User login
Can a Polygenic Risk Score Turn the Tide on Prostate Cancer Screening?
Incorporating a polygenic risk score into prostate cancer screening could enhance the detection of clinically significant prostate cancer that conventional screening may miss, according to results of the BARCODE 1 clinical trial conducted in the United Kingdom.
The study found that about 72% of participants with high polygenic risk scores were diagnosed with clinically significant prostate cancers, which would not have been detected with prostate-specific antigen (PSA) testing or MRI.
“With this test, it could be possible to turn the tide on prostate cancer,” study author Ros Eeles, PhD, professor of oncogenetics at The Institute of Cancer Research, London, England, said in a statement following the publication of the analysis in The New England Journal of Medicine.
Prostate cancer remains the second most commonly diagnosed cancer among men. As a screening tool, PSA testing has been criticized for leading to a high rate of false positive results and overdiagnosis — defined as a screen-detected cancer that would take longer to progress to clinical cancer than the patient’s lifetime. Both issues can result in overtreatment.
Given prostate cancer’s high heritability and the proliferation of genome-wide association studies identifying common genetic variants, there has been growing interest in using polygenic risk scores to improve risk stratification and guide screening.
“Building on decades of research into the genetic markers of prostate cancer, our study shows that the theory does work in practice — we can identify men at risk of aggressive cancers who need further tests and spare the men who are at lower risk from unnecessary treatments,” said Eeles.
An Adjunct to Screening?
The BARCODE 1 study, conducted in the United Kingdom, tested the clinical utility of a polygenic risk score as an adjunct to screening.
The researchers recruited men aged 55-69 years from primary care centers in the United Kingdom. Using germline DNA extracted from saliva, they derived polygenic risk scores from 130 genetic variants known to be associated with an increased risk for prostate cancer.
Among a total of 6393 men who had their scores calculated, 745 (12%) had a score in the top 10% of genetic risk (≥ 90th percentile) and were invited to undergo further screening.
Of these, 468 (63%) accepted the invite and underwent multiparametric MRI and transperineal prostate biopsy, irrespective of the PSA level. Overall, 187 (40%) were diagnosed with prostate cancer following biopsy. Of the 187 men with prostate cancer, 55% (n = 103) had disease classified as intermediate or high risk (Gleason score ≥ 7) per National Comprehensive Cancer Network criteria and therefore warranted further treatment.
Researchers then compared screening that incorporated polygenic risk scores with standard screening with PSA levels and MRI.
When participants’ risk was stratified by their polygenic risk score, 103 patients (55%) with prostate cancer could be classified as intermediate or higher risk, thus warranting treatment. Overall, 74 (71.8%) of those cancers would have been missed using the standard diagnostic pathway in the United Kingdom, which requires patients to have a high PSA level (> 3.0 μg/L) as well as a positive MRI result. These 74 patients either had PSA levels ≤ 3.0 μg/L or negative MRIs, which would mean these patients would typically fall below the action threshold for further testing.
Of the 103 participants warranting treatment, 40 of these men would have been classified as unfavorable intermediate, high, or very high risk, which would require radical treatment. Among this group, roughly 43% would have been missed using the UK diagnostic pathway.
However, the investigators estimated a rate of overdiagnosis with the use of polygenic risk scores of 16%-21%, similar to the overdiagnosis estimates in two prior PSA-based screening studies, signaling that the addition of polygenic risk scores does not necessarily reduce the risk for overdiagnosis.
Overall, “this study is the strongest evidence to date on the clinical utility of a polygenic score for prostate cancer screening,” commented Michael Inouye, professor of systems genomics & population health, University of Cambridge, Cambridge, England, in a statement from the UK nonprofit Science Media Centre (SMC).
“I suspect we will look back on this as a landmark study that really made the clinical case for polygenic scores as a new tool that moved health systems from disease management to early detection and prevention,” said Inouye, who was not involved in the study.
However, other experts were more cautious about the findings.
Dusko Ilic, MD, professor of stem cell sciences, King’s College London, London, England, said the results are “promising, especially in identifying significant cancers that would otherwise be missed,” but cautioned that “there is no direct evidence yet that using [polygenic risk scores] improves long-term outcomes such as mortality or quality-adjusted life years.”
“Modeling suggests benefit, but empirical confirmation is needed,” Ilic said in the SMC statement.
The hope is that the recently launched TRANSFORM trial will help answer some of these outstanding questions.
The current study suggests that polygenic risk scores for prostate cancer “would be a useful component of a multimodality screening program that assesses age, family history of prostate cancer, PSA, and MRI results as triage tools before biopsy is recommended,” David Hunter, MPH, ScD, with Harvard T. H. Chan School of Public Health, Boston, and University of Oxford, Oxford, England, wrote in an editorial accompanying the study.
“To make this integrated program a reality, however, changes to infrastructure would be needed to make running and analyzing a regulated genome array as easy as requesting a PSA level or ordering an MRI. Clearly, we are far from that future,” Hunter cautioned.
“A possible first step that would require less infrastructure could be to order a polygenic risk score only for men with a positive PSA result, then use the polygenic risk score to determine who should undergo an MRI, and then use all the information to determine whether biopsy is recommended,” Hunter said.
In his view, the current study is a “first step on a long road to evaluating new components of any disease screening pathway.”
The research received funding from the European Research Council, the Bob Willis Fund, Cancer Research UK, the Peacock Trust, and the National Institute for Health and Care Research Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research. Disclosures for authors and editorialists are available with the original article. Inouye and Ilic reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Incorporating a polygenic risk score into prostate cancer screening could enhance the detection of clinically significant prostate cancer that conventional screening may miss, according to results of the BARCODE 1 clinical trial conducted in the United Kingdom.
The study found that about 72% of participants with high polygenic risk scores were diagnosed with clinically significant prostate cancers, which would not have been detected with prostate-specific antigen (PSA) testing or MRI.
“With this test, it could be possible to turn the tide on prostate cancer,” study author Ros Eeles, PhD, professor of oncogenetics at The Institute of Cancer Research, London, England, said in a statement following the publication of the analysis in The New England Journal of Medicine.
Prostate cancer remains the second most commonly diagnosed cancer among men. As a screening tool, PSA testing has been criticized for leading to a high rate of false positive results and overdiagnosis — defined as a screen-detected cancer that would take longer to progress to clinical cancer than the patient’s lifetime. Both issues can result in overtreatment.
Given prostate cancer’s high heritability and the proliferation of genome-wide association studies identifying common genetic variants, there has been growing interest in using polygenic risk scores to improve risk stratification and guide screening.
“Building on decades of research into the genetic markers of prostate cancer, our study shows that the theory does work in practice — we can identify men at risk of aggressive cancers who need further tests and spare the men who are at lower risk from unnecessary treatments,” said Eeles.
An Adjunct to Screening?
The BARCODE 1 study, conducted in the United Kingdom, tested the clinical utility of a polygenic risk score as an adjunct to screening.
The researchers recruited men aged 55-69 years from primary care centers in the United Kingdom. Using germline DNA extracted from saliva, they derived polygenic risk scores from 130 genetic variants known to be associated with an increased risk for prostate cancer.
Among a total of 6393 men who had their scores calculated, 745 (12%) had a score in the top 10% of genetic risk (≥ 90th percentile) and were invited to undergo further screening.
Of these, 468 (63%) accepted the invite and underwent multiparametric MRI and transperineal prostate biopsy, irrespective of the PSA level. Overall, 187 (40%) were diagnosed with prostate cancer following biopsy. Of the 187 men with prostate cancer, 55% (n = 103) had disease classified as intermediate or high risk (Gleason score ≥ 7) per National Comprehensive Cancer Network criteria and therefore warranted further treatment.
Researchers then compared screening that incorporated polygenic risk scores with standard screening with PSA levels and MRI.
When participants’ risk was stratified by their polygenic risk score, 103 patients (55%) with prostate cancer could be classified as intermediate or higher risk, thus warranting treatment. Overall, 74 (71.8%) of those cancers would have been missed using the standard diagnostic pathway in the United Kingdom, which requires patients to have a high PSA level (> 3.0 μg/L) as well as a positive MRI result. These 74 patients either had PSA levels ≤ 3.0 μg/L or negative MRIs, which would mean these patients would typically fall below the action threshold for further testing.
Of the 103 participants warranting treatment, 40 of these men would have been classified as unfavorable intermediate, high, or very high risk, which would require radical treatment. Among this group, roughly 43% would have been missed using the UK diagnostic pathway.
However, the investigators estimated a rate of overdiagnosis with the use of polygenic risk scores of 16%-21%, similar to the overdiagnosis estimates in two prior PSA-based screening studies, signaling that the addition of polygenic risk scores does not necessarily reduce the risk for overdiagnosis.
Overall, “this study is the strongest evidence to date on the clinical utility of a polygenic score for prostate cancer screening,” commented Michael Inouye, professor of systems genomics & population health, University of Cambridge, Cambridge, England, in a statement from the UK nonprofit Science Media Centre (SMC).
“I suspect we will look back on this as a landmark study that really made the clinical case for polygenic scores as a new tool that moved health systems from disease management to early detection and prevention,” said Inouye, who was not involved in the study.
However, other experts were more cautious about the findings.
Dusko Ilic, MD, professor of stem cell sciences, King’s College London, London, England, said the results are “promising, especially in identifying significant cancers that would otherwise be missed,” but cautioned that “there is no direct evidence yet that using [polygenic risk scores] improves long-term outcomes such as mortality or quality-adjusted life years.”
“Modeling suggests benefit, but empirical confirmation is needed,” Ilic said in the SMC statement.
The hope is that the recently launched TRANSFORM trial will help answer some of these outstanding questions.
The current study suggests that polygenic risk scores for prostate cancer “would be a useful component of a multimodality screening program that assesses age, family history of prostate cancer, PSA, and MRI results as triage tools before biopsy is recommended,” David Hunter, MPH, ScD, with Harvard T. H. Chan School of Public Health, Boston, and University of Oxford, Oxford, England, wrote in an editorial accompanying the study.
“To make this integrated program a reality, however, changes to infrastructure would be needed to make running and analyzing a regulated genome array as easy as requesting a PSA level or ordering an MRI. Clearly, we are far from that future,” Hunter cautioned.
“A possible first step that would require less infrastructure could be to order a polygenic risk score only for men with a positive PSA result, then use the polygenic risk score to determine who should undergo an MRI, and then use all the information to determine whether biopsy is recommended,” Hunter said.
In his view, the current study is a “first step on a long road to evaluating new components of any disease screening pathway.”
The research received funding from the European Research Council, the Bob Willis Fund, Cancer Research UK, the Peacock Trust, and the National Institute for Health and Care Research Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research. Disclosures for authors and editorialists are available with the original article. Inouye and Ilic reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Incorporating a polygenic risk score into prostate cancer screening could enhance the detection of clinically significant prostate cancer that conventional screening may miss, according to results of the BARCODE 1 clinical trial conducted in the United Kingdom.
The study found that about 72% of participants with high polygenic risk scores were diagnosed with clinically significant prostate cancers, which would not have been detected with prostate-specific antigen (PSA) testing or MRI.
“With this test, it could be possible to turn the tide on prostate cancer,” study author Ros Eeles, PhD, professor of oncogenetics at The Institute of Cancer Research, London, England, said in a statement following the publication of the analysis in The New England Journal of Medicine.
Prostate cancer remains the second most commonly diagnosed cancer among men. As a screening tool, PSA testing has been criticized for leading to a high rate of false positive results and overdiagnosis — defined as a screen-detected cancer that would take longer to progress to clinical cancer than the patient’s lifetime. Both issues can result in overtreatment.
Given prostate cancer’s high heritability and the proliferation of genome-wide association studies identifying common genetic variants, there has been growing interest in using polygenic risk scores to improve risk stratification and guide screening.
“Building on decades of research into the genetic markers of prostate cancer, our study shows that the theory does work in practice — we can identify men at risk of aggressive cancers who need further tests and spare the men who are at lower risk from unnecessary treatments,” said Eeles.
An Adjunct to Screening?
The BARCODE 1 study, conducted in the United Kingdom, tested the clinical utility of a polygenic risk score as an adjunct to screening.
The researchers recruited men aged 55-69 years from primary care centers in the United Kingdom. Using germline DNA extracted from saliva, they derived polygenic risk scores from 130 genetic variants known to be associated with an increased risk for prostate cancer.
Among a total of 6393 men who had their scores calculated, 745 (12%) had a score in the top 10% of genetic risk (≥ 90th percentile) and were invited to undergo further screening.
Of these, 468 (63%) accepted the invite and underwent multiparametric MRI and transperineal prostate biopsy, irrespective of the PSA level. Overall, 187 (40%) were diagnosed with prostate cancer following biopsy. Of the 187 men with prostate cancer, 55% (n = 103) had disease classified as intermediate or high risk (Gleason score ≥ 7) per National Comprehensive Cancer Network criteria and therefore warranted further treatment.
Researchers then compared screening that incorporated polygenic risk scores with standard screening with PSA levels and MRI.
When participants’ risk was stratified by their polygenic risk score, 103 patients (55%) with prostate cancer could be classified as intermediate or higher risk, thus warranting treatment. Overall, 74 (71.8%) of those cancers would have been missed using the standard diagnostic pathway in the United Kingdom, which requires patients to have a high PSA level (> 3.0 μg/L) as well as a positive MRI result. These 74 patients either had PSA levels ≤ 3.0 μg/L or negative MRIs, which would mean these patients would typically fall below the action threshold for further testing.
Of the 103 participants warranting treatment, 40 of these men would have been classified as unfavorable intermediate, high, or very high risk, which would require radical treatment. Among this group, roughly 43% would have been missed using the UK diagnostic pathway.
However, the investigators estimated a rate of overdiagnosis with the use of polygenic risk scores of 16%-21%, similar to the overdiagnosis estimates in two prior PSA-based screening studies, signaling that the addition of polygenic risk scores does not necessarily reduce the risk for overdiagnosis.
Overall, “this study is the strongest evidence to date on the clinical utility of a polygenic score for prostate cancer screening,” commented Michael Inouye, professor of systems genomics & population health, University of Cambridge, Cambridge, England, in a statement from the UK nonprofit Science Media Centre (SMC).
“I suspect we will look back on this as a landmark study that really made the clinical case for polygenic scores as a new tool that moved health systems from disease management to early detection and prevention,” said Inouye, who was not involved in the study.
However, other experts were more cautious about the findings.
Dusko Ilic, MD, professor of stem cell sciences, King’s College London, London, England, said the results are “promising, especially in identifying significant cancers that would otherwise be missed,” but cautioned that “there is no direct evidence yet that using [polygenic risk scores] improves long-term outcomes such as mortality or quality-adjusted life years.”
“Modeling suggests benefit, but empirical confirmation is needed,” Ilic said in the SMC statement.
The hope is that the recently launched TRANSFORM trial will help answer some of these outstanding questions.
The current study suggests that polygenic risk scores for prostate cancer “would be a useful component of a multimodality screening program that assesses age, family history of prostate cancer, PSA, and MRI results as triage tools before biopsy is recommended,” David Hunter, MPH, ScD, with Harvard T. H. Chan School of Public Health, Boston, and University of Oxford, Oxford, England, wrote in an editorial accompanying the study.
“To make this integrated program a reality, however, changes to infrastructure would be needed to make running and analyzing a regulated genome array as easy as requesting a PSA level or ordering an MRI. Clearly, we are far from that future,” Hunter cautioned.
“A possible first step that would require less infrastructure could be to order a polygenic risk score only for men with a positive PSA result, then use the polygenic risk score to determine who should undergo an MRI, and then use all the information to determine whether biopsy is recommended,” Hunter said.
In his view, the current study is a “first step on a long road to evaluating new components of any disease screening pathway.”
The research received funding from the European Research Council, the Bob Willis Fund, Cancer Research UK, the Peacock Trust, and the National Institute for Health and Care Research Biomedical Research Centre at The Royal Marsden and The Institute of Cancer Research. Disclosures for authors and editorialists are available with the original article. Inouye and Ilic reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Simple Score Predicts Advanced Colorectal Neoplasia in Young Adults
While colorectal cancer (CRC) incidence has declined overall due to screening, early-onset CRC is on the rise, particularly in individuals younger than 45 years — an age group not currently recommended for CRC screening.
Studies have shown that the risk for early-onset advanced neoplasia varies based on several factors, including sex, race, family history of CRC, smoking, alcohol consumption, diabetes, hyperlipidemia, obesity, and diet.
A score that incorporates some of these factors to identify which younger adults are at higher risk for advanced neoplasia, a precursor to CRC, could support earlier, more targeted screening interventions.
The simple clinical score can be easily calculated by primary care providers in the office, Carole Macaron, MD, lead author of the study and a gastroenterologist at Cleveland Clinic, told GI & Hepatology News. “Patients with a high-risk score would be referred for colorectal cancer screening.”
The study was published in Digestive Diseases and Sciences.
To develop and validate their risk score, Macaron and colleagues did a retrospective cross-sectional analysis of 9446 individuals aged 18-44 years (mean age, 36.8 years; 61% women) who underwent colonoscopy at their center.
Advanced neoplasia was defined as a tubular adenoma ≥ 10 mm or any adenoma with villous features or high-grade dysplasia, sessile serrated polyp ≥ 10 mm, sessile serrated polyp with dysplasia, traditional serrated adenoma, or invasive adenocarcinoma.
The 346 (3.7%) individuals found to have advanced neoplasia served as the case group, and the remainder with normal colonoscopy or non-advanced neoplasia served as controls.
A multivariate logistic regression model identified three independent risk factors significantly associated with advanced neoplasia: Higher body mass index (BMI; P = .0157), former and current tobacco use (P = .0009 and P = .0015, respectively), and having a first-degree relative with CRC < 60 years (P < .0001) or other family history of CRC (P = .0117).
The researchers used these risk factors to develop a risk prediction score to estimate the likelihood of detecting advanced neoplasia, which ranged from a risk of 1.8% for patients with a score of 1 to 22.2% for those with a score of 12. Individuals with a score of ≥ 9 had a 14% or higher risk for advanced neoplasia.
Based on the risk model, the likelihood of detecting advanced neoplasia in an asymptomatic 32-year-old overweight individual, with a history of previous tobacco use and a first-degree relative younger than age 60 with CRC would be 20.3%, Macaron and colleagues noted.
