User login
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk factors for iatrogenic pneumothorax
- Residency acceptance and use of pharmaceutical industry funding
- Early cholecystectomy outcomes for gallstone pancreatitis
- Use of microbial DNA in sepsis
- Adding rifampicin to vancomycin in MRSA pneumonia
- Rate and outcomes of culture-negative severe sepsis
- Rates of surgical comanagement in U.S. hospitals
- Probiotics and rates of ventilator-associated pneumonia
Ultrasound Guidance and Operator Experience Decrease Risk of Pneumothorax Following Thoracentesis
Clinical question: How often does pneumothorax happen following thoracentesis, and what factors are associated with increased risk of this complication?
Background: Procedural complications are an important source of adverse events in the hospital. Iatrogenic pneumothorax after thoracentesis results in increased hospital length of stay, morbidity, and mortality. Large variation exists in reported pneumothorax rates, and little is known about procedure- and patient-specific factors associated with development of this complication.
Study design: Systematic review and meta-analysis.
Setting: Review of 24 MEDLINE-indexed studies from January 1966 to April 2009.
Synopsis: A total of 349 pneumothoraces were reported after 6,605 thoracenteses (overall incidence 6.0%). Chest-tube insertion was required in 34.1% of the cases. Risk for pneumothorax was significantly higher when larger needles or catheters were used compared with needles smaller than 20-gauge (odds ratio 2.5, 95% confidence interval [CI], 1.1-6.0) and after therapeutic thoracentesis compared with diagnostic procedures (OR 2.6, 95% CI, 1.8-3.8).
Procedures requiring two or more needle passes did not significantly increase pneumothorax risk (OR 2.5, 95% CI, 0.3-20.1). In contrast, pneumothorax rates were significantly lower when using ultrasound guidance (OR 0.3, 95% CI, 0.2-0.7) and with experienced operators (3.9% vs. 8.5%, P=0.04).
Examining patient risk factors, pneumothorax rates were similar regardless of effusion size and patient gender. Additionally, rates were similar among non-ICU inpatients, ICU inpatients, and outpatients. Data did show a trend toward increased risk of pneumothorax with mechanical ventilation (OR 4.0, 95% CI, 0.95-16.8), although no study directly compared rates in ICU patients with and without mechanical ventilation.
Bottom line: Ultrasound guidance is a modifiable factor that decreases the risk of post-thoracentesis pneumothorax. Pneumothorax rates are lower when performed by experienced clinicians, providing an important opportunity to reduce procedure-related complications by increasing direct trainee supervision.
Citation: Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332-339.
Pharmaceutical Industry Support Is Common in U.S. Internal-Medicine Residency Programs
Clinical question: What are the current attitudes of program directors regarding pharmaceutical industry support of internal-medicine residency activities? What are the potential associations between program characteristics and acceptance of industry support?
Background: Increasing evidence suggests that interactions with the pharmaceutical industry influence physician attitudes and practices. Recently, the Association of American Medical Colleges (AAMC) proposed that academic medical centers prohibit the acceptance of all gifts and restrict access by pharmaceutical industry representatives.
Study design: Survey of U.S. internal-medicine residency program directors.
Setting: Web-based survey of residency program directors in 388 U.S. internal-medicine residency programs.
Synopsis: Of the 236 program directors responding to the survey, 132 (55.9%) reported accepting some kind of support from the pharmaceutical industry. Support was most commonly provided in the form of food for conferences (90.9%), educational materials (83.3%), office supplies (68.9%), and drug samples (57.6%).
When programs reported accepting pharmaceutical industry support, 67.9% cited a lack of other funding sources as the reason for acceptance. Only 22.7% of programs with a program director who thinks pharmaceutical support is unacceptable actually accepted industry support. The likelihood of accepting support was associated with location in the Southern U.S. and was inversely associated with the three-year rolling American Board of Internal Medicine (ABIM) pass rates (each 1% decrease in the pass rate was associated with a 21% increase in the odds of accepting pharmaceutical industry support).
Bottom line: While most program directors did not find pharmaceutical industry support desirable, more than half reported acceptance of such support, with most citing lack of other funding resources as the reason for acceptance.
Citation: Loertscher LL, Halvorsen AJ, Beasley BW, Holmboe ES, Kolars JC, McDonald FS. Pharmaceutical industry support and residency education: a survey of internal medicine program directors. Arch Intern Med. 2010;170(4):356-362.
Early Cholecystectomy Safely Decreases Hospital Stay in Patients with Mild Gallstone Pancreatitis
Clinical question: Can laparoscopic cholecystectomy performed within 48 hours of admission for mild gallstone pancreatitis reduce hospital length of stay without increasing perioperative complications?
Background: Although there is a clear consensus that patients who present with gallstone pancreatitis should undergo cholecystectomy to prevent recurrence, precise timing of surgery remains controversial.
Study design: Randomized prospective trial.
Setting: Harbor-UCLA Medical Center, a Los Angeles County public teaching hospital and Level I trauma center.
Synopsis: Patients were prospectively randomized to an early group and a control group. Inclusion criteria consisted of adults from the ages of 18 to 100 with mild gallstone pancreatitis and three or fewer Ranson criteria. The primary endpoint was length of hospital stay. The secondary endpoint was a composite of complications, including the need for conversion to open cholecystectomy, readmission within 30 days, bleeding requiring transfusion, bile duct injury, or wound infection.
The study was terminated after 50 patients, as there was a difference in the length of hospital stay with a predefined alpha level of 0.005. Patients in the early group were taken to the operating room at a mean of 35.1 hours after admission, compared with 77.8 hours in the control group. The overall length of hospital stay was shorter in the early group (mean 3.5 days, 95% CI, 2.7-4.3), compared with the control group (mean 5.8, 95% CI, 3.8-7.9). All cholecystectomies were completed laparoscopically, without conversion to open. No statistically significant difference existed in secondary endpoints (P=0.48, OR 1.66, 95% CI, 0.41-6.78).
Bottom line: Laparoscopic cholecystectomy performed within 48 hours of admission, irrespective of normalization of laboratory values or clinical progress, safely decreases the overall length of stay, compared with delaying laparoscopic cholecystectomy until laboratory values and clinical condition normalize.
Citation: Aboulian A, Chan T, Yaghoubian A, et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg. 2010;251(4): 615-619.
Presence of Microbial DNA in Blood Correlates with Disease Severity
Clinical question: Is the presence of microbial DNA in the blood associated with disease severity in severe sepsis, and how does detection of this microbial DNA by polymerase chain reaction (PCR) compare with blood cultures (BC)?
Background: Inadequate antibiotic therapy is a strong and independent predictor of poor outcomes in sepsis. Diagnostic uncertainty regarding the causative micro-organism is compensated for by liberal use of broad-spectrum antibiotics. As a result, resistance to antibiotics is an increasing public-health problem.
Study design: Prospective multicenter controlled observational study.
Setting: Three ICUs in Germany and France.
Synopsis: From 2005 to 2007, 63 patients were enrolled in the control group and 142 patients were enrolled in the sepsis group. In control patients, blood cultures and specimens were drawn daily at a maximum of three days after admission. In the sepsis group, blood samples were obtained on the day severe sepsis was suspected. Consecutive samples for the next two days after study inclusion were taken.
Taking BC as the laboratory comparison method, the sensitivity of PCR to detect culture-positive bacteremia in sepsis was 0.80 with a specificity of 0.77. PCR detected 29 of 41 microorganisms (70.3%) found in the BC. The highest recovery rate was observed for gram-negative bacteria (78.6%), fungi (50.0%), and gram-positive bacteria (47.6%). PCR from septic patients correlated well with markers of host response (IL-6 and PCT) and disease severity (SOFA score), even when the BC remained negative.
The appropriateness of antimicrobial therapy based on culture-based methods was not recorded, so it’s impossible to conclude whether or not the PCR would have contributed to a more effective therapy.
Bottom line: Concordance between BC and PCR is moderate in septic patients. PCR-based pathogen detection correlated with disease severity even if the BC remained negative, suggesting that the presence of microbial DNA in the bloodstream is a clinically significant event.
Citation: Bloos F, Hinder F, Becker K, et al. A multicenter trial to compare blood culture with polymerase chain reaction in severe human sepsis. Intensive Care Med. 2010;36(2):241-247.
Adding Rifampicin to Vancomycin Improves Outcomes in MRSA Pneumonia
Clinical question: Does adding rifampicin to vancomycin improve outcomes in patients with hospital-acquired MRSA pneumonia?
Background: Hospital-acquired MRSA pneumonia has a mortality of more than 20%. Vancomycin penetrates the lung tissue poorly. The value of adding rifampicin, an antibiotic with broad-spectrum coverage and good tissue penetration, was investigated.
Study design: Randomized open-label trial.
Setting: Medical ICU patients at Ulsan College of Medicine, Asan Medical Center, South Korea.
Synopsis: Patients older than 18 years of age with clinical symptoms suggestive of nosocomial pneumonia were randomized to receive vancomycin alone (V) or vancomycin plus rifampicin (VR). Clinicians could add additional antibiotics for gram-negative coverage as needed.
Of the 183 patients screened, 93 met the inclusion criteria and were randomized in a 1:1 ratio. MRSA infection was microbiologically confirmed. Clinical cure rate in VR patients was significantly greater at day 14 compared with the V group (53.7% vs. 31.0%, P=0.047) based on a modified intention-to-treat model. The overall mortality at day 28 did not significantly differ between the groups (22.0% vs. 38.1%, P=0.15), although the 60-day mortality was lower in the VR group (26.8% vs. 50.0%, P=0.042). Mortality from MRSA pneumonia had a trend toward a decrease in the VR group (14.7% vs. 28.6%, P=0.18).
The trial was limited because it was a single-site study and lacked statistical power to assess certain outcomes. Additionally, treatment protocols were not compared with other antimicrobial therapies.
Bottom line: Vancomycin plus rifampicin improves MRSA pneumonia outcomes in ICU patients.
Citation: Jung YJ, Koh Y, Hong SB, et al. Effect of vancomycin plus rifampicin in the treatment of nosocomial MRSA pneumonia. Crit Care Med. 2010;38(1):175-180.
Severe Sepsis Syndromes Are Not Always Caused by Bacteremia
Clinical question: What are the common causes of clinical sepsis?
Background: When sepsis is defined by systemic inflammatory response syndrome (SIRS) criteria, the etiology is not always infectious. Rapid initiation of antimicrobial therapy for infectious SIRS is a priority, but it could result in treating a significant number of patients who are not bacteremic.
Study design: Prospective secondary analysis of a registry of patients created to evaluate an institutional standard-of-care protocol.
Setting: Urban, 850-bed, tertiary-care teaching institution in North Carolina.
Synopsis: ED cases meeting the criteria for severe sepsis underwent a secondary review that looked at the cause of the sepsis. Only 45% of patients identified as having severe sepsis were blood-culture-positive during that episode of care. The culture-positive group was more likely to have central lines, malignancies, or reside in a nursing home.
Of the subgroup of culture-negative patients, 52% had another infectious etiology, most commonly pneumonia. Other “noninfectious mimics,” including inflammatory colitis, myocardial infarction, and pulmonary embolism, were noted in 32% of patients in the subgroup, and the cause was not identified in 16% of the patients.
In-hospital mortality was higher in the culture-positive group than in the culture-negative group (25% vs. 4%, P=0.05). There was no evidence of harm in patients with culture-negative sepsis treated for a systemic infection.
Bottom line: Many patients with a clinical picture of severe sepsis will not have positive blood cultures or an infectious etiology.
Citation: Heffner AC, Horton JM, Marchick MR, Jones AE. Etiology of illness in patients with severe sepsis admitted to the hospital from the emergency department. Clin Infect Dis. 2010;50(6):814-820.
Comanagement of Surgical Inpatients by Hospitalists Is Rapidly Expanding
Clinical question: What is the prevalence and nature of comanagement of surgical patients by medicine physicians?
Background: Comanagement of surgical patients is a common clinical role for hospitalists, but the relationship is not well characterized in the literature in terms of numbers of patients or types of physicians involved in this practice.
Study design: Retrospective cohort.
Setting: Cross-section of hospitals from a Medicare database.
Synopsis: During the study period, 35.2% of patients were comanaged by a medicine physician—23.7% by a generalist and 14% by a subspecialist. Cardiothoracic surgery patients were more likely to be comanaged by a subspecialist, whereas all other patients were more likely to be comanaged by a generalist.
Although subspecialist comanagement actually declined during the study period, overall comanagement increased from 33.3% in 1996 to 40.8% in 2006. This increase is entirely attributable to the increase in comanagement by hospitalists. Most of this growth occurred with orthopedic patients.
Patient factors associated with comanagement include advanced age, emergency admissions, and increasing comorbidities. Teaching hospitals had less comanagement, while midsize, nonteaching, and for-profit hospitals had more comanagement.
Bottom line: Comanagement of surgical patients by medicine physicians is a common and growing clinical relationship. Hospitalists are responsible for increasing numbers of comanaged surgical patients.
Citation: Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368.
Probiotics Might Decrease Risk of Ventilator-Associated Pneumonia
Clinical question: Does the administration of probiotics decrease the incidence of ventilator-associated pneumonia in critically ill patients?
Background: Ventilator-associated pneumonia (VAP) is a major nosocomial infection in ICUs. Probiotics are thought to decrease colonization and, therefore, infection with serious hospital-acquired pathogens.
Study design: Meta-analysis of five randomized controlled trials.
Setting: ICU patients on mechanical ventilation for at least 24 hours.
Synopsis: Five trials met the inclusion criteria of comparing probiotics to placebo in critically ill patients on mechanical ventilation and reporting the outcome of VAP. Administration of probiotics decreased the incidence of VAP (odds ratio 0.61, 95% CI, 0.41-0.91) and colonization of the respiratory tract with Pseudomonas aeruginosa (OR 0.35, 95% CI, 0.13-0.93).
Length of ICU stay was decreased in the probiotic arm, although this effect was not statistically significant in all analyses. Probiotics had no effect on such outcomes as ICU mortality, in-hospital mortality, or duration of mechanical ventilation.
Bottom line: Probiotics might be an effective strategy to reduce the risk of VAP, even if they do not appear to impact such outcomes as mortality.
Citation: Siempos II, Ntaidou TK, Falagas ME. Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Crit Care Med. 2010;38(3):954-962. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk factors for iatrogenic pneumothorax
- Residency acceptance and use of pharmaceutical industry funding
- Early cholecystectomy outcomes for gallstone pancreatitis
- Use of microbial DNA in sepsis
- Adding rifampicin to vancomycin in MRSA pneumonia
- Rate and outcomes of culture-negative severe sepsis
- Rates of surgical comanagement in U.S. hospitals
- Probiotics and rates of ventilator-associated pneumonia
Ultrasound Guidance and Operator Experience Decrease Risk of Pneumothorax Following Thoracentesis
Clinical question: How often does pneumothorax happen following thoracentesis, and what factors are associated with increased risk of this complication?
Background: Procedural complications are an important source of adverse events in the hospital. Iatrogenic pneumothorax after thoracentesis results in increased hospital length of stay, morbidity, and mortality. Large variation exists in reported pneumothorax rates, and little is known about procedure- and patient-specific factors associated with development of this complication.
Study design: Systematic review and meta-analysis.
Setting: Review of 24 MEDLINE-indexed studies from January 1966 to April 2009.
Synopsis: A total of 349 pneumothoraces were reported after 6,605 thoracenteses (overall incidence 6.0%). Chest-tube insertion was required in 34.1% of the cases. Risk for pneumothorax was significantly higher when larger needles or catheters were used compared with needles smaller than 20-gauge (odds ratio 2.5, 95% confidence interval [CI], 1.1-6.0) and after therapeutic thoracentesis compared with diagnostic procedures (OR 2.6, 95% CI, 1.8-3.8).
Procedures requiring two or more needle passes did not significantly increase pneumothorax risk (OR 2.5, 95% CI, 0.3-20.1). In contrast, pneumothorax rates were significantly lower when using ultrasound guidance (OR 0.3, 95% CI, 0.2-0.7) and with experienced operators (3.9% vs. 8.5%, P=0.04).
Examining patient risk factors, pneumothorax rates were similar regardless of effusion size and patient gender. Additionally, rates were similar among non-ICU inpatients, ICU inpatients, and outpatients. Data did show a trend toward increased risk of pneumothorax with mechanical ventilation (OR 4.0, 95% CI, 0.95-16.8), although no study directly compared rates in ICU patients with and without mechanical ventilation.
Bottom line: Ultrasound guidance is a modifiable factor that decreases the risk of post-thoracentesis pneumothorax. Pneumothorax rates are lower when performed by experienced clinicians, providing an important opportunity to reduce procedure-related complications by increasing direct trainee supervision.
Citation: Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332-339.
Pharmaceutical Industry Support Is Common in U.S. Internal-Medicine Residency Programs
Clinical question: What are the current attitudes of program directors regarding pharmaceutical industry support of internal-medicine residency activities? What are the potential associations between program characteristics and acceptance of industry support?
Background: Increasing evidence suggests that interactions with the pharmaceutical industry influence physician attitudes and practices. Recently, the Association of American Medical Colleges (AAMC) proposed that academic medical centers prohibit the acceptance of all gifts and restrict access by pharmaceutical industry representatives.
Study design: Survey of U.S. internal-medicine residency program directors.
Setting: Web-based survey of residency program directors in 388 U.S. internal-medicine residency programs.
Synopsis: Of the 236 program directors responding to the survey, 132 (55.9%) reported accepting some kind of support from the pharmaceutical industry. Support was most commonly provided in the form of food for conferences (90.9%), educational materials (83.3%), office supplies (68.9%), and drug samples (57.6%).
When programs reported accepting pharmaceutical industry support, 67.9% cited a lack of other funding sources as the reason for acceptance. Only 22.7% of programs with a program director who thinks pharmaceutical support is unacceptable actually accepted industry support. The likelihood of accepting support was associated with location in the Southern U.S. and was inversely associated with the three-year rolling American Board of Internal Medicine (ABIM) pass rates (each 1% decrease in the pass rate was associated with a 21% increase in the odds of accepting pharmaceutical industry support).
Bottom line: While most program directors did not find pharmaceutical industry support desirable, more than half reported acceptance of such support, with most citing lack of other funding resources as the reason for acceptance.
Citation: Loertscher LL, Halvorsen AJ, Beasley BW, Holmboe ES, Kolars JC, McDonald FS. Pharmaceutical industry support and residency education: a survey of internal medicine program directors. Arch Intern Med. 2010;170(4):356-362.
Early Cholecystectomy Safely Decreases Hospital Stay in Patients with Mild Gallstone Pancreatitis
Clinical question: Can laparoscopic cholecystectomy performed within 48 hours of admission for mild gallstone pancreatitis reduce hospital length of stay without increasing perioperative complications?
Background: Although there is a clear consensus that patients who present with gallstone pancreatitis should undergo cholecystectomy to prevent recurrence, precise timing of surgery remains controversial.
Study design: Randomized prospective trial.
Setting: Harbor-UCLA Medical Center, a Los Angeles County public teaching hospital and Level I trauma center.
Synopsis: Patients were prospectively randomized to an early group and a control group. Inclusion criteria consisted of adults from the ages of 18 to 100 with mild gallstone pancreatitis and three or fewer Ranson criteria. The primary endpoint was length of hospital stay. The secondary endpoint was a composite of complications, including the need for conversion to open cholecystectomy, readmission within 30 days, bleeding requiring transfusion, bile duct injury, or wound infection.
The study was terminated after 50 patients, as there was a difference in the length of hospital stay with a predefined alpha level of 0.005. Patients in the early group were taken to the operating room at a mean of 35.1 hours after admission, compared with 77.8 hours in the control group. The overall length of hospital stay was shorter in the early group (mean 3.5 days, 95% CI, 2.7-4.3), compared with the control group (mean 5.8, 95% CI, 3.8-7.9). All cholecystectomies were completed laparoscopically, without conversion to open. No statistically significant difference existed in secondary endpoints (P=0.48, OR 1.66, 95% CI, 0.41-6.78).
Bottom line: Laparoscopic cholecystectomy performed within 48 hours of admission, irrespective of normalization of laboratory values or clinical progress, safely decreases the overall length of stay, compared with delaying laparoscopic cholecystectomy until laboratory values and clinical condition normalize.
Citation: Aboulian A, Chan T, Yaghoubian A, et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg. 2010;251(4): 615-619.
Presence of Microbial DNA in Blood Correlates with Disease Severity
Clinical question: Is the presence of microbial DNA in the blood associated with disease severity in severe sepsis, and how does detection of this microbial DNA by polymerase chain reaction (PCR) compare with blood cultures (BC)?
Background: Inadequate antibiotic therapy is a strong and independent predictor of poor outcomes in sepsis. Diagnostic uncertainty regarding the causative micro-organism is compensated for by liberal use of broad-spectrum antibiotics. As a result, resistance to antibiotics is an increasing public-health problem.
Study design: Prospective multicenter controlled observational study.
Setting: Three ICUs in Germany and France.
Synopsis: From 2005 to 2007, 63 patients were enrolled in the control group and 142 patients were enrolled in the sepsis group. In control patients, blood cultures and specimens were drawn daily at a maximum of three days after admission. In the sepsis group, blood samples were obtained on the day severe sepsis was suspected. Consecutive samples for the next two days after study inclusion were taken.
Taking BC as the laboratory comparison method, the sensitivity of PCR to detect culture-positive bacteremia in sepsis was 0.80 with a specificity of 0.77. PCR detected 29 of 41 microorganisms (70.3%) found in the BC. The highest recovery rate was observed for gram-negative bacteria (78.6%), fungi (50.0%), and gram-positive bacteria (47.6%). PCR from septic patients correlated well with markers of host response (IL-6 and PCT) and disease severity (SOFA score), even when the BC remained negative.
The appropriateness of antimicrobial therapy based on culture-based methods was not recorded, so it’s impossible to conclude whether or not the PCR would have contributed to a more effective therapy.
Bottom line: Concordance between BC and PCR is moderate in septic patients. PCR-based pathogen detection correlated with disease severity even if the BC remained negative, suggesting that the presence of microbial DNA in the bloodstream is a clinically significant event.
Citation: Bloos F, Hinder F, Becker K, et al. A multicenter trial to compare blood culture with polymerase chain reaction in severe human sepsis. Intensive Care Med. 2010;36(2):241-247.
Adding Rifampicin to Vancomycin Improves Outcomes in MRSA Pneumonia
Clinical question: Does adding rifampicin to vancomycin improve outcomes in patients with hospital-acquired MRSA pneumonia?
Background: Hospital-acquired MRSA pneumonia has a mortality of more than 20%. Vancomycin penetrates the lung tissue poorly. The value of adding rifampicin, an antibiotic with broad-spectrum coverage and good tissue penetration, was investigated.
Study design: Randomized open-label trial.
Setting: Medical ICU patients at Ulsan College of Medicine, Asan Medical Center, South Korea.
Synopsis: Patients older than 18 years of age with clinical symptoms suggestive of nosocomial pneumonia were randomized to receive vancomycin alone (V) or vancomycin plus rifampicin (VR). Clinicians could add additional antibiotics for gram-negative coverage as needed.
Of the 183 patients screened, 93 met the inclusion criteria and were randomized in a 1:1 ratio. MRSA infection was microbiologically confirmed. Clinical cure rate in VR patients was significantly greater at day 14 compared with the V group (53.7% vs. 31.0%, P=0.047) based on a modified intention-to-treat model. The overall mortality at day 28 did not significantly differ between the groups (22.0% vs. 38.1%, P=0.15), although the 60-day mortality was lower in the VR group (26.8% vs. 50.0%, P=0.042). Mortality from MRSA pneumonia had a trend toward a decrease in the VR group (14.7% vs. 28.6%, P=0.18).
The trial was limited because it was a single-site study and lacked statistical power to assess certain outcomes. Additionally, treatment protocols were not compared with other antimicrobial therapies.
Bottom line: Vancomycin plus rifampicin improves MRSA pneumonia outcomes in ICU patients.
Citation: Jung YJ, Koh Y, Hong SB, et al. Effect of vancomycin plus rifampicin in the treatment of nosocomial MRSA pneumonia. Crit Care Med. 2010;38(1):175-180.
Severe Sepsis Syndromes Are Not Always Caused by Bacteremia
Clinical question: What are the common causes of clinical sepsis?
Background: When sepsis is defined by systemic inflammatory response syndrome (SIRS) criteria, the etiology is not always infectious. Rapid initiation of antimicrobial therapy for infectious SIRS is a priority, but it could result in treating a significant number of patients who are not bacteremic.
Study design: Prospective secondary analysis of a registry of patients created to evaluate an institutional standard-of-care protocol.
Setting: Urban, 850-bed, tertiary-care teaching institution in North Carolina.
Synopsis: ED cases meeting the criteria for severe sepsis underwent a secondary review that looked at the cause of the sepsis. Only 45% of patients identified as having severe sepsis were blood-culture-positive during that episode of care. The culture-positive group was more likely to have central lines, malignancies, or reside in a nursing home.
Of the subgroup of culture-negative patients, 52% had another infectious etiology, most commonly pneumonia. Other “noninfectious mimics,” including inflammatory colitis, myocardial infarction, and pulmonary embolism, were noted in 32% of patients in the subgroup, and the cause was not identified in 16% of the patients.
In-hospital mortality was higher in the culture-positive group than in the culture-negative group (25% vs. 4%, P=0.05). There was no evidence of harm in patients with culture-negative sepsis treated for a systemic infection.
Bottom line: Many patients with a clinical picture of severe sepsis will not have positive blood cultures or an infectious etiology.
Citation: Heffner AC, Horton JM, Marchick MR, Jones AE. Etiology of illness in patients with severe sepsis admitted to the hospital from the emergency department. Clin Infect Dis. 2010;50(6):814-820.
Comanagement of Surgical Inpatients by Hospitalists Is Rapidly Expanding
Clinical question: What is the prevalence and nature of comanagement of surgical patients by medicine physicians?
Background: Comanagement of surgical patients is a common clinical role for hospitalists, but the relationship is not well characterized in the literature in terms of numbers of patients or types of physicians involved in this practice.
Study design: Retrospective cohort.
Setting: Cross-section of hospitals from a Medicare database.
Synopsis: During the study period, 35.2% of patients were comanaged by a medicine physician—23.7% by a generalist and 14% by a subspecialist. Cardiothoracic surgery patients were more likely to be comanaged by a subspecialist, whereas all other patients were more likely to be comanaged by a generalist.
Although subspecialist comanagement actually declined during the study period, overall comanagement increased from 33.3% in 1996 to 40.8% in 2006. This increase is entirely attributable to the increase in comanagement by hospitalists. Most of this growth occurred with orthopedic patients.
Patient factors associated with comanagement include advanced age, emergency admissions, and increasing comorbidities. Teaching hospitals had less comanagement, while midsize, nonteaching, and for-profit hospitals had more comanagement.
Bottom line: Comanagement of surgical patients by medicine physicians is a common and growing clinical relationship. Hospitalists are responsible for increasing numbers of comanaged surgical patients.
Citation: Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368.
Probiotics Might Decrease Risk of Ventilator-Associated Pneumonia
Clinical question: Does the administration of probiotics decrease the incidence of ventilator-associated pneumonia in critically ill patients?
Background: Ventilator-associated pneumonia (VAP) is a major nosocomial infection in ICUs. Probiotics are thought to decrease colonization and, therefore, infection with serious hospital-acquired pathogens.
Study design: Meta-analysis of five randomized controlled trials.
Setting: ICU patients on mechanical ventilation for at least 24 hours.
Synopsis: Five trials met the inclusion criteria of comparing probiotics to placebo in critically ill patients on mechanical ventilation and reporting the outcome of VAP. Administration of probiotics decreased the incidence of VAP (odds ratio 0.61, 95% CI, 0.41-0.91) and colonization of the respiratory tract with Pseudomonas aeruginosa (OR 0.35, 95% CI, 0.13-0.93).
Length of ICU stay was decreased in the probiotic arm, although this effect was not statistically significant in all analyses. Probiotics had no effect on such outcomes as ICU mortality, in-hospital mortality, or duration of mechanical ventilation.
Bottom line: Probiotics might be an effective strategy to reduce the risk of VAP, even if they do not appear to impact such outcomes as mortality.
Citation: Siempos II, Ntaidou TK, Falagas ME. Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Crit Care Med. 2010;38(3):954-962. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Risk factors for iatrogenic pneumothorax
- Residency acceptance and use of pharmaceutical industry funding
- Early cholecystectomy outcomes for gallstone pancreatitis
- Use of microbial DNA in sepsis
- Adding rifampicin to vancomycin in MRSA pneumonia
- Rate and outcomes of culture-negative severe sepsis
- Rates of surgical comanagement in U.S. hospitals
- Probiotics and rates of ventilator-associated pneumonia
Ultrasound Guidance and Operator Experience Decrease Risk of Pneumothorax Following Thoracentesis
Clinical question: How often does pneumothorax happen following thoracentesis, and what factors are associated with increased risk of this complication?
Background: Procedural complications are an important source of adverse events in the hospital. Iatrogenic pneumothorax after thoracentesis results in increased hospital length of stay, morbidity, and mortality. Large variation exists in reported pneumothorax rates, and little is known about procedure- and patient-specific factors associated with development of this complication.
Study design: Systematic review and meta-analysis.
Setting: Review of 24 MEDLINE-indexed studies from January 1966 to April 2009.
Synopsis: A total of 349 pneumothoraces were reported after 6,605 thoracenteses (overall incidence 6.0%). Chest-tube insertion was required in 34.1% of the cases. Risk for pneumothorax was significantly higher when larger needles or catheters were used compared with needles smaller than 20-gauge (odds ratio 2.5, 95% confidence interval [CI], 1.1-6.0) and after therapeutic thoracentesis compared with diagnostic procedures (OR 2.6, 95% CI, 1.8-3.8).
Procedures requiring two or more needle passes did not significantly increase pneumothorax risk (OR 2.5, 95% CI, 0.3-20.1). In contrast, pneumothorax rates were significantly lower when using ultrasound guidance (OR 0.3, 95% CI, 0.2-0.7) and with experienced operators (3.9% vs. 8.5%, P=0.04).
Examining patient risk factors, pneumothorax rates were similar regardless of effusion size and patient gender. Additionally, rates were similar among non-ICU inpatients, ICU inpatients, and outpatients. Data did show a trend toward increased risk of pneumothorax with mechanical ventilation (OR 4.0, 95% CI, 0.95-16.8), although no study directly compared rates in ICU patients with and without mechanical ventilation.
Bottom line: Ultrasound guidance is a modifiable factor that decreases the risk of post-thoracentesis pneumothorax. Pneumothorax rates are lower when performed by experienced clinicians, providing an important opportunity to reduce procedure-related complications by increasing direct trainee supervision.
Citation: Gordon CE, Feller-Kopman D, Balk EM, Smetana GW. Pneumothorax following thoracentesis: a systematic review and meta-analysis. Arch Intern Med. 2010;170(4):332-339.
Pharmaceutical Industry Support Is Common in U.S. Internal-Medicine Residency Programs
Clinical question: What are the current attitudes of program directors regarding pharmaceutical industry support of internal-medicine residency activities? What are the potential associations between program characteristics and acceptance of industry support?
Background: Increasing evidence suggests that interactions with the pharmaceutical industry influence physician attitudes and practices. Recently, the Association of American Medical Colleges (AAMC) proposed that academic medical centers prohibit the acceptance of all gifts and restrict access by pharmaceutical industry representatives.
Study design: Survey of U.S. internal-medicine residency program directors.
Setting: Web-based survey of residency program directors in 388 U.S. internal-medicine residency programs.
Synopsis: Of the 236 program directors responding to the survey, 132 (55.9%) reported accepting some kind of support from the pharmaceutical industry. Support was most commonly provided in the form of food for conferences (90.9%), educational materials (83.3%), office supplies (68.9%), and drug samples (57.6%).
When programs reported accepting pharmaceutical industry support, 67.9% cited a lack of other funding sources as the reason for acceptance. Only 22.7% of programs with a program director who thinks pharmaceutical support is unacceptable actually accepted industry support. The likelihood of accepting support was associated with location in the Southern U.S. and was inversely associated with the three-year rolling American Board of Internal Medicine (ABIM) pass rates (each 1% decrease in the pass rate was associated with a 21% increase in the odds of accepting pharmaceutical industry support).
Bottom line: While most program directors did not find pharmaceutical industry support desirable, more than half reported acceptance of such support, with most citing lack of other funding resources as the reason for acceptance.
Citation: Loertscher LL, Halvorsen AJ, Beasley BW, Holmboe ES, Kolars JC, McDonald FS. Pharmaceutical industry support and residency education: a survey of internal medicine program directors. Arch Intern Med. 2010;170(4):356-362.
Early Cholecystectomy Safely Decreases Hospital Stay in Patients with Mild Gallstone Pancreatitis
Clinical question: Can laparoscopic cholecystectomy performed within 48 hours of admission for mild gallstone pancreatitis reduce hospital length of stay without increasing perioperative complications?
Background: Although there is a clear consensus that patients who present with gallstone pancreatitis should undergo cholecystectomy to prevent recurrence, precise timing of surgery remains controversial.
Study design: Randomized prospective trial.
Setting: Harbor-UCLA Medical Center, a Los Angeles County public teaching hospital and Level I trauma center.
Synopsis: Patients were prospectively randomized to an early group and a control group. Inclusion criteria consisted of adults from the ages of 18 to 100 with mild gallstone pancreatitis and three or fewer Ranson criteria. The primary endpoint was length of hospital stay. The secondary endpoint was a composite of complications, including the need for conversion to open cholecystectomy, readmission within 30 days, bleeding requiring transfusion, bile duct injury, or wound infection.
The study was terminated after 50 patients, as there was a difference in the length of hospital stay with a predefined alpha level of 0.005. Patients in the early group were taken to the operating room at a mean of 35.1 hours after admission, compared with 77.8 hours in the control group. The overall length of hospital stay was shorter in the early group (mean 3.5 days, 95% CI, 2.7-4.3), compared with the control group (mean 5.8, 95% CI, 3.8-7.9). All cholecystectomies were completed laparoscopically, without conversion to open. No statistically significant difference existed in secondary endpoints (P=0.48, OR 1.66, 95% CI, 0.41-6.78).
Bottom line: Laparoscopic cholecystectomy performed within 48 hours of admission, irrespective of normalization of laboratory values or clinical progress, safely decreases the overall length of stay, compared with delaying laparoscopic cholecystectomy until laboratory values and clinical condition normalize.
Citation: Aboulian A, Chan T, Yaghoubian A, et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg. 2010;251(4): 615-619.
Presence of Microbial DNA in Blood Correlates with Disease Severity
Clinical question: Is the presence of microbial DNA in the blood associated with disease severity in severe sepsis, and how does detection of this microbial DNA by polymerase chain reaction (PCR) compare with blood cultures (BC)?
Background: Inadequate antibiotic therapy is a strong and independent predictor of poor outcomes in sepsis. Diagnostic uncertainty regarding the causative micro-organism is compensated for by liberal use of broad-spectrum antibiotics. As a result, resistance to antibiotics is an increasing public-health problem.
Study design: Prospective multicenter controlled observational study.
Setting: Three ICUs in Germany and France.
Synopsis: From 2005 to 2007, 63 patients were enrolled in the control group and 142 patients were enrolled in the sepsis group. In control patients, blood cultures and specimens were drawn daily at a maximum of three days after admission. In the sepsis group, blood samples were obtained on the day severe sepsis was suspected. Consecutive samples for the next two days after study inclusion were taken.
Taking BC as the laboratory comparison method, the sensitivity of PCR to detect culture-positive bacteremia in sepsis was 0.80 with a specificity of 0.77. PCR detected 29 of 41 microorganisms (70.3%) found in the BC. The highest recovery rate was observed for gram-negative bacteria (78.6%), fungi (50.0%), and gram-positive bacteria (47.6%). PCR from septic patients correlated well with markers of host response (IL-6 and PCT) and disease severity (SOFA score), even when the BC remained negative.
The appropriateness of antimicrobial therapy based on culture-based methods was not recorded, so it’s impossible to conclude whether or not the PCR would have contributed to a more effective therapy.
Bottom line: Concordance between BC and PCR is moderate in septic patients. PCR-based pathogen detection correlated with disease severity even if the BC remained negative, suggesting that the presence of microbial DNA in the bloodstream is a clinically significant event.
Citation: Bloos F, Hinder F, Becker K, et al. A multicenter trial to compare blood culture with polymerase chain reaction in severe human sepsis. Intensive Care Med. 2010;36(2):241-247.
Adding Rifampicin to Vancomycin Improves Outcomes in MRSA Pneumonia
Clinical question: Does adding rifampicin to vancomycin improve outcomes in patients with hospital-acquired MRSA pneumonia?
Background: Hospital-acquired MRSA pneumonia has a mortality of more than 20%. Vancomycin penetrates the lung tissue poorly. The value of adding rifampicin, an antibiotic with broad-spectrum coverage and good tissue penetration, was investigated.
Study design: Randomized open-label trial.
Setting: Medical ICU patients at Ulsan College of Medicine, Asan Medical Center, South Korea.
Synopsis: Patients older than 18 years of age with clinical symptoms suggestive of nosocomial pneumonia were randomized to receive vancomycin alone (V) or vancomycin plus rifampicin (VR). Clinicians could add additional antibiotics for gram-negative coverage as needed.
Of the 183 patients screened, 93 met the inclusion criteria and were randomized in a 1:1 ratio. MRSA infection was microbiologically confirmed. Clinical cure rate in VR patients was significantly greater at day 14 compared with the V group (53.7% vs. 31.0%, P=0.047) based on a modified intention-to-treat model. The overall mortality at day 28 did not significantly differ between the groups (22.0% vs. 38.1%, P=0.15), although the 60-day mortality was lower in the VR group (26.8% vs. 50.0%, P=0.042). Mortality from MRSA pneumonia had a trend toward a decrease in the VR group (14.7% vs. 28.6%, P=0.18).
The trial was limited because it was a single-site study and lacked statistical power to assess certain outcomes. Additionally, treatment protocols were not compared with other antimicrobial therapies.
Bottom line: Vancomycin plus rifampicin improves MRSA pneumonia outcomes in ICU patients.
Citation: Jung YJ, Koh Y, Hong SB, et al. Effect of vancomycin plus rifampicin in the treatment of nosocomial MRSA pneumonia. Crit Care Med. 2010;38(1):175-180.
Severe Sepsis Syndromes Are Not Always Caused by Bacteremia
Clinical question: What are the common causes of clinical sepsis?
Background: When sepsis is defined by systemic inflammatory response syndrome (SIRS) criteria, the etiology is not always infectious. Rapid initiation of antimicrobial therapy for infectious SIRS is a priority, but it could result in treating a significant number of patients who are not bacteremic.
Study design: Prospective secondary analysis of a registry of patients created to evaluate an institutional standard-of-care protocol.
Setting: Urban, 850-bed, tertiary-care teaching institution in North Carolina.
Synopsis: ED cases meeting the criteria for severe sepsis underwent a secondary review that looked at the cause of the sepsis. Only 45% of patients identified as having severe sepsis were blood-culture-positive during that episode of care. The culture-positive group was more likely to have central lines, malignancies, or reside in a nursing home.
