User login
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
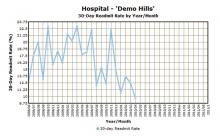
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.