User login
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What may help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt, an ACS Fellow, compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
Spread of robot-assisted surgery
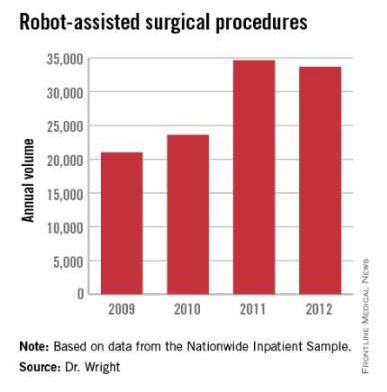
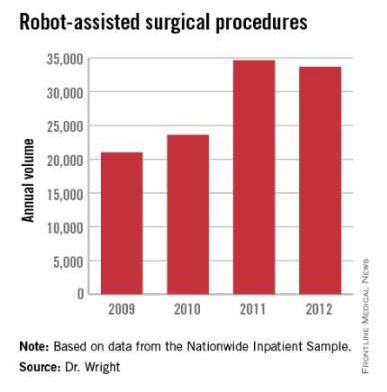
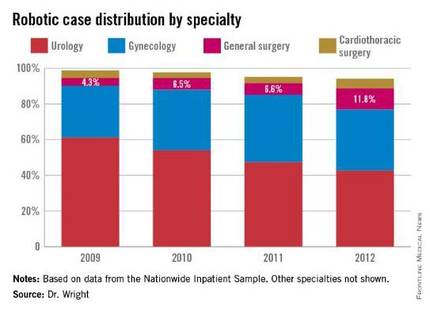
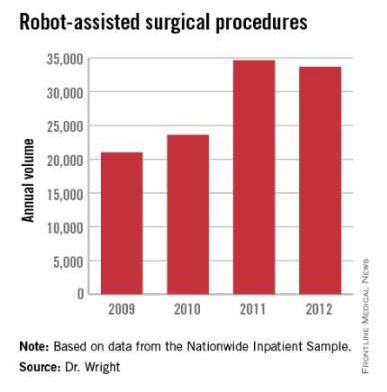
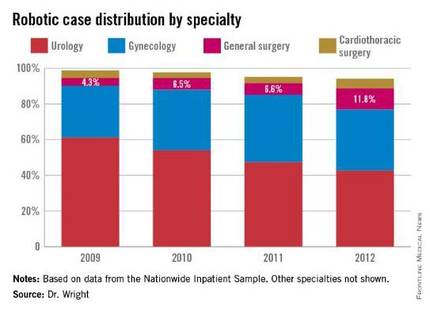
Research by the surgical robot industry and independent investigators shows that use of robotics is on an upward climb. A presentation at the 2015 American College of Surgeons Clinical Congress reveals that, based on retrospective review of the Nationwide Inpatient Sample from 2009-2012 using the ICD-9 code that identifies robot-assisted procedures, there were 113,022 robot-assisted procedures in that period.
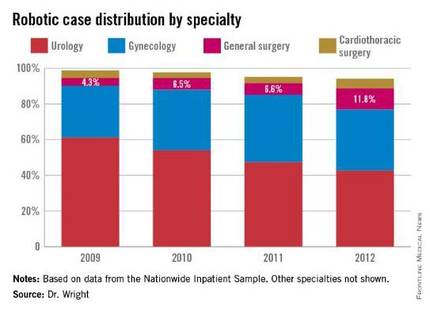
In 2009, there were 21,006 procedures, with the volume growing to 33,713 in 2012. Perhaps more telling about the use of robotics is that it is not confined to specialties with a proven track record such as gynecology and urology. The study, led by Dr. G. Paul Wright of Grand Rapids Medical Education Partners and Michigan State University, shows an increase in robotics use in general surgery procedures by 4.5-fold from 2009-2012, with steady increases each year. General surgery accounted for 11.8% of robot-assisted cases in 2012, Dr. Wright and colleagues reported.
Dr. Wright suggested a number of factors contributing to the “surprising” growth of robotics in general surgery.
“I think the growth is stimulated, at least in part, by market forces,” he said in an interview. “For patients who are the consumers of health care, they are often drawn to [surgeons] whom they perceive to be on the cutting edge. Robotic surgery certainly offers that intrigue. With greater access to the technology, if a patient is seeking a robotic surgery that you do not offer as a surgeon, they can likely find that elsewhere, potentially at your competitor. Another driving force is potentially the ease of suturing with the robot which more resembles open surgery while advanced laparoscopic suturing in tight spaces is a more limited skill set among general surgeons.”
Dr. Wright added that “some of the stigma of robotic surgery is dissolving among surgeons as they become more familiar with the technology. I also believe the market forces will help drive down costs in robotics which may help to increase utilization as well.”