Of the subgroup of culture-negative patients, 52% had another infectious etiology, most commonly pneumonia. Other “noninfectious mimics,” including inflammatory colitis, myocardial infarction, and pulmonary embolism, were noted in 32% of patients in the subgroup, and the cause was not identified in 16% of the patients.
In-hospital mortality was higher in the culture-positive group than in the culture-negative group (25% vs. 4%, P=0.05). There was no evidence of harm in patients with culture-negative sepsis treated for a systemic infection.
Bottom line: Many patients with a clinical picture of severe sepsis will not have positive blood cultures or an infectious etiology.
Citation: Heffner AC, Horton JM, Marchick MR, Jones AE. Etiology of illness in patients with severe sepsis admitted to the hospital from the emergency department. Clin Infect Dis. 2010;50(6):814-820.
Comanagement of Surgical Inpatients by Hospitalists Is Rapidly Expanding
Clinical question: What is the prevalence and nature of comanagement of surgical patients by medicine physicians?
Background: Comanagement of surgical patients is a common clinical role for hospitalists, but the relationship is not well characterized in the literature in terms of numbers of patients or types of physicians involved in this practice.
Study design: Retrospective cohort.
Setting: Cross-section of hospitals from a Medicare database.
Synopsis: During the study period, 35.2% of patients were comanaged by a medicine physician—23.7% by a generalist and 14% by a subspecialist. Cardiothoracic surgery patients were more likely to be comanaged by a subspecialist, whereas all other patients were more likely to be comanaged by a generalist.
Although subspecialist comanagement actually declined during the study period, overall comanagement increased from 33.3% in 1996 to 40.8% in 2006. This increase is entirely attributable to the increase in comanagement by hospitalists. Most of this growth occurred with orthopedic patients.
Patient factors associated with comanagement include advanced age, emergency admissions, and increasing comorbidities. Teaching hospitals had less comanagement, while midsize, nonteaching, and for-profit hospitals had more comanagement.
Bottom line: Comanagement of surgical patients by medicine physicians is a common and growing clinical relationship. Hospitalists are responsible for increasing numbers of comanaged surgical patients.
Citation: Sharma G, Kuo YF, Freeman J, Zhang DD, Goodwin JS. Comanagement of hospitalized surgical patients by medicine physicians in the United States. Arch Intern Med. 2010;170(4):363-368.
Probiotics Might Decrease Risk of Ventilator-Associated Pneumonia
Clinical question: Does the administration of probiotics decrease the incidence of ventilator-associated pneumonia in critically ill patients?
Background: Ventilator-associated pneumonia (VAP) is a major nosocomial infection in ICUs. Probiotics are thought to decrease colonization and, therefore, infection with serious hospital-acquired pathogens.
Study design: Meta-analysis of five randomized controlled trials.
Setting: ICU patients on mechanical ventilation for at least 24 hours.
Synopsis: Five trials met the inclusion criteria of comparing probiotics to placebo in critically ill patients on mechanical ventilation and reporting the outcome of VAP. Administration of probiotics decreased the incidence of VAP (odds ratio 0.61, 95% CI, 0.41-0.91) and colonization of the respiratory tract with Pseudomonas aeruginosa (OR 0.35, 95% CI, 0.13-0.93).
Length of ICU stay was decreased in the probiotic arm, although this effect was not statistically significant in all analyses. Probiotics had no effect on such outcomes as ICU mortality, in-hospital mortality, or duration of mechanical ventilation.
Bottom line: Probiotics might be an effective strategy to reduce the risk of VAP, even if they do not appear to impact such outcomes as mortality.
Citation: Siempos II, Ntaidou TK, Falagas ME. Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Crit Care Med. 2010;38(3):954-962. TH
How Should Hypertensive Emergencies Be Managed?
Case
A 57-year-old male with hypertension and end-stage renal disease is brought into the ED by his family for evaluation of headache, nausea, blurry vision, and confusion. Blood pressure is 235/130 mmHg. He is somnolent but arousable and oriented only to person; the remainder of his neurologic exam is nonfocal. A fundoscopic exam shows retinal hemorrhages, exudates, and papilledema. How should this patient be managed?
Overview
Hypertension (HTN) is a medical problem that affects an estimated 1 in 3 adults in the U.S. and more than 1 billion people worldwide. The Joint National Committee (JNC) 7 Report defines hypertensive emergency as severe hypertension with evidence of impending or progressive end-organ dysfunction.1 Systolic blood pressure (SBP) in these settings often is >180 mm Hg with diastolic blood pressure (DBP) >120 mm Hg. The JNC 7 Report defines hypertensive urgency as severe HTN without acute end-organ dysfunction. Whereas hypertensive urgencies can be treated with oral antihypertensive agents with close outpatient follow-up, hypertensive emergencies require immediate BP reduction to halt the progression of end-organ damage.
Severe HTN causes shear stress and endothelial injury, leading to activation of the coagulation cascade, fibrinoid necrosis, and tissue ischemia.2 Due to adaptive vascular changes, pre-existing hypertension lowers the probability of a hypertensive emergency developing at a particular BP. The rate of BP rise, rather than the absolute level, determines most end-organ damage.3 In previously normotensive patients, end-organ damage can occur at BPs >160/100 mm Hg; however, organ dysfunction is uncommon in chronically hypertensive individuals, unless BP >220/120 mm Hg.
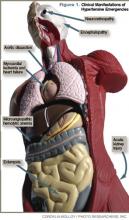
Clinical manifestations of hypertensive emergency depend on the target organs involved (see Figure 1, right). When a patient presents with severe hypertension, a focused evaluation should attempt to identify the presence of end-organ damage. If present, these patients should be admitted to an ICU for close monitoring, and administration of parenteral antihypertensive agents should be started. (Online Exclusive: View a chart of “Parenteral Antihypertensive Agents Used in Hypertensive Emergencies”)
Review of the Data
General principles: The initial therapeutic goal in most hypertensive emergencies is to reduce the mean arterial pressure (MAP) by no more than 25% within the first hour. Precipitous or excessive decreases in BP might worsen renal, cerebral, or coronary ischemia. Due to pressure natriuresis, patients with primary malignant hypertension might be volume-depleted. Restoration of intravascular volume with intravenous (IV) saline can prevent precipitous falls in BP when antihypertensive agents are started.
After the patient stabilizes, the BP can be lowered about 10% per hour to 160/100-110 mm Hg. A gradual reduction to the patient’s baseline BP is targeted over the ensuing 24 to 48 hours. Once there is stable BP control and end-organ damage has ceased, patients can be transitioned to oral therapy.
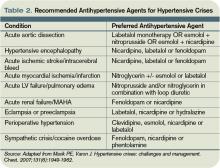
No large clinical trials have investigated optimal drug therapy in patients with hypertensive emergencies. The choice of pharmacologic agent should be individualized based on drug properties, patient comorbidities, and the end-organ(s) involved.
Selected pharmacologic agents: Sodium nitroprusside (SNP) is a short-acting, potent arterial and venous dilator that has been used extensively in the treatment of hypertensive emergencies. Despite its familiarity, there are several important limitations to its use. SNP can increase intracranial pressure (ICP), worsen myocardial ischemia through coronary steal, and is associated with cyanide and/or thiocyanate toxicity. Although used broadly across many types of hypertensive emergencies, SNP should be considered a first-line agent in acute left ventricular (LV) failure and, when combined with beta-blockers, in acute aortic dissection.
Labetalol is an alpha-1 and nonselective beta-blocker that reduces systemic vascular resistance while preserving cerebral, renal, and coronary blood flow. It is considered a first-line agent in most hypertensive emergencies, with the exception of acute LV failure.
Esmolol is a short-acting, selective beta-blocker that decreases heart rate, myocardial contractility, and cardiac output.
Nicardipine is a second-generation dihydropyridine calcium channel blocker. Although it has a longer duration of action, excess hypotension has not been seen in clinical trials comparing it with SNP.4 Nicardipine is used safely in such hypertensive emergencies as hypertensive encephalopathy, cerebral vascular accidents, and postoperatively.
Fenoldopam creates vasodilation by acting on peripheral dopamine type 1 receptors. It improves creatinine clearance and urine output, and is most useful in acute kidney injury.5 It is a well-tolerated and highly effective agent for use in most hypertensive crises, although is expensive and has limited hard outcome data.
Nitroglycerin is a potent venodilator that is used as an adjunct to other anti-hypertensives in the treatment of acute coronary syndromes and acute pulmonary edema.
Immediate-release nifedipine and clonidine are not recommended; they are long-acting and poorly titratable, with unpredictable hypotensive effects.
Hydralazine may be used in LV failure and in pregnancy.
Specific emergencies: Aortic dissection is the most rapidly fatal complication of severe HTN. Untreated, approximately 80% of patients with acute type-A dissections die within two weeks.6 In this specific setting, SBP should be decreased as rapidly as possible to <110 mm Hg in order to halt propagation of the dissection prior to surgery. Therapy should aim to reduce the shear stress on the aortic wall by decreasing both BP and heart rate. This can be accomplished with a combination of esmolol and SNP. Nicardipine and fenoldopam are effective alternatives to SNP. Labetalol is a good single-agent option, provided adequate heart rate suppression is achieved.
LV failure and acute pulmonary edema are associated with high systemic vascular resistance and activation of the Renin Angiotensin Aldosterone (RAAS) system. First-line therapy should consist of arterial vasodilators (e.g., SNP, nicardipine, fenoldopam) in combination with a loop diuretic. Nitroglycerin can be used as an adjunct to reduce LV preload.
In hypertensive encephalopathy, blood pressure exceeds the cerebral autoregulatory threshold, leading to breakthrough vasodilation and the development of cerebral edema. Characteristic symptoms include the insidious onset of headache, nausea, vomiting, and nonlocalizing neurologic signs (e.g., lethargy, confusion, seizures). It is important to exclude stroke, as treatment strategies differ. SNP is used widely in the treatment of hypertensive encephalopathy; it may increase ICP and should be used with caution. Nicardipine and labetalol are effective alternatives with favorable cerebral hemodynamic profiles.
Malignant HTN is characterized by neuroretinopathy: cotton wool spots, flame hemorrhages, and papilledema. Encephalopathy and other evidence of end-organ dysfunction might not be present, although renal disease is common. Preferred drugs are SNP and labetalol, although fenoldopam has been used successfully.
Appropriate BP management following acute ischemic stroke remains controversial. Elevated BP often is a protective physiologic response to maintain cerebral perfusion. The American Heart Association (AHA) recommends initiating IV antihypertensive therapy for thrombolysis candidates when SBP >185 or DBP >110 mm Hg. For those who are not thrombolysis candidates, the recommended threshold for initiating IV antihypertensives is SBP >220 or DBP >120 mm Hg.7 The goal is to lower the BP by 15% to 25% within the first 24 hours. These goals are less aggressive than in patients with hypertensive encephalopathy without stroke.
Spontaneous intracerebral hemorrhage causes a rise in ICP with reflex systemic hypertension. Although a correlation between HTN and hematoma expansion exists, there is no evidence that shows lowering BP is protective. Two clinical trials are evaluating the effects of BP reduction to specified target levels.8 Pending those results, the AHA recommends BP reduction for patients with SBP >200 or MAP >150 mm Hg, or for patients with SBP >180 or MAP >130 mm Hg and evidence of elevated ICP.7 In both ischemic and hemorrhagic stroke, nicardipine and labetalol are appropriate first-line agents.
Most sympathetic crises are related to the recreational use of sympathomimetic drugs, pheochromocytoma, abrupt antihypertensive withdrawal, or concurrent ingestion of monoamine-oxidase inhibitors and tyramine-containing foods. Selective beta-blockers can increase BP and worsen HTN through unopposed alpha effects.
Although labetalol traditionally has been considered the ideal agent—due to its alpha and beta antagonism—studies have failed to support its use in this clinical setting.9 Phentolamine, nicardipine, and fenoldopam are reasonable selections.
Hypertension is common in the early postoperative period following cardiothoracic, vascular, head and neck, and neurosurgical procedures. No consensus exists regarding the treatment of noncardiac surgery patients, but treatment is recommended for BP >140/90 or MAP >105 mmHg in cardiac surgery patients. Nicardipine, clevidipine, and esmolol are proven agents. All three have been shown more effective than SNP in maintaining target BP, and each is associated with less BP variability.10
In patients with pregnancy-induced hypertension, initial therapy for preeclampsia includes magnesium sulfate for seizure prophylaxis and BP control until delivery of the fetus can be safely undertaken. The FDA does not recommend any specific antihypertensive agents; however, ACE inhibitors and SNP are contraindicated. Although hydralazine is used extensively in this setting, a meta-analysis showed increased risk of maternal hypotension, Cesarean section, placental abruptions, and low Apgar scores.11 Labetalol and nicardipine appear to be safe and effective in pregnant hypertensive patients.
Back to the Case
This case represents a classic presentation of malignant hypertension with hypertensive encephalopathy, which is reversible with timely and appropriate management. The patient’s MAP is approximately 165 mmHg, well above the upper threshold of cerebral vascular autoregulation in most patients with chronic hypertension. A brain MRI should be obtained to definitively rule out stroke, as management goals would be considerably different.
If the scan is negative, treatment should be initiated immediately with a goal of reducing the MAP by no more than 25% within the first hour. Nicardipine or labetalol would be appropriate therapeutic choices, administered in an ICU with close hemodynamic monitoring.
Given the patient’s end-stage renal disease and evidence of intracranial hypertension, SNP would be a suboptimal choice. Over hours two through six, BP could be lowered gradually to 160/100, then to his baseline BP over the ensuing 24 to 48 hours, monitoring closely for signs of neurologic deterioration. Once BP is stable and there is no evidence of worsening end-organ damage, he can be safely transitioned to oral agents.
Bottom Line
The therapeutic goal in hypertensive emergencies is to immediately and safely lower BP to halt end-organ damage. Drug selection should be individualized. TH
Dr. Shanahan is a hospitalist and assistant professor at the Denver VA Medical Center. Dr. Linas is professor of medicine in the division of renal diseases and hypertension at the University of Colorado Denver School of Medicine. Dr. Anderson is associate professor and chief of the hospital medicine section at the Denver VA Medical Center.
References
- Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41(6):1178-1179.
- Ault MJ, Ellrodt AG. Pathophysiological events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10-15.
- Vaughan CJ, Delanty N. Hypertensive emergencies. Lancet. 2000;356(9227):411-417.
- Neutel JM, Smith DH, Wallin D, et al. A comparison of intravenous nicardipine and sodium nitroprusside in the immediate treatment of severe hypertension. Am J Hypertens. 1994;7(7 Pt 1):623-628.
- Shusterman NH, Elliott WJ, White WB. Fenoldopam, but not nitroprusside, improves renal function in severely hypertensive patients with impaired renal function. Am J Med. 1993;95(2):161-168.
- Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest. 2002;122(1):311-328.
- Adams HP Jr., del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478-534.
- Qureshi AI. Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH): rationale and design. Neurocrit Care. 2007;6(1):56-66.
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949-1962.
- Aronson S, Dyke CM, Stierer KA, et al. The ECLIPSE trials: comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patients. Anesth Analg. 2008;107(4):1110-1121.
- Magee LA, Cham C, Waterman EJ, Ohlsson A, von Dadelszen P. Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003;327(7421):955-960.
- Aggarwal M, Khan IA. Hypertensive crisis: hypertensive emergencies and urgencies. Cardiol Clin. 2006; 24(1):135-146.
- Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 1. Am J Health Syst Pharm. 2009;66(15):1343-1352.
- Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 2. Am J Health Syst Pharm. 2009;66(16):1448-1457.
- Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs. 2008;68(3):283-297.
Case
A 57-year-old male with hypertension and end-stage renal disease is brought into the ED by his family for evaluation of headache, nausea, blurry vision, and confusion. Blood pressure is 235/130 mmHg. He is somnolent but arousable and oriented only to person; the remainder of his neurologic exam is nonfocal. A fundoscopic exam shows retinal hemorrhages, exudates, and papilledema. How should this patient be managed?
Overview
Hypertension (HTN) is a medical problem that affects an estimated 1 in 3 adults in the U.S. and more than 1 billion people worldwide. The Joint National Committee (JNC) 7 Report defines hypertensive emergency as severe hypertension with evidence of impending or progressive end-organ dysfunction.1 Systolic blood pressure (SBP) in these settings often is >180 mm Hg with diastolic blood pressure (DBP) >120 mm Hg. The JNC 7 Report defines hypertensive urgency as severe HTN without acute end-organ dysfunction. Whereas hypertensive urgencies can be treated with oral antihypertensive agents with close outpatient follow-up, hypertensive emergencies require immediate BP reduction to halt the progression of end-organ damage.
Severe HTN causes shear stress and endothelial injury, leading to activation of the coagulation cascade, fibrinoid necrosis, and tissue ischemia.2 Due to adaptive vascular changes, pre-existing hypertension lowers the probability of a hypertensive emergency developing at a particular BP. The rate of BP rise, rather than the absolute level, determines most end-organ damage.3 In previously normotensive patients, end-organ damage can occur at BPs >160/100 mm Hg; however, organ dysfunction is uncommon in chronically hypertensive individuals, unless BP >220/120 mm Hg.
Clinical manifestations of hypertensive emergency depend on the target organs involved (see Figure 1, right). When a patient presents with severe hypertension, a focused evaluation should attempt to identify the presence of end-organ damage. If present, these patients should be admitted to an ICU for close monitoring, and administration of parenteral antihypertensive agents should be started. (Online Exclusive: View a chart of “Parenteral Antihypertensive Agents Used in Hypertensive Emergencies”)
Review of the Data
General principles: The initial therapeutic goal in most hypertensive emergencies is to reduce the mean arterial pressure (MAP) by no more than 25% within the first hour. Precipitous or excessive decreases in BP might worsen renal, cerebral, or coronary ischemia. Due to pressure natriuresis, patients with primary malignant hypertension might be volume-depleted. Restoration of intravascular volume with intravenous (IV) saline can prevent precipitous falls in BP when antihypertensive agents are started.
After the patient stabilizes, the BP can be lowered about 10% per hour to 160/100-110 mm Hg. A gradual reduction to the patient’s baseline BP is targeted over the ensuing 24 to 48 hours. Once there is stable BP control and end-organ damage has ceased, patients can be transitioned to oral therapy.
No large clinical trials have investigated optimal drug therapy in patients with hypertensive emergencies. The choice of pharmacologic agent should be individualized based on drug properties, patient comorbidities, and the end-organ(s) involved.
Selected pharmacologic agents: Sodium nitroprusside (SNP) is a short-acting, potent arterial and venous dilator that has been used extensively in the treatment of hypertensive emergencies. Despite its familiarity, there are several important limitations to its use. SNP can increase intracranial pressure (ICP), worsen myocardial ischemia through coronary steal, and is associated with cyanide and/or thiocyanate toxicity. Although used broadly across many types of hypertensive emergencies, SNP should be considered a first-line agent in acute left ventricular (LV) failure and, when combined with beta-blockers, in acute aortic dissection.
Labetalol is an alpha-1 and nonselective beta-blocker that reduces systemic vascular resistance while preserving cerebral, renal, and coronary blood flow. It is considered a first-line agent in most hypertensive emergencies, with the exception of acute LV failure.
Esmolol is a short-acting, selective beta-blocker that decreases heart rate, myocardial contractility, and cardiac output.
Nicardipine is a second-generation dihydropyridine calcium channel blocker. Although it has a longer duration of action, excess hypotension has not been seen in clinical trials comparing it with SNP.4 Nicardipine is used safely in such hypertensive emergencies as hypertensive encephalopathy, cerebral vascular accidents, and postoperatively.
Fenoldopam creates vasodilation by acting on peripheral dopamine type 1 receptors. It improves creatinine clearance and urine output, and is most useful in acute kidney injury.5 It is a well-tolerated and highly effective agent for use in most hypertensive crises, although is expensive and has limited hard outcome data.
Nitroglycerin is a potent venodilator that is used as an adjunct to other anti-hypertensives in the treatment of acute coronary syndromes and acute pulmonary edema.
Immediate-release nifedipine and clonidine are not recommended; they are long-acting and poorly titratable, with unpredictable hypotensive effects.
Hydralazine may be used in LV failure and in pregnancy.
Specific emergencies: Aortic dissection is the most rapidly fatal complication of severe HTN. Untreated, approximately 80% of patients with acute type-A dissections die within two weeks.6 In this specific setting, SBP should be decreased as rapidly as possible to <110 mm Hg in order to halt propagation of the dissection prior to surgery. Therapy should aim to reduce the shear stress on the aortic wall by decreasing both BP and heart rate. This can be accomplished with a combination of esmolol and SNP. Nicardipine and fenoldopam are effective alternatives to SNP. Labetalol is a good single-agent option, provided adequate heart rate suppression is achieved.
LV failure and acute pulmonary edema are associated with high systemic vascular resistance and activation of the Renin Angiotensin Aldosterone (RAAS) system. First-line therapy should consist of arterial vasodilators (e.g., SNP, nicardipine, fenoldopam) in combination with a loop diuretic. Nitroglycerin can be used as an adjunct to reduce LV preload.
In hypertensive encephalopathy, blood pressure exceeds the cerebral autoregulatory threshold, leading to breakthrough vasodilation and the development of cerebral edema. Characteristic symptoms include the insidious onset of headache, nausea, vomiting, and nonlocalizing neurologic signs (e.g., lethargy, confusion, seizures). It is important to exclude stroke, as treatment strategies differ. SNP is used widely in the treatment of hypertensive encephalopathy; it may increase ICP and should be used with caution. Nicardipine and labetalol are effective alternatives with favorable cerebral hemodynamic profiles.
Malignant HTN is characterized by neuroretinopathy: cotton wool spots, flame hemorrhages, and papilledema. Encephalopathy and other evidence of end-organ dysfunction might not be present, although renal disease is common. Preferred drugs are SNP and labetalol, although fenoldopam has been used successfully.
Appropriate BP management following acute ischemic stroke remains controversial. Elevated BP often is a protective physiologic response to maintain cerebral perfusion. The American Heart Association (AHA) recommends initiating IV antihypertensive therapy for thrombolysis candidates when SBP >185 or DBP >110 mm Hg. For those who are not thrombolysis candidates, the recommended threshold for initiating IV antihypertensives is SBP >220 or DBP >120 mm Hg.7 The goal is to lower the BP by 15% to 25% within the first 24 hours. These goals are less aggressive than in patients with hypertensive encephalopathy without stroke.
Spontaneous intracerebral hemorrhage causes a rise in ICP with reflex systemic hypertension. Although a correlation between HTN and hematoma expansion exists, there is no evidence that shows lowering BP is protective. Two clinical trials are evaluating the effects of BP reduction to specified target levels.8 Pending those results, the AHA recommends BP reduction for patients with SBP >200 or MAP >150 mm Hg, or for patients with SBP >180 or MAP >130 mm Hg and evidence of elevated ICP.7 In both ischemic and hemorrhagic stroke, nicardipine and labetalol are appropriate first-line agents.
Most sympathetic crises are related to the recreational use of sympathomimetic drugs, pheochromocytoma, abrupt antihypertensive withdrawal, or concurrent ingestion of monoamine-oxidase inhibitors and tyramine-containing foods. Selective beta-blockers can increase BP and worsen HTN through unopposed alpha effects.
Although labetalol traditionally has been considered the ideal agent—due to its alpha and beta antagonism—studies have failed to support its use in this clinical setting.9 Phentolamine, nicardipine, and fenoldopam are reasonable selections.
Hypertension is common in the early postoperative period following cardiothoracic, vascular, head and neck, and neurosurgical procedures. No consensus exists regarding the treatment of noncardiac surgery patients, but treatment is recommended for BP >140/90 or MAP >105 mmHg in cardiac surgery patients. Nicardipine, clevidipine, and esmolol are proven agents. All three have been shown more effective than SNP in maintaining target BP, and each is associated with less BP variability.10
In patients with pregnancy-induced hypertension, initial therapy for preeclampsia includes magnesium sulfate for seizure prophylaxis and BP control until delivery of the fetus can be safely undertaken. The FDA does not recommend any specific antihypertensive agents; however, ACE inhibitors and SNP are contraindicated. Although hydralazine is used extensively in this setting, a meta-analysis showed increased risk of maternal hypotension, Cesarean section, placental abruptions, and low Apgar scores.11 Labetalol and nicardipine appear to be safe and effective in pregnant hypertensive patients.
Back to the Case
This case represents a classic presentation of malignant hypertension with hypertensive encephalopathy, which is reversible with timely and appropriate management. The patient’s MAP is approximately 165 mmHg, well above the upper threshold of cerebral vascular autoregulation in most patients with chronic hypertension. A brain MRI should be obtained to definitively rule out stroke, as management goals would be considerably different.
If the scan is negative, treatment should be initiated immediately with a goal of reducing the MAP by no more than 25% within the first hour. Nicardipine or labetalol would be appropriate therapeutic choices, administered in an ICU with close hemodynamic monitoring.
Given the patient’s end-stage renal disease and evidence of intracranial hypertension, SNP would be a suboptimal choice. Over hours two through six, BP could be lowered gradually to 160/100, then to his baseline BP over the ensuing 24 to 48 hours, monitoring closely for signs of neurologic deterioration. Once BP is stable and there is no evidence of worsening end-organ damage, he can be safely transitioned to oral agents.
Bottom Line
The therapeutic goal in hypertensive emergencies is to immediately and safely lower BP to halt end-organ damage. Drug selection should be individualized. TH
Dr. Shanahan is a hospitalist and assistant professor at the Denver VA Medical Center. Dr. Linas is professor of medicine in the division of renal diseases and hypertension at the University of Colorado Denver School of Medicine. Dr. Anderson is associate professor and chief of the hospital medicine section at the Denver VA Medical Center.
References
- Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41(6):1178-1179.
- Ault MJ, Ellrodt AG. Pathophysiological events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10-15.
- Vaughan CJ, Delanty N. Hypertensive emergencies. Lancet. 2000;356(9227):411-417.
- Neutel JM, Smith DH, Wallin D, et al. A comparison of intravenous nicardipine and sodium nitroprusside in the immediate treatment of severe hypertension. Am J Hypertens. 1994;7(7 Pt 1):623-628.
- Shusterman NH, Elliott WJ, White WB. Fenoldopam, but not nitroprusside, improves renal function in severely hypertensive patients with impaired renal function. Am J Med. 1993;95(2):161-168.
- Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest. 2002;122(1):311-328.
- Adams HP Jr., del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478-534.
- Qureshi AI. Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH): rationale and design. Neurocrit Care. 2007;6(1):56-66.
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949-1962.
- Aronson S, Dyke CM, Stierer KA, et al. The ECLIPSE trials: comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patients. Anesth Analg. 2008;107(4):1110-1121.
- Magee LA, Cham C, Waterman EJ, Ohlsson A, von Dadelszen P. Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003;327(7421):955-960.
- Aggarwal M, Khan IA. Hypertensive crisis: hypertensive emergencies and urgencies. Cardiol Clin. 2006; 24(1):135-146.
- Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 1. Am J Health Syst Pharm. 2009;66(15):1343-1352.
- Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 2. Am J Health Syst Pharm. 2009;66(16):1448-1457.
- Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs. 2008;68(3):283-297.
Case
A 57-year-old male with hypertension and end-stage renal disease is brought into the ED by his family for evaluation of headache, nausea, blurry vision, and confusion. Blood pressure is 235/130 mmHg. He is somnolent but arousable and oriented only to person; the remainder of his neurologic exam is nonfocal. A fundoscopic exam shows retinal hemorrhages, exudates, and papilledema. How should this patient be managed?
Overview
Hypertension (HTN) is a medical problem that affects an estimated 1 in 3 adults in the U.S. and more than 1 billion people worldwide. The Joint National Committee (JNC) 7 Report defines hypertensive emergency as severe hypertension with evidence of impending or progressive end-organ dysfunction.1 Systolic blood pressure (SBP) in these settings often is >180 mm Hg with diastolic blood pressure (DBP) >120 mm Hg. The JNC 7 Report defines hypertensive urgency as severe HTN without acute end-organ dysfunction. Whereas hypertensive urgencies can be treated with oral antihypertensive agents with close outpatient follow-up, hypertensive emergencies require immediate BP reduction to halt the progression of end-organ damage.
Severe HTN causes shear stress and endothelial injury, leading to activation of the coagulation cascade, fibrinoid necrosis, and tissue ischemia.2 Due to adaptive vascular changes, pre-existing hypertension lowers the probability of a hypertensive emergency developing at a particular BP. The rate of BP rise, rather than the absolute level, determines most end-organ damage.3 In previously normotensive patients, end-organ damage can occur at BPs >160/100 mm Hg; however, organ dysfunction is uncommon in chronically hypertensive individuals, unless BP >220/120 mm Hg.
Clinical manifestations of hypertensive emergency depend on the target organs involved (see Figure 1, right). When a patient presents with severe hypertension, a focused evaluation should attempt to identify the presence of end-organ damage. If present, these patients should be admitted to an ICU for close monitoring, and administration of parenteral antihypertensive agents should be started. (Online Exclusive: View a chart of “Parenteral Antihypertensive Agents Used in Hypertensive Emergencies”)
Review of the Data
General principles: The initial therapeutic goal in most hypertensive emergencies is to reduce the mean arterial pressure (MAP) by no more than 25% within the first hour. Precipitous or excessive decreases in BP might worsen renal, cerebral, or coronary ischemia. Due to pressure natriuresis, patients with primary malignant hypertension might be volume-depleted. Restoration of intravascular volume with intravenous (IV) saline can prevent precipitous falls in BP when antihypertensive agents are started.
After the patient stabilizes, the BP can be lowered about 10% per hour to 160/100-110 mm Hg. A gradual reduction to the patient’s baseline BP is targeted over the ensuing 24 to 48 hours. Once there is stable BP control and end-organ damage has ceased, patients can be transitioned to oral therapy.
No large clinical trials have investigated optimal drug therapy in patients with hypertensive emergencies. The choice of pharmacologic agent should be individualized based on drug properties, patient comorbidities, and the end-organ(s) involved.
Selected pharmacologic agents: Sodium nitroprusside (SNP) is a short-acting, potent arterial and venous dilator that has been used extensively in the treatment of hypertensive emergencies. Despite its familiarity, there are several important limitations to its use. SNP can increase intracranial pressure (ICP), worsen myocardial ischemia through coronary steal, and is associated with cyanide and/or thiocyanate toxicity. Although used broadly across many types of hypertensive emergencies, SNP should be considered a first-line agent in acute left ventricular (LV) failure and, when combined with beta-blockers, in acute aortic dissection.
Labetalol is an alpha-1 and nonselective beta-blocker that reduces systemic vascular resistance while preserving cerebral, renal, and coronary blood flow. It is considered a first-line agent in most hypertensive emergencies, with the exception of acute LV failure.
Esmolol is a short-acting, selective beta-blocker that decreases heart rate, myocardial contractility, and cardiac output.
Nicardipine is a second-generation dihydropyridine calcium channel blocker. Although it has a longer duration of action, excess hypotension has not been seen in clinical trials comparing it with SNP.4 Nicardipine is used safely in such hypertensive emergencies as hypertensive encephalopathy, cerebral vascular accidents, and postoperatively.
Fenoldopam creates vasodilation by acting on peripheral dopamine type 1 receptors. It improves creatinine clearance and urine output, and is most useful in acute kidney injury.5 It is a well-tolerated and highly effective agent for use in most hypertensive crises, although is expensive and has limited hard outcome data.
Nitroglycerin is a potent venodilator that is used as an adjunct to other anti-hypertensives in the treatment of acute coronary syndromes and acute pulmonary edema.
Immediate-release nifedipine and clonidine are not recommended; they are long-acting and poorly titratable, with unpredictable hypotensive effects.
Hydralazine may be used in LV failure and in pregnancy.
Specific emergencies: Aortic dissection is the most rapidly fatal complication of severe HTN. Untreated, approximately 80% of patients with acute type-A dissections die within two weeks.6 In this specific setting, SBP should be decreased as rapidly as possible to <110 mm Hg in order to halt propagation of the dissection prior to surgery. Therapy should aim to reduce the shear stress on the aortic wall by decreasing both BP and heart rate. This can be accomplished with a combination of esmolol and SNP. Nicardipine and fenoldopam are effective alternatives to SNP. Labetalol is a good single-agent option, provided adequate heart rate suppression is achieved.
LV failure and acute pulmonary edema are associated with high systemic vascular resistance and activation of the Renin Angiotensin Aldosterone (RAAS) system. First-line therapy should consist of arterial vasodilators (e.g., SNP, nicardipine, fenoldopam) in combination with a loop diuretic. Nitroglycerin can be used as an adjunct to reduce LV preload.
In hypertensive encephalopathy, blood pressure exceeds the cerebral autoregulatory threshold, leading to breakthrough vasodilation and the development of cerebral edema. Characteristic symptoms include the insidious onset of headache, nausea, vomiting, and nonlocalizing neurologic signs (e.g., lethargy, confusion, seizures). It is important to exclude stroke, as treatment strategies differ. SNP is used widely in the treatment of hypertensive encephalopathy; it may increase ICP and should be used with caution. Nicardipine and labetalol are effective alternatives with favorable cerebral hemodynamic profiles.
Malignant HTN is characterized by neuroretinopathy: cotton wool spots, flame hemorrhages, and papilledema. Encephalopathy and other evidence of end-organ dysfunction might not be present, although renal disease is common. Preferred drugs are SNP and labetalol, although fenoldopam has been used successfully.
Appropriate BP management following acute ischemic stroke remains controversial. Elevated BP often is a protective physiologic response to maintain cerebral perfusion. The American Heart Association (AHA) recommends initiating IV antihypertensive therapy for thrombolysis candidates when SBP >185 or DBP >110 mm Hg. For those who are not thrombolysis candidates, the recommended threshold for initiating IV antihypertensives is SBP >220 or DBP >120 mm Hg.7 The goal is to lower the BP by 15% to 25% within the first 24 hours. These goals are less aggressive than in patients with hypertensive encephalopathy without stroke.
Spontaneous intracerebral hemorrhage causes a rise in ICP with reflex systemic hypertension. Although a correlation between HTN and hematoma expansion exists, there is no evidence that shows lowering BP is protective. Two clinical trials are evaluating the effects of BP reduction to specified target levels.8 Pending those results, the AHA recommends BP reduction for patients with SBP >200 or MAP >150 mm Hg, or for patients with SBP >180 or MAP >130 mm Hg and evidence of elevated ICP.7 In both ischemic and hemorrhagic stroke, nicardipine and labetalol are appropriate first-line agents.
Most sympathetic crises are related to the recreational use of sympathomimetic drugs, pheochromocytoma, abrupt antihypertensive withdrawal, or concurrent ingestion of monoamine-oxidase inhibitors and tyramine-containing foods. Selective beta-blockers can increase BP and worsen HTN through unopposed alpha effects.
Although labetalol traditionally has been considered the ideal agent—due to its alpha and beta antagonism—studies have failed to support its use in this clinical setting.9 Phentolamine, nicardipine, and fenoldopam are reasonable selections.
Hypertension is common in the early postoperative period following cardiothoracic, vascular, head and neck, and neurosurgical procedures. No consensus exists regarding the treatment of noncardiac surgery patients, but treatment is recommended for BP >140/90 or MAP >105 mmHg in cardiac surgery patients. Nicardipine, clevidipine, and esmolol are proven agents. All three have been shown more effective than SNP in maintaining target BP, and each is associated with less BP variability.10
In patients with pregnancy-induced hypertension, initial therapy for preeclampsia includes magnesium sulfate for seizure prophylaxis and BP control until delivery of the fetus can be safely undertaken. The FDA does not recommend any specific antihypertensive agents; however, ACE inhibitors and SNP are contraindicated. Although hydralazine is used extensively in this setting, a meta-analysis showed increased risk of maternal hypotension, Cesarean section, placental abruptions, and low Apgar scores.11 Labetalol and nicardipine appear to be safe and effective in pregnant hypertensive patients.
Back to the Case
This case represents a classic presentation of malignant hypertension with hypertensive encephalopathy, which is reversible with timely and appropriate management. The patient’s MAP is approximately 165 mmHg, well above the upper threshold of cerebral vascular autoregulation in most patients with chronic hypertension. A brain MRI should be obtained to definitively rule out stroke, as management goals would be considerably different.
If the scan is negative, treatment should be initiated immediately with a goal of reducing the MAP by no more than 25% within the first hour. Nicardipine or labetalol would be appropriate therapeutic choices, administered in an ICU with close hemodynamic monitoring.
Given the patient’s end-stage renal disease and evidence of intracranial hypertension, SNP would be a suboptimal choice. Over hours two through six, BP could be lowered gradually to 160/100, then to his baseline BP over the ensuing 24 to 48 hours, monitoring closely for signs of neurologic deterioration. Once BP is stable and there is no evidence of worsening end-organ damage, he can be safely transitioned to oral agents.
Bottom Line
The therapeutic goal in hypertensive emergencies is to immediately and safely lower BP to halt end-organ damage. Drug selection should be individualized. TH
Dr. Shanahan is a hospitalist and assistant professor at the Denver VA Medical Center. Dr. Linas is professor of medicine in the division of renal diseases and hypertension at the University of Colorado Denver School of Medicine. Dr. Anderson is associate professor and chief of the hospital medicine section at the Denver VA Medical Center.
References
- Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41(6):1178-1179.
- Ault MJ, Ellrodt AG. Pathophysiological events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10-15.
- Vaughan CJ, Delanty N. Hypertensive emergencies. Lancet. 2000;356(9227):411-417.
- Neutel JM, Smith DH, Wallin D, et al. A comparison of intravenous nicardipine and sodium nitroprusside in the immediate treatment of severe hypertension. Am J Hypertens. 1994;7(7 Pt 1):623-628.
- Shusterman NH, Elliott WJ, White WB. Fenoldopam, but not nitroprusside, improves renal function in severely hypertensive patients with impaired renal function. Am J Med. 1993;95(2):161-168.
- Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest. 2002;122(1):311-328.
- Adams HP Jr., del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478-534.
- Qureshi AI. Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH): rationale and design. Neurocrit Care. 2007;6(1):56-66.
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949-1962.
- Aronson S, Dyke CM, Stierer KA, et al. The ECLIPSE trials: comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patients. Anesth Analg. 2008;107(4):1110-1121.
- Magee LA, Cham C, Waterman EJ, Ohlsson A, von Dadelszen P. Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003;327(7421):955-960.
- Aggarwal M, Khan IA. Hypertensive crisis: hypertensive emergencies and urgencies. Cardiol Clin. 2006; 24(1):135-146.
- Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 1. Am J Health Syst Pharm. 2009;66(15):1343-1352.
- Rhoney D, Peacock WF. Intravenous therapy for hypertensive emergencies, part 2. Am J Health Syst Pharm. 2009;66(16):1448-1457.
- Varon J. Treatment of acute severe hypertension: current and newer agents. Drugs. 2008;68(3):283-297.
Change You Should Believe In
Christina Payne, MD, is a third-year resident at Emory University Hospital in Atlanta who will begin her first hospitalist job, with Emory in September. In spite of her dearth of practical experience, she already has experience researching one of the most vexing problems confronting HM: how to improve transitions of care.
Dr. Payne has been studying the benefits of a structured electronic tool that generates a standardized sign-out list of a hospital team’s full census at the time of shift change, compared with the usual, highly variable sign-out practices of medical residents. At a poster presentation at Internal Medicine 2010 in April in Toronto, Dr. Payne and colleagues reported that residents using the tool were twice as confident at performing handoffs, had lower rates of perceived near-miss events, and were happier.1
“Hospitalists everywhere are starting to realize the importance of trying to reduce opportunities for human error that occur during care transitions,” Dr. Payne says. “The biggest thing I learned from this research is the importance of standardizing the handoff process [with information communicated consistently].
