User login
according to a study published in Chest.
The evidence suggests that chronic obstructive pulmonary disease (COPD) may be a disease of accelerated aging, partly because of its relation to other senescence-related disorders such as osteoporosis and dementia, but also because it shows an exponential increase in prevalence in older age.
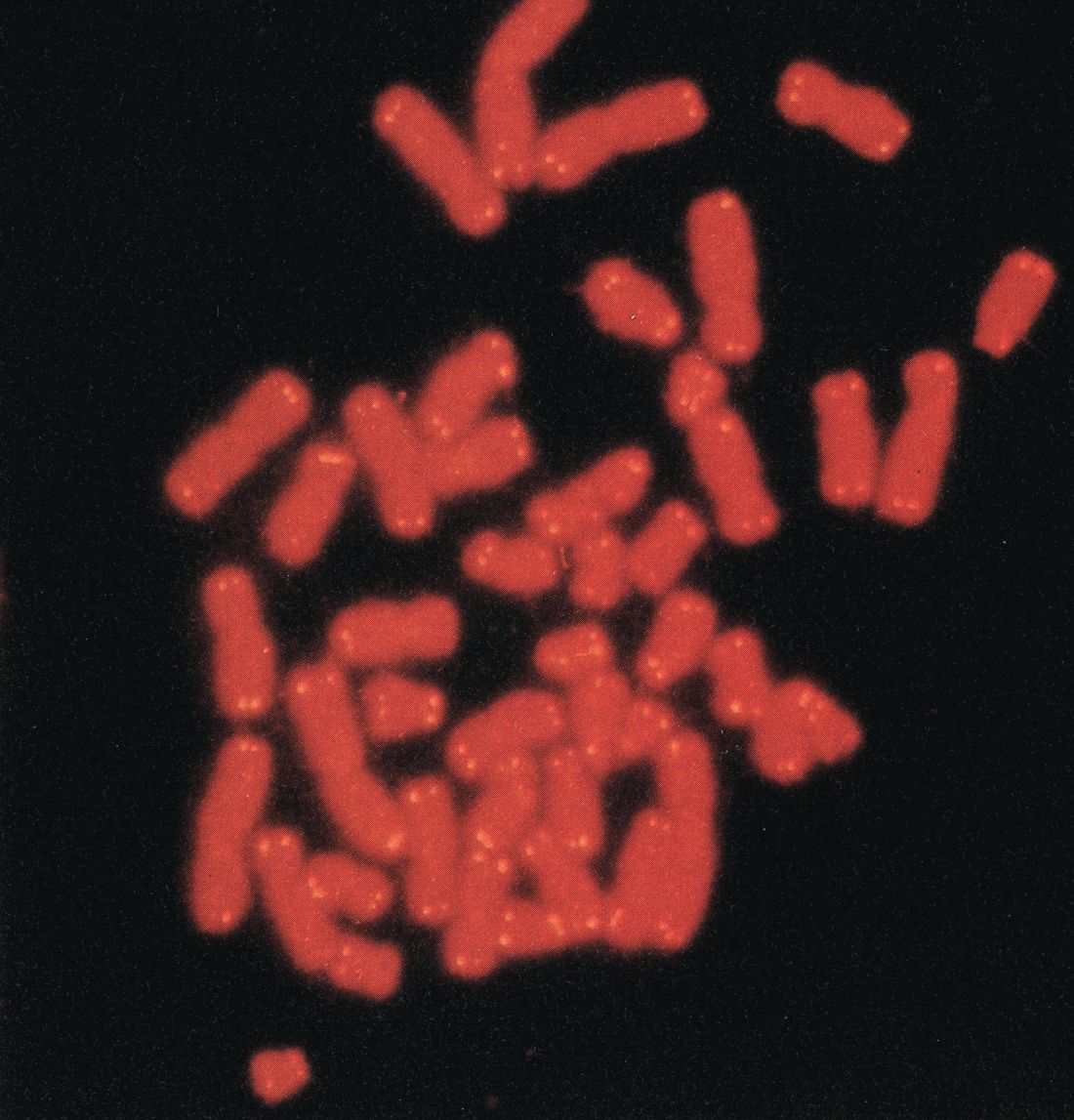
Telomere lengths are a measure of cellular senescence, and previous research has found that the telomeres are shortened in the peripheral leukocytes of patients with COPD, compared with healthy controls.