Industry touts cost effectiveness
And while Dr. Pitt is looking forward, the industry is energetically promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci surgery robot presented in a recent press briefing data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now (view the report at http://goo.gl/AfAuT3). But in recent years, the large number of clinical trials comparing robotic vs. laparoscopic surgery for colorectal disease, for example, is equivocal. For many procedures, trials appear to show similar between laparoscopic and robot-assisted approaches, with the main factors in play being length of operation time, hospital stay, and surgical site infection.
According to Intuitive Surgical’s manager of clinical economics, Andrew Yiu, a review of peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures outcomes shows improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others. Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculated the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci IX Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
Costs and other trade-offs
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, an ACS Fellow, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spent in other areas of need.
“Cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
In a study presented by at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao and her colleagues found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery. The study showed that the potential up-front costs can be $1 to $2 million for the robot in addition to ongoing costs related to training and maintenance. Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in the mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
[email protected]
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What may help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt, an ACS Fellow, compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
Spread of robot-assisted surgery
Research by the surgical robot industry and independent investigators shows that use of robotics is on an upward climb. A presentation at the 2015 American College of Surgeons Clinical Congress reveals that, based on retrospective review of the Nationwide Inpatient Sample from 2009-2012 using the ICD-9 code that identifies robot-assisted procedures, there were 113,022 robot-assisted procedures in that period.
In 2009, there were 21,006 procedures, with the volume growing to 33,713 in 2012. Perhaps more telling about the use of robotics is that it is not confined to specialties with a proven track record such as gynecology and urology. The study, led by Dr. G. Paul Wright of Grand Rapids Medical Education Partners and Michigan State University, shows an increase in robotics use in general surgery procedures by 4.5-fold from 2009-2012, with steady increases each year. General surgery accounted for 11.8% of robot-assisted cases in 2012, Dr. Wright and colleagues reported.
Dr. Wright suggested a number of factors contributing to the “surprising” growth of robotics in general surgery.
“I think the growth is stimulated, at least in part, by market forces,” he said in an interview. “For patients who are the consumers of health care, they are often drawn to [surgeons] whom they perceive to be on the cutting edge. Robotic surgery certainly offers that intrigue. With greater access to the technology, if a patient is seeking a robotic surgery that you do not offer as a surgeon, they can likely find that elsewhere, potentially at your competitor. Another driving force is potentially the ease of suturing with the robot which more resembles open surgery while advanced laparoscopic suturing in tight spaces is a more limited skill set among general surgeons.”
Dr. Wright added that “some of the stigma of robotic surgery is dissolving among surgeons as they become more familiar with the technology. I also believe the market forces will help drive down costs in robotics which may help to increase utilization as well.”
Industry touts cost effectiveness
And while Dr. Pitt is looking forward, the industry is energetically promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci surgery robot presented in a recent press briefing data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now (view the report at http://goo.gl/AfAuT3). But in recent years, the large number of clinical trials comparing robotic vs. laparoscopic surgery for colorectal disease, for example, is equivocal. For many procedures, trials appear to show similar between laparoscopic and robot-assisted approaches, with the main factors in play being length of operation time, hospital stay, and surgical site infection.
According to Intuitive Surgical’s manager of clinical economics, Andrew Yiu, a review of peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures outcomes shows improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others. Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculated the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci IX Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
Costs and other trade-offs
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, an ACS Fellow, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spent in other areas of need.
“Cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
In a study presented by at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao and her colleagues found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery. The study showed that the potential up-front costs can be $1 to $2 million for the robot in addition to ongoing costs related to training and maintenance. Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in the mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
[email protected]
Despite the lack of a clear-cut cost-effectiveness case, it appears that the use of robotics in surgery is on its way to becoming the norm.
What may help make that cost-effectiveness case is time, as the hardware becomes cheaper and the technology becomes more widespread.
“I think there are many surgeons who are doing robotic surgery who truly believe that the current of state of the art will bear only a partial resemblance to the state of the art 5-10 years from now,” Dr. Henry Pitt, chief quality officer of the Temple University Health System, Philadelphia, said in an interview. “And part of the persistence by many of the robotic surgeons, while they fully understand that what they are doing is not cost effective now, is that they believe that the next few generations of this technology will become the state of the art and will become cost effective.”
Dr. Pitt, an ACS Fellow, compared the evolution of robotic surgery to that of computers and the application of Moore’s Law, by which the technology advances rapidly while the price eventually comes down.
Spread of robot-assisted surgery
Research by the surgical robot industry and independent investigators shows that use of robotics is on an upward climb. A presentation at the 2015 American College of Surgeons Clinical Congress reveals that, based on retrospective review of the Nationwide Inpatient Sample from 2009-2012 using the ICD-9 code that identifies robot-assisted procedures, there were 113,022 robot-assisted procedures in that period.
In 2009, there were 21,006 procedures, with the volume growing to 33,713 in 2012. Perhaps more telling about the use of robotics is that it is not confined to specialties with a proven track record such as gynecology and urology. The study, led by Dr. G. Paul Wright of Grand Rapids Medical Education Partners and Michigan State University, shows an increase in robotics use in general surgery procedures by 4.5-fold from 2009-2012, with steady increases each year. General surgery accounted for 11.8% of robot-assisted cases in 2012, Dr. Wright and colleagues reported.