“It is essential to keep communication lines open,” Dr. Payne adds. “No tool can replace the importance of communication between doctors and the need to sit down and talk. The ideal signout happens in a quiet room where the two of you can talk about active patients and achieve rapport. But, realistically, how often does that happen?”
Standardization is one of a handful of strategies hospitalists, researchers, and policymakers are using to tackle transitions—both in-hospital handoffs and post-discharge transitions—with outpatient care. Some hospitalists are using practice simulations and training strategies; others have implemented medication reconciliation checks at every discharge, checklists and other communication strategies, team-based quality-improvement (QI) initiatives, and new technologies to enhance and streamline communication. Some interventions follow the patient from the hospital to the community physician with a phone call, follow-up clinic, or other contact; others aim to empower the patient to be a better self-advocate. But for hospitalists, the challenge is to communicate the right amount of transfer information to the right receiver at the right time.
No matter the technique, the goal is the same: Improve the handoff and discharge process in a way that promotes efficiency and patient safety. And hospitalists are at the forefront of the changing landscape of care transitions.
Under the Microscope
Care transitions of all kinds are under the magnifying glass of national healthcare reform, with growing recognition of the need to make care safer and reduce the preventable, costly hospital readmissions caused by incomplete handoffs. Care transitions for hospitalists include internal handoffs, both at daily shift changes and at service changes when an outgoing provider is leaving after a period of consecutive daily shifts. These typically involve a sign-out process and face-to-face encounter, with some kind of written backup. One teaching institution reported that such handoffs take place 4,000 times per day in the hospital, or 1.6 million times per year.2

—Arpana Vidyarthi, MD, University of California at San Francisco
Geographical transitions can be from one floor or department to another, or out the hospital door to another facility or home. Transitions typically involve a discharge process and a written discharge summary. Care transitions also include hospital admissions, which put the hospitalist in the role of handoff receiver rather than initiator, plus a variety of other transitions involving nurses, physician extenders, and other practitioners.
Each transition is a major decision point in the course of a patient’s hospitalization; each transition also presents a time of heightened vulnerability (e.g., potential communication breakdowns, medication errors, patient anxiety or confusion, etc.). In fact, according to a Transitions of Care Consensus Policy Statement published in 2009 by SHM and five other medical societies, handoffs are ubiquitous in HM, with significant patient safety and quality deficiencies in handoffs existing in the current system.3
Poor communication at the time of handoff has been implicated in near-misses and adverse events in a variety of healthcare contexts, including 70% of hospital sentinel events studied by The Joint Commission, which named standardized handoffs (with an opportunity for interactive communication) as a National Patient Safety Goal in 2006.4 The federal government is studying care transitions, supporting demonstration projects for Medicare enrollees, and including readmission rates in national hospital report card data.
“Transitions of care and handoffs are a huge focus right now because of the increased fragmentation of care in the United States. Hospitalists are in charge of a greater percentage of hospitalized patients, which means more coordination of care is needed,” says Vineet Arora, MD, MA, FHM, assistant professor of medicine and associate director of the internal-medicine residency at the University of Chicago, and chair of the SHM task force on handoffs.
Inadequate communication and poor care transitions can undermine hospitalists’ best care-planning efforts, erode patients’ and families’ confidence and satisfaction with hospital care, and leave primary-care physicians (PCPs) feeling unsatisfied with the relationship. As many as 1 in 5 Medicare beneficiary hospitalizations result in a readmission within 30 days, and while not all of these are preventable, far too many are.5 Another prospective cohort study found that 1 in 5 patients discharged from the hospital to the home experienced an adverse event within three weeks of discharge.6 Complex comorbidities, advanced age, unknown PCP, and limited healthcare literacy present hospitalists with extremely difficult transitions.
Patient safety and cost control are the linchpins to national efforts to improve transitions of care. Dr. Arora recently coauthored an original research paper, which will be published in the Journal of Hospital Medicine in September, showing older hospitalized patients are twice as likely to report problems after discharge if their PCPs were not aware they were hospitalized.
“With escalating healthcare costs, people are looking at ways to save money and reduce redundant care,” Dr. Arora explains, pointing out, as an example, repeated tests resulting from inadequate communication between healthcare providers.
The System Must Change
“All of the effort we put into saving someone’s life—the years of experience, training, medical school, and residency—all of it comes to bear on that hospitalized patient. And it can all be unraveled at the time of discharge if it’s not handled properly,” says Arpana Vidyarthi, MD, a hospitalist and director of quality at the University of California at San Francisco.
Dr. Vidyarthi views in-hospital and discharge transitions as integrally related. “The analysis is similar, even if different techniques may be needed,” she says, adding that, fundamentally, it involves having a system that allows people—or forces them—to do the “right thing.”
That’s why achieving effective care transitions will require more than just a standardized tool or process, Dr. Vidyarthi says. “This is about understanding the ways people communicate and finding ways to train them to communicate better,” she says. “The problem we have is not a lack of information, but how to communicate what, to whom, and when.”
What’s really needed, Dr. Vidyarthi says, is a hospital’s commitment to more effective transitions and its hospitalists’ leadership in driving a comprehensive, multidisciplinary, team- and evidence-based QI process. The new process should be a QI-based solution to a hospital’s care-transitions issues. “Before you can standardize your process, you need to understand it,” she says. “This is a complex problem, and it needs a multifaceted solution. But this lies squarely within the hospitalist arena. We’re part of everything that happens in the hospital.

—Anuj Dalal, MD, Brigham and Women’s Hospital, Boston
Hospital administrators are looking to HM to solve transition and readmission problems now, says Tina Budnitz, MPH, BOOST Project Director (Better Outcomes for Older Adults through Safe Transitions). She expects the scrutiny from the C-suite, legislators, and watchdog groups to increase as the spotlight continues to shine on the healthcare system.
“Any hospitalist can act as a leader in their institution,” Budnitz says. “Be a change agent, pull a group together, and start asking questions: Do we have safe care-transitions practices and processes in place? Just by asking the right question, you can be a catalyst for the system.”
Budnitz also emphasizes the importance of teamwork in the hospital setting. “How can I help my teammates? What am I communicating to the nurses on rounds?” she says. “Can you initiate dialogue with your outpatient medical groups: ‘These faxes we’re sending you—is that information getting to you in ways and times that are helpful? And, by the way, when your patient is admitted, this information would really help me.’ ”
Innovative Strategies
One of the most important initiatives responding to concerns about care transitions is Project BOOST (www.hos pitalmedicine.org/BOOST), a comprehensive toolkit for improving a hospital’s transitions of care. The project aims to build a national consensus for best practices in transitions; collaborate with representatives from the Agency for Healthcare Research and Quality (AHRQ), the Centers for Medicare and Medicaid Services (CMS), and the Joint Commission; and develop a national resource library, Budnitz says.
“Project BOOST not only puts forth best practices for admitting patients, planning for discharge, and then doing the discharge, it also helps show facilities how to change their systems, with resources and tools for analyzing and re-engineering the system,” she says. “Sites get one-to-one assistance from a mentor.”
Six hospitals signed on to the pilot program in 2008; 24 more joined last year. In January, SHM announced a collaborative with the University of Michigan and Blue Cross Blue Shield of Michigan for 15 Michigan hospitals to receive training and mentorship starting in May. And last month, SHM and the California HealthCare Foundation announced a Project BOOST initiative for 20 of the health system’s hospitals (see “California Dreamin’”, p. 6). Other free resources offered on the BOOST Web portal include clinical, data collection, and project management tools. SHM also has a DVD that explains how to use the “teachback” method to improve communication with patients.
Jennifer Myers, MD, FHM, assistant professor of clinical medicine and patient-safety officer at the Hospital of the University of Pennsylvania in Philadelphia, is a Project BOOST participant who spearheaded a process change to improve the quality of her facility’s discharge summary, along with accompanying resident education.7 The discharge summary recently was integrated with the hospital’s electronic health record (EHR) system.
“We’ve gone from dictating the discharge summary to an electronic version completed by the hospitalist, with prompts for key components of the summary, which allows us to create summaries more efficiently—ideally on the day of discharge, but usually within 48 hours,” Dr. Myers says. “We previously researched whether teaching made a difference in the quality of discharges; we found that it did. So we look forward to standardizing our teaching approach around this important topic for all residents.”
Another care-transitions innovation receiving a lot of attention from the government and the private sector is Project RED (Re-Engineered Discharge), led by Brian Jack, MD, vice chair of the department of family medicine at Boston Medical Center. The Project RED research group develops and tests strategies to improve the hospital discharge process to promote patient safety and reduce rehospitalization rates.
“We used re-engineering tools borrowed from other fields, brought together experts from all over the hospital, divided up the whole discharge process, and identified key principles,” Dr. Jack explains. The resulting discharge strategy is reflected in an 11-item checklist of discrete, mutually reinforcing components, which have been shown to reduce rehospitalization rates by 32% while raising patient satisfaction.8 It includes comprehensive discharge and after-hospital plans, a nurse discharge advocate, and a medication reconciliation phone call to the patient. A virtual “patient advocate,” a computerized avatar named Louise, is now being tested. If successful, it will allow patients to interact with a touch-screen teacher of the after-care plan who has time to work at the patient’s pace.
Technology and Transitions
Informatics can be a key player in facilitating care transitions, says Anuj Dalal, MD, a hospitalist and instructor in medicine at Brigham and Women’s Hospital in Boston. He is using one of his hospital’s technological strengths—a well-established, firewall-protected e-mail system—to help improve the discharge process.
“We decided to try to improve awareness of test results pending at the time of discharge,” Dr. Dalal explains. “We created an intervention that automatically triggers an e-mail with the finalized test results to the responsible providers. The intervention creates a loop of communication between the inpatient attending and the PCP. What we hope to show in our research over the next year or two is whether the intervention actually increases awareness of test results by providers.”
One thing to remember is that “all kinds of things can go wrong with care transitions,” no matter the size of the institution, the experience of the staff, or technological limitations, says Vineet Chopra, MD, FACP, a hospitalist at the University of Michigan Health System in Ann Arbor. “The problems of transitions vary from place to place, day to day, time of day, shift changes; and let’s not forget physician extenders and the other members of the healthcare team,” he says. “The more complicated the team, the more complicated the information needing to be handed off becomes.”
Before he joined the group at the university, Dr. Chopra worked at a community hospital, St. Joseph’s Mercy Hospital in Hot Springs, Ark. “It’s hard to come up with a one-size-fits-all solution when there are so many variables,” he says. At the community hospital, “we mandated that the hospitalist call the PCP at the time of discharge. At the academic medical center, we share an EHR with the PCPs and can reach them electronically. We are required to have the discharge summary in the computer before the patient leaves the hospital, and we mandate that hospitalists are reachable by e-mail or phone when they are off.
“I’m not a believer in throwing more technology at problems and just adding more layers of information tools,” Dr. Chopra adds. “Hospitalists who used to carry stethoscopes now also have a clipboard, phone, pager, PDA, and nine different signouts in their pockets. What we want to do is make their life easier. Here, we are looking at technology as a means to do that.”
Dr. Chopra and hospitalist colleague Prasanth Gosineni, MD, have been working with an Ann Arbor tech company called Synaptin to develop a lightweight, mobile client application designed to work on smartphones. Still in pilot testing, it would allow for task-oriented and priority-based messaging in real time and the systematic transfer of important information for the next hospitalist shift.
“You need to be able to share information in a systematic way, but that’s only half of the answer. The other half is the ability to ask specific questions,” Dr. Chopra says. “Technology doesn’t take away from the face-to-face encounter that needs to happen. Nothing will replace face time, but part of the solution is to provide data efficiently and in a way that is easily accessible.”
Dr. Chopra admits that EHR presents both positives and negatives to improved transitions and patient care, “depending on how well it works and what smart features it offers,” he says, “but also recognizing that EHR and other technologies have also taken us farther away from face-to-face exchanges. Some would say that’s part of the problem.”
Handoffs, discharges, and other transitions are ubiquitous in HM—and fraught with the potential for costly and harmful errors. The ideal of an interactive, face-to-face handoff simply is not available for many care transitions. However, hospitalists are challenged to find solutions that will work in their hospitals, with their teams, and their types of patients. Patients and policymakers expect nothing less. TH
Larry Beresford is a freelance writer based in Oakland, Calif.
References
- Payne C, Stein J, Dressler D. Implementation of a structured electronic tool to improve patient handoffs and resident satisfaction. Poster abstract: Internal Medicine 2010, April 21-24, 2010, Toronto.
- Vidyarthi AR. Triple Handoff. AHRQ WebM&M website. Available at: webmm.ahrq.gov/case.aspx? caseID=134. Published May 2006. Accessed May 29, 2010.
- Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364-370.
- 2006 National Patient Safety Goals. The Joint Commission website. Available at: www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsgs.htm. Accessed June 8, 2010.
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 2:360:1418-1428.
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167.
- Myers JS, Jaipaul CK, Kogan JR, Krekun S, Bellini LM, Shea JA. Are discharge summaries teachable? The effects of a discharge summary curriculum on the quality of discharge summaries in an internal medicine residency program. Acad Med. 2006; 81(10):S5-S8.
- Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187.
- Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7): 433-440.
- Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354-360.
- Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Int Med. 2006;166(5):565-571.
- Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B): 26S-30S.
Christina Payne, MD, is a third-year resident at Emory University Hospital in Atlanta who will begin her first hospitalist job, with Emory in September. In spite of her dearth of practical experience, she already has experience researching one of the most vexing problems confronting HM: how to improve transitions of care.
Dr. Payne has been studying the benefits of a structured electronic tool that generates a standardized sign-out list of a hospital team’s full census at the time of shift change, compared with the usual, highly variable sign-out practices of medical residents. At a poster presentation at Internal Medicine 2010 in April in Toronto, Dr. Payne and colleagues reported that residents using the tool were twice as confident at performing handoffs, had lower rates of perceived near-miss events, and were happier.1
“Hospitalists everywhere are starting to realize the importance of trying to reduce opportunities for human error that occur during care transitions,” Dr. Payne says. “The biggest thing I learned from this research is the importance of standardizing the handoff process [with information communicated consistently].
“It is essential to keep communication lines open,” Dr. Payne adds. “No tool can replace the importance of communication between doctors and the need to sit down and talk. The ideal signout happens in a quiet room where the two of you can talk about active patients and achieve rapport. But, realistically, how often does that happen?”
Standardization is one of a handful of strategies hospitalists, researchers, and policymakers are using to tackle transitions—both in-hospital handoffs and post-discharge transitions—with outpatient care. Some hospitalists are using practice simulations and training strategies; others have implemented medication reconciliation checks at every discharge, checklists and other communication strategies, team-based quality-improvement (QI) initiatives, and new technologies to enhance and streamline communication. Some interventions follow the patient from the hospital to the community physician with a phone call, follow-up clinic, or other contact; others aim to empower the patient to be a better self-advocate. But for hospitalists, the challenge is to communicate the right amount of transfer information to the right receiver at the right time.
No matter the technique, the goal is the same: Improve the handoff and discharge process in a way that promotes efficiency and patient safety. And hospitalists are at the forefront of the changing landscape of care transitions.
Under the Microscope
Care transitions of all kinds are under the magnifying glass of national healthcare reform, with growing recognition of the need to make care safer and reduce the preventable, costly hospital readmissions caused by incomplete handoffs. Care transitions for hospitalists include internal handoffs, both at daily shift changes and at service changes when an outgoing provider is leaving after a period of consecutive daily shifts. These typically involve a sign-out process and face-to-face encounter, with some kind of written backup. One teaching institution reported that such handoffs take place 4,000 times per day in the hospital, or 1.6 million times per year.2

—Arpana Vidyarthi, MD, University of California at San Francisco
Geographical transitions can be from one floor or department to another, or out the hospital door to another facility or home. Transitions typically involve a discharge process and a written discharge summary. Care transitions also include hospital admissions, which put the hospitalist in the role of handoff receiver rather than initiator, plus a variety of other transitions involving nurses, physician extenders, and other practitioners.
Each transition is a major decision point in the course of a patient’s hospitalization; each transition also presents a time of heightened vulnerability (e.g., potential communication breakdowns, medication errors, patient anxiety or confusion, etc.). In fact, according to a Transitions of Care Consensus Policy Statement published in 2009 by SHM and five other medical societies, handoffs are ubiquitous in HM, with significant patient safety and quality deficiencies in handoffs existing in the current system.3
Poor communication at the time of handoff has been implicated in near-misses and adverse events in a variety of healthcare contexts, including 70% of hospital sentinel events studied by The Joint Commission, which named standardized handoffs (with an opportunity for interactive communication) as a National Patient Safety Goal in 2006.4 The federal government is studying care transitions, supporting demonstration projects for Medicare enrollees, and including readmission rates in national hospital report card data.
“Transitions of care and handoffs are a huge focus right now because of the increased fragmentation of care in the United States. Hospitalists are in charge of a greater percentage of hospitalized patients, which means more coordination of care is needed,” says Vineet Arora, MD, MA, FHM, assistant professor of medicine and associate director of the internal-medicine residency at the University of Chicago, and chair of the SHM task force on handoffs.
Inadequate communication and poor care transitions can undermine hospitalists’ best care-planning efforts, erode patients’ and families’ confidence and satisfaction with hospital care, and leave primary-care physicians (PCPs) feeling unsatisfied with the relationship. As many as 1 in 5 Medicare beneficiary hospitalizations result in a readmission within 30 days, and while not all of these are preventable, far too many are.5 Another prospective cohort study found that 1 in 5 patients discharged from the hospital to the home experienced an adverse event within three weeks of discharge.6 Complex comorbidities, advanced age, unknown PCP, and limited healthcare literacy present hospitalists with extremely difficult transitions.
Patient safety and cost control are the linchpins to national efforts to improve transitions of care. Dr. Arora recently coauthored an original research paper, which will be published in the Journal of Hospital Medicine in September, showing older hospitalized patients are twice as likely to report problems after discharge if their PCPs were not aware they were hospitalized.
“With escalating healthcare costs, people are looking at ways to save money and reduce redundant care,” Dr. Arora explains, pointing out, as an example, repeated tests resulting from inadequate communication between healthcare providers.
The System Must Change
“All of the effort we put into saving someone’s life—the years of experience, training, medical school, and residency—all of it comes to bear on that hospitalized patient. And it can all be unraveled at the time of discharge if it’s not handled properly,” says Arpana Vidyarthi, MD, a hospitalist and director of quality at the University of California at San Francisco.
Dr. Vidyarthi views in-hospital and discharge transitions as integrally related. “The analysis is similar, even if different techniques may be needed,” she says, adding that, fundamentally, it involves having a system that allows people—or forces them—to do the “right thing.”
That’s why achieving effective care transitions will require more than just a standardized tool or process, Dr. Vidyarthi says. “This is about understanding the ways people communicate and finding ways to train them to communicate better,” she says. “The problem we have is not a lack of information, but how to communicate what, to whom, and when.”
What’s really needed, Dr. Vidyarthi says, is a hospital’s commitment to more effective transitions and its hospitalists’ leadership in driving a comprehensive, multidisciplinary, team- and evidence-based QI process. The new process should be a QI-based solution to a hospital’s care-transitions issues. “Before you can standardize your process, you need to understand it,” she says. “This is a complex problem, and it needs a multifaceted solution. But this lies squarely within the hospitalist arena. We’re part of everything that happens in the hospital.

—Anuj Dalal, MD, Brigham and Women’s Hospital, Boston
Hospital administrators are looking to HM to solve transition and readmission problems now, says Tina Budnitz, MPH, BOOST Project Director (Better Outcomes for Older Adults through Safe Transitions). She expects the scrutiny from the C-suite, legislators, and watchdog groups to increase as the spotlight continues to shine on the healthcare system.
“Any hospitalist can act as a leader in their institution,” Budnitz says. “Be a change agent, pull a group together, and start asking questions: Do we have safe care-transitions practices and processes in place? Just by asking the right question, you can be a catalyst for the system.”
Budnitz also emphasizes the importance of teamwork in the hospital setting. “How can I help my teammates? What am I communicating to the nurses on rounds?” she says. “Can you initiate dialogue with your outpatient medical groups: ‘These faxes we’re sending you—is that information getting to you in ways and times that are helpful? And, by the way, when your patient is admitted, this information would really help me.’ ”
Innovative Strategies
One of the most important initiatives responding to concerns about care transitions is Project BOOST (www.hos pitalmedicine.org/BOOST), a comprehensive toolkit for improving a hospital’s transitions of care. The project aims to build a national consensus for best practices in transitions; collaborate with representatives from the Agency for Healthcare Research and Quality (AHRQ), the Centers for Medicare and Medicaid Services (CMS), and the Joint Commission; and develop a national resource library, Budnitz says.
“Project BOOST not only puts forth best practices for admitting patients, planning for discharge, and then doing the discharge, it also helps show facilities how to change their systems, with resources and tools for analyzing and re-engineering the system,” she says. “Sites get one-to-one assistance from a mentor.”
Six hospitals signed on to the pilot program in 2008; 24 more joined last year. In January, SHM announced a collaborative with the University of Michigan and Blue Cross Blue Shield of Michigan for 15 Michigan hospitals to receive training and mentorship starting in May. And last month, SHM and the California HealthCare Foundation announced a Project BOOST initiative for 20 of the health system’s hospitals (see “California Dreamin’”, p. 6). Other free resources offered on the BOOST Web portal include clinical, data collection, and project management tools. SHM also has a DVD that explains how to use the “teachback” method to improve communication with patients.
Jennifer Myers, MD, FHM, assistant professor of clinical medicine and patient-safety officer at the Hospital of the University of Pennsylvania in Philadelphia, is a Project BOOST participant who spearheaded a process change to improve the quality of her facility’s discharge summary, along with accompanying resident education.7 The discharge summary recently was integrated with the hospital’s electronic health record (EHR) system.
“We’ve gone from dictating the discharge summary to an electronic version completed by the hospitalist, with prompts for key components of the summary, which allows us to create summaries more efficiently—ideally on the day of discharge, but usually within 48 hours,” Dr. Myers says. “We previously researched whether teaching made a difference in the quality of discharges; we found that it did. So we look forward to standardizing our teaching approach around this important topic for all residents.”
Another care-transitions innovation receiving a lot of attention from the government and the private sector is Project RED (Re-Engineered Discharge), led by Brian Jack, MD, vice chair of the department of family medicine at Boston Medical Center. The Project RED research group develops and tests strategies to improve the hospital discharge process to promote patient safety and reduce rehospitalization rates.
“We used re-engineering tools borrowed from other fields, brought together experts from all over the hospital, divided up the whole discharge process, and identified key principles,” Dr. Jack explains. The resulting discharge strategy is reflected in an 11-item checklist of discrete, mutually reinforcing components, which have been shown to reduce rehospitalization rates by 32% while raising patient satisfaction.8 It includes comprehensive discharge and after-hospital plans, a nurse discharge advocate, and a medication reconciliation phone call to the patient. A virtual “patient advocate,” a computerized avatar named Louise, is now being tested. If successful, it will allow patients to interact with a touch-screen teacher of the after-care plan who has time to work at the patient’s pace.
Technology and Transitions
Informatics can be a key player in facilitating care transitions, says Anuj Dalal, MD, a hospitalist and instructor in medicine at Brigham and Women’s Hospital in Boston. He is using one of his hospital’s technological strengths—a well-established, firewall-protected e-mail system—to help improve the discharge process.
“We decided to try to improve awareness of test results pending at the time of discharge,” Dr. Dalal explains. “We created an intervention that automatically triggers an e-mail with the finalized test results to the responsible providers. The intervention creates a loop of communication between the inpatient attending and the PCP. What we hope to show in our research over the next year or two is whether the intervention actually increases awareness of test results by providers.”
One thing to remember is that “all kinds of things can go wrong with care transitions,” no matter the size of the institution, the experience of the staff, or technological limitations, says Vineet Chopra, MD, FACP, a hospitalist at the University of Michigan Health System in Ann Arbor. “The problems of transitions vary from place to place, day to day, time of day, shift changes; and let’s not forget physician extenders and the other members of the healthcare team,” he says. “The more complicated the team, the more complicated the information needing to be handed off becomes.”
Before he joined the group at the university, Dr. Chopra worked at a community hospital, St. Joseph’s Mercy Hospital in Hot Springs, Ark. “It’s hard to come up with a one-size-fits-all solution when there are so many variables,” he says. At the community hospital, “we mandated that the hospitalist call the PCP at the time of discharge. At the academic medical center, we share an EHR with the PCPs and can reach them electronically. We are required to have the discharge summary in the computer before the patient leaves the hospital, and we mandate that hospitalists are reachable by e-mail or phone when they are off.
“I’m not a believer in throwing more technology at problems and just adding more layers of information tools,” Dr. Chopra adds. “Hospitalists who used to carry stethoscopes now also have a clipboard, phone, pager, PDA, and nine different signouts in their pockets. What we want to do is make their life easier. Here, we are looking at technology as a means to do that.”
Dr. Chopra and hospitalist colleague Prasanth Gosineni, MD, have been working with an Ann Arbor tech company called Synaptin to develop a lightweight, mobile client application designed to work on smartphones. Still in pilot testing, it would allow for task-oriented and priority-based messaging in real time and the systematic transfer of important information for the next hospitalist shift.
“You need to be able to share information in a systematic way, but that’s only half of the answer. The other half is the ability to ask specific questions,” Dr. Chopra says. “Technology doesn’t take away from the face-to-face encounter that needs to happen. Nothing will replace face time, but part of the solution is to provide data efficiently and in a way that is easily accessible.”
Dr. Chopra admits that EHR presents both positives and negatives to improved transitions and patient care, “depending on how well it works and what smart features it offers,” he says, “but also recognizing that EHR and other technologies have also taken us farther away from face-to-face exchanges. Some would say that’s part of the problem.”
Handoffs, discharges, and other transitions are ubiquitous in HM—and fraught with the potential for costly and harmful errors. The ideal of an interactive, face-to-face handoff simply is not available for many care transitions. However, hospitalists are challenged to find solutions that will work in their hospitals, with their teams, and their types of patients. Patients and policymakers expect nothing less. TH
Larry Beresford is a freelance writer based in Oakland, Calif.
References
- Payne C, Stein J, Dressler D. Implementation of a structured electronic tool to improve patient handoffs and resident satisfaction. Poster abstract: Internal Medicine 2010, April 21-24, 2010, Toronto.
- Vidyarthi AR. Triple Handoff. AHRQ WebM&M website. Available at: webmm.ahrq.gov/case.aspx? caseID=134. Published May 2006. Accessed May 29, 2010.
- Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364-370.
- 2006 National Patient Safety Goals. The Joint Commission website. Available at: www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsgs.htm. Accessed June 8, 2010.
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 2:360:1418-1428.
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167.
- Myers JS, Jaipaul CK, Kogan JR, Krekun S, Bellini LM, Shea JA. Are discharge summaries teachable? The effects of a discharge summary curriculum on the quality of discharge summaries in an internal medicine residency program. Acad Med. 2006; 81(10):S5-S8.
- Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187.
- Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7): 433-440.
- Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354-360.
- Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Int Med. 2006;166(5):565-571.
- Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B): 26S-30S.
Christina Payne, MD, is a third-year resident at Emory University Hospital in Atlanta who will begin her first hospitalist job, with Emory in September. In spite of her dearth of practical experience, she already has experience researching one of the most vexing problems confronting HM: how to improve transitions of care.
Dr. Payne has been studying the benefits of a structured electronic tool that generates a standardized sign-out list of a hospital team’s full census at the time of shift change, compared with the usual, highly variable sign-out practices of medical residents. At a poster presentation at Internal Medicine 2010 in April in Toronto, Dr. Payne and colleagues reported that residents using the tool were twice as confident at performing handoffs, had lower rates of perceived near-miss events, and were happier.1
“Hospitalists everywhere are starting to realize the importance of trying to reduce opportunities for human error that occur during care transitions,” Dr. Payne says. “The biggest thing I learned from this research is the importance of standardizing the handoff process [with information communicated consistently].
“It is essential to keep communication lines open,” Dr. Payne adds. “No tool can replace the importance of communication between doctors and the need to sit down and talk. The ideal signout happens in a quiet room where the two of you can talk about active patients and achieve rapport. But, realistically, how often does that happen?”
Standardization is one of a handful of strategies hospitalists, researchers, and policymakers are using to tackle transitions—both in-hospital handoffs and post-discharge transitions—with outpatient care. Some hospitalists are using practice simulations and training strategies; others have implemented medication reconciliation checks at every discharge, checklists and other communication strategies, team-based quality-improvement (QI) initiatives, and new technologies to enhance and streamline communication. Some interventions follow the patient from the hospital to the community physician with a phone call, follow-up clinic, or other contact; others aim to empower the patient to be a better self-advocate. But for hospitalists, the challenge is to communicate the right amount of transfer information to the right receiver at the right time.
No matter the technique, the goal is the same: Improve the handoff and discharge process in a way that promotes efficiency and patient safety. And hospitalists are at the forefront of the changing landscape of care transitions.
Under the Microscope
Care transitions of all kinds are under the magnifying glass of national healthcare reform, with growing recognition of the need to make care safer and reduce the preventable, costly hospital readmissions caused by incomplete handoffs. Care transitions for hospitalists include internal handoffs, both at daily shift changes and at service changes when an outgoing provider is leaving after a period of consecutive daily shifts. These typically involve a sign-out process and face-to-face encounter, with some kind of written backup. One teaching institution reported that such handoffs take place 4,000 times per day in the hospital, or 1.6 million times per year.2

—Arpana Vidyarthi, MD, University of California at San Francisco
Geographical transitions can be from one floor or department to another, or out the hospital door to another facility or home. Transitions typically involve a discharge process and a written discharge summary. Care transitions also include hospital admissions, which put the hospitalist in the role of handoff receiver rather than initiator, plus a variety of other transitions involving nurses, physician extenders, and other practitioners.
Each transition is a major decision point in the course of a patient’s hospitalization; each transition also presents a time of heightened vulnerability (e.g., potential communication breakdowns, medication errors, patient anxiety or confusion, etc.). In fact, according to a Transitions of Care Consensus Policy Statement published in 2009 by SHM and five other medical societies, handoffs are ubiquitous in HM, with significant patient safety and quality deficiencies in handoffs existing in the current system.3
Poor communication at the time of handoff has been implicated in near-misses and adverse events in a variety of healthcare contexts, including 70% of hospital sentinel events studied by The Joint Commission, which named standardized handoffs (with an opportunity for interactive communication) as a National Patient Safety Goal in 2006.4 The federal government is studying care transitions, supporting demonstration projects for Medicare enrollees, and including readmission rates in national hospital report card data.
“Transitions of care and handoffs are a huge focus right now because of the increased fragmentation of care in the United States. Hospitalists are in charge of a greater percentage of hospitalized patients, which means more coordination of care is needed,” says Vineet Arora, MD, MA, FHM, assistant professor of medicine and associate director of the internal-medicine residency at the University of Chicago, and chair of the SHM task force on handoffs.
Inadequate communication and poor care transitions can undermine hospitalists’ best care-planning efforts, erode patients’ and families’ confidence and satisfaction with hospital care, and leave primary-care physicians (PCPs) feeling unsatisfied with the relationship. As many as 1 in 5 Medicare beneficiary hospitalizations result in a readmission within 30 days, and while not all of these are preventable, far too many are.5 Another prospective cohort study found that 1 in 5 patients discharged from the hospital to the home experienced an adverse event within three weeks of discharge.6 Complex comorbidities, advanced age, unknown PCP, and limited healthcare literacy present hospitalists with extremely difficult transitions.
Patient safety and cost control are the linchpins to national efforts to improve transitions of care. Dr. Arora recently coauthored an original research paper, which will be published in the Journal of Hospital Medicine in September, showing older hospitalized patients are twice as likely to report problems after discharge if their PCPs were not aware they were hospitalized.
“With escalating healthcare costs, people are looking at ways to save money and reduce redundant care,” Dr. Arora explains, pointing out, as an example, repeated tests resulting from inadequate communication between healthcare providers.
The System Must Change
“All of the effort we put into saving someone’s life—the years of experience, training, medical school, and residency—all of it comes to bear on that hospitalized patient. And it can all be unraveled at the time of discharge if it’s not handled properly,” says Arpana Vidyarthi, MD, a hospitalist and director of quality at the University of California at San Francisco.
Dr. Vidyarthi views in-hospital and discharge transitions as integrally related. “The analysis is similar, even if different techniques may be needed,” she says, adding that, fundamentally, it involves having a system that allows people—or forces them—to do the “right thing.”
That’s why achieving effective care transitions will require more than just a standardized tool or process, Dr. Vidyarthi says. “This is about understanding the ways people communicate and finding ways to train them to communicate better,” she says. “The problem we have is not a lack of information, but how to communicate what, to whom, and when.”
What’s really needed, Dr. Vidyarthi says, is a hospital’s commitment to more effective transitions and its hospitalists’ leadership in driving a comprehensive, multidisciplinary, team- and evidence-based QI process. The new process should be a QI-based solution to a hospital’s care-transitions issues. “Before you can standardize your process, you need to understand it,” she says. “This is a complex problem, and it needs a multifaceted solution. But this lies squarely within the hospitalist arena. We’re part of everything that happens in the hospital.

—Anuj Dalal, MD, Brigham and Women’s Hospital, Boston
Hospital administrators are looking to HM to solve transition and readmission problems now, says Tina Budnitz, MPH, BOOST Project Director (Better Outcomes for Older Adults through Safe Transitions). She expects the scrutiny from the C-suite, legislators, and watchdog groups to increase as the spotlight continues to shine on the healthcare system.
“Any hospitalist can act as a leader in their institution,” Budnitz says. “Be a change agent, pull a group together, and start asking questions: Do we have safe care-transitions practices and processes in place? Just by asking the right question, you can be a catalyst for the system.”
Budnitz also emphasizes the importance of teamwork in the hospital setting. “How can I help my teammates? What am I communicating to the nurses on rounds?” she says. “Can you initiate dialogue with your outpatient medical groups: ‘These faxes we’re sending you—is that information getting to you in ways and times that are helpful? And, by the way, when your patient is admitted, this information would really help me.’ ”
Innovative Strategies
One of the most important initiatives responding to concerns about care transitions is Project BOOST (www.hos pitalmedicine.org/BOOST), a comprehensive toolkit for improving a hospital’s transitions of care. The project aims to build a national consensus for best practices in transitions; collaborate with representatives from the Agency for Healthcare Research and Quality (AHRQ), the Centers for Medicare and Medicaid Services (CMS), and the Joint Commission; and develop a national resource library, Budnitz says.
“Project BOOST not only puts forth best practices for admitting patients, planning for discharge, and then doing the discharge, it also helps show facilities how to change their systems, with resources and tools for analyzing and re-engineering the system,” she says. “Sites get one-to-one assistance from a mentor.”
Six hospitals signed on to the pilot program in 2008; 24 more joined last year. In January, SHM announced a collaborative with the University of Michigan and Blue Cross Blue Shield of Michigan for 15 Michigan hospitals to receive training and mentorship starting in May. And last month, SHM and the California HealthCare Foundation announced a Project BOOST initiative for 20 of the health system’s hospitals (see “California Dreamin’”, p. 6). Other free resources offered on the BOOST Web portal include clinical, data collection, and project management tools. SHM also has a DVD that explains how to use the “teachback” method to improve communication with patients.
Jennifer Myers, MD, FHM, assistant professor of clinical medicine and patient-safety officer at the Hospital of the University of Pennsylvania in Philadelphia, is a Project BOOST participant who spearheaded a process change to improve the quality of her facility’s discharge summary, along with accompanying resident education.7 The discharge summary recently was integrated with the hospital’s electronic health record (EHR) system.
“We’ve gone from dictating the discharge summary to an electronic version completed by the hospitalist, with prompts for key components of the summary, which allows us to create summaries more efficiently—ideally on the day of discharge, but usually within 48 hours,” Dr. Myers says. “We previously researched whether teaching made a difference in the quality of discharges; we found that it did. So we look forward to standardizing our teaching approach around this important topic for all residents.”
Another care-transitions innovation receiving a lot of attention from the government and the private sector is Project RED (Re-Engineered Discharge), led by Brian Jack, MD, vice chair of the department of family medicine at Boston Medical Center. The Project RED research group develops and tests strategies to improve the hospital discharge process to promote patient safety and reduce rehospitalization rates.
“We used re-engineering tools borrowed from other fields, brought together experts from all over the hospital, divided up the whole discharge process, and identified key principles,” Dr. Jack explains. The resulting discharge strategy is reflected in an 11-item checklist of discrete, mutually reinforcing components, which have been shown to reduce rehospitalization rates by 32% while raising patient satisfaction.8 It includes comprehensive discharge and after-hospital plans, a nurse discharge advocate, and a medication reconciliation phone call to the patient. A virtual “patient advocate,” a computerized avatar named Louise, is now being tested. If successful, it will allow patients to interact with a touch-screen teacher of the after-care plan who has time to work at the patient’s pace.
Technology and Transitions
Informatics can be a key player in facilitating care transitions, says Anuj Dalal, MD, a hospitalist and instructor in medicine at Brigham and Women’s Hospital in Boston. He is using one of his hospital’s technological strengths—a well-established, firewall-protected e-mail system—to help improve the discharge process.
“We decided to try to improve awareness of test results pending at the time of discharge,” Dr. Dalal explains. “We created an intervention that automatically triggers an e-mail with the finalized test results to the responsible providers. The intervention creates a loop of communication between the inpatient attending and the PCP. What we hope to show in our research over the next year or two is whether the intervention actually increases awareness of test results by providers.”
One thing to remember is that “all kinds of things can go wrong with care transitions,” no matter the size of the institution, the experience of the staff, or technological limitations, says Vineet Chopra, MD, FACP, a hospitalist at the University of Michigan Health System in Ann Arbor. “The problems of transitions vary from place to place, day to day, time of day, shift changes; and let’s not forget physician extenders and the other members of the healthcare team,” he says. “The more complicated the team, the more complicated the information needing to be handed off becomes.”
Before he joined the group at the university, Dr. Chopra worked at a community hospital, St. Joseph’s Mercy Hospital in Hot Springs, Ark. “It’s hard to come up with a one-size-fits-all solution when there are so many variables,” he says. At the community hospital, “we mandated that the hospitalist call the PCP at the time of discharge. At the academic medical center, we share an EHR with the PCPs and can reach them electronically. We are required to have the discharge summary in the computer before the patient leaves the hospital, and we mandate that hospitalists are reachable by e-mail or phone when they are off.
“I’m not a believer in throwing more technology at problems and just adding more layers of information tools,” Dr. Chopra adds. “Hospitalists who used to carry stethoscopes now also have a clipboard, phone, pager, PDA, and nine different signouts in their pockets. What we want to do is make their life easier. Here, we are looking at technology as a means to do that.”
Dr. Chopra and hospitalist colleague Prasanth Gosineni, MD, have been working with an Ann Arbor tech company called Synaptin to develop a lightweight, mobile client application designed to work on smartphones. Still in pilot testing, it would allow for task-oriented and priority-based messaging in real time and the systematic transfer of important information for the next hospitalist shift.