The model demonstrated “moderate” discriminatory power in the validation set (C-statistic: 0.645), indicating that it can effectively differentiate between individuals at a higher and lower risk for advanced neoplasia.
Additionally, the authors are exploring ways to improve the discriminatory power of the score, possibly by including additional risk factors.
Given the score is calculated using easily obtainable risk factors for individuals younger than 45 who are at risk for early-onset colorectal neoplasia, it could help guide individualized screening decisions for those in whom screening is not currently offered, Macaron said. It could also serve as a tool for risk communication and shared decision-making.
Integration into electronic health records or online calculators may enhance its accessibility and clinical utility.
The authors noted that this retrospective study was conducted at a single center caring mainly for White non-Hispanic adults, limiting generalizability to the general population and to other races and ethnicities.
Validation in Real-World Setting Needed
“There are no currently accepted advanced colorectal neoplasia risk scores that are used in general practice,” said Steven H. Itzkowitz, MD, AGAF, professor of medicine, oncological sciences, and medical education, Icahn School of Medicine at Mount Sinai in New York City. “If these lesions can be predicted, it would enable these young individuals to undergo screening colonoscopy, which could detect and remove these lesions, thereby preventing CRC.”
Many of the known risk factors (family history, high BMI, or smoking) for CRC development at any age are incorporated within this tool, so it should be feasible to collect these data,” said Itzkowitz, who was not involved with the study.
But he cautioned that accurate and adequate family histories are not always performed. Clinicians also may not have considered combining these factors into an actionable risk score.
“If this score can be externally validated in a real-world setting, it could be a useful addition in our efforts to lower CRC rates among young individuals,” Itzkowitz said.
The study did not receive any funding. Macaron and Itzkowitz reported no competing interests.
A version of this article first appeared on Medscape.com.
While colorectal cancer (CRC) incidence has declined overall due to screening, early-onset CRC is on the rise, particularly in individuals younger than 45 years — an age group not currently recommended for CRC screening.
Studies have shown that the risk for early-onset advanced neoplasia varies based on several factors, including sex, race, family history of CRC, smoking, alcohol consumption, diabetes, hyperlipidemia, obesity, and diet.
A score that incorporates some of these factors to identify which younger adults are at higher risk for advanced neoplasia, a precursor to CRC, could support earlier, more targeted screening interventions.
The simple clinical score can be easily calculated by primary care providers in the office, Carole Macaron, MD, lead author of the study and a gastroenterologist at Cleveland Clinic, told GI & Hepatology News. “Patients with a high-risk score would be referred for colorectal cancer screening.”
The study was published in Digestive Diseases and Sciences.
To develop and validate their risk score, Macaron and colleagues did a retrospective cross-sectional analysis of 9446 individuals aged 18-44 years (mean age, 36.8 years; 61% women) who underwent colonoscopy at their center.
Advanced neoplasia was defined as a tubular adenoma ≥ 10 mm or any adenoma with villous features or high-grade dysplasia, sessile serrated polyp ≥ 10 mm, sessile serrated polyp with dysplasia, traditional serrated adenoma, or invasive adenocarcinoma.
The 346 (3.7%) individuals found to have advanced neoplasia served as the case group, and the remainder with normal colonoscopy or non-advanced neoplasia served as controls.
A multivariate logistic regression model identified three independent risk factors significantly associated with advanced neoplasia: Higher body mass index (BMI; P = .0157), former and current tobacco use (P = .0009 and P = .0015, respectively), and having a first-degree relative with CRC < 60 years (P < .0001) or other family history of CRC (P = .0117).
The researchers used these risk factors to develop a risk prediction score to estimate the likelihood of detecting advanced neoplasia, which ranged from a risk of 1.8% for patients with a score of 1 to 22.2% for those with a score of 12. Individuals with a score of ≥ 9 had a 14% or higher risk for advanced neoplasia.
Based on the risk model, the likelihood of detecting advanced neoplasia in an asymptomatic 32-year-old overweight individual, with a history of previous tobacco use and a first-degree relative younger than age 60 with CRC would be 20.3%, Macaron and colleagues noted.
The model demonstrated “moderate” discriminatory power in the validation set (C-statistic: 0.645), indicating that it can effectively differentiate between individuals at a higher and lower risk for advanced neoplasia.
Additionally, the authors are exploring ways to improve the discriminatory power of the score, possibly by including additional risk factors.
Given the score is calculated using easily obtainable risk factors for individuals younger than 45 who are at risk for early-onset colorectal neoplasia, it could help guide individualized screening decisions for those in whom screening is not currently offered, Macaron said. It could also serve as a tool for risk communication and shared decision-making.
Integration into electronic health records or online calculators may enhance its accessibility and clinical utility.
The authors noted that this retrospective study was conducted at a single center caring mainly for White non-Hispanic adults, limiting generalizability to the general population and to other races and ethnicities.
Validation in Real-World Setting Needed
“There are no currently accepted advanced colorectal neoplasia risk scores that are used in general practice,” said Steven H. Itzkowitz, MD, AGAF, professor of medicine, oncological sciences, and medical education, Icahn School of Medicine at Mount Sinai in New York City. “If these lesions can be predicted, it would enable these young individuals to undergo screening colonoscopy, which could detect and remove these lesions, thereby preventing CRC.”
Many of the known risk factors (family history, high BMI, or smoking) for CRC development at any age are incorporated within this tool, so it should be feasible to collect these data,” said Itzkowitz, who was not involved with the study.
But he cautioned that accurate and adequate family histories are not always performed. Clinicians also may not have considered combining these factors into an actionable risk score.
“If this score can be externally validated in a real-world setting, it could be a useful addition in our efforts to lower CRC rates among young individuals,” Itzkowitz said.
The study did not receive any funding. Macaron and Itzkowitz reported no competing interests.
A version of this article first appeared on Medscape.com.
While colorectal cancer (CRC) incidence has declined overall due to screening, early-onset CRC is on the rise, particularly in individuals younger than 45 years — an age group not currently recommended for CRC screening.
Studies have shown that the risk for early-onset advanced neoplasia varies based on several factors, including sex, race, family history of CRC, smoking, alcohol consumption, diabetes, hyperlipidemia, obesity, and diet.
A score that incorporates some of these factors to identify which younger adults are at higher risk for advanced neoplasia, a precursor to CRC, could support earlier, more targeted screening interventions.
The simple clinical score can be easily calculated by primary care providers in the office, Carole Macaron, MD, lead author of the study and a gastroenterologist at Cleveland Clinic, told GI & Hepatology News. “Patients with a high-risk score would be referred for colorectal cancer screening.”
The study was published in Digestive Diseases and Sciences.
To develop and validate their risk score, Macaron and colleagues did a retrospective cross-sectional analysis of 9446 individuals aged 18-44 years (mean age, 36.8 years; 61% women) who underwent colonoscopy at their center.
Advanced neoplasia was defined as a tubular adenoma ≥ 10 mm or any adenoma with villous features or high-grade dysplasia, sessile serrated polyp ≥ 10 mm, sessile serrated polyp with dysplasia, traditional serrated adenoma, or invasive adenocarcinoma.
The 346 (3.7%) individuals found to have advanced neoplasia served as the case group, and the remainder with normal colonoscopy or non-advanced neoplasia served as controls.
A multivariate logistic regression model identified three independent risk factors significantly associated with advanced neoplasia: Higher body mass index (BMI; P = .0157), former and current tobacco use (P = .0009 and P = .0015, respectively), and having a first-degree relative with CRC < 60 years (P < .0001) or other family history of CRC (P = .0117).
The researchers used these risk factors to develop a risk prediction score to estimate the likelihood of detecting advanced neoplasia, which ranged from a risk of 1.8% for patients with a score of 1 to 22.2% for those with a score of 12. Individuals with a score of ≥ 9 had a 14% or higher risk for advanced neoplasia.
Based on the risk model, the likelihood of detecting advanced neoplasia in an asymptomatic 32-year-old overweight individual, with a history of previous tobacco use and a first-degree relative younger than age 60 with CRC would be 20.3%, Macaron and colleagues noted.
The model demonstrated “moderate” discriminatory power in the validation set (C-statistic: 0.645), indicating that it can effectively differentiate between individuals at a higher and lower risk for advanced neoplasia.
Additionally, the authors are exploring ways to improve the discriminatory power of the score, possibly by including additional risk factors.
Given the score is calculated using easily obtainable risk factors for individuals younger than 45 who are at risk for early-onset colorectal neoplasia, it could help guide individualized screening decisions for those in whom screening is not currently offered, Macaron said. It could also serve as a tool for risk communication and shared decision-making.
Integration into electronic health records or online calculators may enhance its accessibility and clinical utility.
The authors noted that this retrospective study was conducted at a single center caring mainly for White non-Hispanic adults, limiting generalizability to the general population and to other races and ethnicities.
Validation in Real-World Setting Needed
“There are no currently accepted advanced colorectal neoplasia risk scores that are used in general practice,” said Steven H. Itzkowitz, MD, AGAF, professor of medicine, oncological sciences, and medical education, Icahn School of Medicine at Mount Sinai in New York City. “If these lesions can be predicted, it would enable these young individuals to undergo screening colonoscopy, which could detect and remove these lesions, thereby preventing CRC.”
Many of the known risk factors (family history, high BMI, or smoking) for CRC development at any age are incorporated within this tool, so it should be feasible to collect these data,” said Itzkowitz, who was not involved with the study.
But he cautioned that accurate and adequate family histories are not always performed. Clinicians also may not have considered combining these factors into an actionable risk score.
“If this score can be externally validated in a real-world setting, it could be a useful addition in our efforts to lower CRC rates among young individuals,” Itzkowitz said.
The study did not receive any funding. Macaron and Itzkowitz reported no competing interests.
A version of this article first appeared on Medscape.com.
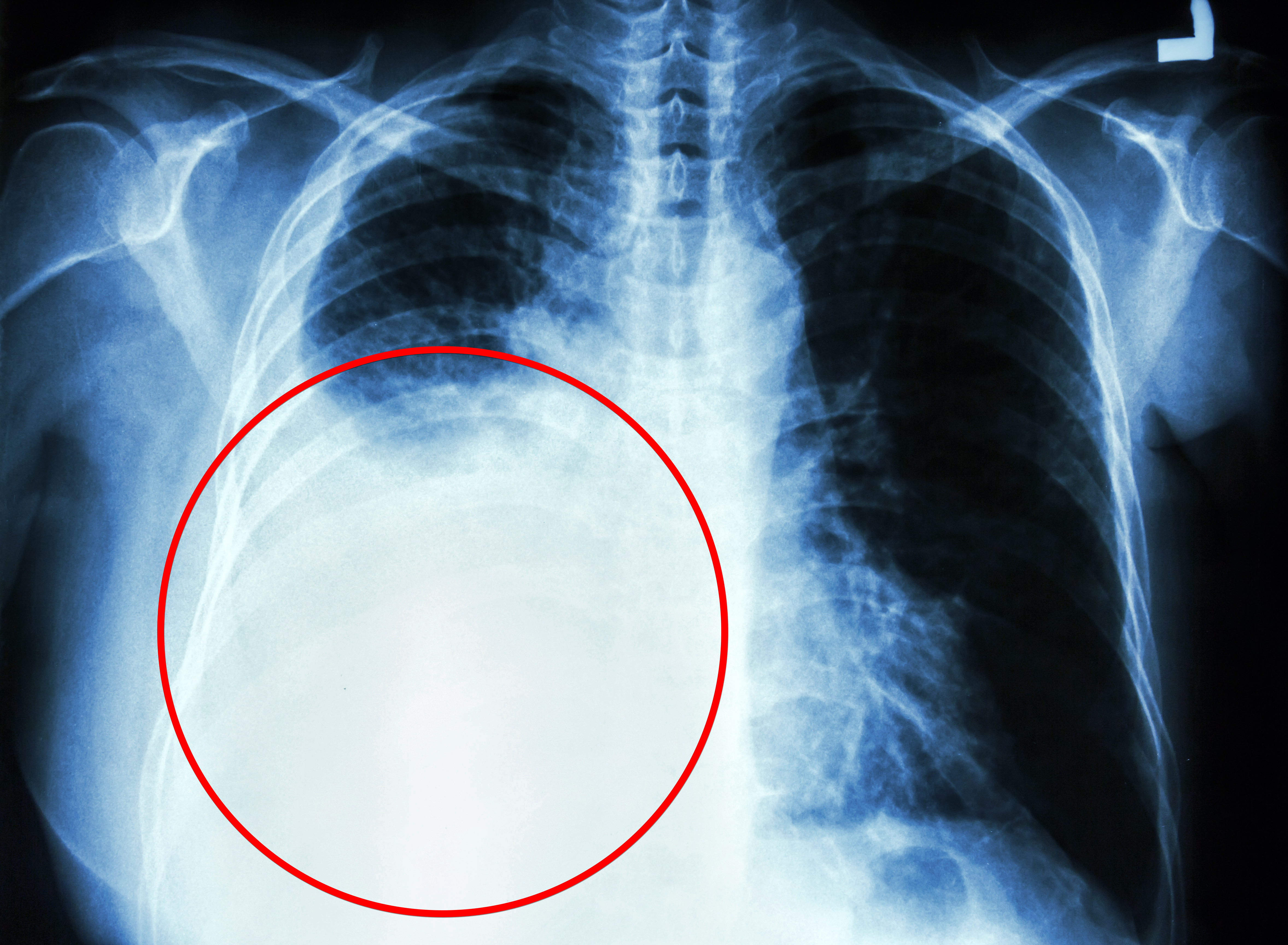
A ‘Fool’s Errand’? Picking a Winner for Treating Early-Stage NSCLC
For years, the default definitive treatment for patients with early-stage I non–small cell lung cancer (NSCLC) has been surgical resection, typically minimally invasive lobectomy with systematic lymph node dissection.
Guidelines from the National Comprehensive Cancer Network (NCCN), the American Society of Clinical Oncology, and the European Society for Medical Oncology all list surgery (in particular, lobectomy) as the primary local therapy for fit, operable patients with stage I NSCLC.
More recently, however, stereotactic body radiotherapy (SBRT), also called stereotactic ablative radiotherapy, has emerged as a definitive treatment option for stage I NSCLC, especially for older, less fit patients who are unsuitable or deemed high-risk for surgery.
“We see patients in our practice who cannot undergo surgery or who may not have adequate lung function to be able to tolerate surgery, and for these patients who are medically inoperable or surgically unresectable, radiation therapy may be a reasonable option,” Charu Aggarwal, MD, MPH, professor and lung cancer specialist, University of Pennsylvania, Philadelphia, told this news organization.
Given some encouraging data suggesting that SBRT could provide similar survival outcomes and be an alternative to surgery for operable disease, SBRT is also increasingly being considered in these early-stage patients. However, other evidence indicates that SBRT may be associated with higher rates of regional and distant recurrences and worse long-term survival, particularly in operable patients.
What may ultimately matter most is carefully selecting operable patients who undergo SBRT.
Aggarwal has encountered certain patients who are fit for surgery but would rather have radiation therapy. “This is an individual decision, and these patients are usually discussed at tumor board and in multidisciplinary discussions to really make sure that they’re making the right decision for themselves,” she explained.
The Pros and Cons of SBRT
SBRT is a nonsurgical approach in which precision high-dose radiation is delivered in just a few fractions — typically, 3, 5, or 8, depending on institutional protocols and tumor characteristics.
SBRT is performed on an outpatient basis, usually over 1-2 weeks, with most patients able to resume usual activities with minimal to no delay. Surgery, on the other hand, requires a hospital stay and takes most people about 2-6 weeks to return to regular activities. SBRT also avoids anesthesia and surgical incisions, both of which come with risks.
The data on SBRT in early-stage NSCLC are mixed. While some studies indicate that SBRT comes with promising survival outcomes, other research has reported worse survival and recurrence rates.
One potential reason for higher recurrence rates with SBRT is the lack of pathologic nodal staging, which only happens after surgery, as well as lower rates of nodal evaluation with endobronchial ultrasound or mediastinoscopy before surgery or SBRT. Without nodal assessments, clinicians may miss a more aggressive histology or more advanced nodal stage, which would go undertreated if patients received SBRT.
Latest Data in Large Cohort
A recent study published in Lung Cancer indicated that, when carefully selected, operable patients with early NSCLC have comparable survival with lobectomy or SBRT.
In the study, Dutch researchers took an in-depth look at survival and recurrence patterns in a retrospective cohort study of 2183 patients with clinical stage I NSCLC treated with minimally invasive lobectomy or SBRT. The study includes one of the largest cohorts to date, with robust data collection on baseline characteristics, comorbidities, tumor size, performance status, and follow-up.
Patients receiving SBRT were typically older (median age, 74 vs 67 years), had higher comorbidity burdens (Charlson index ≥ 5 in 57% of SBRT patients vs 23% of surgical patients), worse performance status, and lower lung function. To adjust for these differences, the researchers used propensity score weighting so the SBRT group’s baseline characteristics were comparable with those in the surgery group.
The surgery cohort had more invasive nodal evaluation: 21% underwent endobronchial ultrasound or mediastinoscopy vs only 12% in the SBRT group. The vast majority in both groups had PET-CT staging, reflecting modern imaging-based workups.
While 5-year local recurrence rates between the two groups were similar (13.1% for SBRT vs 12.1% for surgery), the 5-year regional recurrence rate was significantly higher after SBRT than lobectomy (18.1% vs 14.2%; hazard ratio [HR], 0.74), as was the distant metastasis rate (26.2% vs 20.2%; HR, 0.72).
Mortality at 30 days was higher after surgery than SBRT (1.0% vs 0.2%). And in the unadjusted analysis, 5-year overall survival was significantly better with lobectomy than SBRT (70.2% vs 40.3%).
However, when the analysis only included patients with similar baseline characteristics, overall survival was no longer significantly different in the two groups (HR, 0.89; 95% CI, 0.65-1.20). Lung cancer–specific mortality was also not significantly different between the two treatments (HR, 1.08), but the study was underpowered to detect significant differences in this outcome on the basis of a relatively low number of deaths from NSCLC.
Still, even after comparing similar patients, recurrence-free survival was notably better with surgery (HR, 0.70), due to fewer regional recurrences and distant metastases. Overall, 13% of the surgical cohort had nodal upstaging at pathology, meaning that even in clinically “node-negative” stage I disease, a subset of patients had unsuspected nodal involvement.
