User login
Starting from the ground up!
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).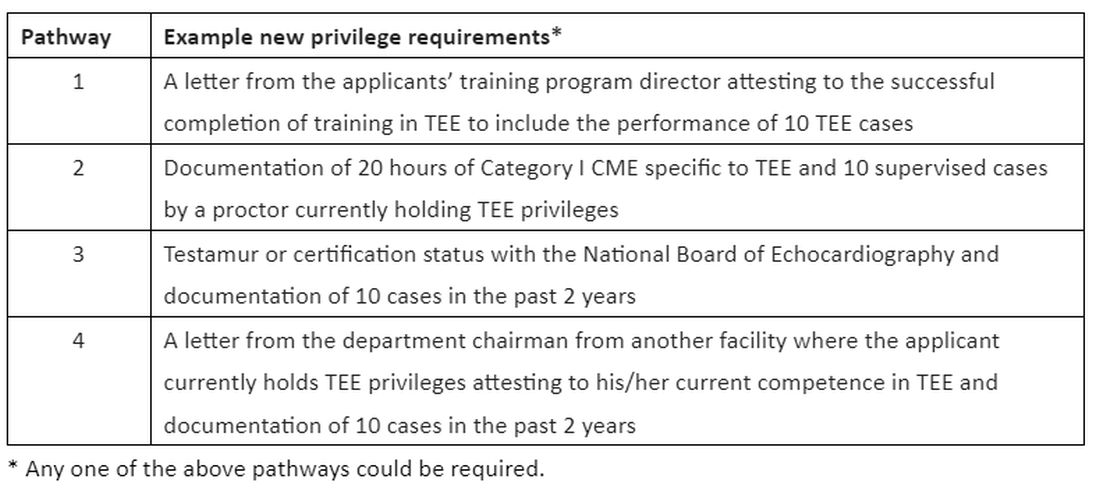
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
Starting from the ground up!
Starting from the ground up!
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).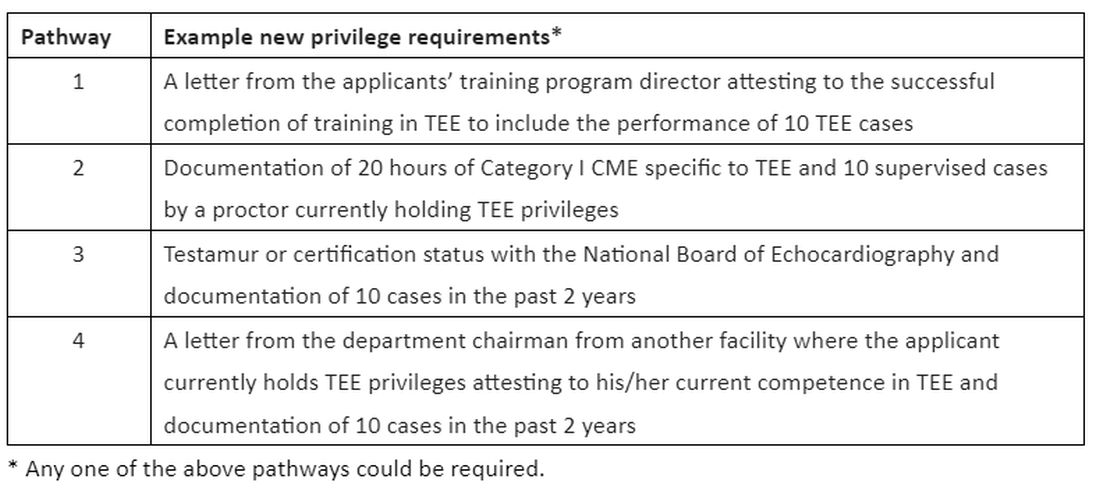
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
Bedside-focused cardiac ultrasound assessment, or cardiac point-of-care ultrasound (POCUS), has become common in intensive care units throughout the US and the world.