“You need to be able to share information in a systematic way, but that’s only half of the answer. The other half is the ability to ask specific questions,” Dr. Chopra says. “Technology doesn’t take away from the face-to-face encounter that needs to happen. Nothing will replace face time, but part of the solution is to provide data efficiently and in a way that is easily accessible.”
Dr. Chopra admits that EHR presents both positives and negatives to improved transitions and patient care, “depending on how well it works and what smart features it offers,” he says, “but also recognizing that EHR and other technologies have also taken us farther away from face-to-face exchanges. Some would say that’s part of the problem.”
Handoffs, discharges, and other transitions are ubiquitous in HM—and fraught with the potential for costly and harmful errors. The ideal of an interactive, face-to-face handoff simply is not available for many care transitions. However, hospitalists are challenged to find solutions that will work in their hospitals, with their teams, and their types of patients. Patients and policymakers expect nothing less. TH
Larry Beresford is a freelance writer based in Oakland, Calif.
References
- Payne C, Stein J, Dressler D. Implementation of a structured electronic tool to improve patient handoffs and resident satisfaction. Poster abstract: Internal Medicine 2010, April 21-24, 2010, Toronto.
- Vidyarthi AR. Triple Handoff. AHRQ WebM&M website. Available at: webmm.ahrq.gov/case.aspx? caseID=134. Published May 2006. Accessed May 29, 2010.
- Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364-370.
- 2006 National Patient Safety Goals. The Joint Commission website. Available at: www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsgs.htm. Accessed June 8, 2010.
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 2:360:1418-1428.
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167.
- Myers JS, Jaipaul CK, Kogan JR, Krekun S, Bellini LM, Shea JA. Are discharge summaries teachable? The effects of a discharge summary curriculum on the quality of discharge summaries in an internal medicine residency program. Acad Med. 2006; 81(10):S5-S8.
- Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-187.
- Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7): 433-440.
- Halasyamani L, Kripalani S, Coleman E, et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354-360.
- Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Int Med. 2006;166(5):565-571.
- Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111(9B): 26S-30S.
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effect of restrictive antibiotic policies on dosing timeliness
- Desired consultation format and content
- Risk of cancer associated with CT imaging
- Bleeding, mortality with aspirin after peptic ulcer bleed
- Diagnosis of lung cancer after pneumonia
- Outcomes associated with hyponatremia
- Patient awareness, interest in inpatient medication list
- Monoclonal antibodies in C. difficile
Restrictive Antimicrobial Policy Delays Administration
Clinical question: Does the approval process for restricted on-formulary antimicrobials cause a significant delay in their administration?
Background: Widespread and often unwarranted, antimicrobial use in the hospital lends itself to the development of microbial resistance and increases overall costs. To curb such practices, many hospitals require subspecialty approval prior to dispensing select broad-spectrum antimicrobials. Though shown to improve outcomes, the impact of the approval process on the timeliness of antimicrobial administration remains to be seen.
Study design: Retrospective cohort study.
Setting: Tertiary-care university hospital.
Synopsis: The study included 3,251 inpatients with computerized orders for a “stat” first dose of any of 24 pre-selected, parenteral antimicrobials. Time lag (more than one hour, and more than two hours) to nursing documentation of drug administration was separately analyzed for restricted and unrestricted antimicrobials.
Delay of more than one hour was significantly higher for restricted antimicrobials with an odds ratio of 1.49 (95% CI; 1.23-1.82), while the odds ratio for a delay of more than two hours was 1.78 (95% CI, 1.39-2.21). Also, for restricted antimicrobials, the percentage of orders delayed for more than one hour was significantly different between daytime and nighttime (when the first dose was exempt from pre-approval) orders: 46.1% versus 38.8% (P<0.001). For unrestricted drugs, delay was uniform irrespective of time of day (36.4% of daytime and 36.6% of nighttime orders were delayed more than one hour). The effect of delay in drug administration on patient outcomes was not evaluated.
Though the approval process aims in part to affect resistance patterns and overall costs, this research highlights the need to minimize the delay in administration and probably skip the approval for the first dose in critically ill patients.
Bottom line: Antibiotic approval processes can delay their administration in hospitalized patients, but the effect of this delay on patient outcomes is not yet known.
Citation: Winters BD, Thiemann DR, Brotman DJ. Impact of a restrictive antimicrobial policy on the process and timing of antimicrobial administration. J Hosp Med. 2010;5(1):E41-45.
Physicians Uphold Tenets of Effective Consultation while Highlighting Some Newer Viewpoints
Clinical question: What key features of a consultation are most desirable for physicians?
Background: With new changes in healthcare delivery, the standardization offered by the electronic health record (EHR) system will undoubtedly be confronted by the heterogeneity of clinical consultations. Determination of the various characteristics considered essential for a consultation can help standardize the processes and improve the quality of communication.
Study design: Opinion surveys with a 16-question, Web-based questionnaire about inpatient consultations.
Setting: Four Minnesota teaching hospitals affiliated with the University of Minnesota.
Synopsis: This study surveyed 651 physicians, mostly from general medicine and pediatrics (30% in-training; 54% were more than five years out of training). The response rate to the survey was 50% (323). Responses were analyzed separately for physicians predominantly requesting consultations (requesters) and those predominantly providing them (consultants).
Regarding the consultation request, the majority of consultants preferred a precise consult question (94%), contact information of the ordering provider (68%), and the urgency of consultation (66%), with telephonic communication for emergent consults (75%). Responses were similar regardless of practice site, specialty, or experience.
Regarding the consultation, more requesters desired verbal communication over written advice alone: Sixty-six percent preferred to have the rationale of the recommendations explained. They also preferred a separate recommendations section (48%) with bulleted suggestions (69%) at the top or bottom of the note (74%). Emphasis was placed on specificity of drug names, dose, and duration of therapy (80%), along with alternative options (76%). Most requesters desired a clear “signoff” note when appropriate, with a follow-up plan (74%) or scheduled appointments (44%).
Bottom line: For consultations, the majority of physicians prefer an explanation of medical decision-making, a crisp recommendation section, and specific directions for follow-up.
Citation: Boulware DR, Dekarske AS, Filice GA. Physician preferences for elements of effective consultations. J Gen Intern Med. 2010;25(1):25-30.
CT Scanning Could Be Related to a Future Risk of Cancer at a Population Level
Clinical question: Does the accelerated use of CT scans increase the future risk for radiation-related cancer?
Background: Computed tomography (CT) has come through as a powerful diagnostic and interventional imaging modality at the cost of higher radiation exposures. The potential cancer risk is minimal at an individual level; however, CT technology is used in more than 70 million scans annually. This volume can translate into a significant number of future cancers in the population.
Study design: Indirect risk modeling based on CT scan frequencies and radiation risk models.
Synopsis: Annual frequencies of CT scans (age- and sex-specific) were extracted from insurance claims. The study included 57 million scans, of which 30% were performed in adults 35 to 54 years old. The majority of scans were in females (60%).
Age-specific cancer risk for each CT scan type was estimated through published radiation risk models and national surveys. The projected number of incident cancers per 10,000 scans was highest for chest or abdominal CT angiography (CTA) and whole-body CT. Incidence was higher for females.
The CT scan frequencies were combined with the cancer risk, and it was estimated that approximately 29,000 (95% UL, 15,000-45,000) future cancers could be related to the exposure from CT scans. Uncertainty limits (UL), an estimation of the total error of measurement, accounted for statistical and subjective uncertainties. The risk was dependent on the radiation dose (chest CTA) and frequency of use (abdomen/pelvis followed by chest and head). The most common cancers were lung, colon, and leukemia.
Two-thirds of the projected cancers were in females and attributable to the higher frequency of scans in women coupled with their dual risk of breast and lung cancer with chest radiation. The results provide potential study targets for risk-reduction efforts.
Bottom line: CTA of the chest, abdomen, or pelvis could be related to risk of future cancers, especially in middle-aged females.
Citation: Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
Early Resumption of Low-Dose Aspirin after Peptic Ulcer Bleeding Might Be Beneficial
Clinical question: Is it safe to restart aspirin after acute gastrointestinal (GI) bleeding in patients with cardiovascular or cerebrovascular disease?
Background: The increasing cardiovascular burden in the aging population has indirectly increased aspirin-related peptic ulcer bleeding. Proton-pump inhibitors (PPI) have shown promise in reducing recurrent GI bleeding in non-aspirin-related cases. It is unclear if this protective effect applies to patients on aspirin and, if so, if aspirin resumption after endoscopic treatment is safe.
Study design: Parallel, randomized, placebo-controlled, noninferiority trial.
Setting: Single tertiary endoscopy center in Hong Kong.
Synopsis: One hundred fifty-six patients with aspirin-related peptic ulcer bleeding were selected for the study. After successful endoscopic treatment and 72 hours on pantoprazole infusion, the patients were started on oral pantoprazole for the duration of the study (eight weeks). Patients were equally randomized to receive low-dose aspirin (80 mg/d) or placebo. Primary outcome was recurrent bleeding within 30 days. Secondary outcomes included eight-week all-cause mortality, cause-specific mortality, and recurrence of cardiovascular events.
The aspirin group had a 50% higher risk of recurrent bleeding within 30 days compared with placebo (10.3% vs. 5.4%). However, for the secondary endpoints, aspirin had lower all-cause mortality (1.3% vs. 12.9%), which was not related to increased GI bleeding. On the other hand, discontinuation of aspirin and use of PPI in the placebo group did not prevent mortality related to GI complications.
The small numbers restrict interpretation of the mortality rates but offer support to the fact that the cardioprotective effects of aspirin outweigh its potential for GI bleeding. It is to be noted that these results cannot be extrapolated to higher doses of aspirin.
Bottom line: Early resumption of aspirin after successful treatment of peptic ulcer bleeding might increase the risk of rebleeding but potentially decreases overall mortality.
Citation: Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152(1):1-9.
A Substantial Number of Elderly Patients with Pneumonia Have Pulmonary Malignancy
Clinical question: What is the incidence of, and risk factors for, diagnosis of lung cancer after discharge for pneumonia?
Background: Pneumonia-related admissions in elderly individuals have increased by nearly 20% during the past two decades. Based on the risk profile of this age group, many physicians recommend follow-up chest imaging after pneumonia to ensure resolution and exclude underlying malignancy. However, this practice is not backed by substantial evidence.
Study design: Retrospective cohort study from administrative databases of the VA system.
Setting: Veteran Affairs (VA) Health Care System.
Synopsis: More than 40,000 patients (older than 65, 98.1% male) hospitalized for pneumonia were included in the study. These patients had no pneumonia in the preceding year and did not carry a diagnosis of lung cancer. During the follow-up period of up to five years, a significant proportion (9.2%) of these patients were diagnosed with pulmonary malignancy.
Pertinent factors associated with increased risk of diagnosis included active tobacco use, COPD, and prior nonpulmonary malignancy. Interestingly, stroke, diabetes, dementia, and heart failure were associated with a lower risk of diagnosis, likely due to early mortality from these diseases prior to diagnosis of lung cancer.
Mean time to diagnosis was 297 days, with just 27% diagnosed within 30 days. On mortality analysis, 12.9% (n=5270) of the patients died within 30 days and 20.7% (n=8451) within 90 days. Thus, a period of surveillance of 30 to 90 days following pneumonia, especially in patients with risk factors, could be beneficial.
This study was limited due to the shortcomings of database analyses. Also, the predominantly male, elderly, veteran population restricts extrapolation to the general population.
Bottom line: Patients with risk factors for lung cancer might benefit from surveillance chest imaging after hospitalization for pneumonia to rule out an underlying malignancy.
Citation: Mortensen EM, Copeland LA, Pugh MJ, et al. Diagnosis of pulmonary malignancy after hospitalization for pneumonia. Am J Med. 2010:123(1):66-71.
Hospital-Associated Hyponatremia of Any Severity Adversely Impacts Mortality and Financial Metrics
Clinical question: Does hyponatremia during a hospitalization prophesize a worse outcome?
Study design: Retrospective cohort study from 2002-2007.
Setting: Urban academic medical center.
Synopsis: This study included 53,236 adults based on the presence of admission or subsequent hyponatremia (defined as [Na+] <138 mEq/L). The patients were classified as community-acquired (CAH=37.9%), hospital-aggravated (5.7%), or hospital-acquired hyponatremia (HAH=38.2%).
Across all subgroups, all types of hyponatremia were independently associated with worse primary outcomes, including an increase in hospital mortality (CAH 52%, HAH 66%), prolongation of hospital stay, and discharge to a facility. Also, for the same [Na+], HAH had significantly increased mortality compared with CAH. Though the elderly were more prone to develop hyponatremia, patients younger than 65 had worse outcomes.
The severity of hyponatremia prognosticated adverse outcomes. The liberal definition of hyponatremia, as opposed to the current standard of <135 mEq/L, explains the large numbers in prevalence. However, even mild hyponatremia (133 mEq/L to 137) was linked to poor outcomes (adjusted OR 1.34; CI 1.18-1.51).
The study weaknesses include the use of administrative codes to identify comorbidities, less applicability to outpatient setting, and lack of evaluation of outcomes postdischarge. However, the robust numbers do establish inpatient hyponatremia as a marker of worse outcomes.
Bottom line: Inpatient hyponatremia of any severity is a marker of increased mortality and excessive financial burden.
Citation: Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170(3):294-302.
Patients Lack Awareness and Prefer to Be Updated Regarding Their Inpatient Medications
Clinical question: Is patient knowledge of their medications deficient, and does this reflect a lack of desire to be involved in the medication reconciliation process?
Background: Medication errors remain a significant healthcare problem due to their potential to increase morbidity. For medication administration errors, apart from the dispensing pharmacist and the nurses, patients could be the final checkpoint to ensure medication safety. However, their awareness and enthusiasm to participate has not been adequately assessed in the literature.
Study design: A cross-sectional study using individual surveys to assess awareness and attitudes regarding inpatient medications.
Setting: Single tertiary-care academic teaching hospital.
Synopsis: Fifty cognitively intact adult patients were consented for the study. Of these, 54% provided an accurate recollection of their outpatient medications. When they were surveyed regarding inpatient medications, 96% omitted at least one medication, with the average of 6.8 medication omissions. This was noted to correlate with age >65 years. Also, 44% erroneously presumed they were on a medication while they were in the hospital, even though they weren’t.
When attitudes were surveyed, most of the patients would have preferred to get an inpatient medication list (78%) with the goal of improving their satisfaction (81%) and reducing errors (94%). Also, no association was found between patients’ errors of omission and their reported desire to be involved in the medication safety process.
This small study was limited to cognitively intact patients only. Also, the relatively younger age might cause an overestimation of patient interest in participation. However, the results highlight key medication reconciliation issues. Although patient involvement is desirable, a systematic program of educating them about their medications would be required to make their feedback effective and useful.
Bottom line: Healthy patients might be unaware of their exact hospital medications but prefer to be kept in the loop.
Citation: Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2010;5(2):83-86.
Monoclonal Antibodies against Clostridium difficile Toxins Prevent Recurrence
Clinical question: Are human monoclonal antibodies against C. difficile toxin A (CDA1) and B (CDB1) effective in preventing recurrence of C. diff infection (CDI)?
Background: Widespread use of antibiotics, coupled with the emergence of the hypervirulent (B1/NAP1/027) strain of C. diff, has altered the epidemiology of CDI. Even with effective treatment regimens, there is an escalation in severity, treatment failures, and recurrences. Antibodies against the C. diff toxins are being evaluated as the next frontier in treatment of CDI.
Study design: Phase 2 randomized, double-blind, placebo-controlled trial.
Setting: Thirty study centers in Canada and the U.S.
Synopsis: Two hundred patients with laboratory documented CDI on standard therapy with either metronidazole or vancomycin were randomized to receive a single IV infusion of combined monoclonal antibodies against CDA1 and CDB1 (n=101) or a normal saline placebo infusion (n=99). Patients were followed for 84 days with daily stool counts and intermittent blood samples for immunogenicity analysis.
The primary endpoint of recurrence of laboratory-proven C. diff diarrhea was significantly lower in the monoclonal antibody group (7% vs. 25% in placebo. 95% CI, 7-29; P <0.001). In a subgroup analysis of the epidemic BI/NAP1/027 strain, this favorable association persisted (8% vs. 32%). Recurrence in the antibody group was seen more in elderly patients hospitalized with a higher severity of underlying disease.
Secondary endpoints relating to the initial episode of CDI including treatment failure, severity of diarrhea, and duration to resolution were not significantly different between the two groups. Fewer accounts of serious adverse events were documented in the antibody group (18 patients vs. 28 patients in placebo, P=0.09), and immunogenicity was not detected in any patient.
Bottom line: Monoclonal antibody infusion against C. diff toxins reduces recurrence of infection, even with a hypervirulent (B1/NAP1/027) strain, without any significant adverse events.
Citation: Lowy I, Molrine DC, Leav BA, et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N Engl J Med. 2010; 362(3):197-205. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effect of restrictive antibiotic policies on dosing timeliness
- Desired consultation format and content
- Risk of cancer associated with CT imaging
- Bleeding, mortality with aspirin after peptic ulcer bleed
- Diagnosis of lung cancer after pneumonia
- Outcomes associated with hyponatremia
- Patient awareness, interest in inpatient medication list
- Monoclonal antibodies in C. difficile
Restrictive Antimicrobial Policy Delays Administration
Clinical question: Does the approval process for restricted on-formulary antimicrobials cause a significant delay in their administration?
Background: Widespread and often unwarranted, antimicrobial use in the hospital lends itself to the development of microbial resistance and increases overall costs. To curb such practices, many hospitals require subspecialty approval prior to dispensing select broad-spectrum antimicrobials. Though shown to improve outcomes, the impact of the approval process on the timeliness of antimicrobial administration remains to be seen.
Study design: Retrospective cohort study.
Setting: Tertiary-care university hospital.
Synopsis: The study included 3,251 inpatients with computerized orders for a “stat” first dose of any of 24 pre-selected, parenteral antimicrobials. Time lag (more than one hour, and more than two hours) to nursing documentation of drug administration was separately analyzed for restricted and unrestricted antimicrobials.
Delay of more than one hour was significantly higher for restricted antimicrobials with an odds ratio of 1.49 (95% CI; 1.23-1.82), while the odds ratio for a delay of more than two hours was 1.78 (95% CI, 1.39-2.21). Also, for restricted antimicrobials, the percentage of orders delayed for more than one hour was significantly different between daytime and nighttime (when the first dose was exempt from pre-approval) orders: 46.1% versus 38.8% (P<0.001). For unrestricted drugs, delay was uniform irrespective of time of day (36.4% of daytime and 36.6% of nighttime orders were delayed more than one hour). The effect of delay in drug administration on patient outcomes was not evaluated.
Though the approval process aims in part to affect resistance patterns and overall costs, this research highlights the need to minimize the delay in administration and probably skip the approval for the first dose in critically ill patients.
Bottom line: Antibiotic approval processes can delay their administration in hospitalized patients, but the effect of this delay on patient outcomes is not yet known.
Citation: Winters BD, Thiemann DR, Brotman DJ. Impact of a restrictive antimicrobial policy on the process and timing of antimicrobial administration. J Hosp Med. 2010;5(1):E41-45.
Physicians Uphold Tenets of Effective Consultation while Highlighting Some Newer Viewpoints
Clinical question: What key features of a consultation are most desirable for physicians?
Background: With new changes in healthcare delivery, the standardization offered by the electronic health record (EHR) system will undoubtedly be confronted by the heterogeneity of clinical consultations. Determination of the various characteristics considered essential for a consultation can help standardize the processes and improve the quality of communication.
Study design: Opinion surveys with a 16-question, Web-based questionnaire about inpatient consultations.
Setting: Four Minnesota teaching hospitals affiliated with the University of Minnesota.
Synopsis: This study surveyed 651 physicians, mostly from general medicine and pediatrics (30% in-training; 54% were more than five years out of training). The response rate to the survey was 50% (323). Responses were analyzed separately for physicians predominantly requesting consultations (requesters) and those predominantly providing them (consultants).
Regarding the consultation request, the majority of consultants preferred a precise consult question (94%), contact information of the ordering provider (68%), and the urgency of consultation (66%), with telephonic communication for emergent consults (75%). Responses were similar regardless of practice site, specialty, or experience.
Regarding the consultation, more requesters desired verbal communication over written advice alone: Sixty-six percent preferred to have the rationale of the recommendations explained. They also preferred a separate recommendations section (48%) with bulleted suggestions (69%) at the top or bottom of the note (74%). Emphasis was placed on specificity of drug names, dose, and duration of therapy (80%), along with alternative options (76%). Most requesters desired a clear “signoff” note when appropriate, with a follow-up plan (74%) or scheduled appointments (44%).
Bottom line: For consultations, the majority of physicians prefer an explanation of medical decision-making, a crisp recommendation section, and specific directions for follow-up.
Citation: Boulware DR, Dekarske AS, Filice GA. Physician preferences for elements of effective consultations. J Gen Intern Med. 2010;25(1):25-30.
CT Scanning Could Be Related to a Future Risk of Cancer at a Population Level
Clinical question: Does the accelerated use of CT scans increase the future risk for radiation-related cancer?
Background: Computed tomography (CT) has come through as a powerful diagnostic and interventional imaging modality at the cost of higher radiation exposures. The potential cancer risk is minimal at an individual level; however, CT technology is used in more than 70 million scans annually. This volume can translate into a significant number of future cancers in the population.
Study design: Indirect risk modeling based on CT scan frequencies and radiation risk models.
Synopsis: Annual frequencies of CT scans (age- and sex-specific) were extracted from insurance claims. The study included 57 million scans, of which 30% were performed in adults 35 to 54 years old. The majority of scans were in females (60%).
Age-specific cancer risk for each CT scan type was estimated through published radiation risk models and national surveys. The projected number of incident cancers per 10,000 scans was highest for chest or abdominal CT angiography (CTA) and whole-body CT. Incidence was higher for females.
The CT scan frequencies were combined with the cancer risk, and it was estimated that approximately 29,000 (95% UL, 15,000-45,000) future cancers could be related to the exposure from CT scans. Uncertainty limits (UL), an estimation of the total error of measurement, accounted for statistical and subjective uncertainties. The risk was dependent on the radiation dose (chest CTA) and frequency of use (abdomen/pelvis followed by chest and head). The most common cancers were lung, colon, and leukemia.
Two-thirds of the projected cancers were in females and attributable to the higher frequency of scans in women coupled with their dual risk of breast and lung cancer with chest radiation. The results provide potential study targets for risk-reduction efforts.
Bottom line: CTA of the chest, abdomen, or pelvis could be related to risk of future cancers, especially in middle-aged females.
Citation: Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
Early Resumption of Low-Dose Aspirin after Peptic Ulcer Bleeding Might Be Beneficial
Clinical question: Is it safe to restart aspirin after acute gastrointestinal (GI) bleeding in patients with cardiovascular or cerebrovascular disease?
Background: The increasing cardiovascular burden in the aging population has indirectly increased aspirin-related peptic ulcer bleeding. Proton-pump inhibitors (PPI) have shown promise in reducing recurrent GI bleeding in non-aspirin-related cases. It is unclear if this protective effect applies to patients on aspirin and, if so, if aspirin resumption after endoscopic treatment is safe.
Study design: Parallel, randomized, placebo-controlled, noninferiority trial.
Setting: Single tertiary endoscopy center in Hong Kong.
Synopsis: One hundred fifty-six patients with aspirin-related peptic ulcer bleeding were selected for the study. After successful endoscopic treatment and 72 hours on pantoprazole infusion, the patients were started on oral pantoprazole for the duration of the study (eight weeks). Patients were equally randomized to receive low-dose aspirin (80 mg/d) or placebo. Primary outcome was recurrent bleeding within 30 days. Secondary outcomes included eight-week all-cause mortality, cause-specific mortality, and recurrence of cardiovascular events.
The aspirin group had a 50% higher risk of recurrent bleeding within 30 days compared with placebo (10.3% vs. 5.4%). However, for the secondary endpoints, aspirin had lower all-cause mortality (1.3% vs. 12.9%), which was not related to increased GI bleeding. On the other hand, discontinuation of aspirin and use of PPI in the placebo group did not prevent mortality related to GI complications.
The small numbers restrict interpretation of the mortality rates but offer support to the fact that the cardioprotective effects of aspirin outweigh its potential for GI bleeding. It is to be noted that these results cannot be extrapolated to higher doses of aspirin.
Bottom line: Early resumption of aspirin after successful treatment of peptic ulcer bleeding might increase the risk of rebleeding but potentially decreases overall mortality.
Citation: Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152(1):1-9.
A Substantial Number of Elderly Patients with Pneumonia Have Pulmonary Malignancy
Clinical question: What is the incidence of, and risk factors for, diagnosis of lung cancer after discharge for pneumonia?
Background: Pneumonia-related admissions in elderly individuals have increased by nearly 20% during the past two decades. Based on the risk profile of this age group, many physicians recommend follow-up chest imaging after pneumonia to ensure resolution and exclude underlying malignancy. However, this practice is not backed by substantial evidence.
Study design: Retrospective cohort study from administrative databases of the VA system.
Setting: Veteran Affairs (VA) Health Care System.
Synopsis: More than 40,000 patients (older than 65, 98.1% male) hospitalized for pneumonia were included in the study. These patients had no pneumonia in the preceding year and did not carry a diagnosis of lung cancer. During the follow-up period of up to five years, a significant proportion (9.2%) of these patients were diagnosed with pulmonary malignancy.
Pertinent factors associated with increased risk of diagnosis included active tobacco use, COPD, and prior nonpulmonary malignancy. Interestingly, stroke, diabetes, dementia, and heart failure were associated with a lower risk of diagnosis, likely due to early mortality from these diseases prior to diagnosis of lung cancer.
Mean time to diagnosis was 297 days, with just 27% diagnosed within 30 days. On mortality analysis, 12.9% (n=5270) of the patients died within 30 days and 20.7% (n=8451) within 90 days. Thus, a period of surveillance of 30 to 90 days following pneumonia, especially in patients with risk factors, could be beneficial.
This study was limited due to the shortcomings of database analyses. Also, the predominantly male, elderly, veteran population restricts extrapolation to the general population.
Bottom line: Patients with risk factors for lung cancer might benefit from surveillance chest imaging after hospitalization for pneumonia to rule out an underlying malignancy.
Citation: Mortensen EM, Copeland LA, Pugh MJ, et al. Diagnosis of pulmonary malignancy after hospitalization for pneumonia. Am J Med. 2010:123(1):66-71.
Hospital-Associated Hyponatremia of Any Severity Adversely Impacts Mortality and Financial Metrics
Clinical question: Does hyponatremia during a hospitalization prophesize a worse outcome?
Study design: Retrospective cohort study from 2002-2007.
Setting: Urban academic medical center.
Synopsis: This study included 53,236 adults based on the presence of admission or subsequent hyponatremia (defined as [Na+] <138 mEq/L). The patients were classified as community-acquired (CAH=37.9%), hospital-aggravated (5.7%), or hospital-acquired hyponatremia (HAH=38.2%).
Across all subgroups, all types of hyponatremia were independently associated with worse primary outcomes, including an increase in hospital mortality (CAH 52%, HAH 66%), prolongation of hospital stay, and discharge to a facility. Also, for the same [Na+], HAH had significantly increased mortality compared with CAH. Though the elderly were more prone to develop hyponatremia, patients younger than 65 had worse outcomes.
The severity of hyponatremia prognosticated adverse outcomes. The liberal definition of hyponatremia, as opposed to the current standard of <135 mEq/L, explains the large numbers in prevalence. However, even mild hyponatremia (133 mEq/L to 137) was linked to poor outcomes (adjusted OR 1.34; CI 1.18-1.51).
The study weaknesses include the use of administrative codes to identify comorbidities, less applicability to outpatient setting, and lack of evaluation of outcomes postdischarge. However, the robust numbers do establish inpatient hyponatremia as a marker of worse outcomes.
Bottom line: Inpatient hyponatremia of any severity is a marker of increased mortality and excessive financial burden.
Citation: Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170(3):294-302.
Patients Lack Awareness and Prefer to Be Updated Regarding Their Inpatient Medications
Clinical question: Is patient knowledge of their medications deficient, and does this reflect a lack of desire to be involved in the medication reconciliation process?
Background: Medication errors remain a significant healthcare problem due to their potential to increase morbidity. For medication administration errors, apart from the dispensing pharmacist and the nurses, patients could be the final checkpoint to ensure medication safety. However, their awareness and enthusiasm to participate has not been adequately assessed in the literature.
Study design: A cross-sectional study using individual surveys to assess awareness and attitudes regarding inpatient medications.
Setting: Single tertiary-care academic teaching hospital.
Synopsis: Fifty cognitively intact adult patients were consented for the study. Of these, 54% provided an accurate recollection of their outpatient medications. When they were surveyed regarding inpatient medications, 96% omitted at least one medication, with the average of 6.8 medication omissions. This was noted to correlate with age >65 years. Also, 44% erroneously presumed they were on a medication while they were in the hospital, even though they weren’t.
When attitudes were surveyed, most of the patients would have preferred to get an inpatient medication list (78%) with the goal of improving their satisfaction (81%) and reducing errors (94%). Also, no association was found between patients’ errors of omission and their reported desire to be involved in the medication safety process.
This small study was limited to cognitively intact patients only. Also, the relatively younger age might cause an overestimation of patient interest in participation. However, the results highlight key medication reconciliation issues. Although patient involvement is desirable, a systematic program of educating them about their medications would be required to make their feedback effective and useful.
Bottom line: Healthy patients might be unaware of their exact hospital medications but prefer to be kept in the loop.
Citation: Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2010;5(2):83-86.
Monoclonal Antibodies against Clostridium difficile Toxins Prevent Recurrence
Clinical question: Are human monoclonal antibodies against C. difficile toxin A (CDA1) and B (CDB1) effective in preventing recurrence of C. diff infection (CDI)?
Background: Widespread use of antibiotics, coupled with the emergence of the hypervirulent (B1/NAP1/027) strain of C. diff, has altered the epidemiology of CDI. Even with effective treatment regimens, there is an escalation in severity, treatment failures, and recurrences. Antibodies against the C. diff toxins are being evaluated as the next frontier in treatment of CDI.
Study design: Phase 2 randomized, double-blind, placebo-controlled trial.
Setting: Thirty study centers in Canada and the U.S.
Synopsis: Two hundred patients with laboratory documented CDI on standard therapy with either metronidazole or vancomycin were randomized to receive a single IV infusion of combined monoclonal antibodies against CDA1 and CDB1 (n=101) or a normal saline placebo infusion (n=99). Patients were followed for 84 days with daily stool counts and intermittent blood samples for immunogenicity analysis.
The primary endpoint of recurrence of laboratory-proven C. diff diarrhea was significantly lower in the monoclonal antibody group (7% vs. 25% in placebo. 95% CI, 7-29; P <0.001). In a subgroup analysis of the epidemic BI/NAP1/027 strain, this favorable association persisted (8% vs. 32%). Recurrence in the antibody group was seen more in elderly patients hospitalized with a higher severity of underlying disease.
Secondary endpoints relating to the initial episode of CDI including treatment failure, severity of diarrhea, and duration to resolution were not significantly different between the two groups. Fewer accounts of serious adverse events were documented in the antibody group (18 patients vs. 28 patients in placebo, P=0.09), and immunogenicity was not detected in any patient.
Bottom line: Monoclonal antibody infusion against C. diff toxins reduces recurrence of infection, even with a hypervirulent (B1/NAP1/027) strain, without any significant adverse events.
Citation: Lowy I, Molrine DC, Leav BA, et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N Engl J Med. 2010; 362(3):197-205. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- Effect of restrictive antibiotic policies on dosing timeliness
- Desired consultation format and content
- Risk of cancer associated with CT imaging
- Bleeding, mortality with aspirin after peptic ulcer bleed
- Diagnosis of lung cancer after pneumonia
- Outcomes associated with hyponatremia
- Patient awareness, interest in inpatient medication list
- Monoclonal antibodies in C. difficile
Restrictive Antimicrobial Policy Delays Administration
Clinical question: Does the approval process for restricted on-formulary antimicrobials cause a significant delay in their administration?
Background: Widespread and often unwarranted, antimicrobial use in the hospital lends itself to the development of microbial resistance and increases overall costs. To curb such practices, many hospitals require subspecialty approval prior to dispensing select broad-spectrum antimicrobials. Though shown to improve outcomes, the impact of the approval process on the timeliness of antimicrobial administration remains to be seen.
Study design: Retrospective cohort study.
Setting: Tertiary-care university hospital.
Synopsis: The study included 3,251 inpatients with computerized orders for a “stat” first dose of any of 24 pre-selected, parenteral antimicrobials. Time lag (more than one hour, and more than two hours) to nursing documentation of drug administration was separately analyzed for restricted and unrestricted antimicrobials.
Delay of more than one hour was significantly higher for restricted antimicrobials with an odds ratio of 1.49 (95% CI; 1.23-1.82), while the odds ratio for a delay of more than two hours was 1.78 (95% CI, 1.39-2.21). Also, for restricted antimicrobials, the percentage of orders delayed for more than one hour was significantly different between daytime and nighttime (when the first dose was exempt from pre-approval) orders: 46.1% versus 38.8% (P<0.001). For unrestricted drugs, delay was uniform irrespective of time of day (36.4% of daytime and 36.6% of nighttime orders were delayed more than one hour). The effect of delay in drug administration on patient outcomes was not evaluated.
Though the approval process aims in part to affect resistance patterns and overall costs, this research highlights the need to minimize the delay in administration and probably skip the approval for the first dose in critically ill patients.
Bottom line: Antibiotic approval processes can delay their administration in hospitalized patients, but the effect of this delay on patient outcomes is not yet known.
Citation: Winters BD, Thiemann DR, Brotman DJ. Impact of a restrictive antimicrobial policy on the process and timing of antimicrobial administration. J Hosp Med. 2010;5(1):E41-45.
Physicians Uphold Tenets of Effective Consultation while Highlighting Some Newer Viewpoints
Clinical question: What key features of a consultation are most desirable for physicians?
Background: With new changes in healthcare delivery, the standardization offered by the electronic health record (EHR) system will undoubtedly be confronted by the heterogeneity of clinical consultations. Determination of the various characteristics considered essential for a consultation can help standardize the processes and improve the quality of communication.
Study design: Opinion surveys with a 16-question, Web-based questionnaire about inpatient consultations.
Setting: Four Minnesota teaching hospitals affiliated with the University of Minnesota.
Synopsis: This study surveyed 651 physicians, mostly from general medicine and pediatrics (30% in-training; 54% were more than five years out of training). The response rate to the survey was 50% (323). Responses were analyzed separately for physicians predominantly requesting consultations (requesters) and those predominantly providing them (consultants).
Regarding the consultation request, the majority of consultants preferred a precise consult question (94%), contact information of the ordering provider (68%), and the urgency of consultation (66%), with telephonic communication for emergent consults (75%). Responses were similar regardless of practice site, specialty, or experience.
Regarding the consultation, more requesters desired verbal communication over written advice alone: Sixty-six percent preferred to have the rationale of the recommendations explained. They also preferred a separate recommendations section (48%) with bulleted suggestions (69%) at the top or bottom of the note (74%). Emphasis was placed on specificity of drug names, dose, and duration of therapy (80%), along with alternative options (76%). Most requesters desired a clear “signoff” note when appropriate, with a follow-up plan (74%) or scheduled appointments (44%).
Bottom line: For consultations, the majority of physicians prefer an explanation of medical decision-making, a crisp recommendation section, and specific directions for follow-up.
Citation: Boulware DR, Dekarske AS, Filice GA. Physician preferences for elements of effective consultations. J Gen Intern Med. 2010;25(1):25-30.
CT Scanning Could Be Related to a Future Risk of Cancer at a Population Level
Clinical question: Does the accelerated use of CT scans increase the future risk for radiation-related cancer?
Background: Computed tomography (CT) has come through as a powerful diagnostic and interventional imaging modality at the cost of higher radiation exposures. The potential cancer risk is minimal at an individual level; however, CT technology is used in more than 70 million scans annually. This volume can translate into a significant number of future cancers in the population.
Study design: Indirect risk modeling based on CT scan frequencies and radiation risk models.
Synopsis: Annual frequencies of CT scans (age- and sex-specific) were extracted from insurance claims. The study included 57 million scans, of which 30% were performed in adults 35 to 54 years old. The majority of scans were in females (60%).
Age-specific cancer risk for each CT scan type was estimated through published radiation risk models and national surveys. The projected number of incident cancers per 10,000 scans was highest for chest or abdominal CT angiography (CTA) and whole-body CT. Incidence was higher for females.
The CT scan frequencies were combined with the cancer risk, and it was estimated that approximately 29,000 (95% UL, 15,000-45,000) future cancers could be related to the exposure from CT scans. Uncertainty limits (UL), an estimation of the total error of measurement, accounted for statistical and subjective uncertainties. The risk was dependent on the radiation dose (chest CTA) and frequency of use (abdomen/pelvis followed by chest and head). The most common cancers were lung, colon, and leukemia.
Two-thirds of the projected cancers were in females and attributable to the higher frequency of scans in women coupled with their dual risk of breast and lung cancer with chest radiation. The results provide potential study targets for risk-reduction efforts.
Bottom line: CTA of the chest, abdomen, or pelvis could be related to risk of future cancers, especially in middle-aged females.
Citation: Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
Early Resumption of Low-Dose Aspirin after Peptic Ulcer Bleeding Might Be Beneficial
Clinical question: Is it safe to restart aspirin after acute gastrointestinal (GI) bleeding in patients with cardiovascular or cerebrovascular disease?
Background: The increasing cardiovascular burden in the aging population has indirectly increased aspirin-related peptic ulcer bleeding. Proton-pump inhibitors (PPI) have shown promise in reducing recurrent GI bleeding in non-aspirin-related cases. It is unclear if this protective effect applies to patients on aspirin and, if so, if aspirin resumption after endoscopic treatment is safe.
Study design: Parallel, randomized, placebo-controlled, noninferiority trial.
Setting: Single tertiary endoscopy center in Hong Kong.
Synopsis: One hundred fifty-six patients with aspirin-related peptic ulcer bleeding were selected for the study. After successful endoscopic treatment and 72 hours on pantoprazole infusion, the patients were started on oral pantoprazole for the duration of the study (eight weeks). Patients were equally randomized to receive low-dose aspirin (80 mg/d) or placebo. Primary outcome was recurrent bleeding within 30 days. Secondary outcomes included eight-week all-cause mortality, cause-specific mortality, and recurrence of cardiovascular events.
The aspirin group had a 50% higher risk of recurrent bleeding within 30 days compared with placebo (10.3% vs. 5.4%). However, for the secondary endpoints, aspirin had lower all-cause mortality (1.3% vs. 12.9%), which was not related to increased GI bleeding. On the other hand, discontinuation of aspirin and use of PPI in the placebo group did not prevent mortality related to GI complications.
The small numbers restrict interpretation of the mortality rates but offer support to the fact that the cardioprotective effects of aspirin outweigh its potential for GI bleeding. It is to be noted that these results cannot be extrapolated to higher doses of aspirin.
Bottom line: Early resumption of aspirin after successful treatment of peptic ulcer bleeding might increase the risk of rebleeding but potentially decreases overall mortality.
Citation: Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152(1):1-9.
A Substantial Number of Elderly Patients with Pneumonia Have Pulmonary Malignancy
Clinical question: What is the incidence of, and risk factors for, diagnosis of lung cancer after discharge for pneumonia?
