User login
› Recommend a
one-time Tdap (tetanus-diphtheria-acellular pertussis) combination vaccine for adults younger than age 64 who need tetanus booster vaccination. A
› Suspect pertussis in a patient who presents with a persistent, paroxysmal cough, with an inspiratory “whoop,” that has lasted for at least
2 weeks. B
› Prescribe a macrolide antibiotic as a first-line treatment for infants, children, and adults who have pertussis. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Despite a high vaccination rate, pertussis is the only vaccine-preventable disease whose incidence is on the rise.1-3 The Centers for Disease Control and Prevention (CDC) reported 48,277 laboratory-confirmed cases in 2012—the most since 1955—and 20 pertussis-related deaths.4 And while only 28,639 pertussis cases were reported in 2013, more than 17,000 cases had already been reported through August 15, 2014, suggesting that the incidence may again be on the rise this year.4
This uptick is likely due to a combination of factors, including a growing awareness of pertussis, and therefore a lower threshold for physicians to test for it. In addition, there’s some evidence that the immunity provided by the currently used pertussis vaccines may wane over time. Recently reported epidemics, including those in California this year and in 2010, as well as in Washington in 2011, have added to this concern.5 This article outlines what you can do to improve prevention, diagnosis, and treatment of pertussis.
A 3-STAGE COURSE OF DISEASE
Bordetella pertussis is an aerobic, gram-negative bacterium that causes symptoms by producing multiple antigenic and biologically active components, including pertussis toxin, filamentous hemagglutinin, and agglutinogens. The bacteria adhere to the cilia in the respiratory tract and initiate an inflammatory cascade that paralyzes the cilia and inhibits the respiratory functions responsible for clearing secretions, largely through an immune-mediated response.
Pertussis has an incubation period of approximately 7 days, but this can last as long as 3 to 6 weeks. The 3 stages in the course of the disease are:6
- Catarrhal. This stage lasts 1 to 2 weeks and is characterized by coryza, sneezing, and a mild, occasional cough.
- Paroxysmal. This stage lasts 1 to 6 weeks, and is characterized by periods of severe coughing “fits” that include the inspiratory "whoop." These coughing episodes may occur more often at night and may worsen in intensity and frequency in the first 2 to 3 weeks and then gradually decrease. This stage also may include posttussive vomiting.
- Convalescent. During this stage, the cough begins to wane.
Next page: Vaccination >>
VACCINATION: DON'T FORGET ADULTS
The 2 vaccines used to prevent pertussis are DTaP (diphtheria-tetanus-acellular pertussis) and Tdap (tetanus-diphtheria-acellular pertussis). The difference between the 2 is that the Tdap vaccine contains a reduced dose of the diphtheria and acellular pertussis vaccines. DTaP is designed primarily for children younger than 7 years of age. Tdap is given to older children and adults. The CDC and Advisory Committee on Immunization Practices recommend that children receive 5 doses of DTaP, one dose at each of the following ages: 2, 4, 6, and 15 to 18 months and at 4 to 6 years.7 All adults 19 years of age and older who have not yet received a dose of Tdap should receive a single dose regardless of when they last received any immunization for tetanus or diphtheria.7-10 A one-time Tdap booster should be given to all adults in place of a tetanus booster (TABLE 1).7-10
What about pregnant women? Tdap should be administered to every pregnant woman between 27 to 36 weeks gestation regardless of Tdap history.7,11 This strategy allows maternal antibodies to transfer to the infant, thus providing some protection to the newborn prior to pediatric vaccinations.
Is the vaccine becoming less effective? Since 1991, the number of cases of pertussis reported in previously vaccinated adolescents and adults has increased, which suggests waning immunity.12,13 Another recent trial investigating the acellular pertussis vaccine found that immunity decreases dramatically 5 years after the fifth dose.14
Recommendations on who should receive pertussis vaccination have been expanded to include adolescents and adults, including pregnant women and those ages 65 and older in close contact with infants, and this should decrease the overall incidence of disease through decreased communicability.15 Current recommendations call for a single adult vaccination; however, ongoing studies are evaluating whether a booster later in life might be necessary.15
DIAGNOSIS NEEDS TO BE CONFIRMED BY LAB TESTING
Any patient who reports having a persistent cough should be considered for pertussis testing and treatment, and any clinician who triages such patients should ask detailed questions about the characteristics and duration of the patient’s symptoms. However, while a prolonged cough is the hallmark of pertussis, there are many other potential causes of this symptom. Therefore, diagnosis of pertussis requires a combination of clinical and laboratory testing, because clinical parameters alone are neither sensitive nor specific enough for pertussis infection.
TABLE 216 outlines the clinical and laboratory diagnostic criteria for pertussis from the CDC and the World Health Organization. Suspect pertussis in a patient who’s had a cough for more than 14 days that includes an inspiratory “whoop.” In infants, pertussis should be suspected in those with symptoms that suggest cough and associated apnea.16 Order laboratory testing for any patients who have clinical signs or symptoms of pertussis.
Continue for the four methods of lab testing >>
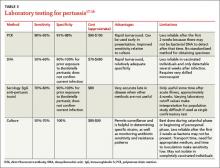
Four methods of lab testing for pertussis infection are polymerase chain reaction (PCR), direct fluorescent antibody (DFA) testing, serologic testing, and culture (TABLE 3).17-19 The sensitivity of these tests is as follows: PCR, 90% to 95%; DFA, 50% to 60%; serologic testing, 70% to 80%; and culture, 50% to 70%. The specificity is: PCR, 95% to 98%; DFA, 90% to 100%; serologic testing, 90% to 100%; and culture, 100%.