Patients receiving SBRT did not have pathologic nodal staging, raising the possibility of occult micrometastases. The authors noted that the proportion of SBRT patients with occult lymph node metastases is likely at least equal to that in the surgery group, but these metastases would go undetected without pathologic assessment.
Missing potential occult micrometastases in the SBRT group likely contributed to higher regional recurrence rates over time. By improving nodal staging, more patients with occult lymph node metastases who would be undertreated with SBRT may be identified before treatment, the authors said.
What Do Experts Say?
So, is SBRT an option for patients with stage I NSCLC?
Opinions vary.
“If you got one shot for a cure, then you want to do the surgery because that’s what results in a cure,” said Raja Flores, MD, chairman of Thoracic Surgery, Mount Sinai Health System, New York City.
Flores noted that the survival rate with surgery is high in this population. “There’s really nothing out there that can compare,” he said.
In his view, surgery “remains the gold standard.” However, “radiation could be considered in nonsurgical candidates,” he said.
The most recent NCCN guidelines align with Flores’ take. The guidelines say that SBRT is indicated for stage IA-IIA (N0) NSCLC in patients who are deemed “medically inoperable, high surgical risk as determined by thoracic surgeon, and those who decline surgery after thoracic surgical consultation.”
Clifford G. Robinson, MD, agreed. “In the United States, we largely treat patients with SBRT who are medically inoperable or high-risk operable and a much smaller proportion who decline surgery,” said Robinson, professor of radiation oncology and chief of SBRT at Washington University in St. Louis, St. Louis. “Many patients who are deemed operable are not offered SBRT.”
Still, for Robinson, determining which patients are best suited for surgery or SBRT remains unclear.
“Retrospective comparisons are fraught with problems because of confounding,” Robinson told this news organization. “That is, the healthier patients get surgery, and the less healthy ones get SBRT. No manner of fancy statistical manipulation can remove that fact.”
In fact, a recent meta-analysis found that the most significant variable predicting whether surgery or SBRT was superior in retrospective studies was whether the author was a surgeon or radiation oncologist.
Robinson noted that multiple randomized trials have attempted to randomize patients with medically operable early-stage NSCLC to surgery or SBRT and failed to accrue, largely due to patients’ “understandable unwillingness to be randomized between operative vs nonoperative interventions when most already prefer one or the other approach.”
Flores highlighted another point of caution about interpreting trial results: Not all early-stage NSCLC behaves similarly. “Some are slow-growing ‘turtles,’ and others are aggressive ‘rabbits’ — and the turtles are usually the ones that have been included in these radiotherapy trials, and that’s the danger,” he said.
While medical operability is the primary factor for deciding the treatment modality for early-stage NSCLC, there are other more subtle factors that can play into the decision.
These include prior surgery or radiotherapy to the chest, prior cancers, and social issues, such as the patient being a primary caregiver for another person and job insecurity, that might make recovery from surgery more challenging. And in rare instances, a patient may be medically fit to undergo surgery, but the cancer is technically challenging to resect due to anatomic issues or prior surgery to the chest, Robinson added.
A Winner?
Results from two ongoing, highly anticipated randomized trials expected in the next several years will hopefully provide additional insights and clarify ongoing uncertainties about the optimal treatment strategies for operable patients with stage I NSCLC.
STABLE-MATES is comparing outcomes after sublobar resection and SBRT in high-risk operable stage I NSCLC, and VALOR is evaluating outcomes after anatomic pulmonary resections and SBRT in patients with stage I NSCLC who have a long life expectancy and are fit enough to tolerate surgery.
But Robinson said his group believes that trying to decide on a winner is a “fool’s errand” and is instead running a pragmatic study across multiple academic and community centers around the United States and Canada where patients choose therapy based on their personal preferences and guidance from their physicians. The researchers will carefully track baseline comorbidity and frailty and assess serial quality-of-life changes over time.
“The goal is to create a calculator that a given patient might use in the future to determine what patients like them would have received, complete with expected outcomes and side effects,” Robinson said.
Robinson cautioned, however, that it “seems unlikely, given the existing literature, that one of the treatments will be truly ‘superior’ to the other one and lead to the ‘losing’ treatment fading away since both are excellent options with pros and cons.”
Aggarwal, Robinson, and Flores had no relevant disclosures.
A version of this article first appeared on Medscape.com.
For years, the default definitive treatment for patients with early-stage I non–small cell lung cancer (NSCLC) has been surgical resection, typically minimally invasive lobectomy with systematic lymph node dissection.
Guidelines from the National Comprehensive Cancer Network (NCCN), the American Society of Clinical Oncology, and the European Society for Medical Oncology all list surgery (in particular, lobectomy) as the primary local therapy for fit, operable patients with stage I NSCLC.
More recently, however, stereotactic body radiotherapy (SBRT), also called stereotactic ablative radiotherapy, has emerged as a definitive treatment option for stage I NSCLC, especially for older, less fit patients who are unsuitable or deemed high-risk for surgery.
“We see patients in our practice who cannot undergo surgery or who may not have adequate lung function to be able to tolerate surgery, and for these patients who are medically inoperable or surgically unresectable, radiation therapy may be a reasonable option,” Charu Aggarwal, MD, MPH, professor and lung cancer specialist, University of Pennsylvania, Philadelphia, told this news organization.
Given some encouraging data suggesting that SBRT could provide similar survival outcomes and be an alternative to surgery for operable disease, SBRT is also increasingly being considered in these early-stage patients. However, other evidence indicates that SBRT may be associated with higher rates of regional and distant recurrences and worse long-term survival, particularly in operable patients.
What may ultimately matter most is carefully selecting operable patients who undergo SBRT.
Aggarwal has encountered certain patients who are fit for surgery but would rather have radiation therapy. “This is an individual decision, and these patients are usually discussed at tumor board and in multidisciplinary discussions to really make sure that they’re making the right decision for themselves,” she explained.
The Pros and Cons of SBRT
SBRT is a nonsurgical approach in which precision high-dose radiation is delivered in just a few fractions — typically, 3, 5, or 8, depending on institutional protocols and tumor characteristics.
SBRT is performed on an outpatient basis, usually over 1-2 weeks, with most patients able to resume usual activities with minimal to no delay. Surgery, on the other hand, requires a hospital stay and takes most people about 2-6 weeks to return to regular activities. SBRT also avoids anesthesia and surgical incisions, both of which come with risks.
The data on SBRT in early-stage NSCLC are mixed. While some studies indicate that SBRT comes with promising survival outcomes, other research has reported worse survival and recurrence rates.
One potential reason for higher recurrence rates with SBRT is the lack of pathologic nodal staging, which only happens after surgery, as well as lower rates of nodal evaluation with endobronchial ultrasound or mediastinoscopy before surgery or SBRT. Without nodal assessments, clinicians may miss a more aggressive histology or more advanced nodal stage, which would go undertreated if patients received SBRT.
Latest Data in Large Cohort
A recent study published in Lung Cancer indicated that, when carefully selected, operable patients with early NSCLC have comparable survival with lobectomy or SBRT.
In the study, Dutch researchers took an in-depth look at survival and recurrence patterns in a retrospective cohort study of 2183 patients with clinical stage I NSCLC treated with minimally invasive lobectomy or SBRT. The study includes one of the largest cohorts to date, with robust data collection on baseline characteristics, comorbidities, tumor size, performance status, and follow-up.
Patients receiving SBRT were typically older (median age, 74 vs 67 years), had higher comorbidity burdens (Charlson index ≥ 5 in 57% of SBRT patients vs 23% of surgical patients), worse performance status, and lower lung function. To adjust for these differences, the researchers used propensity score weighting so the SBRT group’s baseline characteristics were comparable with those in the surgery group.
The surgery cohort had more invasive nodal evaluation: 21% underwent endobronchial ultrasound or mediastinoscopy vs only 12% in the SBRT group. The vast majority in both groups had PET-CT staging, reflecting modern imaging-based workups.
While 5-year local recurrence rates between the two groups were similar (13.1% for SBRT vs 12.1% for surgery), the 5-year regional recurrence rate was significantly higher after SBRT than lobectomy (18.1% vs 14.2%; hazard ratio [HR], 0.74), as was the distant metastasis rate (26.2% vs 20.2%; HR, 0.72).
Mortality at 30 days was higher after surgery than SBRT (1.0% vs 0.2%). And in the unadjusted analysis, 5-year overall survival was significantly better with lobectomy than SBRT (70.2% vs 40.3%).
However, when the analysis only included patients with similar baseline characteristics, overall survival was no longer significantly different in the two groups (HR, 0.89; 95% CI, 0.65-1.20). Lung cancer–specific mortality was also not significantly different between the two treatments (HR, 1.08), but the study was underpowered to detect significant differences in this outcome on the basis of a relatively low number of deaths from NSCLC.
Still, even after comparing similar patients, recurrence-free survival was notably better with surgery (HR, 0.70), due to fewer regional recurrences and distant metastases. Overall, 13% of the surgical cohort had nodal upstaging at pathology, meaning that even in clinically “node-negative” stage I disease, a subset of patients had unsuspected nodal involvement.
Patients receiving SBRT did not have pathologic nodal staging, raising the possibility of occult micrometastases. The authors noted that the proportion of SBRT patients with occult lymph node metastases is likely at least equal to that in the surgery group, but these metastases would go undetected without pathologic assessment.
Missing potential occult micrometastases in the SBRT group likely contributed to higher regional recurrence rates over time. By improving nodal staging, more patients with occult lymph node metastases who would be undertreated with SBRT may be identified before treatment, the authors said.
What Do Experts Say?
So, is SBRT an option for patients with stage I NSCLC?
Opinions vary.
“If you got one shot for a cure, then you want to do the surgery because that’s what results in a cure,” said Raja Flores, MD, chairman of Thoracic Surgery, Mount Sinai Health System, New York City.
Flores noted that the survival rate with surgery is high in this population. “There’s really nothing out there that can compare,” he said.
In his view, surgery “remains the gold standard.” However, “radiation could be considered in nonsurgical candidates,” he said.
The most recent NCCN guidelines align with Flores’ take. The guidelines say that SBRT is indicated for stage IA-IIA (N0) NSCLC in patients who are deemed “medically inoperable, high surgical risk as determined by thoracic surgeon, and those who decline surgery after thoracic surgical consultation.”
Clifford G. Robinson, MD, agreed. “In the United States, we largely treat patients with SBRT who are medically inoperable or high-risk operable and a much smaller proportion who decline surgery,” said Robinson, professor of radiation oncology and chief of SBRT at Washington University in St. Louis, St. Louis. “Many patients who are deemed operable are not offered SBRT.”
Still, for Robinson, determining which patients are best suited for surgery or SBRT remains unclear.
“Retrospective comparisons are fraught with problems because of confounding,” Robinson told this news organization. “That is, the healthier patients get surgery, and the less healthy ones get SBRT. No manner of fancy statistical manipulation can remove that fact.”
In fact, a recent meta-analysis found that the most significant variable predicting whether surgery or SBRT was superior in retrospective studies was whether the author was a surgeon or radiation oncologist.
Robinson noted that multiple randomized trials have attempted to randomize patients with medically operable early-stage NSCLC to surgery or SBRT and failed to accrue, largely due to patients’ “understandable unwillingness to be randomized between operative vs nonoperative interventions when most already prefer one or the other approach.”
Flores highlighted another point of caution about interpreting trial results: Not all early-stage NSCLC behaves similarly. “Some are slow-growing ‘turtles,’ and others are aggressive ‘rabbits’ — and the turtles are usually the ones that have been included in these radiotherapy trials, and that’s the danger,” he said.
While medical operability is the primary factor for deciding the treatment modality for early-stage NSCLC, there are other more subtle factors that can play into the decision.
These include prior surgery or radiotherapy to the chest, prior cancers, and social issues, such as the patient being a primary caregiver for another person and job insecurity, that might make recovery from surgery more challenging. And in rare instances, a patient may be medically fit to undergo surgery, but the cancer is technically challenging to resect due to anatomic issues or prior surgery to the chest, Robinson added.
A Winner?
Results from two ongoing, highly anticipated randomized trials expected in the next several years will hopefully provide additional insights and clarify ongoing uncertainties about the optimal treatment strategies for operable patients with stage I NSCLC.
STABLE-MATES is comparing outcomes after sublobar resection and SBRT in high-risk operable stage I NSCLC, and VALOR is evaluating outcomes after anatomic pulmonary resections and SBRT in patients with stage I NSCLC who have a long life expectancy and are fit enough to tolerate surgery.
But Robinson said his group believes that trying to decide on a winner is a “fool’s errand” and is instead running a pragmatic study across multiple academic and community centers around the United States and Canada where patients choose therapy based on their personal preferences and guidance from their physicians. The researchers will carefully track baseline comorbidity and frailty and assess serial quality-of-life changes over time.
“The goal is to create a calculator that a given patient might use in the future to determine what patients like them would have received, complete with expected outcomes and side effects,” Robinson said.
Robinson cautioned, however, that it “seems unlikely, given the existing literature, that one of the treatments will be truly ‘superior’ to the other one and lead to the ‘losing’ treatment fading away since both are excellent options with pros and cons.”
Aggarwal, Robinson, and Flores had no relevant disclosures.
A version of this article first appeared on Medscape.com.
For years, the default definitive treatment for patients with early-stage I non–small cell lung cancer (NSCLC) has been surgical resection, typically minimally invasive lobectomy with systematic lymph node dissection.
Guidelines from the National Comprehensive Cancer Network (NCCN), the American Society of Clinical Oncology, and the European Society for Medical Oncology all list surgery (in particular, lobectomy) as the primary local therapy for fit, operable patients with stage I NSCLC.
More recently, however, stereotactic body radiotherapy (SBRT), also called stereotactic ablative radiotherapy, has emerged as a definitive treatment option for stage I NSCLC, especially for older, less fit patients who are unsuitable or deemed high-risk for surgery.
“We see patients in our practice who cannot undergo surgery or who may not have adequate lung function to be able to tolerate surgery, and for these patients who are medically inoperable or surgically unresectable, radiation therapy may be a reasonable option,” Charu Aggarwal, MD, MPH, professor and lung cancer specialist, University of Pennsylvania, Philadelphia, told this news organization.
Given some encouraging data suggesting that SBRT could provide similar survival outcomes and be an alternative to surgery for operable disease, SBRT is also increasingly being considered in these early-stage patients. However, other evidence indicates that SBRT may be associated with higher rates of regional and distant recurrences and worse long-term survival, particularly in operable patients.
What may ultimately matter most is carefully selecting operable patients who undergo SBRT.
Aggarwal has encountered certain patients who are fit for surgery but would rather have radiation therapy. “This is an individual decision, and these patients are usually discussed at tumor board and in multidisciplinary discussions to really make sure that they’re making the right decision for themselves,” she explained.
The Pros and Cons of SBRT
SBRT is a nonsurgical approach in which precision high-dose radiation is delivered in just a few fractions — typically, 3, 5, or 8, depending on institutional protocols and tumor characteristics.
SBRT is performed on an outpatient basis, usually over 1-2 weeks, with most patients able to resume usual activities with minimal to no delay. Surgery, on the other hand, requires a hospital stay and takes most people about 2-6 weeks to return to regular activities. SBRT also avoids anesthesia and surgical incisions, both of which come with risks.
The data on SBRT in early-stage NSCLC are mixed. While some studies indicate that SBRT comes with promising survival outcomes, other research has reported worse survival and recurrence rates.
One potential reason for higher recurrence rates with SBRT is the lack of pathologic nodal staging, which only happens after surgery, as well as lower rates of nodal evaluation with endobronchial ultrasound or mediastinoscopy before surgery or SBRT. Without nodal assessments, clinicians may miss a more aggressive histology or more advanced nodal stage, which would go undertreated if patients received SBRT.
Latest Data in Large Cohort
A recent study published in Lung Cancer indicated that, when carefully selected, operable patients with early NSCLC have comparable survival with lobectomy or SBRT.
In the study, Dutch researchers took an in-depth look at survival and recurrence patterns in a retrospective cohort study of 2183 patients with clinical stage I NSCLC treated with minimally invasive lobectomy or SBRT. The study includes one of the largest cohorts to date, with robust data collection on baseline characteristics, comorbidities, tumor size, performance status, and follow-up.
Patients receiving SBRT were typically older (median age, 74 vs 67 years), had higher comorbidity burdens (Charlson index ≥ 5 in 57% of SBRT patients vs 23% of surgical patients), worse performance status, and lower lung function. To adjust for these differences, the researchers used propensity score weighting so the SBRT group’s baseline characteristics were comparable with those in the surgery group.
The surgery cohort had more invasive nodal evaluation: 21% underwent endobronchial ultrasound or mediastinoscopy vs only 12% in the SBRT group. The vast majority in both groups had PET-CT staging, reflecting modern imaging-based workups.
While 5-year local recurrence rates between the two groups were similar (13.1% for SBRT vs 12.1% for surgery), the 5-year regional recurrence rate was significantly higher after SBRT than lobectomy (18.1% vs 14.2%; hazard ratio [HR], 0.74), as was the distant metastasis rate (26.2% vs 20.2%; HR, 0.72).
Mortality at 30 days was higher after surgery than SBRT (1.0% vs 0.2%). And in the unadjusted analysis, 5-year overall survival was significantly better with lobectomy than SBRT (70.2% vs 40.3%).
However, when the analysis only included patients with similar baseline characteristics, overall survival was no longer significantly different in the two groups (HR, 0.89; 95% CI, 0.65-1.20). Lung cancer–specific mortality was also not significantly different between the two treatments (HR, 1.08), but the study was underpowered to detect significant differences in this outcome on the basis of a relatively low number of deaths from NSCLC.
Still, even after comparing similar patients, recurrence-free survival was notably better with surgery (HR, 0.70), due to fewer regional recurrences and distant metastases. Overall, 13% of the surgical cohort had nodal upstaging at pathology, meaning that even in clinically “node-negative” stage I disease, a subset of patients had unsuspected nodal involvement.
Patients receiving SBRT did not have pathologic nodal staging, raising the possibility of occult micrometastases. The authors noted that the proportion of SBRT patients with occult lymph node metastases is likely at least equal to that in the surgery group, but these metastases would go undetected without pathologic assessment.
Missing potential occult micrometastases in the SBRT group likely contributed to higher regional recurrence rates over time. By improving nodal staging, more patients with occult lymph node metastases who would be undertreated with SBRT may be identified before treatment, the authors said.
What Do Experts Say?
