User login
SAN FRANCISCO – Controlled ovarian hyperstimulation and oocyte vitrification were similarly successful in preserving fertility in women with or without cancer, based on a retrospective study of 5 years of experience at one European center.
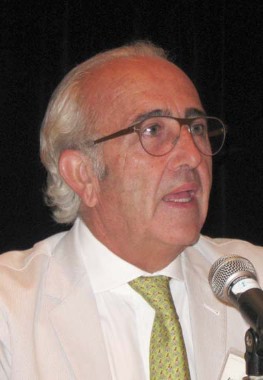
Among 475 oncologic patients and 560 patients with no cancer, 1,080 oocyte vitrification cycles were performed, 33% of them in women with cancer and 67% for nonmedical reasons. So far, 30 women have returned to use their frozen eggs (4 cancer patients and 26 noncancer patients), resulting in 20 pregnancies and 6 live births (in 1 cancer patient and 5 noncancer patients), with 8 pregnancies ongoing, Dr. Antonio Pellicer said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Some differences between the patient groups were seen. The total dose of gonadotropins used and serum estradiol levels were lower in patients who’d had cancer, said Dr. Pellicer, professor of obstetrics and gynecology and director of the Instituto Valenciano de Infertilidad at the University of Valencia (Spain) (Fertil. Steril. 2013;99:1994-9).
The quality of the oocytes seemed similar between groups, but fewer eggs can be retrieved after controlled ovarian stimulation in patients with cancer because some cancers affect the ovaries. Previous work by Dr. Pellicer and his associates showed that a mean of two fewer oocytes are retrieved from patients with hormone-dependent breast cancer, compared with noncancer controls.
Oocyte vitrification is a safe, promising method for fertility preservation not only in patients with cancer but in noncancer patients as well, he said. Approximately 91% of the nonmedical reasons for oocyte vitrification at his center were "social" reasons, Dr. Pellicer said. "This is a procedure that is increasing more and more."
A majority of women treated for breast cancer at his institution lose some ovarian function. Fertility preservation in female cancer patients can take three forms: medical protection of the gonads, ovarian cortex freezing and transplantation, and/or oocyte and embryo vitrification.
Five years of experience with reimplantation of frozen and then thawed ovarian tissue at three European centers showed that 11 of 60 patients who underwent orthotropic reimplantations of cryopreserved ovarian tissue became pregnant, and 6 patients so far have been delivered of 12 healthy infants (Fertil. Steril. 2013;99:1503-13).
The centers in the study included Dr. Pellicer’s institution and centers in Belgium and Denmark. "All of us have done between 800 and 1,000" cases of harvesting and freezing ovarian tissue. Cryopreservation of ovarian tissue may be the only option available to preserve fertility in prepubertal girls facing cancer treatment and for women who cannot delay the start of chemotherapy.
"The technique is promising and improving. I think there is room for it to continue in this direction for women who need fertility preservation," Dr. Pellicer said.
The concern with ovarian tissue cryopreservation has been that it may transplant neoplastic cells. Previous studies by other investigators, however, suggest that this risk is true in patients with leukemias but not in patients with breast cancer or non-Hodgkin’s lymphoma, he said.
Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.
On Twitter @sherryboschert
SAN FRANCISCO – Controlled ovarian hyperstimulation and oocyte vitrification were similarly successful in preserving fertility in women with or without cancer, based on a retrospective study of 5 years of experience at one European center.
Among 475 oncologic patients and 560 patients with no cancer, 1,080 oocyte vitrification cycles were performed, 33% of them in women with cancer and 67% for nonmedical reasons. So far, 30 women have returned to use their frozen eggs (4 cancer patients and 26 noncancer patients), resulting in 20 pregnancies and 6 live births (in 1 cancer patient and 5 noncancer patients), with 8 pregnancies ongoing, Dr. Antonio Pellicer said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Some differences between the patient groups were seen. The total dose of gonadotropins used and serum estradiol levels were lower in patients who’d had cancer, said Dr. Pellicer, professor of obstetrics and gynecology and director of the Instituto Valenciano de Infertilidad at the University of Valencia (Spain) (Fertil. Steril. 2013;99:1994-9).
The quality of the oocytes seemed similar between groups, but fewer eggs can be retrieved after controlled ovarian stimulation in patients with cancer because some cancers affect the ovaries. Previous work by Dr. Pellicer and his associates showed that a mean of two fewer oocytes are retrieved from patients with hormone-dependent breast cancer, compared with noncancer controls.
Oocyte vitrification is a safe, promising method for fertility preservation not only in patients with cancer but in noncancer patients as well, he said. Approximately 91% of the nonmedical reasons for oocyte vitrification at his center were "social" reasons, Dr. Pellicer said. "This is a procedure that is increasing more and more."
