User login
Health Care Integration: Part 2
[for Part 1, click here.]
The waves of changes in health care have been flowing (crashing?) over us for the past couple years. One can barely get dry before the next one comes on. In psychiatry, we have several big waves hitting us now. Adoption of electronic health records. DSM-5. Integration of mental health, addiction, and somatic health care.
Integration of health care, to me, seems like the most challenging one. It involves changing many of our beliefs and practices about how behavioral health (I am using this BH term to encompass both mental health and addiction treatment) care is provided. Much of this new direction has been driven by a series of factors, including the Mental Health Parity Act of 1996, the New Freedom Commission report in 2002, and the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008.
A good resource for the MHPAEA is parityispersonal.org. The ultimate realization of parity, and of the end of the stigma so long attached to behavioral health, is the full integration of BH into the rest of health care, in the same way that cardiology and neurology are both integrated into health care. There is not a separate health insurance company to manage cardiology services. Neurology patients do not have to pay a higher co-pay for neurology services than they do for other specialty care services. And when you need to find a cardiologist in your insurance company’s provider directory, they are listed there with the other specialties, not in some other directory on some other website.
In my July 2012 column, entitled Health Care Integration, I discussed the process of integration in Maryland Medicaid and promised an update. Every state is addressing this to varying degrees and at different paces. Maryland’s efforts are led by Health Secretary Joshua Sharfstein, a pediatrician and public health expert who clearly gets the value of integration, and Chuck Milligan, the deputy secretary overseeing the entire project. A long process of stakeholder meetings culminated on Oct. 1 in a final recommendation report that can be found at http://dhmh.maryland.gov/bhd/SitePages/integrationefforts.aspx.
The report concludes: “While noting the strengths in the current system, including generally good access in each service domain (mental health, substance use treatment, and somatic care), the resulting report reached five conclusions: (1) benefit design and management across the domains are poorly aligned; (2) purchasing and financing are fragmented; (3) care management is not coordinated; (4) performance and risk are lacking; and (5) care integration needs improvement.”
The current system includes several managed care organizations (MCOs) that provide somatic and addiction care services, and a single administrative services organization (ASO) – Value Options – that is responsible for mental health services. The final recommendation to Secretary Sharfstein is “that Maryland pursue a transformative behavioral health carve-out that combines treatment for specialty mental illness and substance use disorders under the management of a single administrative services organization (ASO).” The transformation part refers to the development of a “performance-based ASO,” whose features include the following:
- Financial performance risk (likely including shared savings) at the ASO level;
- Financial performance risk (which could include shared savings) at the behavioral health provider level;
- Incorporation of behavioral health financial incentives at the primary care and MCO level; and
- Incorporation of non-financial tools that distinguish providers who achieve positive outcomes from providers who achieve average or poor outcomes, including tools such as differential rules for prior authorization, utilization review, and consumer self-referral.
Other changes might include greater integration between the ASO and the MCOs:
- Requiring an MCO to assign a care coordinator when one of its members receives services in the specialty behavioral health system;
- Developing policies and approaches to coordinate (or integrate) primary care with the specialty behavioral health services provided through the new behavioral Health Home;
- Increasing bi-directional data sharing between the MCOs and the ASO to improve beneficiary care, which could include an approach that aligns electronic health records; and
- Shared savings models across somatic and behavioral health.
I think we are moving in the right direction, despite some criticism in the path to get there. We are making less of an issue now about what model to choose (Model 2 has been chosen, the ASO model), and beginning to focus more on the details. Based on the Principles of Integration from the Maryland Psychiatric Association (enumerated in Part 1 of this series), the last four points, such as care coordination, bi-directional data-sharing, shared savings and risk, and stakeholder oversight and data transparency, are all elements that MUST (not “may”) be included.
One interesting development is that the addiction community is largely refuting previous attributions that the integration of addictions with primary care was a disaster, and is now clarifying that – while there were early challenges – things are just fine now, thank you very much. So they are quite concerned about losing their advances when addictions get carved back out of somatic care and included in mental health.
The primary care community, led by MedChi, the state medical society, is also backing the integration principles that the MPS has championed. And we are now hearing from some MCOs and hospitals that a fully integrated approach, all rolled into one or several MCOs, is preferred. A hearing before the legislature was to occur last week, but Hurricane Sandy interfered. Public comments are being collected until Nov. 9, and the rescheduled hearing is set for Dec. 18.
I’ll be back before Christmas with Part 3. I am certain that there are at least a couple states going through the same discussions that we are going through. Log in to CLINICAL PSYCHIATRY NEWS and post your comments so we can all learn from one anothers’ experiences.
—Steven Roy Davis, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog and drdavissATgmailDOTcom.
[for Part 1, click here.]
The waves of changes in health care have been flowing (crashing?) over us for the past couple years. One can barely get dry before the next one comes on. In psychiatry, we have several big waves hitting us now. Adoption of electronic health records. DSM-5. Integration of mental health, addiction, and somatic health care.
Integration of health care, to me, seems like the most challenging one. It involves changing many of our beliefs and practices about how behavioral health (I am using this BH term to encompass both mental health and addiction treatment) care is provided. Much of this new direction has been driven by a series of factors, including the Mental Health Parity Act of 1996, the New Freedom Commission report in 2002, and the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008.
A good resource for the MHPAEA is parityispersonal.org. The ultimate realization of parity, and of the end of the stigma so long attached to behavioral health, is the full integration of BH into the rest of health care, in the same way that cardiology and neurology are both integrated into health care. There is not a separate health insurance company to manage cardiology services. Neurology patients do not have to pay a higher co-pay for neurology services than they do for other specialty care services. And when you need to find a cardiologist in your insurance company’s provider directory, they are listed there with the other specialties, not in some other directory on some other website.
In my July 2012 column, entitled Health Care Integration, I discussed the process of integration in Maryland Medicaid and promised an update. Every state is addressing this to varying degrees and at different paces. Maryland’s efforts are led by Health Secretary Joshua Sharfstein, a pediatrician and public health expert who clearly gets the value of integration, and Chuck Milligan, the deputy secretary overseeing the entire project. A long process of stakeholder meetings culminated on Oct. 1 in a final recommendation report that can be found at http://dhmh.maryland.gov/bhd/SitePages/integrationefforts.aspx.
The report concludes: “While noting the strengths in the current system, including generally good access in each service domain (mental health, substance use treatment, and somatic care), the resulting report reached five conclusions: (1) benefit design and management across the domains are poorly aligned; (2) purchasing and financing are fragmented; (3) care management is not coordinated; (4) performance and risk are lacking; and (5) care integration needs improvement.”
The current system includes several managed care organizations (MCOs) that provide somatic and addiction care services, and a single administrative services organization (ASO) – Value Options – that is responsible for mental health services. The final recommendation to Secretary Sharfstein is “that Maryland pursue a transformative behavioral health carve-out that combines treatment for specialty mental illness and substance use disorders under the management of a single administrative services organization (ASO).” The transformation part refers to the development of a “performance-based ASO,” whose features include the following:
- Financial performance risk (likely including shared savings) at the ASO level;
- Financial performance risk (which could include shared savings) at the behavioral health provider level;
- Incorporation of behavioral health financial incentives at the primary care and MCO level; and
- Incorporation of non-financial tools that distinguish providers who achieve positive outcomes from providers who achieve average or poor outcomes, including tools such as differential rules for prior authorization, utilization review, and consumer self-referral.
Other changes might include greater integration between the ASO and the MCOs:
- Requiring an MCO to assign a care coordinator when one of its members receives services in the specialty behavioral health system;
- Developing policies and approaches to coordinate (or integrate) primary care with the specialty behavioral health services provided through the new behavioral Health Home;
- Increasing bi-directional data sharing between the MCOs and the ASO to improve beneficiary care, which could include an approach that aligns electronic health records; and
- Shared savings models across somatic and behavioral health.
I think we are moving in the right direction, despite some criticism in the path to get there. We are making less of an issue now about what model to choose (Model 2 has been chosen, the ASO model), and beginning to focus more on the details. Based on the Principles of Integration from the Maryland Psychiatric Association (enumerated in Part 1 of this series), the last four points, such as care coordination, bi-directional data-sharing, shared savings and risk, and stakeholder oversight and data transparency, are all elements that MUST (not “may”) be included.
One interesting development is that the addiction community is largely refuting previous attributions that the integration of addictions with primary care was a disaster, and is now clarifying that – while there were early challenges – things are just fine now, thank you very much. So they are quite concerned about losing their advances when addictions get carved back out of somatic care and included in mental health.
The primary care community, led by MedChi, the state medical society, is also backing the integration principles that the MPS has championed. And we are now hearing from some MCOs and hospitals that a fully integrated approach, all rolled into one or several MCOs, is preferred. A hearing before the legislature was to occur last week, but Hurricane Sandy interfered. Public comments are being collected until Nov. 9, and the rescheduled hearing is set for Dec. 18.
I’ll be back before Christmas with Part 3. I am certain that there are at least a couple states going through the same discussions that we are going through. Log in to CLINICAL PSYCHIATRY NEWS and post your comments so we can all learn from one anothers’ experiences.
—Steven Roy Davis, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog and drdavissATgmailDOTcom.
[for Part 1, click here.]
The waves of changes in health care have been flowing (crashing?) over us for the past couple years. One can barely get dry before the next one comes on. In psychiatry, we have several big waves hitting us now. Adoption of electronic health records. DSM-5. Integration of mental health, addiction, and somatic health care.
Integration of health care, to me, seems like the most challenging one. It involves changing many of our beliefs and practices about how behavioral health (I am using this BH term to encompass both mental health and addiction treatment) care is provided. Much of this new direction has been driven by a series of factors, including the Mental Health Parity Act of 1996, the New Freedom Commission report in 2002, and the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008.
A good resource for the MHPAEA is parityispersonal.org. The ultimate realization of parity, and of the end of the stigma so long attached to behavioral health, is the full integration of BH into the rest of health care, in the same way that cardiology and neurology are both integrated into health care. There is not a separate health insurance company to manage cardiology services. Neurology patients do not have to pay a higher co-pay for neurology services than they do for other specialty care services. And when you need to find a cardiologist in your insurance company’s provider directory, they are listed there with the other specialties, not in some other directory on some other website.
In my July 2012 column, entitled Health Care Integration, I discussed the process of integration in Maryland Medicaid and promised an update. Every state is addressing this to varying degrees and at different paces. Maryland’s efforts are led by Health Secretary Joshua Sharfstein, a pediatrician and public health expert who clearly gets the value of integration, and Chuck Milligan, the deputy secretary overseeing the entire project. A long process of stakeholder meetings culminated on Oct. 1 in a final recommendation report that can be found at http://dhmh.maryland.gov/bhd/SitePages/integrationefforts.aspx.
The report concludes: “While noting the strengths in the current system, including generally good access in each service domain (mental health, substance use treatment, and somatic care), the resulting report reached five conclusions: (1) benefit design and management across the domains are poorly aligned; (2) purchasing and financing are fragmented; (3) care management is not coordinated; (4) performance and risk are lacking; and (5) care integration needs improvement.”
The current system includes several managed care organizations (MCOs) that provide somatic and addiction care services, and a single administrative services organization (ASO) – Value Options – that is responsible for mental health services. The final recommendation to Secretary Sharfstein is “that Maryland pursue a transformative behavioral health carve-out that combines treatment for specialty mental illness and substance use disorders under the management of a single administrative services organization (ASO).” The transformation part refers to the development of a “performance-based ASO,” whose features include the following:
- Financial performance risk (likely including shared savings) at the ASO level;
- Financial performance risk (which could include shared savings) at the behavioral health provider level;
- Incorporation of behavioral health financial incentives at the primary care and MCO level; and
- Incorporation of non-financial tools that distinguish providers who achieve positive outcomes from providers who achieve average or poor outcomes, including tools such as differential rules for prior authorization, utilization review, and consumer self-referral.
Other changes might include greater integration between the ASO and the MCOs:
- Requiring an MCO to assign a care coordinator when one of its members receives services in the specialty behavioral health system;
- Developing policies and approaches to coordinate (or integrate) primary care with the specialty behavioral health services provided through the new behavioral Health Home;
- Increasing bi-directional data sharing between the MCOs and the ASO to improve beneficiary care, which could include an approach that aligns electronic health records; and
- Shared savings models across somatic and behavioral health.
I think we are moving in the right direction, despite some criticism in the path to get there. We are making less of an issue now about what model to choose (Model 2 has been chosen, the ASO model), and beginning to focus more on the details. Based on the Principles of Integration from the Maryland Psychiatric Association (enumerated in Part 1 of this series), the last four points, such as care coordination, bi-directional data-sharing, shared savings and risk, and stakeholder oversight and data transparency, are all elements that MUST (not “may”) be included.
One interesting development is that the addiction community is largely refuting previous attributions that the integration of addictions with primary care was a disaster, and is now clarifying that – while there were early challenges – things are just fine now, thank you very much. So they are quite concerned about losing their advances when addictions get carved back out of somatic care and included in mental health.
The primary care community, led by MedChi, the state medical society, is also backing the integration principles that the MPS has championed. And we are now hearing from some MCOs and hospitals that a fully integrated approach, all rolled into one or several MCOs, is preferred. A hearing before the legislature was to occur last week, but Hurricane Sandy interfered. Public comments are being collected until Nov. 9, and the rescheduled hearing is set for Dec. 18.
I’ll be back before Christmas with Part 3. I am certain that there are at least a couple states going through the same discussions that we are going through. Log in to CLINICAL PSYCHIATRY NEWS and post your comments so we can all learn from one anothers’ experiences.
—Steven Roy Davis, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog and drdavissATgmailDOTcom.
'Systematic Psychiatric Evaluation': A Review
I was a medical student in Manhattan in the late 1980s. From the beginning, I knew I wanted to go into psychiatry, and I watched the psychoanalysts and psychopharmacologists chase each other back and forth across town from institution to institution, debating questions of nature vs. nurture for the both the cause and cure of mental disorders.
When I moved to Baltimore to begin my psychiatry residency at Johns Hopkins Hospital, I was introduced to a way of thinking about human behavior and emotions that involved considering the individual from four different perspectives as described by our chairman, Dr. Paul McHugh, and our residency director, Dr. Phillip Slavney, in their book, The Perspectives of Psychiatry. At the time, this approach seemed almost obvious to me; of course the causes of psychopathology were multifactorial; how could they not be?
Fast-forward two decades and what seemed obvious to a newly minted psychiatry resident no longer feels quiet so evident. We’ve become a field of diagnosis by checklist and rapid-fire appointments to ask about symptoms and side effects. In fact, most psychiatric care is rendered by primary care physicians with little formal training in psychiatric diagnosis. Twenty years later, and it seems we’ve lost our curiosity (“no time”) and with that, the inclination to learn about a patient’s difficulties in the context of not only a disease, but also by giving consideration to their motivated behaviors, their individual temperaments, and their complete life stories.
