User login
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
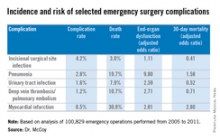
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.

|
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.

|
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.

|
| Dr. Frank Podbielski |
Dr. Frank Podbielski, FCCP, comments: The authors have identified prevention and early treatment of pneumonia as an opportunity to decrease complications and length of stay after emergency surgery. Pneumonia, however, is often a subjective diagnosis with an unclear etiology.
We look forward to the authors' ongoing work on identifying suspected causes of this problem - whether preexisting (prior to the surgical illness), direct sequelae of the surgical illness (e.g., aspiration pneumonia), or hospital acquired (no predisposing etiology).
To best plan a strategy to reduce the complications of pneumonia associated with emergency surgery, it would be helpful to assign a provisional etiology in each case, as well as define "pneumonia" with specific radiographic and clinical parameters.
Dr. Podbielski practices with the department of surgery at St. Joseph Hospital in Chicago, Illinois.
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.
PHILADELPHIA – Emergency surgery accounts for a disproportionate share of surgery-related deaths and complications, and while quality programs focus on prevention of surgical site infections, investigators at Duke University, Durham, N.C., found that pneumonia is the most consequential sequelae of emergency surgery, accounting for more than half of all deaths.
Dr. C. Cameron McCoy, presenting the paper at the annual meeting of the American Association for the Surgery of Trauma, called on the organization to lead efforts to focus quality improvement measures on pneumonia after emergency surgery. “Given their large contribution to postoperative morbidity and mortality, emergency surgery patients in general surgery represent ideal targets for quality improvement programs, but little is known about the incidence of complications and their association with subsequent mortality,” Dr. McCoy said.
He cited the Michigan Surgical Quality Collaborative, which reported that while emergency operations account for approximately one-tenth (11%) of surgeries, they represented almost half (47%) of all postoperative deaths and more than a quarter (28%) of surgical complications (Ann Surg. 2013;257:596-602).
The Duke investigators reviewed 100,829 emergency operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) performed from 2005 to 2011 for eight diagnoses: acute appendicitis, gallbladder disease, gastroduodenal ulcer, diverticulitis, abdominal wall hernia, and intestinal ischemia, obstruction or perforation.
They analyzed the data for rates of five complications, including urinary tract infection, deep vein thrombosis, and pulmonary embolism, in addition to pneumonia, heart attack, and surgical site infection (SSI), and then factored three outcome measures: end organ dysfunction, death, and hospital length of stay. Demographics among the analyzed population were similar.
“Postoperative pneumonia and postoperative myocardial infarction are the only two of our variables to be associated with a significant increase in 30-day postoperative mortality,” Dr. McCoy said. “Of note, pneumonia is also associated with the absolute greatest number of deaths.”
The Duke investigators’ findings were consistent with previous studies, Dr. McCoy said: Emergency operations accounted for 15% of all surgeries and 53% of postoperative deaths. “SSI was the most frequent complication, in 4.2% of our study patients; in second was pneumonia, occurring in about 2.8%. The most infrequent complication was myocardial infarction at 0.5%,” Dr. McCoy said.
However, the consequences of those complications varied significantly. “Surgical site infection was the only studied complication of the five not to be associated with end organ dysfunction,” Dr. McCoy said. All complications resulted in longer postoperative hospital stays, but again, the results varied. “Postoperative pneumonia was associated with the longest postoperative length of stay, with a median of 18 days; surgical site infection was associated with the shortest, with a median of 7 days, for patients with one of the five complications,” he said.
“The data presented here suggest we should focus our efforts on the prevention, recognition, and treatment of postoperative pneumonia following emergency general surgery,” Dr. McCoy said. “Assuming we only have finite resources to pursue quality improvement in acute care surgery, this makes SSI potentially the least relevant to critical care surgeons. In addition, as quality improvement measures are being utilized in pay-for-performance models, it is necessary to validate these measures prior to their application in acute care surgery.”
He added, “The American Association for the Surgery of Trauma is the most appropriate organization to lead the development of quality improvement measures targeting postoperative pneumonia following emergency general surgery.”
Dr. McCoy noted a couple potential limitations of the study: while it did adjust for a wide array of preexisting diseases or conditions that could have affected outcomes; a disproportionate number of cases involved appendectomy.
Dr. McCoy had no financial conflicts to disclose.
Key clinical point: Target pneumonia for prevention after emergency general surgery.
Major finding: Emergency operations account for only 15% of all operations but more than half of postoperative deaths. Of the studied complications, pneumonia was associated with the greatest number of deaths after emergency general surgery.
Data source: Analysis of 100,829 emergency surgery cases in the American College of Surgeons National Surgical Quality Improvement Program database.
Disclosures: Dr. McCoy had no financial conflicts to disclose.