Background: Pneumonia-related admissions in elderly individuals have increased by nearly 20% during the past two decades. Based on the risk profile of this age group, many physicians recommend follow-up chest imaging after pneumonia to ensure resolution and exclude underlying malignancy. However, this practice is not backed by substantial evidence.
Study design: Retrospective cohort study from administrative databases of the VA system.
Setting: Veteran Affairs (VA) Health Care System.
Synopsis: More than 40,000 patients (older than 65, 98.1% male) hospitalized for pneumonia were included in the study. These patients had no pneumonia in the preceding year and did not carry a diagnosis of lung cancer. During the follow-up period of up to five years, a significant proportion (9.2%) of these patients were diagnosed with pulmonary malignancy.
Pertinent factors associated with increased risk of diagnosis included active tobacco use, COPD, and prior nonpulmonary malignancy. Interestingly, stroke, diabetes, dementia, and heart failure were associated with a lower risk of diagnosis, likely due to early mortality from these diseases prior to diagnosis of lung cancer.
Mean time to diagnosis was 297 days, with just 27% diagnosed within 30 days. On mortality analysis, 12.9% (n=5270) of the patients died within 30 days and 20.7% (n=8451) within 90 days. Thus, a period of surveillance of 30 to 90 days following pneumonia, especially in patients with risk factors, could be beneficial.
This study was limited due to the shortcomings of database analyses. Also, the predominantly male, elderly, veteran population restricts extrapolation to the general population.
Bottom line: Patients with risk factors for lung cancer might benefit from surveillance chest imaging after hospitalization for pneumonia to rule out an underlying malignancy.
Citation: Mortensen EM, Copeland LA, Pugh MJ, et al. Diagnosis of pulmonary malignancy after hospitalization for pneumonia. Am J Med. 2010:123(1):66-71.
Hospital-Associated Hyponatremia of Any Severity Adversely Impacts Mortality and Financial Metrics
Clinical question: Does hyponatremia during a hospitalization prophesize a worse outcome?
Study design: Retrospective cohort study from 2002-2007.
Setting: Urban academic medical center.
Synopsis: This study included 53,236 adults based on the presence of admission or subsequent hyponatremia (defined as [Na+] <138 mEq/L). The patients were classified as community-acquired (CAH=37.9%), hospital-aggravated (5.7%), or hospital-acquired hyponatremia (HAH=38.2%).
Across all subgroups, all types of hyponatremia were independently associated with worse primary outcomes, including an increase in hospital mortality (CAH 52%, HAH 66%), prolongation of hospital stay, and discharge to a facility. Also, for the same [Na+], HAH had significantly increased mortality compared with CAH. Though the elderly were more prone to develop hyponatremia, patients younger than 65 had worse outcomes.
The severity of hyponatremia prognosticated adverse outcomes. The liberal definition of hyponatremia, as opposed to the current standard of <135 mEq/L, explains the large numbers in prevalence. However, even mild hyponatremia (133 mEq/L to 137) was linked to poor outcomes (adjusted OR 1.34; CI 1.18-1.51).
The study weaknesses include the use of administrative codes to identify comorbidities, less applicability to outpatient setting, and lack of evaluation of outcomes postdischarge. However, the robust numbers do establish inpatient hyponatremia as a marker of worse outcomes.
Bottom line: Inpatient hyponatremia of any severity is a marker of increased mortality and excessive financial burden.
Citation: Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170(3):294-302.
Patients Lack Awareness and Prefer to Be Updated Regarding Their Inpatient Medications
Clinical question: Is patient knowledge of their medications deficient, and does this reflect a lack of desire to be involved in the medication reconciliation process?
Background: Medication errors remain a significant healthcare problem due to their potential to increase morbidity. For medication administration errors, apart from the dispensing pharmacist and the nurses, patients could be the final checkpoint to ensure medication safety. However, their awareness and enthusiasm to participate has not been adequately assessed in the literature.
Study design: A cross-sectional study using individual surveys to assess awareness and attitudes regarding inpatient medications.
Setting: Single tertiary-care academic teaching hospital.
Synopsis: Fifty cognitively intact adult patients were consented for the study. Of these, 54% provided an accurate recollection of their outpatient medications. When they were surveyed regarding inpatient medications, 96% omitted at least one medication, with the average of 6.8 medication omissions. This was noted to correlate with age >65 years. Also, 44% erroneously presumed they were on a medication while they were in the hospital, even though they weren’t.
When attitudes were surveyed, most of the patients would have preferred to get an inpatient medication list (78%) with the goal of improving their satisfaction (81%) and reducing errors (94%). Also, no association was found between patients’ errors of omission and their reported desire to be involved in the medication safety process.
This small study was limited to cognitively intact patients only. Also, the relatively younger age might cause an overestimation of patient interest in participation. However, the results highlight key medication reconciliation issues. Although patient involvement is desirable, a systematic program of educating them about their medications would be required to make their feedback effective and useful.
Bottom line: Healthy patients might be unaware of their exact hospital medications but prefer to be kept in the loop.
Citation: Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2010;5(2):83-86.
Monoclonal Antibodies against Clostridium difficile Toxins Prevent Recurrence
Clinical question: Are human monoclonal antibodies against C. difficile toxin A (CDA1) and B (CDB1) effective in preventing recurrence of C. diff infection (CDI)?
Background: Widespread use of antibiotics, coupled with the emergence of the hypervirulent (B1/NAP1/027) strain of C. diff, has altered the epidemiology of CDI. Even with effective treatment regimens, there is an escalation in severity, treatment failures, and recurrences. Antibodies against the C. diff toxins are being evaluated as the next frontier in treatment of CDI.
Study design: Phase 2 randomized, double-blind, placebo-controlled trial.
Setting: Thirty study centers in Canada and the U.S.
Synopsis: Two hundred patients with laboratory documented CDI on standard therapy with either metronidazole or vancomycin were randomized to receive a single IV infusion of combined monoclonal antibodies against CDA1 and CDB1 (n=101) or a normal saline placebo infusion (n=99). Patients were followed for 84 days with daily stool counts and intermittent blood samples for immunogenicity analysis.
The primary endpoint of recurrence of laboratory-proven C. diff diarrhea was significantly lower in the monoclonal antibody group (7% vs. 25% in placebo. 95% CI, 7-29; P <0.001). In a subgroup analysis of the epidemic BI/NAP1/027 strain, this favorable association persisted (8% vs. 32%). Recurrence in the antibody group was seen more in elderly patients hospitalized with a higher severity of underlying disease.
Secondary endpoints relating to the initial episode of CDI including treatment failure, severity of diarrhea, and duration to resolution were not significantly different between the two groups. Fewer accounts of serious adverse events were documented in the antibody group (18 patients vs. 28 patients in placebo, P=0.09), and immunogenicity was not detected in any patient.
Bottom line: Monoclonal antibody infusion against C. diff toxins reduces recurrence of infection, even with a hypervirulent (B1/NAP1/027) strain, without any significant adverse events.
Citation: Lowy I, Molrine DC, Leav BA, et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N Engl J Med. 2010; 362(3):197-205. TH
What Is the Most Cost- Effective Evaluation for a First Syncopal Episode?
Case
A 71-year-old woman is admitted after losing consciousness and falling at home. Her history is significant for hypertension, bilateral internal carotid artery stenoses, chronic kidney disease, and diabetes. Resting vital signs are normal. Cardiac, pulmonary, and neurologic exams are unremarkable, as is an electrocardiogram (ECG). She was noted to have a small scalp laceration. Noncontrast CT of the head demonstrates a small occipital subdural bleed thought to be a result of her fall.
What is the most cost-effective evaluation for this patient admitted with suspected first syncopal episode?
Overview
Syncope is defined as sudden, self-terminating loss of consciousness. The final common pathway of all causes of syncope is global cerebral hypoperfusion—specifically, hypoperfusion of the reticular activating system. The differential diagnosis of syncopal loss of consciousness includes neurally mediated (e.g., vasovagal) syncope, orthostatic hypotension, cardiac arrhythmias, structural heart disease, and cerebrovascular disease.
Among young, otherwise healthy people, neurally mediated syncope, which has a relatively benign prognosis, is by far the most common etiology, while in older patients, primary cardiac causes are more common. Nonsyncopal mechanisms, such as seizure and hypoglycemia, should also be considered in the differential diagnosis of transient loss of consciousness (see Table 1, p. 19).1
Syncope is a common problem, accounting for 1% to 2% of ED visits in the U.S.2 The primary objective for evaluation is identification of individuals at increased risk of death due to associated conditions, especially cardiac conditions such as structural heart disease; myocardial ischemia and infarction (MI); Wolff-Parkinson-White, Brugada, or long QT syndromes; and polymorphic ventricular tachycardia.3 True syncope can be associated with other concerning causes, such as aortic stenosis, aortic dissection, and massive pulmonary embolus, as well as arrhythmias from underlying cardiac disease.4
Review of the Data
History: A detailed history and physical examination reveals the cause in 50% of syncopal episodes. Key factors include the account of third-party observers, although it is important to note that tonic-clonic movements can be associated with the global cerebral hypoperfusion of syncope as well as with seizure.4 History of dyspnea, chest pain, or palpitations argue for a primary cardiac or pulmonary cause.
Among patients who endorse a history of palpitations, the sensation of rapid and regular pulsations in the neck points very strongly toward an AV-nodal re-entrant tachycardia, because the carotid pulse and cannon A wave arrive simultaneously in the neck.5 Postictal confusion and focal neurologic exam findings suggest a neurologic rather than syncopal cause, although there are exceptions, and the relationship between seizure and impaired myocardial perfusion is complex.
One factor shown to be significantly associated with a cardiac cause for episodic syncope is family history of sudden cardiac death.4
Physical exam: A thorough general and neurologic exam is critical in evaluation of a first syncopal episode. Supine and standing blood pressure and heart rate should be measured, waiting at least one minute (and by some protocols up to three minutes) after the patient stands up to record standing vitals. Measurement of sitting vitals is not necessary. Neither postural hypotension nor tachycardia are sensitive for hypovolemia in normal volunteers, but a 30-point increase in heart rate is more than 99% specific; a 20-point drop in systolic blood pressure (SBP) is less so.5 A difference of more than 20 mmHg between systolic arm pressures in an individual with chest pain suggests aortic dissection.
Other findings useful in diagnosis of syncope include signs of aortic stenosis, pulmonary hypertension, and myxoma. Absent aortic component of S2, a late-peaking or prolonged murmur, sustained apical impulse, and delayed carotid upstroke (“pulsus tardus”) strongly support the presence of severe aortic stenosis. Absence of a palpable pulmonic component of S2 argues strongly against significant pulmonary hypertension.
There are few physical exam findings reliably seen in pulmonary embolism, but the presence of tachycardia is reliably seen about 80% of the time.4 Although atrial myxoma is associated with a characteristic “tumor plop” heard in early diastole, the finding is not common.5
Diagnostic studies: In a recent observational study of more than 2,000 adults older than 65 hospitalized after a syncopal episode, cardiac enzymes, electroencephalography, CT scan of the head, and carotid ultrasonography determined the etiology of syncope in less than 1% of cases. Inpatient monitoring on telemetry was helpful about 5% of the time. On the other hand, postural vital signs contributed to the diagnosis more than 20% of the time, at a fraction of the cost of these other diagnostics (see Table 2, above).6
The role of transthoracic echocardiogram (echo) is more controversial. It does seem clear, however, that echo is more likely to be diagnostic in adults older than 60, in the presence of a heart murmur on physical exam or with an abnormal ECG.7 Although it demonstrated an arrhythmia that determined the etiology of syncope in only 3% of cases in this study, ECG is still routinely recommended; it is relatively inexpensive, risk-free, and can reveal abnormalities, including bundle-branch block, prior MI, and nonsustained ventricular tachycardia, which may be associated with cardiovascular comorbidities.4
Although the diagnostic tests above are of limited utility in uncovering the cause of syncopal episodes, they may be helpful when history or physical examination suggests a specific cause. For example, in individuals presenting with syncope who have lateralizing neurologic signs or symptoms or carotid bruits, carotid ultrasound is an appropriate diagnostic tool. In a retrospective analysis of 140 older adults who underwent carotid ultrasonography as part of a syncope evaluation, carotid lesions were identified in just 2% of subjects.8 These lesions were not thought to have been the primary etiology of syncope but did prompt additional evaluation or intervention.
Among older individuals or individuals with known heart disease, longer-term cardiac monitoring might be appropriate. The method of cardiac monitoring should be guided by the frequency of episodes. For events occurring daily, Holter monitoring is appropriate. For events occurring at least monthly, an event monitor is appropriate.
For less frequent events, the clinician can consider an implantable loop recorder (ILR).3 In a study of 167 individuals without a clear cause of syncope after initial evaluation, diagnosis was achieved in 90% of patients after one year of monitoring by ILR.9
Among individuals in whom the etiology remains unclear, tilt-table testing is often considered. This modality remains controversial and is unlikely to establish a diagnosis in individuals with an otherwise normal evaluation.3 Electrophysiologic testing is of similarly low yield in individuals with otherwise normal evaluation and is generally not recommended, except in individuals with known heart disease, including history of MI, congestive heart failure (CHF), and pre-excitation.10
Diagnostic algorithms: Algorithm-driven diagnostic protocols for evaluation of syncope do exist, but they are generally based on expert consensus opinion rather than large-scale studies. There are evidence-based syncope risk scores under development, but definitive validation is forthcoming. Examination of two such protocols is provided here.
The San Francisco Syncope Rule is among the most well-known algorithms, and predicts adverse outcomes at seven days. The study cohort included 684 patients presenting with syncope to an academic ED. Adverse outcomes, including death, myocardial infarction, arrhythmia, pulmonary embolus, stroke, subarachnoid hemorrhage, ED return, or hospitalization at seven days, were identified. History of CHF, hematocrit less than 30%, ECG abnormality, shortness of breath, and SBP less than 90 mmHg at presentation were associated with increased risk of an adverse outcome. If any of these findings is present, a patient is considered at high risk for adverse outcome at one week.2 The rule is simple to use; however, external validation has been controversial.
In another risk-prediction study—a large multicenter study of patients older than 60—age greater than 90 years, male sex, history of arrhythmia, SBP greater than 160 mm Hg, ECG abnormality, and elevated troponin I were used to construct a score for risk stratification.11 Specific ECG abnormalities included nonsinus rhythm, heart rate less than 40 beats per minute, evidence of acute or chronic ischemic heart disease, prolonged QRS or QT, left or right ventricular hypertrophy, left-axis deviation, and bundle-branch block. Notably, in this older cohort, CHF (specifically, systolic dysfunction with ejection fraction less than 40%) was not significantly associated with risk of adverse event at 30 days. Study authors stratified participants into low- (score ≤0), intermediate- (score 1-2), and high-risk groups (score >2), with 30-day risk of an adverse event ranging from 2.5% to 20%.
One caveat to the interpretation of these data is the fact that even in the “low risk” group, risk of adverse event was still 2.5%, a figure that many clinicians might consider intolerably high.11 This risk score has not been externally validated.
Back to the Case
Our patient was admitted to the inpatient medicine service. She was monitored overnight on telemetry without evidence of arrhythmia. Collateral history revealed new use of multiple antihypertensives prescribed by outside providers, including both atenolol and propranolol. Her subdural hematoma was managed conservatively and she remained free of neurologic deficits. On discharge, her hypertension regimen was simplified. She was referred for outpatient stress echocardiogram.
Bottom Line
Detailed history and physical exam, including postural vital signs, should form the backbone of the routine evaluation of syncope. An ECG is a critical—and inexpensive—initial diagnostic test, while inpatient telemetry, although a routine component of inpatient evaluation, is expensive and relatively low-yield. Risk prediction rules might ultimately help guide admission decisions and inpatient workup, but definitive external validation of these rules has yet to be accomplished. TH
Dr. Wander is a resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is an assistant professor of medicine in the Division of General Internal Medicine at the University of Washington School of Medicine.
References
- Jhanjee R, Can I, Benditt DG. Syncope. Dis Mon. 2009;55(9):532-585.
- Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224-232.
- Strickberger SA, Benson DW, Biaggioni I, et al. AHA/ACCF Scientific Statement on the evaluation of syncope: from the American Heart Association Councils on Clinical Cardiology, Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke, and the Quality of Care and Outcomes Research Interdisciplinary Working Group; and the American College of Cardiology Foundation: in collaboration with the Heart Rhythm Society: endorsed by the American Autonomic Society. Circulation. 2006;113(2):316-327.
- Linzer M, Yang EH, Estes NA 3rd, Wang P, Vorperian VR, Kapoor WN. Diagnosing syncope. Part 1: Value of history, physical examination, and electrocardiography. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;126(12):989-996.
- McGee S. Evidence-Based Physical Diagnosis. Saunders; 2001.
- Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14):1299-1305.
- Panther R, Mahmood S, Gal R. Echocardiography in the diagnostic evaluation of syncope. J Am Soc Echocardiogr. 1998;11(3):294-298.
- Schnipper JL, Ackerman RH, Krier JB, Honour M. Diagnostic yield and utility of neurovascular ultrasonography in the evaluation of patients with syncope. Mayo Clin Proc. 2005;80(4):480-488.
- Assar MD, Krahn AD, Klein GJ, Yee R, Skanes AC. Optimal duration of monitoring in patients with unexplained syncope. Am J Cardiol. 2003;92(10):1231-1233.
- Linzer M, Yang EH, Estes NA 3rd, Wang P, Vorperian VR, Kapoor WN. Diagnosing syncope. Part 2: Unexplained syncope. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;127(1):76-86.
- Sun BC, Derose SF, Liang LJ, et al. Predictors of 30-day serious events in older patients with syncope. Ann Emerg Med. 2009;54(6):769-778.e1-5.
Case
A 71-year-old woman is admitted after losing consciousness and falling at home. Her history is significant for hypertension, bilateral internal carotid artery stenoses, chronic kidney disease, and diabetes. Resting vital signs are normal. Cardiac, pulmonary, and neurologic exams are unremarkable, as is an electrocardiogram (ECG). She was noted to have a small scalp laceration. Noncontrast CT of the head demonstrates a small occipital subdural bleed thought to be a result of her fall.
What is the most cost-effective evaluation for this patient admitted with suspected first syncopal episode?
Overview
Syncope is defined as sudden, self-terminating loss of consciousness. The final common pathway of all causes of syncope is global cerebral hypoperfusion—specifically, hypoperfusion of the reticular activating system. The differential diagnosis of syncopal loss of consciousness includes neurally mediated (e.g., vasovagal) syncope, orthostatic hypotension, cardiac arrhythmias, structural heart disease, and cerebrovascular disease.
Among young, otherwise healthy people, neurally mediated syncope, which has a relatively benign prognosis, is by far the most common etiology, while in older patients, primary cardiac causes are more common. Nonsyncopal mechanisms, such as seizure and hypoglycemia, should also be considered in the differential diagnosis of transient loss of consciousness (see Table 1, p. 19).1
Syncope is a common problem, accounting for 1% to 2% of ED visits in the U.S.2 The primary objective for evaluation is identification of individuals at increased risk of death due to associated conditions, especially cardiac conditions such as structural heart disease; myocardial ischemia and infarction (MI); Wolff-Parkinson-White, Brugada, or long QT syndromes; and polymorphic ventricular tachycardia.3 True syncope can be associated with other concerning causes, such as aortic stenosis, aortic dissection, and massive pulmonary embolus, as well as arrhythmias from underlying cardiac disease.4
Review of the Data
History: A detailed history and physical examination reveals the cause in 50% of syncopal episodes. Key factors include the account of third-party observers, although it is important to note that tonic-clonic movements can be associated with the global cerebral hypoperfusion of syncope as well as with seizure.4 History of dyspnea, chest pain, or palpitations argue for a primary cardiac or pulmonary cause.
Among patients who endorse a history of palpitations, the sensation of rapid and regular pulsations in the neck points very strongly toward an AV-nodal re-entrant tachycardia, because the carotid pulse and cannon A wave arrive simultaneously in the neck.5 Postictal confusion and focal neurologic exam findings suggest a neurologic rather than syncopal cause, although there are exceptions, and the relationship between seizure and impaired myocardial perfusion is complex.
One factor shown to be significantly associated with a cardiac cause for episodic syncope is family history of sudden cardiac death.4
Physical exam: A thorough general and neurologic exam is critical in evaluation of a first syncopal episode. Supine and standing blood pressure and heart rate should be measured, waiting at least one minute (and by some protocols up to three minutes) after the patient stands up to record standing vitals. Measurement of sitting vitals is not necessary. Neither postural hypotension nor tachycardia are sensitive for hypovolemia in normal volunteers, but a 30-point increase in heart rate is more than 99% specific; a 20-point drop in systolic blood pressure (SBP) is less so.5 A difference of more than 20 mmHg between systolic arm pressures in an individual with chest pain suggests aortic dissection.
Other findings useful in diagnosis of syncope include signs of aortic stenosis, pulmonary hypertension, and myxoma. Absent aortic component of S2, a late-peaking or prolonged murmur, sustained apical impulse, and delayed carotid upstroke (“pulsus tardus”) strongly support the presence of severe aortic stenosis. Absence of a palpable pulmonic component of S2 argues strongly against significant pulmonary hypertension.
There are few physical exam findings reliably seen in pulmonary embolism, but the presence of tachycardia is reliably seen about 80% of the time.4 Although atrial myxoma is associated with a characteristic “tumor plop” heard in early diastole, the finding is not common.5
Diagnostic studies: In a recent observational study of more than 2,000 adults older than 65 hospitalized after a syncopal episode, cardiac enzymes, electroencephalography, CT scan of the head, and carotid ultrasonography determined the etiology of syncope in less than 1% of cases. Inpatient monitoring on telemetry was helpful about 5% of the time. On the other hand, postural vital signs contributed to the diagnosis more than 20% of the time, at a fraction of the cost of these other diagnostics (see Table 2, above).6
The role of transthoracic echocardiogram (echo) is more controversial. It does seem clear, however, that echo is more likely to be diagnostic in adults older than 60, in the presence of a heart murmur on physical exam or with an abnormal ECG.7 Although it demonstrated an arrhythmia that determined the etiology of syncope in only 3% of cases in this study, ECG is still routinely recommended; it is relatively inexpensive, risk-free, and can reveal abnormalities, including bundle-branch block, prior MI, and nonsustained ventricular tachycardia, which may be associated with cardiovascular comorbidities.4
Although the diagnostic tests above are of limited utility in uncovering the cause of syncopal episodes, they may be helpful when history or physical examination suggests a specific cause. For example, in individuals presenting with syncope who have lateralizing neurologic signs or symptoms or carotid bruits, carotid ultrasound is an appropriate diagnostic tool. In a retrospective analysis of 140 older adults who underwent carotid ultrasonography as part of a syncope evaluation, carotid lesions were identified in just 2% of subjects.8 These lesions were not thought to have been the primary etiology of syncope but did prompt additional evaluation or intervention.
Among older individuals or individuals with known heart disease, longer-term cardiac monitoring might be appropriate. The method of cardiac monitoring should be guided by the frequency of episodes. For events occurring daily, Holter monitoring is appropriate. For events occurring at least monthly, an event monitor is appropriate.
For less frequent events, the clinician can consider an implantable loop recorder (ILR).3 In a study of 167 individuals without a clear cause of syncope after initial evaluation, diagnosis was achieved in 90% of patients after one year of monitoring by ILR.9
Among individuals in whom the etiology remains unclear, tilt-table testing is often considered. This modality remains controversial and is unlikely to establish a diagnosis in individuals with an otherwise normal evaluation.3 Electrophysiologic testing is of similarly low yield in individuals with otherwise normal evaluation and is generally not recommended, except in individuals with known heart disease, including history of MI, congestive heart failure (CHF), and pre-excitation.10
Diagnostic algorithms: Algorithm-driven diagnostic protocols for evaluation of syncope do exist, but they are generally based on expert consensus opinion rather than large-scale studies. There are evidence-based syncope risk scores under development, but definitive validation is forthcoming. Examination of two such protocols is provided here.
The San Francisco Syncope Rule is among the most well-known algorithms, and predicts adverse outcomes at seven days. The study cohort included 684 patients presenting with syncope to an academic ED. Adverse outcomes, including death, myocardial infarction, arrhythmia, pulmonary embolus, stroke, subarachnoid hemorrhage, ED return, or hospitalization at seven days, were identified. History of CHF, hematocrit less than 30%, ECG abnormality, shortness of breath, and SBP less than 90 mmHg at presentation were associated with increased risk of an adverse outcome. If any of these findings is present, a patient is considered at high risk for adverse outcome at one week.2 The rule is simple to use; however, external validation has been controversial.
In another risk-prediction study—a large multicenter study of patients older than 60—age greater than 90 years, male sex, history of arrhythmia, SBP greater than 160 mm Hg, ECG abnormality, and elevated troponin I were used to construct a score for risk stratification.11 Specific ECG abnormalities included nonsinus rhythm, heart rate less than 40 beats per minute, evidence of acute or chronic ischemic heart disease, prolonged QRS or QT, left or right ventricular hypertrophy, left-axis deviation, and bundle-branch block. Notably, in this older cohort, CHF (specifically, systolic dysfunction with ejection fraction less than 40%) was not significantly associated with risk of adverse event at 30 days. Study authors stratified participants into low- (score ≤0), intermediate- (score 1-2), and high-risk groups (score >2), with 30-day risk of an adverse event ranging from 2.5% to 20%.
One caveat to the interpretation of these data is the fact that even in the “low risk” group, risk of adverse event was still 2.5%, a figure that many clinicians might consider intolerably high.11 This risk score has not been externally validated.
Back to the Case
Our patient was admitted to the inpatient medicine service. She was monitored overnight on telemetry without evidence of arrhythmia. Collateral history revealed new use of multiple antihypertensives prescribed by outside providers, including both atenolol and propranolol. Her subdural hematoma was managed conservatively and she remained free of neurologic deficits. On discharge, her hypertension regimen was simplified. She was referred for outpatient stress echocardiogram.
Bottom Line
Detailed history and physical exam, including postural vital signs, should form the backbone of the routine evaluation of syncope. An ECG is a critical—and inexpensive—initial diagnostic test, while inpatient telemetry, although a routine component of inpatient evaluation, is expensive and relatively low-yield. Risk prediction rules might ultimately help guide admission decisions and inpatient workup, but definitive external validation of these rules has yet to be accomplished. TH
Dr. Wander is a resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is an assistant professor of medicine in the Division of General Internal Medicine at the University of Washington School of Medicine.
References
- Jhanjee R, Can I, Benditt DG. Syncope. Dis Mon. 2009;55(9):532-585.
- Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224-232.
- Strickberger SA, Benson DW, Biaggioni I, et al. AHA/ACCF Scientific Statement on the evaluation of syncope: from the American Heart Association Councils on Clinical Cardiology, Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke, and the Quality of Care and Outcomes Research Interdisciplinary Working Group; and the American College of Cardiology Foundation: in collaboration with the Heart Rhythm Society: endorsed by the American Autonomic Society. Circulation. 2006;113(2):316-327.
- Linzer M, Yang EH, Estes NA 3rd, Wang P, Vorperian VR, Kapoor WN. Diagnosing syncope. Part 1: Value of history, physical examination, and electrocardiography. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;126(12):989-996.
- McGee S. Evidence-Based Physical Diagnosis. Saunders; 2001.
- Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14):1299-1305.
- Panther R, Mahmood S, Gal R. Echocardiography in the diagnostic evaluation of syncope. J Am Soc Echocardiogr. 1998;11(3):294-298.
- Schnipper JL, Ackerman RH, Krier JB, Honour M. Diagnostic yield and utility of neurovascular ultrasonography in the evaluation of patients with syncope. Mayo Clin Proc. 2005;80(4):480-488.
- Assar MD, Krahn AD, Klein GJ, Yee R, Skanes AC. Optimal duration of monitoring in patients with unexplained syncope. Am J Cardiol. 2003;92(10):1231-1233.
- Linzer M, Yang EH, Estes NA 3rd, Wang P, Vorperian VR, Kapoor WN. Diagnosing syncope. Part 2: Unexplained syncope. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;127(1):76-86.
- Sun BC, Derose SF, Liang LJ, et al. Predictors of 30-day serious events in older patients with syncope. Ann Emerg Med. 2009;54(6):769-778.e1-5.
Case
A 71-year-old woman is admitted after losing consciousness and falling at home. Her history is significant for hypertension, bilateral internal carotid artery stenoses, chronic kidney disease, and diabetes. Resting vital signs are normal. Cardiac, pulmonary, and neurologic exams are unremarkable, as is an electrocardiogram (ECG). She was noted to have a small scalp laceration. Noncontrast CT of the head demonstrates a small occipital subdural bleed thought to be a result of her fall.
What is the most cost-effective evaluation for this patient admitted with suspected first syncopal episode?
Overview
Syncope is defined as sudden, self-terminating loss of consciousness. The final common pathway of all causes of syncope is global cerebral hypoperfusion—specifically, hypoperfusion of the reticular activating system. The differential diagnosis of syncopal loss of consciousness includes neurally mediated (e.g., vasovagal) syncope, orthostatic hypotension, cardiac arrhythmias, structural heart disease, and cerebrovascular disease.
Among young, otherwise healthy people, neurally mediated syncope, which has a relatively benign prognosis, is by far the most common etiology, while in older patients, primary cardiac causes are more common. Nonsyncopal mechanisms, such as seizure and hypoglycemia, should also be considered in the differential diagnosis of transient loss of consciousness (see Table 1, p. 19).1
Syncope is a common problem, accounting for 1% to 2% of ED visits in the U.S.2 The primary objective for evaluation is identification of individuals at increased risk of death due to associated conditions, especially cardiac conditions such as structural heart disease; myocardial ischemia and infarction (MI); Wolff-Parkinson-White, Brugada, or long QT syndromes; and polymorphic ventricular tachycardia.3 True syncope can be associated with other concerning causes, such as aortic stenosis, aortic dissection, and massive pulmonary embolus, as well as arrhythmias from underlying cardiac disease.4
Review of the Data
History: A detailed history and physical examination reveals the cause in 50% of syncopal episodes. Key factors include the account of third-party observers, although it is important to note that tonic-clonic movements can be associated with the global cerebral hypoperfusion of syncope as well as with seizure.4 History of dyspnea, chest pain, or palpitations argue for a primary cardiac or pulmonary cause.
Among patients who endorse a history of palpitations, the sensation of rapid and regular pulsations in the neck points very strongly toward an AV-nodal re-entrant tachycardia, because the carotid pulse and cannon A wave arrive simultaneously in the neck.5 Postictal confusion and focal neurologic exam findings suggest a neurologic rather than syncopal cause, although there are exceptions, and the relationship between seizure and impaired myocardial perfusion is complex.
One factor shown to be significantly associated with a cardiac cause for episodic syncope is family history of sudden cardiac death.4
Physical exam: A thorough general and neurologic exam is critical in evaluation of a first syncopal episode. Supine and standing blood pressure and heart rate should be measured, waiting at least one minute (and by some protocols up to three minutes) after the patient stands up to record standing vitals. Measurement of sitting vitals is not necessary. Neither postural hypotension nor tachycardia are sensitive for hypovolemia in normal volunteers, but a 30-point increase in heart rate is more than 99% specific; a 20-point drop in systolic blood pressure (SBP) is less so.5 A difference of more than 20 mmHg between systolic arm pressures in an individual with chest pain suggests aortic dissection.
Other findings useful in diagnosis of syncope include signs of aortic stenosis, pulmonary hypertension, and myxoma. Absent aortic component of S2, a late-peaking or prolonged murmur, sustained apical impulse, and delayed carotid upstroke (“pulsus tardus”) strongly support the presence of severe aortic stenosis. Absence of a palpable pulmonic component of S2 argues strongly against significant pulmonary hypertension.
There are few physical exam findings reliably seen in pulmonary embolism, but the presence of tachycardia is reliably seen about 80% of the time.4 Although atrial myxoma is associated with a characteristic “tumor plop” heard in early diastole, the finding is not common.5
Diagnostic studies: In a recent observational study of more than 2,000 adults older than 65 hospitalized after a syncopal episode, cardiac enzymes, electroencephalography, CT scan of the head, and carotid ultrasonography determined the etiology of syncope in less than 1% of cases. Inpatient monitoring on telemetry was helpful about 5% of the time. On the other hand, postural vital signs contributed to the diagnosis more than 20% of the time, at a fraction of the cost of these other diagnostics (see Table 2, above).6
The role of transthoracic echocardiogram (echo) is more controversial. It does seem clear, however, that echo is more likely to be diagnostic in adults older than 60, in the presence of a heart murmur on physical exam or with an abnormal ECG.7 Although it demonstrated an arrhythmia that determined the etiology of syncope in only 3% of cases in this study, ECG is still routinely recommended; it is relatively inexpensive, risk-free, and can reveal abnormalities, including bundle-branch block, prior MI, and nonsustained ventricular tachycardia, which may be associated with cardiovascular comorbidities.4
Although the diagnostic tests above are of limited utility in uncovering the cause of syncopal episodes, they may be helpful when history or physical examination suggests a specific cause. For example, in individuals presenting with syncope who have lateralizing neurologic signs or symptoms or carotid bruits, carotid ultrasound is an appropriate diagnostic tool. In a retrospective analysis of 140 older adults who underwent carotid ultrasonography as part of a syncope evaluation, carotid lesions were identified in just 2% of subjects.8 These lesions were not thought to have been the primary etiology of syncope but did prompt additional evaluation or intervention.
Among older individuals or individuals with known heart disease, longer-term cardiac monitoring might be appropriate. The method of cardiac monitoring should be guided by the frequency of episodes. For events occurring daily, Holter monitoring is appropriate. For events occurring at least monthly, an event monitor is appropriate.
For less frequent events, the clinician can consider an implantable loop recorder (ILR).3 In a study of 167 individuals without a clear cause of syncope after initial evaluation, diagnosis was achieved in 90% of patients after one year of monitoring by ILR.9
Among individuals in whom the etiology remains unclear, tilt-table testing is often considered. This modality remains controversial and is unlikely to establish a diagnosis in individuals with an otherwise normal evaluation.3 Electrophysiologic testing is of similarly low yield in individuals with otherwise normal evaluation and is generally not recommended, except in individuals with known heart disease, including history of MI, congestive heart failure (CHF), and pre-excitation.10
Diagnostic algorithms: Algorithm-driven diagnostic protocols for evaluation of syncope do exist, but they are generally based on expert consensus opinion rather than large-scale studies. There are evidence-based syncope risk scores under development, but definitive validation is forthcoming. Examination of two such protocols is provided here.
The San Francisco Syncope Rule is among the most well-known algorithms, and predicts adverse outcomes at seven days. The study cohort included 684 patients presenting with syncope to an academic ED. Adverse outcomes, including death, myocardial infarction, arrhythmia, pulmonary embolus, stroke, subarachnoid hemorrhage, ED return, or hospitalization at seven days, were identified. History of CHF, hematocrit less than 30%, ECG abnormality, shortness of breath, and SBP less than 90 mmHg at presentation were associated with increased risk of an adverse outcome. If any of these findings is present, a patient is considered at high risk for adverse outcome at one week.2 The rule is simple to use; however, external validation has been controversial.
In another risk-prediction study—a large multicenter study of patients older than 60—age greater than 90 years, male sex, history of arrhythmia, SBP greater than 160 mm Hg, ECG abnormality, and elevated troponin I were used to construct a score for risk stratification.11 Specific ECG abnormalities included nonsinus rhythm, heart rate less than 40 beats per minute, evidence of acute or chronic ischemic heart disease, prolonged QRS or QT, left or right ventricular hypertrophy, left-axis deviation, and bundle-branch block. Notably, in this older cohort, CHF (specifically, systolic dysfunction with ejection fraction less than 40%) was not significantly associated with risk of adverse event at 30 days. Study authors stratified participants into low- (score ≤0), intermediate- (score 1-2), and high-risk groups (score >2), with 30-day risk of an adverse event ranging from 2.5% to 20%.
One caveat to the interpretation of these data is the fact that even in the “low risk” group, risk of adverse event was still 2.5%, a figure that many clinicians might consider intolerably high.11 This risk score has not been externally validated.
Back to the Case
Our patient was admitted to the inpatient medicine service. She was monitored overnight on telemetry without evidence of arrhythmia. Collateral history revealed new use of multiple antihypertensives prescribed by outside providers, including both atenolol and propranolol. Her subdural hematoma was managed conservatively and she remained free of neurologic deficits. On discharge, her hypertension regimen was simplified. She was referred for outpatient stress echocardiogram.
Bottom Line
Detailed history and physical exam, including postural vital signs, should form the backbone of the routine evaluation of syncope. An ECG is a critical—and inexpensive—initial diagnostic test, while inpatient telemetry, although a routine component of inpatient evaluation, is expensive and relatively low-yield. Risk prediction rules might ultimately help guide admission decisions and inpatient workup, but definitive external validation of these rules has yet to be accomplished. TH
Dr. Wander is a resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is an assistant professor of medicine in the Division of General Internal Medicine at the University of Washington School of Medicine.
References
- Jhanjee R, Can I, Benditt DG. Syncope. Dis Mon. 2009;55(9):532-585.
- Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224-232.
- Strickberger SA, Benson DW, Biaggioni I, et al. AHA/ACCF Scientific Statement on the evaluation of syncope: from the American Heart Association Councils on Clinical Cardiology, Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke, and the Quality of Care and Outcomes Research Interdisciplinary Working Group; and the American College of Cardiology Foundation: in collaboration with the Heart Rhythm Society: endorsed by the American Autonomic Society. Circulation. 2006;113(2):316-327.
- Linzer M, Yang EH, Estes NA 3rd, Wang P, Vorperian VR, Kapoor WN. Diagnosing syncope. Part 1: Value of history, physical examination, and electrocardiography. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;126(12):989-996.
- McGee S. Evidence-Based Physical Diagnosis. Saunders; 2001.
- Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14):1299-1305.
- Panther R, Mahmood S, Gal R. Echocardiography in the diagnostic evaluation of syncope. J Am Soc Echocardiogr. 1998;11(3):294-298.
- Schnipper JL, Ackerman RH, Krier JB, Honour M. Diagnostic yield and utility of neurovascular ultrasonography in the evaluation of patients with syncope. Mayo Clin Proc. 2005;80(4):480-488.
- Assar MD, Krahn AD, Klein GJ, Yee R, Skanes AC. Optimal duration of monitoring in patients with unexplained syncope. Am J Cardiol. 2003;92(10):1231-1233.
- Linzer M, Yang EH, Estes NA 3rd, Wang P, Vorperian VR, Kapoor WN. Diagnosing syncope. Part 2: Unexplained syncope. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;127(1):76-86.
- Sun BC, Derose SF, Liang LJ, et al. Predictors of 30-day serious events in older patients with syncope. Ann Emerg Med. 2009;54(6):769-778.e1-5.
In the Literature: HM-Related Research You Need to Know
In This Edition:
- Catheter ablation for atrial fibrillation
- Noncontrast CT for appendicitis diagnosis
- Effectiveness of whole-leg ultrasound for DVT diagnosis
- Physician localization and nurse-physician communication
- PPI versus H2 blocker in patients with aspirin-related peptic ulcer disease
- Intensive insulin therapy in steroid-induced hyperglycemia associated with septic shock
- S. aureus decolonization and surgical-site infections
- ABCD2 score and risk of subsequent stroke
Catheter Ablation of Paroxysmal AF Might Be More Effective than Antiarrhythmic Therapy
Clinical question: In patients with paroxysmal atrial fibrillation (AF) unresponsive to initial antiarrhythmic therapy, what is the efficacy of catheter ablation compared with continued attempts at rhythm control?
