User login
Discuss this article at www.facebook.com/CurrentPsychiatry
• Venlafaxine has been shown to decrease indinavir concentrations in cellular models and healthy individuals in a controlled trial.
• It is not known if this effect would occur with other protease inhibitors; however, most protease inhibitors are P-glycoprotein substrates.
• In preliminary cellular models, desvenlafaxine did not have the same effect.
• It is not known if other psychotropics have the same effect on P-glycoprotein or other efflux proteins.
Mr. B, age 32, was diagnosed with human immunodeficiency virus (HIV) approximately 10 years ago. His current HIV regimen is highly active antiretroviral therapy, which includes the protease inhibitor (PI) indinavir and the combination product lamivudine and zidovudine, 2 nucleoside reverse transcriptase inhibitors. He shows no symptoms and his viral load has been undetectable for 9 years.
Several months ago, Mr. B reported to his primary care physician feelings of depressed mood, anhedonia, significant weight loss, fatigue, and feelings of worthlessness. He was diagnosed with major depressive disorder and started venlafaxine, 150 mg/d. The depressive episode is now in remission and the only major side effect he experiences is lethargy. His physician decides to check Mr. B’s viral load, which is 1,100 copies/mL. This viral load value indicates a significant elevation from the baseline (<48 copies/mL), which although still low, is considered virologic failure.1 To rule out a lab error the viral load test is replicated, but the result is the same.
Mr. B’s case may represent an interaction between his antidepressant and one of his antiviral drugs that is a P-glycoprotein substrate. This protein transports a variety of drug substrates across cell membranes and affects the distribution and elimination of many prescription and nonprescription medications. Whether a drug induces or inhibits P-glycoprotein can affect plasma and cellular concentrations of drugs and can lead to unexpected increases or decreases in plasma concentrations of the affected drug. Understanding P-glycoprotein’s role can help you choose effective psychotropics for patients such as Mr. B.
Change in drug effect
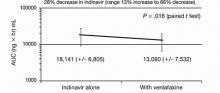
Because depression is common among patients with HIV, my colleagues and I evaluated the pharmacokinetic effects of indinavir on venlafaxine and venlafaxine on indinavir to determine if venlafaxine would be safe to use in a patient taking a PI because of potential cytochrome P450 (CYP450) drug interactions in both classes of medications.2 Adding venlafaxine resulted in a 36% decrease in maximum concentrations for indinavir and a 28% decrease in area under the curve Figure.2 Study participants were healthy individuals; however, we concluded that had we studied patients with HIV, indinavir efficacy could decrease, resulting in an increased viral load. After this study, the manufacturer of venlafaxine included a caution about this combination in the product labeling.3 Because the extended-release formulation includes the same compound, the same effect could be expected and was included in the most recent version of the extended-release venlafaxine prescribing information.4
What is interesting about the venlafaxine-indinavir interaction is that there was no change in either agent’s half-life and therefore no reason to assume this effect was a traditional CYP450 drug interaction. The investigators considered other types of drug interactions and focused on mechanisms that could be presystemic, ie, affecting the absorption and bioavailability of indinavir. This led investigators to believe that the mechanism involved a drug transport protein such as P-glycoprotein, which is present in gut lumen. Subsequent studies have shown in a cellular model that venlafaxine—but not desvenlafaxine—is an inducer of P-glycoprotein and breast cancer resistant protein (BCRP).5,6 Researchers are conducting animal studies to attempt to duplicate the cellular models. However, it could be presumed that the study of venlafaxine and indinavir in healthy individuals already had demonstrated this effect.2
Figure: Indinavir area under the curve before and after steady state venlafaxine
Decrease in area under the curve (AUC) for indinavir when healthy individuals achieved steady state dosing of venlafaxine
Source: Reference 2
Cause and effect
P-glycoprotein transports drugs or other foreign compounds out of the cells (efflux) of the target tissue so they can be further metabolized by metabolic enzymes for elimination. These proteins are called efflux proteins. There are many efflux proteins in addition to P-glycoprotein; a common one is BCRP, which confers resistance to some anticancer drugs. In addition to the gut lumen and breast tissue, efflux proteins are present in most tissues throughout the body, including the blood-brain barrier.
If drug A inhibits an efflux protein, then drug B would be able to enter the target tissue with greater ease and not be “kicked out” because the efflux system would be disabled. This could result in higher-than-expected tissue concentrations of drug B. Pharmaceutical companies often perform P-glycoprotein inhibition studies before a drug is marketed and include this data in the prescribing information.
