User login
Palliative and end-of-life care
Nurse-driven palliative care screening
Palliative care (PC) aims to improve quality of life for patients with a life-threatening illness, providing holistic patient-centered support along the continuum of the disease process. Although frequently implemented in critical care settings, integrating PC in the neuro ICU has been difficult to adopt in practice due to the uncertainty in prognostication of definitive outcomes and practice culture beliefs such as the self-fulfilling prophecy (Frontera, et al. Crit Care Med. 2015;43[9]:1964; Rubin, et al. Curr Opin Crit Care. 2017;23[2]:134; Knies, et al. Semin Neurol. 2016;36[6]:631).
At our institution, a nursing education project was conducted to pilot nurse-driven PC screenings on admission to the neuro ICU. The project evaluated nurse comfort and knowledge with identifying and recommending PC consults. Pre- and post-intervention surveys revealed that education and introduction of a PC screening tool significantly increased nurse comfort and knowledge of PC eligibility.
PC in the neuro ICU can exist to contribute to successful outcomes in patient and family care. Within neurocritical care, incorporating PC is essential to provide extra support to patients and families (Frontera, et al. 2015).
For these reasons and data from the project, nurse-driven screening may encourage appropriate early PC consults. Patient-centered care is the ultimate goal in the management of our patients. Nurse-driven PC screening can help bring various unmet PC needs to the health-care team for opportunities that might not have been met or otherwise assessed. Consider implementing nurse-driven PC screening protocols at your institution to aid in collaborative and proactive interdisciplinary care.
Danielle McCamey, ACNP
Steering Committee Member
Sleep medicine
Diagnostics, devices, and sleep
The past several months have been busy for the Sleep Medicine NetWork. We have been working to represent the interests of our membership and our patients in many arenas.
Devices coded as E0464, defined as life support mechanical ventilators used with mask-based ventilation in the home are being more frequently used. According to the Office of the Inspector General (OIG), there has been an 89-fold increase in billing for E0464 ventilators for Medicare and its beneficiaries between 2009 and 2015, increasing from $3.8M to $340M. In response, the Agency for Healthcare Research and Quality (AHRQ) requested a response to specific questions related to these devices.
In 2018, the CHEST Sleep Medicine NetWork will be participating in a Federal Drug Association-sponsored workshop entitled “Study Design Considerations for Devices including Digital Health Technologies for Sleep-Disordered Breathing (SDB) in Adults,” along with other national organizations and leaders in our field. This workshop will address available technologies for the diagnosis, monitoring, and treatment of SDB, as well as trends for digital health technologies and clinical trial design considerations.
Finally, the Sleep Medicine NetWork has wasted no time after a successful CHEST 2017 in Toronto in planning for the next annual meeting in San Antonio. We are excited to present an exciting curriculum in Sleep Medicine at CHEST 2018, so stay tuned.
Aneesa M. Das, MD, FCCP
NetWork Chair
Occupational and environmental health
Post-deployment lung disease
Since the early 1990s, ongoing military deployments to Southwest Asia remain a unique challenge from a pulmonary symptomology and diagnostic perspective.
