User login
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
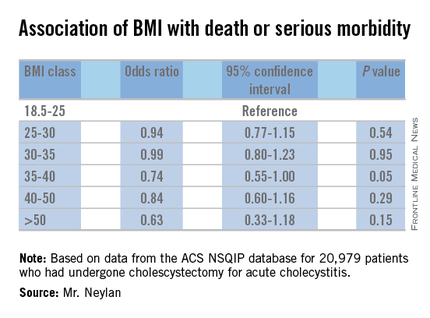
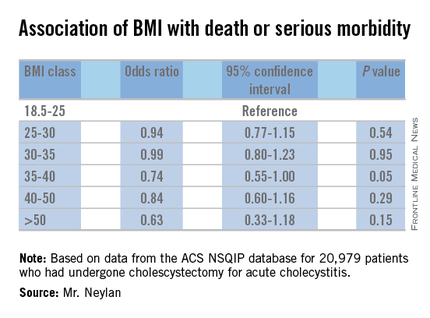
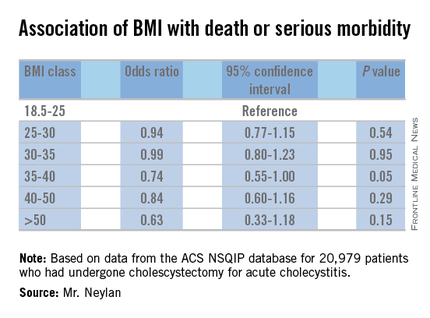
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – Obesity has not been found to be an independent risk factor for death or serious morbidity following cholecystectomy.
Recent, single-center studies have found that cholecystectomy for acute cholecystitis is equally safe in obese and normal weight patients, a finding that a retrospective analysis of 20,979 patients drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database has confirmed.
In presenting the study at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress, Christopher Neylan, the Harrison Surgical Scholar at the Hospital of the University of Pennsylvania, Philadelphia, reported that approximately 900,000 cholecystectomies are performed each year in the United States, about 75% of them on individuals with a body mass index of 25 kg/m2 or greater. “But limited studies into the association of BMI and outcomes following cholecystectomy are available,” Mr. Neylan said. The data from the single-center and institutional reports “may not be applicable across a national sample,” he said.
The primary study endpoint was death/serious morbidity following surgery, with secondary outcomes being system-based complications, such as cardiac and respiratory problems. “When we control for certain factors, there is no independent association between BMI class and death or serious morbidity,” he said. “Elevated BMI class does not independently increase the risk of death or serious morbidity following cholecystectomy for acute cholecystitis,” he said.
The study also found that a patient’s BMI status has no association with secondary outcomes, which included pulmonary and cardiac complications, Neylan said.
The retrospective analysis sampled patients in the ACS NSQIP database who had cholecystectomy for acute cholecystitis from 2008 to 2013. In the dataset, 46% were considered obese with a BMI of 30 or greater; the remainder with BMI less than 30 were considered normal. A total of 87% of the sample had intended laparoscopic cholecystectomy and the conversion rate to open surgery was 4%.
The rates of death/serious morbidity by BMI class were as follows: BMI 18.5-25, 8%; BMI 25-30, 7%; BMI 30-35, 7%; BMI 35-40, 6%; BMI 40-50, 7%; and BMI 50 or greater, 9%.
The investigators developed a multivariable model to assess the independent relationship between BMI class and the primary outcome of death or serious morbidity. The model controlled for the procedure type (open vs. laparoscopic), an interaction term between procedure type and BMI class, and patient-level characteristics such as age, smoking status and the presence of diabetes or hypertension, among other factors. Using BMI 18.5-25 as the reference group, the odds ratios for each subsequent BMI class were each less than 1, and none of the associated P values reached the level of statistical significance (P less than .01).
Mr. Neylan and his coauthors had no financial relationships to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Cholecystectomy for acute cholecystitis has been found to have a similar safety profile in obese and normal-weight patients.
Major finding: Rates of death/serious morbidity ranged from 6% to 9% across six different weight classes ranging from normal weight to morbidly obese.
Data source: Retrospective analysis of 20,979 patients who had cholecystectomy for cholecystitis from 2008 to 2015 drawn from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database.
Disclosures: The study authors reported having no financial disclosures.