If, on the other hand, drug A induces an efflux protein, then drug B would be “kicked out” at a greater rate than normal because the efflux system would be working in overdrive. In this case, tissue concentrations of drug B would be lower than expected and could lead to therapeutic failure. Typically, pharmaceutical companies either do not conduct these induction studies, or if they are performed, they often are not described in prescribing information. This lack of efficacy has been well documented with chemotherapeutic failure caused by drug efflux by BCRP.7 It is likely that Mr. B’s viral load increased when venlafaxine was added to his regimen—the antidepressant induced P-glycoprotein, which reduced indinavir concentrations and subsequent therapeutic effect.
Clinicians should review specific medications they are considering using if the drugs have a narrow therapeutic index or if therapeutic failure from subtherapeutic or supratherapeutic doses would be considered problematic Table.8 Kim9 provides a comprehensive list of P-glycoprotein substrates, inhibitors, and inducers. However, keep in mind that the list of substrates, inhibitors, and inducers changes regularly as new research becomes available.
Table
Selected psychotropics that affect P-glycoprotein
| Substrates | |
| Amitriptyline | Paroxetine |
| Carbamazepine | Quetiapine |
| Chlorpromazine | Risperidone |
| Citalopram | Sertraline |
| Doxepin | Topiramate |
| Nortriptyline | Venlafaxine |
| Olanzapine | |
| Inhibitors | |
| Amitriptyline | Imipramine |
| Carbamazepine | Nefazodone |
| Chlorpromazine | Paroxetine |
| Desipramine | Sertraline |
| Disulfiram | Thioridazine |
| Fluoxetine | Trifluoperazine |
| Fluvoxamine | Trimipramine |
| Haloperidol | |
| Inducersa | |
| Amitriptyline | Phenothiazines |
| Nefazodone | Trazodone |
| aData supporting induction is limited Source: Reference 8 | |
- Linnet K, Ejsing TB. A review on the impact of P-glycoprotein on the penetration of drugs into the brain. Focus on psychotropic drugs. Eur Neuropsychopharmacol. 2008;18(3):157-169.
- Weiss J, Dormann SM, Martin-Facklam M, et al. Inhibition of P-glycoprotein by newer antidepressants. J Pharmacol Exp Ther. 2003;305(1):197-204.
Drug Brand Names
- Amitriptyline • Elavil
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Citalopram • Celexa
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Disulfiram • Antabuse
- Doxepin • Adapin, Silenor
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Imipramine • Tofranil
- Indinavir • Crixivan
- Lamivudine and zidovudine • Combivir
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Thioridazine • Melleril
- Topiramate • Topamax
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimipramine • Surmontil
- Venlafaxine • Effexor
Disclosure
Dr. Levin receives grant/research support from Pfizer.
1. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Washington DC: Department of Health and Human Services; January 10, 2011;1-166.
2. Levin GM, Nelson LA, DeVane CL, et al. A pharmacokinetic drug-drug interaction study of venlafaxine and indinavir. Psychopharmacol Bull. 2001;35(2):62-71.
3. Effexor [package insert]. Philadelphia PA: Wyeth Pharmaceuticals Inc.; 2010.
4. Effexor XR [package insert]. Philadelphia PA: Wyeth Pharmaceuticals Inc.; 2011.
5. Ehret MJ, Levin GM, Narasimhan M, et al. Venlafaxine induces P-glycoprotein in human Caco-2 cells. Hum Psychopharmacol. 2007;22(1):49-53.
6. Bachmeier CJ, Beaulieu-Abdelahad D, Ganey NJ, et al. Induction of drug efflux protein expression by venlafaxine but not desvenlafaxine. Biopharm Drug Dispos. 2011;32(4):233-244.
7. Rosenberg MF, Bikadi Z, Chan J, et al. The human breast cancer resistance protein (BCRP/ABCG2) shows conformational changes with mitoxantrone. Structure. 2010;18(4):482-493.
8. Oesterheld J. P-glycoprotein (PGP) table - the effect of drugs and foods. http://www.genemedrx.com/PGPtable.php. Accessed February 3 2012.
