User login
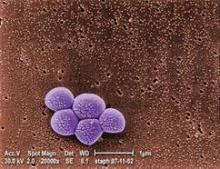
Children who are to have open airway surgery should first be screened for methicillin-resistant Staphylococcus aureus colonization because the prevalence is particularly high in this patient group and treatment drastically reduces postoperative infections, graft loss, and wound dehiscence, researchers reported.
In a retrospective cohort study at a single tertiary pediatric medical center, the prevalence of MRSA colonization was 32.5% during a 2-year period among 175 children who underwent 197 open airway operations, a rate considerably higher than has been reported in patients undergoing other types of surgery, said Dr. Melissa McCarty Statham of the department of otolaryngology–head and neck surgery, Emory University, Atlanta, and her associates. The findings were reported in the February issue of the Archives of Otolaryngology and Head & Neck Surgery.
Because these MRSA-colonized patients were identified and treated appropriately, they did not develop any postoperative MRSA infections, graft losses, or cases of surgical site dehiscence, the investigators noted.
Dr. McCarty Statham and her colleagues studied this issue because, "in our experience, MRSA infection in open airway procedures can be a devastating complication." Such procedures include laryngotracheal reconstruction and grafting, correction of laryngotracheoesophageal clefts, repair of tracheoesophageal fistulas, and laryngotracheal separations.
These patients are at high risk for MRSA colonization because most are preterm; have been tracheotomized; and have serious comorbidities such as pulmonary, gastrointestinal, and cardiac disease. "We consider these factors to be proxies for frequent hospitalization and exposure to antibiotics," the researchers said.
They assessed the 175 patients who underwent such surgery (at a median age of 4 years) at the Cincinnati Children’s Hospital Medical Center in the 2 years after a program of MRSA screening and treatment had been instituted there. Their purpose was to document the prevalence of MRSA colonization in this vulnerable patient population and to assess the effect of the program. Preoperatively, all patients were cultured for MRSA at the nares, perianal area, axila, gastrostomy tube (if present), and tracheotomy tube aspirate (if present).
Colonized patients were given double-strength trimethoprim-sulfamethoxazole empirically for 72 hours before surgery, with clindamycin serving as an alternative in patients who were allergic to sulfa drugs or were carrying organisms resistant to TMP-SMX. Patients with positive nasal cultures also received intranasal mupirocin twice daily.
Perioperatively, colonized patients received either intravenous vancomycin or clindamycin. Postoperatively, they received the same antibiotic regimen for 14 days as they had been given before surgery.
No MRSA-associated infections developed in patients treated according to this protocol, Dr. McCarty Statham and her associates said (Arch. Otolaryngol. Head Neck Surg. 2012;138:153-7).
Postoperative rates of any infection were comparable between the patients colonized with MRSA and those not colonized. There were 10 infections in the MRSA-positive patients (a rate of 15.9%) and 23 infections in the noncolonized patients (a rate of 17.4%).
All 10 infections in the MRSA-colonized patients were caused by nosocomial non-MRSA organisms, as were 19 of the 23 infections in the noncolonized patients.
Three patients who had been MRSA-negative at screening nevertheless developed postoperative MRSA infections after surgery, suggesting that their MRSA was acquired during this hospitalization, the investigators said.
Overall, there were two failures of laryngotracheal reconstruction cartilage grafts and one case of surgical site dehiscence, but none of them occurred in MRSA-positive patients. One graft failure was attributed to impaired wound healing as a result of corticosteroid use; the other to beta-hemolytic Streptococcus infection. The dehiscence was caused by Haemophilus influenzae infection at the surgical site.
This finding suggests that "there is an inherent risk of graft loss and dehiscence in all patients who undergo airway surgery. Infections other than MRSA may be causative factors," Dr. McCarty Statham and her associates noted.
"In view of our results, we advise instituting MRSA screening and treatment protocols in patients undergoing airway surgery," they added.
One of Dr. McCarty Statham’s associates reported being an adviser or consultant to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.