In this study, researchers examined the absolute telomere length of 576 people with moderate to severe COPD who were participating in the MACRO (Macrolide Azithromycin for Prevention of Exacerbations of COPD) study.
They found that individuals in the lowest quartile of telomere lengths had significantly worse health status and a higher exacerbation rate after accounting for treatment, compared with individuals in the higher quartile.
Patients with shorter telomere length had worse health status, as defined by higher St. George’s Respiratory Questionnaire scores. In the placebo arm of the study, the exacerbation rate (rate ratio, 1.50; 95% confidence interval, 1.16-1.95; P = .002) and mortality risk (hazard ratio, 9.45; 95% CI, 2.85-31.36; P = .015) were significantly higher in the shorter telomere group than in the longer telomere group; these differences were not observed in the azithromycin arm.
Patients with shorter telomeres also had a 800% higher risk of total mortality, compared with individuals with longer telomeres, although this was only evident in the placebo arm of the study, not the azithromycin arm. However, the authors noted that these data should be interpreted with caution because of the small number of deaths during the study.
“Together, these data support the notion that COPD is a systemic disease of accelerated aging and that replicative senescence, denoted by peripheral blood telomeres, is associated with poor health outcomes in COPD,” wrote Minhee Jin, of the University of British Columbia, Vancouver, and coauthors.
“It is now well established that replicative senescence results in a change of cellular phenotype to a proinflammatory state, a process that has been referred to as senescence-associated secretory phenotype,” they added.
The study also found that the median value for telomere length across the study participants – who had a mean age of 66 years – was equivalent to the expected value for someone in their 80s, “suggesting that on average MACRO participants were biologically much older than their chronological age.”
Researchers also noted that patients in the lowest quartile of telomere length had significantly lower forced vital capacity values, which suggested shorter telomeres could be a biomarker of restrictive physiology.
MACRO was funded by the U.S. National Heart, Lung, and Blood Institute, and the biomarker component of the study was funded by the Canadian Respiratory Research Network, Genome Canada, and the St. Paul’s Hospital Foundation. One author was an employee of GenomeDx Biosciences, three declared funding from or consultancies with the pharmaceutical industry. No other conflicts of interest were reported.
SOURCE: Jin M et al. Chest. 2018 Jul 12. doi: 10.1016/j.chest.2018.05.022.
according to a study published in Chest.
The evidence suggests that chronic obstructive pulmonary disease (COPD) may be a disease of accelerated aging, partly because of its relation to other senescence-related disorders such as osteoporosis and dementia, but also because it shows an exponential increase in prevalence in older age.
Telomere lengths are a measure of cellular senescence, and previous research has found that the telomeres are shortened in the peripheral leukocytes of patients with COPD, compared with healthy controls.
In this study, researchers examined the absolute telomere length of 576 people with moderate to severe COPD who were participating in the MACRO (Macrolide Azithromycin for Prevention of Exacerbations of COPD) study.
They found that individuals in the lowest quartile of telomere lengths had significantly worse health status and a higher exacerbation rate after accounting for treatment, compared with individuals in the higher quartile.
Patients with shorter telomere length had worse health status, as defined by higher St. George’s Respiratory Questionnaire scores. In the placebo arm of the study, the exacerbation rate (rate ratio, 1.50; 95% confidence interval, 1.16-1.95; P = .002) and mortality risk (hazard ratio, 9.45; 95% CI, 2.85-31.36; P = .015) were significantly higher in the shorter telomere group than in the longer telomere group; these differences were not observed in the azithromycin arm.
Patients with shorter telomeres also had a 800% higher risk of total mortality, compared with individuals with longer telomeres, although this was only evident in the placebo arm of the study, not the azithromycin arm. However, the authors noted that these data should be interpreted with caution because of the small number of deaths during the study.
“Together, these data support the notion that COPD is a systemic disease of accelerated aging and that replicative senescence, denoted by peripheral blood telomeres, is associated with poor health outcomes in COPD,” wrote Minhee Jin, of the University of British Columbia, Vancouver, and coauthors.
“It is now well established that replicative senescence results in a change of cellular phenotype to a proinflammatory state, a process that has been referred to as senescence-associated secretory phenotype,” they added.
The study also found that the median value for telomere length across the study participants – who had a mean age of 66 years – was equivalent to the expected value for someone in their 80s, “suggesting that on average MACRO participants were biologically much older than their chronological age.”