9. Kim RB. Drugs as P-glycoprotein substrates inhibitors, and inducers. Drug Metab Rev. 2002;34(1-2):47-54.
Discuss this article at www.facebook.com/CurrentPsychiatry
• Venlafaxine has been shown to decrease indinavir concentrations in cellular models and healthy individuals in a controlled trial.
• It is not known if this effect would occur with other protease inhibitors; however, most protease inhibitors are P-glycoprotein substrates.
• In preliminary cellular models, desvenlafaxine did not have the same effect.
• It is not known if other psychotropics have the same effect on P-glycoprotein or other efflux proteins.
Mr. B, age 32, was diagnosed with human immunodeficiency virus (HIV) approximately 10 years ago. His current HIV regimen is highly active antiretroviral therapy, which includes the protease inhibitor (PI) indinavir and the combination product lamivudine and zidovudine, 2 nucleoside reverse transcriptase inhibitors. He shows no symptoms and his viral load has been undetectable for 9 years.
Several months ago, Mr. B reported to his primary care physician feelings of depressed mood, anhedonia, significant weight loss, fatigue, and feelings of worthlessness. He was diagnosed with major depressive disorder and started venlafaxine, 150 mg/d. The depressive episode is now in remission and the only major side effect he experiences is lethargy. His physician decides to check Mr. B’s viral load, which is 1,100 copies/mL. This viral load value indicates a significant elevation from the baseline (<48 copies/mL), which although still low, is considered virologic failure.1 To rule out a lab error the viral load test is replicated, but the result is the same.
Mr. B’s case may represent an interaction between his antidepressant and one of his antiviral drugs that is a P-glycoprotein substrate. This protein transports a variety of drug substrates across cell membranes and affects the distribution and elimination of many prescription and nonprescription medications. Whether a drug induces or inhibits P-glycoprotein can affect plasma and cellular concentrations of drugs and can lead to unexpected increases or decreases in plasma concentrations of the affected drug. Understanding P-glycoprotein’s role can help you choose effective psychotropics for patients such as Mr. B.
Change in drug effect
Because depression is common among patients with HIV, my colleagues and I evaluated the pharmacokinetic effects of indinavir on venlafaxine and venlafaxine on indinavir to determine if venlafaxine would be safe to use in a patient taking a PI because of potential cytochrome P450 (CYP450) drug interactions in both classes of medications.2 Adding venlafaxine resulted in a 36% decrease in maximum concentrations for indinavir and a 28% decrease in area under the curve Figure.2 Study participants were healthy individuals; however, we concluded that had we studied patients with HIV, indinavir efficacy could decrease, resulting in an increased viral load. After this study, the manufacturer of venlafaxine included a caution about this combination in the product labeling.3 Because the extended-release formulation includes the same compound, the same effect could be expected and was included in the most recent version of the extended-release venlafaxine prescribing information.4
What is interesting about the venlafaxine-indinavir interaction is that there was no change in either agent’s half-life and therefore no reason to assume this effect was a traditional CYP450 drug interaction. The investigators considered other types of drug interactions and focused on mechanisms that could be presystemic, ie, affecting the absorption and bioavailability of indinavir. This led investigators to believe that the mechanism involved a drug transport protein such as P-glycoprotein, which is present in gut lumen. Subsequent studies have shown in a cellular model that venlafaxine—but not desvenlafaxine—is an inducer of P-glycoprotein and breast cancer resistant protein (BCRP).5,6 Researchers are conducting animal studies to attempt to duplicate the cellular models. However, it could be presumed that the study of venlafaxine and indinavir in healthy individuals already had demonstrated this effect.2
Figure: Indinavir area under the curve before and after steady state venlafaxine
Decrease in area under the curve (AUC) for indinavir when healthy individuals achieved steady state dosing of venlafaxine
Source: Reference 2
Cause and effect
P-glycoprotein transports drugs or other foreign compounds out of the cells (efflux) of the target tissue so they can be further metabolized by metabolic enzymes for elimination. These proteins are called efflux proteins. There are many efflux proteins in addition to P-glycoprotein; a common one is BCRP, which confers resistance to some anticancer drugs. In addition to the gut lumen and breast tissue, efflux proteins are present in most tissues throughout the body, including the blood-brain barrier.
If drug A inhibits an efflux protein, then drug B would be able to enter the target tissue with greater ease and not be “kicked out” because the efflux system would be disabled. This could result in higher-than-expected tissue concentrations of drug B. Pharmaceutical companies often perform P-glycoprotein inhibition studies before a drug is marketed and include this data in the prescribing information.