So on our current landscape of checklist diagnosis and the full-court press by insurers to reimburse psychiatrists best for brief visits, it is refreshing to read Systematic Psychiatric Evaluation, A Step-by-Step Guide to Applying The Perspectives of Psychiatry, by two of my residency classmates, Dr. Margaret S. Chisolm and Dr. Constantine G. Lyketsos, M.H.S. Nothing about this book is about learning to diagnose in Chinese menu format, or about rushed appointments with patients; instead it is about how to do thoughtful and caring evaluations (including, but not limited to, diagnoses) of patients with emotional and/or behavioral turmoil.
The authors begin with a hint of humor – probably best understood by those of us who live in Charm City – by presenting the historical case history of Baltimore poet Edgar Allen Poe, done first as a typical psychiatric presentation, and then as a full case study per the four perspectives. They go on to present a series of patient case histories, beginning with reconstructed interviews, an analysis that integrates a multifactorial approach to understanding the problems, a conclusion, and summary points.
One of the treasures of this book is that the back-and-forth dialogue of the interviews is included, illustrating to students exactly which words an experienced clinician might use to elicit specific material, and giving the reader the sense of being in the room during the interview. The wording is designed to convey empathy, warmth, and to put the patient at ease. And while the case studies are comprehensive, the book is done as an engaging, concise, and quick read.
Whether or not psychiatrists choose to practice in time-pressured environments, teaching institutions need to remain a place where our students learn to evaluate patients in a systematic and comprehensive manner and, in psychiatry, this is not a quick process and it does not involve cutting corners or boiling the complex work of psychiatric evaluations down to checklists.
Systematic Psychiatric Evaluation is the best go-to book I have seen for teaching thoughtful evaluation.
Please also see Dr. Chisolm’s guest post about her book on the main Shrink Rap blog here.
—Dinah Miller, M.D.
Dr. Miller’s books and novels are listed here.
I was a medical student in Manhattan in the late 1980s. From the beginning, I knew I wanted to go into psychiatry, and I watched the psychoanalysts and psychopharmacologists chase each other back and forth across town from institution to institution, debating questions of nature vs. nurture for the both the cause and cure of mental disorders.
When I moved to Baltimore to begin my psychiatry residency at Johns Hopkins Hospital, I was introduced to a way of thinking about human behavior and emotions that involved considering the individual from four different perspectives as described by our chairman, Dr. Paul McHugh, and our residency director, Dr. Phillip Slavney, in their book, The Perspectives of Psychiatry. At the time, this approach seemed almost obvious to me; of course the causes of psychopathology were multifactorial; how could they not be?
Fast-forward two decades and what seemed obvious to a newly minted psychiatry resident no longer feels quiet so evident. We’ve become a field of diagnosis by checklist and rapid-fire appointments to ask about symptoms and side effects. In fact, most psychiatric care is rendered by primary care physicians with little formal training in psychiatric diagnosis. Twenty years later, and it seems we’ve lost our curiosity (“no time”) and with that, the inclination to learn about a patient’s difficulties in the context of not only a disease, but also by giving consideration to their motivated behaviors, their individual temperaments, and their complete life stories.
So on our current landscape of checklist diagnosis and the full-court press by insurers to reimburse psychiatrists best for brief visits, it is refreshing to read Systematic Psychiatric Evaluation, A Step-by-Step Guide to Applying The Perspectives of Psychiatry, by two of my residency classmates, Dr. Margaret S. Chisolm and Dr. Constantine G. Lyketsos, M.H.S. Nothing about this book is about learning to diagnose in Chinese menu format, or about rushed appointments with patients; instead it is about how to do thoughtful and caring evaluations (including, but not limited to, diagnoses) of patients with emotional and/or behavioral turmoil.
The authors begin with a hint of humor – probably best understood by those of us who live in Charm City – by presenting the historical case history of Baltimore poet Edgar Allen Poe, done first as a typical psychiatric presentation, and then as a full case study per the four perspectives. They go on to present a series of patient case histories, beginning with reconstructed interviews, an analysis that integrates a multifactorial approach to understanding the problems, a conclusion, and summary points.
One of the treasures of this book is that the back-and-forth dialogue of the interviews is included, illustrating to students exactly which words an experienced clinician might use to elicit specific material, and giving the reader the sense of being in the room during the interview. The wording is designed to convey empathy, warmth, and to put the patient at ease. And while the case studies are comprehensive, the book is done as an engaging, concise, and quick read.
Whether or not psychiatrists choose to practice in time-pressured environments, teaching institutions need to remain a place where our students learn to evaluate patients in a systematic and comprehensive manner and, in psychiatry, this is not a quick process and it does not involve cutting corners or boiling the complex work of psychiatric evaluations down to checklists.
Systematic Psychiatric Evaluation is the best go-to book I have seen for teaching thoughtful evaluation.
Please also see Dr. Chisolm’s guest post about her book on the main Shrink Rap blog here.
—Dinah Miller, M.D.
Dr. Miller’s books and novels are listed here.
I was a medical student in Manhattan in the late 1980s. From the beginning, I knew I wanted to go into psychiatry, and I watched the psychoanalysts and psychopharmacologists chase each other back and forth across town from institution to institution, debating questions of nature vs. nurture for the both the cause and cure of mental disorders.
When I moved to Baltimore to begin my psychiatry residency at Johns Hopkins Hospital, I was introduced to a way of thinking about human behavior and emotions that involved considering the individual from four different perspectives as described by our chairman, Dr. Paul McHugh, and our residency director, Dr. Phillip Slavney, in their book, The Perspectives of Psychiatry. At the time, this approach seemed almost obvious to me; of course the causes of psychopathology were multifactorial; how could they not be?
Fast-forward two decades and what seemed obvious to a newly minted psychiatry resident no longer feels quiet so evident. We’ve become a field of diagnosis by checklist and rapid-fire appointments to ask about symptoms and side effects. In fact, most psychiatric care is rendered by primary care physicians with little formal training in psychiatric diagnosis. Twenty years later, and it seems we’ve lost our curiosity (“no time”) and with that, the inclination to learn about a patient’s difficulties in the context of not only a disease, but also by giving consideration to their motivated behaviors, their individual temperaments, and their complete life stories.
So on our current landscape of checklist diagnosis and the full-court press by insurers to reimburse psychiatrists best for brief visits, it is refreshing to read Systematic Psychiatric Evaluation, A Step-by-Step Guide to Applying The Perspectives of Psychiatry, by two of my residency classmates, Dr. Margaret S. Chisolm and Dr. Constantine G. Lyketsos, M.H.S. Nothing about this book is about learning to diagnose in Chinese menu format, or about rushed appointments with patients; instead it is about how to do thoughtful and caring evaluations (including, but not limited to, diagnoses) of patients with emotional and/or behavioral turmoil.
The authors begin with a hint of humor – probably best understood by those of us who live in Charm City – by presenting the historical case history of Baltimore poet Edgar Allen Poe, done first as a typical psychiatric presentation, and then as a full case study per the four perspectives. They go on to present a series of patient case histories, beginning with reconstructed interviews, an analysis that integrates a multifactorial approach to understanding the problems, a conclusion, and summary points.
One of the treasures of this book is that the back-and-forth dialogue of the interviews is included, illustrating to students exactly which words an experienced clinician might use to elicit specific material, and giving the reader the sense of being in the room during the interview. The wording is designed to convey empathy, warmth, and to put the patient at ease. And while the case studies are comprehensive, the book is done as an engaging, concise, and quick read.
Whether or not psychiatrists choose to practice in time-pressured environments, teaching institutions need to remain a place where our students learn to evaluate patients in a systematic and comprehensive manner and, in psychiatry, this is not a quick process and it does not involve cutting corners or boiling the complex work of psychiatric evaluations down to checklists.
Systematic Psychiatric Evaluation is the best go-to book I have seen for teaching thoughtful evaluation.
Please also see Dr. Chisolm’s guest post about her book on the main Shrink Rap blog here.
—Dinah Miller, M.D.
Dr. Miller’s books and novels are listed here.
New Study Debunks the 'Mad Artistic Genius' Myth
In the October issue of the Journal of Psychiatric Research, Dr. Simon Kyaga and his colleagues examined the relationship between various psychiatric disorders and the creative occupations. They used Swedish census data as well as the medical and mortality registry information of more than 1.1 million subjects involved in either scientific or traditional creative professions. A scientific occupation was considered creative if it involved academic research and teaching at a university level. The traditional creative professions were defined as visual or non-visual artists, with particular attention paid to writers.
An additional control group was added for comparison to a “lesser creative” occupation, specifically accountants and auditors. First degree relatives of each subject were also included. The authors considered a wide variety of disorders, including schizophrenia, bipolar disorder, depression, anxiety, autism, anorexia nervosa, ADHD, and substance use disorders.
The study showed that there was no overall difference between the creative and lesser creative occupations with regard to any psychiatric disorder other than bipolar disorder, which was more prevalent among scientific creatives.
Participation in a creative occupation appeared to be protective for the development of most disorders, and decreased the likelihood of suicide.
Being in a creative profession was associated with a family history of schizophrenia and bipolar disorder. The authors speculated that creativity and unconventional thinking exist along a spectrum with psychopathology, and that there is an overall evolutionary benefit. Some degree of pathology leads to productivity, while too much is pathological.
Writers were an exception to these findings. Authors were twice as likely as other creative professionals to have schizophrenia and bipolar disorder, and were at increased risk of both depression and substance abuse. Writers, and poets in particular, were at an increased risk of suicide even in the absence of a psychiatric diagnosis.
There were several unique aspects to this study: the extremely large number of subjects, the 40-year follow-up period, and the extensive list of psychiatric disorders that were included. It was also unique because it included “everyday” artists – creative individuals who were not celebrity figures or award-winning authors. Thus, the study may be more reflective of the real-world experience of most visual and verbal artistic professionals.
While I found the research fascinating, it was not designed to answer the question of why creativity may protect against mental illness for most professions or why writers may be particularly vulnerable. Certainly, there are aspects of an artist’s life that would affect emotional functioning: living in a society were artistic accomplishments are less valued or rewarded, being professionally isolated or being involved in an activity that requires a considerable investment of one’s identity or some degree of public personal disclosure. The creative endeavor itself may compensate for all this.
The study also isn’t able to answer the question of how best to care for the mentally ill artist or the role of the creative process in recovery from mental illness. Nevertheless, this paper will hopefully put to rest the myth of the mad but tragic artistic genius. While creativity and madness may make for a compelling narrative, the reality of serious mental illness and suicide is a much uglier picture.
—Annette Hanson, M.D.
DR. HANSON is a forensic psychiatrist and co-author of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
In the October issue of the Journal of Psychiatric Research, Dr. Simon Kyaga and his colleagues examined the relationship between various psychiatric disorders and the creative occupations. They used Swedish census data as well as the medical and mortality registry information of more than 1.1 million subjects involved in either scientific or traditional creative professions. A scientific occupation was considered creative if it involved academic research and teaching at a university level. The traditional creative professions were defined as visual or non-visual artists, with particular attention paid to writers.
An additional control group was added for comparison to a “lesser creative” occupation, specifically accountants and auditors. First degree relatives of each subject were also included. The authors considered a wide variety of disorders, including schizophrenia, bipolar disorder, depression, anxiety, autism, anorexia nervosa, ADHD, and substance use disorders.
The study showed that there was no overall difference between the creative and lesser creative occupations with regard to any psychiatric disorder other than bipolar disorder, which was more prevalent among scientific creatives.
Participation in a creative occupation appeared to be protective for the development of most disorders, and decreased the likelihood of suicide.
Being in a creative profession was associated with a family history of schizophrenia and bipolar disorder. The authors speculated that creativity and unconventional thinking exist along a spectrum with psychopathology, and that there is an overall evolutionary benefit. Some degree of pathology leads to productivity, while too much is pathological.
Writers were an exception to these findings. Authors were twice as likely as other creative professionals to have schizophrenia and bipolar disorder, and were at increased risk of both depression and substance abuse. Writers, and poets in particular, were at an increased risk of suicide even in the absence of a psychiatric diagnosis.
There were several unique aspects to this study: the extremely large number of subjects, the 40-year follow-up period, and the extensive list of psychiatric disorders that were included. It was also unique because it included “everyday” artists – creative individuals who were not celebrity figures or award-winning authors. Thus, the study may be more reflective of the real-world experience of most visual and verbal artistic professionals.
While I found the research fascinating, it was not designed to answer the question of why creativity may protect against mental illness for most professions or why writers may be particularly vulnerable. Certainly, there are aspects of an artist’s life that would affect emotional functioning: living in a society were artistic accomplishments are less valued or rewarded, being professionally isolated or being involved in an activity that requires a considerable investment of one’s identity or some degree of public personal disclosure. The creative endeavor itself may compensate for all this.
The study also isn’t able to answer the question of how best to care for the mentally ill artist or the role of the creative process in recovery from mental illness. Nevertheless, this paper will hopefully put to rest the myth of the mad but tragic artistic genius. While creativity and madness may make for a compelling narrative, the reality of serious mental illness and suicide is a much uglier picture.
—Annette Hanson, M.D.
DR. HANSON is a forensic psychiatrist and co-author of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
In the October issue of the Journal of Psychiatric Research, Dr. Simon Kyaga and his colleagues examined the relationship between various psychiatric disorders and the creative occupations. They used Swedish census data as well as the medical and mortality registry information of more than 1.1 million subjects involved in either scientific or traditional creative professions. A scientific occupation was considered creative if it involved academic research and teaching at a university level. The traditional creative professions were defined as visual or non-visual artists, with particular attention paid to writers.
An additional control group was added for comparison to a “lesser creative” occupation, specifically accountants and auditors. First degree relatives of each subject were also included. The authors considered a wide variety of disorders, including schizophrenia, bipolar disorder, depression, anxiety, autism, anorexia nervosa, ADHD, and substance use disorders.
The study showed that there was no overall difference between the creative and lesser creative occupations with regard to any psychiatric disorder other than bipolar disorder, which was more prevalent among scientific creatives.
Participation in a creative occupation appeared to be protective for the development of most disorders, and decreased the likelihood of suicide.
Being in a creative profession was associated with a family history of schizophrenia and bipolar disorder. The authors speculated that creativity and unconventional thinking exist along a spectrum with psychopathology, and that there is an overall evolutionary benefit. Some degree of pathology leads to productivity, while too much is pathological.
Writers were an exception to these findings. Authors were twice as likely as other creative professionals to have schizophrenia and bipolar disorder, and were at increased risk of both depression and substance abuse. Writers, and poets in particular, were at an increased risk of suicide even in the absence of a psychiatric diagnosis.
There were several unique aspects to this study: the extremely large number of subjects, the 40-year follow-up period, and the extensive list of psychiatric disorders that were included. It was also unique because it included “everyday” artists – creative individuals who were not celebrity figures or award-winning authors. Thus, the study may be more reflective of the real-world experience of most visual and verbal artistic professionals.
While I found the research fascinating, it was not designed to answer the question of why creativity may protect against mental illness for most professions or why writers may be particularly vulnerable. Certainly, there are aspects of an artist’s life that would affect emotional functioning: living in a society were artistic accomplishments are less valued or rewarded, being professionally isolated or being involved in an activity that requires a considerable investment of one’s identity or some degree of public personal disclosure. The creative endeavor itself may compensate for all this.