Background: Although antiarrhythmic drug therapy (ADT) is generally first-line AF therapy, AF recurrence is high and treatment is associated with adverse effects. Catheter ablation is an alternative treatment. Recent studies comparing antiarrhythmic drugs and catheter ablation have involved small populations and have shown mixed results.
Study design: Prospective, multicenter, unblinded, randomized trial.
Setting: Nineteen hospitals—15 in the U.S.—with considerable experience in AF ablation.
Synopsis: This trial compared catheter ablation (n=106) vs. ADT (n=61) for symptomatic, paroxysmal AF refractory to at least one antiarrhythmic drug. Patients in the ablation arm were allowed up to three procedures within an 80-day period; patients in the ADT arm were treated with a previously unused class I or class III antiarrhythmic. After nine months, 34% of ablated patients had failed treatment compared with 84% of patients receiving ADT (HR 0.30 [95% CI, 0.19-0.47]).
While the results are encouraging, some limitations should be noted. Attempts to generalize the results of this study might be limited, as the hospitals had considerable experience in AF ablation, the patient population was relatively young (mean age=56 years), and patients with significant left ventrical dysfunction and persistent AF were excluded.
Furthermore, the long-term effectiveness of ablation was not evaluated, and the study did not assess such outcomes as mortality, stroke, or AF progression. The effectiveness of specific ablation techniques could not be determined because a variety of approaches was employed.
Bottom line: Patients with symptomatic paroxysmal AF without advanced heart failure might benefit from catheter ablation at experienced institutions.
Citation: Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303(4):333-340.
Noncontrast CT Can Be Used to Evaluate Suspected Appendicitis
Clinical question: What is the diagnostic accuracy of noncontrast helical CT in the evaluation of suspected acute appendicitis in the ED?
Background: In the workup of acute appendicitis, various CT protocols are used, including combinations of oral, intravenous, and rectal contrast, as well as noncontrast protocols. Noncontrast CT is less time-consuming and avoids risk of allergic reaction or contrast-induced nephropathy. The diagnostic accuracy of noncontrast CT, however, is controversial.
Study design: Systematic review/meta-analysis.
Setting: Seven studies evaluating acute appendicitis with noncontrast CT in ED settings.
Synopsis: This is the first systematic review of noncontrast CT (helical/multislice) in adults with suspected appendicitis. The authors pooled seven studies (1,060 patients) comparing noncontrast CT with a reference standard of final diagnosis at surgery or followup at a minimum of two weeks. The review yielded the following pooled estimates: sensitivity 93%, specificity 96%, positive likelihood ratio 24, and negative likelihood ratio 0.08. Overall, the diagnostic accuracy of noncontrast CT was high.
A few limitations should be noted. In the original studies, results were reported inconsistently. In one study, 24% of scans were inconclusive, with an associated likelihood ratio of approximately 1. Future studies must address this important clinical question of how to treat patients with inconclusive scans. Another question is to what degree the accuracy reported in this study reflects the expertise of the institutions, the majority of which were university-affiliated. According to one study author, “a certain level of experience is required for skillful interpretation” of noncontrast CT.
Bottom line: Noncontrast CT has a high sensitivity and specificity for acute appendicitis, and should be considered an alternative to contrast CT, particularly in patients with contraindications to contrast or those at risk of contrast-induced nephropathy.
Citation: Hlibczuk V, Dattaro JA, Jin Z, Falzon L, Brown MD. Diagnostic accuracy of noncontrast computed tomography for appendicitis in adults: a systematic review. Ann Emerg Med. 2010;55(1):51-59.e1.
Whole-Leg Compression Ultrasound for DVT Has a Low Failure Rate in Outpatients
Clinical question: How useful is compression ultrasound (CUS) for diagnosing distal DVT?
Background: CUS can reliably evaluate proximal DVT, but its accuracy for distal DVT is controversial. Because of the risk of extension of distal DVT (up to 25%), guidelines recommend that some patients undergo serial proximal CUS after an initial negative result. As an alternative, recent studies have evaluated one-time, whole-leg CUS.
Study design: Systematic review and meta-analysis.
Setting: Review of randomized controlled trials and prospective cohort studies.
Synopsis: The study pooled data from seven studies and more than 4,700 patients with suspected DVT for whom anticoagulation was withheld after a single, negative, whole-leg CUS. At the three-month followup, the combined symptomatic VTE event rate was 0.57%, and the authors concluded that withholding anticoagulation was associated with a low VTE risk.
Although encouraging, this study had several limitations. First, whole-leg CUS is not widely performed or standardized, and the CUS technique varied slightly across the studies. Second, any attempt to generalize the results of this study might be limited, as the proportion of pregnant patients and those with malignancy was low. Furthermore, only one of the seven studies included inpatients that might be at higher VTE risk. Third, pre-test probability was assessed for only a subset of patients, limiting assessment of VTE by risk level. For example, the overall finding of the study—an event rate of 0.57%—appears low but is difficult to apply clinically when subset analyses for high-risk patients yielded a VTE rate of 2.5% with wide confidence intervals ranging from 0% to 7%.
Bottom line: Whole-leg CUS might be a practical alternative to serial proximal CUS, but more data incorporating pre-test probabilities and involving more inpatients are needed. Hospitalists should be cautious in applying pooled summary estimates.
Citation: Johnson SA, Stevens SM, Woller SC, et al. Risk of deep vein thrombosis following a single negative whole-leg compression ultrasound: a systematic review and meta-analysis. JAMA. 2010;303(5):438-445.
Localization of Inpatient Physicians on Hospital Units Increases Provider Communication Frequency
Clinical question: Does localization of inpatient physicians on hospital units improve communication with nursing staff?
Background: While nurses are typically localized on a hospital unit, inpatient physicians often care for patients on multiple units. This lack of regionalization makes it difficult for physicians and nurses to discuss care plans directly. No prior research has evaluated the effect of physician localization on nurse-physician communication.
Study design: Cross-sectional, pre- and postintervention study.
Setting: Tertiary-care teaching hospital, general medical service.
Synopsis: The study was a cross-sectional survey of nurses and physicians prelocalization (n=342 patients) and postlocalization (n=294 patients) of physicians on hospital units. Localization was associated with increased frequency of communication; however, it did not improve the consistency of nurse-physician agreement on the care plan. Nurse-physician agreement was improved on two aspects of the care plan—planned tests and anticipated length of stay—but not on primary diagnosis, planned procedures, medication changes, or consultations.
Limitations of the study were that it was conducted at a single teaching hospital, communication patterns might have changed during the year between pre- and postlocalization, and physicians were not completely localized to specific units (73% localization).
Despite the limitations, this study is the first to evaluate staff localization and communication on a general medical service. The findings suggest that localization is a first step toward interdisciplinary communication. It also shows that quality and content of communication require further assessment.
Future studies must assess the impact of communication on the quality of patient care.
Bottom line: Physician localization improved the frequency of nurse-physician dialogue but did not consistently facilitate a shared understanding of the care plan. Although not assessed in this study, the implication is that the quality of communication between providers needs improvement.
Citation: O’Leary KJ, Wayne DB, Landler MP, et al. J Gen Int Med. 2009;24(11):1223-1227.
Pantoprazole Better than Double-Dose Famotidine in Secondary Prevention of Aspirin-Related Injury
Clinical question: Is a twice-daily H2-receptor antagonist (H2RA) or a once-daily proton pump inhibitor (PPI) better in patients who must continue low-dose-aspirin therapy despite aspirin-related peptic ulcer disease?
Background: Some patients with aspirin-related peptic ulcer disease require continued aspirin therapy. It often is assumed that PPIs are superior to H2RAs in secondary prevention of low-dose aspirin-related injury, although no randomized trials have specifically addressed this question.
Study design: A prospective, double-blind, randomized controlled trial.
Setting: A university hospital in Hong Kong.
Synopsis: In this trial, 160 patients with aspirin-related peptic ulcers/erosions were randomized to 48 weeks of oral famotidine (40 mg twice daily) or pantoprazole (20 mg daily) after mucosal healing and eradication of H pylori. During this time, all patients continued to receive aspirin (80 mg daily).
The rates of recurrent dyspeptic or bleeding ulcers/erosions within 48 weeks were 20% with famotidine versus 0% with pantoprazole. The rates of gastrointestinal (GI) bleeding alone were 7.7% versus 0%, respectively.
Of note, none of the five patients with GI bleeding had significant dyspepsia, which is consistent with prior reports that NSAID-induced injury might be silent.
Overall, high-dose famotidine was inferior to pantoprazole in the prevention of recurrent aspirin-related injury. These findings support the ACCF/ACG/AHA 2008 recommendation of PPIs over double-dose H2RAs in this clinical setting. It is not known, however, whether the PPI strategy extends to average GI-risk patients taking aspirin.
Furthermore, although not demonstrated in this study, it is possible that the lower rates of dyspepsia with pantoprazole might facilitate adherence to prolonged aspirin therapy.
Bottom line: High-dose famotidine was inferior to pantoprazole in the prevention of recurrent low-dose-aspirin-related injury.
Citation: Ng FH, Wong SY, Lam KF, et al. Famotidine is inferior to pantoprazole in preventing recurrence of aspirin-related peptic ulcers or erosions. Gastroenterology. 2010;138
(1):82-88.
Intensive Insulin Therapy Is Not Beneficial in Corticosteroid-Induced Hyperglycemia Associated with Septic Shock
Clinical question: In septic shock treated with hydrocortisone, does intensive insulin therapy reduce in-hospital mortality compared with conventional glucose management?
Background: Corticosteroids might benefit patients with septic shock, but they also can exacerbate illness-induced hyperglycemia. It is hypothesized that normalization of blood glucose with intensive insulin might improve outcomes in these patients.
Study design: A multicenter, 2x2 factorial, randomized controlled trial.
Setting: Eleven ICUs in France.
Synopsis: In this 2x2 factorial comparison, 509 patients with septic shock treated with hydrocortisone were randomized to IV insulin, conventional insulin, fludrocortisone plus IV insulin, and fludrocortisone plus conventional insulin. The primary objective was to assess intensive IV versus conventional insulin, and a secondary objective was to assess the benefit of adding fludrocortisone to hydrocortisone therapy.
Overall, analysis showed no difference in in-hospital mortality in either of the two comparisons.
These null findings should be interpreted considering the following study limitations. In the intensive-insulin groups, there was a failure to reach target glucose levels of 80 mg/dL to 110 mg/dL (mean achieved levels 120 mg/dL to 130 mg/dL and higher). These levels overlapped to some degree with the control group, which targeted glucose levels <150 mg/dL and achieved mean levels of 140 mg/dL to 150 mg/dL.
The lack of substantial difference in glucose levels might have contributed to the null findings. Furthermore, the absolute risk reduction in the original sample-size calculations was overestimated. The result was an underpowered study, which also might have contributed to the null findings.
Bottom line: In septic shock treated with hydrocortisone, the optimal blood-glucose level and insulin strategy are unknown.
Citation: Annane D, Cariou A, Maxime V, et al. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: a randomized controlled trial. JAMA. 2010;303(4):341-348.
Mupirocin-Chlorhexidine Decolonization of Nasal S. Aureus Carriers Reduces Surgical-Site Infections
Clinical question: Can rapid screening and decolonization of nasal carriers of Staphylococcus aureus on admission reduce surgical-site S. aureus infections?
Background: More than 80% of healthcare-associated (HCA) S. aureus infections are endogenous in origin. High-level nasal carriers have a three- to sixfold increased risk of infection with this organism compared with noncarriers and low-level carriers. Decolonization of nasal and extranasal S. aureus on admission might reduce this risk of infection.
Study design: Randomized, double-blinded, placebo-controlled, multicenter trial.
Setting: Three university hospitals and two general hospitals in the Netherlands.
Synopsis: In this study, 918 mostly surgical patients with nasal S. aureus identified preoperatively by PCR tests were randomized to decolonization versus placebo. The five-day decolonization protocol involved mupirocin nasal ointment and chlorhexidine soap baths. Decolonization reduced length of stay by nearly two days. Through six weeks postdischarge, the cumulative incidence of S. aureus infection was 3.4% after decolonization versus 7.7% with placebo (RR 0.42; 95% CI, 0.23-0.75). Among the sites of infection, deep surgical sites had the greatest risk reduction (RR 0.21; 95% CI, 0.07-0.62).
The results of this study are encouraging, but a few limitations should be noted. The decolonization protocol lasted five days, which might make implementation less practical. Also, the relative contributions of mupirocin and chlorhexidine are unclear.
S. aureus is important, but it represents a minority of surgical-site infections; the effect of the protocol on other organisms is unknown. Lastly, MRSA is not prevalent in the Netherlands and no carriers were identified in the study. Although the protocol was designed to eradicate MRSA, such carriers might have different carriage patterns requiring throat swabs in addition to nasal swabs.
Bottom line: Preoperative detection of S. aureus nasal carriage and nasal and extranasal decolonization significantly reduced endogenous S. aureus infection and length of stay. Decolonization might be most beneficial for carriers at increased risk of deep infection, such as those undergoing cardiac surgery.
Citation: Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362(1):9-17.
ABCD2 Is a Poor Predictor of Early Ischemic Stroke after Transient Ischemic Attack
Clinical question: How well does the ABCD2 score predict stroke risk within seven days of transient ischemic attack (TIA)?
Background: After TIA diagnosis, the seven-day risk of ischemic stroke is approximately 5%. Identifying these high-risk patients might facilitate ED decision-making. The ABCD2 score, a prediction tool for stroke after TIA, might be useful but has not been prospectively validated in a large, broad-patient population.
Study design: Prospective validation study, convenience sample.
Setting: Sixteen hospitals in North Carolina.
Synopsis: The ABCD2 score (range 0-7 points) predicts stroke risk after TIA. The investigators evaluated the accuracy of ABCD2 in predicting seven-day ischemic stroke risk in a convenience sample of 1,667 TIA patients. Strokes were categorized as disabling or nondisabling.
Overall, the score was poorly predictive of all ischemic stroke (c stat 0.59) and moderately predictive of the subset of disabling ischemic stroke (c stat 0.71). The ABCD2 had the most discriminatory power when used to identify patients at low risk of disabling stroke (0-3 points); for these patients, the negative likelihood ratio (LR) was 0.16 (0.04-0.64).
The study is the largest published external-validation study of the ABCD2 score, but it had significant limitations that should be considered. There was potential sampling bias because of nonconsecutive sampling, and unaccounted patients with TIA were discharged from the ED. Furthermore, ABCD2 scores were incalculable for 35% of patients, although the authors report that imputed data did not change the findings significantly.
Bottom line: The ABCD2 score does not sufficiently predict the seven-day risk of ischemic stroke after TIA. Further validation studies are needed.
Citation: Asimos AW, Johnson AM, Rosamond WD, et al. A multicenter evaluation of the ABCD2 score’s accuracy for predicting early ischemic stroke in admitted patients with transient ischemic attack. Ann Emerg Med. 2010;55(2):201-210.e5. TH
Dr. Kim is a hospitalist at Brigham and Women’s Hospital in Boston, and an instructor at Harvard Medical School.
In This Edition:
- Catheter ablation for atrial fibrillation
- Noncontrast CT for appendicitis diagnosis
- Effectiveness of whole-leg ultrasound for DVT diagnosis
- Physician localization and nurse-physician communication
- PPI versus H2 blocker in patients with aspirin-related peptic ulcer disease
- Intensive insulin therapy in steroid-induced hyperglycemia associated with septic shock
- S. aureus decolonization and surgical-site infections
- ABCD2 score and risk of subsequent stroke
Catheter Ablation of Paroxysmal AF Might Be More Effective than Antiarrhythmic Therapy
Clinical question: In patients with paroxysmal atrial fibrillation (AF) unresponsive to initial antiarrhythmic therapy, what is the efficacy of catheter ablation compared with continued attempts at rhythm control?
Background: Although antiarrhythmic drug therapy (ADT) is generally first-line AF therapy, AF recurrence is high and treatment is associated with adverse effects. Catheter ablation is an alternative treatment. Recent studies comparing antiarrhythmic drugs and catheter ablation have involved small populations and have shown mixed results.
Study design: Prospective, multicenter, unblinded, randomized trial.
Setting: Nineteen hospitals—15 in the U.S.—with considerable experience in AF ablation.
Synopsis: This trial compared catheter ablation (n=106) vs. ADT (n=61) for symptomatic, paroxysmal AF refractory to at least one antiarrhythmic drug. Patients in the ablation arm were allowed up to three procedures within an 80-day period; patients in the ADT arm were treated with a previously unused class I or class III antiarrhythmic. After nine months, 34% of ablated patients had failed treatment compared with 84% of patients receiving ADT (HR 0.30 [95% CI, 0.19-0.47]).
While the results are encouraging, some limitations should be noted. Attempts to generalize the results of this study might be limited, as the hospitals had considerable experience in AF ablation, the patient population was relatively young (mean age=56 years), and patients with significant left ventrical dysfunction and persistent AF were excluded.
Furthermore, the long-term effectiveness of ablation was not evaluated, and the study did not assess such outcomes as mortality, stroke, or AF progression. The effectiveness of specific ablation techniques could not be determined because a variety of approaches was employed.
Bottom line: Patients with symptomatic paroxysmal AF without advanced heart failure might benefit from catheter ablation at experienced institutions.
Citation: Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303(4):333-340.
Noncontrast CT Can Be Used to Evaluate Suspected Appendicitis
Clinical question: What is the diagnostic accuracy of noncontrast helical CT in the evaluation of suspected acute appendicitis in the ED?
Background: In the workup of acute appendicitis, various CT protocols are used, including combinations of oral, intravenous, and rectal contrast, as well as noncontrast protocols. Noncontrast CT is less time-consuming and avoids risk of allergic reaction or contrast-induced nephropathy. The diagnostic accuracy of noncontrast CT, however, is controversial.
Study design: Systematic review/meta-analysis.
Setting: Seven studies evaluating acute appendicitis with noncontrast CT in ED settings.
Synopsis: This is the first systematic review of noncontrast CT (helical/multislice) in adults with suspected appendicitis. The authors pooled seven studies (1,060 patients) comparing noncontrast CT with a reference standard of final diagnosis at surgery or followup at a minimum of two weeks. The review yielded the following pooled estimates: sensitivity 93%, specificity 96%, positive likelihood ratio 24, and negative likelihood ratio 0.08. Overall, the diagnostic accuracy of noncontrast CT was high.
A few limitations should be noted. In the original studies, results were reported inconsistently. In one study, 24% of scans were inconclusive, with an associated likelihood ratio of approximately 1. Future studies must address this important clinical question of how to treat patients with inconclusive scans. Another question is to what degree the accuracy reported in this study reflects the expertise of the institutions, the majority of which were university-affiliated. According to one study author, “a certain level of experience is required for skillful interpretation” of noncontrast CT.
Bottom line: Noncontrast CT has a high sensitivity and specificity for acute appendicitis, and should be considered an alternative to contrast CT, particularly in patients with contraindications to contrast or those at risk of contrast-induced nephropathy.
Citation: Hlibczuk V, Dattaro JA, Jin Z, Falzon L, Brown MD. Diagnostic accuracy of noncontrast computed tomography for appendicitis in adults: a systematic review. Ann Emerg Med. 2010;55(1):51-59.e1.
Whole-Leg Compression Ultrasound for DVT Has a Low Failure Rate in Outpatients
Clinical question: How useful is compression ultrasound (CUS) for diagnosing distal DVT?
Background: CUS can reliably evaluate proximal DVT, but its accuracy for distal DVT is controversial. Because of the risk of extension of distal DVT (up to 25%), guidelines recommend that some patients undergo serial proximal CUS after an initial negative result. As an alternative, recent studies have evaluated one-time, whole-leg CUS.
Study design: Systematic review and meta-analysis.
Setting: Review of randomized controlled trials and prospective cohort studies.
Synopsis: The study pooled data from seven studies and more than 4,700 patients with suspected DVT for whom anticoagulation was withheld after a single, negative, whole-leg CUS. At the three-month followup, the combined symptomatic VTE event rate was 0.57%, and the authors concluded that withholding anticoagulation was associated with a low VTE risk.
Although encouraging, this study had several limitations. First, whole-leg CUS is not widely performed or standardized, and the CUS technique varied slightly across the studies. Second, any attempt to generalize the results of this study might be limited, as the proportion of pregnant patients and those with malignancy was low. Furthermore, only one of the seven studies included inpatients that might be at higher VTE risk. Third, pre-test probability was assessed for only a subset of patients, limiting assessment of VTE by risk level. For example, the overall finding of the study—an event rate of 0.57%—appears low but is difficult to apply clinically when subset analyses for high-risk patients yielded a VTE rate of 2.5% with wide confidence intervals ranging from 0% to 7%.
Bottom line: Whole-leg CUS might be a practical alternative to serial proximal CUS, but more data incorporating pre-test probabilities and involving more inpatients are needed. Hospitalists should be cautious in applying pooled summary estimates.
Citation: Johnson SA, Stevens SM, Woller SC, et al. Risk of deep vein thrombosis following a single negative whole-leg compression ultrasound: a systematic review and meta-analysis. JAMA. 2010;303(5):438-445.
Localization of Inpatient Physicians on Hospital Units Increases Provider Communication Frequency
Clinical question: Does localization of inpatient physicians on hospital units improve communication with nursing staff?
Background: While nurses are typically localized on a hospital unit, inpatient physicians often care for patients on multiple units. This lack of regionalization makes it difficult for physicians and nurses to discuss care plans directly. No prior research has evaluated the effect of physician localization on nurse-physician communication.
Study design: Cross-sectional, pre- and postintervention study.
Setting: Tertiary-care teaching hospital, general medical service.
Synopsis: The study was a cross-sectional survey of nurses and physicians prelocalization (n=342 patients) and postlocalization (n=294 patients) of physicians on hospital units. Localization was associated with increased frequency of communication; however, it did not improve the consistency of nurse-physician agreement on the care plan. Nurse-physician agreement was improved on two aspects of the care plan—planned tests and anticipated length of stay—but not on primary diagnosis, planned procedures, medication changes, or consultations.
Limitations of the study were that it was conducted at a single teaching hospital, communication patterns might have changed during the year between pre- and postlocalization, and physicians were not completely localized to specific units (73% localization).
Despite the limitations, this study is the first to evaluate staff localization and communication on a general medical service. The findings suggest that localization is a first step toward interdisciplinary communication. It also shows that quality and content of communication require further assessment.
Future studies must assess the impact of communication on the quality of patient care.
Bottom line: Physician localization improved the frequency of nurse-physician dialogue but did not consistently facilitate a shared understanding of the care plan. Although not assessed in this study, the implication is that the quality of communication between providers needs improvement.
Citation: O’Leary KJ, Wayne DB, Landler MP, et al. J Gen Int Med. 2009;24(11):1223-1227.
Pantoprazole Better than Double-Dose Famotidine in Secondary Prevention of Aspirin-Related Injury
Clinical question: Is a twice-daily H2-receptor antagonist (H2RA) or a once-daily proton pump inhibitor (PPI) better in patients who must continue low-dose-aspirin therapy despite aspirin-related peptic ulcer disease?
Background: Some patients with aspirin-related peptic ulcer disease require continued aspirin therapy. It often is assumed that PPIs are superior to H2RAs in secondary prevention of low-dose aspirin-related injury, although no randomized trials have specifically addressed this question.
Study design: A prospective, double-blind, randomized controlled trial.
Setting: A university hospital in Hong Kong.
Synopsis: In this trial, 160 patients with aspirin-related peptic ulcers/erosions were randomized to 48 weeks of oral famotidine (40 mg twice daily) or pantoprazole (20 mg daily) after mucosal healing and eradication of H pylori. During this time, all patients continued to receive aspirin (80 mg daily).
The rates of recurrent dyspeptic or bleeding ulcers/erosions within 48 weeks were 20% with famotidine versus 0% with pantoprazole. The rates of gastrointestinal (GI) bleeding alone were 7.7% versus 0%, respectively.
Of note, none of the five patients with GI bleeding had significant dyspepsia, which is consistent with prior reports that NSAID-induced injury might be silent.
Overall, high-dose famotidine was inferior to pantoprazole in the prevention of recurrent aspirin-related injury. These findings support the ACCF/ACG/AHA 2008 recommendation of PPIs over double-dose H2RAs in this clinical setting. It is not known, however, whether the PPI strategy extends to average GI-risk patients taking aspirin.
Furthermore, although not demonstrated in this study, it is possible that the lower rates of dyspepsia with pantoprazole might facilitate adherence to prolonged aspirin therapy.
Bottom line: High-dose famotidine was inferior to pantoprazole in the prevention of recurrent low-dose-aspirin-related injury.
Citation: Ng FH, Wong SY, Lam KF, et al. Famotidine is inferior to pantoprazole in preventing recurrence of aspirin-related peptic ulcers or erosions. Gastroenterology. 2010;138
(1):82-88.
Intensive Insulin Therapy Is Not Beneficial in Corticosteroid-Induced Hyperglycemia Associated with Septic Shock
Clinical question: In septic shock treated with hydrocortisone, does intensive insulin therapy reduce in-hospital mortality compared with conventional glucose management?
Background: Corticosteroids might benefit patients with septic shock, but they also can exacerbate illness-induced hyperglycemia. It is hypothesized that normalization of blood glucose with intensive insulin might improve outcomes in these patients.
Study design: A multicenter, 2x2 factorial, randomized controlled trial.
Setting: Eleven ICUs in France.
Synopsis: In this 2x2 factorial comparison, 509 patients with septic shock treated with hydrocortisone were randomized to IV insulin, conventional insulin, fludrocortisone plus IV insulin, and fludrocortisone plus conventional insulin. The primary objective was to assess intensive IV versus conventional insulin, and a secondary objective was to assess the benefit of adding fludrocortisone to hydrocortisone therapy.
Overall, analysis showed no difference in in-hospital mortality in either of the two comparisons.
These null findings should be interpreted considering the following study limitations. In the intensive-insulin groups, there was a failure to reach target glucose levels of 80 mg/dL to 110 mg/dL (mean achieved levels 120 mg/dL to 130 mg/dL and higher). These levels overlapped to some degree with the control group, which targeted glucose levels <150 mg/dL and achieved mean levels of 140 mg/dL to 150 mg/dL.
The lack of substantial difference in glucose levels might have contributed to the null findings. Furthermore, the absolute risk reduction in the original sample-size calculations was overestimated. The result was an underpowered study, which also might have contributed to the null findings.
Bottom line: In septic shock treated with hydrocortisone, the optimal blood-glucose level and insulin strategy are unknown.
Citation: Annane D, Cariou A, Maxime V, et al. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: a randomized controlled trial. JAMA. 2010;303(4):341-348.
Mupirocin-Chlorhexidine Decolonization of Nasal S. Aureus Carriers Reduces Surgical-Site Infections
Clinical question: Can rapid screening and decolonization of nasal carriers of Staphylococcus aureus on admission reduce surgical-site S. aureus infections?
Background: More than 80% of healthcare-associated (HCA) S. aureus infections are endogenous in origin. High-level nasal carriers have a three- to sixfold increased risk of infection with this organism compared with noncarriers and low-level carriers. Decolonization of nasal and extranasal S. aureus on admission might reduce this risk of infection.
Study design: Randomized, double-blinded, placebo-controlled, multicenter trial.
Setting: Three university hospitals and two general hospitals in the Netherlands.
Synopsis: In this study, 918 mostly surgical patients with nasal S. aureus identified preoperatively by PCR tests were randomized to decolonization versus placebo. The five-day decolonization protocol involved mupirocin nasal ointment and chlorhexidine soap baths. Decolonization reduced length of stay by nearly two days. Through six weeks postdischarge, the cumulative incidence of S. aureus infection was 3.4% after decolonization versus 7.7% with placebo (RR 0.42; 95% CI, 0.23-0.75). Among the sites of infection, deep surgical sites had the greatest risk reduction (RR 0.21; 95% CI, 0.07-0.62).
The results of this study are encouraging, but a few limitations should be noted. The decolonization protocol lasted five days, which might make implementation less practical. Also, the relative contributions of mupirocin and chlorhexidine are unclear.
S. aureus is important, but it represents a minority of surgical-site infections; the effect of the protocol on other organisms is unknown. Lastly, MRSA is not prevalent in the Netherlands and no carriers were identified in the study. Although the protocol was designed to eradicate MRSA, such carriers might have different carriage patterns requiring throat swabs in addition to nasal swabs.
Bottom line: Preoperative detection of S. aureus nasal carriage and nasal and extranasal decolonization significantly reduced endogenous S. aureus infection and length of stay. Decolonization might be most beneficial for carriers at increased risk of deep infection, such as those undergoing cardiac surgery.
Citation: Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362(1):9-17.
ABCD2 Is a Poor Predictor of Early Ischemic Stroke after Transient Ischemic Attack
Clinical question: How well does the ABCD2 score predict stroke risk within seven days of transient ischemic attack (TIA)?
Background: After TIA diagnosis, the seven-day risk of ischemic stroke is approximately 5%. Identifying these high-risk patients might facilitate ED decision-making. The ABCD2 score, a prediction tool for stroke after TIA, might be useful but has not been prospectively validated in a large, broad-patient population.
Study design: Prospective validation study, convenience sample.
Setting: Sixteen hospitals in North Carolina.
Synopsis: The ABCD2 score (range 0-7 points) predicts stroke risk after TIA. The investigators evaluated the accuracy of ABCD2 in predicting seven-day ischemic stroke risk in a convenience sample of 1,667 TIA patients. Strokes were categorized as disabling or nondisabling.
Overall, the score was poorly predictive of all ischemic stroke (c stat 0.59) and moderately predictive of the subset of disabling ischemic stroke (c stat 0.71). The ABCD2 had the most discriminatory power when used to identify patients at low risk of disabling stroke (0-3 points); for these patients, the negative likelihood ratio (LR) was 0.16 (0.04-0.64).
The study is the largest published external-validation study of the ABCD2 score, but it had significant limitations that should be considered. There was potential sampling bias because of nonconsecutive sampling, and unaccounted patients with TIA were discharged from the ED. Furthermore, ABCD2 scores were incalculable for 35% of patients, although the authors report that imputed data did not change the findings significantly.
Bottom line: The ABCD2 score does not sufficiently predict the seven-day risk of ischemic stroke after TIA. Further validation studies are needed.
Citation: Asimos AW, Johnson AM, Rosamond WD, et al. A multicenter evaluation of the ABCD2 score’s accuracy for predicting early ischemic stroke in admitted patients with transient ischemic attack. Ann Emerg Med. 2010;55(2):201-210.e5. TH
Dr. Kim is a hospitalist at Brigham and Women’s Hospital in Boston, and an instructor at Harvard Medical School.
In This Edition:
- Catheter ablation for atrial fibrillation
- Noncontrast CT for appendicitis diagnosis
- Effectiveness of whole-leg ultrasound for DVT diagnosis
- Physician localization and nurse-physician communication
- PPI versus H2 blocker in patients with aspirin-related peptic ulcer disease
- Intensive insulin therapy in steroid-induced hyperglycemia associated with septic shock
- S. aureus decolonization and surgical-site infections
- ABCD2 score and risk of subsequent stroke
Catheter Ablation of Paroxysmal AF Might Be More Effective than Antiarrhythmic Therapy
Clinical question: In patients with paroxysmal atrial fibrillation (AF) unresponsive to initial antiarrhythmic therapy, what is the efficacy of catheter ablation compared with continued attempts at rhythm control?
Background: Although antiarrhythmic drug therapy (ADT) is generally first-line AF therapy, AF recurrence is high and treatment is associated with adverse effects. Catheter ablation is an alternative treatment. Recent studies comparing antiarrhythmic drugs and catheter ablation have involved small populations and have shown mixed results.
Study design: Prospective, multicenter, unblinded, randomized trial.
Setting: Nineteen hospitals—15 in the U.S.—with considerable experience in AF ablation.
Synopsis: This trial compared catheter ablation (n=106) vs. ADT (n=61) for symptomatic, paroxysmal AF refractory to at least one antiarrhythmic drug. Patients in the ablation arm were allowed up to three procedures within an 80-day period; patients in the ADT arm were treated with a previously unused class I or class III antiarrhythmic. After nine months, 34% of ablated patients had failed treatment compared with 84% of patients receiving ADT (HR 0.30 [95% CI, 0.19-0.47]).
While the results are encouraging, some limitations should be noted. Attempts to generalize the results of this study might be limited, as the hospitals had considerable experience in AF ablation, the patient population was relatively young (mean age=56 years), and patients with significant left ventrical dysfunction and persistent AF were excluded.
Furthermore, the long-term effectiveness of ablation was not evaluated, and the study did not assess such outcomes as mortality, stroke, or AF progression. The effectiveness of specific ablation techniques could not be determined because a variety of approaches was employed.
Bottom line: Patients with symptomatic paroxysmal AF without advanced heart failure might benefit from catheter ablation at experienced institutions.
Citation: Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303(4):333-340.
Noncontrast CT Can Be Used to Evaluate Suspected Appendicitis
Clinical question: What is the diagnostic accuracy of noncontrast helical CT in the evaluation of suspected acute appendicitis in the ED?
Background: In the workup of acute appendicitis, various CT protocols are used, including combinations of oral, intravenous, and rectal contrast, as well as noncontrast protocols. Noncontrast CT is less time-consuming and avoids risk of allergic reaction or contrast-induced nephropathy. The diagnostic accuracy of noncontrast CT, however, is controversial.
Study design: Systematic review/meta-analysis.
Setting: Seven studies evaluating acute appendicitis with noncontrast CT in ED settings.
Synopsis: This is the first systematic review of noncontrast CT (helical/multislice) in adults with suspected appendicitis. The authors pooled seven studies (1,060 patients) comparing noncontrast CT with a reference standard of final diagnosis at surgery or followup at a minimum of two weeks. The review yielded the following pooled estimates: sensitivity 93%, specificity 96%, positive likelihood ratio 24, and negative likelihood ratio 0.08. Overall, the diagnostic accuracy of noncontrast CT was high.
A few limitations should be noted. In the original studies, results were reported inconsistently. In one study, 24% of scans were inconclusive, with an associated likelihood ratio of approximately 1. Future studies must address this important clinical question of how to treat patients with inconclusive scans. Another question is to what degree the accuracy reported in this study reflects the expertise of the institutions, the majority of which were university-affiliated. According to one study author, “a certain level of experience is required for skillful interpretation” of noncontrast CT.
Bottom line: Noncontrast CT has a high sensitivity and specificity for acute appendicitis, and should be considered an alternative to contrast CT, particularly in patients with contraindications to contrast or those at risk of contrast-induced nephropathy.
Citation: Hlibczuk V, Dattaro JA, Jin Z, Falzon L, Brown MD. Diagnostic accuracy of noncontrast computed tomography for appendicitis in adults: a systematic review. Ann Emerg Med. 2010;55(1):51-59.e1.
Whole-Leg Compression Ultrasound for DVT Has a Low Failure Rate in Outpatients
Clinical question: How useful is compression ultrasound (CUS) for diagnosing distal DVT?
Background: CUS can reliably evaluate proximal DVT, but its accuracy for distal DVT is controversial. Because of the risk of extension of distal DVT (up to 25%), guidelines recommend that some patients undergo serial proximal CUS after an initial negative result. As an alternative, recent studies have evaluated one-time, whole-leg CUS.
Study design: Systematic review and meta-analysis.
Setting: Review of randomized controlled trials and prospective cohort studies.
Synopsis: The study pooled data from seven studies and more than 4,700 patients with suspected DVT for whom anticoagulation was withheld after a single, negative, whole-leg CUS. At the three-month followup, the combined symptomatic VTE event rate was 0.57%, and the authors concluded that withholding anticoagulation was associated with a low VTE risk.
Although encouraging, this study had several limitations. First, whole-leg CUS is not widely performed or standardized, and the CUS technique varied slightly across the studies. Second, any attempt to generalize the results of this study might be limited, as the proportion of pregnant patients and those with malignancy was low. Furthermore, only one of the seven studies included inpatients that might be at higher VTE risk. Third, pre-test probability was assessed for only a subset of patients, limiting assessment of VTE by risk level. For example, the overall finding of the study—an event rate of 0.57%—appears low but is difficult to apply clinically when subset analyses for high-risk patients yielded a VTE rate of 2.5% with wide confidence intervals ranging from 0% to 7%.
Bottom line: Whole-leg CUS might be a practical alternative to serial proximal CUS, but more data incorporating pre-test probabilities and involving more inpatients are needed. Hospitalists should be cautious in applying pooled summary estimates.
Citation: Johnson SA, Stevens SM, Woller SC, et al. Risk of deep vein thrombosis following a single negative whole-leg compression ultrasound: a systematic review and meta-analysis. JAMA. 2010;303(5):438-445.
Localization of Inpatient Physicians on Hospital Units Increases Provider Communication Frequency
Clinical question: Does localization of inpatient physicians on hospital units improve communication with nursing staff?
Background: While nurses are typically localized on a hospital unit, inpatient physicians often care for patients on multiple units. This lack of regionalization makes it difficult for physicians and nurses to discuss care plans directly. No prior research has evaluated the effect of physician localization on nurse-physician communication.
Study design: Cross-sectional, pre- and postintervention study.
Setting: Tertiary-care teaching hospital, general medical service.
Synopsis: The study was a cross-sectional survey of nurses and physicians prelocalization (n=342 patients) and postlocalization (n=294 patients) of physicians on hospital units. Localization was associated with increased frequency of communication; however, it did not improve the consistency of nurse-physician agreement on the care plan. Nurse-physician agreement was improved on two aspects of the care plan—planned tests and anticipated length of stay—but not on primary diagnosis, planned procedures, medication changes, or consultations.
Limitations of the study were that it was conducted at a single teaching hospital, communication patterns might have changed during the year between pre- and postlocalization, and physicians were not completely localized to specific units (73% localization).
Despite the limitations, this study is the first to evaluate staff localization and communication on a general medical service. The findings suggest that localization is a first step toward interdisciplinary communication. It also shows that quality and content of communication require further assessment.
Future studies must assess the impact of communication on the quality of patient care.
Bottom line: Physician localization improved the frequency of nurse-physician dialogue but did not consistently facilitate a shared understanding of the care plan. Although not assessed in this study, the implication is that the quality of communication between providers needs improvement.
Citation: O’Leary KJ, Wayne DB, Landler MP, et al. J Gen Int Med. 2009;24(11):1223-1227.
Pantoprazole Better than Double-Dose Famotidine in Secondary Prevention of Aspirin-Related Injury
Clinical question: Is a twice-daily H2-receptor antagonist (H2RA) or a once-daily proton pump inhibitor (PPI) better in patients who must continue low-dose-aspirin therapy despite aspirin-related peptic ulcer disease?
Background: Some patients with aspirin-related peptic ulcer disease require continued aspirin therapy. It often is assumed that PPIs are superior to H2RAs in secondary prevention of low-dose aspirin-related injury, although no randomized trials have specifically addressed this question.
Study design: A prospective, double-blind, randomized controlled trial.
Setting: A university hospital in Hong Kong.