Dr. Wright suggested a number of factors contributing to the “surprising” growth of robotics in general surgery.
“I think the growth is stimulated, at least in part, by market forces,” he said in an interview. “For patients who are the consumers of health care, they are often drawn to [surgeons] whom they perceive to be on the cutting edge. Robotic surgery certainly offers that intrigue. With greater access to the technology, if a patient is seeking a robotic surgery that you do not offer as a surgeon, they can likely find that elsewhere, potentially at your competitor. Another driving force is potentially the ease of suturing with the robot which more resembles open surgery while advanced laparoscopic suturing in tight spaces is a more limited skill set among general surgeons.”
Dr. Wright added that “some of the stigma of robotic surgery is dissolving among surgeons as they become more familiar with the technology. I also believe the market forces will help drive down costs in robotics which may help to increase utilization as well.”
Industry touts cost effectiveness
And while Dr. Pitt is looking forward, the industry is energetically promoting the cost effectiveness of robotics today. Intuitive Surgical Inc., manufacturer of the da Vinci surgery robot presented in a recent press briefing data culled from literature found on PubMed showing that robotic surgery, at least with their product, is cost effective now (view the report at http://goo.gl/AfAuT3). But in recent years, the large number of clinical trials comparing robotic vs. laparoscopic surgery for colorectal disease, for example, is equivocal. For many procedures, trials appear to show similar between laparoscopic and robot-assisted approaches, with the main factors in play being length of operation time, hospital stay, and surgical site infection.
According to Intuitive Surgical’s manager of clinical economics, Andrew Yiu, a review of peer-reviewed articles that featured nationwide cohorts of comparisons and included comparisons to both open and laparoscopic procedures outcomes shows improvements across a variety of procedures in terms of hospital stay, lower conversion rates, reduced complications, reduced 30-day readmissions, and improved patient satisfaction, though outcomes were more pronounced in some areas compared with others. Highlighting one procedure in particular – benign hysterectomy – Mr. Yiu noted that rates of minor and major complications associated with robotic vs. laparoscopic surgery were relatively similar but that the conversion rate to open surgery from laparoscopic surgery was 3.9%, compared with 0.9% for da Vinci–assisted surgery.
Overall, Intuitive Surgical calculated the potential savings on the episode of care with the da Vinci system at $1,087 vs. laparoscopic procedures and $2,996 over open surgery.
The company is currently promoting its da Vinci IX Surgical System. Cleared by the Food and Drug Administration in April 2014, Intuitive Surgical says that this latest version has broader capabilities than earlier generations and has been optimized for complex, multiquadrant surgeries.
Costs and other trade-offs
In some ways, robot-assisted surgery is following the same path as laparoscopic surgery, observed Dr. Tyler Hughes of the department of general surgery at McPherson (Kan.) Hospital.
“Certainly, we had the issue back in the late ‘80s and early ‘90s of laparoscopy,” Dr. Hughes said in an interview. “Was it cost effective? Because at the time $30,000 or $40,000 for a laparoscopic set-up seemed like a horse-choking amount of money. However, it converted a 5-day in-the-hospital experience to a 4-hour day-surgery experience. The nonclinical benefits to the patient were so enormous that it took the whole place by storm.”
Dr. Hughes, an ACS Fellow, suggested that the leap in savings elsewhere in the episode of care when using laparoscopic surgery over open surgery is not being mirrored in the robotic space and suggested that money should be spent in other areas of need.
“Cost is going to choke the future if we’re not careful. We need nurses. We need infrastructure. We need to be careful to buy things that really make a big difference,” he said.
In a study presented by at the ACS Clinical Congress on a cost-benefit analysis of robotic vs. laparoscopic colectomy, Anastasia Postoev, a fourth-year medical student at Caribbean Medical University in Willemstad, Curacao and her colleagues found little difference in clinical outcomes but higher costs as a result of added time needed to prepare the robot for surgery. The study showed that the potential up-front costs can be $1 to $2 million for the robot in addition to ongoing costs related to training and maintenance. Dr. Hughes said. “It is a terrific marketing tool in the sense that you can certainly attract a lot of people to a hospital with robotic surgery, but whether or not those outcomes are truly different and the cost of those outcomes are justifiable is yet to be determined.”
The ease of use of robotics, however, could end up being a double-edged sword, particularly if there are areas of the country where robotics may not be as pervasive, or in cases when a conversion to open surgery might be required.
“It is a real concern that trainees are being taught robotic surgery for what is not really needed to be robotic in the mainstream,” Dr. Hughes said. “Then they come out with less experience with straight stick laparoscopy and we’ve certainly seen lots of problems in the laparoscopic range for people once they get to the point that they have to convert to open. We really don’t have a large volume of trainee experience in complex open surgery. That’s a big problem. Robotics certainly isn’t going to make that a lot better.”
[email protected]