The study also isn’t able to answer the question of how best to care for the mentally ill artist or the role of the creative process in recovery from mental illness. Nevertheless, this paper will hopefully put to rest the myth of the mad but tragic artistic genius. While creativity and madness may make for a compelling narrative, the reality of serious mental illness and suicide is a much uglier picture.
—Annette Hanson, M.D.
DR. HANSON is a forensic psychiatrist and co-author of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
World Mental Health Day: Oct. 10
Today, Oct. 10, 2012, is the anniversary of World Mental Health Day, started by the World Federation for Mental Health (WFMH) 20 years ago. Many other advocacy organizations and governments have since recognized this day as a mechanism to promote mental health, including National Depression Screening Day in the United States (which is the next day, on Oct. 11).
This year’s theme is Depression: A Global Crisis. Depression has long been a significant problem globally, but has particularly taken hold in recent years, associated with the global economic downturn. Some facts from the WFMH, the World Health Organization (WHO), and the National Institute for Mental Health (NIMH) about depression are rather alarming:
- More than 350 millionMore than 350 million people worldwide have depression
- Unipolar depression was the third-leading cause of global disease burden in 2004
- It is expected to be the #1 leading cause by 2030
- The World Mental Health Survey of people in 17 countries found that 1 in 20 had an episode of depression in the past year
- Depression is the leading cause of disability in terms of work years lost to disease
- 16% of U.S. adults have a history of at least one episode of depression... the average age of onset is 32
- 3,000: number of people lost to suicide ... every day (most have depression)
- 60,000: number of people attempting suicide ... every day
- Every 1% rise in unemployment is associated with a 0.79% rise in suicides in nonelderly adults
- Greece has experienced a 36% increase in suicide attempts since its economic crisis began
- Less than half of people with depression receive any treatment
- Only 20% (in the United States) receive minimally adequate treatment
- At least one-sixth of people with depression actually have bipolar depression
- People with diabetes or heart disease who also have depression do more poorly and have a higher mortality
- People on Medicaid who have a chronic medical condition as well as a mental health diagnosis are hospitalized as much as 2-4 times more often for their medical condition than those who do not have a mental health diagnosis
- If they also have an addiction diagnosis, they are hospitalized 8-15 times more often for their chronic medical condition
Here is a list of resources for more information on depression:
- Take a free screening for depression, bipolar, anxiety, and posttraumatic stress disorders
—Steven R. Daviss, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog.
Today, Oct. 10, 2012, is the anniversary of World Mental Health Day, started by the World Federation for Mental Health (WFMH) 20 years ago. Many other advocacy organizations and governments have since recognized this day as a mechanism to promote mental health, including National Depression Screening Day in the United States (which is the next day, on Oct. 11).
This year’s theme is Depression: A Global Crisis. Depression has long been a significant problem globally, but has particularly taken hold in recent years, associated with the global economic downturn. Some facts from the WFMH, the World Health Organization (WHO), and the National Institute for Mental Health (NIMH) about depression are rather alarming:
- More than 350 millionMore than 350 million people worldwide have depression
- Unipolar depression was the third-leading cause of global disease burden in 2004
- It is expected to be the #1 leading cause by 2030
- The World Mental Health Survey of people in 17 countries found that 1 in 20 had an episode of depression in the past year
- Depression is the leading cause of disability in terms of work years lost to disease
- 16% of U.S. adults have a history of at least one episode of depression... the average age of onset is 32
- 3,000: number of people lost to suicide ... every day (most have depression)
- 60,000: number of people attempting suicide ... every day
- Every 1% rise in unemployment is associated with a 0.79% rise in suicides in nonelderly adults
- Greece has experienced a 36% increase in suicide attempts since its economic crisis began
- Less than half of people with depression receive any treatment
- Only 20% (in the United States) receive minimally adequate treatment
- At least one-sixth of people with depression actually have bipolar depression
- People with diabetes or heart disease who also have depression do more poorly and have a higher mortality
- People on Medicaid who have a chronic medical condition as well as a mental health diagnosis are hospitalized as much as 2-4 times more often for their medical condition than those who do not have a mental health diagnosis
- If they also have an addiction diagnosis, they are hospitalized 8-15 times more often for their chronic medical condition
Here is a list of resources for more information on depression:
- Take a free screening for depression, bipolar, anxiety, and posttraumatic stress disorders
—Steven R. Daviss, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog.
Today, Oct. 10, 2012, is the anniversary of World Mental Health Day, started by the World Federation for Mental Health (WFMH) 20 years ago. Many other advocacy organizations and governments have since recognized this day as a mechanism to promote mental health, including National Depression Screening Day in the United States (which is the next day, on Oct. 11).
This year’s theme is Depression: A Global Crisis. Depression has long been a significant problem globally, but has particularly taken hold in recent years, associated with the global economic downturn. Some facts from the WFMH, the World Health Organization (WHO), and the National Institute for Mental Health (NIMH) about depression are rather alarming:
- More than 350 millionMore than 350 million people worldwide have depression
- Unipolar depression was the third-leading cause of global disease burden in 2004
- It is expected to be the #1 leading cause by 2030
- The World Mental Health Survey of people in 17 countries found that 1 in 20 had an episode of depression in the past year
- Depression is the leading cause of disability in terms of work years lost to disease
- 16% of U.S. adults have a history of at least one episode of depression... the average age of onset is 32
- 3,000: number of people lost to suicide ... every day (most have depression)
- 60,000: number of people attempting suicide ... every day
- Every 1% rise in unemployment is associated with a 0.79% rise in suicides in nonelderly adults
- Greece has experienced a 36% increase in suicide attempts since its economic crisis began
- Less than half of people with depression receive any treatment
- Only 20% (in the United States) receive minimally adequate treatment
- At least one-sixth of people with depression actually have bipolar depression
- People with diabetes or heart disease who also have depression do more poorly and have a higher mortality
- People on Medicaid who have a chronic medical condition as well as a mental health diagnosis are hospitalized as much as 2-4 times more often for their medical condition than those who do not have a mental health diagnosis
- If they also have an addiction diagnosis, they are hospitalized 8-15 times more often for their chronic medical condition
Here is a list of resources for more information on depression:
- Take a free screening for depression, bipolar, anxiety, and posttraumatic stress disorders
—Steven R. Daviss, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog.
The Med Check Racket: More Controversy
A reader from Carlisle, Pa., writes:
If Dr. Miller has ever practiced in a community mental health setting, she gives no evidence of it in her article. The title itself being offensive, the suggestion that “the economics might be clear” eludes me. The economics are not at all clear to me.
I am employed (and therefore have no personal stake in the fee schedule whatsoever) by a community mental health center that serves two counties in south-central Pennsylvania. My practice includes, I am told, about 1,400 patients, the vast majority of them without insurance other than Medicaid and/or Medicare. Many of these patients have no coverage for prescription medications, or have a carrier whose formulary is so restrictive as to require many hours of a nurse’s time to "prior auth" a mainstream medication, or to beg the drug rep for samples.
So, 1,400 patients, 40-hour/week work schedule: You do the math. The med-check “racket” here provides service for patients to which they would not otherwise have access.
The reader was offended by my post “The Med Check Racket,” which appeared on this blog in July, and in the August print edition of Clinical Psychiatry News. He is in good company; my article was so offensive to Dr. Anne Hanson, my co-blogger/author and good friend, that she responded the following week with her own post titled, “Those Evil Med Checks,” where she talks about her clinical work in the prisons. If you haven’t read it, please do.
I have worked at a number of community mental health centers. When I finished residency, I worked half-time at a CMHC, while I simultaneously began a private practice. I left that job to become medical director of a different CMHC, a position that enabled me to learn about the finances of public mental health clinics.
Since 1998, I have consulted part-time to the Johns Hopkins Community Psychiatry Program, and for a few years, I volunteered for HealthCare for the Homeless. I do know at least a little about community psychiatry.
“The Med Check Racket” was titled by a friend who complained to me about a private practice psychiatrist who sees him for 15 minutes every 6 months and asks a few, checklist-style, questions. I borrowed his comment as a title because I thought it was provocative, but I did not intend it to be offensive. Obviously, I was wrong!
I still believe that it does our profession no good to have patients who walk away feeling they have not been heard, and that psychiatry is too complicated to put every patient into a med-check slot, regardless of what they require. But I believe that the term “racket” is reserved for fee-for-service practices where the physician makes more money by seeing more patients. I don’t believe it’s a term that anyone would apply to an over-taxed, under-funded setting where the doctor is paid a set salary (often well below private practice rates), regardless of how many, or how few, patients s/he sees.
The issues for private practice are different from those of clinics or prisons. In an outpatient practice, the psychiatrist often does not have an easy means to communicate with the psychotherapist. It requires obtaining and transmitting a release form, then taking time to call the therapist or to send notes. Care may be fragmented. In a clinic setting, while the psychiatrist does not do the psychotherapy, a single chart is shared among team members – including the psychiatrists, psychotherapists, nurses (to give depot injections, check vital sign, and do psychotherapy), and case managers. The therapists and case managers are often in communication with residential care providers and day program personnel, and they are able to relay pertinent information to the psychiatrist.
In the Community Psychiatry Program at Johns Hopkins, the therapist attends the routine 90 day review visits with the psychiatrist and patient in the same room.
In addition to issues related to communications and information exchange, clinic/prison care is often provided at little or no cost to the patient, and the psychiatrist is salaried. In Maryland, state regulators require that patients in publicly funded Outpatient Mental Health Centers be seen every 90 days, and psychiatrists don’t have the leeway to either recommend or accommodate a less frequent schedule. Patients may well be aware that the system is overtaxed, and the décor at every clinic I have worked at leaves no one doubting that finances are tight.
Still, I am perplexed by the ratio of 1 psychiatrist to 1,400 patients. The expectation at every clinic I have worked in has been that a full-time (40 hour/week) psychiatrist is responsible for the care of roughly 300 patients.
Certainly, this reflects life in a major city, one with two large psychiatric training programs, where it is possible to recruit physicians. There are areas of the country where the supply of psychiatrists simply does not meet the demand, and the available psychiatrists should be lauded for providing the care that no one else wants to give, even if it means they are stretched too thin. If, however, the clinic setting is unable to attract psychiatrists because the salaries being offered are not commensurate with what other area psychiatrists earn, then the system (not the doctor) should be criticized for expecting one doctor to care for 1,400 patients.
So the evil med check racket: It seems it’s a way not only for insurance companies to minimize their expenses and to leave at least some patients feeling unheard, but also to divide us as a profession when it comes to appreciating what we each do.
—Dinah Miller, M.D.
DR. MILLER is the author of two new novels, Home Inspection and Double Billing and she is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work.
A reader from Carlisle, Pa., writes:
If Dr. Miller has ever practiced in a community mental health setting, she gives no evidence of it in her article. The title itself being offensive, the suggestion that “the economics might be clear” eludes me. The economics are not at all clear to me.
I am employed (and therefore have no personal stake in the fee schedule whatsoever) by a community mental health center that serves two counties in south-central Pennsylvania. My practice includes, I am told, about 1,400 patients, the vast majority of them without insurance other than Medicaid and/or Medicare. Many of these patients have no coverage for prescription medications, or have a carrier whose formulary is so restrictive as to require many hours of a nurse’s time to "prior auth" a mainstream medication, or to beg the drug rep for samples.
So, 1,400 patients, 40-hour/week work schedule: You do the math. The med-check “racket” here provides service for patients to which they would not otherwise have access.
The reader was offended by my post “The Med Check Racket,” which appeared on this blog in July, and in the August print edition of Clinical Psychiatry News. He is in good company; my article was so offensive to Dr. Anne Hanson, my co-blogger/author and good friend, that she responded the following week with her own post titled, “Those Evil Med Checks,” where she talks about her clinical work in the prisons. If you haven’t read it, please do.
I have worked at a number of community mental health centers. When I finished residency, I worked half-time at a CMHC, while I simultaneously began a private practice. I left that job to become medical director of a different CMHC, a position that enabled me to learn about the finances of public mental health clinics.
Since 1998, I have consulted part-time to the Johns Hopkins Community Psychiatry Program, and for a few years, I volunteered for HealthCare for the Homeless. I do know at least a little about community psychiatry.
“The Med Check Racket” was titled by a friend who complained to me about a private practice psychiatrist who sees him for 15 minutes every 6 months and asks a few, checklist-style, questions. I borrowed his comment as a title because I thought it was provocative, but I did not intend it to be offensive. Obviously, I was wrong!
I still believe that it does our profession no good to have patients who walk away feeling they have not been heard, and that psychiatry is too complicated to put every patient into a med-check slot, regardless of what they require. But I believe that the term “racket” is reserved for fee-for-service practices where the physician makes more money by seeing more patients. I don’t believe it’s a term that anyone would apply to an over-taxed, under-funded setting where the doctor is paid a set salary (often well below private practice rates), regardless of how many, or how few, patients s/he sees.
The issues for private practice are different from those of clinics or prisons. In an outpatient practice, the psychiatrist often does not have an easy means to communicate with the psychotherapist. It requires obtaining and transmitting a release form, then taking time to call the therapist or to send notes. Care may be fragmented. In a clinic setting, while the psychiatrist does not do the psychotherapy, a single chart is shared among team members – including the psychiatrists, psychotherapists, nurses (to give depot injections, check vital sign, and do psychotherapy), and case managers. The therapists and case managers are often in communication with residential care providers and day program personnel, and they are able to relay pertinent information to the psychiatrist.
In the Community Psychiatry Program at Johns Hopkins, the therapist attends the routine 90 day review visits with the psychiatrist and patient in the same room.
In addition to issues related to communications and information exchange, clinic/prison care is often provided at little or no cost to the patient, and the psychiatrist is salaried. In Maryland, state regulators require that patients in publicly funded Outpatient Mental Health Centers be seen every 90 days, and psychiatrists don’t have the leeway to either recommend or accommodate a less frequent schedule. Patients may well be aware that the system is overtaxed, and the décor at every clinic I have worked at leaves no one doubting that finances are tight.
Still, I am perplexed by the ratio of 1 psychiatrist to 1,400 patients. The expectation at every clinic I have worked in has been that a full-time (40 hour/week) psychiatrist is responsible for the care of roughly 300 patients.
Certainly, this reflects life in a major city, one with two large psychiatric training programs, where it is possible to recruit physicians. There are areas of the country where the supply of psychiatrists simply does not meet the demand, and the available psychiatrists should be lauded for providing the care that no one else wants to give, even if it means they are stretched too thin. If, however, the clinic setting is unable to attract psychiatrists because the salaries being offered are not commensurate with what other area psychiatrists earn, then the system (not the doctor) should be criticized for expecting one doctor to care for 1,400 patients.
So the evil med check racket: It seems it’s a way not only for insurance companies to minimize their expenses and to leave at least some patients feeling unheard, but also to divide us as a profession when it comes to appreciating what we each do.
—Dinah Miller, M.D.
DR. MILLER is the author of two new novels, Home Inspection and Double Billing and she is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work.
