User login
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
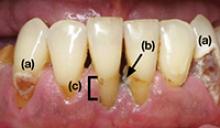
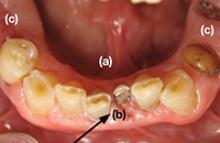
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.