So, is SBRT an option for patients with stage I NSCLC?
Opinions vary.
“If you got one shot for a cure, then you want to do the surgery because that’s what results in a cure,” said Raja Flores, MD, chairman of Thoracic Surgery, Mount Sinai Health System, New York City.
Flores noted that the survival rate with surgery is high in this population. “There’s really nothing out there that can compare,” he said.
In his view, surgery “remains the gold standard.” However, “radiation could be considered in nonsurgical candidates,” he said.
The most recent NCCN guidelines align with Flores’ take. The guidelines say that SBRT is indicated for stage IA-IIA (N0) NSCLC in patients who are deemed “medically inoperable, high surgical risk as determined by thoracic surgeon, and those who decline surgery after thoracic surgical consultation.”
Clifford G. Robinson, MD, agreed. “In the United States, we largely treat patients with SBRT who are medically inoperable or high-risk operable and a much smaller proportion who decline surgery,” said Robinson, professor of radiation oncology and chief of SBRT at Washington University in St. Louis, St. Louis. “Many patients who are deemed operable are not offered SBRT.”
Still, for Robinson, determining which patients are best suited for surgery or SBRT remains unclear.
“Retrospective comparisons are fraught with problems because of confounding,” Robinson told this news organization. “That is, the healthier patients get surgery, and the less healthy ones get SBRT. No manner of fancy statistical manipulation can remove that fact.”
In fact, a recent meta-analysis found that the most significant variable predicting whether surgery or SBRT was superior in retrospective studies was whether the author was a surgeon or radiation oncologist.
Robinson noted that multiple randomized trials have attempted to randomize patients with medically operable early-stage NSCLC to surgery or SBRT and failed to accrue, largely due to patients’ “understandable unwillingness to be randomized between operative vs nonoperative interventions when most already prefer one or the other approach.”
Flores highlighted another point of caution about interpreting trial results: Not all early-stage NSCLC behaves similarly. “Some are slow-growing ‘turtles,’ and others are aggressive ‘rabbits’ — and the turtles are usually the ones that have been included in these radiotherapy trials, and that’s the danger,” he said.
While medical operability is the primary factor for deciding the treatment modality for early-stage NSCLC, there are other more subtle factors that can play into the decision.
These include prior surgery or radiotherapy to the chest, prior cancers, and social issues, such as the patient being a primary caregiver for another person and job insecurity, that might make recovery from surgery more challenging. And in rare instances, a patient may be medically fit to undergo surgery, but the cancer is technically challenging to resect due to anatomic issues or prior surgery to the chest, Robinson added.
A Winner?
Results from two ongoing, highly anticipated randomized trials expected in the next several years will hopefully provide additional insights and clarify ongoing uncertainties about the optimal treatment strategies for operable patients with stage I NSCLC.
STABLE-MATES is comparing outcomes after sublobar resection and SBRT in high-risk operable stage I NSCLC, and VALOR is evaluating outcomes after anatomic pulmonary resections and SBRT in patients with stage I NSCLC who have a long life expectancy and are fit enough to tolerate surgery.
But Robinson said his group believes that trying to decide on a winner is a “fool’s errand” and is instead running a pragmatic study across multiple academic and community centers around the United States and Canada where patients choose therapy based on their personal preferences and guidance from their physicians. The researchers will carefully track baseline comorbidity and frailty and assess serial quality-of-life changes over time.
“The goal is to create a calculator that a given patient might use in the future to determine what patients like them would have received, complete with expected outcomes and side effects,” Robinson said.
Robinson cautioned, however, that it “seems unlikely, given the existing literature, that one of the treatments will be truly ‘superior’ to the other one and lead to the ‘losing’ treatment fading away since both are excellent options with pros and cons.”
Aggarwal, Robinson, and Flores had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FDA OKs Guselkumab for Crohn’s Disease
The approval marks the fourth indication for guselkumab, which was approved for moderate to severe plaque psoriasis in 2017, active psoriatic arthritis in 2020, and moderately to severely active ulcerative colitis in 2024.
Guselkumab is the first and only interleukin-23 (IL-23) inhibitor that offers both subcutaneous (SC) and intravenous (IV) induction options for CD, the company said in a news release.
“Despite the progress in the management of Crohn’s disease, many patients experience debilitating symptoms and are in need of new treatment options,” Remo Panaccione, MD, director of the Inflammatory Bowel Disease Unit at the University of Calgary, Calgary, Alberta, Canada, said in the release.
“The approval of Tremfya offers an IL-23 inhibitor that has shown robust rates of endoscopic remission with both subcutaneous and intravenous induction regimens. Importantly, the fully subcutaneous regimen offers choice and flexibility for patients and providers not available before,” said Panaccione.
The FDA nod in CD was based on positive results from three phase 3 trials evaluating guselkumab in more than 1300 patients with moderately to severely active CD who failed or were intolerant to corticosteroids, immunomodulators, or biologics.
The GRAVITI trial showed that guselkumab as SC induction and maintenance therapy was superior to placebo in clinical remission as well as endoscopic response and remission and deep remission.
Results from GALAXI 2 and GALAXI 3 showed that guselkumab was superior to ustekinumab (Stelara) on all pooled endoscopic endpoints.
Guselkumab is the only IL-23 inhibitor to demonstrate “clinical remission and endoscopic response, both at 1 year, with a fully subcutaneous induction regimen,” the company said.
The recommended SC induction dose of guselkumab is 400 mg (given as two consecutive injections of 200 mg each, dispensed in one induction pack) at weeks 0, 4 and 8. The drug is also available in a 200 mg prefilled syringe. For the IV induction option, 200 mg IV infusions are administered at weeks 0, 4, and 8.
The recommended maintenance dosage is 100 mg administered by SC injection at week 16, and every 8 weeks thereafter, or 200 mg administered by SC injection at week 12, and every 4 weeks thereafter.
Use of the lowest effective recommended dosage to maintain therapeutic response is recommended.
Full prescribing information and medication guide are available online.
A version of this article first appeared on Medscape.com.
The approval marks the fourth indication for guselkumab, which was approved for moderate to severe plaque psoriasis in 2017, active psoriatic arthritis in 2020, and moderately to severely active ulcerative colitis in 2024.
Guselkumab is the first and only interleukin-23 (IL-23) inhibitor that offers both subcutaneous (SC) and intravenous (IV) induction options for CD, the company said in a news release.
“Despite the progress in the management of Crohn’s disease, many patients experience debilitating symptoms and are in need of new treatment options,” Remo Panaccione, MD, director of the Inflammatory Bowel Disease Unit at the University of Calgary, Calgary, Alberta, Canada, said in the release.
“The approval of Tremfya offers an IL-23 inhibitor that has shown robust rates of endoscopic remission with both subcutaneous and intravenous induction regimens. Importantly, the fully subcutaneous regimen offers choice and flexibility for patients and providers not available before,” said Panaccione.
The FDA nod in CD was based on positive results from three phase 3 trials evaluating guselkumab in more than 1300 patients with moderately to severely active CD who failed or were intolerant to corticosteroids, immunomodulators, or biologics.
The GRAVITI trial showed that guselkumab as SC induction and maintenance therapy was superior to placebo in clinical remission as well as endoscopic response and remission and deep remission.
Results from GALAXI 2 and GALAXI 3 showed that guselkumab was superior to ustekinumab (Stelara) on all pooled endoscopic endpoints.
Guselkumab is the only IL-23 inhibitor to demonstrate “clinical remission and endoscopic response, both at 1 year, with a fully subcutaneous induction regimen,” the company said.
The recommended SC induction dose of guselkumab is 400 mg (given as two consecutive injections of 200 mg each, dispensed in one induction pack) at weeks 0, 4 and 8. The drug is also available in a 200 mg prefilled syringe. For the IV induction option, 200 mg IV infusions are administered at weeks 0, 4, and 8.
The recommended maintenance dosage is 100 mg administered by SC injection at week 16, and every 8 weeks thereafter, or 200 mg administered by SC injection at week 12, and every 4 weeks thereafter.
Use of the lowest effective recommended dosage to maintain therapeutic response is recommended.
Full prescribing information and medication guide are available online.
A version of this article first appeared on Medscape.com.
The approval marks the fourth indication for guselkumab, which was approved for moderate to severe plaque psoriasis in 2017, active psoriatic arthritis in 2020, and moderately to severely active ulcerative colitis in 2024.
Guselkumab is the first and only interleukin-23 (IL-23) inhibitor that offers both subcutaneous (SC) and intravenous (IV) induction options for CD, the company said in a news release.
“Despite the progress in the management of Crohn’s disease, many patients experience debilitating symptoms and are in need of new treatment options,” Remo Panaccione, MD, director of the Inflammatory Bowel Disease Unit at the University of Calgary, Calgary, Alberta, Canada, said in the release.
“The approval of Tremfya offers an IL-23 inhibitor that has shown robust rates of endoscopic remission with both subcutaneous and intravenous induction regimens. Importantly, the fully subcutaneous regimen offers choice and flexibility for patients and providers not available before,” said Panaccione.
The FDA nod in CD was based on positive results from three phase 3 trials evaluating guselkumab in more than 1300 patients with moderately to severely active CD who failed or were intolerant to corticosteroids, immunomodulators, or biologics.
The GRAVITI trial showed that guselkumab as SC induction and maintenance therapy was superior to placebo in clinical remission as well as endoscopic response and remission and deep remission.
Results from GALAXI 2 and GALAXI 3 showed that guselkumab was superior to ustekinumab (Stelara) on all pooled endoscopic endpoints.
Guselkumab is the only IL-23 inhibitor to demonstrate “clinical remission and endoscopic response, both at 1 year, with a fully subcutaneous induction regimen,” the company said.
The recommended SC induction dose of guselkumab is 400 mg (given as two consecutive injections of 200 mg each, dispensed in one induction pack) at weeks 0, 4 and 8. The drug is also available in a 200 mg prefilled syringe. For the IV induction option, 200 mg IV infusions are administered at weeks 0, 4, and 8.
The recommended maintenance dosage is 100 mg administered by SC injection at week 16, and every 8 weeks thereafter, or 200 mg administered by SC injection at week 12, and every 4 weeks thereafter.
Use of the lowest effective recommended dosage to maintain therapeutic response is recommended.
Full prescribing information and medication guide are available online.
A version of this article first appeared on Medscape.com.
WATS-3D Biopsy Increases Detection of Barrett’s Esophagus in GERD
, new research showed.
Compared with forceps biopsies (FB) alone, the addition of WATS-3D led to confirmation of BE in an additional one fifth of patients, roughly doubled dysplasia diagnoses, and influenced clinical management in the majority of patients.
“The big take-home point here is that the use of WATS-3D brushing along with conventional biopsies increases the likelihood that intestinal metaplasia will be identified,” first author Nicholas Shaheen, MD, MPH, AGAF, with the Center for Esophageal Diseases and Swallowing, University of North Carolina School of Medicine at Chapel Hill, North Carolina, told GI & Hepatology News.
“Almost 20% of patients who harbor BE were only identified by WATS-3D and might have otherwise gone undiagnosed had only forceps biopsies been performed,” Shaheen said.
The study was published in The American Journal of Gastroenterology.
Beyond Traditional Biopsies
BE develops as a complication of chronic GERD and is the chief precursor to esophageal adenocarcinoma. Early detection of BE and dysplasia is crucial to enable timely intervention.
The current gold standard for BE screening involves upper endoscopy with FB following the Seattle protocol, which consists of four-quadrant biopsies from every 1-2 cm of areas of columnar-lined epithelium (CLE) to confirm the presence of intestinal metaplasia. However, this protocol is prone to sampling errors and high false-negative rates, leading to repeat endoscopy, the study team pointed out.
WATS-3D (CDx Diagnostics) is a complementary technique designed to improve diagnostic yield by using brush biopsy to sample more tissue than routine biopsies.
WATS-3D has been shown to increase detection of dysplasia in patients with BE undergoing surveillance for BE, but less is known about the value of WATS-3D for BE screening in a community-based cohort of patients with GERD.
To investigate, Shaheen and colleagues studied 23,933 consecutive patients enrolled in a prospective observational registry assessing the utility of WATS-3D in the screening of symptomatic GERD patients for BE.
Patients had both WATS-3D and FB in the same endoscopic session. No patient had a history of BE, intestinal metaplasia or dysplasia in esophageal mucosa, or esophageal surgery, endoscopic ablation or endoscopic mucosal resection prior to enrollment.
Overall, 6829 patients (29%) met endoscopic criteria for BE (≥ 1 cm esophageal CLE with accompanying biopsies showing intestinal metaplasia).
Of these, 2878 (42%) had intestinal metaplasia identified by either FB or WATS-3D, but 19.3% had their BE diagnosis confirmed solely on the basis of WATS-3D findings.
Among patients who fulfilled the endoscopic criteria for BE, the adjunctive yield of WATS-3D was 76.5% and the absolute yield was 18.1%.
Of the 240 (1.0%) patients with dysplasia, 107 (45%) were found solely by WATS-3D.
‘Clinically Valuable Adjunct’
Among patients with positive WATS-3D but negative FB results, clinical management changed in 90.7% of cases, mostly involving initiation or modification of surveillance and proton pump inhibitor therapy.
These results suggest that WATS-3D is a “clinically valuable adjunct” to FB for the diagnosis of BE when used as a screening tool in symptomatic GERD patients and particularly in patients with endoscopic evidence of > 1 cm esophageal columnar-lined epithelium, the study team wrote.
Adjunctive use of WATS-3D when BE is suspected “may save endoscopies and lead to quicker, more accurate diagnoses,” they added.
The investigators said a limitation of the study is the lack of central pathology review, potentially leading to diagnostic variability. They also noted that over half of the detected dysplasia cases were crypt dysplasia or indefinite for dysplasia, raising concerns about clinical significance.
Reached for comment, Philip O. Katz, MD, AGAF, professor of medicine and director of the GI Function Laboratories, Weill Cornell Medicine in New York, said he’s been using WATS for more than a decade as an adjunct to standard biopsy in patients undergoing screening and surveillance for BE and finds it clinically helpful in managing his patients.
This new study provides “further information that WATS added to biopsy that has been traditionally done with the Seattle protocol increases the yield of intestinal metaplasia and likely dysplasia in patients being screened for Barrett’s,” Katz, who wasn’t involved in the study, told GI & Hepatology News.
Funding for the study was provided by CDx Diagnostics. Shaheen and several coauthors disclosed relationships with the company. Katz disclosed relationships (consultant/advisor) for Phathom Pharmaceuticals and Sebella.
A version of this article appeared on Medscape.com.
, new research showed.
Compared with forceps biopsies (FB) alone, the addition of WATS-3D led to confirmation of BE in an additional one fifth of patients, roughly doubled dysplasia diagnoses, and influenced clinical management in the majority of patients.
“The big take-home point here is that the use of WATS-3D brushing along with conventional biopsies increases the likelihood that intestinal metaplasia will be identified,” first author Nicholas Shaheen, MD, MPH, AGAF, with the Center for Esophageal Diseases and Swallowing, University of North Carolina School of Medicine at Chapel Hill, North Carolina, told GI & Hepatology News.
“Almost 20% of patients who harbor BE were only identified by WATS-3D and might have otherwise gone undiagnosed had only forceps biopsies been performed,” Shaheen said.
The study was published in The American Journal of Gastroenterology.
Beyond Traditional Biopsies
BE develops as a complication of chronic GERD and is the chief precursor to esophageal adenocarcinoma. Early detection of BE and dysplasia is crucial to enable timely intervention.
The current gold standard for BE screening involves upper endoscopy with FB following the Seattle protocol, which consists of four-quadrant biopsies from every 1-2 cm of areas of columnar-lined epithelium (CLE) to confirm the presence of intestinal metaplasia. However, this protocol is prone to sampling errors and high false-negative rates, leading to repeat endoscopy, the study team pointed out.
WATS-3D (CDx Diagnostics) is a complementary technique designed to improve diagnostic yield by using brush biopsy to sample more tissue than routine biopsies.
WATS-3D has been shown to increase detection of dysplasia in patients with BE undergoing surveillance for BE, but less is known about the value of WATS-3D for BE screening in a community-based cohort of patients with GERD.
To investigate, Shaheen and colleagues studied 23,933 consecutive patients enrolled in a prospective observational registry assessing the utility of WATS-3D in the screening of symptomatic GERD patients for BE.
Patients had both WATS-3D and FB in the same endoscopic session. No patient had a history of BE, intestinal metaplasia or dysplasia in esophageal mucosa, or esophageal surgery, endoscopic ablation or endoscopic mucosal resection prior to enrollment.
Overall, 6829 patients (29%) met endoscopic criteria for BE (≥ 1 cm esophageal CLE with accompanying biopsies showing intestinal metaplasia).
Of these, 2878 (42%) had intestinal metaplasia identified by either FB or WATS-3D, but 19.3% had their BE diagnosis confirmed solely on the basis of WATS-3D findings.
Among patients who fulfilled the endoscopic criteria for BE, the adjunctive yield of WATS-3D was 76.5% and the absolute yield was 18.1%.
Of the 240 (1.0%) patients with dysplasia, 107 (45%) were found solely by WATS-3D.
‘Clinically Valuable Adjunct’
Among patients with positive WATS-3D but negative FB results, clinical management changed in 90.7% of cases, mostly involving initiation or modification of surveillance and proton pump inhibitor therapy.
These results suggest that WATS-3D is a “clinically valuable adjunct” to FB for the diagnosis of BE when used as a screening tool in symptomatic GERD patients and particularly in patients with endoscopic evidence of > 1 cm esophageal columnar-lined epithelium, the study team wrote.
Adjunctive use of WATS-3D when BE is suspected “may save endoscopies and lead to quicker, more accurate diagnoses,” they added.
The investigators said a limitation of the study is the lack of central pathology review, potentially leading to diagnostic variability. They also noted that over half of the detected dysplasia cases were crypt dysplasia or indefinite for dysplasia, raising concerns about clinical significance.
Reached for comment, Philip O. Katz, MD, AGAF, professor of medicine and director of the GI Function Laboratories, Weill Cornell Medicine in New York, said he’s been using WATS for more than a decade as an adjunct to standard biopsy in patients undergoing screening and surveillance for BE and finds it clinically helpful in managing his patients.
This new study provides “further information that WATS added to biopsy that has been traditionally done with the Seattle protocol increases the yield of intestinal metaplasia and likely dysplasia in patients being screened for Barrett’s,” Katz, who wasn’t involved in the study, told GI & Hepatology News.
