User login
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
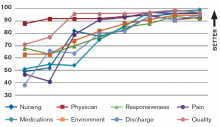
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.