PCR is the preferred method because of its rapid turnaround and fairly high sensitivity. The reliability of PCR decreases, however, for a patient who’s had a cough for more than 2 weeks because the individual may have transitioned to the convalescent phase, when less bacterial DNA remain.
Results from DFA testing also are rapidly available, but the need for specialized equipment and a well-trained examiner of the specimen limits widespread use of this test. It also is not particularly sensitive for pertussis.
Serologic testing is less reliable in patients who have received an acellular pertussis vaccine and is not helpful in the first few weeks of infection.
The sensitivity of culture is best if the sample is collected appropriately (more on this in a bit) and within the first 2 weeks of symptoms (catarrhal stage). Culture is also very specific.
Given the strengths and weakness of the different tests, an acceptable method of laboratory confirmation is to obtain PCR and/or culture within the first 2 weeks of symptoms in all age groups.17-20 Testing after 2 weeks should include a combination of PCR and serology.17 It is essential that the clinical specimen used for PCR or culture testing for pertussis is properly collected. (See “Collecting a swab for pertussis testing” below.21)
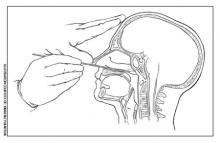
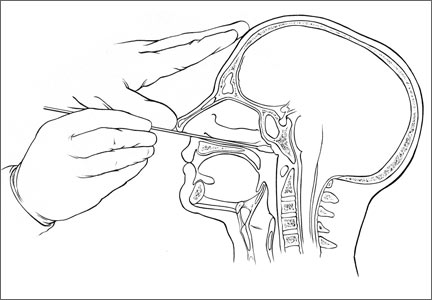
The illustration below shows the correct swab and sampling method. Swab tips may be polyester (such as Dacron or rayon) or they may be nylon-flocked. Cotton-tipped or calcium alginate swabs are not acceptable because the residue will inhibit DNA assays.21 The specimen must be obtained from the posterior nasopharynx and not the nares or oropharynx. The Centers for Disease Control and Prevention offers a video that demonstrates how to properly collect a specimen for testing at http://www.cdc.gov/pertussis/clinical/diagnostic-testing/specimen-collection.html.
Next page: Antibiotics as treatment >>
Tx IS EFFECTIVE WHEN STARTED EARLY
Antibiotics are an effective treatment for pertussis, but they need to be started within the first few weeks of developing symptoms. Studies have not found evidence that antibiotics shorten the duration of pertussis symptoms unless they are given in the catarrhal phase.22,23 It can be challenging to get treatment started during this window, however, because patients may put off seeking care for symptoms they perceive as only minor, such as a cough, until the disease progresses. In addition, physicians may not suspect pertussis in patients who present with a cough they have had for only a short time, and therefore may not test for it.
It may be necessary to rely on clinical suspicion when deciding whether to initiate treatment for pertussis before testing to confirm the diagnosis. For patients in whom clinical suspicion of pertussis is high and who may be in contact with high-risk individuals, it may be acceptable to begin treatment before receiving lab test results.24,25 A recent Cochrane meta-analysis26 recommended initiating treatment to render a patient who has pertussis “noninfectious” but without an expectation of diminishing symptoms.
Limited role for prophylaxis. There is little evidence that prophylactic treatment for pertussis can decrease the spread of the disease. Studies that investigated potential benefits of prophylactic treatment for pertussis have been inconclusive, except for individuals who are in close contact with an infant younger than 6 months of age who has not been fully immunized.27,28
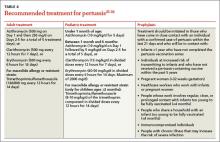
A macrolide antibiotic is generally used to treat pertussis (TABLE 4).25-30 Erythromycin had been the drug of choice, but recent studies have found similar efficacy for azithromycin and clarithromycin.29 For infants younger than one month of age, azithromycin is preferred because in addition to being as effective as other macrolides, it has a better adverse effect profile.29 For patients who are at least 2 months of age, trimethoprim-sulfamethoxazole is an acceptable alternative to a macrolide.
The CDC recommends that any adolescent or adult who has a cough and has had close contact with an individual with a laboratory-confirmed case of pertussis within the past 21 days should be treated.30 Close contacts younger than 7 years of age who have not received the first 4 doses of the pertussis vaccine should be offered treatment.
CORRESPONDENCE
Gary Rivard, DO, Family Medicine Residency Program, Central Maine Medical Center, 76 High Street, Lewiston, ME 04282; [email protected]
1. Orenstein WA. Pertussis in adults: epidemiology, signs, symptoms, and implications for vaccination. Clin Infect Dis. 1999;28 suppl 2:S147-S150.
2. Tanaka M, Vitek CR, Pascual FB, et al. Trends in pertussis among infants in the United States, 1980-1999. JAMA. 2003;290:2968-2975.
3. Vitek CR, Pascual FB, Baughman AL, et al. Increase in deaths from pertussis among young infants in the United States in the 1990s. Pediatr Infect Dis J. 2003;22:628-634.
4. Centers for Disease Control and Prevention. Pertussis outbreak trends. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/pertussis/outbreaks/trends.html. Accessed October 10, 2014.
5. Shapiro ED. Acellular vaccines and resurgence of pertussis. JAMA. 2012;308:2149-2150.
6. Centers for Disease Control and Prevention. Pertussis. In: Epidemiology and Prevention of Vaccine-Preventable Diseases. The Pink Book. 2012. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/pert.html. Accessed October 10, 2014.