Funding for the study was provided by CDx Diagnostics. Shaheen and several coauthors disclosed relationships with the company. Katz disclosed relationships (consultant/advisor) for Phathom Pharmaceuticals and Sebella.
A version of this article appeared on Medscape.com.
, new research showed.
Compared with forceps biopsies (FB) alone, the addition of WATS-3D led to confirmation of BE in an additional one fifth of patients, roughly doubled dysplasia diagnoses, and influenced clinical management in the majority of patients.
“The big take-home point here is that the use of WATS-3D brushing along with conventional biopsies increases the likelihood that intestinal metaplasia will be identified,” first author Nicholas Shaheen, MD, MPH, AGAF, with the Center for Esophageal Diseases and Swallowing, University of North Carolina School of Medicine at Chapel Hill, North Carolina, told GI & Hepatology News.
“Almost 20% of patients who harbor BE were only identified by WATS-3D and might have otherwise gone undiagnosed had only forceps biopsies been performed,” Shaheen said.
The study was published in The American Journal of Gastroenterology.
Beyond Traditional Biopsies
BE develops as a complication of chronic GERD and is the chief precursor to esophageal adenocarcinoma. Early detection of BE and dysplasia is crucial to enable timely intervention.
The current gold standard for BE screening involves upper endoscopy with FB following the Seattle protocol, which consists of four-quadrant biopsies from every 1-2 cm of areas of columnar-lined epithelium (CLE) to confirm the presence of intestinal metaplasia. However, this protocol is prone to sampling errors and high false-negative rates, leading to repeat endoscopy, the study team pointed out.
WATS-3D (CDx Diagnostics) is a complementary technique designed to improve diagnostic yield by using brush biopsy to sample more tissue than routine biopsies.
WATS-3D has been shown to increase detection of dysplasia in patients with BE undergoing surveillance for BE, but less is known about the value of WATS-3D for BE screening in a community-based cohort of patients with GERD.
To investigate, Shaheen and colleagues studied 23,933 consecutive patients enrolled in a prospective observational registry assessing the utility of WATS-3D in the screening of symptomatic GERD patients for BE.
Patients had both WATS-3D and FB in the same endoscopic session. No patient had a history of BE, intestinal metaplasia or dysplasia in esophageal mucosa, or esophageal surgery, endoscopic ablation or endoscopic mucosal resection prior to enrollment.
Overall, 6829 patients (29%) met endoscopic criteria for BE (≥ 1 cm esophageal CLE with accompanying biopsies showing intestinal metaplasia).
Of these, 2878 (42%) had intestinal metaplasia identified by either FB or WATS-3D, but 19.3% had their BE diagnosis confirmed solely on the basis of WATS-3D findings.
Among patients who fulfilled the endoscopic criteria for BE, the adjunctive yield of WATS-3D was 76.5% and the absolute yield was 18.1%.
Of the 240 (1.0%) patients with dysplasia, 107 (45%) were found solely by WATS-3D.
‘Clinically Valuable Adjunct’
Among patients with positive WATS-3D but negative FB results, clinical management changed in 90.7% of cases, mostly involving initiation or modification of surveillance and proton pump inhibitor therapy.
These results suggest that WATS-3D is a “clinically valuable adjunct” to FB for the diagnosis of BE when used as a screening tool in symptomatic GERD patients and particularly in patients with endoscopic evidence of > 1 cm esophageal columnar-lined epithelium, the study team wrote.
Adjunctive use of WATS-3D when BE is suspected “may save endoscopies and lead to quicker, more accurate diagnoses,” they added.
The investigators said a limitation of the study is the lack of central pathology review, potentially leading to diagnostic variability. They also noted that over half of the detected dysplasia cases were crypt dysplasia or indefinite for dysplasia, raising concerns about clinical significance.
Reached for comment, Philip O. Katz, MD, AGAF, professor of medicine and director of the GI Function Laboratories, Weill Cornell Medicine in New York, said he’s been using WATS for more than a decade as an adjunct to standard biopsy in patients undergoing screening and surveillance for BE and finds it clinically helpful in managing his patients.
This new study provides “further information that WATS added to biopsy that has been traditionally done with the Seattle protocol increases the yield of intestinal metaplasia and likely dysplasia in patients being screened for Barrett’s,” Katz, who wasn’t involved in the study, told GI & Hepatology News.
Funding for the study was provided by CDx Diagnostics. Shaheen and several coauthors disclosed relationships with the company. Katz disclosed relationships (consultant/advisor) for Phathom Pharmaceuticals and Sebella.
A version of this article appeared on Medscape.com.
Intensive Nutrition Therapy Improves Outcomes in Alcohol-Related ACLF
In a randomized controlled trial, compared with standard care, dietitian-supported, intensive nutritional therapy improved survival, reduced frailty, and lowered hospitalization rates in men with alcohol-related ACLF.
The study, performed by a team from the Postgraduate Institute of Medical Education and Research, Chandigarh, India, was published in Clinical Gastroenterology and Hepatology.
ACLF related to alcohol use is associated with poor outcomes due to poor nutritional intake and frailty. Frail patients with ACLF face higher morbidity, mortality, and hospitalization rates than their nonfrail counterparts. However, research on the role of structured nutritional interventions in improving these outcomes is limited.
Patal Giri, MBBS, MD, and colleagues enrolled 70 men with alcohol-related ACLF and frailty (liver frailty index [LFI] > 4.5) in a single-center, open-label study. Half were randomly allocated to an intervention group receiving outpatient intensive nutrition therapy (OINT) plus standard medical treatment (SMT) and half to a control group receiving SMT alone for 3 months.
The intervention group received a monitored high-calorie, high-protein, and salt-restricted diet as prescribed by a dedicated senior liver dietitian. The control group received regular nutritional recommendations and were managed for the ACLF-associated complications, without intervention or guidance by the study team.
After 3 months follow-up, overall survival (the primary outcome) was significantly improved in the OINT group compared with the control group (91.4% vs 57.1%), “suggesting that the improvement in nutrition status is associated with better survival,” the study team noted. Three patients died in the OINT group vs 15 in the SMT group.
OINT also led to a significant improvement in frailty, with LFI scores decreasing by an average of 0.93 in the intervention group vs 0.33 in the control group; 97% of patients improved from frail to prefrail status in the OINT group, whereas only 20% of patients improved in the SMT group.
The mean change in LFI of 0.93 with OINT is “well above the substantially clinically important difference” (change of 0.8) established in a previous study, the authors noted.
Significant improvements in weight and body mass index were also observed in the OINT group relative to the control group.
Liver disease severity, including model for end-stage liver disease (MELD) scores, showed greater improvement in the OINT group than in the control group (−8.7 vs −6.3 points from baseline to 3 months).
During the follow-up period, fewer patients in the intervention group than in the control group required a hospital stay (17% vs 45.7%).
Limitations of the study include the single-center design and the short follow-up period of 3 months, which limits long-term outcome assessment. Further, the study only included patients meeting Asia Pacific Association for Study of Liver criteria for ACLF, which does not include the patients with organ failure as defined by European Association for the Study of the Liver-Chronic Liver Failure Consortium criteria. Patients with ACLF who had more severe disease (MELD score > 30 or AARC > 10) were also not included.
Despite these limitations, the authors said their study showed that “dietician-monitored goal-directed nutrition therapy is very important in the management of patients with alcohol-related ACLF along with SMT.”
Confirmatory Data
Reached for comment, Katherine Patton, MEd, RD, a registered dietitian with the Center for Human Nutrition at Cleveland Clinic, Cleveland, Ohio, said it’s well known that the ACLF patient population has a “very high rate of morbidity and mortality and their quality of life tends to be poor due to their frailty. It is also fairly well-known that proper nutrition therapy can improve outcomes, however barriers to adequate nutrition include decreased appetite, nausea, pain, altered taste, and early satiety from ascites.”
“Hepatologists are likely stressing the importance of adequate protein energy intake and doctors may refer patients to an outpatient dietitian, but it is up to the patient to make that appointment and act on the recommendations,” Patton told GI & Hepatology News.
“If a dietitian works in the same clinic as the hepatologist and patients can be referred and seen the same day, this is ideal. During a hospital admission, protein/calorie intake can be more closely monitored and encouraged by a multi-disciplinary team,” Patton explained.
She cautioned that “the average patient is not familiar with how to apply general calorie and protein goals to their everyday eating habits. This study amplifies the role of a dietitian and what consistent education and resources can do to improve a patient’s quality of life and survival.”
This study had no specific funding. The authors have declared no relevant conflicts of interest. Patton had no relevant disclosures.
A version of this article appeared on Medscape.com.
In a randomized controlled trial, compared with standard care, dietitian-supported, intensive nutritional therapy improved survival, reduced frailty, and lowered hospitalization rates in men with alcohol-related ACLF.
The study, performed by a team from the Postgraduate Institute of Medical Education and Research, Chandigarh, India, was published in Clinical Gastroenterology and Hepatology.
ACLF related to alcohol use is associated with poor outcomes due to poor nutritional intake and frailty. Frail patients with ACLF face higher morbidity, mortality, and hospitalization rates than their nonfrail counterparts. However, research on the role of structured nutritional interventions in improving these outcomes is limited.
Patal Giri, MBBS, MD, and colleagues enrolled 70 men with alcohol-related ACLF and frailty (liver frailty index [LFI] > 4.5) in a single-center, open-label study. Half were randomly allocated to an intervention group receiving outpatient intensive nutrition therapy (OINT) plus standard medical treatment (SMT) and half to a control group receiving SMT alone for 3 months.
The intervention group received a monitored high-calorie, high-protein, and salt-restricted diet as prescribed by a dedicated senior liver dietitian. The control group received regular nutritional recommendations and were managed for the ACLF-associated complications, without intervention or guidance by the study team.
After 3 months follow-up, overall survival (the primary outcome) was significantly improved in the OINT group compared with the control group (91.4% vs 57.1%), “suggesting that the improvement in nutrition status is associated with better survival,” the study team noted. Three patients died in the OINT group vs 15 in the SMT group.
OINT also led to a significant improvement in frailty, with LFI scores decreasing by an average of 0.93 in the intervention group vs 0.33 in the control group; 97% of patients improved from frail to prefrail status in the OINT group, whereas only 20% of patients improved in the SMT group.
The mean change in LFI of 0.93 with OINT is “well above the substantially clinically important difference” (change of 0.8) established in a previous study, the authors noted.
Significant improvements in weight and body mass index were also observed in the OINT group relative to the control group.
Liver disease severity, including model for end-stage liver disease (MELD) scores, showed greater improvement in the OINT group than in the control group (−8.7 vs −6.3 points from baseline to 3 months).
During the follow-up period, fewer patients in the intervention group than in the control group required a hospital stay (17% vs 45.7%).
Limitations of the study include the single-center design and the short follow-up period of 3 months, which limits long-term outcome assessment. Further, the study only included patients meeting Asia Pacific Association for Study of Liver criteria for ACLF, which does not include the patients with organ failure as defined by European Association for the Study of the Liver-Chronic Liver Failure Consortium criteria. Patients with ACLF who had more severe disease (MELD score > 30 or AARC > 10) were also not included.
Despite these limitations, the authors said their study showed that “dietician-monitored goal-directed nutrition therapy is very important in the management of patients with alcohol-related ACLF along with SMT.”
Confirmatory Data
Reached for comment, Katherine Patton, MEd, RD, a registered dietitian with the Center for Human Nutrition at Cleveland Clinic, Cleveland, Ohio, said it’s well known that the ACLF patient population has a “very high rate of morbidity and mortality and their quality of life tends to be poor due to their frailty. It is also fairly well-known that proper nutrition therapy can improve outcomes, however barriers to adequate nutrition include decreased appetite, nausea, pain, altered taste, and early satiety from ascites.”
“Hepatologists are likely stressing the importance of adequate protein energy intake and doctors may refer patients to an outpatient dietitian, but it is up to the patient to make that appointment and act on the recommendations,” Patton told GI & Hepatology News.
“If a dietitian works in the same clinic as the hepatologist and patients can be referred and seen the same day, this is ideal. During a hospital admission, protein/calorie intake can be more closely monitored and encouraged by a multi-disciplinary team,” Patton explained.
She cautioned that “the average patient is not familiar with how to apply general calorie and protein goals to their everyday eating habits. This study amplifies the role of a dietitian and what consistent education and resources can do to improve a patient’s quality of life and survival.”
This study had no specific funding. The authors have declared no relevant conflicts of interest. Patton had no relevant disclosures.
A version of this article appeared on Medscape.com.
In a randomized controlled trial, compared with standard care, dietitian-supported, intensive nutritional therapy improved survival, reduced frailty, and lowered hospitalization rates in men with alcohol-related ACLF.
The study, performed by a team from the Postgraduate Institute of Medical Education and Research, Chandigarh, India, was published in Clinical Gastroenterology and Hepatology.
ACLF related to alcohol use is associated with poor outcomes due to poor nutritional intake and frailty. Frail patients with ACLF face higher morbidity, mortality, and hospitalization rates than their nonfrail counterparts. However, research on the role of structured nutritional interventions in improving these outcomes is limited.
Patal Giri, MBBS, MD, and colleagues enrolled 70 men with alcohol-related ACLF and frailty (liver frailty index [LFI] > 4.5) in a single-center, open-label study. Half were randomly allocated to an intervention group receiving outpatient intensive nutrition therapy (OINT) plus standard medical treatment (SMT) and half to a control group receiving SMT alone for 3 months.
The intervention group received a monitored high-calorie, high-protein, and salt-restricted diet as prescribed by a dedicated senior liver dietitian. The control group received regular nutritional recommendations and were managed for the ACLF-associated complications, without intervention or guidance by the study team.
After 3 months follow-up, overall survival (the primary outcome) was significantly improved in the OINT group compared with the control group (91.4% vs 57.1%), “suggesting that the improvement in nutrition status is associated with better survival,” the study team noted. Three patients died in the OINT group vs 15 in the SMT group.
OINT also led to a significant improvement in frailty, with LFI scores decreasing by an average of 0.93 in the intervention group vs 0.33 in the control group; 97% of patients improved from frail to prefrail status in the OINT group, whereas only 20% of patients improved in the SMT group.
The mean change in LFI of 0.93 with OINT is “well above the substantially clinically important difference” (change of 0.8) established in a previous study, the authors noted.
Significant improvements in weight and body mass index were also observed in the OINT group relative to the control group.
Liver disease severity, including model for end-stage liver disease (MELD) scores, showed greater improvement in the OINT group than in the control group (−8.7 vs −6.3 points from baseline to 3 months).
During the follow-up period, fewer patients in the intervention group than in the control group required a hospital stay (17% vs 45.7%).
Limitations of the study include the single-center design and the short follow-up period of 3 months, which limits long-term outcome assessment. Further, the study only included patients meeting Asia Pacific Association for Study of Liver criteria for ACLF, which does not include the patients with organ failure as defined by European Association for the Study of the Liver-Chronic Liver Failure Consortium criteria. Patients with ACLF who had more severe disease (MELD score > 30 or AARC > 10) were also not included.
Despite these limitations, the authors said their study showed that “dietician-monitored goal-directed nutrition therapy is very important in the management of patients with alcohol-related ACLF along with SMT.”
Confirmatory Data
Reached for comment, Katherine Patton, MEd, RD, a registered dietitian with the Center for Human Nutrition at Cleveland Clinic, Cleveland, Ohio, said it’s well known that the ACLF patient population has a “very high rate of morbidity and mortality and their quality of life tends to be poor due to their frailty. It is also fairly well-known that proper nutrition therapy can improve outcomes, however barriers to adequate nutrition include decreased appetite, nausea, pain, altered taste, and early satiety from ascites.”
“Hepatologists are likely stressing the importance of adequate protein energy intake and doctors may refer patients to an outpatient dietitian, but it is up to the patient to make that appointment and act on the recommendations,” Patton told GI & Hepatology News.
“If a dietitian works in the same clinic as the hepatologist and patients can be referred and seen the same day, this is ideal. During a hospital admission, protein/calorie intake can be more closely monitored and encouraged by a multi-disciplinary team,” Patton explained.
She cautioned that “the average patient is not familiar with how to apply general calorie and protein goals to their everyday eating habits. This study amplifies the role of a dietitian and what consistent education and resources can do to improve a patient’s quality of life and survival.”
This study had no specific funding. The authors have declared no relevant conflicts of interest. Patton had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
OK to Skip Pelvic Lymph Node Dissection in Cervical Cancer?
Results from the PHENIX-I trial support skipping pelvic lymphadenectomy in women with early cervical cancer who have a negative sentinel lymph node biopsy.
Omitting pelvic lymphadenectomy in these patients “did not compromise disease-free survival and potentially [led to] improved overall survival,” reported lead investigator Jihong Liu, MD, gynecologic oncologist, Sun Yat-sen University Cancer Center, Guangzhou, China.
Forgoing the additional procedure also decreased the incidence of retroperitoneal lymph node recurrence and adverse events and demonstrated superior surgical outcomes including shorter operative duration, reduced blood loss, and a lower morbidity.
Liu reported the PHENIX-I results at this year’s Society of Gynecologic Oncology Annual Meeting on Women’s Cancers (SGO) 2025.
Pelvic lymphadenectomy has been part of standard care for early-stage cervical cancer for over a century, even though the incidence of lymph node metastasis in early-stage cervical cancer is relatively low. Overtreatment and increased morbidity have been notable drawbacks of the procedure.
It may be possible to forgo pelvic lymphadenectomy in early-stage cervical cancer when sentinel lymph node biopsy findings are negative, but evidence from randomized controlled trials are lacking, Liu explained.
The PHENIX-I trial prospectively assessed survival outcomes among patients who received pelvic lymphadenectomy and those who did not. More specifically, all patients underwent sentinel lymph node biopsy and patients with negative lymph nodes were then intraoperatively randomized (1:1) to undergo pelvic lymphadenectomy (417 patients) or not (416 patients).
The multicenter, randomized controlled trial involved patients undergoing radical hysterectomy for stage IA1 (lymphovascular invasion), IA2, IB1, IB2 or IIA1 cervical cancer with tumor size not exceeding 3 cm.
“The only difference between the two groups was that patients in the experimental arm did not have pelvic lymphadenectomy,” Liu said.