If, on the other hand, drug A induces an efflux protein, then drug B would be “kicked out” at a greater rate than normal because the efflux system would be working in overdrive. In this case, tissue concentrations of drug B would be lower than expected and could lead to therapeutic failure. Typically, pharmaceutical companies either do not conduct these induction studies, or if they are performed, they often are not described in prescribing information. This lack of efficacy has been well documented with chemotherapeutic failure caused by drug efflux by BCRP.7 It is likely that Mr. B’s viral load increased when venlafaxine was added to his regimen—the antidepressant induced P-glycoprotein, which reduced indinavir concentrations and subsequent therapeutic effect.
Clinicians should review specific medications they are considering using if the drugs have a narrow therapeutic index or if therapeutic failure from subtherapeutic or supratherapeutic doses would be considered problematic Table.8 Kim9 provides a comprehensive list of P-glycoprotein substrates, inhibitors, and inducers. However, keep in mind that the list of substrates, inhibitors, and inducers changes regularly as new research becomes available.
Table
Selected psychotropics that affect P-glycoprotein
| Substrates | |
| Amitriptyline | Paroxetine |
| Carbamazepine | Quetiapine |
| Chlorpromazine | Risperidone |
| Citalopram | Sertraline |
| Doxepin | Topiramate |
| Nortriptyline | Venlafaxine |
| Olanzapine | |
| Inhibitors | |
| Amitriptyline | Imipramine |
| Carbamazepine | Nefazodone |
| Chlorpromazine | Paroxetine |
| Desipramine | Sertraline |
| Disulfiram | Thioridazine |
| Fluoxetine | Trifluoperazine |
| Fluvoxamine | Trimipramine |
| Haloperidol | |
| Inducersa | |
| Amitriptyline | Phenothiazines |
| Nefazodone | Trazodone |
| aData supporting induction is limited Source: Reference 8 | |
- Linnet K, Ejsing TB. A review on the impact of P-glycoprotein on the penetration of drugs into the brain. Focus on psychotropic drugs. Eur Neuropsychopharmacol. 2008;18(3):157-169.
- Weiss J, Dormann SM, Martin-Facklam M, et al. Inhibition of P-glycoprotein by newer antidepressants. J Pharmacol Exp Ther. 2003;305(1):197-204.
Drug Brand Names
- Amitriptyline • Elavil
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Citalopram • Celexa
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Disulfiram • Antabuse
- Doxepin • Adapin, Silenor
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Imipramine • Tofranil
- Indinavir • Crixivan
- Lamivudine and zidovudine • Combivir
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Thioridazine • Melleril
- Topiramate • Topamax
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimipramine • Surmontil
- Venlafaxine • Effexor
Disclosure
Dr. Levin receives grant/research support from Pfizer.
Discuss this article at www.facebook.com/CurrentPsychiatry
• Venlafaxine has been shown to decrease indinavir concentrations in cellular models and healthy individuals in a controlled trial.
• It is not known if this effect would occur with other protease inhibitors; however, most protease inhibitors are P-glycoprotein substrates.
• In preliminary cellular models, desvenlafaxine did not have the same effect.
• It is not known if other psychotropics have the same effect on P-glycoprotein or other efflux proteins.
Mr. B, age 32, was diagnosed with human immunodeficiency virus (HIV) approximately 10 years ago. His current HIV regimen is highly active antiretroviral therapy, which includes the protease inhibitor (PI) indinavir and the combination product lamivudine and zidovudine, 2 nucleoside reverse transcriptase inhibitors. He shows no symptoms and his viral load has been undetectable for 9 years.
Several months ago, Mr. B reported to his primary care physician feelings of depressed mood, anhedonia, significant weight loss, fatigue, and feelings of worthlessness. He was diagnosed with major depressive disorder and started venlafaxine, 150 mg/d. The depressive episode is now in remission and the only major side effect he experiences is lethargy. His physician decides to check Mr. B’s viral load, which is 1,100 copies/mL. This viral load value indicates a significant elevation from the baseline (<48 copies/mL), which although still low, is considered virologic failure.1 To rule out a lab error the viral load test is replicated, but the result is the same.