A reader from Carlisle, Pa., writes:
If Dr. Miller has ever practiced in a community mental health setting, she gives no evidence of it in her article. The title itself being offensive, the suggestion that “the economics might be clear” eludes me. The economics are not at all clear to me.
I am employed (and therefore have no personal stake in the fee schedule whatsoever) by a community mental health center that serves two counties in south-central Pennsylvania. My practice includes, I am told, about 1,400 patients, the vast majority of them without insurance other than Medicaid and/or Medicare. Many of these patients have no coverage for prescription medications, or have a carrier whose formulary is so restrictive as to require many hours of a nurse’s time to "prior auth" a mainstream medication, or to beg the drug rep for samples.
So, 1,400 patients, 40-hour/week work schedule: You do the math. The med-check “racket” here provides service for patients to which they would not otherwise have access.
The reader was offended by my post “The Med Check Racket,” which appeared on this blog in July, and in the August print edition of Clinical Psychiatry News. He is in good company; my article was so offensive to Dr. Anne Hanson, my co-blogger/author and good friend, that she responded the following week with her own post titled, “Those Evil Med Checks,” where she talks about her clinical work in the prisons. If you haven’t read it, please do.
I have worked at a number of community mental health centers. When I finished residency, I worked half-time at a CMHC, while I simultaneously began a private practice. I left that job to become medical director of a different CMHC, a position that enabled me to learn about the finances of public mental health clinics.
Since 1998, I have consulted part-time to the Johns Hopkins Community Psychiatry Program, and for a few years, I volunteered for HealthCare for the Homeless. I do know at least a little about community psychiatry.
“The Med Check Racket” was titled by a friend who complained to me about a private practice psychiatrist who sees him for 15 minutes every 6 months and asks a few, checklist-style, questions. I borrowed his comment as a title because I thought it was provocative, but I did not intend it to be offensive. Obviously, I was wrong!
I still believe that it does our profession no good to have patients who walk away feeling they have not been heard, and that psychiatry is too complicated to put every patient into a med-check slot, regardless of what they require. But I believe that the term “racket” is reserved for fee-for-service practices where the physician makes more money by seeing more patients. I don’t believe it’s a term that anyone would apply to an over-taxed, under-funded setting where the doctor is paid a set salary (often well below private practice rates), regardless of how many, or how few, patients s/he sees.
The issues for private practice are different from those of clinics or prisons. In an outpatient practice, the psychiatrist often does not have an easy means to communicate with the psychotherapist. It requires obtaining and transmitting a release form, then taking time to call the therapist or to send notes. Care may be fragmented. In a clinic setting, while the psychiatrist does not do the psychotherapy, a single chart is shared among team members – including the psychiatrists, psychotherapists, nurses (to give depot injections, check vital sign, and do psychotherapy), and case managers. The therapists and case managers are often in communication with residential care providers and day program personnel, and they are able to relay pertinent information to the psychiatrist.
In the Community Psychiatry Program at Johns Hopkins, the therapist attends the routine 90 day review visits with the psychiatrist and patient in the same room.
In addition to issues related to communications and information exchange, clinic/prison care is often provided at little or no cost to the patient, and the psychiatrist is salaried. In Maryland, state regulators require that patients in publicly funded Outpatient Mental Health Centers be seen every 90 days, and psychiatrists don’t have the leeway to either recommend or accommodate a less frequent schedule. Patients may well be aware that the system is overtaxed, and the décor at every clinic I have worked at leaves no one doubting that finances are tight.
Still, I am perplexed by the ratio of 1 psychiatrist to 1,400 patients. The expectation at every clinic I have worked in has been that a full-time (40 hour/week) psychiatrist is responsible for the care of roughly 300 patients.
Certainly, this reflects life in a major city, one with two large psychiatric training programs, where it is possible to recruit physicians. There are areas of the country where the supply of psychiatrists simply does not meet the demand, and the available psychiatrists should be lauded for providing the care that no one else wants to give, even if it means they are stretched too thin. If, however, the clinic setting is unable to attract psychiatrists because the salaries being offered are not commensurate with what other area psychiatrists earn, then the system (not the doctor) should be criticized for expecting one doctor to care for 1,400 patients.
So the evil med check racket: It seems it’s a way not only for insurance companies to minimize their expenses and to leave at least some patients feeling unheard, but also to divide us as a profession when it comes to appreciating what we each do.
—Dinah Miller, M.D.
DR. MILLER is the author of two new novels, Home Inspection and Double Billing and she is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work.
This Funny Thing We Call Privacy
When I go to the dentist, I sign in at the window, check off box that says I haven’t moved or changed insurance, and then have a seat in the waiting room with the other patients and a large tank of colorful fish. A secretary takes the sign-in sheet, in a HIPAA-compliant fashion, blacks out my name with a Sharpee. This is, I’m told, good. If you’re not another patient in the waiting room, a colorful fish, a dentist, hygenicist, or office staff at this large practice, and if you don’t happen to see my name posted on the schedule on the wall in the treatroom, then no one has to know that I get my teeth cleaned. I’m all for privacy in medical care.
The same issues come up in psychiatry, and all of medicine for that matter. The government mandates all types of procedures that protect patient privacy, and these procedures take time, effort, and money. Since I value privacy for medical treatment, I should be happy, but instead, I find many of the privacy regulations to be burdensome, and they create this odd state of perception of privacy when the reality remains that the privacy of medical treatment is compromised.
It’s regulated that sign-in sheets compromise privacy, but there remains the risk that patients might see each other in the waiting room. Perhaps every patient should have a mini-cubicle with black curtains to sit in? To protect privacy, when I sign in to my clinic’s electronic medical record and its e-prescribing program, both programs automatically sign me out every few minutes, a minor annoyance, but one of many.
The electronic medical record provides many conveniences, especially since psychiatric outpatient records have not yet been incorporated into them. I can access labs, read notes by other physicians, and I don’t have to spend time entering sensitive psychiatric information, except for medications. Given that psychiatric records have extra protections, can a patient elect to not to tell another physician that they see a psychiatrist? Well, not really, because the medications get entered into the record, it is recorded that the patient had an appointment with psychiatry, and patients often tell their primary care doctors that they are treated by a psychiatrist, so their diagnoses and medications are recorded by those doctors in their notes.
If patients are not comfortable telling their dermatologist that they have been treated for bipolar disorder, or had three abortions, they lose that option. Perhaps it’s not all bad – their lithium could be making their skin condition worse, and patients don’t always know which information it is important to share. But it may also be true that a physician may ascribe patients’ symptoms to their psychiatric condition and not evaluate them with the same diligence they would if a psychiatric condition were not revealed. (Does this still happen? That’s it’s own blog post, but see Discrimination Against Patients with a Psychiatric History for another medical blogger’s insights on this.)
So our illusion of privacy goes one step further with electronic records. In the institution where I work, I believe (and I could be wrong about the number) that approximately 9,000 people have access to the records. There are checks on the system to determine that those accessing have valid reason, but those checks are random, and the major impediment to obliging curiosity and looking at the records of a friend, neighbor, colleague, or ex-girlfriend, remains the fear of being discovered and the serious repercussions that would occur.
In Maryland, our state legislature has spent years debating whether the state’s Board of Physicians should be able to look at patient records if a third party lodges a complaint against a doctor and patients do not want their records released. Yet, hospital regulators regularly review psychiatric charts to determine if they are in compliance for accreditation purposes, without getting the patient’s authorization first. And insurance companies access patient records with patient authorization, then often use this information to deny coverage, but is it really “authorization” (a valid form of consent) if desperately ill patients are told they won’t be treated if they don’t sign?
So we shred. We pay for secure portals for email. We follow rules regarding secured, HIPAA-compliant fax locations. We sign in and out of the various computer screens every 7 minutes to make sure no unauthorized soul sneaks in and reads when we aren’t looking. Our government pays physicians to install EMRs with the promise that this will make medicine better. We refuse to speak with families and with physicians outside our system without signed releases, even if doing so delays care or creates inconvenience. All patients sign off that they were offered privacy notices.
Our patients see all this, and it leads them to believe that confidentiality laws make their treatment more private, that the system has many safeguards, and that only the fish know they are getting their teeth cleaned. I can’t help but think it would be so nice if there were a little less in the way of regulation and requirements and a little more attention to the best interest and privacy needs of the individual patient.
—Dinah Miller, M.D.
DR. MILLER is the author of two new novels, Home Inspection and Double Billing and she is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work.
When I go to the dentist, I sign in at the window, check off box that says I haven’t moved or changed insurance, and then have a seat in the waiting room with the other patients and a large tank of colorful fish. A secretary takes the sign-in sheet, in a HIPAA-compliant fashion, blacks out my name with a Sharpee. This is, I’m told, good. If you’re not another patient in the waiting room, a colorful fish, a dentist, hygenicist, or office staff at this large practice, and if you don’t happen to see my name posted on the schedule on the wall in the treatroom, then no one has to know that I get my teeth cleaned. I’m all for privacy in medical care.
The same issues come up in psychiatry, and all of medicine for that matter. The government mandates all types of procedures that protect patient privacy, and these procedures take time, effort, and money. Since I value privacy for medical treatment, I should be happy, but instead, I find many of the privacy regulations to be burdensome, and they create this odd state of perception of privacy when the reality remains that the privacy of medical treatment is compromised.
It’s regulated that sign-in sheets compromise privacy, but there remains the risk that patients might see each other in the waiting room. Perhaps every patient should have a mini-cubicle with black curtains to sit in? To protect privacy, when I sign in to my clinic’s electronic medical record and its e-prescribing program, both programs automatically sign me out every few minutes, a minor annoyance, but one of many.
The electronic medical record provides many conveniences, especially since psychiatric outpatient records have not yet been incorporated into them. I can access labs, read notes by other physicians, and I don’t have to spend time entering sensitive psychiatric information, except for medications. Given that psychiatric records have extra protections, can a patient elect to not to tell another physician that they see a psychiatrist? Well, not really, because the medications get entered into the record, it is recorded that the patient had an appointment with psychiatry, and patients often tell their primary care doctors that they are treated by a psychiatrist, so their diagnoses and medications are recorded by those doctors in their notes.
If patients are not comfortable telling their dermatologist that they have been treated for bipolar disorder, or had three abortions, they lose that option. Perhaps it’s not all bad – their lithium could be making their skin condition worse, and patients don’t always know which information it is important to share. But it may also be true that a physician may ascribe patients’ symptoms to their psychiatric condition and not evaluate them with the same diligence they would if a psychiatric condition were not revealed. (Does this still happen? That’s it’s own blog post, but see Discrimination Against Patients with a Psychiatric History for another medical blogger’s insights on this.)
So our illusion of privacy goes one step further with electronic records. In the institution where I work, I believe (and I could be wrong about the number) that approximately 9,000 people have access to the records. There are checks on the system to determine that those accessing have valid reason, but those checks are random, and the major impediment to obliging curiosity and looking at the records of a friend, neighbor, colleague, or ex-girlfriend, remains the fear of being discovered and the serious repercussions that would occur.
In Maryland, our state legislature has spent years debating whether the state’s Board of Physicians should be able to look at patient records if a third party lodges a complaint against a doctor and patients do not want their records released. Yet, hospital regulators regularly review psychiatric charts to determine if they are in compliance for accreditation purposes, without getting the patient’s authorization first. And insurance companies access patient records with patient authorization, then often use this information to deny coverage, but is it really “authorization” (a valid form of consent) if desperately ill patients are told they won’t be treated if they don’t sign?
So we shred. We pay for secure portals for email. We follow rules regarding secured, HIPAA-compliant fax locations. We sign in and out of the various computer screens every 7 minutes to make sure no unauthorized soul sneaks in and reads when we aren’t looking. Our government pays physicians to install EMRs with the promise that this will make medicine better. We refuse to speak with families and with physicians outside our system without signed releases, even if doing so delays care or creates inconvenience. All patients sign off that they were offered privacy notices.
Our patients see all this, and it leads them to believe that confidentiality laws make their treatment more private, that the system has many safeguards, and that only the fish know they are getting their teeth cleaned. I can’t help but think it would be so nice if there were a little less in the way of regulation and requirements and a little more attention to the best interest and privacy needs of the individual patient.
—Dinah Miller, M.D.
DR. MILLER is the author of two new novels, Home Inspection and Double Billing and she is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work.
When I go to the dentist, I sign in at the window, check off box that says I haven’t moved or changed insurance, and then have a seat in the waiting room with the other patients and a large tank of colorful fish. A secretary takes the sign-in sheet, in a HIPAA-compliant fashion, blacks out my name with a Sharpee. This is, I’m told, good. If you’re not another patient in the waiting room, a colorful fish, a dentist, hygenicist, or office staff at this large practice, and if you don’t happen to see my name posted on the schedule on the wall in the treatroom, then no one has to know that I get my teeth cleaned. I’m all for privacy in medical care.
The same issues come up in psychiatry, and all of medicine for that matter. The government mandates all types of procedures that protect patient privacy, and these procedures take time, effort, and money. Since I value privacy for medical treatment, I should be happy, but instead, I find many of the privacy regulations to be burdensome, and they create this odd state of perception of privacy when the reality remains that the privacy of medical treatment is compromised.
It’s regulated that sign-in sheets compromise privacy, but there remains the risk that patients might see each other in the waiting room. Perhaps every patient should have a mini-cubicle with black curtains to sit in? To protect privacy, when I sign in to my clinic’s electronic medical record and its e-prescribing program, both programs automatically sign me out every few minutes, a minor annoyance, but one of many.
The electronic medical record provides many conveniences, especially since psychiatric outpatient records have not yet been incorporated into them. I can access labs, read notes by other physicians, and I don’t have to spend time entering sensitive psychiatric information, except for medications. Given that psychiatric records have extra protections, can a patient elect to not to tell another physician that they see a psychiatrist? Well, not really, because the medications get entered into the record, it is recorded that the patient had an appointment with psychiatry, and patients often tell their primary care doctors that they are treated by a psychiatrist, so their diagnoses and medications are recorded by those doctors in their notes.
If patients are not comfortable telling their dermatologist that they have been treated for bipolar disorder, or had three abortions, they lose that option. Perhaps it’s not all bad – their lithium could be making their skin condition worse, and patients don’t always know which information it is important to share. But it may also be true that a physician may ascribe patients’ symptoms to their psychiatric condition and not evaluate them with the same diligence they would if a psychiatric condition were not revealed. (Does this still happen? That’s it’s own blog post, but see Discrimination Against Patients with a Psychiatric History for another medical blogger’s insights on this.)
So our illusion of privacy goes one step further with electronic records. In the institution where I work, I believe (and I could be wrong about the number) that approximately 9,000 people have access to the records. There are checks on the system to determine that those accessing have valid reason, but those checks are random, and the major impediment to obliging curiosity and looking at the records of a friend, neighbor, colleague, or ex-girlfriend, remains the fear of being discovered and the serious repercussions that would occur.
In Maryland, our state legislature has spent years debating whether the state’s Board of Physicians should be able to look at patient records if a third party lodges a complaint against a doctor and patients do not want their records released. Yet, hospital regulators regularly review psychiatric charts to determine if they are in compliance for accreditation purposes, without getting the patient’s authorization first. And insurance companies access patient records with patient authorization, then often use this information to deny coverage, but is it really “authorization” (a valid form of consent) if desperately ill patients are told they won’t be treated if they don’t sign?