Liu and colleagues reported that 23 patients (2.8%) had a positive lymph node on postoperative pathology examination. The rate of false-negative sentinel lymph node biopsy was < 1%. About half the patients in both groups received postoperative adjuvant therapy, and there was no significant between-group difference in the rates and time to initiate adjuvant therapy.
Overall, about 3.85% of patients (n = 16) in the biopsy-only group had a recurrence compared with 6.24% (n = 26) in the pelvic lymphadenectomy group at a median follow-up of 50 months.
But no patients in the biopsy-only group had a recurrence in the retroperitoneal lymph nodes compared with 9 patients in the pelvic lymphadenectomy group.
The 3-year disease-free survival (primary endpoint) rates were similar between the two groups — 96.8% in the biopsy-only group and 94.5% in the lymphadenectomy group (hazard ratio [HR], 0.61; P = .12). However, the 3-year overall survival was significantly higher in biopsy-only group — 100% vs 97.8% in the lymphadenectomy group (HR, 0.21; P = .007). Overall, three patients (19%) in the biopsy-only group died from cervical cancer vs 14 (54%) in the lymphadenectomy group.
As for surgical complications, pelvic lymphadenectomy was associated with a higher incidence of pain (5.8% vs 1.7%), lymphocyst (22.1% vs 8.4%), and lymphedema (10.1% vs 2.4%), as well as longer operating time and more blood loss.
Offering perspective on PHENIX-I, discussant Premal Thaker, MD, noted that this is the first randomized trial to report on the use of sentinel lymph node biopsy alone vs biopsy plus pelvic lymphadenectomy after radical hysterectomy.
Key takeaways are the “equivalent” 3-year disease-free outcomes but “lower” overall survival in the pelvic lymphadenectomy group as well as more adverse events, said Thaker, gynecologic oncologist and surgeon, Siteman Cancer Center, Washington University, St Louis.
Although quality of life data was not presented in the trial, patients who skipped pelvic lymphadenectomy had fewer adverse events, “which is very important for our patients,” Thaker added.
This study had no commercial funding. Liu and Thaker had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Results from the PHENIX-I trial support skipping pelvic lymphadenectomy in women with early cervical cancer who have a negative sentinel lymph node biopsy.
Omitting pelvic lymphadenectomy in these patients “did not compromise disease-free survival and potentially [led to] improved overall survival,” reported lead investigator Jihong Liu, MD, gynecologic oncologist, Sun Yat-sen University Cancer Center, Guangzhou, China.
Forgoing the additional procedure also decreased the incidence of retroperitoneal lymph node recurrence and adverse events and demonstrated superior surgical outcomes including shorter operative duration, reduced blood loss, and a lower morbidity.
Liu reported the PHENIX-I results at this year’s Society of Gynecologic Oncology Annual Meeting on Women’s Cancers (SGO) 2025.
Pelvic lymphadenectomy has been part of standard care for early-stage cervical cancer for over a century, even though the incidence of lymph node metastasis in early-stage cervical cancer is relatively low. Overtreatment and increased morbidity have been notable drawbacks of the procedure.
It may be possible to forgo pelvic lymphadenectomy in early-stage cervical cancer when sentinel lymph node biopsy findings are negative, but evidence from randomized controlled trials are lacking, Liu explained.
The PHENIX-I trial prospectively assessed survival outcomes among patients who received pelvic lymphadenectomy and those who did not. More specifically, all patients underwent sentinel lymph node biopsy and patients with negative lymph nodes were then intraoperatively randomized (1:1) to undergo pelvic lymphadenectomy (417 patients) or not (416 patients).
The multicenter, randomized controlled trial involved patients undergoing radical hysterectomy for stage IA1 (lymphovascular invasion), IA2, IB1, IB2 or IIA1 cervical cancer with tumor size not exceeding 3 cm.
“The only difference between the two groups was that patients in the experimental arm did not have pelvic lymphadenectomy,” Liu said.
Liu and colleagues reported that 23 patients (2.8%) had a positive lymph node on postoperative pathology examination. The rate of false-negative sentinel lymph node biopsy was < 1%. About half the patients in both groups received postoperative adjuvant therapy, and there was no significant between-group difference in the rates and time to initiate adjuvant therapy.
Overall, about 3.85% of patients (n = 16) in the biopsy-only group had a recurrence compared with 6.24% (n = 26) in the pelvic lymphadenectomy group at a median follow-up of 50 months.
But no patients in the biopsy-only group had a recurrence in the retroperitoneal lymph nodes compared with 9 patients in the pelvic lymphadenectomy group.
The 3-year disease-free survival (primary endpoint) rates were similar between the two groups — 96.8% in the biopsy-only group and 94.5% in the lymphadenectomy group (hazard ratio [HR], 0.61; P = .12). However, the 3-year overall survival was significantly higher in biopsy-only group — 100% vs 97.8% in the lymphadenectomy group (HR, 0.21; P = .007). Overall, three patients (19%) in the biopsy-only group died from cervical cancer vs 14 (54%) in the lymphadenectomy group.
As for surgical complications, pelvic lymphadenectomy was associated with a higher incidence of pain (5.8% vs 1.7%), lymphocyst (22.1% vs 8.4%), and lymphedema (10.1% vs 2.4%), as well as longer operating time and more blood loss.
Offering perspective on PHENIX-I, discussant Premal Thaker, MD, noted that this is the first randomized trial to report on the use of sentinel lymph node biopsy alone vs biopsy plus pelvic lymphadenectomy after radical hysterectomy.
Key takeaways are the “equivalent” 3-year disease-free outcomes but “lower” overall survival in the pelvic lymphadenectomy group as well as more adverse events, said Thaker, gynecologic oncologist and surgeon, Siteman Cancer Center, Washington University, St Louis.
Although quality of life data was not presented in the trial, patients who skipped pelvic lymphadenectomy had fewer adverse events, “which is very important for our patients,” Thaker added.
This study had no commercial funding. Liu and Thaker had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Results from the PHENIX-I trial support skipping pelvic lymphadenectomy in women with early cervical cancer who have a negative sentinel lymph node biopsy.
Omitting pelvic lymphadenectomy in these patients “did not compromise disease-free survival and potentially [led to] improved overall survival,” reported lead investigator Jihong Liu, MD, gynecologic oncologist, Sun Yat-sen University Cancer Center, Guangzhou, China.
Forgoing the additional procedure also decreased the incidence of retroperitoneal lymph node recurrence and adverse events and demonstrated superior surgical outcomes including shorter operative duration, reduced blood loss, and a lower morbidity.
Liu reported the PHENIX-I results at this year’s Society of Gynecologic Oncology Annual Meeting on Women’s Cancers (SGO) 2025.
Pelvic lymphadenectomy has been part of standard care for early-stage cervical cancer for over a century, even though the incidence of lymph node metastasis in early-stage cervical cancer is relatively low. Overtreatment and increased morbidity have been notable drawbacks of the procedure.
It may be possible to forgo pelvic lymphadenectomy in early-stage cervical cancer when sentinel lymph node biopsy findings are negative, but evidence from randomized controlled trials are lacking, Liu explained.
The PHENIX-I trial prospectively assessed survival outcomes among patients who received pelvic lymphadenectomy and those who did not. More specifically, all patients underwent sentinel lymph node biopsy and patients with negative lymph nodes were then intraoperatively randomized (1:1) to undergo pelvic lymphadenectomy (417 patients) or not (416 patients).
The multicenter, randomized controlled trial involved patients undergoing radical hysterectomy for stage IA1 (lymphovascular invasion), IA2, IB1, IB2 or IIA1 cervical cancer with tumor size not exceeding 3 cm.
“The only difference between the two groups was that patients in the experimental arm did not have pelvic lymphadenectomy,” Liu said.
Liu and colleagues reported that 23 patients (2.8%) had a positive lymph node on postoperative pathology examination. The rate of false-negative sentinel lymph node biopsy was < 1%. About half the patients in both groups received postoperative adjuvant therapy, and there was no significant between-group difference in the rates and time to initiate adjuvant therapy.
Overall, about 3.85% of patients (n = 16) in the biopsy-only group had a recurrence compared with 6.24% (n = 26) in the pelvic lymphadenectomy group at a median follow-up of 50 months.
But no patients in the biopsy-only group had a recurrence in the retroperitoneal lymph nodes compared with 9 patients in the pelvic lymphadenectomy group.
The 3-year disease-free survival (primary endpoint) rates were similar between the two groups — 96.8% in the biopsy-only group and 94.5% in the lymphadenectomy group (hazard ratio [HR], 0.61; P = .12). However, the 3-year overall survival was significantly higher in biopsy-only group — 100% vs 97.8% in the lymphadenectomy group (HR, 0.21; P = .007). Overall, three patients (19%) in the biopsy-only group died from cervical cancer vs 14 (54%) in the lymphadenectomy group.
As for surgical complications, pelvic lymphadenectomy was associated with a higher incidence of pain (5.8% vs 1.7%), lymphocyst (22.1% vs 8.4%), and lymphedema (10.1% vs 2.4%), as well as longer operating time and more blood loss.
Offering perspective on PHENIX-I, discussant Premal Thaker, MD, noted that this is the first randomized trial to report on the use of sentinel lymph node biopsy alone vs biopsy plus pelvic lymphadenectomy after radical hysterectomy.
Key takeaways are the “equivalent” 3-year disease-free outcomes but “lower” overall survival in the pelvic lymphadenectomy group as well as more adverse events, said Thaker, gynecologic oncologist and surgeon, Siteman Cancer Center, Washington University, St Louis.
Although quality of life data was not presented in the trial, patients who skipped pelvic lymphadenectomy had fewer adverse events, “which is very important for our patients,” Thaker added.
This study had no commercial funding. Liu and Thaker had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SGO 2025
ACG Issues First Guidance on Diagnosis and Management of Gastric Premalignant Conditions
including atrophic gastritis, gastric intestinal metaplasia, dysplasia, and certain gastric epithelial polyps, all of which have an increased risk of progressing to gastric cancer.
The guideline was published online in The American Journal of Gastroenterology.
GPMCs are “common in gastroenterology practices, but in the US, at least, we’ve not had concrete guidance,” first author Douglas Morgan, MD, MPH, AGAF, Division of Gastroenterology, The University of Alabama at Birmingham, noted in an interview.
With these guidelines, we hope there “will be a paradigm shift to finally establish surveillance in the stomach, much like we’ve been doing for decades in the colon and the esophagus,” Morgan said.
Gastric cancer is a common cancer in the United States with disproportionately higher incidence rates in immigrants from countries with a high incidence of gastric cancer and certain non-White populations.
In addition, the 5-year survival rate in the United States for gastric cancer is 36%, which falls short of global standards and is driven by the fact that only a small percentage of these cancers are diagnosed in the early, curable stage.
These guidelines will help address this marked disparity and the burden on minority and marginalized populations, the guideline authors wrote. “The overarching goals are to reduce [gastric cancer] incidence in the United States, increase the detection of early-stage disease (early gastric cancer), and to significantly increase the 5-year survival rates in the near term.”
Key Recommendations
The guideline includes recommendations on endoscopic surveillance for high-risk patients, the performance of high-quality endoscopy and image-enhanced endoscopy (IEE) for diagnosis and surveillance, GPMC histology criteria and reporting, endoscopic treatment of dysplasia, the role of Helicobacter pylori eradication, general risk reduction measures, and the management of autoimmune gastritis and gastric epithelial polyps.
In terms of screening, the guidelines recommend against routine upper endoscopy screening for gastric cancer and GPMC in the general US population (low quality of evidence; conditional recommendation).
They also noted that there is “insufficient” direct US evidence to make a recommendation on opportunistic endoscopy screening for gastric cancer and GPMC in patients deemed at high risk based on race/ethnicity and family history. In addition, they recommend against the use of noninvasive biomarkers for screening or surveillance of GPMC or gastric cancer.
In terms of endoscopic and histologic diagnosis of GPMC, high-quality endoscopic evaluation is crucial to detect premalignant conditions or gastric cancer, the authors said. This includes adequate mucosal cleansing and insufflation, and photodocumentation of anatomic landmarks, as well as use of high-definition white light endoscopy (HDWLE) and IEE.
Systematic gastric biopsies should follow the updated Sydney protocol, with at least two separate containers for antrum/incisura and corpus biopsies. Histology should document the subtype of gastric intestinal metaplasia — incomplete, complete, or mixed — and severity and extent of atrophic gastritis and metaplasia.
Morgan emphasized the importance of coordination between the gastroenterologist and pathologist. “Several of these measures are not routinely reported, so we need to be in conversations with our collaborating pathologists,” he told this news organization.
In terms of GPMC surveillance, the authors suggest surveillance endoscopy every 3 years in high-risk patients with gastric intestinal metaplasia who meet one of the following criteria: High-risk histology (incomplete vs complete subtype, extending into the corpus); family history of gastric cancer in a first-degree relative; foreign-born individuals from high-gastric cancer incidence nations; or high-risk race/ethnicity (East Asian, Latino/a, Black, American Indian, or Alaska Native).
Individuals with multiple risk factors for gastric cancer may be considered for shorter than 3-year intervals.
Low-risk gastric intestinal metaplasia (limited to antrum, mild atrophy, and complete gastric intestinal metaplasia subtype) does not require routine endoscopic surveillance.
In terms of endoscopic management of dysplastic GPMC, endoscopic resection is suggested for dysplasia with visible margins. If dysplasia is not visible, repeat endoscopy with HDWLE and IEE by an experienced endoscopist is advised.
In patients appropriate for endoscopic resection of dysplasia, particularly endoscopic submucosal dissection, referral to a high-volume center with appropriate expertise in the diagnosis and therapeutic resection of gastric neoplasia is strongly recommended.
In patients with confirmed complete resection of dysplasia, endoscopic surveillance is also strongly recommended. Surveillance examinations should be performed by an experienced endoscopist using HDWLE and IEE, with biopsies according to the systematic biopsy protocol in addition to targeted biopsies.
In terms of nonendoscopic GPMC management, testing for H pylori (and eradication treatment if possible) is strongly recommended for patients with GPMC and those with a history of resected early gastric cancer.
Aspirin, nonsteroidal anti-inflammatory drugs, cyclooxygenase 2 inhibitors, or antioxidants are not recommended for patients with GPMC for the purpose of preventing gastric cancer.
In patients with autoimmune gastritis, testing for H pylori with a nonserological test, eradication treatment if positive, and posttreatment testing to confirm eradication is advised.
There is not enough evidence to make a formal recommendation on endoscopic surveillance in those with autoimmune gastritis; surveillance should be individualized, considering the risk for neuroendocrine tumors and possibly gastric cancer.
In terms of gastric epithelial polyps, endoscopic resection of all gastric adenomas is recommended, regardless of size, to exclude or prevent dysplasia and early gastric cancer. Adenomas that are not amenable to endoscopic resection should be referred for surgical resection, if clinically appropriate.
Morgan noted that the ACG GPMC guideline aligns with the updated ACG/American Society for Gastrointestinal Endoscopy upper endoscopy quality indicators released earlier this year.
Implementation of the ACG GPMC guideline and “change in clinical practice will require concrete targets and include training and quality initiatives,” the authors said.
This research received no commercial support. Morgan disclosed research support from Panbela Therapeutics, Thorne, and American Molecular Laboratories.
A version of this article first appeared on Medscape.com.
including atrophic gastritis, gastric intestinal metaplasia, dysplasia, and certain gastric epithelial polyps, all of which have an increased risk of progressing to gastric cancer.
The guideline was published online in The American Journal of Gastroenterology.
GPMCs are “common in gastroenterology practices, but in the US, at least, we’ve not had concrete guidance,” first author Douglas Morgan, MD, MPH, AGAF, Division of Gastroenterology, The University of Alabama at Birmingham, noted in an interview.
With these guidelines, we hope there “will be a paradigm shift to finally establish surveillance in the stomach, much like we’ve been doing for decades in the colon and the esophagus,” Morgan said.
Gastric cancer is a common cancer in the United States with disproportionately higher incidence rates in immigrants from countries with a high incidence of gastric cancer and certain non-White populations.
In addition, the 5-year survival rate in the United States for gastric cancer is 36%, which falls short of global standards and is driven by the fact that only a small percentage of these cancers are diagnosed in the early, curable stage.
These guidelines will help address this marked disparity and the burden on minority and marginalized populations, the guideline authors wrote. “The overarching goals are to reduce [gastric cancer] incidence in the United States, increase the detection of early-stage disease (early gastric cancer), and to significantly increase the 5-year survival rates in the near term.”
Key Recommendations
The guideline includes recommendations on endoscopic surveillance for high-risk patients, the performance of high-quality endoscopy and image-enhanced endoscopy (IEE) for diagnosis and surveillance, GPMC histology criteria and reporting, endoscopic treatment of dysplasia, the role of Helicobacter pylori eradication, general risk reduction measures, and the management of autoimmune gastritis and gastric epithelial polyps.
In terms of screening, the guidelines recommend against routine upper endoscopy screening for gastric cancer and GPMC in the general US population (low quality of evidence; conditional recommendation).
They also noted that there is “insufficient” direct US evidence to make a recommendation on opportunistic endoscopy screening for gastric cancer and GPMC in patients deemed at high risk based on race/ethnicity and family history. In addition, they recommend against the use of noninvasive biomarkers for screening or surveillance of GPMC or gastric cancer.
In terms of endoscopic and histologic diagnosis of GPMC, high-quality endoscopic evaluation is crucial to detect premalignant conditions or gastric cancer, the authors said. This includes adequate mucosal cleansing and insufflation, and photodocumentation of anatomic landmarks, as well as use of high-definition white light endoscopy (HDWLE) and IEE.
Systematic gastric biopsies should follow the updated Sydney protocol, with at least two separate containers for antrum/incisura and corpus biopsies. Histology should document the subtype of gastric intestinal metaplasia — incomplete, complete, or mixed — and severity and extent of atrophic gastritis and metaplasia.
Morgan emphasized the importance of coordination between the gastroenterologist and pathologist. “Several of these measures are not routinely reported, so we need to be in conversations with our collaborating pathologists,” he told this news organization.
In terms of GPMC surveillance, the authors suggest surveillance endoscopy every 3 years in high-risk patients with gastric intestinal metaplasia who meet one of the following criteria: High-risk histology (incomplete vs complete subtype, extending into the corpus); family history of gastric cancer in a first-degree relative; foreign-born individuals from high-gastric cancer incidence nations; or high-risk race/ethnicity (East Asian, Latino/a, Black, American Indian, or Alaska Native).
