User login
The updated practice guideline for managing adults with valvular heart disease has a new, "modular" format to facilitate clinicians' access to "concise, relevant bytes of information at the point of care, when clinical knowledge is needed most," according to reports published online simultaneously March 3 in Circulation and the Journal of the American College of Cardiology.
The guideline, compiled by a committee of cardiologists, interventionalists, surgeons, and anesthesiologists under the aegis of the American Heart Association and the American College of Cardiology, was last updated in 2008.
"Some recommendations from the earlier valvular heart disease guideline have been updated as warranted by new evidence or a better understanding of earlier evidence, whereas others that were inaccurate, irrelevant, or overlapping were deleted or modified," said writing committee cochairs Dr. Rick A. Nishimura of the division of cardiovascular diseases, Mayo Clinic, Rochester, Minn.; and Dr. Catherine M. Otto, director of the University of Washington Medical Center's Heart Valve Clinic, Seattle.
The narrative text of the guideline is limited, and instead it uses decision pathway diagrams and numerous summary tables of current evidence and recommendations. These include links to relevant references. It is hoped that clinicians can more easily use the new guideline as a quick reference. This format also will enable individual sections to be updated or amended as new evidence comes to light. The PDF of the guideline is available for free.
"This novel approach to evidence-based guideline development will revolutionize the clinical impact of guideline recommendations, ensuring they are always current and allowing seamless integration with electronic medical record systems," Dr. Otto said in a press statement accompanying the reports.
The guideline now includes gradations of disease severity, to help clinicians determine the optimal timing of intervention. Whether or not intervention is indicated depends on five factors: the presence or absence of symptoms, the severity of valvular heart disease, the response of the left and/or right ventricle to the volume or pressure overload caused by the valvular disease, the effect on the pulmonary or systemic circulation, and any change in heart rhythm.
Disease severity ranges from stage A, "at risk," which denotes patients who have risk factors for developing valvular heart disease; through stage B, "progressive," which indicates patients who are asymptomatic but have mildly to moderately severe disease; through stage C, "asymptomatic severe," which includes patients with severe yet still asymptomatic valvular disease in which the left or right ventricle remains compensated or in which the left or right ventricle has decompensated; to stage D, "symptomatic severe," which indicates patients whose severe valvular disease has produced symptoms.
"In patients with stenotic lesions, there is an additional category of 'very severe' stenosis based on studies of the natural history showing that prognosis becomes poorer as the severity of stenosis increases," the guideline states.
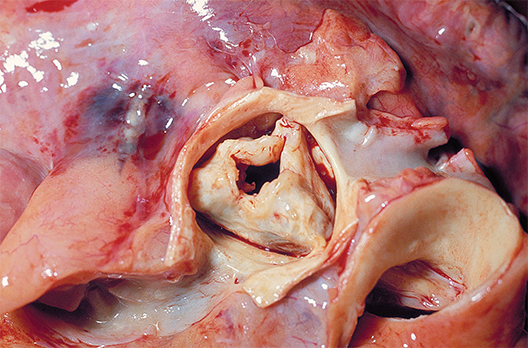
Information is provided for assessing the various disease states associated with the aortic, mitral, and tricuspid valves, and addresses the issues of valve repair, replacement, and the use of prosthetic valves.
Compared with the previous guideline, the new one suggests surgical intervention at an earlier stage for certain patients. "Due to more knowledge regarding the natural history of untreated patients with severe valvular heart disease and better outcomes from surgery, we've lowered the threshold for operation to include more patients with asymptomatic severe disease. Now, select patients with severe asymptomatic aortic stenosis and severe asymptomatic mitral regurgitation can be considered for intervention, depending on certain other factors such as operative mortality and … the ability to achieve a durable valve repair," Dr. Nishimura said in the press statement.
The new guideline also proposes a new approach to risk assessment, to be applied to all patients for whom intervention is being considered. Previous risk scoring systems were "useful but limited"; the new approach takes into consideration "procedure-specific impediments, major organ system compromise, comorbidities, patient frailty, and the Society of Thoracic Surgeons predicted risk of mortality model."
For the first time, the guideline discusses transcatheter aortic valve replacement and other catheter-based treatments, new technologies that have improved patient care but also have complicated risk assessment. Separate recommendations are now offered regarding the choice and the timing of these interventions.