However, obtaining images adequate for decision making via standard transthoracic echo (TTE) is not possible in a significant number of patients; as high as 30% of critically ill patients, according to The American Society of Echocardiography (ASE) guidelines.1 Factors common to critically ill patients, such as invasive mechanical ventilation, external dressings, and limited mobility, contribute to poor image acquisition.
In almost all these cases, the factors limiting image acquisition can be eliminated by utilizing a transesophageal approach. In a recent study, researchers were able to demonstrate that adding transesophageal echocardiography (TEE) to TTE in critically ill patients yielded a new diagnosis or a change in management about 45% of the time.2
Using transesophageal ultrasound for a focused cardiac assessment in hemodynamically unstable patients is not new—and is often referred to as rescue TEE or resuscitative TEE. A broader term, transesophageal ultrasound, has also been used to include sonographic evaluation of the lungs in patients with poor acoustic windows. At my institution, we use the term critical care TEE to define TEE performed by a noncardiology-trained intensivist in an intubated critically ill patient.
Regardless of the term, the use of transesophageal ultrasound by the noncardiologist in the ICU appears to be a developing trend. As with other uses of POCUS, ultrasound machines continue to be able to “do more” at a lower price point. In 2024, several cart-based ultrasound machines are compatible with transesophageal probes and contain software packages capable of common cardiac measurements.
Despite this growing interest, intensivists are likely to encounter barriers to implementing critical care TEE. Our division recently implemented adding TEE to our practice. Our practice involves two separate systems: a Veterans Administration hospital and a university-based county hospital. Our division has integrated the use of TEE in the medical ICU at both institutions. Having navigated the process at both institutions, I can offer some guidance in navigating barriers.
The development of a critical care TEE program must start with a strong base in transthoracic cardiac POCUS, at least for the foreseeable future. Having a strong background in TTE gives learners a solid foundation in cardiac anatomy, cardiac function, and ultrasound properties. Obtaining testamur status or board certification in critical care echocardiography is not an absolute must but is a definite benefit. Having significant experience in TTE image acquisition and interpretation will flatten the learning curve for TEE. Interestingly, image acquisition in TEE is often easier than in TTE, so the paradigm of learning TTE before TEE may reverse in the years to come.
Two barriers often work together to create a vicious cycle that stops the development of a TEE program at its start. These barriers include the lack of training and lack of equipment, specifically a TEE probe. Those who do not understand the value of TEE may ask, “Why purchase equipment for a procedure that you do not yet know how to do?” The opposite question can also be asked, “Why get trained to do something you don’t have the equipment to perform?”
My best advice to break this cycle is to “dive in” to whichever barrier seems easier to overcome first. I started with obtaining knowledge and training. Obtaining training and education in a procedure that is historically not done in your specialty is challenging but is not impossible. It takes a combination of high levels of self-motivation and at least one colleague with the training to support you. I approached a cardiac anesthesiologist, whom I knew from the surgical ICU. Cardiologists can also be a resource, but working with cardiac anesthesiologists offers several advantages. TEEs done by cardiac anesthesiologists are similar to those done in ICU patients (ie, all patients are intubated and sedated). The procedures are also scheduled several days in advance, making it easier to integrate training into your daily work schedule. Lastly, the TEE probe remains in place for several hours, so repeating the probe manipulations again as a learner does not add additional risk to the patient. In my case, we somewhat arbitrarily agreed that I participate in 25 TEE exams. (CME courses, both online and in-person simulation, exist and greatly supplement self-study.)
Obtaining equipment is also a common barrier, though this has become less restrictive in the last several years. As previously mentioned, many cart-based ultrasound machines can accommodate a TEE probe. This changes the request from purchasing a new machine to “just a probe.” Despite the higher cost than most other probes, those in charge of purchasing are often more open to purchasing “a probe” than to purchasing an ultrasound machine.
Additionally, the purchasing decision regarding probes may fall to a different person than it does for an ultrasound machine. If available, POCUS image archiving into the medical record can help offset the cost of equipment, both by increasing revenue via billing and by demonstrating that equipment is being used. If initially declined, continue to ask and work to integrate the purchase into the next year’s budget. Inquire about the process of making a formal request and follow that process. This will often involve obtaining a quote or quotes from the ultrasound manufacturer(s).