Various airborne hazards in the deployment environment include geologic dusts, burn pit smoke, vehicle emissions, and industrial air pollution. Exposures can give rise to both acute respiratory symptoms and, in some instances, chronic lung disease. Currently, data are limited on whether inhalation of airborne particulate matter by military personnel is linked to increases in pulmonary diseases (Morris MJ, et al. US Army Med Dep J. 2016:173).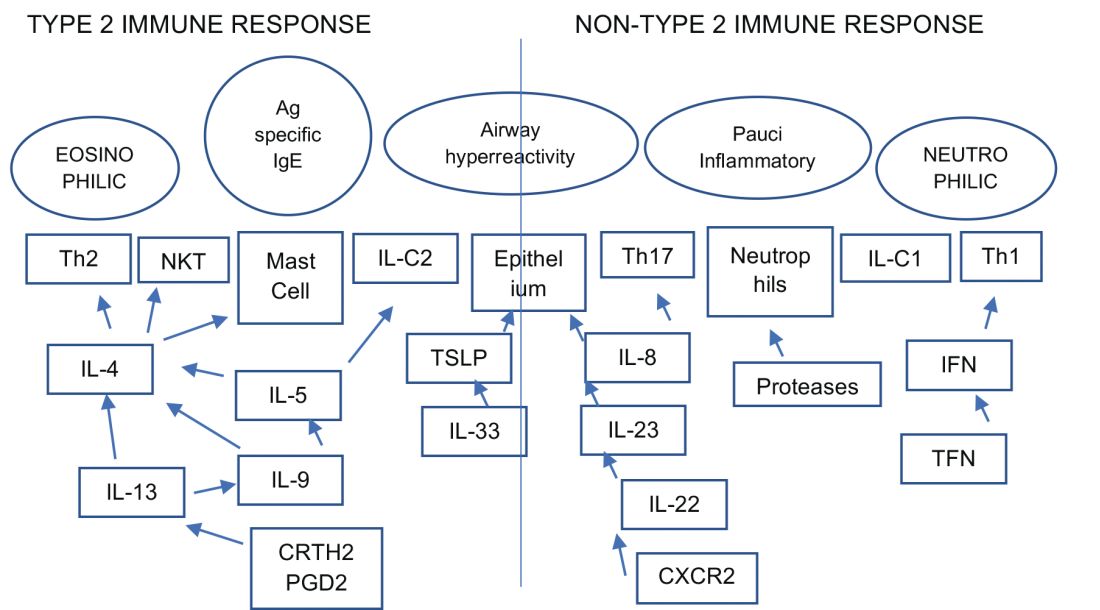
Ongoing research by the Veterans Affairs continues to enroll post-deployed personnel in an Airborne Hazard and Burn Pit Registry. Past approaches in evaluation of deployed individuals ranged from common tests such as spirometry, HRCT scanning, full PFTs, bronchoprovocation challenges, and, in some instances, lung biopsies (Krefft SD, et al. Fed Pract. 2015;32[6]:32). More novel evaluations of postdeployment dyspnea include impulse oscillometry, exhaled nitric oxide, bronchoscopy, and cardiopulmonary exercise testing (Huprikar, et al. Chest. 2016;150[4]:S934A).
Members of the CHEST Occupational and Environmental Health NetWork are currently updating comprehensive approaches to evaluate military personnel with chronic respiratory symptoms from deployments. Continued emphasis, however, should be placed on diagnosing and treating common diseases such as asthma, exercise-induced bronchospasm, GERD, and upper airway disorders.
Pedro F. Lucero, MD, FCCP
Steering Committee Member
Clinical pulmonary medicine
Biologics – Birth of a new era of precision management in asthma
An estimated 10% to 20% of patients with severe uncontrolled asthma do not respond to maximal best standard treatments, leading to substantial health-care costs. A paradigm shift is now underway in our approach to the care of these patients with the emergence of novel biologics targeting the complex and interconnected inflammatory pathways in asthma that result in a diverse profile of asthma endotypes and phenotypes (Fig 1).
Current FDA-approved biologics primarily target patients with a T2 high phenotype (Table1).
Dupilumab binds to the alpha unit of the IL-4 receptor and blocks both IL-4 and IL-13. It shows potential efficacy in patients with T2 high asthma with or without eosinophilia but has not yet received FDA approval.
Multiple newer biologics are currently in development (Table 2).
Pulmonologists need to get familiar with the logistics of administration of these novel agents. The two common methods of administering biologics are (1) buy and bill – where the provider buys the drug directly from the distributor; and (2) assignment of benefits (typically administered by a Pharmacy Benefit Manager) - specific dose of the medication is shipped to the physician’s office and physician only bills for the administration. CPT and J codes are shown in Table 1.