7. Centers for Disease Control and Prevention. Pertussis: Summary of vaccine recommendations. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/vpd-vac/pertussis/recs-summary.htm. Accessed October 10, 2014.
8. Lee GM, Murphy TV, Lett S, et al. Cost effectiveness of pertussis vaccination in adults. Am J Prev Med. 2007;32:186-193.
9. Pertussis vaccines: WHO position paper. Wkly Epidemiol Rec. 2010;85:385-400.
10. Kretsinger K, Broder KR, Cortese MM, et al; Centers for Disease Control and Prevention; Advisory Committee on Immunization Practices; Healthcare Infection Control Practices Advisory Committee. Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among healthcare personnel. MMWR Recomm Rep. 2006;55(RR-17):1-37.
11. English P. Pertussis vaccination in pregnant women will protect neonates. Practitioner. 2012;256:5.
12. Winter K, Harriman K, Zipprich J, et al. California pertussis epidemic, 2010. J Pediatr. 2012;161:1091-1096.
13. Centers for Disease Control and Prevention (CDC). Pertussis epidemic—Washington, 2012. MMWR Morb Mortal Wkly Rep. 2012;61:517-522.
14. Klein NP, Bartlett J, Rowhani-Rahbar A, et al. Waning protection after fifth dose of acellular pertussis vaccine in children. N Engl J Med. 2012;367:1012-1019.
15. Centers for Disease Control and Prevention (CDC). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in adults aged 65 years and older - Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2012;61:468-470.
16. Cherry JD, Tan T, Wirsing von Konig C, et al. Clinical definitions of pertussis: Summary of a global pertussis initiative roundtable meeting, February 2011. Clin Infect Dis. 2012;54:1756-1764.
17. Zouari A, Smaoui H, Kechrid A. The diagnosis of pertussis: which method to choose?. Crit Rev Microbiol. 2012;38:111-121.
18. Loeffelholz MJ, Thompson CJ, Long KS, et al. Comparison of PCR, culture, and direct fluorescent-antibody testing for detection of Bordetella pertussis. J Clin Microbiol. 1999;37:2872-2876.
19. Tozzi A, Celentano L, Ciofi degli Atti ML, et al. Diagnosis and management of pertussis. CMAJ. 2005;172:509-515.
20. von König CH, Halperin S, Riffelmann M, et al. Pertussis of adults and infants. Lancet Infect Dis. 2002;2:744-750.
21. Cattaneo LA, Edwards KM. Bordetella pertussis (whooping cough). Semin Pediatr Infect Dis. 1995;6:107-117.
22. Hoppe JE, Eichhorn A. Activity of new macrolides against Bordetella pertussis and Bordetella parapertussis. Eur J Clin Microbiol Infect Dis. 1989;8:653-654.
23. Bass JW. Erythromycin for treatment and prevention of pertussis. Pediatr Infect Dis. 1986;5:154-157.
24. Health Protection Surveillance Centre. Guidelines for the Public Health Management of Pertussis: Public Health Medicine Communicable Disease Group HSE—October 2013. Health Protection Surveillance Centre Web site. Available at: http://www.hpsc.ie/A-Z/VaccinePreventable/PertussisWhoopingCough/InformationforHealthcareWorkers/File,13577,en.pdf. Accessed October 2, 2014.
25. Dodhia H, Miller E. Review of the evidence for the use of erythromycin in the management of persons exposed to pertussis. Epidemiol Infect. 1998;120:143-149.
26. Altunaiji S, Kukuruzovic R, Curtis N, et al. Antibiotics for whooping cough (pertussis). Cochrane Database Syst Rev. 2007;(3):CD004404.
27. Prophylactic erythromycin for whooping-cough contacts. Lancet. 1981;1:772.
28. Halperin SA, Bortolussi R, Langley JM, et al. A randomized, placebo-controlled trial of erythromycin estolate chemoprophylaxis for household contacts of children with culture-positive bordetella pertussis infection. Pediatrics. 1999;104:e42.
29. Langley JM, Halperin SA, Boucher FD, et al; Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC). Azithromycin is as effective as and better tolerated than erythromycin estolate for the treatment of pertussis. Pediatrics. 2004;114:e96-e101.
30. Tiwari T, Murphy TV, Moran J; National Immunization Program, CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR Recomm Rep. 2005;54(RR-14):1-16.
› Recommend a
one-time Tdap (tetanus-diphtheria-acellular pertussis) combination vaccine for adults younger than age 64 who need tetanus booster vaccination. A
› Suspect pertussis in a patient who presents with a persistent, paroxysmal cough, with an inspiratory “whoop,” that has lasted for at least
2 weeks. B
› Prescribe a macrolide antibiotic as a first-line treatment for infants, children, and adults who have pertussis. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Despite a high vaccination rate, pertussis is the only vaccine-preventable disease whose incidence is on the rise.1-3 The Centers for Disease Control and Prevention (CDC) reported 48,277 laboratory-confirmed cases in 2012—the most since 1955—and 20 pertussis-related deaths.4 And while only 28,639 pertussis cases were reported in 2013, more than 17,000 cases had already been reported through August 15, 2014, suggesting that the incidence may again be on the rise this year.4
This uptick is likely due to a combination of factors, including a growing awareness of pertussis, and therefore a lower threshold for physicians to test for it. In addition, there’s some evidence that the immunity provided by the currently used pertussis vaccines may wane over time. Recently reported epidemics, including those in California this year and in 2010, as well as in Washington in 2011, have added to this concern.5 This article outlines what you can do to improve prevention, diagnosis, and treatment of pertussis.
