User login
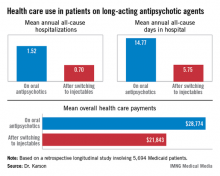
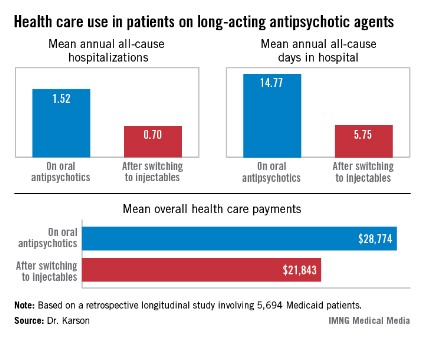
HOLLYWOOD, FLA. – Once patients were switched from oral antipsychotic agents to long-acting injectable ones, their annual all-cause hospitalization rate was cut by more than half in an observational study involving nearly 6,000 Medicaid patients with schizophrenia.
Moreover, the mean number of days per year spent in the hospital for any reason also dropped dramatically after the switch. Plus, the mean overall annual health care costs decreased by $6,901, Dr. Craig N. Karson reported at a meeting of the New Clinical Drug Evaluation Unit sponsored by the National Institute of Mental Health.
"We may have an opportunity here to improve the management of schizophrenia, and in particular the cost management," said Dr. Karson, a psychiatrist in Wayne, Pa.
He presented a retrospective longitudinal study of 5,694 Medicaid patients with schizophrenia who switched from oral to long-acting injectable antipsychotics during 2005-2010. The data came from the Thomson Reuters MarketScan Research Medicaid Database.
Forty-four percent of patients were placed on long-acting injectable risperidone, 41% on haloperidol, and the rest on fluphenazine, which were the three antipsychotic agents available in depot form during the study period.
Roughly 80% of the all-cause hospitalizations in this study were for schizophrenia.
The switch from oral to long-acting injectable antipsychotic agents was associated with a striking reduction in overall health care resource use, including a decrease in the mean annual number of all-cause hospitalizations from 1.52 to 0.70 (see box).
In order to see whether patients’ duration on long-acting injectable antipsychotics was related to health care resource use, Dr. Karson and his coinvestigators divided the study population into two groups: the 2,856 patients who were short-term users of long-acting injectable therapy, defined as less than 180 days of treatment; and the 2,838 users of long-acting injectables for at least 180 days. The short-term users averaged 0.79 all-cause hospitalizations annually; the long-term users, 0.61. The mean annualized total days in the hospital was 6.56 for the short-term users, compared with 4.93 in longer-term users.
Several speakers argued that the MarketScan database has significant methodologic shortcomings, including selection bias, rendering it better suited as a basis for hypothesis generation than for drawing firm conclusions. Dr. Karson acknowledged that the database is limited in that it provides a convenience sample rather than a random sample of the Medicaid population, but he argued that the shear size of the study population overcomes that limitation.
"Ask yourself, how many treatment studies do we have in psychiatry with almost 6,000 patients? Very few," he said. "When you get into these kinds of patient numbers, which provide enormous statistical power, and then use a very hard endpoint like annual all-cause hospitalizations, I think it changes the game a little. I would argue that these patients are representative of the Medicaid population with serious mental illness, regardless."
Discussant Dr. Stephen R. Marder, who was not involved in the study, agreed that the data are compelling."
"The differences seen in your study were large and persuasive. And I thought the analysis of short- versus long-term use showing a dose-response effect added to the confidence in the results. Being on depot medication longer makes a difference," concluded Dr. Marder, director of the section on psychosis at the University of California, Los Angeles, Neuropsychiatric Institute.
"The problem lies with us as providers: We see long-acting injectable antipsychotics as the last resort, said Dr. Marder, also professor of psychiatry and behavioral sciences at UCLA. "We’re probably reluctant to do it because we see the infrastructure for providing the therapy is very poor in many places."
At the VA medical center where he works, for example, patients formerly had access to depot medication on a 24/7 basis, so that if they had a job, they could obtain treatment without missing work. That service isn’t available, anymore, Dr. Marder noted.
His hope, he added, is that thought leaders in psychiatry will be able to influence implementation of the Affordable Care Act so as to create a much better infrastructure for providing long-acting injectable antipsychotic therapy. Ideally, access to long-acting injectable antipsychotics should be available in places where psychosocial and rehabilitation services are located. "That’s what seems to work the best," according to the psychiatrist.
