User login
BOSTON – It’s been just a year since Bani Chander Roland, MD, FACG, was awarded the 2017 AGA-Medtronic Research & Development Pilot Award in Technology by the AGA Research Foundation, and her team already has recruited 30 patients with irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO) for a study of the gut microbiome and its function. Interim data from her grant will be presented at Digestive Disease Week® 2018 in June in Washington as a poster of distinction.
“Dr. Roland’s research is innovative and clinically relevant. It’s great to see the progress her team has made since receiving this grant from the AGA Research Foundation,” said Robert S. Sandler, MD, MPH, AGAF, chair of the AGA Research Foundation. “I want to thank Medtronic for their partnership on this award and their shared commitment to funding innovative research projects.”
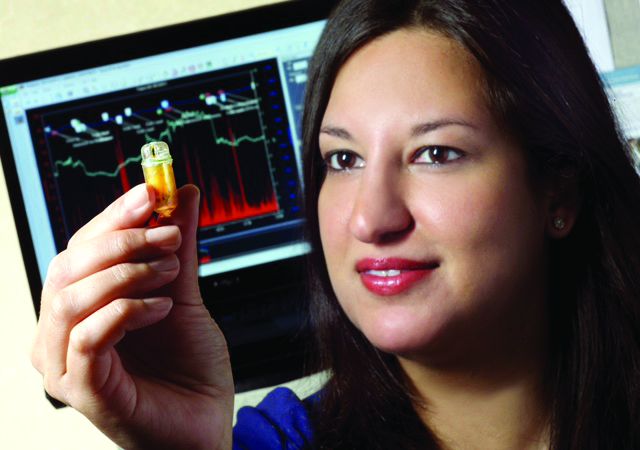
Dr. Roland and her team are testing the hypothesis that IBS and SIBO result from several distinct pathophysiological mechanisms, each of which are associated with their own distinct microbial and inflammatory profile. For the study, they are using a wireless motility capsule (PillCam) – just the kind of technology fostered by the AGA GI Center for Innovation and Technology – to assess alterations in gastrointestinal pathophysiology in patients with suspected IBS and SIBO. They also are obtaining microflora from oropharyngeal, gastric, small bowel, and fecal samples for DNA sequencing. In addition, the team is beginning to study serum samples to test the hypothesis that patients with both IBS and SIBO have increased expression of proinflammatory markers, compared with those with IBS only; they are attempting to correlate the inflammatory markers to specific bacteria.
“IBS is a very common gastrointestinal disorder, and we’re continuing to see an increase in prevalence in Western countries without understanding the etiology for this syndrome,” said Dr. Roland, the director of gastrointestinal motility at Lenox Hill Hospital and Northwell Health System in New York. “Unfortunately, we don’t have any specific or targeted therapies for this patient population because the underlying physiological mechanisms that cause IBS are not very well understood. When we treat these patients with antibiotics, often their symptoms come right back. If we can target the causes of disease in subsets of these patients, we may be able to successfully treat them.”
“We’re very excited to see what changes in the microbiome exist in this patient population, to determine if the microbiome may be another potential area that we can target for treatment,” she added.
To capture the data to be presented in the DDW poster, Dr. Roland’s team used the wireless motility capsule to measure the gastrointestinal transit times, pH, and ileocecal junction pressures of patients with IBS and SIBO as compared with patients who have IBS without evidence of SIBO
“Interestingly, patients who had IBS and SIBO had significantly higher contraction frequency in the stomach and small bowel compared to patients with IBS alone,” Dr. Roland said. Those with both conditions also had lower ileocecal junction pressures. “These are physiological mechanisms that have not been well understood before,” Dr. Roland said. “We have been able to begin delineating some of the underlying physiological mechanisms in this challenging patient population for the first time, using a noninvasive, wireless motility capsule.”
Dr. Roland’s team is now partnering with the hospital’s endocrinology division to compare the circulating inflammatory markers in patients with IBS and SIBO, such as tumor necrosis factor–alpha and interleukin 6, with those in patients who have only IBS. They will use their data to apply for future funding.
Since 2014, the AGA Research Foundation has partnered with medical technology companies such as Medtronic to provide a total of over $450,000 in research grants to six investigators working on novel and innovative technology projects. The AGA Research Foundation will begin accepting applications for the next round of research grants in summer 2018. Stay tuned to www.gastro.org/research-funding.
BOSTON – It’s been just a year since Bani Chander Roland, MD, FACG, was awarded the 2017 AGA-Medtronic Research & Development Pilot Award in Technology by the AGA Research Foundation, and her team already has recruited 30 patients with irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO) for a study of the gut microbiome and its function. Interim data from her grant will be presented at Digestive Disease Week® 2018 in June in Washington as a poster of distinction.
“Dr. Roland’s research is innovative and clinically relevant. It’s great to see the progress her team has made since receiving this grant from the AGA Research Foundation,” said Robert S. Sandler, MD, MPH, AGAF, chair of the AGA Research Foundation. “I want to thank Medtronic for their partnership on this award and their shared commitment to funding innovative research projects.”
Dr. Roland and her team are testing the hypothesis that IBS and SIBO result from several distinct pathophysiological mechanisms, each of which are associated with their own distinct microbial and inflammatory profile. For the study, they are using a wireless motility capsule (PillCam) – just the kind of technology fostered by the AGA GI Center for Innovation and Technology – to assess alterations in gastrointestinal pathophysiology in patients with suspected IBS and SIBO. They also are obtaining microflora from oropharyngeal, gastric, small bowel, and fecal samples for DNA sequencing. In addition, the team is beginning to study serum samples to test the hypothesis that patients with both IBS and SIBO have increased expression of proinflammatory markers, compared with those with IBS only; they are attempting to correlate the inflammatory markers to specific bacteria.