Shyamsunder Subramanian, MD, FCCP
Steering Committee Member
Palliative and end-of-life care
Nurse-driven palliative care screening
Palliative care (PC) aims to improve quality of life for patients with a life-threatening illness, providing holistic patient-centered support along the continuum of the disease process. Although frequently implemented in critical care settings, integrating PC in the neuro ICU has been difficult to adopt in practice due to the uncertainty in prognostication of definitive outcomes and practice culture beliefs such as the self-fulfilling prophecy (Frontera, et al. Crit Care Med. 2015;43[9]:1964; Rubin, et al. Curr Opin Crit Care. 2017;23[2]:134; Knies, et al. Semin Neurol. 2016;36[6]:631).
At our institution, a nursing education project was conducted to pilot nurse-driven PC screenings on admission to the neuro ICU. The project evaluated nurse comfort and knowledge with identifying and recommending PC consults. Pre- and post-intervention surveys revealed that education and introduction of a PC screening tool significantly increased nurse comfort and knowledge of PC eligibility.
PC in the neuro ICU can exist to contribute to successful outcomes in patient and family care. Within neurocritical care, incorporating PC is essential to provide extra support to patients and families (Frontera, et al. 2015).
For these reasons and data from the project, nurse-driven screening may encourage appropriate early PC consults. Patient-centered care is the ultimate goal in the management of our patients. Nurse-driven PC screening can help bring various unmet PC needs to the health-care team for opportunities that might not have been met or otherwise assessed. Consider implementing nurse-driven PC screening protocols at your institution to aid in collaborative and proactive interdisciplinary care.
Danielle McCamey, ACNP
Steering Committee Member
Sleep medicine
Diagnostics, devices, and sleep
The past several months have been busy for the Sleep Medicine NetWork. We have been working to represent the interests of our membership and our patients in many arenas.
Devices coded as E0464, defined as life support mechanical ventilators used with mask-based ventilation in the home are being more frequently used. According to the Office of the Inspector General (OIG), there has been an 89-fold increase in billing for E0464 ventilators for Medicare and its beneficiaries between 2009 and 2015, increasing from $3.8M to $340M. In response, the Agency for Healthcare Research and Quality (AHRQ) requested a response to specific questions related to these devices.
In 2018, the CHEST Sleep Medicine NetWork will be participating in a Federal Drug Association-sponsored workshop entitled “Study Design Considerations for Devices including Digital Health Technologies for Sleep-Disordered Breathing (SDB) in Adults,” along with other national organizations and leaders in our field. This workshop will address available technologies for the diagnosis, monitoring, and treatment of SDB, as well as trends for digital health technologies and clinical trial design considerations.
Finally, the Sleep Medicine NetWork has wasted no time after a successful CHEST 2017 in Toronto in planning for the next annual meeting in San Antonio. We are excited to present an exciting curriculum in Sleep Medicine at CHEST 2018, so stay tuned.
Aneesa M. Das, MD, FCCP
NetWork Chair
Occupational and environmental health
Post-deployment lung disease
Since the early 1990s, ongoing military deployments to Southwest Asia remain a unique challenge from a pulmonary symptomology and diagnostic perspective.