Keep in mind that the probe will require a special storage cabinet specifically designed for TEE probes. It is prudent to include this in budget requests. If needed, the echocardiography lab can be a useful resource for additional information regarding the cabinet requirements. It is strongly recommended to discuss TEE probe models with sterile processing before any purchasing. If options are available, it is wise to choose a model the hospital already uses, as the cleaning protocol is well established. Our unit purchased a model that did not have an established protocol, which took nearly 6 months to develop. If probe options are limited, involving sterile processing early to start developing a protocol will help decrease delays.
Obtaining hospital privileges is also a common barrier, though this may not be as challenging as expected. Hospitals typically have well-outlined policies on obtaining privileges for established procedures. One of our hospital systems had four different options; the most straightforward required 20 hours of CME specific to TEE and 10 supervised cases by a proctor currently holding TEE privileges (see Table 1).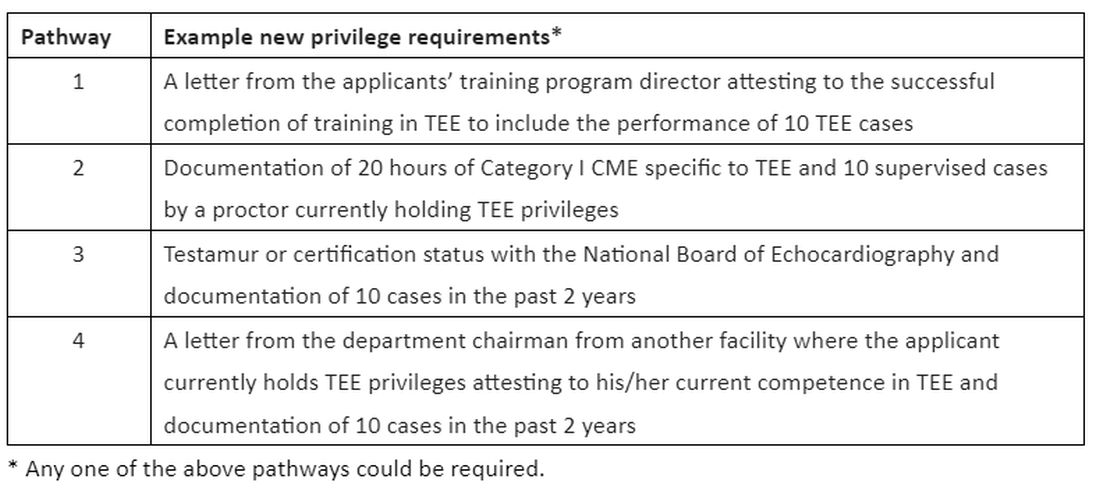
Discussions about obtaining privileges should involve your division chief, chair of medicine, and the cardiology division chief. Clearly outlining the plan to perform this procedure only in critically ill patients who are already intubated for other reasons made these conversations go much more smoothly. In the development of delineation of privileges, we used the term critical care TEE to clearly define this patient population. During these conversations, highlight the safety of the procedure; ASE guidelines3 estimate a severe complication rate of less than 1 in 10,000 cases and explain the anticipated benefits to critically ill patients.
In conclusion, at an institution that is already adept at the use of POCUS in the ICU, the additional of critical care TEE within 1 to 2 years is a very realistic achievement. It will undoubtedly require patience, persistence, and self-motivation, but the barriers are becoming smaller every day. Stay motivated!
Dr. Proud is Associate Professor of Medicine, Division of Pulmonary and Critical Care Medicine, Pulmonary and Critical Care Medicine Program Director, UT Health San Antonio.
References:
1. Porter TR, Abdelmoneim S, Belcik FT, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2024;27(8):797-810.
2. Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med. 2020;8(12):785.
3. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a cmprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardioraphy and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.