A 3-STAGE COURSE OF DISEASE
Bordetella pertussis is an aerobic, gram-negative bacterium that causes symptoms by producing multiple antigenic and biologically active components, including pertussis toxin, filamentous hemagglutinin, and agglutinogens. The bacteria adhere to the cilia in the respiratory tract and initiate an inflammatory cascade that paralyzes the cilia and inhibits the respiratory functions responsible for clearing secretions, largely through an immune-mediated response.
Pertussis has an incubation period of approximately 7 days, but this can last as long as 3 to 6 weeks. The 3 stages in the course of the disease are:6
- Catarrhal. This stage lasts 1 to 2 weeks and is characterized by coryza, sneezing, and a mild, occasional cough.
- Paroxysmal. This stage lasts 1 to 6 weeks, and is characterized by periods of severe coughing “fits” that include the inspiratory "whoop." These coughing episodes may occur more often at night and may worsen in intensity and frequency in the first 2 to 3 weeks and then gradually decrease. This stage also may include posttussive vomiting.
- Convalescent. During this stage, the cough begins to wane.
Next page: Vaccination >>
VACCINATION: DON'T FORGET ADULTS
The 2 vaccines used to prevent pertussis are DTaP (diphtheria-tetanus-acellular pertussis) and Tdap (tetanus-diphtheria-acellular pertussis). The difference between the 2 is that the Tdap vaccine contains a reduced dose of the diphtheria and acellular pertussis vaccines. DTaP is designed primarily for children younger than 7 years of age. Tdap is given to older children and adults. The CDC and Advisory Committee on Immunization Practices recommend that children receive 5 doses of DTaP, one dose at each of the following ages: 2, 4, 6, and 15 to 18 months and at 4 to 6 years.7 All adults 19 years of age and older who have not yet received a dose of Tdap should receive a single dose regardless of when they last received any immunization for tetanus or diphtheria.7-10 A one-time Tdap booster should be given to all adults in place of a tetanus booster (TABLE 1).7-10
What about pregnant women? Tdap should be administered to every pregnant woman between 27 to 36 weeks gestation regardless of Tdap history.7,11 This strategy allows maternal antibodies to transfer to the infant, thus providing some protection to the newborn prior to pediatric vaccinations.
Is the vaccine becoming less effective? Since 1991, the number of cases of pertussis reported in previously vaccinated adolescents and adults has increased, which suggests waning immunity.12,13 Another recent trial investigating the acellular pertussis vaccine found that immunity decreases dramatically 5 years after the fifth dose.14
Recommendations on who should receive pertussis vaccination have been expanded to include adolescents and adults, including pregnant women and those ages 65 and older in close contact with infants, and this should decrease the overall incidence of disease through decreased communicability.15 Current recommendations call for a single adult vaccination; however, ongoing studies are evaluating whether a booster later in life might be necessary.15
DIAGNOSIS NEEDS TO BE CONFIRMED BY LAB TESTING
Any patient who reports having a persistent cough should be considered for pertussis testing and treatment, and any clinician who triages such patients should ask detailed questions about the characteristics and duration of the patient’s symptoms. However, while a prolonged cough is the hallmark of pertussis, there are many other potential causes of this symptom. Therefore, diagnosis of pertussis requires a combination of clinical and laboratory testing, because clinical parameters alone are neither sensitive nor specific enough for pertussis infection.
TABLE 216 outlines the clinical and laboratory diagnostic criteria for pertussis from the CDC and the World Health Organization. Suspect pertussis in a patient who’s had a cough for more than 14 days that includes an inspiratory “whoop.” In infants, pertussis should be suspected in those with symptoms that suggest cough and associated apnea.16 Order laboratory testing for any patients who have clinical signs or symptoms of pertussis.
Continue for the four methods of lab testing >>
Four methods of lab testing for pertussis infection are polymerase chain reaction (PCR), direct fluorescent antibody (DFA) testing, serologic testing, and culture (TABLE 3).17-19 The sensitivity of these tests is as follows: PCR, 90% to 95%; DFA, 50% to 60%; serologic testing, 70% to 80%; and culture, 50% to 70%. The specificity is: PCR, 95% to 98%; DFA, 90% to 100%; serologic testing, 90% to 100%; and culture, 100%.
PCR is the preferred method because of its rapid turnaround and fairly high sensitivity. The reliability of PCR decreases, however, for a patient who’s had a cough for more than 2 weeks because the individual may have transitioned to the convalescent phase, when less bacterial DNA remain.
Results from DFA testing also are rapidly available, but the need for specialized equipment and a well-trained examiner of the specimen limits widespread use of this test. It also is not particularly sensitive for pertussis.
Serologic testing is less reliable in patients who have received an acellular pertussis vaccine and is not helpful in the first few weeks of infection.
The sensitivity of culture is best if the sample is collected appropriately (more on this in a bit) and within the first 2 weeks of symptoms (catarrhal stage). Culture is also very specific.
Given the strengths and weakness of the different tests, an acceptable method of laboratory confirmation is to obtain PCR and/or culture within the first 2 weeks of symptoms in all age groups.17-20 Testing after 2 weeks should include a combination of PCR and serology.17 It is essential that the clinical specimen used for PCR or culture testing for pertussis is properly collected. (See “Collecting a swab for pertussis testing” below.21)
The illustration below shows the correct swab and sampling method. Swab tips may be polyester (such as Dacron or rayon) or they may be nylon-flocked. Cotton-tipped or calcium alginate swabs are not acceptable because the residue will inhibit DNA assays.21 The specimen must be obtained from the posterior nasopharynx and not the nares or oropharynx. The Centers for Disease Control and Prevention offers a video that demonstrates how to properly collect a specimen for testing at http://www.cdc.gov/pertussis/clinical/diagnostic-testing/specimen-collection.html.