Various airborne hazards in the deployment environment include geologic dusts, burn pit smoke, vehicle emissions, and industrial air pollution. Exposures can give rise to both acute respiratory symptoms and, in some instances, chronic lung disease. Currently, data are limited on whether inhalation of airborne particulate matter by military personnel is linked to increases in pulmonary diseases (Morris MJ, et al. US Army Med Dep J. 2016:173).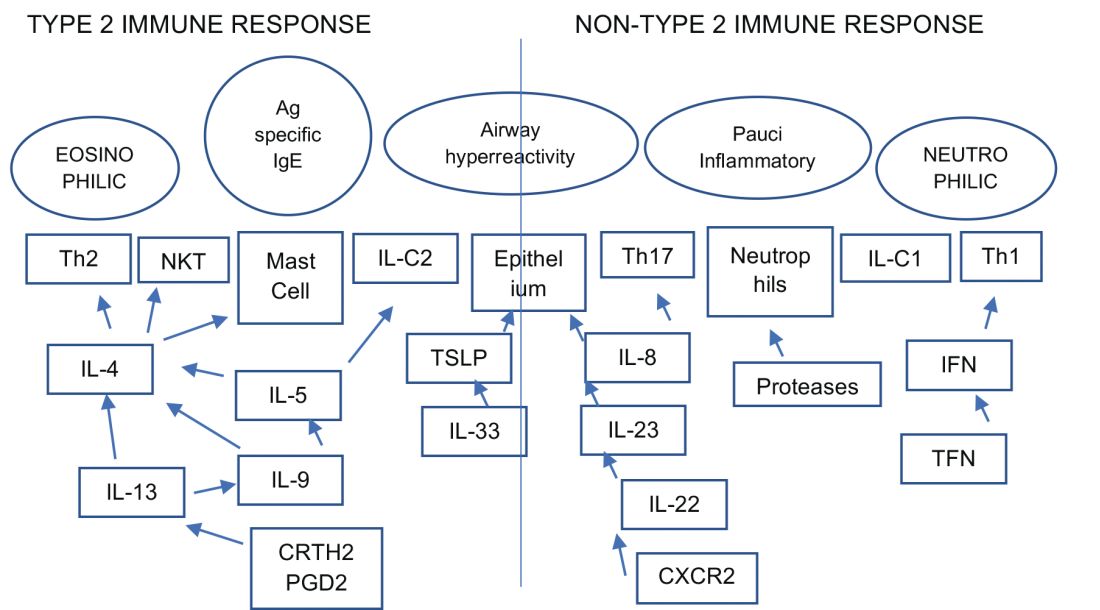
Ongoing research by the Veterans Affairs continues to enroll post-deployed personnel in an Airborne Hazard and Burn Pit Registry. Past approaches in evaluation of deployed individuals ranged from common tests such as spirometry, HRCT scanning, full PFTs, bronchoprovocation challenges, and, in some instances, lung biopsies (Krefft SD, et al. Fed Pract. 2015;32[6]:32). More novel evaluations of postdeployment dyspnea include impulse oscillometry, exhaled nitric oxide, bronchoscopy, and cardiopulmonary exercise testing (Huprikar, et al. Chest. 2016;150[4]:S934A).
Members of the CHEST Occupational and Environmental Health NetWork are currently updating comprehensive approaches to evaluate military personnel with chronic respiratory symptoms from deployments. Continued emphasis, however, should be placed on diagnosing and treating common diseases such as asthma, exercise-induced bronchospasm, GERD, and upper airway disorders.
Pedro F. Lucero, MD, FCCP
Steering Committee Member
Clinical pulmonary medicine
Biologics – Birth of a new era of precision management in asthma
An estimated 10% to 20% of patients with severe uncontrolled asthma do not respond to maximal best standard treatments, leading to substantial health-care costs. A paradigm shift is now underway in our approach to the care of these patients with the emergence of novel biologics targeting the complex and interconnected inflammatory pathways in asthma that result in a diverse profile of asthma endotypes and phenotypes (Fig 1).
Current FDA-approved biologics primarily target patients with a T2 high phenotype (Table1).
Dupilumab binds to the alpha unit of the IL-4 receptor and blocks both IL-4 and IL-13. It shows potential efficacy in patients with T2 high asthma with or without eosinophilia but has not yet received FDA approval.
Multiple newer biologics are currently in development (Table 2).
Pulmonologists need to get familiar with the logistics of administration of these novel agents. The two common methods of administering biologics are (1) buy and bill – where the provider buys the drug directly from the distributor; and (2) assignment of benefits (typically administered by a Pharmacy Benefit Manager) - specific dose of the medication is shipped to the physician’s office and physician only bills for the administration. CPT and J codes are shown in Table 1.