Mr. B’s case may represent an interaction between his antidepressant and one of his antiviral drugs that is a P-glycoprotein substrate. This protein transports a variety of drug substrates across cell membranes and affects the distribution and elimination of many prescription and nonprescription medications. Whether a drug induces or inhibits P-glycoprotein can affect plasma and cellular concentrations of drugs and can lead to unexpected increases or decreases in plasma concentrations of the affected drug. Understanding P-glycoprotein’s role can help you choose effective psychotropics for patients such as Mr. B.
Change in drug effect
Because depression is common among patients with HIV, my colleagues and I evaluated the pharmacokinetic effects of indinavir on venlafaxine and venlafaxine on indinavir to determine if venlafaxine would be safe to use in a patient taking a PI because of potential cytochrome P450 (CYP450) drug interactions in both classes of medications.2 Adding venlafaxine resulted in a 36% decrease in maximum concentrations for indinavir and a 28% decrease in area under the curve Figure.2 Study participants were healthy individuals; however, we concluded that had we studied patients with HIV, indinavir efficacy could decrease, resulting in an increased viral load. After this study, the manufacturer of venlafaxine included a caution about this combination in the product labeling.3 Because the extended-release formulation includes the same compound, the same effect could be expected and was included in the most recent version of the extended-release venlafaxine prescribing information.4
What is interesting about the venlafaxine-indinavir interaction is that there was no change in either agent’s half-life and therefore no reason to assume this effect was a traditional CYP450 drug interaction. The investigators considered other types of drug interactions and focused on mechanisms that could be presystemic, ie, affecting the absorption and bioavailability of indinavir. This led investigators to believe that the mechanism involved a drug transport protein such as P-glycoprotein, which is present in gut lumen. Subsequent studies have shown in a cellular model that venlafaxine—but not desvenlafaxine—is an inducer of P-glycoprotein and breast cancer resistant protein (BCRP).5,6 Researchers are conducting animal studies to attempt to duplicate the cellular models. However, it could be presumed that the study of venlafaxine and indinavir in healthy individuals already had demonstrated this effect.2
Figure: Indinavir area under the curve before and after steady state venlafaxine
Decrease in area under the curve (AUC) for indinavir when healthy individuals achieved steady state dosing of venlafaxine
Source: Reference 2
Cause and effect
P-glycoprotein transports drugs or other foreign compounds out of the cells (efflux) of the target tissue so they can be further metabolized by metabolic enzymes for elimination. These proteins are called efflux proteins. There are many efflux proteins in addition to P-glycoprotein; a common one is BCRP, which confers resistance to some anticancer drugs. In addition to the gut lumen and breast tissue, efflux proteins are present in most tissues throughout the body, including the blood-brain barrier.
If drug A inhibits an efflux protein, then drug B would be able to enter the target tissue with greater ease and not be “kicked out” because the efflux system would be disabled. This could result in higher-than-expected tissue concentrations of drug B. Pharmaceutical companies often perform P-glycoprotein inhibition studies before a drug is marketed and include this data in the prescribing information.
If, on the other hand, drug A induces an efflux protein, then drug B would be “kicked out” at a greater rate than normal because the efflux system would be working in overdrive. In this case, tissue concentrations of drug B would be lower than expected and could lead to therapeutic failure. Typically, pharmaceutical companies either do not conduct these induction studies, or if they are performed, they often are not described in prescribing information. This lack of efficacy has been well documented with chemotherapeutic failure caused by drug efflux by BCRP.7 It is likely that Mr. B’s viral load increased when venlafaxine was added to his regimen—the antidepressant induced P-glycoprotein, which reduced indinavir concentrations and subsequent therapeutic effect.
Clinicians should review specific medications they are considering using if the drugs have a narrow therapeutic index or if therapeutic failure from subtherapeutic or supratherapeutic doses would be considered problematic Table.8 Kim9 provides a comprehensive list of P-glycoprotein substrates, inhibitors, and inducers. However, keep in mind that the list of substrates, inhibitors, and inducers changes regularly as new research becomes available.
