User login
The newly approved 52-mg levonorgestrel intrauterine contraceptive (LNG20) system demonstrated safety and efficacy for 3 years for a range of women, regardless of weight or parity, according to a study of 1,750 women recently published in Contraception.
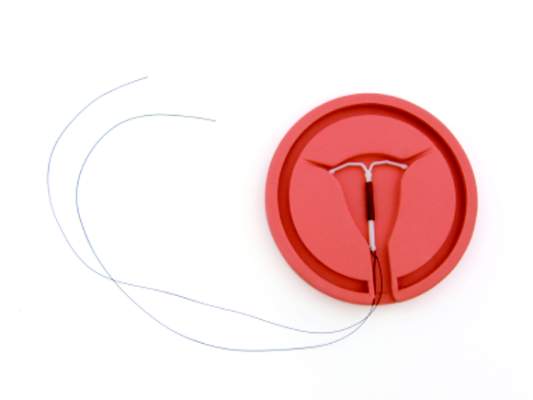
In February, the Food and Drug Administration approved the new hormonal intrauterine contraceptive system, which is now being marketed in the United States as Liletta (LNG20) by the Dublin-based pharmaceutical company Actavis and the nonprofit women’s health pharmaceutical company Medicines360. The LNG20 is a flexible, plastic T-frame measuring 32 mm × 32 mm with a release rate–controlling membrane over a reservoir containing 52 mg levonorgestrel. The system is indicated to prevent pregnancy for up to 3 years.
The newly published data include 3 years of results from the ACCESS IUS study (A Comprehensive Contraceptive Efficacy and Safety Study of an IUS). The multicenter study is ongoing and will evaluate the safety and effectiveness of the system for up to 7 years of use.
Dr. Mitchell Creinin of the University of California, Davis, and colleagues recruited 1,600 U.S. women aged 16-35 years and 151 women aged 36-45 years.
Overall, the pregnancy rate (as measured by the Pearl Index) was 0.15 (95% confidence interval, 0.02-0.55) per 100 women-years through the first year of the study. Through year 2, the Pearl Index was 0.26 (95% CI, 0.10-0.57), and 0.22 (95% CI, 0.08-0.49) through year 3. The cumulative life-table pregnancy rate was 0.55 (95% CI, 0.24-1.23) through 3 years (Contraception 2015 [doi:10.1016/j.contraception.2015.04.006]).
The researchers reported a total of six pregnancies in the study cohort, four of which were ectopic. Four of the six pregnancies occurred in parous women.
Expulsion of the device leading to discontinuation occurred in 3.5% of women (n = 62), mostly in the first year of use and more frequently among subjects who had previously given birth. Other adverse effects leading to discontinuation of use included bleeding, acne, and mood swings.
Symptomatic ovarian cysts developed in 3.4% of the cohort, though only five patients discontinued for this reason. Pelvic infection (including endometriosis) occurred in 10 women, with seven cases of pelvic inflammatory disease and three cases of endometritis.
Of the 68 women followed for fertility outcomes after discontinuing the device, 70.6% conceived spontaneously within 6 months and 86.8% within a year, with a median time to conception of 4 months.
Based on the safety and effectiveness findings, the researchers concluded that the LNG20 system meets the criteria defined by the Centers for Disease Control and Prevention and the World Health Organization for highly effective contraceptive methods.
The study, conducted exclusively in the United States, is notable because a quarter of the cohort had a body mass index of 30 or greater, with 5% of study participants having a BMI of 40 or greater; nearly 60% of the study participants were nulliparous.
It was conducted at 29 sites including public, private, and university clinics and enrolled 13.3% African American, 14.7% Hispanic, and 78.4% white subjects, in keeping with the expected racial, age, and weight characteristics of women likely to use this method of contraception, the researchers noted.
The study enrolled “a substantial number of nulliparous participants, representing 57.7% of the study efficacy population,” the researchers wrote. “This number was not a result of targeted recruitment and thus may represent the interest of nulliparous U.S. women in using highly effective contraceptives such as an IUS.”
Despite the high number of nulliparous subjects, 98.7% of placement attempts were successful.
