User login
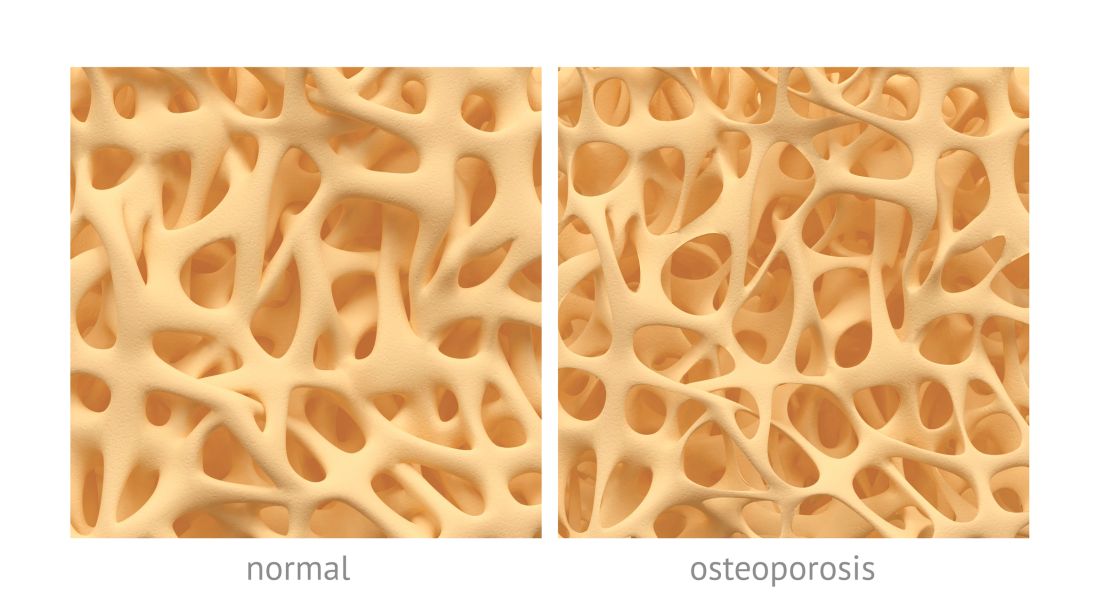
Patients with primary biliary cholangitis (PBC) have lower lumbar spine and hip bone mineral density (BMD) and are at an increased risk of osteoporosis and fracture, according to Junyu Fan, MD, and associates.
In a meta-analysis of 210 potentially relevant articles, only 8 met the study’s criteria. Of those, five studies were pooled and the overall relationship between PBC and osteoporosis risk was assessed. Results found a significant association between PBC (n = 504) and the prevalence of osteoporosis (P = .01), compared with the control group (n = 2,052).
The study additionally examined possible connection between PBC and bone fractures; more fracture events were reported in PBC patients (n = 929) than in controls (n = 8,699; P less than .00001). It is noted that there was no publication bias (P = .476).
“Further clinical management, follow-up, and surveillance issues should be addressed with caution,” researchers concluded. “Given the limited number of studies included, more high-quality studies will be required to determine the mechanisms underpinning the relationship between PBC and osteoporosis risk.”
Find the full study in Clinical Rheumatology (2017. doi: 10.1007/s10067-017-3844-x).
Patients with primary biliary cholangitis (PBC) have lower lumbar spine and hip bone mineral density (BMD) and are at an increased risk of osteoporosis and fracture, according to Junyu Fan, MD, and associates.
In a meta-analysis of 210 potentially relevant articles, only 8 met the study’s criteria. Of those, five studies were pooled and the overall relationship between PBC and osteoporosis risk was assessed. Results found a significant association between PBC (n = 504) and the prevalence of osteoporosis (P = .01), compared with the control group (n = 2,052).
The study additionally examined possible connection between PBC and bone fractures; more fracture events were reported in PBC patients (n = 929) than in controls (n = 8,699; P less than .00001). It is noted that there was no publication bias (P = .476).
“Further clinical management, follow-up, and surveillance issues should be addressed with caution,” researchers concluded. “Given the limited number of studies included, more high-quality studies will be required to determine the mechanisms underpinning the relationship between PBC and osteoporosis risk.”
Find the full study in Clinical Rheumatology (2017. doi: 10.1007/s10067-017-3844-x).
Patients with primary biliary cholangitis (PBC) have lower lumbar spine and hip bone mineral density (BMD) and are at an increased risk of osteoporosis and fracture, according to Junyu Fan, MD, and associates.
In a meta-analysis of 210 potentially relevant articles, only 8 met the study’s criteria. Of those, five studies were pooled and the overall relationship between PBC and osteoporosis risk was assessed. Results found a significant association between PBC (n = 504) and the prevalence of osteoporosis (P = .01), compared with the control group (n = 2,052).
The study additionally examined possible connection between PBC and bone fractures; more fracture events were reported in PBC patients (n = 929) than in controls (n = 8,699; P less than .00001). It is noted that there was no publication bias (P = .476).
“Further clinical management, follow-up, and surveillance issues should be addressed with caution,” researchers concluded. “Given the limited number of studies included, more high-quality studies will be required to determine the mechanisms underpinning the relationship between PBC and osteoporosis risk.”
Find the full study in Clinical Rheumatology (2017. doi: 10.1007/s10067-017-3844-x).
FROM CLINICAL RHEUMATOLOGY