Dr. Karson reported serving as a consultant to Otsuka America Pharmaceutical, which funded the study he presented, and to the Lieber Institute for Brain Development. Dr. Marder is a consultant to and/or has received research funding from Otsuka and 10 other companies.
HOLLYWOOD, FLA. – Once patients were switched from oral antipsychotic agents to long-acting injectable ones, their annual all-cause hospitalization rate was cut by more than half in an observational study involving nearly 6,000 Medicaid patients with schizophrenia.
Moreover, the mean number of days per year spent in the hospital for any reason also dropped dramatically after the switch. Plus, the mean overall annual health care costs decreased by $6,901, Dr. Craig N. Karson reported at a meeting of the New Clinical Drug Evaluation Unit sponsored by the National Institute of Mental Health.
"We may have an opportunity here to improve the management of schizophrenia, and in particular the cost management," said Dr. Karson, a psychiatrist in Wayne, Pa.
He presented a retrospective longitudinal study of 5,694 Medicaid patients with schizophrenia who switched from oral to long-acting injectable antipsychotics during 2005-2010. The data came from the Thomson Reuters MarketScan Research Medicaid Database.
Forty-four percent of patients were placed on long-acting injectable risperidone, 41% on haloperidol, and the rest on fluphenazine, which were the three antipsychotic agents available in depot form during the study period.
Roughly 80% of the all-cause hospitalizations in this study were for schizophrenia.
The switch from oral to long-acting injectable antipsychotic agents was associated with a striking reduction in overall health care resource use, including a decrease in the mean annual number of all-cause hospitalizations from 1.52 to 0.70 (see box).
In order to see whether patients’ duration on long-acting injectable antipsychotics was related to health care resource use, Dr. Karson and his coinvestigators divided the study population into two groups: the 2,856 patients who were short-term users of long-acting injectable therapy, defined as less than 180 days of treatment; and the 2,838 users of long-acting injectables for at least 180 days. The short-term users averaged 0.79 all-cause hospitalizations annually; the long-term users, 0.61. The mean annualized total days in the hospital was 6.56 for the short-term users, compared with 4.93 in longer-term users.
Several speakers argued that the MarketScan database has significant methodologic shortcomings, including selection bias, rendering it better suited as a basis for hypothesis generation than for drawing firm conclusions. Dr. Karson acknowledged that the database is limited in that it provides a convenience sample rather than a random sample of the Medicaid population, but he argued that the shear size of the study population overcomes that limitation.
"Ask yourself, how many treatment studies do we have in psychiatry with almost 6,000 patients? Very few," he said. "When you get into these kinds of patient numbers, which provide enormous statistical power, and then use a very hard endpoint like annual all-cause hospitalizations, I think it changes the game a little. I would argue that these patients are representative of the Medicaid population with serious mental illness, regardless."
Discussant Dr. Stephen R. Marder, who was not involved in the study, agreed that the data are compelling."
"The differences seen in your study were large and persuasive. And I thought the analysis of short- versus long-term use showing a dose-response effect added to the confidence in the results. Being on depot medication longer makes a difference," concluded Dr. Marder, director of the section on psychosis at the University of California, Los Angeles, Neuropsychiatric Institute.
"The problem lies with us as providers: We see long-acting injectable antipsychotics as the last resort, said Dr. Marder, also professor of psychiatry and behavioral sciences at UCLA. "We’re probably reluctant to do it because we see the infrastructure for providing the therapy is very poor in many places."
At the VA medical center where he works, for example, patients formerly had access to depot medication on a 24/7 basis, so that if they had a job, they could obtain treatment without missing work. That service isn’t available, anymore, Dr. Marder noted.
His hope, he added, is that thought leaders in psychiatry will be able to influence implementation of the Affordable Care Act so as to create a much better infrastructure for providing long-acting injectable antipsychotic therapy. Ideally, access to long-acting injectable antipsychotics should be available in places where psychosocial and rehabilitation services are located. "That’s what seems to work the best," according to the psychiatrist.
Dr. Karson reported serving as a consultant to Otsuka America Pharmaceutical, which funded the study he presented, and to the Lieber Institute for Brain Development. Dr. Marder is a consultant to and/or has received research funding from Otsuka and 10 other companies.
HOLLYWOOD, FLA. – Once patients were switched from oral antipsychotic agents to long-acting injectable ones, their annual all-cause hospitalization rate was cut by more than half in an observational study involving nearly 6,000 Medicaid patients with schizophrenia.