“IBS is a very common gastrointestinal disorder, and we’re continuing to see an increase in prevalence in Western countries without understanding the etiology for this syndrome,” said Dr. Roland, the director of gastrointestinal motility at Lenox Hill Hospital and Northwell Health System in New York. “Unfortunately, we don’t have any specific or targeted therapies for this patient population because the underlying physiological mechanisms that cause IBS are not very well understood. When we treat these patients with antibiotics, often their symptoms come right back. If we can target the causes of disease in subsets of these patients, we may be able to successfully treat them.”
“We’re very excited to see what changes in the microbiome exist in this patient population, to determine if the microbiome may be another potential area that we can target for treatment,” she added.
To capture the data to be presented in the DDW poster, Dr. Roland’s team used the wireless motility capsule to measure the gastrointestinal transit times, pH, and ileocecal junction pressures of patients with IBS and SIBO as compared with patients who have IBS without evidence of SIBO
“Interestingly, patients who had IBS and SIBO had significantly higher contraction frequency in the stomach and small bowel compared to patients with IBS alone,” Dr. Roland said. Those with both conditions also had lower ileocecal junction pressures. “These are physiological mechanisms that have not been well understood before,” Dr. Roland said. “We have been able to begin delineating some of the underlying physiological mechanisms in this challenging patient population for the first time, using a noninvasive, wireless motility capsule.”
Dr. Roland’s team is now partnering with the hospital’s endocrinology division to compare the circulating inflammatory markers in patients with IBS and SIBO, such as tumor necrosis factor–alpha and interleukin 6, with those in patients who have only IBS. They will use their data to apply for future funding.
Since 2014, the AGA Research Foundation has partnered with medical technology companies such as Medtronic to provide a total of over $450,000 in research grants to six investigators working on novel and innovative technology projects. The AGA Research Foundation will begin accepting applications for the next round of research grants in summer 2018. Stay tuned to www.gastro.org/research-funding.
BOSTON – It’s been just a year since Bani Chander Roland, MD, FACG, was awarded the 2017 AGA-Medtronic Research & Development Pilot Award in Technology by the AGA Research Foundation, and her team already has recruited 30 patients with irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO) for a study of the gut microbiome and its function. Interim data from her grant will be presented at Digestive Disease Week® 2018 in June in Washington as a poster of distinction.
“Dr. Roland’s research is innovative and clinically relevant. It’s great to see the progress her team has made since receiving this grant from the AGA Research Foundation,” said Robert S. Sandler, MD, MPH, AGAF, chair of the AGA Research Foundation. “I want to thank Medtronic for their partnership on this award and their shared commitment to funding innovative research projects.”
Dr. Roland and her team are testing the hypothesis that IBS and SIBO result from several distinct pathophysiological mechanisms, each of which are associated with their own distinct microbial and inflammatory profile. For the study, they are using a wireless motility capsule (PillCam) – just the kind of technology fostered by the AGA GI Center for Innovation and Technology – to assess alterations in gastrointestinal pathophysiology in patients with suspected IBS and SIBO. They also are obtaining microflora from oropharyngeal, gastric, small bowel, and fecal samples for DNA sequencing. In addition, the team is beginning to study serum samples to test the hypothesis that patients with both IBS and SIBO have increased expression of proinflammatory markers, compared with those with IBS only; they are attempting to correlate the inflammatory markers to specific bacteria.
“IBS is a very common gastrointestinal disorder, and we’re continuing to see an increase in prevalence in Western countries without understanding the etiology for this syndrome,” said Dr. Roland, the director of gastrointestinal motility at Lenox Hill Hospital and Northwell Health System in New York. “Unfortunately, we don’t have any specific or targeted therapies for this patient population because the underlying physiological mechanisms that cause IBS are not very well understood. When we treat these patients with antibiotics, often their symptoms come right back. If we can target the causes of disease in subsets of these patients, we may be able to successfully treat them.”
“We’re very excited to see what changes in the microbiome exist in this patient population, to determine if the microbiome may be another potential area that we can target for treatment,” she added.
To capture the data to be presented in the DDW poster, Dr. Roland’s team used the wireless motility capsule to measure the gastrointestinal transit times, pH, and ileocecal junction pressures of patients with IBS and SIBO as compared with patients who have IBS without evidence of SIBO
“Interestingly, patients who had IBS and SIBO had significantly higher contraction frequency in the stomach and small bowel compared to patients with IBS alone,” Dr. Roland said. Those with both conditions also had lower ileocecal junction pressures. “These are physiological mechanisms that have not been well understood before,” Dr. Roland said. “We have been able to begin delineating some of the underlying physiological mechanisms in this challenging patient population for the first time, using a noninvasive, wireless motility capsule.”
Dr. Roland’s team is now partnering with the hospital’s endocrinology division to compare the circulating inflammatory markers in patients with IBS and SIBO, such as tumor necrosis factor–alpha and interleukin 6, with those in patients who have only IBS. They will use their data to apply for future funding.
Since 2014, the AGA Research Foundation has partnered with medical technology companies such as Medtronic to provide a total of over $450,000 in research grants to six investigators working on novel and innovative technology projects. The AGA Research Foundation will begin accepting applications for the next round of research grants in summer 2018. Stay tuned to www.gastro.org/research-funding.
REPORTING FROM 2018 AGA TECH SUMMIT