Next page: Antibiotics as treatment >>
Tx IS EFFECTIVE WHEN STARTED EARLY
Antibiotics are an effective treatment for pertussis, but they need to be started within the first few weeks of developing symptoms. Studies have not found evidence that antibiotics shorten the duration of pertussis symptoms unless they are given in the catarrhal phase.22,23 It can be challenging to get treatment started during this window, however, because patients may put off seeking care for symptoms they perceive as only minor, such as a cough, until the disease progresses. In addition, physicians may not suspect pertussis in patients who present with a cough they have had for only a short time, and therefore may not test for it.
It may be necessary to rely on clinical suspicion when deciding whether to initiate treatment for pertussis before testing to confirm the diagnosis. For patients in whom clinical suspicion of pertussis is high and who may be in contact with high-risk individuals, it may be acceptable to begin treatment before receiving lab test results.24,25 A recent Cochrane meta-analysis26 recommended initiating treatment to render a patient who has pertussis “noninfectious” but without an expectation of diminishing symptoms.
Limited role for prophylaxis. There is little evidence that prophylactic treatment for pertussis can decrease the spread of the disease. Studies that investigated potential benefits of prophylactic treatment for pertussis have been inconclusive, except for individuals who are in close contact with an infant younger than 6 months of age who has not been fully immunized.27,28
A macrolide antibiotic is generally used to treat pertussis (TABLE 4).25-30 Erythromycin had been the drug of choice, but recent studies have found similar efficacy for azithromycin and clarithromycin.29 For infants younger than one month of age, azithromycin is preferred because in addition to being as effective as other macrolides, it has a better adverse effect profile.29 For patients who are at least 2 months of age, trimethoprim-sulfamethoxazole is an acceptable alternative to a macrolide.
The CDC recommends that any adolescent or adult who has a cough and has had close contact with an individual with a laboratory-confirmed case of pertussis within the past 21 days should be treated.30 Close contacts younger than 7 years of age who have not received the first 4 doses of the pertussis vaccine should be offered treatment.
CORRESPONDENCE
Gary Rivard, DO, Family Medicine Residency Program, Central Maine Medical Center, 76 High Street, Lewiston, ME 04282; [email protected]
› Recommend a
one-time Tdap (tetanus-diphtheria-acellular pertussis) combination vaccine for adults younger than age 64 who need tetanus booster vaccination. A
› Suspect pertussis in a patient who presents with a persistent, paroxysmal cough, with an inspiratory “whoop,” that has lasted for at least
2 weeks. B
› Prescribe a macrolide antibiotic as a first-line treatment for infants, children, and adults who have pertussis. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Despite a high vaccination rate, pertussis is the only vaccine-preventable disease whose incidence is on the rise.1-3 The Centers for Disease Control and Prevention (CDC) reported 48,277 laboratory-confirmed cases in 2012—the most since 1955—and 20 pertussis-related deaths.4 And while only 28,639 pertussis cases were reported in 2013, more than 17,000 cases had already been reported through August 15, 2014, suggesting that the incidence may again be on the rise this year.4
This uptick is likely due to a combination of factors, including a growing awareness of pertussis, and therefore a lower threshold for physicians to test for it. In addition, there’s some evidence that the immunity provided by the currently used pertussis vaccines may wane over time. Recently reported epidemics, including those in California this year and in 2010, as well as in Washington in 2011, have added to this concern.5 This article outlines what you can do to improve prevention, diagnosis, and treatment of pertussis.
A 3-STAGE COURSE OF DISEASE
Bordetella pertussis is an aerobic, gram-negative bacterium that causes symptoms by producing multiple antigenic and biologically active components, including pertussis toxin, filamentous hemagglutinin, and agglutinogens. The bacteria adhere to the cilia in the respiratory tract and initiate an inflammatory cascade that paralyzes the cilia and inhibits the respiratory functions responsible for clearing secretions, largely through an immune-mediated response.
Pertussis has an incubation period of approximately 7 days, but this can last as long as 3 to 6 weeks. The 3 stages in the course of the disease are:6
- Catarrhal. This stage lasts 1 to 2 weeks and is characterized by coryza, sneezing, and a mild, occasional cough.
- Paroxysmal. This stage lasts 1 to 6 weeks, and is characterized by periods of severe coughing “fits” that include the inspiratory "whoop." These coughing episodes may occur more often at night and may worsen in intensity and frequency in the first 2 to 3 weeks and then gradually decrease. This stage also may include posttussive vomiting.
- Convalescent. During this stage, the cough begins to wane.
Next page: Vaccination >>
VACCINATION: DON'T FORGET ADULTS
The 2 vaccines used to prevent pertussis are DTaP (diphtheria-tetanus-acellular pertussis) and Tdap (tetanus-diphtheria-acellular pertussis). The difference between the 2 is that the Tdap vaccine contains a reduced dose of the diphtheria and acellular pertussis vaccines. DTaP is designed primarily for children younger than 7 years of age. Tdap is given to older children and adults. The CDC and Advisory Committee on Immunization Practices recommend that children receive 5 doses of DTaP, one dose at each of the following ages: 2, 4, 6, and 15 to 18 months and at 4 to 6 years.7 All adults 19 years of age and older who have not yet received a dose of Tdap should receive a single dose regardless of when they last received any immunization for tetanus or diphtheria.7-10 A one-time Tdap booster should be given to all adults in place of a tetanus booster (TABLE 1).7-10
What about pregnant women? Tdap should be administered to every pregnant woman between 27 to 36 weeks gestation regardless of Tdap history.7,11 This strategy allows maternal antibodies to transfer to the infant, thus providing some protection to the newborn prior to pediatric vaccinations.