Synopsis: In this trial, 160 patients with aspirin-related peptic ulcers/erosions were randomized to 48 weeks of oral famotidine (40 mg twice daily) or pantoprazole (20 mg daily) after mucosal healing and eradication of H pylori. During this time, all patients continued to receive aspirin (80 mg daily).
The rates of recurrent dyspeptic or bleeding ulcers/erosions within 48 weeks were 20% with famotidine versus 0% with pantoprazole. The rates of gastrointestinal (GI) bleeding alone were 7.7% versus 0%, respectively.
Of note, none of the five patients with GI bleeding had significant dyspepsia, which is consistent with prior reports that NSAID-induced injury might be silent.
Overall, high-dose famotidine was inferior to pantoprazole in the prevention of recurrent aspirin-related injury. These findings support the ACCF/ACG/AHA 2008 recommendation of PPIs over double-dose H2RAs in this clinical setting. It is not known, however, whether the PPI strategy extends to average GI-risk patients taking aspirin.
Furthermore, although not demonstrated in this study, it is possible that the lower rates of dyspepsia with pantoprazole might facilitate adherence to prolonged aspirin therapy.
Bottom line: High-dose famotidine was inferior to pantoprazole in the prevention of recurrent low-dose-aspirin-related injury.
Citation: Ng FH, Wong SY, Lam KF, et al. Famotidine is inferior to pantoprazole in preventing recurrence of aspirin-related peptic ulcers or erosions. Gastroenterology. 2010;138
(1):82-88.
Intensive Insulin Therapy Is Not Beneficial in Corticosteroid-Induced Hyperglycemia Associated with Septic Shock
Clinical question: In septic shock treated with hydrocortisone, does intensive insulin therapy reduce in-hospital mortality compared with conventional glucose management?
Background: Corticosteroids might benefit patients with septic shock, but they also can exacerbate illness-induced hyperglycemia. It is hypothesized that normalization of blood glucose with intensive insulin might improve outcomes in these patients.
Study design: A multicenter, 2x2 factorial, randomized controlled trial.
Setting: Eleven ICUs in France.
Synopsis: In this 2x2 factorial comparison, 509 patients with septic shock treated with hydrocortisone were randomized to IV insulin, conventional insulin, fludrocortisone plus IV insulin, and fludrocortisone plus conventional insulin. The primary objective was to assess intensive IV versus conventional insulin, and a secondary objective was to assess the benefit of adding fludrocortisone to hydrocortisone therapy.
Overall, analysis showed no difference in in-hospital mortality in either of the two comparisons.
These null findings should be interpreted considering the following study limitations. In the intensive-insulin groups, there was a failure to reach target glucose levels of 80 mg/dL to 110 mg/dL (mean achieved levels 120 mg/dL to 130 mg/dL and higher). These levels overlapped to some degree with the control group, which targeted glucose levels <150 mg/dL and achieved mean levels of 140 mg/dL to 150 mg/dL.
The lack of substantial difference in glucose levels might have contributed to the null findings. Furthermore, the absolute risk reduction in the original sample-size calculations was overestimated. The result was an underpowered study, which also might have contributed to the null findings.
Bottom line: In septic shock treated with hydrocortisone, the optimal blood-glucose level and insulin strategy are unknown.
Citation: Annane D, Cariou A, Maxime V, et al. Corticosteroid treatment and intensive insulin therapy for septic shock in adults: a randomized controlled trial. JAMA. 2010;303(4):341-348.
Mupirocin-Chlorhexidine Decolonization of Nasal S. Aureus Carriers Reduces Surgical-Site Infections
Clinical question: Can rapid screening and decolonization of nasal carriers of Staphylococcus aureus on admission reduce surgical-site S. aureus infections?
Background: More than 80% of healthcare-associated (HCA) S. aureus infections are endogenous in origin. High-level nasal carriers have a three- to sixfold increased risk of infection with this organism compared with noncarriers and low-level carriers. Decolonization of nasal and extranasal S. aureus on admission might reduce this risk of infection.
Study design: Randomized, double-blinded, placebo-controlled, multicenter trial.
Setting: Three university hospitals and two general hospitals in the Netherlands.
Synopsis: In this study, 918 mostly surgical patients with nasal S. aureus identified preoperatively by PCR tests were randomized to decolonization versus placebo. The five-day decolonization protocol involved mupirocin nasal ointment and chlorhexidine soap baths. Decolonization reduced length of stay by nearly two days. Through six weeks postdischarge, the cumulative incidence of S. aureus infection was 3.4% after decolonization versus 7.7% with placebo (RR 0.42; 95% CI, 0.23-0.75). Among the sites of infection, deep surgical sites had the greatest risk reduction (RR 0.21; 95% CI, 0.07-0.62).
The results of this study are encouraging, but a few limitations should be noted. The decolonization protocol lasted five days, which might make implementation less practical. Also, the relative contributions of mupirocin and chlorhexidine are unclear.
S. aureus is important, but it represents a minority of surgical-site infections; the effect of the protocol on other organisms is unknown. Lastly, MRSA is not prevalent in the Netherlands and no carriers were identified in the study. Although the protocol was designed to eradicate MRSA, such carriers might have different carriage patterns requiring throat swabs in addition to nasal swabs.
Bottom line: Preoperative detection of S. aureus nasal carriage and nasal and extranasal decolonization significantly reduced endogenous S. aureus infection and length of stay. Decolonization might be most beneficial for carriers at increased risk of deep infection, such as those undergoing cardiac surgery.
Citation: Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362(1):9-17.
ABCD2 Is a Poor Predictor of Early Ischemic Stroke after Transient Ischemic Attack
Clinical question: How well does the ABCD2 score predict stroke risk within seven days of transient ischemic attack (TIA)?
Background: After TIA diagnosis, the seven-day risk of ischemic stroke is approximately 5%. Identifying these high-risk patients might facilitate ED decision-making. The ABCD2 score, a prediction tool for stroke after TIA, might be useful but has not been prospectively validated in a large, broad-patient population.
Study design: Prospective validation study, convenience sample.
Setting: Sixteen hospitals in North Carolina.
Synopsis: The ABCD2 score (range 0-7 points) predicts stroke risk after TIA. The investigators evaluated the accuracy of ABCD2 in predicting seven-day ischemic stroke risk in a convenience sample of 1,667 TIA patients. Strokes were categorized as disabling or nondisabling.
Overall, the score was poorly predictive of all ischemic stroke (c stat 0.59) and moderately predictive of the subset of disabling ischemic stroke (c stat 0.71). The ABCD2 had the most discriminatory power when used to identify patients at low risk of disabling stroke (0-3 points); for these patients, the negative likelihood ratio (LR) was 0.16 (0.04-0.64).
The study is the largest published external-validation study of the ABCD2 score, but it had significant limitations that should be considered. There was potential sampling bias because of nonconsecutive sampling, and unaccounted patients with TIA were discharged from the ED. Furthermore, ABCD2 scores were incalculable for 35% of patients, although the authors report that imputed data did not change the findings significantly.
Bottom line: The ABCD2 score does not sufficiently predict the seven-day risk of ischemic stroke after TIA. Further validation studies are needed.
Citation: Asimos AW, Johnson AM, Rosamond WD, et al. A multicenter evaluation of the ABCD2 score’s accuracy for predicting early ischemic stroke in admitted patients with transient ischemic attack. Ann Emerg Med. 2010;55(2):201-210.e5. TH
Dr. Kim is a hospitalist at Brigham and Women’s Hospital in Boston, and an instructor at Harvard Medical School.
What Is the Appropriate Treatment of Cancer-Associated Venous Thromboembolic Disease?
Case
A 70-year-old woman with recently diagnosed pancreatic cancer is admitted with worsening abdominal pain and new right-lower-extremity edema. A CT scan of the abdomen and pelvis reveals occlusive IVC and common iliac thromboses. A right-common-femoral DVT appears on Doppler ultrasound. A CT angiogram of her chest is negative for pulmonary emboli. What is the appropriate treatment for this patient’s thromboembolic disease?
Overview
VTE in the setting of malignancy is common, and the incidence of VTE among cancer patients is increasing for unclear reasons.1,2,3 VTE occurs in an estimated 4% to 20% of all malignancy patients. Overall, cancer patients are at a sixfold increased risk of developing VTE compared with the general population, and these patients represent approximately 20% of all VTE cases.4,5
VTE is a leading cause of mortality among hospitalized cancer patients; evidence of VTE exists in up to 50% of cancer patients at autopsy.3,4 VTE complications lead to significant morbidity, including recurrent VTE, pulmonary hypertension, post-thrombophlebitic syndrome, bleeding, and decreased quality of life.6,7
The risk is greatest for hospitalized cancer patients and those receiving active chemotherapy, particularly with such antiangiogenic agents as thalidomide and bevacizumab.4,6 Certain malignancies are more frequently associated with VTE; these include gastrointestinal, gynecologic, brain, lung, renal, and hematologic cancers.4 Table 1 (p. 50) summarizes risk factors associated with VTE in cancer patients.4
Patients with malignancy are hypercoagulable, primarily because of tumor-related alterations in the coagulation cascade.8 Tumors contain cell-surface proteins (e.g., tissue factor and cancer procoagulant) that lead to activation of the clotting cascade via interactions with factors IX and/or X. In addition, tumor-released cytokines cause prothrombotic changes in the vascular endothelium.8
This hypercoagulability is exacerbated by cancer-associated treatment events, including immobility, central venous catheters, erythropoiesis-stimulating agents, and packed red-blood-cell and platelet transfusions.5,9
Cancer-related therapy complications further confound VTE management. Drug interactions, chemotherapy-induced thrombocytopenia, malnutrition, bleeding risk from surgery or tumor location, and liver dysfunction make safe management of cancer-associated VTE a challenge.
Review of the Data
Low-molecular-weight heparin (LMWH) vs. vitamin K antagonists (VKA): There is significant evidence that LMWH is the preferred pharmacologic therapy for the initial and long-term treatment of cancer-related VTE. The most convincing data were published as the CLOT trial, and is supported by several smaller studies.10 Recommendations for the preferred use of LMWH are consistent among several national and international guidelines.6,7
In the CLOT (Randomized Comparison of Low-Molecular-Weight Heparin Versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer) trial, six months of treatment with an oral VKA preceded by five to seven days of LMWH was compared with six months of treatment with LMWH (dalteparin). Patients with the diagnosis of acute symptomatic VTE were evaluated. After six months of treatment, 53 of 336 patients in the oral anticoagulant group had recurrent VTE, compared with 27 of 336 patients in the LMWH group—a relative risk reduction of 52% and an absolute risk reduction of 8% (P=0.002). Complication rates (major and minor bleeding) and overall mortality were similar between the two groups.7,10
Two smaller trials compared LMWHs with warfarin in the treatment of VTE in the setting of cancer. In one trial, seven of 67 enoxaparin-treated patients developed bleeding or recurrent VTE, compared with 15 of 71 warfarin-treated subjects; however, this reduction was not statistically significant (P=0.09).11 In another trial, seven of 100 tinzaparin-treated patients developed recurrent VTE, compared with 16 of 100 warfarin-treated patients (P=0.044).12
Thus, LMWH is the preferred therapeutic agent for both DVT and PE in the setting of malignancy.5 Even so, although the clinical evidence supports LMWH use in the treatment of cancer-associated VTE, it’s worth noting that many of the authors of the cited papers received compensation from large pharmaceutical companies. In addition, the CLOT trial was funded by Pharmacia, which supplied the study drug.
Initial treatment (5-10 days): The American Society of Clinical Oncology (ASCO) guidelines advocate the use of LMWH during the initial five to 10 days following VTE diagnosis. Four other cancer research organization guidelines, National Comprehensive Cancer Network (NCCN), the Italian Association of Medical Oncology (AIOM), the European Society of Medical Oncology (ESMO), and the French National Federation of the League of Centers Against Cancer (FNCLCC), echo this approach, with unfractionated heparin (UFH) or fondaparinux as additional initial treatment depending on the clinical situation—i.e., renal failure, heparin-induced thrombocytopenia (HIT), or bleeding risk.6
Table 2 (below) summarizes recommendations for VTE treatment in cancer patients from all five guideline panels.6
Long-term treatment and duration (3-6 months): All of the panels agree LMWH is the preferred agent for long-term therapy of cancer-related VTE. ASCO supports treatment with LMWH for at least six months; oral VKAs with a targeted INR of 2 to 3 are acceptable when LMWH is not feasible. NCCN, AIOM, ESMO, and FNCLCC recommend an LMWH treatment duration from three to six months (ASCO recommends at least six months).
All of the panels, however, advocate indefinite duration of anticoagulation in patients with such continuing risk factors as active (metastatic, recurrent, or persistent) cancer or chemotherapy treatment.6 AIOM and ESMO specify indefinite LMWH, whereas ASCO does not specify oral VKA or LMWH use. Given the difficulties of managing VKA in the setting of advanced malignancy or chemotherapy, LMWH is the most practical choice, if it’s available and isn’t cost-prohibitive.
LMWH availability: Dalteparin, tinzaparin, and enoxaparin are LMWHs currently available in the U.S. for VTE treatment. Dalteparin is the only FDA-approved LMWH drug for long-term use to treat cancer-associated VTE, although enoxaparin and tinzaparin are used in practice. All three are supplied in prefilled syringes, which make self-administration easier and significantly reduce the risk of dosage error.6
LMWH vs. UFH: LMWH is safer and more efficacious than UFH. A summary of 22 clinical trials (including cancer patients and noncancer patients) by a Cochrane systematic review showed that treatment with LMWH in comparison with UFH results in decreased recurrent VTE, bleeding, mortality, HIT, and osteoporosis.7,13
Other agents: Fondaparinux is a factor Xa inhibitor rarely associated with heparin-induced thrombocytopenia (HIT), which makes it an attractive alternate anticoagulant for HIT patients. Its use in comparison with other parenteral anticoagulants has not been established in patients with malignancy.
Fondaparinux is FDA-approved for initial VTE treatment, and is used in practice as an alternative prophylactic anticoagulant for patients with HIT history or heparin allergy.7 However, no randomized clinical trials have evaluated its efficacy in patients with HIT.
Several new oral anticoagulants, including direct thrombin and factor Xa inhibitors, are being investigated; efficacy has not been established in cancer patients.7
Inferior vena cava (IVC) filters: Limited data surround the use of IVC filters, and most consensus guidelines recommend their use only in specific settings. One randomized controlled study (not limited to patients with cancer) showed no difference in overall short-term or long-term survival among patients receiving IVC filters for VTE treatment. However, there was a decrease in symptomatic PE in the filter group 12 days after placement. The tradeoff was significantly more recurrent DVTs at two years’ followup. The authors concluded that systematic use of IVC filters is not recommended.14
Because all of the study participants in this trial were receiving concomitant anticoagulation, it is difficult to generalize results to patients who have contraindications to anticoagulation. Nonetheless, ASCO, NCCN, and several other guideline panels recommend IVC filters only for patients with contraindications to anticoagulation or failure of long-term anticoagulation. NCCN broadens these recommendations for IVC filter placement to include patients with severe cardiac or pulmonary dysfunction.6 However, this recommendation is controversial, given the lack of supporting data, cost, and invasiveness of the procedure.7
All patients with IVC filters without contraindication to anticoagulation should be anticoagulated.9
Prophylaxis: The importance of VTE prophylaxis in all hospitalized patients, including patients with cancer, is under close scrutiny in an attempt to improve patient safety and quality. The Centers for Medicare & Medicaid Services (CMS), in conjunction with the Joint Commission, has added VTE to its list of conditions that are reasonably preventable, and hospitals will no longer be reimbursed for the cost of treatment if acquired during a hospital stay. This rule currently is in effect for knee and hip replacements.15
The need for improvement in aggressive and appropriate prophylaxis of hospitalized patients was demonstrated by a single study in which just one-third of hospitalized patients received appropriate prophylaxis, according to American College of Chest Physicians (ACCP) guidelines.16
Despite a lack of robust data regarding VTE prophylaxis in patients with malignancy, strong data exist for VTE prophylaxis in hospitalized patients. All patients with cancer, and without contraindications to anticoagulation, should receive pharmacologic VTE prophylaxis while hospitalized. In the absence of supporting data, guidelines do not suggest VTE prophylaxis for ambulatory patients with cancer, except in certain multiple myeloma patients.6
Intracranial malignancies: Patients with intracranial malignancies are at risk for VTE, and the presence of intracranial tumors or metastases are not absolute contraindications to anticoagulation. However, data are sparse regarding VTE therapy in this subgroup. Active intracranial bleeding is an absolute contraindication to anticoagulation, and it should be avoided in patients with recent intracranial surgery or thrombocytopenia (e.g., platelet count < 50 x 109).4 In general, the presence of intracranial lesions without high-risk features should not deter the use of prophylactic anticoagulation.
Thrombocytopenia: Cancer patients frequently have chemotherapy-induced cytopenias, including thrombocytopenia. There is a paucity of data regarding anticoagulation in the setting of thrombocytopenia. In a recent review of VTE in the setting of cancer, Lee suggests dose reduction of LMWH by half in patients with platelet counts between 20 and 50 x 109/L.7 At our institution, hematologists suggest halving treatment-dose LMWH at platelet counts between 30 and 50 x 109/L, and discontinuing pharmacologic prophylaxis at platelet counts of less than 50 x 109/L—although there are little data to support these recommendations. Anticoagulation should be discontinued in patients with platelet counts below 20-30 x 109/L, as the risk of bleeding becomes too high.7
Thrombolytic therapy: Catheter-directed thrombolysis or systemic thrombolytic therapy might be appropriate treatment options for acute VTE. Presence of extensive proximal DVT, symptom duration of less than two weeks, life expectancy of greater than one year, good functional status, and low bleeding risk are prerequisites. Anticoagulation recommendations do not change following thrombolytic therapy.17
In the setting of PE, hemodynamic instability is the primary indication for thrombolysis. ACCP does not recommend thrombolytic therapy for the majority of VTE patients.17
Back to the Case
Our patient’s lower-extremity ultrasound and CT of the abdomen and pelvis both revealed extensive clot burden, which likely is related to her underlying pancreatic cancer. She should be started on an LMWH. Given the low likelihood of cure from her cancer, anticoagulation should be continued indefinitely, and an LMWH should be given for at least the first six months. Whether she should be switched to an oral VKA after six months depends on several factors: cost considerations, nutritional status, chemotherapy, presence of cytopenias, and bleeding risk.
IVC filter placement is not indicated at this time, as the patient does not have any contraindications to anticoagulation, has not failed anticoagulation, and does not have impending cardiac or pulmonary compromise. She is not a candidate for thrombolytic therapy due to her poor functional status and limited life expectancy.
Bottom Line
Cancer-associated VTE is increasingly common, and optimally is treated with LMWH for at least six months—indefinitely in the setting of active cancer or treatment. IVC filters have limited and specific indications in the setting of cancer-associated VTE, and should be reserved for situations when anticoagulation is contraindicated. TH
Dr. Weaver is an instructor in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago. Dr. Barsuk is an assistant professor in the division of hospital medicine at Feinberg.
References
- Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer. 2007;110(10): 2339-2346.
- Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olsen RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006(1);119:60-68.
- Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5(3):632-634.
- Lyman GA, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25(34):5490-5505.
- Lyman GH, Khorana AA. Cancer, clots and consensus: new understanding of an old problem. J Clin Oncol. 2009;27(29):4821-4826.
- Khorana AA, Streiff MB, Farge D, et al. Venous thromboembolism prophylaxis and treatment in cancer: a consensus statement of major guidelines panels and call to action. J Clin Oncol. 2009;27(29):4919-4926.
- Lee, AY. Anticoagulation in the treatment of established venous thromboembolism in patients with cancer. J Clin Oncol. 2009;27(29):4895-4901.
- Kuderer NM, Ortel TL, Francis CW. Impact of venous thromboembolism and anticoagulation on cancer and cancer survival. J Clin Oncol. 2009;27(29):4902-4911.
- Prandoni, P. How I treat venous thromboembolism in patients with cancer. Blood. 2005;106(13):4027-4033.
- Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-153.
- Meyer G, Marjanovic Z, Valcke J, et al. Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Intern Med. 2002;162(15):1729-1735.
- Hull RD, Pineo GF, Brant RF, et al. Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med. 2006;119(12):1062-1072.
- Van Dongen CJ, van den Belt AG, Prins MH, Lensing AW. Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2004:18(4);CD001100.
- Decousus H, Leizorovicz A, Parent F, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338(7): 409-415.
- Amin AN, Deitelzweig SB. Optimizing the prevention of venous thromboembolism: recent quality initiatives and strategies to drive improvement. Jt Comm J Qual Patient Saf. 2009;35(11):558-564.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost. 2007;5(8):1610-1616.
- Hirsch J, Guyatt G, Albers W, et al. Executive summary: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed.). Chest. 2008:133(6 Suppl);71S-105S.
Case
A 70-year-old woman with recently diagnosed pancreatic cancer is admitted with worsening abdominal pain and new right-lower-extremity edema. A CT scan of the abdomen and pelvis reveals occlusive IVC and common iliac thromboses. A right-common-femoral DVT appears on Doppler ultrasound. A CT angiogram of her chest is negative for pulmonary emboli. What is the appropriate treatment for this patient’s thromboembolic disease?
Overview
VTE in the setting of malignancy is common, and the incidence of VTE among cancer patients is increasing for unclear reasons.1,2,3 VTE occurs in an estimated 4% to 20% of all malignancy patients. Overall, cancer patients are at a sixfold increased risk of developing VTE compared with the general population, and these patients represent approximately 20% of all VTE cases.4,5
VTE is a leading cause of mortality among hospitalized cancer patients; evidence of VTE exists in up to 50% of cancer patients at autopsy.3,4 VTE complications lead to significant morbidity, including recurrent VTE, pulmonary hypertension, post-thrombophlebitic syndrome, bleeding, and decreased quality of life.6,7
The risk is greatest for hospitalized cancer patients and those receiving active chemotherapy, particularly with such antiangiogenic agents as thalidomide and bevacizumab.4,6 Certain malignancies are more frequently associated with VTE; these include gastrointestinal, gynecologic, brain, lung, renal, and hematologic cancers.4 Table 1 (p. 50) summarizes risk factors associated with VTE in cancer patients.4
Patients with malignancy are hypercoagulable, primarily because of tumor-related alterations in the coagulation cascade.8 Tumors contain cell-surface proteins (e.g., tissue factor and cancer procoagulant) that lead to activation of the clotting cascade via interactions with factors IX and/or X. In addition, tumor-released cytokines cause prothrombotic changes in the vascular endothelium.8
This hypercoagulability is exacerbated by cancer-associated treatment events, including immobility, central venous catheters, erythropoiesis-stimulating agents, and packed red-blood-cell and platelet transfusions.5,9
Cancer-related therapy complications further confound VTE management. Drug interactions, chemotherapy-induced thrombocytopenia, malnutrition, bleeding risk from surgery or tumor location, and liver dysfunction make safe management of cancer-associated VTE a challenge.
Review of the Data
Low-molecular-weight heparin (LMWH) vs. vitamin K antagonists (VKA): There is significant evidence that LMWH is the preferred pharmacologic therapy for the initial and long-term treatment of cancer-related VTE. The most convincing data were published as the CLOT trial, and is supported by several smaller studies.10 Recommendations for the preferred use of LMWH are consistent among several national and international guidelines.6,7
In the CLOT (Randomized Comparison of Low-Molecular-Weight Heparin Versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer) trial, six months of treatment with an oral VKA preceded by five to seven days of LMWH was compared with six months of treatment with LMWH (dalteparin). Patients with the diagnosis of acute symptomatic VTE were evaluated. After six months of treatment, 53 of 336 patients in the oral anticoagulant group had recurrent VTE, compared with 27 of 336 patients in the LMWH group—a relative risk reduction of 52% and an absolute risk reduction of 8% (P=0.002). Complication rates (major and minor bleeding) and overall mortality were similar between the two groups.7,10
Two smaller trials compared LMWHs with warfarin in the treatment of VTE in the setting of cancer. In one trial, seven of 67 enoxaparin-treated patients developed bleeding or recurrent VTE, compared with 15 of 71 warfarin-treated subjects; however, this reduction was not statistically significant (P=0.09).11 In another trial, seven of 100 tinzaparin-treated patients developed recurrent VTE, compared with 16 of 100 warfarin-treated patients (P=0.044).12
Thus, LMWH is the preferred therapeutic agent for both DVT and PE in the setting of malignancy.5 Even so, although the clinical evidence supports LMWH use in the treatment of cancer-associated VTE, it’s worth noting that many of the authors of the cited papers received compensation from large pharmaceutical companies. In addition, the CLOT trial was funded by Pharmacia, which supplied the study drug.
Initial treatment (5-10 days): The American Society of Clinical Oncology (ASCO) guidelines advocate the use of LMWH during the initial five to 10 days following VTE diagnosis. Four other cancer research organization guidelines, National Comprehensive Cancer Network (NCCN), the Italian Association of Medical Oncology (AIOM), the European Society of Medical Oncology (ESMO), and the French National Federation of the League of Centers Against Cancer (FNCLCC), echo this approach, with unfractionated heparin (UFH) or fondaparinux as additional initial treatment depending on the clinical situation—i.e., renal failure, heparin-induced thrombocytopenia (HIT), or bleeding risk.6
Table 2 (below) summarizes recommendations for VTE treatment in cancer patients from all five guideline panels.6
Long-term treatment and duration (3-6 months): All of the panels agree LMWH is the preferred agent for long-term therapy of cancer-related VTE. ASCO supports treatment with LMWH for at least six months; oral VKAs with a targeted INR of 2 to 3 are acceptable when LMWH is not feasible. NCCN, AIOM, ESMO, and FNCLCC recommend an LMWH treatment duration from three to six months (ASCO recommends at least six months).
All of the panels, however, advocate indefinite duration of anticoagulation in patients with such continuing risk factors as active (metastatic, recurrent, or persistent) cancer or chemotherapy treatment.6 AIOM and ESMO specify indefinite LMWH, whereas ASCO does not specify oral VKA or LMWH use. Given the difficulties of managing VKA in the setting of advanced malignancy or chemotherapy, LMWH is the most practical choice, if it’s available and isn’t cost-prohibitive.
LMWH availability: Dalteparin, tinzaparin, and enoxaparin are LMWHs currently available in the U.S. for VTE treatment. Dalteparin is the only FDA-approved LMWH drug for long-term use to treat cancer-associated VTE, although enoxaparin and tinzaparin are used in practice. All three are supplied in prefilled syringes, which make self-administration easier and significantly reduce the risk of dosage error.6
LMWH vs. UFH: LMWH is safer and more efficacious than UFH. A summary of 22 clinical trials (including cancer patients and noncancer patients) by a Cochrane systematic review showed that treatment with LMWH in comparison with UFH results in decreased recurrent VTE, bleeding, mortality, HIT, and osteoporosis.7,13
Other agents: Fondaparinux is a factor Xa inhibitor rarely associated with heparin-induced thrombocytopenia (HIT), which makes it an attractive alternate anticoagulant for HIT patients. Its use in comparison with other parenteral anticoagulants has not been established in patients with malignancy.
Fondaparinux is FDA-approved for initial VTE treatment, and is used in practice as an alternative prophylactic anticoagulant for patients with HIT history or heparin allergy.7 However, no randomized clinical trials have evaluated its efficacy in patients with HIT.
Several new oral anticoagulants, including direct thrombin and factor Xa inhibitors, are being investigated; efficacy has not been established in cancer patients.7
Inferior vena cava (IVC) filters: Limited data surround the use of IVC filters, and most consensus guidelines recommend their use only in specific settings. One randomized controlled study (not limited to patients with cancer) showed no difference in overall short-term or long-term survival among patients receiving IVC filters for VTE treatment. However, there was a decrease in symptomatic PE in the filter group 12 days after placement. The tradeoff was significantly more recurrent DVTs at two years’ followup. The authors concluded that systematic use of IVC filters is not recommended.14
Because all of the study participants in this trial were receiving concomitant anticoagulation, it is difficult to generalize results to patients who have contraindications to anticoagulation. Nonetheless, ASCO, NCCN, and several other guideline panels recommend IVC filters only for patients with contraindications to anticoagulation or failure of long-term anticoagulation. NCCN broadens these recommendations for IVC filter placement to include patients with severe cardiac or pulmonary dysfunction.6 However, this recommendation is controversial, given the lack of supporting data, cost, and invasiveness of the procedure.7
All patients with IVC filters without contraindication to anticoagulation should be anticoagulated.9
Prophylaxis: The importance of VTE prophylaxis in all hospitalized patients, including patients with cancer, is under close scrutiny in an attempt to improve patient safety and quality. The Centers for Medicare & Medicaid Services (CMS), in conjunction with the Joint Commission, has added VTE to its list of conditions that are reasonably preventable, and hospitals will no longer be reimbursed for the cost of treatment if acquired during a hospital stay. This rule currently is in effect for knee and hip replacements.15
The need for improvement in aggressive and appropriate prophylaxis of hospitalized patients was demonstrated by a single study in which just one-third of hospitalized patients received appropriate prophylaxis, according to American College of Chest Physicians (ACCP) guidelines.16
Despite a lack of robust data regarding VTE prophylaxis in patients with malignancy, strong data exist for VTE prophylaxis in hospitalized patients. All patients with cancer, and without contraindications to anticoagulation, should receive pharmacologic VTE prophylaxis while hospitalized. In the absence of supporting data, guidelines do not suggest VTE prophylaxis for ambulatory patients with cancer, except in certain multiple myeloma patients.6
Intracranial malignancies: Patients with intracranial malignancies are at risk for VTE, and the presence of intracranial tumors or metastases are not absolute contraindications to anticoagulation. However, data are sparse regarding VTE therapy in this subgroup. Active intracranial bleeding is an absolute contraindication to anticoagulation, and it should be avoided in patients with recent intracranial surgery or thrombocytopenia (e.g., platelet count < 50 x 109).4 In general, the presence of intracranial lesions without high-risk features should not deter the use of prophylactic anticoagulation.
Thrombocytopenia: Cancer patients frequently have chemotherapy-induced cytopenias, including thrombocytopenia. There is a paucity of data regarding anticoagulation in the setting of thrombocytopenia. In a recent review of VTE in the setting of cancer, Lee suggests dose reduction of LMWH by half in patients with platelet counts between 20 and 50 x 109/L.7 At our institution, hematologists suggest halving treatment-dose LMWH at platelet counts between 30 and 50 x 109/L, and discontinuing pharmacologic prophylaxis at platelet counts of less than 50 x 109/L—although there are little data to support these recommendations. Anticoagulation should be discontinued in patients with platelet counts below 20-30 x 109/L, as the risk of bleeding becomes too high.7
Thrombolytic therapy: Catheter-directed thrombolysis or systemic thrombolytic therapy might be appropriate treatment options for acute VTE. Presence of extensive proximal DVT, symptom duration of less than two weeks, life expectancy of greater than one year, good functional status, and low bleeding risk are prerequisites. Anticoagulation recommendations do not change following thrombolytic therapy.17
In the setting of PE, hemodynamic instability is the primary indication for thrombolysis. ACCP does not recommend thrombolytic therapy for the majority of VTE patients.17
Back to the Case
Our patient’s lower-extremity ultrasound and CT of the abdomen and pelvis both revealed extensive clot burden, which likely is related to her underlying pancreatic cancer. She should be started on an LMWH. Given the low likelihood of cure from her cancer, anticoagulation should be continued indefinitely, and an LMWH should be given for at least the first six months. Whether she should be switched to an oral VKA after six months depends on several factors: cost considerations, nutritional status, chemotherapy, presence of cytopenias, and bleeding risk.
IVC filter placement is not indicated at this time, as the patient does not have any contraindications to anticoagulation, has not failed anticoagulation, and does not have impending cardiac or pulmonary compromise. She is not a candidate for thrombolytic therapy due to her poor functional status and limited life expectancy.
Bottom Line
Cancer-associated VTE is increasingly common, and optimally is treated with LMWH for at least six months—indefinitely in the setting of active cancer or treatment. IVC filters have limited and specific indications in the setting of cancer-associated VTE, and should be reserved for situations when anticoagulation is contraindicated. TH
Dr. Weaver is an instructor in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago. Dr. Barsuk is an assistant professor in the division of hospital medicine at Feinberg.
References
- Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer. 2007;110(10): 2339-2346.
- Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olsen RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006(1);119:60-68.
- Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5(3):632-634.
- Lyman GA, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25(34):5490-5505.
- Lyman GH, Khorana AA. Cancer, clots and consensus: new understanding of an old problem. J Clin Oncol. 2009;27(29):4821-4826.
- Khorana AA, Streiff MB, Farge D, et al. Venous thromboembolism prophylaxis and treatment in cancer: a consensus statement of major guidelines panels and call to action. J Clin Oncol. 2009;27(29):4919-4926.
- Lee, AY. Anticoagulation in the treatment of established venous thromboembolism in patients with cancer. J Clin Oncol. 2009;27(29):4895-4901.
- Kuderer NM, Ortel TL, Francis CW. Impact of venous thromboembolism and anticoagulation on cancer and cancer survival. J Clin Oncol. 2009;27(29):4902-4911.
- Prandoni, P. How I treat venous thromboembolism in patients with cancer. Blood. 2005;106(13):4027-4033.
- Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-153.
- Meyer G, Marjanovic Z, Valcke J, et al. Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Intern Med. 2002;162(15):1729-1735.
- Hull RD, Pineo GF, Brant RF, et al. Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med. 2006;119(12):1062-1072.
- Van Dongen CJ, van den Belt AG, Prins MH, Lensing AW. Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2004:18(4);CD001100.
- Decousus H, Leizorovicz A, Parent F, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338(7): 409-415.
- Amin AN, Deitelzweig SB. Optimizing the prevention of venous thromboembolism: recent quality initiatives and strategies to drive improvement. Jt Comm J Qual Patient Saf. 2009;35(11):558-564.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost. 2007;5(8):1610-1616.
- Hirsch J, Guyatt G, Albers W, et al. Executive summary: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed.). Chest. 2008:133(6 Suppl);71S-105S.
Case
A 70-year-old woman with recently diagnosed pancreatic cancer is admitted with worsening abdominal pain and new right-lower-extremity edema. A CT scan of the abdomen and pelvis reveals occlusive IVC and common iliac thromboses. A right-common-femoral DVT appears on Doppler ultrasound. A CT angiogram of her chest is negative for pulmonary emboli. What is the appropriate treatment for this patient’s thromboembolic disease?
Overview
VTE in the setting of malignancy is common, and the incidence of VTE among cancer patients is increasing for unclear reasons.1,2,3 VTE occurs in an estimated 4% to 20% of all malignancy patients. Overall, cancer patients are at a sixfold increased risk of developing VTE compared with the general population, and these patients represent approximately 20% of all VTE cases.4,5
VTE is a leading cause of mortality among hospitalized cancer patients; evidence of VTE exists in up to 50% of cancer patients at autopsy.3,4 VTE complications lead to significant morbidity, including recurrent VTE, pulmonary hypertension, post-thrombophlebitic syndrome, bleeding, and decreased quality of life.6,7
The risk is greatest for hospitalized cancer patients and those receiving active chemotherapy, particularly with such antiangiogenic agents as thalidomide and bevacizumab.4,6 Certain malignancies are more frequently associated with VTE; these include gastrointestinal, gynecologic, brain, lung, renal, and hematologic cancers.4 Table 1 (p. 50) summarizes risk factors associated with VTE in cancer patients.4
Patients with malignancy are hypercoagulable, primarily because of tumor-related alterations in the coagulation cascade.8 Tumors contain cell-surface proteins (e.g., tissue factor and cancer procoagulant) that lead to activation of the clotting cascade via interactions with factors IX and/or X. In addition, tumor-released cytokines cause prothrombotic changes in the vascular endothelium.8
This hypercoagulability is exacerbated by cancer-associated treatment events, including immobility, central venous catheters, erythropoiesis-stimulating agents, and packed red-blood-cell and platelet transfusions.5,9
Cancer-related therapy complications further confound VTE management. Drug interactions, chemotherapy-induced thrombocytopenia, malnutrition, bleeding risk from surgery or tumor location, and liver dysfunction make safe management of cancer-associated VTE a challenge.
Review of the Data
Low-molecular-weight heparin (LMWH) vs. vitamin K antagonists (VKA): There is significant evidence that LMWH is the preferred pharmacologic therapy for the initial and long-term treatment of cancer-related VTE. The most convincing data were published as the CLOT trial, and is supported by several smaller studies.10 Recommendations for the preferred use of LMWH are consistent among several national and international guidelines.6,7
In the CLOT (Randomized Comparison of Low-Molecular-Weight Heparin Versus Oral Anticoagulant Therapy for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer) trial, six months of treatment with an oral VKA preceded by five to seven days of LMWH was compared with six months of treatment with LMWH (dalteparin). Patients with the diagnosis of acute symptomatic VTE were evaluated. After six months of treatment, 53 of 336 patients in the oral anticoagulant group had recurrent VTE, compared with 27 of 336 patients in the LMWH group—a relative risk reduction of 52% and an absolute risk reduction of 8% (P=0.002). Complication rates (major and minor bleeding) and overall mortality were similar between the two groups.7,10
Two smaller trials compared LMWHs with warfarin in the treatment of VTE in the setting of cancer. In one trial, seven of 67 enoxaparin-treated patients developed bleeding or recurrent VTE, compared with 15 of 71 warfarin-treated subjects; however, this reduction was not statistically significant (P=0.09).11 In another trial, seven of 100 tinzaparin-treated patients developed recurrent VTE, compared with 16 of 100 warfarin-treated patients (P=0.044).12
Thus, LMWH is the preferred therapeutic agent for both DVT and PE in the setting of malignancy.5 Even so, although the clinical evidence supports LMWH use in the treatment of cancer-associated VTE, it’s worth noting that many of the authors of the cited papers received compensation from large pharmaceutical companies. In addition, the CLOT trial was funded by Pharmacia, which supplied the study drug.
Initial treatment (5-10 days): The American Society of Clinical Oncology (ASCO) guidelines advocate the use of LMWH during the initial five to 10 days following VTE diagnosis. Four other cancer research organization guidelines, National Comprehensive Cancer Network (NCCN), the Italian Association of Medical Oncology (AIOM), the European Society of Medical Oncology (ESMO), and the French National Federation of the League of Centers Against Cancer (FNCLCC), echo this approach, with unfractionated heparin (UFH) or fondaparinux as additional initial treatment depending on the clinical situation—i.e., renal failure, heparin-induced thrombocytopenia (HIT), or bleeding risk.6
Table 2 (below) summarizes recommendations for VTE treatment in cancer patients from all five guideline panels.6
Long-term treatment and duration (3-6 months): All of the panels agree LMWH is the preferred agent for long-term therapy of cancer-related VTE. ASCO supports treatment with LMWH for at least six months; oral VKAs with a targeted INR of 2 to 3 are acceptable when LMWH is not feasible. NCCN, AIOM, ESMO, and FNCLCC recommend an LMWH treatment duration from three to six months (ASCO recommends at least six months).
All of the panels, however, advocate indefinite duration of anticoagulation in patients with such continuing risk factors as active (metastatic, recurrent, or persistent) cancer or chemotherapy treatment.6 AIOM and ESMO specify indefinite LMWH, whereas ASCO does not specify oral VKA or LMWH use. Given the difficulties of managing VKA in the setting of advanced malignancy or chemotherapy, LMWH is the most practical choice, if it’s available and isn’t cost-prohibitive.