In addition to the AHA and the ACC, this guideline was developed in collaboration with the American Association for Thoracic Surgery, American Society for Echocardiography, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons.
The complete 2014 Guideline for the Management of Patients With Valvular Heart Disease is available from the American College of Cardiology and the American Heart Association.
Dr. Nishimura and Dr. Otto reported no financial conflicts of interest; their associates on the ACC/AHA Task Force's writing committee reported ties to Edwards Scientific, Medtronic, and St. Jude Medical.
The updated practice guideline for managing adults with valvular heart disease has a new, "modular" format to facilitate clinicians' access to "concise, relevant bytes of information at the point of care, when clinical knowledge is needed most," according to reports published online simultaneously March 3 in Circulation and the Journal of the American College of Cardiology.
The guideline, compiled by a committee of cardiologists, interventionalists, surgeons, and anesthesiologists under the aegis of the American Heart Association and the American College of Cardiology, was last updated in 2008.
"Some recommendations from the earlier valvular heart disease guideline have been updated as warranted by new evidence or a better understanding of earlier evidence, whereas others that were inaccurate, irrelevant, or overlapping were deleted or modified," said writing committee cochairs Dr. Rick A. Nishimura of the division of cardiovascular diseases, Mayo Clinic, Rochester, Minn.; and Dr. Catherine M. Otto, director of the University of Washington Medical Center's Heart Valve Clinic, Seattle.
The narrative text of the guideline is limited, and instead it uses decision pathway diagrams and numerous summary tables of current evidence and recommendations. These include links to relevant references. It is hoped that clinicians can more easily use the new guideline as a quick reference. This format also will enable individual sections to be updated or amended as new evidence comes to light. The PDF of the guideline is available for free.
"This novel approach to evidence-based guideline development will revolutionize the clinical impact of guideline recommendations, ensuring they are always current and allowing seamless integration with electronic medical record systems," Dr. Otto said in a press statement accompanying the reports.
The guideline now includes gradations of disease severity, to help clinicians determine the optimal timing of intervention. Whether or not intervention is indicated depends on five factors: the presence or absence of symptoms, the severity of valvular heart disease, the response of the left and/or right ventricle to the volume or pressure overload caused by the valvular disease, the effect on the pulmonary or systemic circulation, and any change in heart rhythm.
Disease severity ranges from stage A, "at risk," which denotes patients who have risk factors for developing valvular heart disease; through stage B, "progressive," which indicates patients who are asymptomatic but have mildly to moderately severe disease; through stage C, "asymptomatic severe," which includes patients with severe yet still asymptomatic valvular disease in which the left or right ventricle remains compensated or in which the left or right ventricle has decompensated; to stage D, "symptomatic severe," which indicates patients whose severe valvular disease has produced symptoms.
"In patients with stenotic lesions, there is an additional category of 'very severe' stenosis based on studies of the natural history showing that prognosis becomes poorer as the severity of stenosis increases," the guideline states.
Information is provided for assessing the various disease states associated with the aortic, mitral, and tricuspid valves, and addresses the issues of valve repair, replacement, and the use of prosthetic valves.
Compared with the previous guideline, the new one suggests surgical intervention at an earlier stage for certain patients. "Due to more knowledge regarding the natural history of untreated patients with severe valvular heart disease and better outcomes from surgery, we've lowered the threshold for operation to include more patients with asymptomatic severe disease. Now, select patients with severe asymptomatic aortic stenosis and severe asymptomatic mitral regurgitation can be considered for intervention, depending on certain other factors such as operative mortality and … the ability to achieve a durable valve repair," Dr. Nishimura said in the press statement.
The new guideline also proposes a new approach to risk assessment, to be applied to all patients for whom intervention is being considered. Previous risk scoring systems were "useful but limited"; the new approach takes into consideration "procedure-specific impediments, major organ system compromise, comorbidities, patient frailty, and the Society of Thoracic Surgeons predicted risk of mortality model."
For the first time, the guideline discusses transcatheter aortic valve replacement and other catheter-based treatments, new technologies that have improved patient care but also have complicated risk assessment. Separate recommendations are now offered regarding the choice and the timing of these interventions.
In addition to the AHA and the ACC, this guideline was developed in collaboration with the American Association for Thoracic Surgery, American Society for Echocardiography, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons.
The complete 2014 Guideline for the Management of Patients With Valvular Heart Disease is available from the American College of Cardiology and the American Heart Association.