Although IUDs have been available in the United States for decades, adoption remains low, with less than 8% of U.S. women using them as their preferred method of contraception. The new contraceptive system “will address some of the barriers that have previously limited full access to intrauterine contraceptives,” the researchers wrote.
The study was sponsored by Medicines360. The researchers reported having no financial disclosures.
The newly approved 52-mg levonorgestrel intrauterine contraceptive (LNG20) system demonstrated safety and efficacy for 3 years for a range of women, regardless of weight or parity, according to a study of 1,750 women recently published in Contraception.
In February, the Food and Drug Administration approved the new hormonal intrauterine contraceptive system, which is now being marketed in the United States as Liletta (LNG20) by the Dublin-based pharmaceutical company Actavis and the nonprofit women’s health pharmaceutical company Medicines360. The LNG20 is a flexible, plastic T-frame measuring 32 mm × 32 mm with a release rate–controlling membrane over a reservoir containing 52 mg levonorgestrel. The system is indicated to prevent pregnancy for up to 3 years.
The newly published data include 3 years of results from the ACCESS IUS study (A Comprehensive Contraceptive Efficacy and Safety Study of an IUS). The multicenter study is ongoing and will evaluate the safety and effectiveness of the system for up to 7 years of use.
Dr. Mitchell Creinin of the University of California, Davis, and colleagues recruited 1,600 U.S. women aged 16-35 years and 151 women aged 36-45 years.
Overall, the pregnancy rate (as measured by the Pearl Index) was 0.15 (95% confidence interval, 0.02-0.55) per 100 women-years through the first year of the study. Through year 2, the Pearl Index was 0.26 (95% CI, 0.10-0.57), and 0.22 (95% CI, 0.08-0.49) through year 3. The cumulative life-table pregnancy rate was 0.55 (95% CI, 0.24-1.23) through 3 years (Contraception 2015 [doi:10.1016/j.contraception.2015.04.006]).
The researchers reported a total of six pregnancies in the study cohort, four of which were ectopic. Four of the six pregnancies occurred in parous women.
Expulsion of the device leading to discontinuation occurred in 3.5% of women (n = 62), mostly in the first year of use and more frequently among subjects who had previously given birth. Other adverse effects leading to discontinuation of use included bleeding, acne, and mood swings.
Symptomatic ovarian cysts developed in 3.4% of the cohort, though only five patients discontinued for this reason. Pelvic infection (including endometriosis) occurred in 10 women, with seven cases of pelvic inflammatory disease and three cases of endometritis.
Of the 68 women followed for fertility outcomes after discontinuing the device, 70.6% conceived spontaneously within 6 months and 86.8% within a year, with a median time to conception of 4 months.
Based on the safety and effectiveness findings, the researchers concluded that the LNG20 system meets the criteria defined by the Centers for Disease Control and Prevention and the World Health Organization for highly effective contraceptive methods.
The study, conducted exclusively in the United States, is notable because a quarter of the cohort had a body mass index of 30 or greater, with 5% of study participants having a BMI of 40 or greater; nearly 60% of the study participants were nulliparous.
It was conducted at 29 sites including public, private, and university clinics and enrolled 13.3% African American, 14.7% Hispanic, and 78.4% white subjects, in keeping with the expected racial, age, and weight characteristics of women likely to use this method of contraception, the researchers noted.
The study enrolled “a substantial number of nulliparous participants, representing 57.7% of the study efficacy population,” the researchers wrote. “This number was not a result of targeted recruitment and thus may represent the interest of nulliparous U.S. women in using highly effective contraceptives such as an IUS.”
Despite the high number of nulliparous subjects, 98.7% of placement attempts were successful.
Although IUDs have been available in the United States for decades, adoption remains low, with less than 8% of U.S. women using them as their preferred method of contraception. The new contraceptive system “will address some of the barriers that have previously limited full access to intrauterine contraceptives,” the researchers wrote.
The study was sponsored by Medicines360. The researchers reported having no financial disclosures.
The newly approved 52-mg levonorgestrel intrauterine contraceptive (LNG20) system demonstrated safety and efficacy for 3 years for a range of women, regardless of weight or parity, according to a study of 1,750 women recently published in Contraception.