Researchers also noted that patients in the lowest quartile of telomere length had significantly lower forced vital capacity values, which suggested shorter telomeres could be a biomarker of restrictive physiology.
MACRO was funded by the U.S. National Heart, Lung, and Blood Institute, and the biomarker component of the study was funded by the Canadian Respiratory Research Network, Genome Canada, and the St. Paul’s Hospital Foundation. One author was an employee of GenomeDx Biosciences, three declared funding from or consultancies with the pharmaceutical industry. No other conflicts of interest were reported.
SOURCE: Jin M et al. Chest. 2018 Jul 12. doi: 10.1016/j.chest.2018.05.022.
according to a study published in Chest.
The evidence suggests that chronic obstructive pulmonary disease (COPD) may be a disease of accelerated aging, partly because of its relation to other senescence-related disorders such as osteoporosis and dementia, but also because it shows an exponential increase in prevalence in older age.
Telomere lengths are a measure of cellular senescence, and previous research has found that the telomeres are shortened in the peripheral leukocytes of patients with COPD, compared with healthy controls.
In this study, researchers examined the absolute telomere length of 576 people with moderate to severe COPD who were participating in the MACRO (Macrolide Azithromycin for Prevention of Exacerbations of COPD) study.
They found that individuals in the lowest quartile of telomere lengths had significantly worse health status and a higher exacerbation rate after accounting for treatment, compared with individuals in the higher quartile.
Patients with shorter telomere length had worse health status, as defined by higher St. George’s Respiratory Questionnaire scores. In the placebo arm of the study, the exacerbation rate (rate ratio, 1.50; 95% confidence interval, 1.16-1.95; P = .002) and mortality risk (hazard ratio, 9.45; 95% CI, 2.85-31.36; P = .015) were significantly higher in the shorter telomere group than in the longer telomere group; these differences were not observed in the azithromycin arm.
Patients with shorter telomeres also had a 800% higher risk of total mortality, compared with individuals with longer telomeres, although this was only evident in the placebo arm of the study, not the azithromycin arm. However, the authors noted that these data should be interpreted with caution because of the small number of deaths during the study.
“Together, these data support the notion that COPD is a systemic disease of accelerated aging and that replicative senescence, denoted by peripheral blood telomeres, is associated with poor health outcomes in COPD,” wrote Minhee Jin, of the University of British Columbia, Vancouver, and coauthors.
“It is now well established that replicative senescence results in a change of cellular phenotype to a proinflammatory state, a process that has been referred to as senescence-associated secretory phenotype,” they added.
The study also found that the median value for telomere length across the study participants – who had a mean age of 66 years – was equivalent to the expected value for someone in their 80s, “suggesting that on average MACRO participants were biologically much older than their chronological age.”
Researchers also noted that patients in the lowest quartile of telomere length had significantly lower forced vital capacity values, which suggested shorter telomeres could be a biomarker of restrictive physiology.
MACRO was funded by the U.S. National Heart, Lung, and Blood Institute, and the biomarker component of the study was funded by the Canadian Respiratory Research Network, Genome Canada, and the St. Paul’s Hospital Foundation. One author was an employee of GenomeDx Biosciences, three declared funding from or consultancies with the pharmaceutical industry. No other conflicts of interest were reported.
SOURCE: Jin M et al. Chest. 2018 Jul 12. doi: 10.1016/j.chest.2018.05.022.
FROM CHEST
Key clinical point: Shorter telomeres are linked to an increased risk of chronic obstructive pulmonary disease exacerbations.
Major finding: Patients with shorter telomeres had a 800% higher risk of total mortality, compared with individuals with longer telomeres.
Study details: Data from 576 patients with chronic obstructive pulmonary disease who participated in the MACRO study.
Disclosures: MACRO was funded by the U.S. National Heart, Lung, and Blood Institute, and the biomarker component of the study was funded by the Canadian Respiratory Research Network and the Canadian Institutes of Health Research Genome Canada, and the St. Paul’s Hospital Foundation. One author was an employee of GenomeDx Biosciences, and three authors declared funding from or consultancies with the pharmaceutical industry. No other conflicts of interest were reported.
Source: Jin M et al. Chest. 2018 Jul 12. doi: 10.1016/j.chest.2018.05.022.