating Parkinson’s therapies.
Dr. Burciu and her colleagues found that free water increased over the first year post diagnosis in Parkinson’s patients but not in controls (P = .043), confirming similar results from an earlier study (Neurobiol Aging. 2015a;36:1097-104; Brain. 2015b;138:2322-31).
The researchers also looked at data from 46 Parkinson’s patients in the cohort who underwent imaging at 2 and 4 years to learn whether the observed increases in free water corresponded to progression measured on the Hoehn and Yahr scale, a widely used measure of Parkinson’s symptom severity.
Free water continued to increase in the Parkinson’s patients through 4 years, and increases in the first and second years after diagnosis were significantly associated with worsening of symptoms through 4 years (P less than .05 for both). Moreover, the investigators noted, men saw greater 4-year increases in free water levels, compared with women.
“The short-term increase in free water is related to the long-term progression of motor symptoms. Moreover, sex and baseline free water levels significantly predicted the rate of change in free water in [the posterior substantia nigra] over 4 years,” the investigators wrote.
The results were consistent across study sites, they found.
Dr. Burciu and her colleagues disclosed funding from the PPMI, which is supported by the Michael J. Fox Foundation and a consortium of pharmaceutical, biotech, and financial firms. The researchers also received funding from the National Institutes of Health. None disclosed financial conflicts of interest.
Free water in the posterior substantia nigra brain region increased as clinical Parkinson’s disease progressed in a 4-year longitudinal study of participants in the Parkinson’s Progression Markers Initiative.
Free water in this brain region is measurable via diffusion MRI, and this study – the first to look at free water in Parkinson’s patients across this time frame – suggests it to be a viable biomarker of disease progression that could be used in clinical trials evaluating Parkinson’s therapies.
Dr. Burciu and her colleagues found that free water increased over the first year post diagnosis in Parkinson’s patients but not in controls (P = .043), confirming similar results from an earlier study (Neurobiol Aging. 2015a;36:1097-104; Brain. 2015b;138:2322-31).
The researchers also looked at data from 46 Parkinson’s patients in the cohort who underwent imaging at 2 and 4 years to learn whether the observed increases in free water corresponded to progression measured on the Hoehn and Yahr scale, a widely used measure of Parkinson’s symptom severity.
Free water continued to increase in the Parkinson’s patients through 4 years, and increases in the first and second years after diagnosis were significantly associated with worsening of symptoms through 4 years (P less than .05 for both). Moreover, the investigators noted, men saw greater 4-year increases in free water levels, compared with women.
“The short-term increase in free water is related to the long-term progression of motor symptoms. Moreover, sex and baseline free water levels significantly predicted the rate of change in free water in [the posterior substantia nigra] over 4 years,” the investigators wrote.
The results were consistent across study sites, they found.
Dr. Burciu and her colleagues disclosed funding from the PPMI, which is supported by the Michael J. Fox Foundation and a consortium of pharmaceutical, biotech, and financial firms. The researchers also received funding from the National Institutes of Health. None disclosed financial conflicts of interest.
Free water in the posterior substantia nigra brain region increased as clinical Parkinson’s disease progressed in a 4-year longitudinal study of participants in the Parkinson’s Progression Markers Initiative.
Free water in this brain region is measurable via diffusion MRI, and this study – the first to look at free water in Parkinson’s patients across this time frame – suggests it to be a viable biomarker of disease progression that could be used in clinical trials evaluating Parkinson’s therapies.
Dr. Burciu and her colleagues found that free water increased over the first year post diagnosis in Parkinson’s patients but not in controls (P = .043), confirming similar results from an earlier study (Neurobiol Aging. 2015a;36:1097-104; Brain. 2015b;138:2322-31).
The researchers also looked at data from 46 Parkinson’s patients in the cohort who underwent imaging at 2 and 4 years to learn whether the observed increases in free water corresponded to progression measured on the Hoehn and Yahr scale, a widely used measure of Parkinson’s symptom severity.
Free water continued to increase in the Parkinson’s patients through 4 years, and increases in the first and second years after diagnosis were significantly associated with worsening of symptoms through 4 years (P less than .05 for both). Moreover, the investigators noted, men saw greater 4-year increases in free water levels, compared with women.
“The short-term increase in free water is related to the long-term progression of motor symptoms. Moreover, sex and baseline free water levels significantly predicted the rate of change in free water in [the posterior substantia nigra] over 4 years,” the investigators wrote.
The results were consistent across study sites, they found.
Dr. Burciu and her colleagues disclosed funding from the PPMI, which is supported by the Michael J. Fox Foundation and a consortium of pharmaceutical, biotech, and financial firms. The researchers also received funding from the National Institutes of Health. None disclosed financial conflicts of interest.
FROM BRAIN
Key clinical point:
Major finding: Increases measured in years 1 or 2 after diagnosis were associated with worsening of symptoms through year 4 (P less than .05)
Data source: Analysis of 103 patients and 49 controls from a large, multisite, international, observational, longitudinal study seeking Parkinson’s biomarkers.
Disclosures: The National Institutes of Health and the Parkinson’s Progression Markers Initiative (PPMI) funded this analysis. The PPMI receives broad funding from industry and foundations. None of the researchers disclosed financial conflicts of interest.