So we shred. We pay for secure portals for email. We follow rules regarding secured, HIPAA-compliant fax locations. We sign in and out of the various computer screens every 7 minutes to make sure no unauthorized soul sneaks in and reads when we aren’t looking. Our government pays physicians to install EMRs with the promise that this will make medicine better. We refuse to speak with families and with physicians outside our system without signed releases, even if doing so delays care or creates inconvenience. All patients sign off that they were offered privacy notices.
Our patients see all this, and it leads them to believe that confidentiality laws make their treatment more private, that the system has many safeguards, and that only the fish know they are getting their teeth cleaned. I can’t help but think it would be so nice if there were a little less in the way of regulation and requirements and a little more attention to the best interest and privacy needs of the individual patient.
—Dinah Miller, M.D.
DR. MILLER is the author of two new novels, Home Inspection and Double Billing and she is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work.
The Deep, Dark Past of Dr. Lynne Fenton
Let me start with the usual disclaimers. We have very little information about the young man who allegedly shot 70 people at a midnight showing of the "Batman" movie in Aurora, Colo., and from a psychiatrist's standpoint, there is nothing to say. Let me add to my disclaimer that I am going to mention some statistics as my article goes on and they were obtained through a quick, informal, e-mail poll that was not validated and doesn't begin to approach anything one might call science.
I was surprised, and a bit dismayed, last week when the media announced that a package had been recovered from a university mail room that was addressed to Dr. Lynne Fenton, the director of student mental health at the University of Colorado’s Anschutz Medical Campus, where the alleged shooter was a graduate student. While other high-profile mass murderers have had histories of psychiatric treatment, this is the first time that I can recall the name of an alleged treating psychiatrist being released by the media so soon after a tragedy.
I know nothing about this psychiatrist – whether she did in fact treat the alleged shooter, whether or not she offered adequate or appropriate care – I felt badly for her. If she did, in fact, treat the shooter, she must be quite upset.
To me, the hardest part about being a psychiatrist is feeling responsible for the behavior of others. If, as the media reported, there were no warning signs, then this is every psychiatrist’s worst fear.
The journalists proceeded on with a flurry of reports. The first story I saw said Dr. Fenton studies schizophrenia. Wouldn’t that lead the general public to believe that the shooter must have schizophrenia? While that might be the case, it could also be that a student mental health center treats all students requesting care, and that most of them probably do not have schizophrenia. It could also be the case that Dr. Fenton had never treated the alleged shooter, but that he had simply identified her as someone to send a package to.
Soon after, the media began to focus on the psychiatrist's past misdeeds, with headlines about her "dark” and “troubled” past, and this has been the focus of many news stories over the past few days. The implication, I believe, is that the alleged shooter was being treated by a bad psychiatrist.
Dr. Fenton had been disciplined in 2004 for writing prescriptions for herself, her husband, and an employee with a headache, events that occurred in 1997-1999 (Colorado State Board of Medical Examiners Stipulation and Final Agency Order, case no. 5101021920, Sept. 23, 2004). Apparently, her prescribing practices came to the attention of the Drug Enforcement Administration when she reported a former employee who was forging her prescriptions to get large quantities of narcotics.
In the course of the DEA investigation, it was revealed that she had written the following prescriptions without documenting them: Claritin and Ambien for her husband, three tablets of Xanax that she took during a period when her mother was dying, four tablets of Xanax for someone who was anxious about an airline flight, and a prescription for a pain killer and sedative for an employee with a headache. Dr. Fenton admitted to these infractions, received a letter of admonition, and was required to take a course on documentation.
Are these prescriptions, written nearly 15 years ago and sanctioned 8 years ago, somehow relevant to the Aurora shootings? I have a hard time seeing it as anything other than dragging a psychiatrist through mud for the sake of getting muddy. In a quick and dirty e-mail poll, I discovered that 85% of a small sample of psychiatrists had ever written a prescription for themselves, a family member, a colleague, or a friend, while 20% had written a prescription for a controlled substance for someone who is not their patient. Again, my sample was small, my methods were not scientific, but I wanted a frame of reference for a doctor’s infraction that has been so sensationalized.
When a tragedy such as this happens, everyone is quick to look for reasons. We’d like to understand what transpired so that we can prevent it from happening again. None of us want to be killed at the movies, and none of us want to make the wrong call on a potentially violent patient. I don’t know anything about Dr. Fenton or her relationship with the alleged Aurora shooter, but I do believe the media should try to keep the stories relevant.
—Dinah Miller
DR. MILLER is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. Home Inspection, her novel about psychotherapy and the quest for love, was recently released as an Amazon Kindle book. She blogs at Shrink Rap.
Let me start with the usual disclaimers. We have very little information about the young man who allegedly shot 70 people at a midnight showing of the "Batman" movie in Aurora, Colo., and from a psychiatrist's standpoint, there is nothing to say. Let me add to my disclaimer that I am going to mention some statistics as my article goes on and they were obtained through a quick, informal, e-mail poll that was not validated and doesn't begin to approach anything one might call science.
I was surprised, and a bit dismayed, last week when the media announced that a package had been recovered from a university mail room that was addressed to Dr. Lynne Fenton, the director of student mental health at the University of Colorado’s Anschutz Medical Campus, where the alleged shooter was a graduate student. While other high-profile mass murderers have had histories of psychiatric treatment, this is the first time that I can recall the name of an alleged treating psychiatrist being released by the media so soon after a tragedy.
I know nothing about this psychiatrist – whether she did in fact treat the alleged shooter, whether or not she offered adequate or appropriate care – I felt badly for her. If she did, in fact, treat the shooter, she must be quite upset.
To me, the hardest part about being a psychiatrist is feeling responsible for the behavior of others. If, as the media reported, there were no warning signs, then this is every psychiatrist’s worst fear.
The journalists proceeded on with a flurry of reports. The first story I saw said Dr. Fenton studies schizophrenia. Wouldn’t that lead the general public to believe that the shooter must have schizophrenia? While that might be the case, it could also be that a student mental health center treats all students requesting care, and that most of them probably do not have schizophrenia. It could also be the case that Dr. Fenton had never treated the alleged shooter, but that he had simply identified her as someone to send a package to.
Soon after, the media began to focus on the psychiatrist's past misdeeds, with headlines about her "dark” and “troubled” past, and this has been the focus of many news stories over the past few days. The implication, I believe, is that the alleged shooter was being treated by a bad psychiatrist.
Dr. Fenton had been disciplined in 2004 for writing prescriptions for herself, her husband, and an employee with a headache, events that occurred in 1997-1999 (Colorado State Board of Medical Examiners Stipulation and Final Agency Order, case no. 5101021920, Sept. 23, 2004). Apparently, her prescribing practices came to the attention of the Drug Enforcement Administration when she reported a former employee who was forging her prescriptions to get large quantities of narcotics.
In the course of the DEA investigation, it was revealed that she had written the following prescriptions without documenting them: Claritin and Ambien for her husband, three tablets of Xanax that she took during a period when her mother was dying, four tablets of Xanax for someone who was anxious about an airline flight, and a prescription for a pain killer and sedative for an employee with a headache. Dr. Fenton admitted to these infractions, received a letter of admonition, and was required to take a course on documentation.
Are these prescriptions, written nearly 15 years ago and sanctioned 8 years ago, somehow relevant to the Aurora shootings? I have a hard time seeing it as anything other than dragging a psychiatrist through mud for the sake of getting muddy. In a quick and dirty e-mail poll, I discovered that 85% of a small sample of psychiatrists had ever written a prescription for themselves, a family member, a colleague, or a friend, while 20% had written a prescription for a controlled substance for someone who is not their patient. Again, my sample was small, my methods were not scientific, but I wanted a frame of reference for a doctor’s infraction that has been so sensationalized.
When a tragedy such as this happens, everyone is quick to look for reasons. We’d like to understand what transpired so that we can prevent it from happening again. None of us want to be killed at the movies, and none of us want to make the wrong call on a potentially violent patient. I don’t know anything about Dr. Fenton or her relationship with the alleged Aurora shooter, but I do believe the media should try to keep the stories relevant.
—Dinah Miller
DR. MILLER is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. Home Inspection, her novel about psychotherapy and the quest for love, was recently released as an Amazon Kindle book. She blogs at Shrink Rap.
Let me start with the usual disclaimers. We have very little information about the young man who allegedly shot 70 people at a midnight showing of the "Batman" movie in Aurora, Colo., and from a psychiatrist's standpoint, there is nothing to say. Let me add to my disclaimer that I am going to mention some statistics as my article goes on and they were obtained through a quick, informal, e-mail poll that was not validated and doesn't begin to approach anything one might call science.
I was surprised, and a bit dismayed, last week when the media announced that a package had been recovered from a university mail room that was addressed to Dr. Lynne Fenton, the director of student mental health at the University of Colorado’s Anschutz Medical Campus, where the alleged shooter was a graduate student. While other high-profile mass murderers have had histories of psychiatric treatment, this is the first time that I can recall the name of an alleged treating psychiatrist being released by the media so soon after a tragedy.
I know nothing about this psychiatrist – whether she did in fact treat the alleged shooter, whether or not she offered adequate or appropriate care – I felt badly for her. If she did, in fact, treat the shooter, she must be quite upset.
To me, the hardest part about being a psychiatrist is feeling responsible for the behavior of others. If, as the media reported, there were no warning signs, then this is every psychiatrist’s worst fear.
The journalists proceeded on with a flurry of reports. The first story I saw said Dr. Fenton studies schizophrenia. Wouldn’t that lead the general public to believe that the shooter must have schizophrenia? While that might be the case, it could also be that a student mental health center treats all students requesting care, and that most of them probably do not have schizophrenia. It could also be the case that Dr. Fenton had never treated the alleged shooter, but that he had simply identified her as someone to send a package to.
Soon after, the media began to focus on the psychiatrist's past misdeeds, with headlines about her "dark” and “troubled” past, and this has been the focus of many news stories over the past few days. The implication, I believe, is that the alleged shooter was being treated by a bad psychiatrist.
Dr. Fenton had been disciplined in 2004 for writing prescriptions for herself, her husband, and an employee with a headache, events that occurred in 1997-1999 (Colorado State Board of Medical Examiners Stipulation and Final Agency Order, case no. 5101021920, Sept. 23, 2004). Apparently, her prescribing practices came to the attention of the Drug Enforcement Administration when she reported a former employee who was forging her prescriptions to get large quantities of narcotics.
In the course of the DEA investigation, it was revealed that she had written the following prescriptions without documenting them: Claritin and Ambien for her husband, three tablets of Xanax that she took during a period when her mother was dying, four tablets of Xanax for someone who was anxious about an airline flight, and a prescription for a pain killer and sedative for an employee with a headache. Dr. Fenton admitted to these infractions, received a letter of admonition, and was required to take a course on documentation.
Are these prescriptions, written nearly 15 years ago and sanctioned 8 years ago, somehow relevant to the Aurora shootings? I have a hard time seeing it as anything other than dragging a psychiatrist through mud for the sake of getting muddy. In a quick and dirty e-mail poll, I discovered that 85% of a small sample of psychiatrists had ever written a prescription for themselves, a family member, a colleague, or a friend, while 20% had written a prescription for a controlled substance for someone who is not their patient. Again, my sample was small, my methods were not scientific, but I wanted a frame of reference for a doctor’s infraction that has been so sensationalized.
When a tragedy such as this happens, everyone is quick to look for reasons. We’d like to understand what transpired so that we can prevent it from happening again. None of us want to be killed at the movies, and none of us want to make the wrong call on a potentially violent patient. I don’t know anything about Dr. Fenton or her relationship with the alleged Aurora shooter, but I do believe the media should try to keep the stories relevant.
—Dinah Miller
DR. MILLER is the co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. Home Inspection, her novel about psychotherapy and the quest for love, was recently released as an Amazon Kindle book. She blogs at Shrink Rap.
The Aurora Shootings: Why the Mental Health Community Must Show Restraint
One of the hazards of being a forensic psychiatrist is that in the wake of certain high-profile events you get nudged, privately and publicly, to speculate on what you “really think was going on” in the mind of the perpetrator.
Unfortunately, in the last few years, there have been several opportunities for this to happen: following the Amish murders in Lancaster County, the Virginia Tech and Fort Hood incidents, and after six people died in the Arizona shooting. Thanks to social media, you can also now follow the media coverage in real time through Twitter feeds and live-blogging journalists. Social media enabled me to follow public comments made by various mental health professionals immediately following the offense.
Just out of curiosity, I did a little preliminary survey to see what these professionals had to say about the incident. I searched the Internet using the term “Colorado shooter motivation” along with either the term “psychologist” or “psychiatrist.” While the following results are neither complete nor scientific, I think they are symptomatic of a problem in both professions.
What I discovered was that psychiatrists and psychologists from California, Texas, Illinois, Oregon, Pennsylvania, and South Carolina all proffered observations about the alleged shooter’s possible motivation as well as his mental state during a court appearance. Some went so far as to make specific diagnoses such as schizophrenia, an unspecified psychotic disorder, or psychopathy. All based their opinions solely upon information presented in the media, and only one – a psychologist – made a point of couching the opinion with the disclaimer that their information could be incomplete or simply wrong.
The most striking example I found was posted by a guest columnist for an online newspaper. This psychiatrist stated, “This man is mentally ill. I do not have information enough to be diagnosing, but clearly he has a psychotic disorder. No sane person behaves this way.”
While it may be tempting or flattering to be given the opportunity to be a media commentator, psychiatrists do have an ethical duty to restrict our public comments. According to Section 7.3 of the American Psychiatric Association's Principles of Medical Ethics:
“On occasion psychiatrists are asked for an opinion about an individual who is in the light of public attention or who has disclosed information about himself or herself through public media. In such circumstances, a psychiatrist may share with the public his or her expertise about psychiatric issues in general.
However, it is unethical for a psychiatrist to offer a professional opinion unless he or she has conducted an examination and has been granted proper authorization for such a statement.”
The requirement for a personal examination is particularly important when an opinion is derived solely from media sources whose information may be unreliable. In a recent court filing, the district attorney in the Colorado shooting case reportedly stated that the media was obtaining information from “hoaxers, fraudsters, or maybe from nobody at all.” Some of the early information that these professionals relied upon has now been found to be wrong, such as the suspect’s lack of previous contact with mental health care.
Ethical guidelines also require physicians to practice within their area of competence. Mental health professionals without experience or training specific to criminal behavior, violence and mental illness, and the legal assessment of competence or sanity may be practicing outside the scope of their training by offering opinions on these issues.
Not to be completely negative, there were good examples of psychiatric commentary. Dr. Keith Ablow, a member of the Fox News medical team, presented a detailed and careful overview of the sanity evaluation process and addressed a number of public misconceptions about the insanity defense.