Children who are to have open airway surgery should first be screened for methicillin-resistant Staphylococcus aureus colonization because the prevalence is particularly high in this patient group and treatment drastically reduces postoperative infections, graft loss, and wound dehiscence, researchers reported.
In a retrospective cohort study at a single tertiary pediatric medical center, the prevalence of MRSA colonization was 32.5% during a 2-year period among 175 children who underwent 197 open airway operations, a rate considerably higher than has been reported in patients undergoing other types of surgery, said Dr. Melissa McCarty Statham of the department of otolaryngology–head and neck surgery, Emory University, Atlanta, and her associates. The findings were reported in the February issue of the Archives of Otolaryngology and Head & Neck Surgery.
Because these MRSA-colonized patients were identified and treated appropriately, they did not develop any postoperative MRSA infections, graft losses, or cases of surgical site dehiscence, the investigators noted.
Dr. McCarty Statham and her colleagues studied this issue because, "in our experience, MRSA infection in open airway procedures can be a devastating complication." Such procedures include laryngotracheal reconstruction and grafting, correction of laryngotracheoesophageal clefts, repair of tracheoesophageal fistulas, and laryngotracheal separations.
These patients are at high risk for MRSA colonization because most are preterm; have been tracheotomized; and have serious comorbidities such as pulmonary, gastrointestinal, and cardiac disease. "We consider these factors to be proxies for frequent hospitalization and exposure to antibiotics," the researchers said.
They assessed the 175 patients who underwent such surgery (at a median age of 4 years) at the Cincinnati Children’s Hospital Medical Center in the 2 years after a program of MRSA screening and treatment had been instituted there. Their purpose was to document the prevalence of MRSA colonization in this vulnerable patient population and to assess the effect of the program. Preoperatively, all patients were cultured for MRSA at the nares, perianal area, axila, gastrostomy tube (if present), and tracheotomy tube aspirate (if present).
Colonized patients were given double-strength trimethoprim-sulfamethoxazole empirically for 72 hours before surgery, with clindamycin serving as an alternative in patients who were allergic to sulfa drugs or were carrying organisms resistant to TMP-SMX. Patients with positive nasal cultures also received intranasal mupirocin twice daily.
Perioperatively, colonized patients received either intravenous vancomycin or clindamycin. Postoperatively, they received the same antibiotic regimen for 14 days as they had been given before surgery.
No MRSA-associated infections developed in patients treated according to this protocol, Dr. McCarty Statham and her associates said (Arch. Otolaryngol. Head Neck Surg. 2012;138:153-7).
Postoperative rates of any infection were comparable between the patients colonized with MRSA and those not colonized. There were 10 infections in the MRSA-positive patients (a rate of 15.9%) and 23 infections in the noncolonized patients (a rate of 17.4%).
All 10 infections in the MRSA-colonized patients were caused by nosocomial non-MRSA organisms, as were 19 of the 23 infections in the noncolonized patients.
Three patients who had been MRSA-negative at screening nevertheless developed postoperative MRSA infections after surgery, suggesting that their MRSA was acquired during this hospitalization, the investigators said.
Overall, there were two failures of laryngotracheal reconstruction cartilage grafts and one case of surgical site dehiscence, but none of them occurred in MRSA-positive patients. One graft failure was attributed to impaired wound healing as a result of corticosteroid use; the other to beta-hemolytic Streptococcus infection. The dehiscence was caused by Haemophilus influenzae infection at the surgical site.
This finding suggests that "there is an inherent risk of graft loss and dehiscence in all patients who undergo airway surgery. Infections other than MRSA may be causative factors," Dr. McCarty Statham and her associates noted.
"In view of our results, we advise instituting MRSA screening and treatment protocols in patients undergoing airway surgery," they added.
One of Dr. McCarty Statham’s associates reported being an adviser or consultant to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.
Children who are to have open airway surgery should first be screened for methicillin-resistant Staphylococcus aureus colonization because the prevalence is particularly high in this patient group and treatment drastically reduces postoperative infections, graft loss, and wound dehiscence, researchers reported.