Is the vaccine becoming less effective? Since 1991, the number of cases of pertussis reported in previously vaccinated adolescents and adults has increased, which suggests waning immunity.12,13 Another recent trial investigating the acellular pertussis vaccine found that immunity decreases dramatically 5 years after the fifth dose.14
Recommendations on who should receive pertussis vaccination have been expanded to include adolescents and adults, including pregnant women and those ages 65 and older in close contact with infants, and this should decrease the overall incidence of disease through decreased communicability.15 Current recommendations call for a single adult vaccination; however, ongoing studies are evaluating whether a booster later in life might be necessary.15
DIAGNOSIS NEEDS TO BE CONFIRMED BY LAB TESTING
Any patient who reports having a persistent cough should be considered for pertussis testing and treatment, and any clinician who triages such patients should ask detailed questions about the characteristics and duration of the patient’s symptoms. However, while a prolonged cough is the hallmark of pertussis, there are many other potential causes of this symptom. Therefore, diagnosis of pertussis requires a combination of clinical and laboratory testing, because clinical parameters alone are neither sensitive nor specific enough for pertussis infection.
TABLE 216 outlines the clinical and laboratory diagnostic criteria for pertussis from the CDC and the World Health Organization. Suspect pertussis in a patient who’s had a cough for more than 14 days that includes an inspiratory “whoop.” In infants, pertussis should be suspected in those with symptoms that suggest cough and associated apnea.16 Order laboratory testing for any patients who have clinical signs or symptoms of pertussis.
Continue for the four methods of lab testing >>
Four methods of lab testing for pertussis infection are polymerase chain reaction (PCR), direct fluorescent antibody (DFA) testing, serologic testing, and culture (TABLE 3).17-19 The sensitivity of these tests is as follows: PCR, 90% to 95%; DFA, 50% to 60%; serologic testing, 70% to 80%; and culture, 50% to 70%. The specificity is: PCR, 95% to 98%; DFA, 90% to 100%; serologic testing, 90% to 100%; and culture, 100%.
PCR is the preferred method because of its rapid turnaround and fairly high sensitivity. The reliability of PCR decreases, however, for a patient who’s had a cough for more than 2 weeks because the individual may have transitioned to the convalescent phase, when less bacterial DNA remain.
Results from DFA testing also are rapidly available, but the need for specialized equipment and a well-trained examiner of the specimen limits widespread use of this test. It also is not particularly sensitive for pertussis.
Serologic testing is less reliable in patients who have received an acellular pertussis vaccine and is not helpful in the first few weeks of infection.
The sensitivity of culture is best if the sample is collected appropriately (more on this in a bit) and within the first 2 weeks of symptoms (catarrhal stage). Culture is also very specific.
Given the strengths and weakness of the different tests, an acceptable method of laboratory confirmation is to obtain PCR and/or culture within the first 2 weeks of symptoms in all age groups.17-20 Testing after 2 weeks should include a combination of PCR and serology.17 It is essential that the clinical specimen used for PCR or culture testing for pertussis is properly collected. (See “Collecting a swab for pertussis testing” below.21)
The illustration below shows the correct swab and sampling method. Swab tips may be polyester (such as Dacron or rayon) or they may be nylon-flocked. Cotton-tipped or calcium alginate swabs are not acceptable because the residue will inhibit DNA assays.21 The specimen must be obtained from the posterior nasopharynx and not the nares or oropharynx. The Centers for Disease Control and Prevention offers a video that demonstrates how to properly collect a specimen for testing at http://www.cdc.gov/pertussis/clinical/diagnostic-testing/specimen-collection.html.
Next page: Antibiotics as treatment >>
Tx IS EFFECTIVE WHEN STARTED EARLY
Antibiotics are an effective treatment for pertussis, but they need to be started within the first few weeks of developing symptoms. Studies have not found evidence that antibiotics shorten the duration of pertussis symptoms unless they are given in the catarrhal phase.22,23 It can be challenging to get treatment started during this window, however, because patients may put off seeking care for symptoms they perceive as only minor, such as a cough, until the disease progresses. In addition, physicians may not suspect pertussis in patients who present with a cough they have had for only a short time, and therefore may not test for it.
It may be necessary to rely on clinical suspicion when deciding whether to initiate treatment for pertussis before testing to confirm the diagnosis. For patients in whom clinical suspicion of pertussis is high and who may be in contact with high-risk individuals, it may be acceptable to begin treatment before receiving lab test results.24,25 A recent Cochrane meta-analysis26 recommended initiating treatment to render a patient who has pertussis “noninfectious” but without an expectation of diminishing symptoms.
Limited role for prophylaxis. There is little evidence that prophylactic treatment for pertussis can decrease the spread of the disease. Studies that investigated potential benefits of prophylactic treatment for pertussis have been inconclusive, except for individuals who are in close contact with an infant younger than 6 months of age who has not been fully immunized.27,28
A macrolide antibiotic is generally used to treat pertussis (TABLE 4).25-30 Erythromycin had been the drug of choice, but recent studies have found similar efficacy for azithromycin and clarithromycin.29 For infants younger than one month of age, azithromycin is preferred because in addition to being as effective as other macrolides, it has a better adverse effect profile.29 For patients who are at least 2 months of age, trimethoprim-sulfamethoxazole is an acceptable alternative to a macrolide.
