User login
SAN DIEGO – Something as simple as a stamp in a patient’s chart to remind medical providers about vaccinating against human papillomavirus nearly quintupled the percentage of eligible patients being vaccinated in one outpatient office, according to a poster presented at the annual meeting of the American College of Obstetricians and Gynecologists.
The faculty practice was vaccinating only 11% of eligible women before the trial, lower than the 2009 national average vaccination rate of 25%. After the office staff was instructed to place a reminder stamp in the progress notes of all nonpregnant women aged 18-26 years who were scheduled for an appointment with a gynecology provider, the office significantly improved its vaccination rate to 49% of eligible women, Dr. Kerry Rut and her associates reported.
The prospective study compared charts for 86 patients who were eligible to receive the Gardasil vaccine for human papillomavirus (HPV) before use of the stamp and 70 patients after implementation of the stamp. Three of the six health care providers in the office (five physicians and a nurse practitioner) significantly increased their vaccinations of patients after the reminder stamp started appearing in progress notes, said Dr. Rut, an ob.gyn. in private practice in Bay Shore, N.Y. She led the study while she was a resident at Winthrop University Hospital, Mineola, N.Y.
The study received top prize among posters presented at the meeting.
Vaccination rates did not seem to be influenced by the reason for the patient’s visit or a history of abnormal Pap smear results. Only the use of the stamp was associated with vaccination rates.
The charts documented that the physician discussed Gardasil in 19 of 86 (22%) cases before use of the stamp and in 63 of 70 (90%) cases after use of the stamp, a significant increase. Still, less than half of eligible patients received the vaccine. When Gardasil was discussed, patients refused vaccination in 34 of 63 (54%) cases. The high refusal rate despite counseling suggests a need to investigate the type of patient education and its content, Dr. Rut suggested.
Patients averaged 23 years of age before use of the stamp and 22 years after the stamp, a statistically significant difference. The two groups did not differ significantly in the type of insurance, the reason for the visit, or the percentage with a previous abnormal Pap smear.
Each of the six medical providers increased their vaccination rates; the increase was statistically significant for three of them. The nurse practitioner had the highest vaccination rate before use of the stamp (4 of 12, or 33%) and after implementation of the stamp (11 of 14, or 79%), a significant increase.
One physician significantly increased vaccination rates from 6% before the stamp (1 of 17 patients) to 62% after the stamp (8 of 13 patients). Another physician significantly improved from vaccinating none of 14 patients before the stamp to 7 of 12 patients after the stamp (58%).
Of the three physicians whose improvement did not reach statistical significance, one went from vaccinating none of 15 patients before the stamp to 1 of 10 patients (10%) after the stamp. Another physician vaccinated 2 of 12 patients at baseline (17%) and 4 of 7 patients after the stamp started (57%). The third physician vaccinated 2 of 16 patients at baseline (13%) and 3 of 14 patients after the stamp (21%).
Overall, the vaccination rate increased from 9 of 86 patients before the stamp (11%) to 34 of 70 patients with use of the stamp (49%), Dr. Rut said.
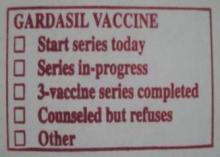
The stamp included five boxes that the physician could check off: "Start series today," "Series in-progress," "3-vaccine series completed," "Counseled but refuses," and "Other."
As the use of electronic health records increases, perhaps a Gardasil reminder could be incorporated instead of a physical stamp to improve vaccination rates even more, she suggested.
Dr. Rut reported having no relevant financial disclosures.
SAN DIEGO – Something as simple as a stamp in a patient’s chart to remind medical providers about vaccinating against human papillomavirus nearly quintupled the percentage of eligible patients being vaccinated in one outpatient office, according to a poster presented at the annual meeting of the American College of Obstetricians and Gynecologists.
The faculty practice was vaccinating only 11% of eligible women before the trial, lower than the 2009 national average vaccination rate of 25%. After the office staff was instructed to place a reminder stamp in the progress notes of all nonpregnant women aged 18-26 years who were scheduled for an appointment with a gynecology provider, the office significantly improved its vaccination rate to 49% of eligible women, Dr. Kerry Rut and her associates reported.
The prospective study compared charts for 86 patients who were eligible to receive the Gardasil vaccine for human papillomavirus (HPV) before use of the stamp and 70 patients after implementation of the stamp. Three of the six health care providers in the office (five physicians and a nurse practitioner) significantly increased their vaccinations of patients after the reminder stamp started appearing in progress notes, said Dr. Rut, an ob.gyn. in private practice in Bay Shore, N.Y. She led the study while she was a resident at Winthrop University Hospital, Mineola, N.Y.
The study received top prize among posters presented at the meeting.
Vaccination rates did not seem to be influenced by the reason for the patient’s visit or a history of abnormal Pap smear results. Only the use of the stamp was associated with vaccination rates.
The charts documented that the physician discussed Gardasil in 19 of 86 (22%) cases before use of the stamp and in 63 of 70 (90%) cases after use of the stamp, a significant increase. Still, less than half of eligible patients received the vaccine. When Gardasil was discussed, patients refused vaccination in 34 of 63 (54%) cases. The high refusal rate despite counseling suggests a need to investigate the type of patient education and its content, Dr. Rut suggested.