Shyamsunder Subramanian, MD, FCCP
Steering Committee Member
Palliative and end-of-life care
Nurse-driven palliative care screening
Palliative care (PC) aims to improve quality of life for patients with a life-threatening illness, providing holistic patient-centered support along the continuum of the disease process. Although frequently implemented in critical care settings, integrating PC in the neuro ICU has been difficult to adopt in practice due to the uncertainty in prognostication of definitive outcomes and practice culture beliefs such as the self-fulfilling prophecy (Frontera, et al. Crit Care Med. 2015;43[9]:1964; Rubin, et al. Curr Opin Crit Care. 2017;23[2]:134; Knies, et al. Semin Neurol. 2016;36[6]:631).
At our institution, a nursing education project was conducted to pilot nurse-driven PC screenings on admission to the neuro ICU. The project evaluated nurse comfort and knowledge with identifying and recommending PC consults. Pre- and post-intervention surveys revealed that education and introduction of a PC screening tool significantly increased nurse comfort and knowledge of PC eligibility.
PC in the neuro ICU can exist to contribute to successful outcomes in patient and family care. Within neurocritical care, incorporating PC is essential to provide extra support to patients and families (Frontera, et al. 2015).
For these reasons and data from the project, nurse-driven screening may encourage appropriate early PC consults. Patient-centered care is the ultimate goal in the management of our patients. Nurse-driven PC screening can help bring various unmet PC needs to the health-care team for opportunities that might not have been met or otherwise assessed. Consider implementing nurse-driven PC screening protocols at your institution to aid in collaborative and proactive interdisciplinary care.
Danielle McCamey, ACNP
Steering Committee Member
Sleep medicine
Diagnostics, devices, and sleep
The past several months have been busy for the Sleep Medicine NetWork. We have been working to represent the interests of our membership and our patients in many arenas.
Devices coded as E0464, defined as life support mechanical ventilators used with mask-based ventilation in the home are being more frequently used. According to the Office of the Inspector General (OIG), there has been an 89-fold increase in billing for E0464 ventilators for Medicare and its beneficiaries between 2009 and 2015, increasing from $3.8M to $340M. In response, the Agency for Healthcare Research and Quality (AHRQ) requested a response to specific questions related to these devices.
In 2018, the CHEST Sleep Medicine NetWork will be participating in a Federal Drug Association-sponsored workshop entitled “Study Design Considerations for Devices including Digital Health Technologies for Sleep-Disordered Breathing (SDB) in Adults,” along with other national organizations and leaders in our field. This workshop will address available technologies for the diagnosis, monitoring, and treatment of SDB, as well as trends for digital health technologies and clinical trial design considerations.
Finally, the Sleep Medicine NetWork has wasted no time after a successful CHEST 2017 in Toronto in planning for the next annual meeting in San Antonio. We are excited to present an exciting curriculum in Sleep Medicine at CHEST 2018, so stay tuned.
Aneesa M. Das, MD, FCCP
NetWork Chair
Occupational and environmental health
Post-deployment lung disease
Since the early 1990s, ongoing military deployments to Southwest Asia remain a unique challenge from a pulmonary symptomology and diagnostic perspective.