LMWH availability: Dalteparin, tinzaparin, and enoxaparin are LMWHs currently available in the U.S. for VTE treatment. Dalteparin is the only FDA-approved LMWH drug for long-term use to treat cancer-associated VTE, although enoxaparin and tinzaparin are used in practice. All three are supplied in prefilled syringes, which make self-administration easier and significantly reduce the risk of dosage error.6
LMWH vs. UFH: LMWH is safer and more efficacious than UFH. A summary of 22 clinical trials (including cancer patients and noncancer patients) by a Cochrane systematic review showed that treatment with LMWH in comparison with UFH results in decreased recurrent VTE, bleeding, mortality, HIT, and osteoporosis.7,13
Other agents: Fondaparinux is a factor Xa inhibitor rarely associated with heparin-induced thrombocytopenia (HIT), which makes it an attractive alternate anticoagulant for HIT patients. Its use in comparison with other parenteral anticoagulants has not been established in patients with malignancy.
Fondaparinux is FDA-approved for initial VTE treatment, and is used in practice as an alternative prophylactic anticoagulant for patients with HIT history or heparin allergy.7 However, no randomized clinical trials have evaluated its efficacy in patients with HIT.
Several new oral anticoagulants, including direct thrombin and factor Xa inhibitors, are being investigated; efficacy has not been established in cancer patients.7
Inferior vena cava (IVC) filters: Limited data surround the use of IVC filters, and most consensus guidelines recommend their use only in specific settings. One randomized controlled study (not limited to patients with cancer) showed no difference in overall short-term or long-term survival among patients receiving IVC filters for VTE treatment. However, there was a decrease in symptomatic PE in the filter group 12 days after placement. The tradeoff was significantly more recurrent DVTs at two years’ followup. The authors concluded that systematic use of IVC filters is not recommended.14
Because all of the study participants in this trial were receiving concomitant anticoagulation, it is difficult to generalize results to patients who have contraindications to anticoagulation. Nonetheless, ASCO, NCCN, and several other guideline panels recommend IVC filters only for patients with contraindications to anticoagulation or failure of long-term anticoagulation. NCCN broadens these recommendations for IVC filter placement to include patients with severe cardiac or pulmonary dysfunction.6 However, this recommendation is controversial, given the lack of supporting data, cost, and invasiveness of the procedure.7
All patients with IVC filters without contraindication to anticoagulation should be anticoagulated.9
Prophylaxis: The importance of VTE prophylaxis in all hospitalized patients, including patients with cancer, is under close scrutiny in an attempt to improve patient safety and quality. The Centers for Medicare & Medicaid Services (CMS), in conjunction with the Joint Commission, has added VTE to its list of conditions that are reasonably preventable, and hospitals will no longer be reimbursed for the cost of treatment if acquired during a hospital stay. This rule currently is in effect for knee and hip replacements.15
The need for improvement in aggressive and appropriate prophylaxis of hospitalized patients was demonstrated by a single study in which just one-third of hospitalized patients received appropriate prophylaxis, according to American College of Chest Physicians (ACCP) guidelines.16
Despite a lack of robust data regarding VTE prophylaxis in patients with malignancy, strong data exist for VTE prophylaxis in hospitalized patients. All patients with cancer, and without contraindications to anticoagulation, should receive pharmacologic VTE prophylaxis while hospitalized. In the absence of supporting data, guidelines do not suggest VTE prophylaxis for ambulatory patients with cancer, except in certain multiple myeloma patients.6
Intracranial malignancies: Patients with intracranial malignancies are at risk for VTE, and the presence of intracranial tumors or metastases are not absolute contraindications to anticoagulation. However, data are sparse regarding VTE therapy in this subgroup. Active intracranial bleeding is an absolute contraindication to anticoagulation, and it should be avoided in patients with recent intracranial surgery or thrombocytopenia (e.g., platelet count < 50 x 109).4 In general, the presence of intracranial lesions without high-risk features should not deter the use of prophylactic anticoagulation.
Thrombocytopenia: Cancer patients frequently have chemotherapy-induced cytopenias, including thrombocytopenia. There is a paucity of data regarding anticoagulation in the setting of thrombocytopenia. In a recent review of VTE in the setting of cancer, Lee suggests dose reduction of LMWH by half in patients with platelet counts between 20 and 50 x 109/L.7 At our institution, hematologists suggest halving treatment-dose LMWH at platelet counts between 30 and 50 x 109/L, and discontinuing pharmacologic prophylaxis at platelet counts of less than 50 x 109/L—although there are little data to support these recommendations. Anticoagulation should be discontinued in patients with platelet counts below 20-30 x 109/L, as the risk of bleeding becomes too high.7
Thrombolytic therapy: Catheter-directed thrombolysis or systemic thrombolytic therapy might be appropriate treatment options for acute VTE. Presence of extensive proximal DVT, symptom duration of less than two weeks, life expectancy of greater than one year, good functional status, and low bleeding risk are prerequisites. Anticoagulation recommendations do not change following thrombolytic therapy.17
In the setting of PE, hemodynamic instability is the primary indication for thrombolysis. ACCP does not recommend thrombolytic therapy for the majority of VTE patients.17
Back to the Case
Our patient’s lower-extremity ultrasound and CT of the abdomen and pelvis both revealed extensive clot burden, which likely is related to her underlying pancreatic cancer. She should be started on an LMWH. Given the low likelihood of cure from her cancer, anticoagulation should be continued indefinitely, and an LMWH should be given for at least the first six months. Whether she should be switched to an oral VKA after six months depends on several factors: cost considerations, nutritional status, chemotherapy, presence of cytopenias, and bleeding risk.
IVC filter placement is not indicated at this time, as the patient does not have any contraindications to anticoagulation, has not failed anticoagulation, and does not have impending cardiac or pulmonary compromise. She is not a candidate for thrombolytic therapy due to her poor functional status and limited life expectancy.
Bottom Line
Cancer-associated VTE is increasingly common, and optimally is treated with LMWH for at least six months—indefinitely in the setting of active cancer or treatment. IVC filters have limited and specific indications in the setting of cancer-associated VTE, and should be reserved for situations when anticoagulation is contraindicated. TH
Dr. Weaver is an instructor in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago. Dr. Barsuk is an assistant professor in the division of hospital medicine at Feinberg.
References
- Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer. 2007;110(10): 2339-2346.
- Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olsen RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006(1);119:60-68.
- Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5(3):632-634.
- Lyman GA, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25(34):5490-5505.
- Lyman GH, Khorana AA. Cancer, clots and consensus: new understanding of an old problem. J Clin Oncol. 2009;27(29):4821-4826.
- Khorana AA, Streiff MB, Farge D, et al. Venous thromboembolism prophylaxis and treatment in cancer: a consensus statement of major guidelines panels and call to action. J Clin Oncol. 2009;27(29):4919-4926.
- Lee, AY. Anticoagulation in the treatment of established venous thromboembolism in patients with cancer. J Clin Oncol. 2009;27(29):4895-4901.
- Kuderer NM, Ortel TL, Francis CW. Impact of venous thromboembolism and anticoagulation on cancer and cancer survival. J Clin Oncol. 2009;27(29):4902-4911.
- Prandoni, P. How I treat venous thromboembolism in patients with cancer. Blood. 2005;106(13):4027-4033.
- Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146-153.
- Meyer G, Marjanovic Z, Valcke J, et al. Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Intern Med. 2002;162(15):1729-1735.
- Hull RD, Pineo GF, Brant RF, et al. Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med. 2006;119(12):1062-1072.
- Van Dongen CJ, van den Belt AG, Prins MH, Lensing AW. Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2004:18(4);CD001100.
- Decousus H, Leizorovicz A, Parent F, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998;338(7): 409-415.
- Amin AN, Deitelzweig SB. Optimizing the prevention of venous thromboembolism: recent quality initiatives and strategies to drive improvement. Jt Comm J Qual Patient Saf. 2009;35(11):558-564.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost. 2007;5(8):1610-1616.
- Hirsch J, Guyatt G, Albers W, et al. Executive summary: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed.). Chest. 2008:133(6 Suppl);71S-105S.
Discharge Services
Discharge day management services (99238-99239) seem unlikely to cause confusion in the physician community; however, continued requests for documentation involving these CPT codes prove the opposite.
Here’s an example of how a billing error might be made for discharge day management services. A patient with diabetes mellitus, hypertension, and chronic kidney disease is stable for discharge. The patient is being transferred to a skilled nursing facility (SNF). Dr. Aardsma prepares the patient for hospital discharge, and Dr. Broxton admits the patient to the SNF later that day. Dr. Aardsma and Dr. Broxton are members of the same group practice, with the same specialty designation. Can both physicians report their services?
Key Elements
Consider the basic billing principles of discharge services: what, who, and when.
Hospital discharge day management codes are used to report the physician’s total duration of time spent preparing the patient for discharge. These codes include, as appropriate:
- Final examination of the patient;
- Discussion of the hospital stay, even if the time spent by the physician on that date is not continuous;
- Instructions for continuing care to all relevant caregivers; and
- Preparation of discharge records, prescriptions, and referral forms.1
Hospitalists should report one discharge code per hospitalization, but only when the service occurs after the initial date of admission: 99238, hospital discharge day management, 30 minutes or less; or 99239, hospital discharge day management, more than 30 minutes.1,2 Select one of the two codes, depending upon the cumulative discharge service time provided on the patient’s hospital unit/floor during a single calendar day. Do not count time for services performed outside of the patient’s unit or floor (i.e., calls to the receiving physician/facility made from the physician’s private office) or services performed after the patient physically leaves the hospital.
Physician documentation must refer to the discharge status, as well as other clinically relevant information. Don’t be misled into believing that the presence of a discharge summary alone satisfies documentation requirements. In addition to the discharge groundwork, hospitalists must physically see the patient on the day he or she reports discharge management. Discharge summaries are not always useful in noting the physician’s required face-to-face encounter with the patient. Simply state, “Patient seen and examined by me on discharge day.”
Alternatively, hospitalists can elect to include details of a discharge day exam. Although a final exam isn’t mandatory for billing 99238-99239, it is the best justification of a face-to-face encounter on discharge day. Documentation of the time is required when reporting 99239 (e.g., discharge time >30 minutes). Time isn’t typically included in a discharge summary, and upon post-payment payor review, a claim involving 99239 without documented time in the patient’s medical record might result in either a service reduction to the lower level of care (99238) or a request for payment refund.3 Physicians can document all necessary details in the formal summary or a progress note.
Transfers of Care
The admitting physician or group is responsible for performing discharge services unless a formal transfer of care occurs, such as the patient’s transfer from the ICU to the standard medical floor as the patient’s condition improves. Without this transfer of care, comanaging physicians should merely report subsequent hospital-care codes (99231-99233) for the final patient encounter. An example of this is surgical comanagement: If a surgeon is identified as the attending of record, they are responsible for postoperative management of the patient, including discharge services.4,5 Providers in a different group or specialty report 99231-99233 for their medically necessary care.
As with all other time-based services, only the billing provider’s time counts. Discharge-related services performed by residents, students, or ancillary staff (i.e., RNs) do not count toward the physician’s discharge service time. Report the date of the physician’s actual discharge visit even if the patient leaves the facility on a different calendar date—for example, if a patient leaves the next day due to availability of the receiving facility.
Pronouncement of Death
Physicians might not realize that they can report discharge day management codes for pronouncement of death.7 Only the hospitalist who performs the pronouncement is allowed to report this service on the date pronouncement occurred, even if the paperwork is delayed to a subsequent date. Completion of the death certificate alone is not sufficient for billing. Hospitalists must “examine” the patient, thus satisfying the “face to face” visit requirement.
Additional services (e.g., speaking with family members, speaking with healthcare providers, filling out the necessary documentation) count toward the cumulative discharge service time, if performed on the patient’s unit or floor. Document the cumulative time when reporting 99239.
Back to the Case
Typical billing and payment rules mandate the reporting of only one E/M service per specialty, per patient, per day. One of the few exceptions involves reporting a hospital discharge code (99238-99239) with initial nursing facility care (99304-99306). Either the same physician or different physicians from the same group and specialty can report the hospital discharge and the nursing facility admission on the same day. When the same physician or group discharges the patient from any other location (e.g., observation unit) on the same day, report only one service: either the observation discharge (99217) or the initial nursing facility care (99304-99306).
When the same physician or group discharges a patient from the hospital and admits the patient to a facility other than a nursing facility on the same day, report only one service: either the hospital discharge (99228-99239) or the admission care (e.g., long-term acute-care hospital: 99221-99223). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1C. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 3, 2010.
- Highmark Medicare Services Provider Bulletins: Hospital Discharge Day Management Codes 99238 and 99239. Highmark Medicare Services Web site. Available at: www.highmarkmedicareservices.com/bulletins/partb/news02212008a.html. Accessed March 4, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.1A. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.3B. Centers for Medicare & Medicaid Services Web site, Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2E. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1d. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Reporting inpatient hospital evaluation and management (E/M) services that could be described by current procedural terminology (CPT) consultation codes. Cigna Government Services Web site. Available at: www.cignagovernmentservices.com/partb/pubs/news/2010/0210/cope11694.html. Accessed March 5, 2010.
Discharge day management services (99238-99239) seem unlikely to cause confusion in the physician community; however, continued requests for documentation involving these CPT codes prove the opposite.
Here’s an example of how a billing error might be made for discharge day management services. A patient with diabetes mellitus, hypertension, and chronic kidney disease is stable for discharge. The patient is being transferred to a skilled nursing facility (SNF). Dr. Aardsma prepares the patient for hospital discharge, and Dr. Broxton admits the patient to the SNF later that day. Dr. Aardsma and Dr. Broxton are members of the same group practice, with the same specialty designation. Can both physicians report their services?
Key Elements
Consider the basic billing principles of discharge services: what, who, and when.
Hospital discharge day management codes are used to report the physician’s total duration of time spent preparing the patient for discharge. These codes include, as appropriate:
- Final examination of the patient;
- Discussion of the hospital stay, even if the time spent by the physician on that date is not continuous;
- Instructions for continuing care to all relevant caregivers; and
- Preparation of discharge records, prescriptions, and referral forms.1
Hospitalists should report one discharge code per hospitalization, but only when the service occurs after the initial date of admission: 99238, hospital discharge day management, 30 minutes or less; or 99239, hospital discharge day management, more than 30 minutes.1,2 Select one of the two codes, depending upon the cumulative discharge service time provided on the patient’s hospital unit/floor during a single calendar day. Do not count time for services performed outside of the patient’s unit or floor (i.e., calls to the receiving physician/facility made from the physician’s private office) or services performed after the patient physically leaves the hospital.
Physician documentation must refer to the discharge status, as well as other clinically relevant information. Don’t be misled into believing that the presence of a discharge summary alone satisfies documentation requirements. In addition to the discharge groundwork, hospitalists must physically see the patient on the day he or she reports discharge management. Discharge summaries are not always useful in noting the physician’s required face-to-face encounter with the patient. Simply state, “Patient seen and examined by me on discharge day.”
Alternatively, hospitalists can elect to include details of a discharge day exam. Although a final exam isn’t mandatory for billing 99238-99239, it is the best justification of a face-to-face encounter on discharge day. Documentation of the time is required when reporting 99239 (e.g., discharge time >30 minutes). Time isn’t typically included in a discharge summary, and upon post-payment payor review, a claim involving 99239 without documented time in the patient’s medical record might result in either a service reduction to the lower level of care (99238) or a request for payment refund.3 Physicians can document all necessary details in the formal summary or a progress note.
Transfers of Care
The admitting physician or group is responsible for performing discharge services unless a formal transfer of care occurs, such as the patient’s transfer from the ICU to the standard medical floor as the patient’s condition improves. Without this transfer of care, comanaging physicians should merely report subsequent hospital-care codes (99231-99233) for the final patient encounter. An example of this is surgical comanagement: If a surgeon is identified as the attending of record, they are responsible for postoperative management of the patient, including discharge services.4,5 Providers in a different group or specialty report 99231-99233 for their medically necessary care.
As with all other time-based services, only the billing provider’s time counts. Discharge-related services performed by residents, students, or ancillary staff (i.e., RNs) do not count toward the physician’s discharge service time. Report the date of the physician’s actual discharge visit even if the patient leaves the facility on a different calendar date—for example, if a patient leaves the next day due to availability of the receiving facility.
Pronouncement of Death
Physicians might not realize that they can report discharge day management codes for pronouncement of death.7 Only the hospitalist who performs the pronouncement is allowed to report this service on the date pronouncement occurred, even if the paperwork is delayed to a subsequent date. Completion of the death certificate alone is not sufficient for billing. Hospitalists must “examine” the patient, thus satisfying the “face to face” visit requirement.
Additional services (e.g., speaking with family members, speaking with healthcare providers, filling out the necessary documentation) count toward the cumulative discharge service time, if performed on the patient’s unit or floor. Document the cumulative time when reporting 99239.
Back to the Case
Typical billing and payment rules mandate the reporting of only one E/M service per specialty, per patient, per day. One of the few exceptions involves reporting a hospital discharge code (99238-99239) with initial nursing facility care (99304-99306). Either the same physician or different physicians from the same group and specialty can report the hospital discharge and the nursing facility admission on the same day. When the same physician or group discharges the patient from any other location (e.g., observation unit) on the same day, report only one service: either the observation discharge (99217) or the initial nursing facility care (99304-99306).
When the same physician or group discharges a patient from the hospital and admits the patient to a facility other than a nursing facility on the same day, report only one service: either the hospital discharge (99228-99239) or the admission care (e.g., long-term acute-care hospital: 99221-99223). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1C. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 3, 2010.
- Highmark Medicare Services Provider Bulletins: Hospital Discharge Day Management Codes 99238 and 99239. Highmark Medicare Services Web site. Available at: www.highmarkmedicareservices.com/bulletins/partb/news02212008a.html. Accessed March 4, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.1A. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.3B. Centers for Medicare & Medicaid Services Web site, Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2E. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1d. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Reporting inpatient hospital evaluation and management (E/M) services that could be described by current procedural terminology (CPT) consultation codes. Cigna Government Services Web site. Available at: www.cignagovernmentservices.com/partb/pubs/news/2010/0210/cope11694.html. Accessed March 5, 2010.
Discharge day management services (99238-99239) seem unlikely to cause confusion in the physician community; however, continued requests for documentation involving these CPT codes prove the opposite.
Here’s an example of how a billing error might be made for discharge day management services. A patient with diabetes mellitus, hypertension, and chronic kidney disease is stable for discharge. The patient is being transferred to a skilled nursing facility (SNF). Dr. Aardsma prepares the patient for hospital discharge, and Dr. Broxton admits the patient to the SNF later that day. Dr. Aardsma and Dr. Broxton are members of the same group practice, with the same specialty designation. Can both physicians report their services?
Key Elements
Consider the basic billing principles of discharge services: what, who, and when.
Hospital discharge day management codes are used to report the physician’s total duration of time spent preparing the patient for discharge. These codes include, as appropriate:
- Final examination of the patient;
- Discussion of the hospital stay, even if the time spent by the physician on that date is not continuous;
- Instructions for continuing care to all relevant caregivers; and
- Preparation of discharge records, prescriptions, and referral forms.1
Hospitalists should report one discharge code per hospitalization, but only when the service occurs after the initial date of admission: 99238, hospital discharge day management, 30 minutes or less; or 99239, hospital discharge day management, more than 30 minutes.1,2 Select one of the two codes, depending upon the cumulative discharge service time provided on the patient’s hospital unit/floor during a single calendar day. Do not count time for services performed outside of the patient’s unit or floor (i.e., calls to the receiving physician/facility made from the physician’s private office) or services performed after the patient physically leaves the hospital.
Physician documentation must refer to the discharge status, as well as other clinically relevant information. Don’t be misled into believing that the presence of a discharge summary alone satisfies documentation requirements. In addition to the discharge groundwork, hospitalists must physically see the patient on the day he or she reports discharge management. Discharge summaries are not always useful in noting the physician’s required face-to-face encounter with the patient. Simply state, “Patient seen and examined by me on discharge day.”
Alternatively, hospitalists can elect to include details of a discharge day exam. Although a final exam isn’t mandatory for billing 99238-99239, it is the best justification of a face-to-face encounter on discharge day. Documentation of the time is required when reporting 99239 (e.g., discharge time >30 minutes). Time isn’t typically included in a discharge summary, and upon post-payment payor review, a claim involving 99239 without documented time in the patient’s medical record might result in either a service reduction to the lower level of care (99238) or a request for payment refund.3 Physicians can document all necessary details in the formal summary or a progress note.
Transfers of Care
The admitting physician or group is responsible for performing discharge services unless a formal transfer of care occurs, such as the patient’s transfer from the ICU to the standard medical floor as the patient’s condition improves. Without this transfer of care, comanaging physicians should merely report subsequent hospital-care codes (99231-99233) for the final patient encounter. An example of this is surgical comanagement: If a surgeon is identified as the attending of record, they are responsible for postoperative management of the patient, including discharge services.4,5 Providers in a different group or specialty report 99231-99233 for their medically necessary care.
As with all other time-based services, only the billing provider’s time counts. Discharge-related services performed by residents, students, or ancillary staff (i.e., RNs) do not count toward the physician’s discharge service time. Report the date of the physician’s actual discharge visit even if the patient leaves the facility on a different calendar date—for example, if a patient leaves the next day due to availability of the receiving facility.
Pronouncement of Death
Physicians might not realize that they can report discharge day management codes for pronouncement of death.7 Only the hospitalist who performs the pronouncement is allowed to report this service on the date pronouncement occurred, even if the paperwork is delayed to a subsequent date. Completion of the death certificate alone is not sufficient for billing. Hospitalists must “examine” the patient, thus satisfying the “face to face” visit requirement.
Additional services (e.g., speaking with family members, speaking with healthcare providers, filling out the necessary documentation) count toward the cumulative discharge service time, if performed on the patient’s unit or floor. Document the cumulative time when reporting 99239.
Back to the Case
Typical billing and payment rules mandate the reporting of only one E/M service per specialty, per patient, per day. One of the few exceptions involves reporting a hospital discharge code (99238-99239) with initial nursing facility care (99304-99306). Either the same physician or different physicians from the same group and specialty can report the hospital discharge and the nursing facility admission on the same day. When the same physician or group discharges the patient from any other location (e.g., observation unit) on the same day, report only one service: either the observation discharge (99217) or the initial nursing facility care (99304-99306).
When the same physician or group discharges a patient from the hospital and admits the patient to a facility other than a nursing facility on the same day, report only one service: either the hospital discharge (99228-99239) or the admission care (e.g., long-term acute-care hospital: 99221-99223). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1C. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 3, 2010.
- Highmark Medicare Services Provider Bulletins: Hospital Discharge Day Management Codes 99238 and 99239. Highmark Medicare Services Web site. Available at: www.highmarkmedicareservices.com/bulletins/partb/news02212008a.html. Accessed March 4, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.1A. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.3B. Centers for Medicare & Medicaid Services Web site, Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2E. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1d. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Reporting inpatient hospital evaluation and management (E/M) services that could be described by current procedural terminology (CPT) consultation codes. Cigna Government Services Web site. Available at: www.cignagovernmentservices.com/partb/pubs/news/2010/0210/cope11694.html. Accessed March 5, 2010.
The Humble Approach
Bijo Chacko, MD, FHM, says the varied resources available in the multispecialty medical group in which he practices help to ensure patients receive the best possible care. The structure at Preferred Health Partners in Brooklyn, N.Y., which offers primary and specialty medical services under one roof, requires hospitalists to collaborate frequently with primary-care physicians (PCPs).
That interaction breaks down barriers, fosters communication, promotes the exchange of ideas, and ultimately improves the transition of care from outpatient to inpatient and vice versa, Dr. Chacko says.
His affinity for that environment might explain his passion for the work done by SHM’s Young Physician Task Force, and why “resources” is the word he repeats most often when describing the value of the group’s efforts. Just as experienced hospitalists can learn by interacting with PCPs and other specialists, those who are new to HM can benefit from those who have established themselves in the profession and cleared the hurdles physicians encounter early in a career, he says.
“The advantage of youth is the inherent energy that comes with it,” says Dr. Chacko, hospitalist program medical director with Preferred Health Partners, medical director of the hospitalist program at Good Samaritan Hospital in Suffern, N.Y., and a member of Team Hospitalist. “You really need that energy in your daily work routine, especially early in a career. The disadvantage is, depending on your training, you may not have the experience or been exposed to resources required to take on some of the challenges you’ll face. Hence, expanding the number of resources available to early-career hospitalists—and encouraging them to utilize what is available to them—becomes pivotal.”
Question: Two years after residency, you made the transition to hospitalist program medical director. What advice would you give to an aspiring HM leader?
Answer: Coming out of medical school or residency, you’re not provided all the tools you need to be a successful leader. Some people may achieve those skills during their training or in their first job. But going through some of the unique courses provided by SHM, such as the Leadership Academy, has been invaluable. The information, as well as the connections you make with others throughout the country, really prepares you for a leadership role and some of the challenges you may not have been taught to face in medical school.
Q: What are some of the challenges you aren’t necessarily taught how to handle?
A: Leadership roles take on a complexity of their own. You’re dealing with communications issues; you’re dealing with conflict resolution. Those are unique areas that have to be approached delicately. And one of the fundamental aspects of being a good leader is to define a shared organizational vision and set of shared values for your group that should be supported and promoted.
Q: Can you describe the vision and values you set for your group?
A: Our vision is to be the hospitalist program of choice for patients and physicians in the region. But the key aspect is, we want to provide high-quality patient care with a touch of humility. A physician who demonstrates his or her empathetic side goes a long way in what we do. Research has shown hospitalists provide efficient care—outcomes on cost savings are good. But the other issue is the patient experience, and that’s where the humility factor comes into play.
Q: How do you teach the physicians in your group to be more humble?
A: One thing we emphasize with the team is to imagine themselves or a family member in the patient’s shoes when they are communicating with them. This hits home the importance of bedside manners, and it has to be revisited at times.
Q: Any other techniques?
A: Positive feedback always translates well. We use examples from patients who say they generally had a great experience. In many cases, it amounts to a patient saying, “The doctor was able to explain things to me in a simpler language than anyone has been able to do before, or even attempted to do.” That positive reinforcement resonates well with the doctors. We also share patient scenarios where there were opportunities for improvement.
Q: Considering the demands of your leadership roles at Preferred Health Partners and Good Samaritan Hospital, why is it still a priority for you to provide inpatient clinical care?
A: The old adage is, if you don’t use it, you lose it. Because clinical care is so broad and diverse, and because it is changing so rapidly, it behooves one to stay abreast of it. Also, when you are leading members of a group, I think it’s important to walk in the trenches with them.
Q: You joined SHM’s Young Physician Task Force and served as chairman for two years. What prompted you to participate?
A: When I joined, I had already begun my leadership role as medical director and I was an early-career hospitalist, so I felt it made sense for my professional growth. I wanted an opportunity to collaborate with leading young hospitalists in the country and help shape some of the programs the (group) was working on.
Q: What issues has the group addressed?
A: Initially, the task force was focused on getting information out to early-career hospitalists and providing resources they could utilize. It redefined its section of the SHM website (www.hospitalmedicine .org/youngphysician), which now serves as a portal with information about everything from careers in hospital medicine to how to approach residency. It also introduced the Resident’s Corner (a quarterly column in The Hospitalist, see p. 25), which caters to residents and helps them make a smooth transition to a possible career in hospital medicine. The group has developed programs for early-career hospitalists at the annual SHM meetings.
Q: What major issues are on the agenda now?
A: The group is working on developing a mentorship program for early-career hospitalists, which would be a really valuable resource. The group also is working on projects to reach medical students and residents. The goal is to get them more engaged, and help them realize the diversity and rewards that accompany a career in hospital medicine.
Q: What do you see as the benefit of the mentor program?
A: The beauty of hospital medicine is there is a lot of diversity. If you have an interest in academia, quality initiatives, or research, that’s available. If you have a leadership interest, that can definitely be attained. …
But when you have someone who has had some experience in hospital medicine and can share that experience, and you can get their insights and hear about the challenges they faced and how they faced them, it can make the transition much easier. This will provide young hospitalists with pearls of wisdom and information they may not have been able to access elsewhere.
Q: So it comes back to the idea that there’s still a lot to learn, even after medical school and residency.
A: That’s exactly right. The scope of questions that can be posed or issues that can be addressed is infinite. Beyond that, someone who has already walked that pathway can help establish the fact that hospital medicine should be looked upon as a career with many opportunities, as opposed to a transition point to an alternative career. TH
Mark Leiser is a freelance writer in New Jersey.
Bijo Chacko, MD, FHM, says the varied resources available in the multispecialty medical group in which he practices help to ensure patients receive the best possible care. The structure at Preferred Health Partners in Brooklyn, N.Y., which offers primary and specialty medical services under one roof, requires hospitalists to collaborate frequently with primary-care physicians (PCPs).
That interaction breaks down barriers, fosters communication, promotes the exchange of ideas, and ultimately improves the transition of care from outpatient to inpatient and vice versa, Dr. Chacko says.
His affinity for that environment might explain his passion for the work done by SHM’s Young Physician Task Force, and why “resources” is the word he repeats most often when describing the value of the group’s efforts. Just as experienced hospitalists can learn by interacting with PCPs and other specialists, those who are new to HM can benefit from those who have established themselves in the profession and cleared the hurdles physicians encounter early in a career, he says.
“The advantage of youth is the inherent energy that comes with it,” says Dr. Chacko, hospitalist program medical director with Preferred Health Partners, medical director of the hospitalist program at Good Samaritan Hospital in Suffern, N.Y., and a member of Team Hospitalist. “You really need that energy in your daily work routine, especially early in a career. The disadvantage is, depending on your training, you may not have the experience or been exposed to resources required to take on some of the challenges you’ll face. Hence, expanding the number of resources available to early-career hospitalists—and encouraging them to utilize what is available to them—becomes pivotal.”
Question: Two years after residency, you made the transition to hospitalist program medical director. What advice would you give to an aspiring HM leader?
Answer: Coming out of medical school or residency, you’re not provided all the tools you need to be a successful leader. Some people may achieve those skills during their training or in their first job. But going through some of the unique courses provided by SHM, such as the Leadership Academy, has been invaluable. The information, as well as the connections you make with others throughout the country, really prepares you for a leadership role and some of the challenges you may not have been taught to face in medical school.
Q: What are some of the challenges you aren’t necessarily taught how to handle?
A: Leadership roles take on a complexity of their own. You’re dealing with communications issues; you’re dealing with conflict resolution. Those are unique areas that have to be approached delicately. And one of the fundamental aspects of being a good leader is to define a shared organizational vision and set of shared values for your group that should be supported and promoted.
Q: Can you describe the vision and values you set for your group?
A: Our vision is to be the hospitalist program of choice for patients and physicians in the region. But the key aspect is, we want to provide high-quality patient care with a touch of humility. A physician who demonstrates his or her empathetic side goes a long way in what we do. Research has shown hospitalists provide efficient care—outcomes on cost savings are good. But the other issue is the patient experience, and that’s where the humility factor comes into play.
Q: How do you teach the physicians in your group to be more humble?
A: One thing we emphasize with the team is to imagine themselves or a family member in the patient’s shoes when they are communicating with them. This hits home the importance of bedside manners, and it has to be revisited at times.
Q: Any other techniques?
A: Positive feedback always translates well. We use examples from patients who say they generally had a great experience. In many cases, it amounts to a patient saying, “The doctor was able to explain things to me in a simpler language than anyone has been able to do before, or even attempted to do.” That positive reinforcement resonates well with the doctors. We also share patient scenarios where there were opportunities for improvement.
Q: Considering the demands of your leadership roles at Preferred Health Partners and Good Samaritan Hospital, why is it still a priority for you to provide inpatient clinical care?
A: The old adage is, if you don’t use it, you lose it. Because clinical care is so broad and diverse, and because it is changing so rapidly, it behooves one to stay abreast of it. Also, when you are leading members of a group, I think it’s important to walk in the trenches with them.
Q: You joined SHM’s Young Physician Task Force and served as chairman for two years. What prompted you to participate?
A: When I joined, I had already begun my leadership role as medical director and I was an early-career hospitalist, so I felt it made sense for my professional growth. I wanted an opportunity to collaborate with leading young hospitalists in the country and help shape some of the programs the (group) was working on.
Q: What issues has the group addressed?
A: Initially, the task force was focused on getting information out to early-career hospitalists and providing resources they could utilize. It redefined its section of the SHM website (www.hospitalmedicine .org/youngphysician), which now serves as a portal with information about everything from careers in hospital medicine to how to approach residency. It also introduced the Resident’s Corner (a quarterly column in The Hospitalist, see p. 25), which caters to residents and helps them make a smooth transition to a possible career in hospital medicine. The group has developed programs for early-career hospitalists at the annual SHM meetings.
Q: What major issues are on the agenda now?
A: The group is working on developing a mentorship program for early-career hospitalists, which would be a really valuable resource. The group also is working on projects to reach medical students and residents. The goal is to get them more engaged, and help them realize the diversity and rewards that accompany a career in hospital medicine.
Q: What do you see as the benefit of the mentor program?
A: The beauty of hospital medicine is there is a lot of diversity. If you have an interest in academia, quality initiatives, or research, that’s available. If you have a leadership interest, that can definitely be attained. …
But when you have someone who has had some experience in hospital medicine and can share that experience, and you can get their insights and hear about the challenges they faced and how they faced them, it can make the transition much easier. This will provide young hospitalists with pearls of wisdom and information they may not have been able to access elsewhere.
Q: So it comes back to the idea that there’s still a lot to learn, even after medical school and residency.
A: That’s exactly right. The scope of questions that can be posed or issues that can be addressed is infinite. Beyond that, someone who has already walked that pathway can help establish the fact that hospital medicine should be looked upon as a career with many opportunities, as opposed to a transition point to an alternative career. TH
Mark Leiser is a freelance writer in New Jersey.
Bijo Chacko, MD, FHM, says the varied resources available in the multispecialty medical group in which he practices help to ensure patients receive the best possible care. The structure at Preferred Health Partners in Brooklyn, N.Y., which offers primary and specialty medical services under one roof, requires hospitalists to collaborate frequently with primary-care physicians (PCPs).
That interaction breaks down barriers, fosters communication, promotes the exchange of ideas, and ultimately improves the transition of care from outpatient to inpatient and vice versa, Dr. Chacko says.
His affinity for that environment might explain his passion for the work done by SHM’s Young Physician Task Force, and why “resources” is the word he repeats most often when describing the value of the group’s efforts. Just as experienced hospitalists can learn by interacting with PCPs and other specialists, those who are new to HM can benefit from those who have established themselves in the profession and cleared the hurdles physicians encounter early in a career, he says.
“The advantage of youth is the inherent energy that comes with it,” says Dr. Chacko, hospitalist program medical director with Preferred Health Partners, medical director of the hospitalist program at Good Samaritan Hospital in Suffern, N.Y., and a member of Team Hospitalist. “You really need that energy in your daily work routine, especially early in a career. The disadvantage is, depending on your training, you may not have the experience or been exposed to resources required to take on some of the challenges you’ll face. Hence, expanding the number of resources available to early-career hospitalists—and encouraging them to utilize what is available to them—becomes pivotal.”
Question: Two years after residency, you made the transition to hospitalist program medical director. What advice would you give to an aspiring HM leader?
Answer: Coming out of medical school or residency, you’re not provided all the tools you need to be a successful leader. Some people may achieve those skills during their training or in their first job. But going through some of the unique courses provided by SHM, such as the Leadership Academy, has been invaluable. The information, as well as the connections you make with others throughout the country, really prepares you for a leadership role and some of the challenges you may not have been taught to face in medical school.
Q: What are some of the challenges you aren’t necessarily taught how to handle?
A: Leadership roles take on a complexity of their own. You’re dealing with communications issues; you’re dealing with conflict resolution. Those are unique areas that have to be approached delicately. And one of the fundamental aspects of being a good leader is to define a shared organizational vision and set of shared values for your group that should be supported and promoted.
Q: Can you describe the vision and values you set for your group?
A: Our vision is to be the hospitalist program of choice for patients and physicians in the region. But the key aspect is, we want to provide high-quality patient care with a touch of humility. A physician who demonstrates his or her empathetic side goes a long way in what we do. Research has shown hospitalists provide efficient care—outcomes on cost savings are good. But the other issue is the patient experience, and that’s where the humility factor comes into play.
Q: How do you teach the physicians in your group to be more humble?
A: One thing we emphasize with the team is to imagine themselves or a family member in the patient’s shoes when they are communicating with them. This hits home the importance of bedside manners, and it has to be revisited at times.
Q: Any other techniques?
A: Positive feedback always translates well. We use examples from patients who say they generally had a great experience. In many cases, it amounts to a patient saying, “The doctor was able to explain things to me in a simpler language than anyone has been able to do before, or even attempted to do.” That positive reinforcement resonates well with the doctors. We also share patient scenarios where there were opportunities for improvement.
Q: Considering the demands of your leadership roles at Preferred Health Partners and Good Samaritan Hospital, why is it still a priority for you to provide inpatient clinical care?
A: The old adage is, if you don’t use it, you lose it. Because clinical care is so broad and diverse, and because it is changing so rapidly, it behooves one to stay abreast of it. Also, when you are leading members of a group, I think it’s important to walk in the trenches with them.
Q: You joined SHM’s Young Physician Task Force and served as chairman for two years. What prompted you to participate?
A: When I joined, I had already begun my leadership role as medical director and I was an early-career hospitalist, so I felt it made sense for my professional growth. I wanted an opportunity to collaborate with leading young hospitalists in the country and help shape some of the programs the (group) was working on.
Q: What issues has the group addressed?
A: Initially, the task force was focused on getting information out to early-career hospitalists and providing resources they could utilize. It redefined its section of the SHM website (www.hospitalmedicine .org/youngphysician), which now serves as a portal with information about everything from careers in hospital medicine to how to approach residency. It also introduced the Resident’s Corner (a quarterly column in The Hospitalist, see p. 25), which caters to residents and helps them make a smooth transition to a possible career in hospital medicine. The group has developed programs for early-career hospitalists at the annual SHM meetings.
Q: What major issues are on the agenda now?
A: The group is working on developing a mentorship program for early-career hospitalists, which would be a really valuable resource. The group also is working on projects to reach medical students and residents. The goal is to get them more engaged, and help them realize the diversity and rewards that accompany a career in hospital medicine.
Q: What do you see as the benefit of the mentor program?
A: The beauty of hospital medicine is there is a lot of diversity. If you have an interest in academia, quality initiatives, or research, that’s available. If you have a leadership interest, that can definitely be attained. …
But when you have someone who has had some experience in hospital medicine and can share that experience, and you can get their insights and hear about the challenges they faced and how they faced them, it can make the transition much easier. This will provide young hospitalists with pearls of wisdom and information they may not have been able to access elsewhere.
Q: So it comes back to the idea that there’s still a lot to learn, even after medical school and residency.
A: That’s exactly right. The scope of questions that can be posed or issues that can be addressed is infinite. Beyond that, someone who has already walked that pathway can help establish the fact that hospital medicine should be looked upon as a career with many opportunities, as opposed to a transition point to an alternative career. TH
Mark Leiser is a freelance writer in New Jersey.
Clinical Session: “The New C. Diff”
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10