In a retrospective cohort study at a single tertiary pediatric medical center, the prevalence of MRSA colonization was 32.5% during a 2-year period among 175 children who underwent 197 open airway operations, a rate considerably higher than has been reported in patients undergoing other types of surgery, said Dr. Melissa McCarty Statham of the department of otolaryngology–head and neck surgery, Emory University, Atlanta, and her associates. The findings were reported in the February issue of the Archives of Otolaryngology and Head & Neck Surgery.
Because these MRSA-colonized patients were identified and treated appropriately, they did not develop any postoperative MRSA infections, graft losses, or cases of surgical site dehiscence, the investigators noted.
Dr. McCarty Statham and her colleagues studied this issue because, "in our experience, MRSA infection in open airway procedures can be a devastating complication." Such procedures include laryngotracheal reconstruction and grafting, correction of laryngotracheoesophageal clefts, repair of tracheoesophageal fistulas, and laryngotracheal separations.
These patients are at high risk for MRSA colonization because most are preterm; have been tracheotomized; and have serious comorbidities such as pulmonary, gastrointestinal, and cardiac disease. "We consider these factors to be proxies for frequent hospitalization and exposure to antibiotics," the researchers said.
They assessed the 175 patients who underwent such surgery (at a median age of 4 years) at the Cincinnati Children’s Hospital Medical Center in the 2 years after a program of MRSA screening and treatment had been instituted there. Their purpose was to document the prevalence of MRSA colonization in this vulnerable patient population and to assess the effect of the program. Preoperatively, all patients were cultured for MRSA at the nares, perianal area, axila, gastrostomy tube (if present), and tracheotomy tube aspirate (if present).
Colonized patients were given double-strength trimethoprim-sulfamethoxazole empirically for 72 hours before surgery, with clindamycin serving as an alternative in patients who were allergic to sulfa drugs or were carrying organisms resistant to TMP-SMX. Patients with positive nasal cultures also received intranasal mupirocin twice daily.
Perioperatively, colonized patients received either intravenous vancomycin or clindamycin. Postoperatively, they received the same antibiotic regimen for 14 days as they had been given before surgery.
No MRSA-associated infections developed in patients treated according to this protocol, Dr. McCarty Statham and her associates said (Arch. Otolaryngol. Head Neck Surg. 2012;138:153-7).
Postoperative rates of any infection were comparable between the patients colonized with MRSA and those not colonized. There were 10 infections in the MRSA-positive patients (a rate of 15.9%) and 23 infections in the noncolonized patients (a rate of 17.4%).
All 10 infections in the MRSA-colonized patients were caused by nosocomial non-MRSA organisms, as were 19 of the 23 infections in the noncolonized patients.
Three patients who had been MRSA-negative at screening nevertheless developed postoperative MRSA infections after surgery, suggesting that their MRSA was acquired during this hospitalization, the investigators said.
Overall, there were two failures of laryngotracheal reconstruction cartilage grafts and one case of surgical site dehiscence, but none of them occurred in MRSA-positive patients. One graft failure was attributed to impaired wound healing as a result of corticosteroid use; the other to beta-hemolytic Streptococcus infection. The dehiscence was caused by Haemophilus influenzae infection at the surgical site.
This finding suggests that "there is an inherent risk of graft loss and dehiscence in all patients who undergo airway surgery. Infections other than MRSA may be causative factors," Dr. McCarty Statham and her associates noted.
"In view of our results, we advise instituting MRSA screening and treatment protocols in patients undergoing airway surgery," they added.
One of Dr. McCarty Statham’s associates reported being an adviser or consultant to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.
FROM ARCHIVES OF OTOLARYNGOLOGY AND HEAD & NECK SURGERY
Major Finding: The overall rate of MRSA colonization was 33%, but no MRSA infections developed in the screened and treated carriers; rates of any postoperative infection were comparable between colonized (15.9%) and noncolonized (17.4%) patients.
Data Source: This was a retrospective cohort study of 175 children who underwent 197 open airway surgeries at a single pediatric medical center in a 2-year period.
Disclosures: One of Dr. McCarty Statham’s associates reported ties to Acclarent, Gyrus/Olympus, Boston Medical Products, Hood Laboratories, Bryan Medical, and Karl Storz.