Various airborne hazards in the deployment environment include geologic dusts, burn pit smoke, vehicle emissions, and industrial air pollution. Exposures can give rise to both acute respiratory symptoms and, in some instances, chronic lung disease. Currently, data are limited on whether inhalation of airborne particulate matter by military personnel is linked to increases in pulmonary diseases (Morris MJ, et al. US Army Med Dep J. 2016:173).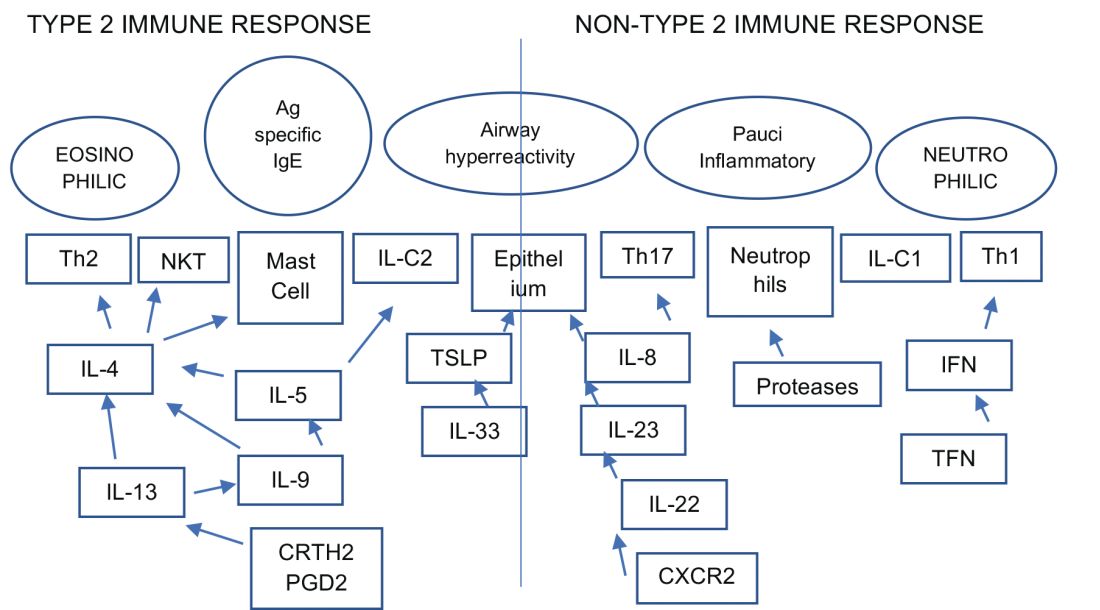
Ongoing research by the Veterans Affairs continues to enroll post-deployed personnel in an Airborne Hazard and Burn Pit Registry. Past approaches in evaluation of deployed individuals ranged from common tests such as spirometry, HRCT scanning, full PFTs, bronchoprovocation challenges, and, in some instances, lung biopsies (Krefft SD, et al. Fed Pract. 2015;32[6]:32). More novel evaluations of postdeployment dyspnea include impulse oscillometry, exhaled nitric oxide, bronchoscopy, and cardiopulmonary exercise testing (Huprikar, et al. Chest. 2016;150[4]:S934A).
Members of the CHEST Occupational and Environmental Health NetWork are currently updating comprehensive approaches to evaluate military personnel with chronic respiratory symptoms from deployments. Continued emphasis, however, should be placed on diagnosing and treating common diseases such as asthma, exercise-induced bronchospasm, GERD, and upper airway disorders.
Pedro F. Lucero, MD, FCCP
Steering Committee Member
Clinical pulmonary medicine
Biologics – Birth of a new era of precision management in asthma
An estimated 10% to 20% of patients with severe uncontrolled asthma do not respond to maximal best standard treatments, leading to substantial health-care costs. A paradigm shift is now underway in our approach to the care of these patients with the emergence of novel biologics targeting the complex and interconnected inflammatory pathways in asthma that result in a diverse profile of asthma endotypes and phenotypes (Fig 1).
Current FDA-approved biologics primarily target patients with a T2 high phenotype (Table1).
Dupilumab binds to the alpha unit of the IL-4 receptor and blocks both IL-4 and IL-13. It shows potential efficacy in patients with T2 high asthma with or without eosinophilia but has not yet received FDA approval.
Multiple newer biologics are currently in development (Table 2).
Pulmonologists need to get familiar with the logistics of administration of these novel agents. The two common methods of administering biologics are (1) buy and bill – where the provider buys the drug directly from the distributor; and (2) assignment of benefits (typically administered by a Pharmacy Benefit Manager) - specific dose of the medication is shipped to the physician’s office and physician only bills for the administration. CPT and J codes are shown in Table 1.
Shyamsunder Subramanian, MD, FCCP
Steering Committee Member