Dr. Nishimura and Dr. Otto reported no financial conflicts of interest; their associates on the ACC/AHA Task Force's writing committee reported ties to Edwards Scientific, Medtronic, and St. Jude Medical.
The updated practice guideline for managing adults with valvular heart disease has a new, "modular" format to facilitate clinicians' access to "concise, relevant bytes of information at the point of care, when clinical knowledge is needed most," according to reports published online simultaneously March 3 in Circulation and the Journal of the American College of Cardiology.
The guideline, compiled by a committee of cardiologists, interventionalists, surgeons, and anesthesiologists under the aegis of the American Heart Association and the American College of Cardiology, was last updated in 2008.
"Some recommendations from the earlier valvular heart disease guideline have been updated as warranted by new evidence or a better understanding of earlier evidence, whereas others that were inaccurate, irrelevant, or overlapping were deleted or modified," said writing committee cochairs Dr. Rick A. Nishimura of the division of cardiovascular diseases, Mayo Clinic, Rochester, Minn.; and Dr. Catherine M. Otto, director of the University of Washington Medical Center's Heart Valve Clinic, Seattle.
The narrative text of the guideline is limited, and instead it uses decision pathway diagrams and numerous summary tables of current evidence and recommendations. These include links to relevant references. It is hoped that clinicians can more easily use the new guideline as a quick reference. This format also will enable individual sections to be updated or amended as new evidence comes to light. The PDF of the guideline is available for free.
"This novel approach to evidence-based guideline development will revolutionize the clinical impact of guideline recommendations, ensuring they are always current and allowing seamless integration with electronic medical record systems," Dr. Otto said in a press statement accompanying the reports.
The guideline now includes gradations of disease severity, to help clinicians determine the optimal timing of intervention. Whether or not intervention is indicated depends on five factors: the presence or absence of symptoms, the severity of valvular heart disease, the response of the left and/or right ventricle to the volume or pressure overload caused by the valvular disease, the effect on the pulmonary or systemic circulation, and any change in heart rhythm.
Disease severity ranges from stage A, "at risk," which denotes patients who have risk factors for developing valvular heart disease; through stage B, "progressive," which indicates patients who are asymptomatic but have mildly to moderately severe disease; through stage C, "asymptomatic severe," which includes patients with severe yet still asymptomatic valvular disease in which the left or right ventricle remains compensated or in which the left or right ventricle has decompensated; to stage D, "symptomatic severe," which indicates patients whose severe valvular disease has produced symptoms.
"In patients with stenotic lesions, there is an additional category of 'very severe' stenosis based on studies of the natural history showing that prognosis becomes poorer as the severity of stenosis increases," the guideline states.
Information is provided for assessing the various disease states associated with the aortic, mitral, and tricuspid valves, and addresses the issues of valve repair, replacement, and the use of prosthetic valves.
Compared with the previous guideline, the new one suggests surgical intervention at an earlier stage for certain patients. "Due to more knowledge regarding the natural history of untreated patients with severe valvular heart disease and better outcomes from surgery, we've lowered the threshold for operation to include more patients with asymptomatic severe disease. Now, select patients with severe asymptomatic aortic stenosis and severe asymptomatic mitral regurgitation can be considered for intervention, depending on certain other factors such as operative mortality and … the ability to achieve a durable valve repair," Dr. Nishimura said in the press statement.
The new guideline also proposes a new approach to risk assessment, to be applied to all patients for whom intervention is being considered. Previous risk scoring systems were "useful but limited"; the new approach takes into consideration "procedure-specific impediments, major organ system compromise, comorbidities, patient frailty, and the Society of Thoracic Surgeons predicted risk of mortality model."
For the first time, the guideline discusses transcatheter aortic valve replacement and other catheter-based treatments, new technologies that have improved patient care but also have complicated risk assessment. Separate recommendations are now offered regarding the choice and the timing of these interventions.
In addition to the AHA and the ACC, this guideline was developed in collaboration with the American Association for Thoracic Surgery, American Society for Echocardiography, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons.
The complete 2014 Guideline for the Management of Patients With Valvular Heart Disease is available from the American College of Cardiology and the American Heart Association.
Dr. Nishimura and Dr. Otto reported no financial conflicts of interest; their associates on the ACC/AHA Task Force's writing committee reported ties to Edwards Scientific, Medtronic, and St. Jude Medical.