Individuals with multiple risk factors for gastric cancer may be considered for shorter than 3-year intervals.
Low-risk gastric intestinal metaplasia (limited to antrum, mild atrophy, and complete gastric intestinal metaplasia subtype) does not require routine endoscopic surveillance.
In terms of endoscopic management of dysplastic GPMC, endoscopic resection is suggested for dysplasia with visible margins. If dysplasia is not visible, repeat endoscopy with HDWLE and IEE by an experienced endoscopist is advised.
In patients appropriate for endoscopic resection of dysplasia, particularly endoscopic submucosal dissection, referral to a high-volume center with appropriate expertise in the diagnosis and therapeutic resection of gastric neoplasia is strongly recommended.
In patients with confirmed complete resection of dysplasia, endoscopic surveillance is also strongly recommended. Surveillance examinations should be performed by an experienced endoscopist using HDWLE and IEE, with biopsies according to the systematic biopsy protocol in addition to targeted biopsies.
In terms of nonendoscopic GPMC management, testing for H pylori (and eradication treatment if possible) is strongly recommended for patients with GPMC and those with a history of resected early gastric cancer.
Aspirin, nonsteroidal anti-inflammatory drugs, cyclooxygenase 2 inhibitors, or antioxidants are not recommended for patients with GPMC for the purpose of preventing gastric cancer.
In patients with autoimmune gastritis, testing for H pylori with a nonserological test, eradication treatment if positive, and posttreatment testing to confirm eradication is advised.
There is not enough evidence to make a formal recommendation on endoscopic surveillance in those with autoimmune gastritis; surveillance should be individualized, considering the risk for neuroendocrine tumors and possibly gastric cancer.
In terms of gastric epithelial polyps, endoscopic resection of all gastric adenomas is recommended, regardless of size, to exclude or prevent dysplasia and early gastric cancer. Adenomas that are not amenable to endoscopic resection should be referred for surgical resection, if clinically appropriate.
Morgan noted that the ACG GPMC guideline aligns with the updated ACG/American Society for Gastrointestinal Endoscopy upper endoscopy quality indicators released earlier this year.
Implementation of the ACG GPMC guideline and “change in clinical practice will require concrete targets and include training and quality initiatives,” the authors said.
This research received no commercial support. Morgan disclosed research support from Panbela Therapeutics, Thorne, and American Molecular Laboratories.
A version of this article first appeared on Medscape.com.
including atrophic gastritis, gastric intestinal metaplasia, dysplasia, and certain gastric epithelial polyps, all of which have an increased risk of progressing to gastric cancer.
The guideline was published online in The American Journal of Gastroenterology.
GPMCs are “common in gastroenterology practices, but in the US, at least, we’ve not had concrete guidance,” first author Douglas Morgan, MD, MPH, AGAF, Division of Gastroenterology, The University of Alabama at Birmingham, noted in an interview.
With these guidelines, we hope there “will be a paradigm shift to finally establish surveillance in the stomach, much like we’ve been doing for decades in the colon and the esophagus,” Morgan said.
Gastric cancer is a common cancer in the United States with disproportionately higher incidence rates in immigrants from countries with a high incidence of gastric cancer and certain non-White populations.
In addition, the 5-year survival rate in the United States for gastric cancer is 36%, which falls short of global standards and is driven by the fact that only a small percentage of these cancers are diagnosed in the early, curable stage.
These guidelines will help address this marked disparity and the burden on minority and marginalized populations, the guideline authors wrote. “The overarching goals are to reduce [gastric cancer] incidence in the United States, increase the detection of early-stage disease (early gastric cancer), and to significantly increase the 5-year survival rates in the near term.”
Key Recommendations
The guideline includes recommendations on endoscopic surveillance for high-risk patients, the performance of high-quality endoscopy and image-enhanced endoscopy (IEE) for diagnosis and surveillance, GPMC histology criteria and reporting, endoscopic treatment of dysplasia, the role of Helicobacter pylori eradication, general risk reduction measures, and the management of autoimmune gastritis and gastric epithelial polyps.
In terms of screening, the guidelines recommend against routine upper endoscopy screening for gastric cancer and GPMC in the general US population (low quality of evidence; conditional recommendation).
They also noted that there is “insufficient” direct US evidence to make a recommendation on opportunistic endoscopy screening for gastric cancer and GPMC in patients deemed at high risk based on race/ethnicity and family history. In addition, they recommend against the use of noninvasive biomarkers for screening or surveillance of GPMC or gastric cancer.
In terms of endoscopic and histologic diagnosis of GPMC, high-quality endoscopic evaluation is crucial to detect premalignant conditions or gastric cancer, the authors said. This includes adequate mucosal cleansing and insufflation, and photodocumentation of anatomic landmarks, as well as use of high-definition white light endoscopy (HDWLE) and IEE.
Systematic gastric biopsies should follow the updated Sydney protocol, with at least two separate containers for antrum/incisura and corpus biopsies. Histology should document the subtype of gastric intestinal metaplasia — incomplete, complete, or mixed — and severity and extent of atrophic gastritis and metaplasia.
Morgan emphasized the importance of coordination between the gastroenterologist and pathologist. “Several of these measures are not routinely reported, so we need to be in conversations with our collaborating pathologists,” he told this news organization.
In terms of GPMC surveillance, the authors suggest surveillance endoscopy every 3 years in high-risk patients with gastric intestinal metaplasia who meet one of the following criteria: High-risk histology (incomplete vs complete subtype, extending into the corpus); family history of gastric cancer in a first-degree relative; foreign-born individuals from high-gastric cancer incidence nations; or high-risk race/ethnicity (East Asian, Latino/a, Black, American Indian, or Alaska Native).
Individuals with multiple risk factors for gastric cancer may be considered for shorter than 3-year intervals.
Low-risk gastric intestinal metaplasia (limited to antrum, mild atrophy, and complete gastric intestinal metaplasia subtype) does not require routine endoscopic surveillance.
In terms of endoscopic management of dysplastic GPMC, endoscopic resection is suggested for dysplasia with visible margins. If dysplasia is not visible, repeat endoscopy with HDWLE and IEE by an experienced endoscopist is advised.
In patients appropriate for endoscopic resection of dysplasia, particularly endoscopic submucosal dissection, referral to a high-volume center with appropriate expertise in the diagnosis and therapeutic resection of gastric neoplasia is strongly recommended.
In patients with confirmed complete resection of dysplasia, endoscopic surveillance is also strongly recommended. Surveillance examinations should be performed by an experienced endoscopist using HDWLE and IEE, with biopsies according to the systematic biopsy protocol in addition to targeted biopsies.
In terms of nonendoscopic GPMC management, testing for H pylori (and eradication treatment if possible) is strongly recommended for patients with GPMC and those with a history of resected early gastric cancer.
Aspirin, nonsteroidal anti-inflammatory drugs, cyclooxygenase 2 inhibitors, or antioxidants are not recommended for patients with GPMC for the purpose of preventing gastric cancer.
In patients with autoimmune gastritis, testing for H pylori with a nonserological test, eradication treatment if positive, and posttreatment testing to confirm eradication is advised.
There is not enough evidence to make a formal recommendation on endoscopic surveillance in those with autoimmune gastritis; surveillance should be individualized, considering the risk for neuroendocrine tumors and possibly gastric cancer.
In terms of gastric epithelial polyps, endoscopic resection of all gastric adenomas is recommended, regardless of size, to exclude or prevent dysplasia and early gastric cancer. Adenomas that are not amenable to endoscopic resection should be referred for surgical resection, if clinically appropriate.
Morgan noted that the ACG GPMC guideline aligns with the updated ACG/American Society for Gastrointestinal Endoscopy upper endoscopy quality indicators released earlier this year.
Implementation of the ACG GPMC guideline and “change in clinical practice will require concrete targets and include training and quality initiatives,” the authors said.
This research received no commercial support. Morgan disclosed research support from Panbela Therapeutics, Thorne, and American Molecular Laboratories.
A version of this article first appeared on Medscape.com.
AI-Enhanced Echocardiography: A Game-Changer for Opportunistic Liver Disease Detection?
An AI algorithm called EchoNet-Liver demonstrated strong performance for detecting cirrhosis and steatotic liver disease (SLD) from routinely acquired transthoracic echocardiography studies containing subcostal images of the liver, the developers reported in NEJM AI.
“We hope that this algorithm enables physicians to opportunistically screen for chronic liver disease to identify asymptomatic and undiagnosed patients, thus enabling us to treat comorbidities relevant to the patient’s cardiovascular and noncardiovascular health,” Alan C. Kwan, MD, assistant professor, Department of Cardiology, Smidt Heart Institute at Cedars-Sinai, Los Angeles, California, told this news organization.
Harnessing Echo to Reveal Liver Trouble
CLD affects over 1.5 billion people globally, with many cases remaining undiagnosed due to the asymptomatic nature of early disease and a lack of routine screening. Traditional diagnostic methods such as liver function tests, ultrasonography, and MRI are often limited by cost, availability, and patient access.
Echocardiography is a commonly performed imaging study that incidentally captures images of the liver but is not utilized for liver disease assessment.
EchoNet-Liver is an AI algorithm that can identify high-quality subcostal images from full echocardiography studies and detect the presence of cirrhosis and SLD.
Kwan and colleagues trained it using nearly 1.6 million echocardiogram videos from 66,922 studies and 24,276 adult patients at Cedars-Sinai Medical Center (CSMC). The model predictions were compared with diagnoses from clinical evaluations of paired abdominal ultrasound or MRI studies. External validation studies were conducted using similar data from Stanford Health Care.
In the “held-out” CSMC ultrasound dataset, EchoNet-Liver detected cirrhosis with an area under the receiver operating characteristic curve (AUROC) of 0.837 (95% CI, 0.828-0.848) and SLD with an AUROC of 0.799 (95% CI, 0.788-0.811).
The algorithm showed a sensitivity of 69.6% and a specificity of 84.6% for detecting cirrhosis, and a sensitivity of 74.1% and a specificity of 72.0% for detecting SLD.
In the Stanford Health Care external-validation test ultrasound cohort, the model detected cirrhosis with an AUROC of 0.830 (95% CI, 0.799-0.859) and SLD with an AUROC of 0.769 (95% CI, 0.733-0.813), with sensitivity and specificity of 80.0% and 70.9%, respectively, for cirrhosis and 66.7% and 78.0%, respectively, for SLD.
In the CSMC MRI-paired cohort, EchoNet-Liver detected cirrhosis with an AUROC of 0.704 (95% CI, 0.699-0.708) and SLD with an AUROC of 0.725 (95% CI, 0.707-0.762).
Identifying Subclinical Liver Disease to Improve Outcomes
“Across diverse populations and disease definitions, deep-learning-enhanced echocardiography enabled high-throughput, automated detection of CLD, which could enable opportunistic screening for asymptomatic liver disease,” the authors wrote.
“By improving the diagnosis of subclinical CLD, we may be able to limit or reverse disease progression and improve care by triaging patients toward appropriate clinical and diagnostic management,” they said.
By way of limitations, the researchers noted that the tool was developed using a cohort of patients who had both abdominal ultrasound and echocardiography within 30 days, and thus probably had a higher prevalence of liver disease compared with the general population receiving echocardiography. The true clinical utility of EchoNet-Liver will depend on whether its application to a general echocardiography population can efficiently detect undiagnosed CLD, they cautioned.
“While we developed this algorithm based on clinical data, the application within the clinic would typically require FDA approval, which we have not yet applied for,” Kwan told this news organization.
“We plan to prospectively validate this algorithm at multiple sites to ensure that application of this algorithm improves patient care without causing excess diagnostic testing, thus providing value to patients and the healthcare system as a whole,” Kwan said.
Funding was provided in part by KAKENHI (Japan Society for the Promotion of Science). Kwan reported receiving consulting fees from InVision.
A version of this article first appeared on Medscape.com.
An AI algorithm called EchoNet-Liver demonstrated strong performance for detecting cirrhosis and steatotic liver disease (SLD) from routinely acquired transthoracic echocardiography studies containing subcostal images of the liver, the developers reported in NEJM AI.
“We hope that this algorithm enables physicians to opportunistically screen for chronic liver disease to identify asymptomatic and undiagnosed patients, thus enabling us to treat comorbidities relevant to the patient’s cardiovascular and noncardiovascular health,” Alan C. Kwan, MD, assistant professor, Department of Cardiology, Smidt Heart Institute at Cedars-Sinai, Los Angeles, California, told this news organization.
Harnessing Echo to Reveal Liver Trouble
CLD affects over 1.5 billion people globally, with many cases remaining undiagnosed due to the asymptomatic nature of early disease and a lack of routine screening. Traditional diagnostic methods such as liver function tests, ultrasonography, and MRI are often limited by cost, availability, and patient access.
Echocardiography is a commonly performed imaging study that incidentally captures images of the liver but is not utilized for liver disease assessment.
EchoNet-Liver is an AI algorithm that can identify high-quality subcostal images from full echocardiography studies and detect the presence of cirrhosis and SLD.
Kwan and colleagues trained it using nearly 1.6 million echocardiogram videos from 66,922 studies and 24,276 adult patients at Cedars-Sinai Medical Center (CSMC). The model predictions were compared with diagnoses from clinical evaluations of paired abdominal ultrasound or MRI studies. External validation studies were conducted using similar data from Stanford Health Care.
In the “held-out” CSMC ultrasound dataset, EchoNet-Liver detected cirrhosis with an area under the receiver operating characteristic curve (AUROC) of 0.837 (95% CI, 0.828-0.848) and SLD with an AUROC of 0.799 (95% CI, 0.788-0.811).
The algorithm showed a sensitivity of 69.6% and a specificity of 84.6% for detecting cirrhosis, and a sensitivity of 74.1% and a specificity of 72.0% for detecting SLD.
In the Stanford Health Care external-validation test ultrasound cohort, the model detected cirrhosis with an AUROC of 0.830 (95% CI, 0.799-0.859) and SLD with an AUROC of 0.769 (95% CI, 0.733-0.813), with sensitivity and specificity of 80.0% and 70.9%, respectively, for cirrhosis and 66.7% and 78.0%, respectively, for SLD.
In the CSMC MRI-paired cohort, EchoNet-Liver detected cirrhosis with an AUROC of 0.704 (95% CI, 0.699-0.708) and SLD with an AUROC of 0.725 (95% CI, 0.707-0.762).
Identifying Subclinical Liver Disease to Improve Outcomes
“Across diverse populations and disease definitions, deep-learning-enhanced echocardiography enabled high-throughput, automated detection of CLD, which could enable opportunistic screening for asymptomatic liver disease,” the authors wrote.
“By improving the diagnosis of subclinical CLD, we may be able to limit or reverse disease progression and improve care by triaging patients toward appropriate clinical and diagnostic management,” they said.
By way of limitations, the researchers noted that the tool was developed using a cohort of patients who had both abdominal ultrasound and echocardiography within 30 days, and thus probably had a higher prevalence of liver disease compared with the general population receiving echocardiography. The true clinical utility of EchoNet-Liver will depend on whether its application to a general echocardiography population can efficiently detect undiagnosed CLD, they cautioned.
“While we developed this algorithm based on clinical data, the application within the clinic would typically require FDA approval, which we have not yet applied for,” Kwan told this news organization.
“We plan to prospectively validate this algorithm at multiple sites to ensure that application of this algorithm improves patient care without causing excess diagnostic testing, thus providing value to patients and the healthcare system as a whole,” Kwan said.
Funding was provided in part by KAKENHI (Japan Society for the Promotion of Science). Kwan reported receiving consulting fees from InVision.
A version of this article first appeared on Medscape.com.
An AI algorithm called EchoNet-Liver demonstrated strong performance for detecting cirrhosis and steatotic liver disease (SLD) from routinely acquired transthoracic echocardiography studies containing subcostal images of the liver, the developers reported in NEJM AI.
“We hope that this algorithm enables physicians to opportunistically screen for chronic liver disease to identify asymptomatic and undiagnosed patients, thus enabling us to treat comorbidities relevant to the patient’s cardiovascular and noncardiovascular health,” Alan C. Kwan, MD, assistant professor, Department of Cardiology, Smidt Heart Institute at Cedars-Sinai, Los Angeles, California, told this news organization.
Harnessing Echo to Reveal Liver Trouble
CLD affects over 1.5 billion people globally, with many cases remaining undiagnosed due to the asymptomatic nature of early disease and a lack of routine screening. Traditional diagnostic methods such as liver function tests, ultrasonography, and MRI are often limited by cost, availability, and patient access.
Echocardiography is a commonly performed imaging study that incidentally captures images of the liver but is not utilized for liver disease assessment.
EchoNet-Liver is an AI algorithm that can identify high-quality subcostal images from full echocardiography studies and detect the presence of cirrhosis and SLD.
Kwan and colleagues trained it using nearly 1.6 million echocardiogram videos from 66,922 studies and 24,276 adult patients at Cedars-Sinai Medical Center (CSMC). The model predictions were compared with diagnoses from clinical evaluations of paired abdominal ultrasound or MRI studies. External validation studies were conducted using similar data from Stanford Health Care.
In the “held-out” CSMC ultrasound dataset, EchoNet-Liver detected cirrhosis with an area under the receiver operating characteristic curve (AUROC) of 0.837 (95% CI, 0.828-0.848) and SLD with an AUROC of 0.799 (95% CI, 0.788-0.811).
The algorithm showed a sensitivity of 69.6% and a specificity of 84.6% for detecting cirrhosis, and a sensitivity of 74.1% and a specificity of 72.0% for detecting SLD.
In the Stanford Health Care external-validation test ultrasound cohort, the model detected cirrhosis with an AUROC of 0.830 (95% CI, 0.799-0.859) and SLD with an AUROC of 0.769 (95% CI, 0.733-0.813), with sensitivity and specificity of 80.0% and 70.9%, respectively, for cirrhosis and 66.7% and 78.0%, respectively, for SLD.
In the CSMC MRI-paired cohort, EchoNet-Liver detected cirrhosis with an AUROC of 0.704 (95% CI, 0.699-0.708) and SLD with an AUROC of 0.725 (95% CI, 0.707-0.762).
Identifying Subclinical Liver Disease to Improve Outcomes
“Across diverse populations and disease definitions, deep-learning-enhanced echocardiography enabled high-throughput, automated detection of CLD, which could enable opportunistic screening for asymptomatic liver disease,” the authors wrote.