In February, the Food and Drug Administration approved the new hormonal intrauterine contraceptive system, which is now being marketed in the United States as Liletta (LNG20) by the Dublin-based pharmaceutical company Actavis and the nonprofit women’s health pharmaceutical company Medicines360. The LNG20 is a flexible, plastic T-frame measuring 32 mm × 32 mm with a release rate–controlling membrane over a reservoir containing 52 mg levonorgestrel. The system is indicated to prevent pregnancy for up to 3 years.
The newly published data include 3 years of results from the ACCESS IUS study (A Comprehensive Contraceptive Efficacy and Safety Study of an IUS). The multicenter study is ongoing and will evaluate the safety and effectiveness of the system for up to 7 years of use.
Dr. Mitchell Creinin of the University of California, Davis, and colleagues recruited 1,600 U.S. women aged 16-35 years and 151 women aged 36-45 years.
Overall, the pregnancy rate (as measured by the Pearl Index) was 0.15 (95% confidence interval, 0.02-0.55) per 100 women-years through the first year of the study. Through year 2, the Pearl Index was 0.26 (95% CI, 0.10-0.57), and 0.22 (95% CI, 0.08-0.49) through year 3. The cumulative life-table pregnancy rate was 0.55 (95% CI, 0.24-1.23) through 3 years (Contraception 2015 [doi:10.1016/j.contraception.2015.04.006]).
The researchers reported a total of six pregnancies in the study cohort, four of which were ectopic. Four of the six pregnancies occurred in parous women.
Expulsion of the device leading to discontinuation occurred in 3.5% of women (n = 62), mostly in the first year of use and more frequently among subjects who had previously given birth. Other adverse effects leading to discontinuation of use included bleeding, acne, and mood swings.
Symptomatic ovarian cysts developed in 3.4% of the cohort, though only five patients discontinued for this reason. Pelvic infection (including endometriosis) occurred in 10 women, with seven cases of pelvic inflammatory disease and three cases of endometritis.
Of the 68 women followed for fertility outcomes after discontinuing the device, 70.6% conceived spontaneously within 6 months and 86.8% within a year, with a median time to conception of 4 months.
Based on the safety and effectiveness findings, the researchers concluded that the LNG20 system meets the criteria defined by the Centers for Disease Control and Prevention and the World Health Organization for highly effective contraceptive methods.
The study, conducted exclusively in the United States, is notable because a quarter of the cohort had a body mass index of 30 or greater, with 5% of study participants having a BMI of 40 or greater; nearly 60% of the study participants were nulliparous.
It was conducted at 29 sites including public, private, and university clinics and enrolled 13.3% African American, 14.7% Hispanic, and 78.4% white subjects, in keeping with the expected racial, age, and weight characteristics of women likely to use this method of contraception, the researchers noted.
The study enrolled “a substantial number of nulliparous participants, representing 57.7% of the study efficacy population,” the researchers wrote. “This number was not a result of targeted recruitment and thus may represent the interest of nulliparous U.S. women in using highly effective contraceptives such as an IUS.”
Despite the high number of nulliparous subjects, 98.7% of placement attempts were successful.
Although IUDs have been available in the United States for decades, adoption remains low, with less than 8% of U.S. women using them as their preferred method of contraception. The new contraceptive system “will address some of the barriers that have previously limited full access to intrauterine contraceptives,” the researchers wrote.
The study was sponsored by Medicines360. The researchers reported having no financial disclosures.
FROM CONTRACEPTION
Key clinical point: A recently approved hormonal intrauterine system (LNG20) is highly effective and safe for up to 3 years of use in parous and nulliparous women, as well as obese women.
Major finding: The Pearl Index for LNG20 was 0.15 (95% CI, 0.02-0.55) through year 1, 0.26 (95% CI, 0.10-0.57) through year 2, and 0.22 (95% CI, 0.08-0.49) through year 3, with an expulsion rate of 3.5%. Conception occurred within 12 months in 87% of patients who discontinued to become pregnant.
Data source: Prospective efficacy and safety cohort study of 1,600 sexually active U.S. women aged 16-35 years and 151 women aged 36-45 years recruited from 29 public, private, and university centers.
Disclosures: Sponsored by Medicines 360, a nonprofit women’s health pharmaceutical company. The researchers reported having no financial disclosures.