The Goldwater rule was intended to protect celebrities, politicians and other high-profile figures from unwarranted invasion of privacy and damage to their reputations. I’m sure the authors of this clause didn’t anticipate the unintended effects such speculation could have on a criminal defendant, the alleged suspect’s family, or the victims of the offense. Public speculation about a criminal defendant has much more serious repercussions than a tarnished reputation.
Eventually, a jury will be empaneled to hear the case. Finding an unbiased juror will be difficult enough for a notorious offense, but may be impossible once the general public has been exposed to repeated statements by psychiatrists and psychologists about a defendant’s aberrant mental state. Even when couched in a disclaimer, jurors will remember the opinion rather than the disclaimer. If a death penalty is requested in this case, implications that a defendant has a serious mental illness could prejudice a sentencing hearing, since research has shown that a capital sentence is more likely to be given to mentally ill defendants.
Journalists will often ask mental health professionals about warning signals or red flags that may have been missed. When a psychiatrist publicly states that signs were missed, he implies that the suspect’s family, friends, and co-workers were somehow negligent for failing to prevent a tragedy. Public safety is not improved by blaming the suspect’s family. Susan Klebold, the mother of Columbine shooter Dylan Klebold, wrote a moving essay about her reaction to her son’s crime in her essay, “I Will Never Know Why”:
“Those of us who cared for Dylan felt responsible for his death. We thought, 'If I had been a better (mother, father, brother, friend, aunt, uncle, cousin), I would have known this was coming.’ We perceived his actions to be our failure. I tried to identify a pivotal event in his upbringing that could account for his anger. Had I been too strict? Not strict enough? Had I pushed too hard, or not hard enough? In the days before he died, I had hugged him and told him how much I loved him. I held his scratchy face between my palms and told him that he was a wonderful person and that I was proud of him. Had he felt pressured by this? Did he feel that he could not live up to my expectations?”
Similarly, survivors and family members of the victims can be traumatized by continued professional speculation. On our Shrink Rap blog, the mother of one Virginia Tech student thanked us for not discussing that crime. Here is how she described the effects on her son:
“The media coverage hurt as much as it helped. Many of those kids don’t want to talk about that day at all. It’s very hard for a young adult when the first thing they get asked about college is not “how do you like classes” or “what’s your major” but rather “Were you there, were you injured, did you know anyone who died?”
Finally, there is the risk of creating a copycat offender. Media attention has been a well-known cause of clustered suicides and can be a precipitant for other violent behavior. Almost on cue, Maryland police recently apprehended a man who threatened to “shoot up” his employer and referred to himself as “a joker.”
Considering all this, I’m grateful that I have consistently maintained one response to high-profile offenses: “No comment.”
—Annette Hanson, M.D.
DR. HANSON is a forensic psychiatrist and co-author of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
One of the hazards of being a forensic psychiatrist is that in the wake of certain high-profile events you get nudged, privately and publicly, to speculate on what you “really think was going on” in the mind of the perpetrator.
Unfortunately, in the last few years, there have been several opportunities for this to happen: following the Amish murders in Lancaster County, the Virginia Tech and Fort Hood incidents, and after six people died in the Arizona shooting. Thanks to social media, you can also now follow the media coverage in real time through Twitter feeds and live-blogging journalists. Social media enabled me to follow public comments made by various mental health professionals immediately following the offense.
Just out of curiosity, I did a little preliminary survey to see what these professionals had to say about the incident. I searched the Internet using the term “Colorado shooter motivation” along with either the term “psychologist” or “psychiatrist.” While the following results are neither complete nor scientific, I think they are symptomatic of a problem in both professions.
What I discovered was that psychiatrists and psychologists from California, Texas, Illinois, Oregon, Pennsylvania, and South Carolina all proffered observations about the alleged shooter’s possible motivation as well as his mental state during a court appearance. Some went so far as to make specific diagnoses such as schizophrenia, an unspecified psychotic disorder, or psychopathy. All based their opinions solely upon information presented in the media, and only one – a psychologist – made a point of couching the opinion with the disclaimer that their information could be incomplete or simply wrong.
The most striking example I found was posted by a guest columnist for an online newspaper. This psychiatrist stated, “This man is mentally ill. I do not have information enough to be diagnosing, but clearly he has a psychotic disorder. No sane person behaves this way.”
While it may be tempting or flattering to be given the opportunity to be a media commentator, psychiatrists do have an ethical duty to restrict our public comments. According to Section 7.3 of the American Psychiatric Association's Principles of Medical Ethics:
“On occasion psychiatrists are asked for an opinion about an individual who is in the light of public attention or who has disclosed information about himself or herself through public media. In such circumstances, a psychiatrist may share with the public his or her expertise about psychiatric issues in general.
However, it is unethical for a psychiatrist to offer a professional opinion unless he or she has conducted an examination and has been granted proper authorization for such a statement.”
The requirement for a personal examination is particularly important when an opinion is derived solely from media sources whose information may be unreliable. In a recent court filing, the district attorney in the Colorado shooting case reportedly stated that the media was obtaining information from “hoaxers, fraudsters, or maybe from nobody at all.” Some of the early information that these professionals relied upon has now been found to be wrong, such as the suspect’s lack of previous contact with mental health care.
Ethical guidelines also require physicians to practice within their area of competence. Mental health professionals without experience or training specific to criminal behavior, violence and mental illness, and the legal assessment of competence or sanity may be practicing outside the scope of their training by offering opinions on these issues.
Not to be completely negative, there were good examples of psychiatric commentary. Dr. Keith Ablow, a member of the Fox News medical team, presented a detailed and careful overview of the sanity evaluation process and addressed a number of public misconceptions about the insanity defense.
The Goldwater rule was intended to protect celebrities, politicians and other high-profile figures from unwarranted invasion of privacy and damage to their reputations. I’m sure the authors of this clause didn’t anticipate the unintended effects such speculation could have on a criminal defendant, the alleged suspect’s family, or the victims of the offense. Public speculation about a criminal defendant has much more serious repercussions than a tarnished reputation.
Eventually, a jury will be empaneled to hear the case. Finding an unbiased juror will be difficult enough for a notorious offense, but may be impossible once the general public has been exposed to repeated statements by psychiatrists and psychologists about a defendant’s aberrant mental state. Even when couched in a disclaimer, jurors will remember the opinion rather than the disclaimer. If a death penalty is requested in this case, implications that a defendant has a serious mental illness could prejudice a sentencing hearing, since research has shown that a capital sentence is more likely to be given to mentally ill defendants.
Journalists will often ask mental health professionals about warning signals or red flags that may have been missed. When a psychiatrist publicly states that signs were missed, he implies that the suspect’s family, friends, and co-workers were somehow negligent for failing to prevent a tragedy. Public safety is not improved by blaming the suspect’s family. Susan Klebold, the mother of Columbine shooter Dylan Klebold, wrote a moving essay about her reaction to her son’s crime in her essay, “I Will Never Know Why”:
“Those of us who cared for Dylan felt responsible for his death. We thought, 'If I had been a better (mother, father, brother, friend, aunt, uncle, cousin), I would have known this was coming.’ We perceived his actions to be our failure. I tried to identify a pivotal event in his upbringing that could account for his anger. Had I been too strict? Not strict enough? Had I pushed too hard, or not hard enough? In the days before he died, I had hugged him and told him how much I loved him. I held his scratchy face between my palms and told him that he was a wonderful person and that I was proud of him. Had he felt pressured by this? Did he feel that he could not live up to my expectations?”
Similarly, survivors and family members of the victims can be traumatized by continued professional speculation. On our Shrink Rap blog, the mother of one Virginia Tech student thanked us for not discussing that crime. Here is how she described the effects on her son:
“The media coverage hurt as much as it helped. Many of those kids don’t want to talk about that day at all. It’s very hard for a young adult when the first thing they get asked about college is not “how do you like classes” or “what’s your major” but rather “Were you there, were you injured, did you know anyone who died?”
Finally, there is the risk of creating a copycat offender. Media attention has been a well-known cause of clustered suicides and can be a precipitant for other violent behavior. Almost on cue, Maryland police recently apprehended a man who threatened to “shoot up” his employer and referred to himself as “a joker.”
Considering all this, I’m grateful that I have consistently maintained one response to high-profile offenses: “No comment.”
—Annette Hanson, M.D.
DR. HANSON is a forensic psychiatrist and co-author of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
One of the hazards of being a forensic psychiatrist is that in the wake of certain high-profile events you get nudged, privately and publicly, to speculate on what you “really think was going on” in the mind of the perpetrator.
Unfortunately, in the last few years, there have been several opportunities for this to happen: following the Amish murders in Lancaster County, the Virginia Tech and Fort Hood incidents, and after six people died in the Arizona shooting. Thanks to social media, you can also now follow the media coverage in real time through Twitter feeds and live-blogging journalists. Social media enabled me to follow public comments made by various mental health professionals immediately following the offense.
Just out of curiosity, I did a little preliminary survey to see what these professionals had to say about the incident. I searched the Internet using the term “Colorado shooter motivation” along with either the term “psychologist” or “psychiatrist.” While the following results are neither complete nor scientific, I think they are symptomatic of a problem in both professions.
What I discovered was that psychiatrists and psychologists from California, Texas, Illinois, Oregon, Pennsylvania, and South Carolina all proffered observations about the alleged shooter’s possible motivation as well as his mental state during a court appearance. Some went so far as to make specific diagnoses such as schizophrenia, an unspecified psychotic disorder, or psychopathy. All based their opinions solely upon information presented in the media, and only one – a psychologist – made a point of couching the opinion with the disclaimer that their information could be incomplete or simply wrong.
The most striking example I found was posted by a guest columnist for an online newspaper. This psychiatrist stated, “This man is mentally ill. I do not have information enough to be diagnosing, but clearly he has a psychotic disorder. No sane person behaves this way.”
While it may be tempting or flattering to be given the opportunity to be a media commentator, psychiatrists do have an ethical duty to restrict our public comments. According to Section 7.3 of the American Psychiatric Association's Principles of Medical Ethics:
“On occasion psychiatrists are asked for an opinion about an individual who is in the light of public attention or who has disclosed information about himself or herself through public media. In such circumstances, a psychiatrist may share with the public his or her expertise about psychiatric issues in general.
However, it is unethical for a psychiatrist to offer a professional opinion unless he or she has conducted an examination and has been granted proper authorization for such a statement.”
The requirement for a personal examination is particularly important when an opinion is derived solely from media sources whose information may be unreliable. In a recent court filing, the district attorney in the Colorado shooting case reportedly stated that the media was obtaining information from “hoaxers, fraudsters, or maybe from nobody at all.” Some of the early information that these professionals relied upon has now been found to be wrong, such as the suspect’s lack of previous contact with mental health care.
Ethical guidelines also require physicians to practice within their area of competence. Mental health professionals without experience or training specific to criminal behavior, violence and mental illness, and the legal assessment of competence or sanity may be practicing outside the scope of their training by offering opinions on these issues.
Not to be completely negative, there were good examples of psychiatric commentary. Dr. Keith Ablow, a member of the Fox News medical team, presented a detailed and careful overview of the sanity evaluation process and addressed a number of public misconceptions about the insanity defense.
The Goldwater rule was intended to protect celebrities, politicians and other high-profile figures from unwarranted invasion of privacy and damage to their reputations. I’m sure the authors of this clause didn’t anticipate the unintended effects such speculation could have on a criminal defendant, the alleged suspect’s family, or the victims of the offense. Public speculation about a criminal defendant has much more serious repercussions than a tarnished reputation.
Eventually, a jury will be empaneled to hear the case. Finding an unbiased juror will be difficult enough for a notorious offense, but may be impossible once the general public has been exposed to repeated statements by psychiatrists and psychologists about a defendant’s aberrant mental state. Even when couched in a disclaimer, jurors will remember the opinion rather than the disclaimer. If a death penalty is requested in this case, implications that a defendant has a serious mental illness could prejudice a sentencing hearing, since research has shown that a capital sentence is more likely to be given to mentally ill defendants.
Journalists will often ask mental health professionals about warning signals or red flags that may have been missed. When a psychiatrist publicly states that signs were missed, he implies that the suspect’s family, friends, and co-workers were somehow negligent for failing to prevent a tragedy. Public safety is not improved by blaming the suspect’s family. Susan Klebold, the mother of Columbine shooter Dylan Klebold, wrote a moving essay about her reaction to her son’s crime in her essay, “I Will Never Know Why”:
“Those of us who cared for Dylan felt responsible for his death. We thought, 'If I had been a better (mother, father, brother, friend, aunt, uncle, cousin), I would have known this was coming.’ We perceived his actions to be our failure. I tried to identify a pivotal event in his upbringing that could account for his anger. Had I been too strict? Not strict enough? Had I pushed too hard, or not hard enough? In the days before he died, I had hugged him and told him how much I loved him. I held his scratchy face between my palms and told him that he was a wonderful person and that I was proud of him. Had he felt pressured by this? Did he feel that he could not live up to my expectations?”
Similarly, survivors and family members of the victims can be traumatized by continued professional speculation. On our Shrink Rap blog, the mother of one Virginia Tech student thanked us for not discussing that crime. Here is how she described the effects on her son:
“The media coverage hurt as much as it helped. Many of those kids don’t want to talk about that day at all. It’s very hard for a young adult when the first thing they get asked about college is not “how do you like classes” or “what’s your major” but rather “Were you there, were you injured, did you know anyone who died?”
Finally, there is the risk of creating a copycat offender. Media attention has been a well-known cause of clustered suicides and can be a precipitant for other violent behavior. Almost on cue, Maryland police recently apprehended a man who threatened to “shoot up” his employer and referred to himself as “a joker.”
Considering all this, I’m grateful that I have consistently maintained one response to high-profile offenses: “No comment.”
—Annette Hanson, M.D.
DR. HANSON is a forensic psychiatrist and co-author of Shrink Rap: Three Psychiatrists Explain Their Work. The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson’s employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Health Care Integration
We’ve been hearing a lot about health care integration lately, particularly around integration of behavioral health care with physical health care. (This term behavioral health can have several meanings; it is most often used to refer to “mental health plus substance use” disorders, which is how I am using it here.)
Since before Descartes, we have disintegrated man and woman into head and torso; brain and body; mind and soul. Only in the past hundred years have we begun the discussion about bringing these parts together again; reintegrating the psyche and the soma; integrating behavioral health and physical health.
The state of Maryland began this process last year, as its Department of Health and Mental Hygiene initiated discussions about merging the “Health” with the “Hygiene.” (As if cleanliness would make the difference.) For the past several months, stakeholders interested in the rights and well-being of people with mental health and addiction problems have been meeting, sometimes several times per week, with state and Medicaid officials, insurance representatives, advocacy organizations, and clinicians, to hash out what the new integrated Medicaid should look like. MCOs, ASOs, MBHOs, and ACOs are spit out like bullets, depending on your position about which organizational model is best able to balance enrollees' health with the applicable cost.
The Maryland Mental Health Coalition, an association of behavioral health providers and advocacy organizations, has been organizing an impressive effort, orchestrated by Linda Raines, who is also executive director of the Maryland chapter of Mental Health America (MHA), to unite our disparate voices into one. They are all mostly in agreement except for two main areas: splitting populations into more and less severe subgroups and the timing of integration of physical health into behavioral health.