“By improving the diagnosis of subclinical CLD, we may be able to limit or reverse disease progression and improve care by triaging patients toward appropriate clinical and diagnostic management,” they said.
By way of limitations, the researchers noted that the tool was developed using a cohort of patients who had both abdominal ultrasound and echocardiography within 30 days, and thus probably had a higher prevalence of liver disease compared with the general population receiving echocardiography. The true clinical utility of EchoNet-Liver will depend on whether its application to a general echocardiography population can efficiently detect undiagnosed CLD, they cautioned.
“While we developed this algorithm based on clinical data, the application within the clinic would typically require FDA approval, which we have not yet applied for,” Kwan told this news organization.
“We plan to prospectively validate this algorithm at multiple sites to ensure that application of this algorithm improves patient care without causing excess diagnostic testing, thus providing value to patients and the healthcare system as a whole,” Kwan said.
Funding was provided in part by KAKENHI (Japan Society for the Promotion of Science). Kwan reported receiving consulting fees from InVision.
A version of this article first appeared on Medscape.com.
Better Prep, Better Scope: Task Force Updates Colonoscopy Bowel Prep Advice
The latest consensus recommendations emphasize the importance of verbal and written patient education, refine diet restrictions, update optimal purgative regimens, and advise tracking bowel prep adequacy rates at both the individual endoscopist and unit levels.
“Colorectal cancer remains the second most common cause of cancer death in the United States, and colonoscopy is considered the gold standard for evaluating the colon, including assessing causes of colon-related signs or symptoms and the detection of precancerous lesions. It is well recognized that the adequacy of bowel preparation is essential for optimal colonoscopy performance,” the task force wrote.
Choice of Prep, Dosing and Timing, and Dietary Restrictions
When choosing bowel preparation regimens, the task force recommends considering the individual’s medical history, medications, and, when available, the adequacy of bowel preparation reported from prior colonoscopies. Other considerations include patient preference, associated additional costs to the patient, and ease in obtaining and consuming any purgatives or adjuncts.
In terms of timing and dose, the task force now “suggests that lower-volume bowel preparation regimens, such as those that rely on only 2 liters of fluid compared to the traditional 4L, are acceptable options for individuals considered unlikely to have an inadequate bowel preparation. This assumes that the purgative is taken in a split-dose fashion (half the evening prior to colonoscopy and half the morning of the colonoscopy),” co–lead author Brian C. Jacobson, MD, MPH, AGAF, with Massachusetts General Hospital and Harvard Medical School, both in Boston, said in an interview.
The task force also states that a same-day bowel preparation regimen for afternoon, but not morning, colonoscopy is a “reasonable alternative to the now-common split-dose regimen,” Jacobson said.
The group did not find one bowel preparation purgative to be better than others, although table 7 in the document details characteristics of commonly used prep regimens including their side effects and contraindications.
Recommendations regarding dietary modifications depend upon the patient’s risk for inadequate bowel prep. For patients at low risk for inadequate bowel prep, the task force recommends limiting dietary restrictions to the day before a colonoscopy, relying on either clear liquids or low-fiber/low-residue diets for the early and midday meals. Table 5 in the document provides a list of low-residue foods and sample meals.
The task force also suggests the adjunctive use of oral simethicone (≥ 320 mg) to bowel prep as a way to potentially improve visualization, although they acknowledge that further research is needed.
How might these updated consensus recommendations change current clinical practice?
Jacobson said: “Some physicians may try to identify individuals who will do just as well with a more patient-friendly, easily tolerated bowel preparation regimen, including less stringent dietary restrictions leading up to colonoscopy.”
He noted that the task force prefers the term “guidance” to “guidelines.”
New Quality Benchmark
The task force recommends documenting bowel prep quality in the endoscopy report after all washing and suctioning have been completed using reliably understood descriptors that communicate the adequacy of the preparation.
They recommend the term “adequate bowel preparation” be used to indicate that standard screening or surveillance intervals can be assigned based on the findings of the colonoscopy.
Additionally, the task force recommends that endoscopy units and individual endoscopists track and aim for ≥ 90% adequacy rates in bowel preparation — up from the 85% benchmark contained in the prior recommendations.
Jacobson told this news organization it’s “currently unknown” how many individual endoscopists and endoscopy units track and meet the 90% benchmark at present.
David Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, who wasn’t on the task force, said endoscopy units and providers “need to be accountable and should be tracking this quality metric.”
Johnson noted that bowel prep inadequacy has “intrinsic costs,” impacting lesion detection, CRC incidence, and patient outcomes. Inadequate prep leads to “increased risk for morbidity, mortality, longer appointment and wait times for rescheduling, and negative connotations that may deter patients from returning.”
Brian Sullivan, MD, MHS, assistant professor of medicine, division of gastroenterology, Duke University School of Medicine, Durham, North Carolina, who wasn’t on the task force, said the recommendation to target a 90% or higher bowel preparation adequacy rate is “appreciated.”
“This benchmark encourages practices to standardize measurement, tracking, and reporting of preparation quality at both the individual and unit levels. Specifically, it should motivate providers to critically evaluate their interpretation of preparation quality and ensure adequate cleansing before making determinations,” Sullivan said in an interview.
“At the unit level, this metric can identify whether there are opportunities for quality improvement, such as by implementing evidence-based initiatives (provided in the guidance) to enhance outpatient preparation processes,” Sullivan noted.
The task force emphasized that the majority of consensus recommendations focus on individuals at average risk for inadequate bowel prep. Patients at high risk for inadequate bowel prep (eg, diabetes, constipation, opioid use) should receive tailored instructions, including a more extended dietary prep and high-volume purgatives.
‘Timely and Important’ Updates
Sullivan said the updated consensus recommendations on optimizing bowel preparation quality for colonoscopy are both “timely and important.”
“Clear guidance facilitates dissemination and adoption, promoting flexible yet evidence-based approaches that enhance patient and provider satisfaction while potentially improving CRC prevention outcomes. For instance, surveys reveal that some practices still do not utilize split-dose bowel preparation, which is proven to improve preparation quality, particularly for the right-side of the colon. This gap underscores the need for standardized guidance to ensure high-quality colonoscopy and effective CRC screening,” Sullivan said.
He also noted that the inclusion of lower-volume bowel prep regimens and less intensive dietary modifications for selected patients is a “welcome update.”
“These options can improve patient adherence and satisfaction, which are critical not only for the quality of the index exam but also for ensuring patients return for future screenings, thereby supporting long-term CRC prevention efforts,” Sullivan said.
The task force includes representatives from the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy.
The consensus document was published online in the three societies’ respective scientific journals — Gastroenterology, the American Journal of Gastroenterology, and Gastrointestinal Endsocopy.
This research had no financial support. Jacobson is a consultant for Curis and Guardant Health. Sullivan had no disclosures. Johnson is an adviser to ISOThrive and a past president of the American College of Gastroenterology.
A version of this article first appeared on Medscape.com.
The latest consensus recommendations emphasize the importance of verbal and written patient education, refine diet restrictions, update optimal purgative regimens, and advise tracking bowel prep adequacy rates at both the individual endoscopist and unit levels.
“Colorectal cancer remains the second most common cause of cancer death in the United States, and colonoscopy is considered the gold standard for evaluating the colon, including assessing causes of colon-related signs or symptoms and the detection of precancerous lesions. It is well recognized that the adequacy of bowel preparation is essential for optimal colonoscopy performance,” the task force wrote.
Choice of Prep, Dosing and Timing, and Dietary Restrictions
When choosing bowel preparation regimens, the task force recommends considering the individual’s medical history, medications, and, when available, the adequacy of bowel preparation reported from prior colonoscopies. Other considerations include patient preference, associated additional costs to the patient, and ease in obtaining and consuming any purgatives or adjuncts.
In terms of timing and dose, the task force now “suggests that lower-volume bowel preparation regimens, such as those that rely on only 2 liters of fluid compared to the traditional 4L, are acceptable options for individuals considered unlikely to have an inadequate bowel preparation. This assumes that the purgative is taken in a split-dose fashion (half the evening prior to colonoscopy and half the morning of the colonoscopy),” co–lead author Brian C. Jacobson, MD, MPH, AGAF, with Massachusetts General Hospital and Harvard Medical School, both in Boston, said in an interview.
The task force also states that a same-day bowel preparation regimen for afternoon, but not morning, colonoscopy is a “reasonable alternative to the now-common split-dose regimen,” Jacobson said.
The group did not find one bowel preparation purgative to be better than others, although table 7 in the document details characteristics of commonly used prep regimens including their side effects and contraindications.
Recommendations regarding dietary modifications depend upon the patient’s risk for inadequate bowel prep. For patients at low risk for inadequate bowel prep, the task force recommends limiting dietary restrictions to the day before a colonoscopy, relying on either clear liquids or low-fiber/low-residue diets for the early and midday meals. Table 5 in the document provides a list of low-residue foods and sample meals.
The task force also suggests the adjunctive use of oral simethicone (≥ 320 mg) to bowel prep as a way to potentially improve visualization, although they acknowledge that further research is needed.
How might these updated consensus recommendations change current clinical practice?
Jacobson said: “Some physicians may try to identify individuals who will do just as well with a more patient-friendly, easily tolerated bowel preparation regimen, including less stringent dietary restrictions leading up to colonoscopy.”
He noted that the task force prefers the term “guidance” to “guidelines.”
New Quality Benchmark
The task force recommends documenting bowel prep quality in the endoscopy report after all washing and suctioning have been completed using reliably understood descriptors that communicate the adequacy of the preparation.
They recommend the term “adequate bowel preparation” be used to indicate that standard screening or surveillance intervals can be assigned based on the findings of the colonoscopy.
Additionally, the task force recommends that endoscopy units and individual endoscopists track and aim for ≥ 90% adequacy rates in bowel preparation — up from the 85% benchmark contained in the prior recommendations.
Jacobson told this news organization it’s “currently unknown” how many individual endoscopists and endoscopy units track and meet the 90% benchmark at present.
David Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, who wasn’t on the task force, said endoscopy units and providers “need to be accountable and should be tracking this quality metric.”
Johnson noted that bowel prep inadequacy has “intrinsic costs,” impacting lesion detection, CRC incidence, and patient outcomes. Inadequate prep leads to “increased risk for morbidity, mortality, longer appointment and wait times for rescheduling, and negative connotations that may deter patients from returning.”
Brian Sullivan, MD, MHS, assistant professor of medicine, division of gastroenterology, Duke University School of Medicine, Durham, North Carolina, who wasn’t on the task force, said the recommendation to target a 90% or higher bowel preparation adequacy rate is “appreciated.”
“This benchmark encourages practices to standardize measurement, tracking, and reporting of preparation quality at both the individual and unit levels. Specifically, it should motivate providers to critically evaluate their interpretation of preparation quality and ensure adequate cleansing before making determinations,” Sullivan said in an interview.
“At the unit level, this metric can identify whether there are opportunities for quality improvement, such as by implementing evidence-based initiatives (provided in the guidance) to enhance outpatient preparation processes,” Sullivan noted.
The task force emphasized that the majority of consensus recommendations focus on individuals at average risk for inadequate bowel prep. Patients at high risk for inadequate bowel prep (eg, diabetes, constipation, opioid use) should receive tailored instructions, including a more extended dietary prep and high-volume purgatives.
‘Timely and Important’ Updates
Sullivan said the updated consensus recommendations on optimizing bowel preparation quality for colonoscopy are both “timely and important.”
“Clear guidance facilitates dissemination and adoption, promoting flexible yet evidence-based approaches that enhance patient and provider satisfaction while potentially improving CRC prevention outcomes. For instance, surveys reveal that some practices still do not utilize split-dose bowel preparation, which is proven to improve preparation quality, particularly for the right-side of the colon. This gap underscores the need for standardized guidance to ensure high-quality colonoscopy and effective CRC screening,” Sullivan said.
He also noted that the inclusion of lower-volume bowel prep regimens and less intensive dietary modifications for selected patients is a “welcome update.”
“These options can improve patient adherence and satisfaction, which are critical not only for the quality of the index exam but also for ensuring patients return for future screenings, thereby supporting long-term CRC prevention efforts,” Sullivan said.
The task force includes representatives from the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy.
The consensus document was published online in the three societies’ respective scientific journals — Gastroenterology, the American Journal of Gastroenterology, and Gastrointestinal Endsocopy.
This research had no financial support. Jacobson is a consultant for Curis and Guardant Health. Sullivan had no disclosures. Johnson is an adviser to ISOThrive and a past president of the American College of Gastroenterology.
A version of this article first appeared on Medscape.com.
The latest consensus recommendations emphasize the importance of verbal and written patient education, refine diet restrictions, update optimal purgative regimens, and advise tracking bowel prep adequacy rates at both the individual endoscopist and unit levels.
“Colorectal cancer remains the second most common cause of cancer death in the United States, and colonoscopy is considered the gold standard for evaluating the colon, including assessing causes of colon-related signs or symptoms and the detection of precancerous lesions. It is well recognized that the adequacy of bowel preparation is essential for optimal colonoscopy performance,” the task force wrote.
Choice of Prep, Dosing and Timing, and Dietary Restrictions
When choosing bowel preparation regimens, the task force recommends considering the individual’s medical history, medications, and, when available, the adequacy of bowel preparation reported from prior colonoscopies. Other considerations include patient preference, associated additional costs to the patient, and ease in obtaining and consuming any purgatives or adjuncts.
In terms of timing and dose, the task force now “suggests that lower-volume bowel preparation regimens, such as those that rely on only 2 liters of fluid compared to the traditional 4L, are acceptable options for individuals considered unlikely to have an inadequate bowel preparation. This assumes that the purgative is taken in a split-dose fashion (half the evening prior to colonoscopy and half the morning of the colonoscopy),” co–lead author Brian C. Jacobson, MD, MPH, AGAF, with Massachusetts General Hospital and Harvard Medical School, both in Boston, said in an interview.
The task force also states that a same-day bowel preparation regimen for afternoon, but not morning, colonoscopy is a “reasonable alternative to the now-common split-dose regimen,” Jacobson said.
The group did not find one bowel preparation purgative to be better than others, although table 7 in the document details characteristics of commonly used prep regimens including their side effects and contraindications.
Recommendations regarding dietary modifications depend upon the patient’s risk for inadequate bowel prep. For patients at low risk for inadequate bowel prep, the task force recommends limiting dietary restrictions to the day before a colonoscopy, relying on either clear liquids or low-fiber/low-residue diets for the early and midday meals. Table 5 in the document provides a list of low-residue foods and sample meals.
The task force also suggests the adjunctive use of oral simethicone (≥ 320 mg) to bowel prep as a way to potentially improve visualization, although they acknowledge that further research is needed.
How might these updated consensus recommendations change current clinical practice?
Jacobson said: “Some physicians may try to identify individuals who will do just as well with a more patient-friendly, easily tolerated bowel preparation regimen, including less stringent dietary restrictions leading up to colonoscopy.”
He noted that the task force prefers the term “guidance” to “guidelines.”
New Quality Benchmark
The task force recommends documenting bowel prep quality in the endoscopy report after all washing and suctioning have been completed using reliably understood descriptors that communicate the adequacy of the preparation.
They recommend the term “adequate bowel preparation” be used to indicate that standard screening or surveillance intervals can be assigned based on the findings of the colonoscopy.
Additionally, the task force recommends that endoscopy units and individual endoscopists track and aim for ≥ 90% adequacy rates in bowel preparation — up from the 85% benchmark contained in the prior recommendations.
Jacobson told this news organization it’s “currently unknown” how many individual endoscopists and endoscopy units track and meet the 90% benchmark at present.
David Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, who wasn’t on the task force, said endoscopy units and providers “need to be accountable and should be tracking this quality metric.”
Johnson noted that bowel prep inadequacy has “intrinsic costs,” impacting lesion detection, CRC incidence, and patient outcomes. Inadequate prep leads to “increased risk for morbidity, mortality, longer appointment and wait times for rescheduling, and negative connotations that may deter patients from returning.”
Brian Sullivan, MD, MHS, assistant professor of medicine, division of gastroenterology, Duke University School of Medicine, Durham, North Carolina, who wasn’t on the task force, said the recommendation to target a 90% or higher bowel preparation adequacy rate is “appreciated.”
“This benchmark encourages practices to standardize measurement, tracking, and reporting of preparation quality at both the individual and unit levels. Specifically, it should motivate providers to critically evaluate their interpretation of preparation quality and ensure adequate cleansing before making determinations,” Sullivan said in an interview.
“At the unit level, this metric can identify whether there are opportunities for quality improvement, such as by implementing evidence-based initiatives (provided in the guidance) to enhance outpatient preparation processes,” Sullivan noted.
The task force emphasized that the majority of consensus recommendations focus on individuals at average risk for inadequate bowel prep. Patients at high risk for inadequate bowel prep (eg, diabetes, constipation, opioid use) should receive tailored instructions, including a more extended dietary prep and high-volume purgatives.
‘Timely and Important’ Updates
Sullivan said the updated consensus recommendations on optimizing bowel preparation quality for colonoscopy are both “timely and important.”
“Clear guidance facilitates dissemination and adoption, promoting flexible yet evidence-based approaches that enhance patient and provider satisfaction while potentially improving CRC prevention outcomes. For instance, surveys reveal that some practices still do not utilize split-dose bowel preparation, which is proven to improve preparation quality, particularly for the right-side of the colon. This gap underscores the need for standardized guidance to ensure high-quality colonoscopy and effective CRC screening,” Sullivan said.
He also noted that the inclusion of lower-volume bowel prep regimens and less intensive dietary modifications for selected patients is a “welcome update.”
“These options can improve patient adherence and satisfaction, which are critical not only for the quality of the index exam but also for ensuring patients return for future screenings, thereby supporting long-term CRC prevention efforts,” Sullivan said.
The task force includes representatives from the American Gastroenterological Association, the American College of Gastroenterology, and the American Society for Gastrointestinal Endoscopy.
The consensus document was published online in the three societies’ respective scientific journals — Gastroenterology, the American Journal of Gastroenterology, and Gastrointestinal Endsocopy.
This research had no financial support. Jacobson is a consultant for Curis and Guardant Health. Sullivan had no disclosures. Johnson is an adviser to ISOThrive and a past president of the American College of Gastroenterology.
A version of this article first appeared on Medscape.com.
FROM GASTROENTEROLOGY