The CDC recommends that any adolescent or adult who has a cough and has had close contact with an individual with a laboratory-confirmed case of pertussis within the past 21 days should be treated.30 Close contacts younger than 7 years of age who have not received the first 4 doses of the pertussis vaccine should be offered treatment.
CORRESPONDENCE
Gary Rivard, DO, Family Medicine Residency Program, Central Maine Medical Center, 76 High Street, Lewiston, ME 04282; [email protected]
1. Orenstein WA. Pertussis in adults: epidemiology, signs, symptoms, and implications for vaccination. Clin Infect Dis. 1999;28 suppl 2:S147-S150.
2. Tanaka M, Vitek CR, Pascual FB, et al. Trends in pertussis among infants in the United States, 1980-1999. JAMA. 2003;290:2968-2975.
3. Vitek CR, Pascual FB, Baughman AL, et al. Increase in deaths from pertussis among young infants in the United States in the 1990s. Pediatr Infect Dis J. 2003;22:628-634.
4. Centers for Disease Control and Prevention. Pertussis outbreak trends. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/pertussis/outbreaks/trends.html. Accessed October 10, 2014.
5. Shapiro ED. Acellular vaccines and resurgence of pertussis. JAMA. 2012;308:2149-2150.
6. Centers for Disease Control and Prevention. Pertussis. In: Epidemiology and Prevention of Vaccine-Preventable Diseases. The Pink Book. 2012. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/pert.html. Accessed October 10, 2014.
7. Centers for Disease Control and Prevention. Pertussis: Summary of vaccine recommendations. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/vpd-vac/pertussis/recs-summary.htm. Accessed October 10, 2014.
8. Lee GM, Murphy TV, Lett S, et al. Cost effectiveness of pertussis vaccination in adults. Am J Prev Med. 2007;32:186-193.
9. Pertussis vaccines: WHO position paper. Wkly Epidemiol Rec. 2010;85:385-400.
10. Kretsinger K, Broder KR, Cortese MM, et al; Centers for Disease Control and Prevention; Advisory Committee on Immunization Practices; Healthcare Infection Control Practices Advisory Committee. Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among healthcare personnel. MMWR Recomm Rep. 2006;55(RR-17):1-37.
11. English P. Pertussis vaccination in pregnant women will protect neonates. Practitioner. 2012;256:5.
12. Winter K, Harriman K, Zipprich J, et al. California pertussis epidemic, 2010. J Pediatr. 2012;161:1091-1096.
13. Centers for Disease Control and Prevention (CDC). Pertussis epidemic—Washington, 2012. MMWR Morb Mortal Wkly Rep. 2012;61:517-522.
14. Klein NP, Bartlett J, Rowhani-Rahbar A, et al. Waning protection after fifth dose of acellular pertussis vaccine in children. N Engl J Med. 2012;367:1012-1019.
15. Centers for Disease Control and Prevention (CDC). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in adults aged 65 years and older - Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2012;61:468-470.
16. Cherry JD, Tan T, Wirsing von Konig C, et al. Clinical definitions of pertussis: Summary of a global pertussis initiative roundtable meeting, February 2011. Clin Infect Dis. 2012;54:1756-1764.
17. Zouari A, Smaoui H, Kechrid A. The diagnosis of pertussis: which method to choose?. Crit Rev Microbiol. 2012;38:111-121.
18. Loeffelholz MJ, Thompson CJ, Long KS, et al. Comparison of PCR, culture, and direct fluorescent-antibody testing for detection of Bordetella pertussis. J Clin Microbiol. 1999;37:2872-2876.
19. Tozzi A, Celentano L, Ciofi degli Atti ML, et al. Diagnosis and management of pertussis. CMAJ. 2005;172:509-515.
20. von König CH, Halperin S, Riffelmann M, et al. Pertussis of adults and infants. Lancet Infect Dis. 2002;2:744-750.
21. Cattaneo LA, Edwards KM. Bordetella pertussis (whooping cough). Semin Pediatr Infect Dis. 1995;6:107-117.
22. Hoppe JE, Eichhorn A. Activity of new macrolides against Bordetella pertussis and Bordetella parapertussis. Eur J Clin Microbiol Infect Dis. 1989;8:653-654.
23. Bass JW. Erythromycin for treatment and prevention of pertussis. Pediatr Infect Dis. 1986;5:154-157.
24. Health Protection Surveillance Centre. Guidelines for the Public Health Management of Pertussis: Public Health Medicine Communicable Disease Group HSE—October 2013. Health Protection Surveillance Centre Web site. Available at: http://www.hpsc.ie/A-Z/VaccinePreventable/PertussisWhoopingCough/InformationforHealthcareWorkers/File,13577,en.pdf. Accessed October 2, 2014.
25. Dodhia H, Miller E. Review of the evidence for the use of erythromycin in the management of persons exposed to pertussis. Epidemiol Infect. 1998;120:143-149.
26. Altunaiji S, Kukuruzovic R, Curtis N, et al. Antibiotics for whooping cough (pertussis). Cochrane Database Syst Rev. 2007;(3):CD004404.
27. Prophylactic erythromycin for whooping-cough contacts. Lancet. 1981;1:772.
28. Halperin SA, Bortolussi R, Langley JM, et al. A randomized, placebo-controlled trial of erythromycin estolate chemoprophylaxis for household contacts of children with culture-positive bordetella pertussis infection. Pediatrics. 1999;104:e42.
29. Langley JM, Halperin SA, Boucher FD, et al; Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC). Azithromycin is as effective as and better tolerated than erythromycin estolate for the treatment of pertussis. Pediatrics. 2004;114:e96-e101.