Table
Selected psychotropics that affect P-glycoprotein
| Substrates | |
| Amitriptyline | Paroxetine |
| Carbamazepine | Quetiapine |
| Chlorpromazine | Risperidone |
| Citalopram | Sertraline |
| Doxepin | Topiramate |
| Nortriptyline | Venlafaxine |
| Olanzapine | |
| Inhibitors | |
| Amitriptyline | Imipramine |
| Carbamazepine | Nefazodone |
| Chlorpromazine | Paroxetine |
| Desipramine | Sertraline |
| Disulfiram | Thioridazine |
| Fluoxetine | Trifluoperazine |
| Fluvoxamine | Trimipramine |
| Haloperidol | |
| Inducersa | |
| Amitriptyline | Phenothiazines |
| Nefazodone | Trazodone |
| aData supporting induction is limited Source: Reference 8 | |
- Linnet K, Ejsing TB. A review on the impact of P-glycoprotein on the penetration of drugs into the brain. Focus on psychotropic drugs. Eur Neuropsychopharmacol. 2008;18(3):157-169.
- Weiss J, Dormann SM, Martin-Facklam M, et al. Inhibition of P-glycoprotein by newer antidepressants. J Pharmacol Exp Ther. 2003;305(1):197-204.
Drug Brand Names
- Amitriptyline • Elavil
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Citalopram • Celexa
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Disulfiram • Antabuse
- Doxepin • Adapin, Silenor
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Imipramine • Tofranil
- Indinavir • Crixivan
- Lamivudine and zidovudine • Combivir
- Nefazodone • Serzone
- Nortriptyline • Aventyl, Pamelor
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Thioridazine • Melleril
- Topiramate • Topamax
- Trazodone • Desyrel, Oleptro
- Trifluoperazine • Stelazine
- Trimipramine • Surmontil
- Venlafaxine • Effexor
Disclosure
Dr. Levin receives grant/research support from Pfizer.
1. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Washington DC: Department of Health and Human Services; January 10, 2011;1-166.
2. Levin GM, Nelson LA, DeVane CL, et al. A pharmacokinetic drug-drug interaction study of venlafaxine and indinavir. Psychopharmacol Bull. 2001;35(2):62-71.
3. Effexor [package insert]. Philadelphia PA: Wyeth Pharmaceuticals Inc.; 2010.
4. Effexor XR [package insert]. Philadelphia PA: Wyeth Pharmaceuticals Inc.; 2011.
5. Ehret MJ, Levin GM, Narasimhan M, et al. Venlafaxine induces P-glycoprotein in human Caco-2 cells. Hum Psychopharmacol. 2007;22(1):49-53.
6. Bachmeier CJ, Beaulieu-Abdelahad D, Ganey NJ, et al. Induction of drug efflux protein expression by venlafaxine but not desvenlafaxine. Biopharm Drug Dispos. 2011;32(4):233-244.
7. Rosenberg MF, Bikadi Z, Chan J, et al. The human breast cancer resistance protein (BCRP/ABCG2) shows conformational changes with mitoxantrone. Structure. 2010;18(4):482-493.
8. Oesterheld J. P-glycoprotein (PGP) table - the effect of drugs and foods. http://www.genemedrx.com/PGPtable.php. Accessed February 3 2012.
9. Kim RB. Drugs as P-glycoprotein substrates inhibitors, and inducers. Drug Metab Rev. 2002;34(1-2):47-54.
1. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Washington DC: Department of Health and Human Services; January 10, 2011;1-166.
2. Levin GM, Nelson LA, DeVane CL, et al. A pharmacokinetic drug-drug interaction study of venlafaxine and indinavir. Psychopharmacol Bull. 2001;35(2):62-71.
3. Effexor [package insert]. Philadelphia PA: Wyeth Pharmaceuticals Inc.; 2010.
4. Effexor XR [package insert]. Philadelphia PA: Wyeth Pharmaceuticals Inc.; 2011.
5. Ehret MJ, Levin GM, Narasimhan M, et al. Venlafaxine induces P-glycoprotein in human Caco-2 cells. Hum Psychopharmacol. 2007;22(1):49-53.
6. Bachmeier CJ, Beaulieu-Abdelahad D, Ganey NJ, et al. Induction of drug efflux protein expression by venlafaxine but not desvenlafaxine. Biopharm Drug Dispos. 2011;32(4):233-244.
7. Rosenberg MF, Bikadi Z, Chan J, et al. The human breast cancer resistance protein (BCRP/ABCG2) shows conformational changes with mitoxantrone. Structure. 2010;18(4):482-493.
8. Oesterheld J. P-glycoprotein (PGP) table - the effect of drugs and foods. http://www.genemedrx.com/PGPtable.php. Accessed February 3 2012.
9. Kim RB. Drugs as P-glycoprotein substrates inhibitors, and inducers. Drug Metab Rev. 2002;34(1-2):47-54.