Some believe that the populations of people with behavioral health problems should be split into those who are less severe and only receiving care from a primary care physician (PCP) and those who are more severely ill and receiving help from specialty mental health providers. The more ill ones, often with severe and chronic mental illness, consume the most resources, both in time and in money. But they are only 10-15% of the entire population of people with any behavioral health problem. The other 85-90% would receive a seemingly less integrated form of care, called collaborative care, which recognizes the fact that the supply of mental health providers is not enough to meet the demand for the entire population.
Collaborative care, which has had somewhat positive to mixed results with respect to outcomes, uses psychiatrists, nurse practitioners, and other mental health providers to review a patient’s electronic health record and discuss the patient’s problems and needs in a collaborative format that provides clinical decision support to the primary care clinician who is primarily managing the care. This is often telephonic and web-based support, though some provide support that is co-located with the PCPs.
The other part of the discussion is the degree to which the behavioral health care should be carved out versus provided by the parent managed care organization. The American Psychiatric Association has a position statement opposing the concept of carve-outs. The paper suggests that:
“Mental health and substance abuse integration occurs when benefits and services for people with mental illness and substance abuse disorders are integrated, funded and administered no differently than for those people with other medical/surgical illnesses.”
The Maryland Psychiatric Society is also pushing on this point, suggesting that “financial rewards and penalties for the payor(s) should be integrated in such a manner that they are incentivized to coordinate services and prevent negative outcomes regardless of who is paying the bill. ” The Maryland chapter of MHA and most of the Coalition members feel that an Administrative Services Organization (ASO) model that uses a behavioral health home for people with severe illnesses, and a collaborative care model for the other 85%, will be the best balance. I liken this to how people like their band-aids torn off – with a sudden amount of pain that subsides quickly, or a drawn-out but consistent level of pain for a longer period of time. It’s a personal choice.
Ask the people who have both a medical problem as well as a behavioral health problem. People with both mental health and addiction illnesses in Maryland Medicaid are 8-15 times more likely to be medically hospitalized for problems like diabetes, epilepsy, infections, and heart failure, than those who do not have a behavioral health condition [See chart below]. Wow! That disparity is impressive.
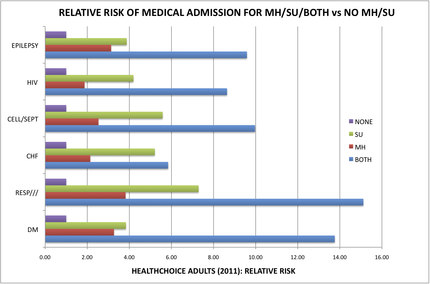
What model will best reduce this disparity the quickest?
Of course, I am a member of MPS and have a bias in my view of this situation (reader beware). But the entire behavioral health advocacy community is coming together to recommend what it thinks is the best financial and administrative framework within which to provide the greatest good. We need to decide, by the end of September, which infrastructure model to use in order to provide more “integrated” health care.
Will it apply equally, regardless of illness severity?
Will it incorporate both somatic health and behavioral health, connecting the brain and the body again? Or will it keep them separate but equal?
Keep track at http://bit.ly/Ouptue.
The data provided by the Maryland’s Integration Data Work Group [The chart is based on this data] clearly and profoundly demonstrate this disparity in chronic medical problems among the 200,000 or so HealthChoice enrollees. People identified as having a mental health illness are medically admitted 2 to 4 times more often for diabetes, heart failure, infections, epilepsy, and pulmonary disease than are people without any behavioral health condition. People identified as having a substance use disorder are medically admitted 4 to 7 times more often than people without any behavioral health condition. And, for people who have both mental health and substance use illness, these people are admitted 8- to 15-times more often than those without.
We estimated the cost for hospitalization for these six medical categories alone, and only for the 19-64 year old age group that we analyzed, to be about $86 million in excess costs over and above what would be expected for people without a behavioral health illness. A full analysis of this data would likely demonstrate more than $150 million in excess costs, much of which is avoidable with improved outpatient care.
The MPS believes that a model that is most likely to adopt a culture of integration is also the one that will most likely reduce these avoidable costs and improve the health care of this population. It is clear that some of the proposed models are more or less likely to deliver a culture of integration and innovation. The Maryland Psychiatric Society believes that Maryland should ensure that the chosen model is hard-wired to contain the following features:
1. Financial rewards and penalties for the payor(s) should be integrated in such a manner that they are incentivized to coordinate services and prevent negative outcomes regardless of who is paying the bill. If the ASO denies a service and this results in an $80,000 bill to the MCO for hospitalization after a suicide attempt, the ASO should be at risk for part of this bill. Similarly, if the MBHO provides case management services that results in improved diabetes care management that leads to reduced hospitalization costs for the MCO, the MBHO should share in those savings. There should be no opportunities for one payor to point to the other payor and say “not me.”
2. Financial rewards and penalties for the clinicians should be integrated such that they are incentivized to pay attention to both somatic and behavioral health (BH) needs. This may include case management services that help behavioral health clinicians coordinate with somatic clinicians and services, as well as collaborative BH services that coordinate with PCPs.
3. Minimize administrative overhead such that the maximum proportion of expenditures are spent on direct care and coordination of services.
4. The spirit and letter of the Mental Health Parity and Addictions Equity Act should be proactively maintained. (There is a risk that a State-run ASO would be able to skirt the United States’s federal Mental Health Parity law, thus being able to provide less costly care to those with behavioral health problems than those with traditional MCO coverage. The Mental Health Parity law applies to Managed Care Organizations, not to states.) The payor must “provide a detailed analysis demonstrating that their utilization management protocols do not have more restrictive nonquantitative treatment limitations compared to those used on the somatic side. The term “protocol” includes “…any processes, strategies, evidentiary standards, or other factors used in applying the nonquantitative treatment limitation to mental health or substance use disorder benefits.”
5. If the organization delegates any of its responsibilities to another contracted organization, it must “specify that the contractor shall comply with, and maintain parity between the MH/SUD benefits it administers and the organization's medical/surgical benefits pursuant to the applicable federal and/or state law or regulation and any binding regulatory or subregulatory guidance related thereto.”
6. Descriptions of the processes that the organization uses to ensure compliance with regulatory health care parity requirements, including regulations pertaining to mental health and/or substance usage disorders (MHPAEA), including:
a. Periodic internal monitoring and auditing of compliance;
b. Periodic review and analysis to determine if there are any changes in its benefits, policies and procedures, and utilization management protocols that impact compliance.
c. Periodic communication to delegated contractors regarding changes impacting compliance, including parity of health care services such as mental health and/or substance use disorder parity (MHPAEA).
7. A comprehensive list of services and procedures that support integrated and comprehensive recovery models must be available to clinicians and consumers.
8. Integration must include all levels and aspects of care – emergency departments; all inpatient hospital care; partial hospitalization; nursing homes; assisted living facilities; group homes, residential programs; day programs; outpatient care; diversion programs; pharmacy, including all medications; and all types of care including mental health, somatic and addiction care.
9. Either require coordination of clinical information via the state-designated HIE or provision of a shared electronic health record service for all integrated care, with appropriate provisions to protect patient privacy.
10. Financial, administrative, and clinical data collection systems must be integrated to permit analysis of expenditures associated with patient outcomes.
11. Consumers should be allowed to receive services from any willing clinician.
12. The comprehensive list of services that patients may receive must be developed using a recovery-based model and covered under the integration of services.
13. Data transparency for all stakeholders is critical for trust and success.
14. An oversight group of stakeholders will monthly review integrated data from all payor sources (MCO, ASO, MBHO, etc) and service utilization sources (ADT, Pharmacy, etc) for the purposes of ongoing review and ensuring coordination of care.
15. Spreadsheets must be developed that permit ongoing ability for stakeholders to view levels of care being provided and denied, as well as their outcomes, for all patient subpopulations at the granular level.
16. Standards should be developed for network provider directories that ensure accurate and up-to-date contact information as well as the ability to indicate if a provider is able to accept new outpatients in a timely manner.
An interesting approach that could merge these ideas is to develop an MCO that is led by people with expertise in managing the health of people with behavioral health conditions. This would be a pretty new animal, one that is savvy to the needs of both behavioral health and primary care and that can effectively incentivize health system behaviors that improve overall health while reducing total costs.
There could also be a role for Maryland’s two large medical systems, University of Maryland and Johns Hopkins, to work together in running such a hybrid animal. With the goal of getting this up and running by 2014, time may be the most limiting factor here, potentially resulting in us going down more familiar, if less effective, pathways.
What is going on in your state? Is there a challenge to integrate care? Which populations? Is somatic care included? Let us know what is going on in your state.
—Steven Roy Daviss, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog.
We’ve been hearing a lot about health care integration lately, particularly around integration of behavioral health care with physical health care. (This term behavioral health can have several meanings; it is most often used to refer to “mental health plus substance use” disorders, which is how I am using it here.)
Since before Descartes, we have disintegrated man and woman into head and torso; brain and body; mind and soul. Only in the past hundred years have we begun the discussion about bringing these parts together again; reintegrating the psyche and the soma; integrating behavioral health and physical health.
The state of Maryland began this process last year, as its Department of Health and Mental Hygiene initiated discussions about merging the “Health” with the “Hygiene.” (As if cleanliness would make the difference.) For the past several months, stakeholders interested in the rights and well-being of people with mental health and addiction problems have been meeting, sometimes several times per week, with state and Medicaid officials, insurance representatives, advocacy organizations, and clinicians, to hash out what the new integrated Medicaid should look like. MCOs, ASOs, MBHOs, and ACOs are spit out like bullets, depending on your position about which organizational model is best able to balance enrollees' health with the applicable cost.
The Maryland Mental Health Coalition, an association of behavioral health providers and advocacy organizations, has been organizing an impressive effort, orchestrated by Linda Raines, who is also executive director of the Maryland chapter of Mental Health America (MHA), to unite our disparate voices into one. They are all mostly in agreement except for two main areas: splitting populations into more and less severe subgroups and the timing of integration of physical health into behavioral health.
Some believe that the populations of people with behavioral health problems should be split into those who are less severe and only receiving care from a primary care physician (PCP) and those who are more severely ill and receiving help from specialty mental health providers. The more ill ones, often with severe and chronic mental illness, consume the most resources, both in time and in money. But they are only 10-15% of the entire population of people with any behavioral health problem. The other 85-90% would receive a seemingly less integrated form of care, called collaborative care, which recognizes the fact that the supply of mental health providers is not enough to meet the demand for the entire population.
Collaborative care, which has had somewhat positive to mixed results with respect to outcomes, uses psychiatrists, nurse practitioners, and other mental health providers to review a patient’s electronic health record and discuss the patient’s problems and needs in a collaborative format that provides clinical decision support to the primary care clinician who is primarily managing the care. This is often telephonic and web-based support, though some provide support that is co-located with the PCPs.
The other part of the discussion is the degree to which the behavioral health care should be carved out versus provided by the parent managed care organization. The American Psychiatric Association has a position statement opposing the concept of carve-outs. The paper suggests that:
“Mental health and substance abuse integration occurs when benefits and services for people with mental illness and substance abuse disorders are integrated, funded and administered no differently than for those people with other medical/surgical illnesses.”
The Maryland Psychiatric Society is also pushing on this point, suggesting that “financial rewards and penalties for the payor(s) should be integrated in such a manner that they are incentivized to coordinate services and prevent negative outcomes regardless of who is paying the bill. ” The Maryland chapter of MHA and most of the Coalition members feel that an Administrative Services Organization (ASO) model that uses a behavioral health home for people with severe illnesses, and a collaborative care model for the other 85%, will be the best balance. I liken this to how people like their band-aids torn off – with a sudden amount of pain that subsides quickly, or a drawn-out but consistent level of pain for a longer period of time. It’s a personal choice.
Ask the people who have both a medical problem as well as a behavioral health problem. People with both mental health and addiction illnesses in Maryland Medicaid are 8-15 times more likely to be medically hospitalized for problems like diabetes, epilepsy, infections, and heart failure, than those who do not have a behavioral health condition [See chart below]. Wow! That disparity is impressive.
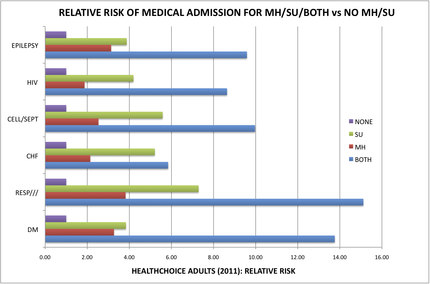
What model will best reduce this disparity the quickest?
Of course, I am a member of MPS and have a bias in my view of this situation (reader beware). But the entire behavioral health advocacy community is coming together to recommend what it thinks is the best financial and administrative framework within which to provide the greatest good. We need to decide, by the end of September, which infrastructure model to use in order to provide more “integrated” health care.
Will it apply equally, regardless of illness severity?
Will it incorporate both somatic health and behavioral health, connecting the brain and the body again? Or will it keep them separate but equal?
Keep track at http://bit.ly/Ouptue.
The data provided by the Maryland’s Integration Data Work Group [The chart is based on this data] clearly and profoundly demonstrate this disparity in chronic medical problems among the 200,000 or so HealthChoice enrollees. People identified as having a mental health illness are medically admitted 2 to 4 times more often for diabetes, heart failure, infections, epilepsy, and pulmonary disease than are people without any behavioral health condition. People identified as having a substance use disorder are medically admitted 4 to 7 times more often than people without any behavioral health condition. And, for people who have both mental health and substance use illness, these people are admitted 8- to 15-times more often than those without.
We estimated the cost for hospitalization for these six medical categories alone, and only for the 19-64 year old age group that we analyzed, to be about $86 million in excess costs over and above what would be expected for people without a behavioral health illness. A full analysis of this data would likely demonstrate more than $150 million in excess costs, much of which is avoidable with improved outpatient care.
The MPS believes that a model that is most likely to adopt a culture of integration is also the one that will most likely reduce these avoidable costs and improve the health care of this population. It is clear that some of the proposed models are more or less likely to deliver a culture of integration and innovation. The Maryland Psychiatric Society believes that Maryland should ensure that the chosen model is hard-wired to contain the following features:
1. Financial rewards and penalties for the payor(s) should be integrated in such a manner that they are incentivized to coordinate services and prevent negative outcomes regardless of who is paying the bill. If the ASO denies a service and this results in an $80,000 bill to the MCO for hospitalization after a suicide attempt, the ASO should be at risk for part of this bill. Similarly, if the MBHO provides case management services that results in improved diabetes care management that leads to reduced hospitalization costs for the MCO, the MBHO should share in those savings. There should be no opportunities for one payor to point to the other payor and say “not me.”
2. Financial rewards and penalties for the clinicians should be integrated such that they are incentivized to pay attention to both somatic and behavioral health (BH) needs. This may include case management services that help behavioral health clinicians coordinate with somatic clinicians and services, as well as collaborative BH services that coordinate with PCPs.
3. Minimize administrative overhead such that the maximum proportion of expenditures are spent on direct care and coordination of services.