30. Tiwari T, Murphy TV, Moran J; National Immunization Program, CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR Recomm Rep. 2005;54(RR-14):1-16.
1. Orenstein WA. Pertussis in adults: epidemiology, signs, symptoms, and implications for vaccination. Clin Infect Dis. 1999;28 suppl 2:S147-S150.
2. Tanaka M, Vitek CR, Pascual FB, et al. Trends in pertussis among infants in the United States, 1980-1999. JAMA. 2003;290:2968-2975.
3. Vitek CR, Pascual FB, Baughman AL, et al. Increase in deaths from pertussis among young infants in the United States in the 1990s. Pediatr Infect Dis J. 2003;22:628-634.
4. Centers for Disease Control and Prevention. Pertussis outbreak trends. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/pertussis/outbreaks/trends.html. Accessed October 10, 2014.
5. Shapiro ED. Acellular vaccines and resurgence of pertussis. JAMA. 2012;308:2149-2150.
6. Centers for Disease Control and Prevention. Pertussis. In: Epidemiology and Prevention of Vaccine-Preventable Diseases. The Pink Book. 2012. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/pubs/pinkbook/pert.html. Accessed October 10, 2014.
7. Centers for Disease Control and Prevention. Pertussis: Summary of vaccine recommendations. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/vaccines/vpd-vac/pertussis/recs-summary.htm. Accessed October 10, 2014.
8. Lee GM, Murphy TV, Lett S, et al. Cost effectiveness of pertussis vaccination in adults. Am J Prev Med. 2007;32:186-193.
9. Pertussis vaccines: WHO position paper. Wkly Epidemiol Rec. 2010;85:385-400.
10. Kretsinger K, Broder KR, Cortese MM, et al; Centers for Disease Control and Prevention; Advisory Committee on Immunization Practices; Healthcare Infection Control Practices Advisory Committee. Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among healthcare personnel. MMWR Recomm Rep. 2006;55(RR-17):1-37.
11. English P. Pertussis vaccination in pregnant women will protect neonates. Practitioner. 2012;256:5.
12. Winter K, Harriman K, Zipprich J, et al. California pertussis epidemic, 2010. J Pediatr. 2012;161:1091-1096.
13. Centers for Disease Control and Prevention (CDC). Pertussis epidemic—Washington, 2012. MMWR Morb Mortal Wkly Rep. 2012;61:517-522.
14. Klein NP, Bartlett J, Rowhani-Rahbar A, et al. Waning protection after fifth dose of acellular pertussis vaccine in children. N Engl J Med. 2012;367:1012-1019.
15. Centers for Disease Control and Prevention (CDC). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in adults aged 65 years and older - Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2012;61:468-470.
16. Cherry JD, Tan T, Wirsing von Konig C, et al. Clinical definitions of pertussis: Summary of a global pertussis initiative roundtable meeting, February 2011. Clin Infect Dis. 2012;54:1756-1764.
17. Zouari A, Smaoui H, Kechrid A. The diagnosis of pertussis: which method to choose?. Crit Rev Microbiol. 2012;38:111-121.
18. Loeffelholz MJ, Thompson CJ, Long KS, et al. Comparison of PCR, culture, and direct fluorescent-antibody testing for detection of Bordetella pertussis. J Clin Microbiol. 1999;37:2872-2876.
19. Tozzi A, Celentano L, Ciofi degli Atti ML, et al. Diagnosis and management of pertussis. CMAJ. 2005;172:509-515.
20. von König CH, Halperin S, Riffelmann M, et al. Pertussis of adults and infants. Lancet Infect Dis. 2002;2:744-750.
21. Cattaneo LA, Edwards KM. Bordetella pertussis (whooping cough). Semin Pediatr Infect Dis. 1995;6:107-117.
22. Hoppe JE, Eichhorn A. Activity of new macrolides against Bordetella pertussis and Bordetella parapertussis. Eur J Clin Microbiol Infect Dis. 1989;8:653-654.
23. Bass JW. Erythromycin for treatment and prevention of pertussis. Pediatr Infect Dis. 1986;5:154-157.
24. Health Protection Surveillance Centre. Guidelines for the Public Health Management of Pertussis: Public Health Medicine Communicable Disease Group HSE—October 2013. Health Protection Surveillance Centre Web site. Available at: http://www.hpsc.ie/A-Z/VaccinePreventable/PertussisWhoopingCough/InformationforHealthcareWorkers/File,13577,en.pdf. Accessed October 2, 2014.
25. Dodhia H, Miller E. Review of the evidence for the use of erythromycin in the management of persons exposed to pertussis. Epidemiol Infect. 1998;120:143-149.
26. Altunaiji S, Kukuruzovic R, Curtis N, et al. Antibiotics for whooping cough (pertussis). Cochrane Database Syst Rev. 2007;(3):CD004404.
27. Prophylactic erythromycin for whooping-cough contacts. Lancet. 1981;1:772.
28. Halperin SA, Bortolussi R, Langley JM, et al. A randomized, placebo-controlled trial of erythromycin estolate chemoprophylaxis for household contacts of children with culture-positive bordetella pertussis infection. Pediatrics. 1999;104:e42.
29. Langley JM, Halperin SA, Boucher FD, et al; Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC). Azithromycin is as effective as and better tolerated than erythromycin estolate for the treatment of pertussis. Pediatrics. 2004;114:e96-e101.
30. Tiwari T, Murphy TV, Moran J; National Immunization Program, CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR Recomm Rep. 2005;54(RR-14):1-16.