A majority of women treated for breast cancer at his institution lose some ovarian function. Fertility preservation in female cancer patients can take three forms: medical protection of the gonads, ovarian cortex freezing and transplantation, and/or oocyte and embryo vitrification.
Five years of experience with reimplantation of frozen and then thawed ovarian tissue at three European centers showed that 11 of 60 patients who underwent orthotropic reimplantations of cryopreserved ovarian tissue became pregnant, and 6 patients so far have been delivered of 12 healthy infants (Fertil. Steril. 2013;99:1503-13).
The centers in the study included Dr. Pellicer’s institution and centers in Belgium and Denmark. "All of us have done between 800 and 1,000" cases of harvesting and freezing ovarian tissue. Cryopreservation of ovarian tissue may be the only option available to preserve fertility in prepubertal girls facing cancer treatment and for women who cannot delay the start of chemotherapy.
"The technique is promising and improving. I think there is room for it to continue in this direction for women who need fertility preservation," Dr. Pellicer said.
The concern with ovarian tissue cryopreservation has been that it may transplant neoplastic cells. Previous studies by other investigators, however, suggest that this risk is true in patients with leukemias but not in patients with breast cancer or non-Hodgkin’s lymphoma, he said.
Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.
On Twitter @sherryboschert
SAN FRANCISCO – Controlled ovarian hyperstimulation and oocyte vitrification were similarly successful in preserving fertility in women with or without cancer, based on a retrospective study of 5 years of experience at one European center.
Among 475 oncologic patients and 560 patients with no cancer, 1,080 oocyte vitrification cycles were performed, 33% of them in women with cancer and 67% for nonmedical reasons. So far, 30 women have returned to use their frozen eggs (4 cancer patients and 26 noncancer patients), resulting in 20 pregnancies and 6 live births (in 1 cancer patient and 5 noncancer patients), with 8 pregnancies ongoing, Dr. Antonio Pellicer said at the UCLA annual in vitro fertilization and embryo transfer update 2013.
Some differences between the patient groups were seen. The total dose of gonadotropins used and serum estradiol levels were lower in patients who’d had cancer, said Dr. Pellicer, professor of obstetrics and gynecology and director of the Instituto Valenciano de Infertilidad at the University of Valencia (Spain) (Fertil. Steril. 2013;99:1994-9).
The quality of the oocytes seemed similar between groups, but fewer eggs can be retrieved after controlled ovarian stimulation in patients with cancer because some cancers affect the ovaries. Previous work by Dr. Pellicer and his associates showed that a mean of two fewer oocytes are retrieved from patients with hormone-dependent breast cancer, compared with noncancer controls.
Oocyte vitrification is a safe, promising method for fertility preservation not only in patients with cancer but in noncancer patients as well, he said. Approximately 91% of the nonmedical reasons for oocyte vitrification at his center were "social" reasons, Dr. Pellicer said. "This is a procedure that is increasing more and more."
A majority of women treated for breast cancer at his institution lose some ovarian function. Fertility preservation in female cancer patients can take three forms: medical protection of the gonads, ovarian cortex freezing and transplantation, and/or oocyte and embryo vitrification.
Five years of experience with reimplantation of frozen and then thawed ovarian tissue at three European centers showed that 11 of 60 patients who underwent orthotropic reimplantations of cryopreserved ovarian tissue became pregnant, and 6 patients so far have been delivered of 12 healthy infants (Fertil. Steril. 2013;99:1503-13).
The centers in the study included Dr. Pellicer’s institution and centers in Belgium and Denmark. "All of us have done between 800 and 1,000" cases of harvesting and freezing ovarian tissue. Cryopreservation of ovarian tissue may be the only option available to preserve fertility in prepubertal girls facing cancer treatment and for women who cannot delay the start of chemotherapy.
"The technique is promising and improving. I think there is room for it to continue in this direction for women who need fertility preservation," Dr. Pellicer said.
The concern with ovarian tissue cryopreservation has been that it may transplant neoplastic cells. Previous studies by other investigators, however, suggest that this risk is true in patients with leukemias but not in patients with breast cancer or non-Hodgkin’s lymphoma, he said.
Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.
On Twitter @sherryboschert
AT A MEETING ON IVF AND EMBRYO TRANSFER
Major finding: Among 26 noncancer patients and 4 cancer patients who reclaimed their frozen oocytes, 5 noncancer patients and 1 cancer patient gave birth to live newborns; 8 pregnancies are ongoing.
Data source: A review of 5 years of experience with controlled ovarian hyperstimulation and oocyte vitrification at one European center.
Disclosures: Dr. Pellicer is a shareholder in Unisense. In his report on oocyte vitrification for patients with cancer, Merck Serono–Spain provided the medication for oncologic patients.