Moreover, the mean number of days per year spent in the hospital for any reason also dropped dramatically after the switch. Plus, the mean overall annual health care costs decreased by $6,901, Dr. Craig N. Karson reported at a meeting of the New Clinical Drug Evaluation Unit sponsored by the National Institute of Mental Health.
"We may have an opportunity here to improve the management of schizophrenia, and in particular the cost management," said Dr. Karson, a psychiatrist in Wayne, Pa.
He presented a retrospective longitudinal study of 5,694 Medicaid patients with schizophrenia who switched from oral to long-acting injectable antipsychotics during 2005-2010. The data came from the Thomson Reuters MarketScan Research Medicaid Database.
Forty-four percent of patients were placed on long-acting injectable risperidone, 41% on haloperidol, and the rest on fluphenazine, which were the three antipsychotic agents available in depot form during the study period.
Roughly 80% of the all-cause hospitalizations in this study were for schizophrenia.
The switch from oral to long-acting injectable antipsychotic agents was associated with a striking reduction in overall health care resource use, including a decrease in the mean annual number of all-cause hospitalizations from 1.52 to 0.70 (see box).
In order to see whether patients’ duration on long-acting injectable antipsychotics was related to health care resource use, Dr. Karson and his coinvestigators divided the study population into two groups: the 2,856 patients who were short-term users of long-acting injectable therapy, defined as less than 180 days of treatment; and the 2,838 users of long-acting injectables for at least 180 days. The short-term users averaged 0.79 all-cause hospitalizations annually; the long-term users, 0.61. The mean annualized total days in the hospital was 6.56 for the short-term users, compared with 4.93 in longer-term users.
Several speakers argued that the MarketScan database has significant methodologic shortcomings, including selection bias, rendering it better suited as a basis for hypothesis generation than for drawing firm conclusions. Dr. Karson acknowledged that the database is limited in that it provides a convenience sample rather than a random sample of the Medicaid population, but he argued that the shear size of the study population overcomes that limitation.
"Ask yourself, how many treatment studies do we have in psychiatry with almost 6,000 patients? Very few," he said. "When you get into these kinds of patient numbers, which provide enormous statistical power, and then use a very hard endpoint like annual all-cause hospitalizations, I think it changes the game a little. I would argue that these patients are representative of the Medicaid population with serious mental illness, regardless."
Discussant Dr. Stephen R. Marder, who was not involved in the study, agreed that the data are compelling."
"The differences seen in your study were large and persuasive. And I thought the analysis of short- versus long-term use showing a dose-response effect added to the confidence in the results. Being on depot medication longer makes a difference," concluded Dr. Marder, director of the section on psychosis at the University of California, Los Angeles, Neuropsychiatric Institute.
"The problem lies with us as providers: We see long-acting injectable antipsychotics as the last resort, said Dr. Marder, also professor of psychiatry and behavioral sciences at UCLA. "We’re probably reluctant to do it because we see the infrastructure for providing the therapy is very poor in many places."
At the VA medical center where he works, for example, patients formerly had access to depot medication on a 24/7 basis, so that if they had a job, they could obtain treatment without missing work. That service isn’t available, anymore, Dr. Marder noted.
His hope, he added, is that thought leaders in psychiatry will be able to influence implementation of the Affordable Care Act so as to create a much better infrastructure for providing long-acting injectable antipsychotic therapy. Ideally, access to long-acting injectable antipsychotics should be available in places where psychosocial and rehabilitation services are located. "That’s what seems to work the best," according to the psychiatrist.
Dr. Karson reported serving as a consultant to Otsuka America Pharmaceutical, which funded the study he presented, and to the Lieber Institute for Brain Development. Dr. Marder is a consultant to and/or has received research funding from Otsuka and 10 other companies.
AT THE NCDEU MEETING
Major finding: Medicaid patients with schizophrenia had a mean 1.52 hospitalizations per year for any cause while they were on oral antipsychotic medication, dropping to 0.7 all-cause hospitalizations per year after they switched to long-acting injectable therapy.
Data source: A retrospective observational study involving 5,694 Medicaid patients with schizophrenia drawn from the Thomson Reuters MarketScan Research Medicaid Database.
Disclosures: Dr. Karson reported serving as a consultant to Otsuka America Pharmaceutical, which funded the study he presented, and to the Lieber Institute for Brain Development. Dr. Marder is a consultant to and/or has received research funding from Otsuka and 10 other companies.