4. The spirit and letter of the Mental Health Parity and Addictions Equity Act should be proactively maintained. (There is a risk that a State-run ASO would be able to skirt the United States’s federal Mental Health Parity law, thus being able to provide less costly care to those with behavioral health problems than those with traditional MCO coverage. The Mental Health Parity law applies to Managed Care Organizations, not to states.) The payor must “provide a detailed analysis demonstrating that their utilization management protocols do not have more restrictive nonquantitative treatment limitations compared to those used on the somatic side. The term “protocol” includes “…any processes, strategies, evidentiary standards, or other factors used in applying the nonquantitative treatment limitation to mental health or substance use disorder benefits.”
5. If the organization delegates any of its responsibilities to another contracted organization, it must “specify that the contractor shall comply with, and maintain parity between the MH/SUD benefits it administers and the organization's medical/surgical benefits pursuant to the applicable federal and/or state law or regulation and any binding regulatory or subregulatory guidance related thereto.”
6. Descriptions of the processes that the organization uses to ensure compliance with regulatory health care parity requirements, including regulations pertaining to mental health and/or substance usage disorders (MHPAEA), including:
a. Periodic internal monitoring and auditing of compliance;
b. Periodic review and analysis to determine if there are any changes in its benefits, policies and procedures, and utilization management protocols that impact compliance.
c. Periodic communication to delegated contractors regarding changes impacting compliance, including parity of health care services such as mental health and/or substance use disorder parity (MHPAEA).
7. A comprehensive list of services and procedures that support integrated and comprehensive recovery models must be available to clinicians and consumers.
8. Integration must include all levels and aspects of care – emergency departments; all inpatient hospital care; partial hospitalization; nursing homes; assisted living facilities; group homes, residential programs; day programs; outpatient care; diversion programs; pharmacy, including all medications; and all types of care including mental health, somatic and addiction care.
9. Either require coordination of clinical information via the state-designated HIE or provision of a shared electronic health record service for all integrated care, with appropriate provisions to protect patient privacy.
10. Financial, administrative, and clinical data collection systems must be integrated to permit analysis of expenditures associated with patient outcomes.
11. Consumers should be allowed to receive services from any willing clinician.
12. The comprehensive list of services that patients may receive must be developed using a recovery-based model and covered under the integration of services.
13. Data transparency for all stakeholders is critical for trust and success.
14. An oversight group of stakeholders will monthly review integrated data from all payor sources (MCO, ASO, MBHO, etc) and service utilization sources (ADT, Pharmacy, etc) for the purposes of ongoing review and ensuring coordination of care.
15. Spreadsheets must be developed that permit ongoing ability for stakeholders to view levels of care being provided and denied, as well as their outcomes, for all patient subpopulations at the granular level.
16. Standards should be developed for network provider directories that ensure accurate and up-to-date contact information as well as the ability to indicate if a provider is able to accept new outpatients in a timely manner.
An interesting approach that could merge these ideas is to develop an MCO that is led by people with expertise in managing the health of people with behavioral health conditions. This would be a pretty new animal, one that is savvy to the needs of both behavioral health and primary care and that can effectively incentivize health system behaviors that improve overall health while reducing total costs.
There could also be a role for Maryland’s two large medical systems, University of Maryland and Johns Hopkins, to work together in running such a hybrid animal. With the goal of getting this up and running by 2014, time may be the most limiting factor here, potentially resulting in us going down more familiar, if less effective, pathways.
What is going on in your state? Is there a challenge to integrate care? Which populations? Is somatic care included? Let us know what is going on in your state.
—Steven Roy Daviss, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog.
We’ve been hearing a lot about health care integration lately, particularly around integration of behavioral health care with physical health care. (This term behavioral health can have several meanings; it is most often used to refer to “mental health plus substance use” disorders, which is how I am using it here.)
Since before Descartes, we have disintegrated man and woman into head and torso; brain and body; mind and soul. Only in the past hundred years have we begun the discussion about bringing these parts together again; reintegrating the psyche and the soma; integrating behavioral health and physical health.
The state of Maryland began this process last year, as its Department of Health and Mental Hygiene initiated discussions about merging the “Health” with the “Hygiene.” (As if cleanliness would make the difference.) For the past several months, stakeholders interested in the rights and well-being of people with mental health and addiction problems have been meeting, sometimes several times per week, with state and Medicaid officials, insurance representatives, advocacy organizations, and clinicians, to hash out what the new integrated Medicaid should look like. MCOs, ASOs, MBHOs, and ACOs are spit out like bullets, depending on your position about which organizational model is best able to balance enrollees' health with the applicable cost.
The Maryland Mental Health Coalition, an association of behavioral health providers and advocacy organizations, has been organizing an impressive effort, orchestrated by Linda Raines, who is also executive director of the Maryland chapter of Mental Health America (MHA), to unite our disparate voices into one. They are all mostly in agreement except for two main areas: splitting populations into more and less severe subgroups and the timing of integration of physical health into behavioral health.
Some believe that the populations of people with behavioral health problems should be split into those who are less severe and only receiving care from a primary care physician (PCP) and those who are more severely ill and receiving help from specialty mental health providers. The more ill ones, often with severe and chronic mental illness, consume the most resources, both in time and in money. But they are only 10-15% of the entire population of people with any behavioral health problem. The other 85-90% would receive a seemingly less integrated form of care, called collaborative care, which recognizes the fact that the supply of mental health providers is not enough to meet the demand for the entire population.
Collaborative care, which has had somewhat positive to mixed results with respect to outcomes, uses psychiatrists, nurse practitioners, and other mental health providers to review a patient’s electronic health record and discuss the patient’s problems and needs in a collaborative format that provides clinical decision support to the primary care clinician who is primarily managing the care. This is often telephonic and web-based support, though some provide support that is co-located with the PCPs.
The other part of the discussion is the degree to which the behavioral health care should be carved out versus provided by the parent managed care organization. The American Psychiatric Association has a position statement opposing the concept of carve-outs. The paper suggests that:
“Mental health and substance abuse integration occurs when benefits and services for people with mental illness and substance abuse disorders are integrated, funded and administered no differently than for those people with other medical/surgical illnesses.”
The Maryland Psychiatric Society is also pushing on this point, suggesting that “financial rewards and penalties for the payor(s) should be integrated in such a manner that they are incentivized to coordinate services and prevent negative outcomes regardless of who is paying the bill. ” The Maryland chapter of MHA and most of the Coalition members feel that an Administrative Services Organization (ASO) model that uses a behavioral health home for people with severe illnesses, and a collaborative care model for the other 85%, will be the best balance. I liken this to how people like their band-aids torn off – with a sudden amount of pain that subsides quickly, or a drawn-out but consistent level of pain for a longer period of time. It’s a personal choice.
Ask the people who have both a medical problem as well as a behavioral health problem. People with both mental health and addiction illnesses in Maryland Medicaid are 8-15 times more likely to be medically hospitalized for problems like diabetes, epilepsy, infections, and heart failure, than those who do not have a behavioral health condition [See chart below]. Wow! That disparity is impressive.
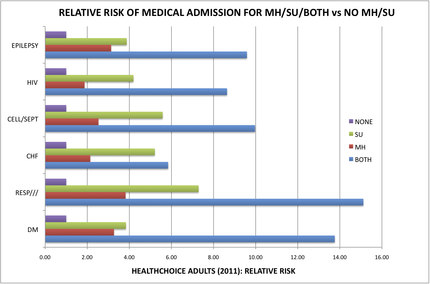
What model will best reduce this disparity the quickest?
Of course, I am a member of MPS and have a bias in my view of this situation (reader beware). But the entire behavioral health advocacy community is coming together to recommend what it thinks is the best financial and administrative framework within which to provide the greatest good. We need to decide, by the end of September, which infrastructure model to use in order to provide more “integrated” health care.
Will it apply equally, regardless of illness severity?
Will it incorporate both somatic health and behavioral health, connecting the brain and the body again? Or will it keep them separate but equal?
Keep track at http://bit.ly/Ouptue.
The data provided by the Maryland’s Integration Data Work Group [The chart is based on this data] clearly and profoundly demonstrate this disparity in chronic medical problems among the 200,000 or so HealthChoice enrollees. People identified as having a mental health illness are medically admitted 2 to 4 times more often for diabetes, heart failure, infections, epilepsy, and pulmonary disease than are people without any behavioral health condition. People identified as having a substance use disorder are medically admitted 4 to 7 times more often than people without any behavioral health condition. And, for people who have both mental health and substance use illness, these people are admitted 8- to 15-times more often than those without.
We estimated the cost for hospitalization for these six medical categories alone, and only for the 19-64 year old age group that we analyzed, to be about $86 million in excess costs over and above what would be expected for people without a behavioral health illness. A full analysis of this data would likely demonstrate more than $150 million in excess costs, much of which is avoidable with improved outpatient care.
The MPS believes that a model that is most likely to adopt a culture of integration is also the one that will most likely reduce these avoidable costs and improve the health care of this population. It is clear that some of the proposed models are more or less likely to deliver a culture of integration and innovation. The Maryland Psychiatric Society believes that Maryland should ensure that the chosen model is hard-wired to contain the following features:
1. Financial rewards and penalties for the payor(s) should be integrated in such a manner that they are incentivized to coordinate services and prevent negative outcomes regardless of who is paying the bill. If the ASO denies a service and this results in an $80,000 bill to the MCO for hospitalization after a suicide attempt, the ASO should be at risk for part of this bill. Similarly, if the MBHO provides case management services that results in improved diabetes care management that leads to reduced hospitalization costs for the MCO, the MBHO should share in those savings. There should be no opportunities for one payor to point to the other payor and say “not me.”
2. Financial rewards and penalties for the clinicians should be integrated such that they are incentivized to pay attention to both somatic and behavioral health (BH) needs. This may include case management services that help behavioral health clinicians coordinate with somatic clinicians and services, as well as collaborative BH services that coordinate with PCPs.
3. Minimize administrative overhead such that the maximum proportion of expenditures are spent on direct care and coordination of services.
4. The spirit and letter of the Mental Health Parity and Addictions Equity Act should be proactively maintained. (There is a risk that a State-run ASO would be able to skirt the United States’s federal Mental Health Parity law, thus being able to provide less costly care to those with behavioral health problems than those with traditional MCO coverage. The Mental Health Parity law applies to Managed Care Organizations, not to states.) The payor must “provide a detailed analysis demonstrating that their utilization management protocols do not have more restrictive nonquantitative treatment limitations compared to those used on the somatic side. The term “protocol” includes “…any processes, strategies, evidentiary standards, or other factors used in applying the nonquantitative treatment limitation to mental health or substance use disorder benefits.”
5. If the organization delegates any of its responsibilities to another contracted organization, it must “specify that the contractor shall comply with, and maintain parity between the MH/SUD benefits it administers and the organization's medical/surgical benefits pursuant to the applicable federal and/or state law or regulation and any binding regulatory or subregulatory guidance related thereto.”
6. Descriptions of the processes that the organization uses to ensure compliance with regulatory health care parity requirements, including regulations pertaining to mental health and/or substance usage disorders (MHPAEA), including:
a. Periodic internal monitoring and auditing of compliance;
b. Periodic review and analysis to determine if there are any changes in its benefits, policies and procedures, and utilization management protocols that impact compliance.
c. Periodic communication to delegated contractors regarding changes impacting compliance, including parity of health care services such as mental health and/or substance use disorder parity (MHPAEA).
7. A comprehensive list of services and procedures that support integrated and comprehensive recovery models must be available to clinicians and consumers.
8. Integration must include all levels and aspects of care – emergency departments; all inpatient hospital care; partial hospitalization; nursing homes; assisted living facilities; group homes, residential programs; day programs; outpatient care; diversion programs; pharmacy, including all medications; and all types of care including mental health, somatic and addiction care.
9. Either require coordination of clinical information via the state-designated HIE or provision of a shared electronic health record service for all integrated care, with appropriate provisions to protect patient privacy.
10. Financial, administrative, and clinical data collection systems must be integrated to permit analysis of expenditures associated with patient outcomes.
11. Consumers should be allowed to receive services from any willing clinician.
12. The comprehensive list of services that patients may receive must be developed using a recovery-based model and covered under the integration of services.
13. Data transparency for all stakeholders is critical for trust and success.
14. An oversight group of stakeholders will monthly review integrated data from all payor sources (MCO, ASO, MBHO, etc) and service utilization sources (ADT, Pharmacy, etc) for the purposes of ongoing review and ensuring coordination of care.
15. Spreadsheets must be developed that permit ongoing ability for stakeholders to view levels of care being provided and denied, as well as their outcomes, for all patient subpopulations at the granular level.
16. Standards should be developed for network provider directories that ensure accurate and up-to-date contact information as well as the ability to indicate if a provider is able to accept new outpatients in a timely manner.
An interesting approach that could merge these ideas is to develop an MCO that is led by people with expertise in managing the health of people with behavioral health conditions. This would be a pretty new animal, one that is savvy to the needs of both behavioral health and primary care and that can effectively incentivize health system behaviors that improve overall health while reducing total costs.
There could also be a role for Maryland’s two large medical systems, University of Maryland and Johns Hopkins, to work together in running such a hybrid animal. With the goal of getting this up and running by 2014, time may be the most limiting factor here, potentially resulting in us going down more familiar, if less effective, pathways.
What is going on in your state? Is there a challenge to integrate care? Which populations? Is somatic care included? Let us know what is going on in your state.
—Steven Roy Daviss, M.D., DFAPA
DR. DAVISS is chair of the department of psychiatry at the University of Maryland’s Baltimore Washington Medical Center, policy wonk for the Maryland Psychiatric Society, chair of the APA Committee on Electronic Health Records, and co-author of Shrink Rap: Three Psychiatrists Explain Their Work, published by Johns Hopkins University Press. In addition to @HITshrink on Twitter, he can be found on the Shrink Rap blog.
Home Inspection--A Novel About Psychotherapy and the Search for Love
Dinah Miller’s novel Home Inspection, is now available on Amazon. For the moment, it is available as an e-novel, and for 4 days only, starting on Sunday, July 22, it will be available as a free download, before it resumes the regular selling price of $3.99. A paperback edition will be available later this month. The link to the book is here.
If you don't own a own a Kindle, you can install a free Kindle app on your computer, tablet, or cell phone by going here, and then you can download any Amazon e-book.
Dinah Miller’s novel Home Inspection, is now available on Amazon. For the moment, it is available as an e-novel, and for 4 days only, starting on Sunday, July 22, it will be available as a free download, before it resumes the regular selling price of $3.99. A paperback edition will be available later this month. The link to the book is here.
If you don't own a own a Kindle, you can install a free Kindle app on your computer, tablet, or cell phone by going here, and then you can download any Amazon e-book.
Dinah Miller’s novel Home Inspection, is now available on Amazon. For the moment, it is available as an e-novel, and for 4 days only, starting on Sunday, July 22, it will be available as a free download, before it resumes the regular selling price of $3.99. A paperback edition will be available later this month. The link to the book is here.
If you don't own a own a Kindle, you can install a free Kindle app on your computer, tablet, or cell phone by going here, and then you can download any Amazon e-book.