User login
In February, SHM published the first performance assessment tool for HM groups. Now, HMGs across the country are using the “Key Principles and Characteristics of an Effective Hospital Medicine Group” to better understand their organizations’ strengths and areas needing improvement. Knoxville-based TeamHealth is the first to share its findings with SHM and The Hospitalist.
Before SHM published the assessment tool, there were very few objective attempts to provide guidelines that define an effective HMG. At TeamHealth, we viewed this tool as a way to proactively analyze our HMGs—a starting point if you will, to measure our performance against the principles identified in this assessment.
To this end, we allocated an internal analyst to work with our regional leadership teams. We felt it was important to have one person coordinating the analysis in order to ensure consistency with regard to how performance was defined. The analyst, along with the regional medical director and vice president of client services, went through each of the 47 key characteristics and identified the program’s status by evaluating the following statements:
- This characteristic does not apply to our HMG;
- Yes, we fully address the characteristic;
- Yes, we partially address the characteristic; or
- No, we do not materially address the characteristic.
For purposes of scoring, we then assigned a weight to each of the characteristics: three points if “fully addressed”; two points if “partially addressed”; one point if not addressed. We did not find that any of the characteristics fell under the “does not apply to our HMG” category.
A “100% effective” HMG was defined as scoring the highest possible score of 141 (i.e., three points for “fully addressing” each of the 47 characteristics).
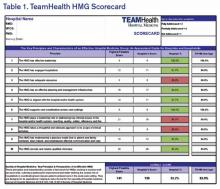
We are currently at the next step in our assessment process. This step involves completion of a scorecard for each individual HMG (see Table 1). Additionally, the individual HMG score will be benchmarked against TeamHealth Hospital Medicine performance overall.
Finally, our regional teams will take the scorecard and meet with their hospital administrators to review the assessment tool, our methodology for completion, and the hospital’s performance.
We fully recognize that some of our hospital partners have measurement standards that differ from those presented by SHM in this assessment; nonetheless, TeamHealth feels the tool in its present state is a significant first step toward quantifying a high-functioning HMG—and will ultimately help improve both hospitalists and hospital performance.
Roberta P. Himebaugh is executive vice president of TeamHealth Hospital Medicine.
In February, SHM published the first performance assessment tool for HM groups. Now, HMGs across the country are using the “Key Principles and Characteristics of an Effective Hospital Medicine Group” to better understand their organizations’ strengths and areas needing improvement. Knoxville-based TeamHealth is the first to share its findings with SHM and The Hospitalist.
Before SHM published the assessment tool, there were very few objective attempts to provide guidelines that define an effective HMG. At TeamHealth, we viewed this tool as a way to proactively analyze our HMGs—a starting point if you will, to measure our performance against the principles identified in this assessment.
To this end, we allocated an internal analyst to work with our regional leadership teams. We felt it was important to have one person coordinating the analysis in order to ensure consistency with regard to how performance was defined. The analyst, along with the regional medical director and vice president of client services, went through each of the 47 key characteristics and identified the program’s status by evaluating the following statements:
- This characteristic does not apply to our HMG;
- Yes, we fully address the characteristic;
- Yes, we partially address the characteristic; or
- No, we do not materially address the characteristic.
For purposes of scoring, we then assigned a weight to each of the characteristics: three points if “fully addressed”; two points if “partially addressed”; one point if not addressed. We did not find that any of the characteristics fell under the “does not apply to our HMG” category.
A “100% effective” HMG was defined as scoring the highest possible score of 141 (i.e., three points for “fully addressing” each of the 47 characteristics).
We are currently at the next step in our assessment process. This step involves completion of a scorecard for each individual HMG (see Table 1). Additionally, the individual HMG score will be benchmarked against TeamHealth Hospital Medicine performance overall.
Finally, our regional teams will take the scorecard and meet with their hospital administrators to review the assessment tool, our methodology for completion, and the hospital’s performance.
We fully recognize that some of our hospital partners have measurement standards that differ from those presented by SHM in this assessment; nonetheless, TeamHealth feels the tool in its present state is a significant first step toward quantifying a high-functioning HMG—and will ultimately help improve both hospitalists and hospital performance.
Roberta P. Himebaugh is executive vice president of TeamHealth Hospital Medicine.
In February, SHM published the first performance assessment tool for HM groups. Now, HMGs across the country are using the “Key Principles and Characteristics of an Effective Hospital Medicine Group” to better understand their organizations’ strengths and areas needing improvement. Knoxville-based TeamHealth is the first to share its findings with SHM and The Hospitalist.
Before SHM published the assessment tool, there were very few objective attempts to provide guidelines that define an effective HMG. At TeamHealth, we viewed this tool as a way to proactively analyze our HMGs—a starting point if you will, to measure our performance against the principles identified in this assessment.
To this end, we allocated an internal analyst to work with our regional leadership teams. We felt it was important to have one person coordinating the analysis in order to ensure consistency with regard to how performance was defined. The analyst, along with the regional medical director and vice president of client services, went through each of the 47 key characteristics and identified the program’s status by evaluating the following statements:
- This characteristic does not apply to our HMG;
- Yes, we fully address the characteristic;
- Yes, we partially address the characteristic; or
- No, we do not materially address the characteristic.
For purposes of scoring, we then assigned a weight to each of the characteristics: three points if “fully addressed”; two points if “partially addressed”; one point if not addressed. We did not find that any of the characteristics fell under the “does not apply to our HMG” category.
A “100% effective” HMG was defined as scoring the highest possible score of 141 (i.e., three points for “fully addressing” each of the 47 characteristics).
We are currently at the next step in our assessment process. This step involves completion of a scorecard for each individual HMG (see Table 1). Additionally, the individual HMG score will be benchmarked against TeamHealth Hospital Medicine performance overall.
Finally, our regional teams will take the scorecard and meet with their hospital administrators to review the assessment tool, our methodology for completion, and the hospital’s performance.
We fully recognize that some of our hospital partners have measurement standards that differ from those presented by SHM in this assessment; nonetheless, TeamHealth feels the tool in its present state is a significant first step toward quantifying a high-functioning HMG—and will ultimately help improve both hospitalists and hospital performance.
Roberta P. Himebaugh is executive vice president of TeamHealth Hospital Medicine.