Patients averaged 23 years of age before use of the stamp and 22 years after the stamp, a statistically significant difference. The two groups did not differ significantly in the type of insurance, the reason for the visit, or the percentage with a previous abnormal Pap smear.
Each of the six medical providers increased their vaccination rates; the increase was statistically significant for three of them. The nurse practitioner had the highest vaccination rate before use of the stamp (4 of 12, or 33%) and after implementation of the stamp (11 of 14, or 79%), a significant increase.
One physician significantly increased vaccination rates from 6% before the stamp (1 of 17 patients) to 62% after the stamp (8 of 13 patients). Another physician significantly improved from vaccinating none of 14 patients before the stamp to 7 of 12 patients after the stamp (58%).
Of the three physicians whose improvement did not reach statistical significance, one went from vaccinating none of 15 patients before the stamp to 1 of 10 patients (10%) after the stamp. Another physician vaccinated 2 of 12 patients at baseline (17%) and 4 of 7 patients after the stamp started (57%). The third physician vaccinated 2 of 16 patients at baseline (13%) and 3 of 14 patients after the stamp (21%).
Overall, the vaccination rate increased from 9 of 86 patients before the stamp (11%) to 34 of 70 patients with use of the stamp (49%), Dr. Rut said.
The stamp included five boxes that the physician could check off: "Start series today," "Series in-progress," "3-vaccine series completed," "Counseled but refuses," and "Other."
As the use of electronic health records increases, perhaps a Gardasil reminder could be incorporated instead of a physical stamp to improve vaccination rates even more, she suggested.
Dr. Rut reported having no relevant financial disclosures.
SAN DIEGO – Something as simple as a stamp in a patient’s chart to remind medical providers about vaccinating against human papillomavirus nearly quintupled the percentage of eligible patients being vaccinated in one outpatient office, according to a poster presented at the annual meeting of the American College of Obstetricians and Gynecologists.
The faculty practice was vaccinating only 11% of eligible women before the trial, lower than the 2009 national average vaccination rate of 25%. After the office staff was instructed to place a reminder stamp in the progress notes of all nonpregnant women aged 18-26 years who were scheduled for an appointment with a gynecology provider, the office significantly improved its vaccination rate to 49% of eligible women, Dr. Kerry Rut and her associates reported.
The prospective study compared charts for 86 patients who were eligible to receive the Gardasil vaccine for human papillomavirus (HPV) before use of the stamp and 70 patients after implementation of the stamp. Three of the six health care providers in the office (five physicians and a nurse practitioner) significantly increased their vaccinations of patients after the reminder stamp started appearing in progress notes, said Dr. Rut, an ob.gyn. in private practice in Bay Shore, N.Y. She led the study while she was a resident at Winthrop University Hospital, Mineola, N.Y.
The study received top prize among posters presented at the meeting.
Vaccination rates did not seem to be influenced by the reason for the patient’s visit or a history of abnormal Pap smear results. Only the use of the stamp was associated with vaccination rates.
The charts documented that the physician discussed Gardasil in 19 of 86 (22%) cases before use of the stamp and in 63 of 70 (90%) cases after use of the stamp, a significant increase. Still, less than half of eligible patients received the vaccine. When Gardasil was discussed, patients refused vaccination in 34 of 63 (54%) cases. The high refusal rate despite counseling suggests a need to investigate the type of patient education and its content, Dr. Rut suggested.
Patients averaged 23 years of age before use of the stamp and 22 years after the stamp, a statistically significant difference. The two groups did not differ significantly in the type of insurance, the reason for the visit, or the percentage with a previous abnormal Pap smear.
Each of the six medical providers increased their vaccination rates; the increase was statistically significant for three of them. The nurse practitioner had the highest vaccination rate before use of the stamp (4 of 12, or 33%) and after implementation of the stamp (11 of 14, or 79%), a significant increase.
One physician significantly increased vaccination rates from 6% before the stamp (1 of 17 patients) to 62% after the stamp (8 of 13 patients). Another physician significantly improved from vaccinating none of 14 patients before the stamp to 7 of 12 patients after the stamp (58%).
Of the three physicians whose improvement did not reach statistical significance, one went from vaccinating none of 15 patients before the stamp to 1 of 10 patients (10%) after the stamp. Another physician vaccinated 2 of 12 patients at baseline (17%) and 4 of 7 patients after the stamp started (57%). The third physician vaccinated 2 of 16 patients at baseline (13%) and 3 of 14 patients after the stamp (21%).
Overall, the vaccination rate increased from 9 of 86 patients before the stamp (11%) to 34 of 70 patients with use of the stamp (49%), Dr. Rut said.
The stamp included five boxes that the physician could check off: "Start series today," "Series in-progress," "3-vaccine series completed," "Counseled but refuses," and "Other."
As the use of electronic health records increases, perhaps a Gardasil reminder could be incorporated instead of a physical stamp to improve vaccination rates even more, she suggested.
Dr. Rut reported having no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS