User login
New Questions on Lung Cancer Screening
By PATRICE WENDLING
Elsevier Global Medical News
Would you allow patients to self-refer for a CT lung cancer screening? Would you screen a never-smoker? What size nodule would trigger a follow-up exam? What is your lower age limit and lower pack-year limit for screening? These are just a few of the questions that were tackled during an interactive lung cancer screening session at the recent Radiological Society of North America meeting, and that highlight the uncharted waters physicians face in the wake of the pivotal National Lung Screening Trial.
The NLST demonstrated a 20% reduction in lung cancer mortality when low-dose CT screening was used, compared with chest x-ray, among 53,000 asymptomatic current or former heavy smokers. However, CT produced more than three times the number of positive results and a higher false-positive rate than radiography.
Without a clear plan to manage abnormal findings or a firm handle on cost, policy makers and payers are hesitant to back reimbursement for widespread lung cancer screening. Results of the ongoing NLST cost-effectiveness analysis are expected early next year. Based on already published data, however, a crude back-of-the-envelope estimate puts the incremental cost-effectiveness ratio at $38,000 per life-year gained, NLST investigator Dr. William Black told attendees.
"That actually is a pretty good deal compared to a lot of things we do in medicine, and in fact most people would put the threshold for acceptability somewhere between $50,000 to $100,000 per life-year gained," he said. "So it certainly is feasible"
Dr. Black pointed out that low-dose CT saved 1 lung cancer death per 346 persons screened in NLST, which again is very favorable, compared with the rate of 1 per 2,000 patients for mammography.
Although the session provided just a small snapshot in time, audience responses suggested there is much work ahead. A full 77% of attendees were not using low-dose CT to screen for lung cancer, and 72% reported not being familiar with the recently published National Comprehensive Cancer Network guidelines for lung cancer screening. One-quarter of the audience had no lower age limit for screening, and 34% said they neither provide decision support nor obtained informed consent.
Radiologist and NLST collaborator Dr. Caroline Chiles said that informed consent in NLST helped prepare patients for the potential risks of a screen, for the likelihood of a positive result, and for the fact that a positive result didn’t mean they had lung cancer. "It made a huge difference once they got that letter saying they had a positive screen, because at that point you don’t want everyone rushing out to a surgeon to get that nodule resected," she added.
What attendees and panelists could agree on was the need for smoking cessation to be included in any future lung cancer CT screening program, with 60% of attendees saying they already do so.
Dr. Chiles pointed out that 16.6% of participants in the NELSON lung screening trial quit smoking, compared with 3%-7% in the general public, but that participants were less likely to stay nonsmokers. She also cited a recent MMWR article that said 70% of adult smokers want to quit smoking, but only about half had been advised by a health professional to quit.
"We really have to think of lung cancer screening as being a teachable moment," she said. She suggested that physicians visit www.smokefree.gov for help in guiding their patients. Dr. Black also noted the NLST team is working on a screening fact sheet for physicians and patients that will be made available on the Internet.☐
By PATRICE WENDLING
Elsevier Global Medical News
Would you allow patients to self-refer for a CT lung cancer screening? Would you screen a never-smoker? What size nodule would trigger a follow-up exam? What is your lower age limit and lower pack-year limit for screening? These are just a few of the questions that were tackled during an interactive lung cancer screening session at the recent Radiological Society of North America meeting, and that highlight the uncharted waters physicians face in the wake of the pivotal National Lung Screening Trial.
The NLST demonstrated a 20% reduction in lung cancer mortality when low-dose CT screening was used, compared with chest x-ray, among 53,000 asymptomatic current or former heavy smokers. However, CT produced more than three times the number of positive results and a higher false-positive rate than radiography.
Without a clear plan to manage abnormal findings or a firm handle on cost, policy makers and payers are hesitant to back reimbursement for widespread lung cancer screening. Results of the ongoing NLST cost-effectiveness analysis are expected early next year. Based on already published data, however, a crude back-of-the-envelope estimate puts the incremental cost-effectiveness ratio at $38,000 per life-year gained, NLST investigator Dr. William Black told attendees.
"That actually is a pretty good deal compared to a lot of things we do in medicine, and in fact most people would put the threshold for acceptability somewhere between $50,000 to $100,000 per life-year gained," he said. "So it certainly is feasible"
Dr. Black pointed out that low-dose CT saved 1 lung cancer death per 346 persons screened in NLST, which again is very favorable, compared with the rate of 1 per 2,000 patients for mammography.
Although the session provided just a small snapshot in time, audience responses suggested there is much work ahead. A full 77% of attendees were not using low-dose CT to screen for lung cancer, and 72% reported not being familiar with the recently published National Comprehensive Cancer Network guidelines for lung cancer screening. One-quarter of the audience had no lower age limit for screening, and 34% said they neither provide decision support nor obtained informed consent.
Radiologist and NLST collaborator Dr. Caroline Chiles said that informed consent in NLST helped prepare patients for the potential risks of a screen, for the likelihood of a positive result, and for the fact that a positive result didn’t mean they had lung cancer. "It made a huge difference once they got that letter saying they had a positive screen, because at that point you don’t want everyone rushing out to a surgeon to get that nodule resected," she added.
What attendees and panelists could agree on was the need for smoking cessation to be included in any future lung cancer CT screening program, with 60% of attendees saying they already do so.
Dr. Chiles pointed out that 16.6% of participants in the NELSON lung screening trial quit smoking, compared with 3%-7% in the general public, but that participants were less likely to stay nonsmokers. She also cited a recent MMWR article that said 70% of adult smokers want to quit smoking, but only about half had been advised by a health professional to quit.
"We really have to think of lung cancer screening as being a teachable moment," she said. She suggested that physicians visit www.smokefree.gov for help in guiding their patients. Dr. Black also noted the NLST team is working on a screening fact sheet for physicians and patients that will be made available on the Internet.☐
By PATRICE WENDLING
Elsevier Global Medical News
Would you allow patients to self-refer for a CT lung cancer screening? Would you screen a never-smoker? What size nodule would trigger a follow-up exam? What is your lower age limit and lower pack-year limit for screening? These are just a few of the questions that were tackled during an interactive lung cancer screening session at the recent Radiological Society of North America meeting, and that highlight the uncharted waters physicians face in the wake of the pivotal National Lung Screening Trial.
The NLST demonstrated a 20% reduction in lung cancer mortality when low-dose CT screening was used, compared with chest x-ray, among 53,000 asymptomatic current or former heavy smokers. However, CT produced more than three times the number of positive results and a higher false-positive rate than radiography.
Without a clear plan to manage abnormal findings or a firm handle on cost, policy makers and payers are hesitant to back reimbursement for widespread lung cancer screening. Results of the ongoing NLST cost-effectiveness analysis are expected early next year. Based on already published data, however, a crude back-of-the-envelope estimate puts the incremental cost-effectiveness ratio at $38,000 per life-year gained, NLST investigator Dr. William Black told attendees.
"That actually is a pretty good deal compared to a lot of things we do in medicine, and in fact most people would put the threshold for acceptability somewhere between $50,000 to $100,000 per life-year gained," he said. "So it certainly is feasible"
Dr. Black pointed out that low-dose CT saved 1 lung cancer death per 346 persons screened in NLST, which again is very favorable, compared with the rate of 1 per 2,000 patients for mammography.
Although the session provided just a small snapshot in time, audience responses suggested there is much work ahead. A full 77% of attendees were not using low-dose CT to screen for lung cancer, and 72% reported not being familiar with the recently published National Comprehensive Cancer Network guidelines for lung cancer screening. One-quarter of the audience had no lower age limit for screening, and 34% said they neither provide decision support nor obtained informed consent.
Radiologist and NLST collaborator Dr. Caroline Chiles said that informed consent in NLST helped prepare patients for the potential risks of a screen, for the likelihood of a positive result, and for the fact that a positive result didn’t mean they had lung cancer. "It made a huge difference once they got that letter saying they had a positive screen, because at that point you don’t want everyone rushing out to a surgeon to get that nodule resected," she added.
What attendees and panelists could agree on was the need for smoking cessation to be included in any future lung cancer CT screening program, with 60% of attendees saying they already do so.
Dr. Chiles pointed out that 16.6% of participants in the NELSON lung screening trial quit smoking, compared with 3%-7% in the general public, but that participants were less likely to stay nonsmokers. She also cited a recent MMWR article that said 70% of adult smokers want to quit smoking, but only about half had been advised by a health professional to quit.
"We really have to think of lung cancer screening as being a teachable moment," she said. She suggested that physicians visit www.smokefree.gov for help in guiding their patients. Dr. Black also noted the NLST team is working on a screening fact sheet for physicians and patients that will be made available on the Internet.☐
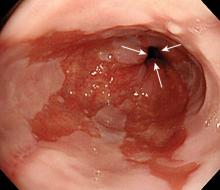
Follow-Up Ablation of Barrett's Didn't Aid Outcome
NATIONAL HARBOR, MD. – Patients with short-segment Barrett’s esophagus who had additional ablative therapies after endoscopic mucosal resection had no significant improvement in recurrence or mortality rates, compared with patients who did not have additional therapies.
The study of 213 patients was presented at the annual meeting of the American College of Gastroenterology. "Endoscopic mucosal resection and ablative therapies are now widely used to remove and ablate the Barrett’s mucosa," said Dr. Jianmin Tian of the Mayo Clinic in Rochester, Minn.
However, it is unclear whether additional ablative therapies after endoscopic mucosal resection (EMR) can improve outcomes for patients with short-segment Barrett’s esophagus (SSBE), defined as less than 3 cm.
To assess the value of additional ablation, Dr. Tian and colleagues conducted a retrospective cohort study of 213 adults with SSBE who were treated in a tertiary referral center. The study population included 93 patients who underwent EMR and 120 patients who underwent EMR plus additional ablative therapies.
The additional ablative therapies included radiofrequency ablation, photodynamic therapy, multipolar/bipolar electrocautery, cryotherapy, and argon plasma coagulation.
The recurrence rate was not significantly different in the EMR-only group, compared with the EMR-plus-ablation group (10% vs. 12%), after control for age, sex, Charlson comorbidity index, and specific condition (either intestinal metaplasia or dysplasia), Dr. Tian said. Similarly, the mortality rate was not significantly different between the two groups (15% vs. 18%, respectively).
The study included patients with SSBE and high-grade dysplasia or early esophageal cancer who had achieved complete remission of their dysplasia or intestinal metaplasia. Patients with a history of esophagectomy were excluded. Recurrence was defined as finding dysplasia or early esophageal cancer after two consecutive negative esophagogastroduodenoscopy exams with complete response.
The findings suggest that ablation of the gastroesophageal junction may not reduce recurrence, said Dr. Tian. The study was limited by its retrospective design and small size. But the study’s strengths include a relatively long follow-up period, the inclusion of two consecutive negative esophagogastroduodenoscopy exams, and systematic surveillance biopsies from the esophagus and the gastroesophageal junction, he noted.
Areas for further research include validating the findings in a randomized, controlled trial; data collection from patients with long-segment Barrett’s esophagus; and investigating the clinical significance of recurrence at the gastroesophageal junction, he said.
Dr. Tian reported no conflicts. ☐
NATIONAL HARBOR, MD. – Patients with short-segment Barrett’s esophagus who had additional ablative therapies after endoscopic mucosal resection had no significant improvement in recurrence or mortality rates, compared with patients who did not have additional therapies.
The study of 213 patients was presented at the annual meeting of the American College of Gastroenterology. "Endoscopic mucosal resection and ablative therapies are now widely used to remove and ablate the Barrett’s mucosa," said Dr. Jianmin Tian of the Mayo Clinic in Rochester, Minn.
However, it is unclear whether additional ablative therapies after endoscopic mucosal resection (EMR) can improve outcomes for patients with short-segment Barrett’s esophagus (SSBE), defined as less than 3 cm.
To assess the value of additional ablation, Dr. Tian and colleagues conducted a retrospective cohort study of 213 adults with SSBE who were treated in a tertiary referral center. The study population included 93 patients who underwent EMR and 120 patients who underwent EMR plus additional ablative therapies.
The additional ablative therapies included radiofrequency ablation, photodynamic therapy, multipolar/bipolar electrocautery, cryotherapy, and argon plasma coagulation.
The recurrence rate was not significantly different in the EMR-only group, compared with the EMR-plus-ablation group (10% vs. 12%), after control for age, sex, Charlson comorbidity index, and specific condition (either intestinal metaplasia or dysplasia), Dr. Tian said. Similarly, the mortality rate was not significantly different between the two groups (15% vs. 18%, respectively).
The study included patients with SSBE and high-grade dysplasia or early esophageal cancer who had achieved complete remission of their dysplasia or intestinal metaplasia. Patients with a history of esophagectomy were excluded. Recurrence was defined as finding dysplasia or early esophageal cancer after two consecutive negative esophagogastroduodenoscopy exams with complete response.
The findings suggest that ablation of the gastroesophageal junction may not reduce recurrence, said Dr. Tian. The study was limited by its retrospective design and small size. But the study’s strengths include a relatively long follow-up period, the inclusion of two consecutive negative esophagogastroduodenoscopy exams, and systematic surveillance biopsies from the esophagus and the gastroesophageal junction, he noted.
Areas for further research include validating the findings in a randomized, controlled trial; data collection from patients with long-segment Barrett’s esophagus; and investigating the clinical significance of recurrence at the gastroesophageal junction, he said.
Dr. Tian reported no conflicts. ☐
NATIONAL HARBOR, MD. – Patients with short-segment Barrett’s esophagus who had additional ablative therapies after endoscopic mucosal resection had no significant improvement in recurrence or mortality rates, compared with patients who did not have additional therapies.
The study of 213 patients was presented at the annual meeting of the American College of Gastroenterology. "Endoscopic mucosal resection and ablative therapies are now widely used to remove and ablate the Barrett’s mucosa," said Dr. Jianmin Tian of the Mayo Clinic in Rochester, Minn.
However, it is unclear whether additional ablative therapies after endoscopic mucosal resection (EMR) can improve outcomes for patients with short-segment Barrett’s esophagus (SSBE), defined as less than 3 cm.
To assess the value of additional ablation, Dr. Tian and colleagues conducted a retrospective cohort study of 213 adults with SSBE who were treated in a tertiary referral center. The study population included 93 patients who underwent EMR and 120 patients who underwent EMR plus additional ablative therapies.
The additional ablative therapies included radiofrequency ablation, photodynamic therapy, multipolar/bipolar electrocautery, cryotherapy, and argon plasma coagulation.
The recurrence rate was not significantly different in the EMR-only group, compared with the EMR-plus-ablation group (10% vs. 12%), after control for age, sex, Charlson comorbidity index, and specific condition (either intestinal metaplasia or dysplasia), Dr. Tian said. Similarly, the mortality rate was not significantly different between the two groups (15% vs. 18%, respectively).
The study included patients with SSBE and high-grade dysplasia or early esophageal cancer who had achieved complete remission of their dysplasia or intestinal metaplasia. Patients with a history of esophagectomy were excluded. Recurrence was defined as finding dysplasia or early esophageal cancer after two consecutive negative esophagogastroduodenoscopy exams with complete response.
The findings suggest that ablation of the gastroesophageal junction may not reduce recurrence, said Dr. Tian. The study was limited by its retrospective design and small size. But the study’s strengths include a relatively long follow-up period, the inclusion of two consecutive negative esophagogastroduodenoscopy exams, and systematic surveillance biopsies from the esophagus and the gastroesophageal junction, he noted.
Areas for further research include validating the findings in a randomized, controlled trial; data collection from patients with long-segment Barrett’s esophagus; and investigating the clinical significance of recurrence at the gastroesophageal junction, he said.
Dr. Tian reported no conflicts. ☐
Major Finding: Short-segment Barrett’s esophagus that was initially treated with EMR did not have a lower recurrence rate if the patient had additional ablative therapy, compared with EMR only with no additional ablative therapy (12% vs. 10%, respectively).
Data Source: Data from 213 adults with short-segment Barrett’s esophagus.
Disclosures: Dr. Tian had no financial conflicts to disclose. Several study coauthors disclosed financial relationships with companies including Olympus, Fujinon, and Barrx.
Follow-Up Ablation of Barrett's Didn't Aid Outcome
NATIONAL HARBOR, MD. – Patients with short-segment Barrett’s esophagus who had additional ablative therapies after endoscopic mucosal resection had no significant improvement in recurrence or mortality rates, compared with patients who did not have additional therapies.
The study of 213 patients was presented at the annual meeting of the American College of Gastroenterology. "Endoscopic mucosal resection and ablative therapies are now widely used to remove and ablate the Barrett’s mucosa," said Dr. Jianmin Tian of the Mayo Clinic in Rochester, Minn.
However, it is unclear whether additional ablative therapies after endoscopic mucosal resection (EMR) can improve outcomes for patients with short-segment Barrett’s esophagus (SSBE), defined as less than 3 cm.
To assess the value of additional ablation, Dr. Tian and colleagues conducted a retrospective cohort study of 213 adults with SSBE who were treated in a tertiary referral center. The study population included 93 patients who underwent EMR and 120 patients who underwent EMR plus additional ablative therapies.
The additional ablative therapies included radiofrequency ablation, photodynamic therapy, multipolar/bipolar electrocautery, cryotherapy, and argon plasma coagulation.
The recurrence rate was not significantly different in the EMR-only group, compared with the EMR-plus-ablation group (10% vs. 12%), after control for age, sex, Charlson comorbidity index, and specific condition (either intestinal metaplasia or dysplasia), Dr. Tian said. Similarly, the mortality rate was not significantly different between the two groups (15% vs. 18%, respectively).
The study included patients with SSBE and high-grade dysplasia or early esophageal cancer who had achieved complete remission of their dysplasia or intestinal metaplasia. Patients with a history of esophagectomy were excluded. Recurrence was defined as finding dysplasia or early esophageal cancer after two consecutive negative esophagogastroduodenoscopy exams with complete response.
The findings suggest that ablation of the gastroesophageal junction may not reduce recurrence, said Dr. Tian. The study was limited by its retrospective design and small size. But the study’s strengths include a relatively long follow-up period, the inclusion of two consecutive negative esophagogastroduodenoscopy exams, and systematic surveillance biopsies from the esophagus and the gastroesophageal junction, he noted.
Areas for further research include validating the findings in a randomized, controlled trial; data collection from patients with long-segment Barrett’s esophagus; and investigating the clinical significance of recurrence at the gastroesophageal junction, he said.
Dr. Tian reported no conflicts. ☐
NATIONAL HARBOR, MD. – Patients with short-segment Barrett’s esophagus who had additional ablative therapies after endoscopic mucosal resection had no significant improvement in recurrence or mortality rates, compared with patients who did not have additional therapies.
The study of 213 patients was presented at the annual meeting of the American College of Gastroenterology. "Endoscopic mucosal resection and ablative therapies are now widely used to remove and ablate the Barrett’s mucosa," said Dr. Jianmin Tian of the Mayo Clinic in Rochester, Minn.
However, it is unclear whether additional ablative therapies after endoscopic mucosal resection (EMR) can improve outcomes for patients with short-segment Barrett’s esophagus (SSBE), defined as less than 3 cm.
To assess the value of additional ablation, Dr. Tian and colleagues conducted a retrospective cohort study of 213 adults with SSBE who were treated in a tertiary referral center. The study population included 93 patients who underwent EMR and 120 patients who underwent EMR plus additional ablative therapies.
The additional ablative therapies included radiofrequency ablation, photodynamic therapy, multipolar/bipolar electrocautery, cryotherapy, and argon plasma coagulation.
The recurrence rate was not significantly different in the EMR-only group, compared with the EMR-plus-ablation group (10% vs. 12%), after control for age, sex, Charlson comorbidity index, and specific condition (either intestinal metaplasia or dysplasia), Dr. Tian said. Similarly, the mortality rate was not significantly different between the two groups (15% vs. 18%, respectively).
The study included patients with SSBE and high-grade dysplasia or early esophageal cancer who had achieved complete remission of their dysplasia or intestinal metaplasia. Patients with a history of esophagectomy were excluded. Recurrence was defined as finding dysplasia or early esophageal cancer after two consecutive negative esophagogastroduodenoscopy exams with complete response.
The findings suggest that ablation of the gastroesophageal junction may not reduce recurrence, said Dr. Tian. The study was limited by its retrospective design and small size. But the study’s strengths include a relatively long follow-up period, the inclusion of two consecutive negative esophagogastroduodenoscopy exams, and systematic surveillance biopsies from the esophagus and the gastroesophageal junction, he noted.
Areas for further research include validating the findings in a randomized, controlled trial; data collection from patients with long-segment Barrett’s esophagus; and investigating the clinical significance of recurrence at the gastroesophageal junction, he said.
Dr. Tian reported no conflicts. ☐
NATIONAL HARBOR, MD. – Patients with short-segment Barrett’s esophagus who had additional ablative therapies after endoscopic mucosal resection had no significant improvement in recurrence or mortality rates, compared with patients who did not have additional therapies.
The study of 213 patients was presented at the annual meeting of the American College of Gastroenterology. "Endoscopic mucosal resection and ablative therapies are now widely used to remove and ablate the Barrett’s mucosa," said Dr. Jianmin Tian of the Mayo Clinic in Rochester, Minn.
However, it is unclear whether additional ablative therapies after endoscopic mucosal resection (EMR) can improve outcomes for patients with short-segment Barrett’s esophagus (SSBE), defined as less than 3 cm.
To assess the value of additional ablation, Dr. Tian and colleagues conducted a retrospective cohort study of 213 adults with SSBE who were treated in a tertiary referral center. The study population included 93 patients who underwent EMR and 120 patients who underwent EMR plus additional ablative therapies.
The additional ablative therapies included radiofrequency ablation, photodynamic therapy, multipolar/bipolar electrocautery, cryotherapy, and argon plasma coagulation.
The recurrence rate was not significantly different in the EMR-only group, compared with the EMR-plus-ablation group (10% vs. 12%), after control for age, sex, Charlson comorbidity index, and specific condition (either intestinal metaplasia or dysplasia), Dr. Tian said. Similarly, the mortality rate was not significantly different between the two groups (15% vs. 18%, respectively).
The study included patients with SSBE and high-grade dysplasia or early esophageal cancer who had achieved complete remission of their dysplasia or intestinal metaplasia. Patients with a history of esophagectomy were excluded. Recurrence was defined as finding dysplasia or early esophageal cancer after two consecutive negative esophagogastroduodenoscopy exams with complete response.
The findings suggest that ablation of the gastroesophageal junction may not reduce recurrence, said Dr. Tian. The study was limited by its retrospective design and small size. But the study’s strengths include a relatively long follow-up period, the inclusion of two consecutive negative esophagogastroduodenoscopy exams, and systematic surveillance biopsies from the esophagus and the gastroesophageal junction, he noted.
Areas for further research include validating the findings in a randomized, controlled trial; data collection from patients with long-segment Barrett’s esophagus; and investigating the clinical significance of recurrence at the gastroesophageal junction, he said.
Dr. Tian reported no conflicts. ☐
Major Finding: Short-segment Barrett’s esophagus that was initially treated with EMR did not have a lower recurrence rate if the patient had additional ablative therapy, compared with EMR only with no additional ablative therapy (12% vs. 10%, respectively).
Data Source: Data from 213 adults with short-segment Barrett’s esophagus.
Disclosures: Dr. Tian had no financial conflicts to disclose. Several study coauthors disclosed financial relationships with companies including Olympus, Fujinon, and Barrx.
Noninvasive Scan Has Promise For Lung Cancer Genotyping
AMSTERDAM – An experimental combination of PET scanning and a positron-emitting form of erlotinib appeared to work as a noninvasive way of identifying patients with advanced non–small cell lung cancer tumors that have the right genotype to receive erlotinib therapy.
"[11C]erlotinib PET shows promise as a noninvasive, in vivo means of selecting patients who may benefit from thymidine kinase inhibitor therapy," Dr. Idris Bahce said, reporting on a pilot study of 10 patients. Erlotinib (Tarceva) is from the thymidine kinase inhibitor drug class.
In his study, uptake of 11C-labeled erlotinib was significantly linked to the patients’ having an activating mutation in their epidermal growth factor receptor (EGFR) gene, specifically an exon 19 deletion.
Patients positive for erlotinib uptake on the PET scan also showed a tendency for better clinical responses to a therapeutic erlotinib regimen, reported Dr. Bahce, a pulmonologist at VU University, Amsterdam, during the World Conference on Lung Cancer.
Until now, the only way to identify advanced non–small cell lung cancer (NSCLC) tumors that are candidates for treatment with a tyrosine kinase inhibitor has been to biopsy the tumor and run an in vitro genetic analysis on the tumor cells. That can be challenging in some patients, such as when the tumor is not easy to biopsy, a limited amount of tissue is available, or the tumor is genetically heterogeneous. To get a reliable result from biopsy and testing, at least 30% of the specimen must contain malignant cells, Dr. Bahce said at the conference, sponsored by the International Association for the Study of Lung Cancer.
"It is a very early study, but ... it’s important because personalized treatment [for cancer] has gone to the next level, where we use new agents and match them to the right patients by doing biopsies," commented Dr. Roy S. Herbst, chief of medical oncology at the Yale Cancer Center in New Haven. "The PET method also allows physicians to assess the volume of cancer carrying the EGFR mutation following treatment, a way to track treatment efficacy," said Dr. Herbst in an interview.
"Instead of getting tissue at one point in time, you can image more frequently. It’s a way to track the course of treatment noninvasively," and in real time, he said.
He also predicted that the [11C]erlotinib PET test will become commercialized, although currently Dr. Bahce’s studies do not have any commercial funding.
"This is a proof of concept study," commented Dr. Luis Paz-Ares, chief of medical oncology at University Hospital Virgin del Rocio in Seville, Spain. "We need to define the positive predictive value and the negative predictive value" of the test, he added. The long-term future of a test like this may also be limited because future testing will probably need to look at multiple biomarkers, Dr. Paz-Ares said.
The study enrolled five patients with advanced NSCLC who had exon 19 deletion EGFR mutations, and five advanced NSCLC patients with wild-type EGFR genes. Each patient underwent a pair of [11C]erlotinib PET scans, each preceded by a [15O]water PET scan to assess blood perfusion of the tumors. A 4-hour interval separated the two sets of scans.
The scan results showed that the volume of distribution of the tagged erlotinib in the patients with EGFR mutations ran about 50% higher than in the patients with wild-type tumors, a difference that was significant (P = .03). Clinically, two of the five wild-type patients had nonetheless received erlotinib treatment prior to testing, and neither patient responded, with both showing progressive disease.
Three of the five patients with an EGFR mutation began receiving erlotinib treatment after testing and responded. In one of these patients, the tumor remained in check for 13 months. In a second patient, the tumor began to progress after 17 months of no progression on treatment. In the third patient, the tumor began to progress again after about 4 weeks of no progression on erlotinib treatment, Dr. Bahce said. A fourth patient went on erlotinib treatment before testing, and did not respond and continued to have progressive disease.
The two patient subgroups showed no difference in blood perfusion into the tumors or in EGFR expression in cell membranes.
Dr. Bahce said he had no disclosures.☐
AMSTERDAM – An experimental combination of PET scanning and a positron-emitting form of erlotinib appeared to work as a noninvasive way of identifying patients with advanced non–small cell lung cancer tumors that have the right genotype to receive erlotinib therapy.
"[11C]erlotinib PET shows promise as a noninvasive, in vivo means of selecting patients who may benefit from thymidine kinase inhibitor therapy," Dr. Idris Bahce said, reporting on a pilot study of 10 patients. Erlotinib (Tarceva) is from the thymidine kinase inhibitor drug class.
In his study, uptake of 11C-labeled erlotinib was significantly linked to the patients’ having an activating mutation in their epidermal growth factor receptor (EGFR) gene, specifically an exon 19 deletion.
Patients positive for erlotinib uptake on the PET scan also showed a tendency for better clinical responses to a therapeutic erlotinib regimen, reported Dr. Bahce, a pulmonologist at VU University, Amsterdam, during the World Conference on Lung Cancer.
Until now, the only way to identify advanced non–small cell lung cancer (NSCLC) tumors that are candidates for treatment with a tyrosine kinase inhibitor has been to biopsy the tumor and run an in vitro genetic analysis on the tumor cells. That can be challenging in some patients, such as when the tumor is not easy to biopsy, a limited amount of tissue is available, or the tumor is genetically heterogeneous. To get a reliable result from biopsy and testing, at least 30% of the specimen must contain malignant cells, Dr. Bahce said at the conference, sponsored by the International Association for the Study of Lung Cancer.
"It is a very early study, but ... it’s important because personalized treatment [for cancer] has gone to the next level, where we use new agents and match them to the right patients by doing biopsies," commented Dr. Roy S. Herbst, chief of medical oncology at the Yale Cancer Center in New Haven. "The PET method also allows physicians to assess the volume of cancer carrying the EGFR mutation following treatment, a way to track treatment efficacy," said Dr. Herbst in an interview.
"Instead of getting tissue at one point in time, you can image more frequently. It’s a way to track the course of treatment noninvasively," and in real time, he said.
He also predicted that the [11C]erlotinib PET test will become commercialized, although currently Dr. Bahce’s studies do not have any commercial funding.
"This is a proof of concept study," commented Dr. Luis Paz-Ares, chief of medical oncology at University Hospital Virgin del Rocio in Seville, Spain. "We need to define the positive predictive value and the negative predictive value" of the test, he added. The long-term future of a test like this may also be limited because future testing will probably need to look at multiple biomarkers, Dr. Paz-Ares said.
The study enrolled five patients with advanced NSCLC who had exon 19 deletion EGFR mutations, and five advanced NSCLC patients with wild-type EGFR genes. Each patient underwent a pair of [11C]erlotinib PET scans, each preceded by a [15O]water PET scan to assess blood perfusion of the tumors. A 4-hour interval separated the two sets of scans.
The scan results showed that the volume of distribution of the tagged erlotinib in the patients with EGFR mutations ran about 50% higher than in the patients with wild-type tumors, a difference that was significant (P = .03). Clinically, two of the five wild-type patients had nonetheless received erlotinib treatment prior to testing, and neither patient responded, with both showing progressive disease.
Three of the five patients with an EGFR mutation began receiving erlotinib treatment after testing and responded. In one of these patients, the tumor remained in check for 13 months. In a second patient, the tumor began to progress after 17 months of no progression on treatment. In the third patient, the tumor began to progress again after about 4 weeks of no progression on erlotinib treatment, Dr. Bahce said. A fourth patient went on erlotinib treatment before testing, and did not respond and continued to have progressive disease.
The two patient subgroups showed no difference in blood perfusion into the tumors or in EGFR expression in cell membranes.
Dr. Bahce said he had no disclosures.☐
AMSTERDAM – An experimental combination of PET scanning and a positron-emitting form of erlotinib appeared to work as a noninvasive way of identifying patients with advanced non–small cell lung cancer tumors that have the right genotype to receive erlotinib therapy.
"[11C]erlotinib PET shows promise as a noninvasive, in vivo means of selecting patients who may benefit from thymidine kinase inhibitor therapy," Dr. Idris Bahce said, reporting on a pilot study of 10 patients. Erlotinib (Tarceva) is from the thymidine kinase inhibitor drug class.
In his study, uptake of 11C-labeled erlotinib was significantly linked to the patients’ having an activating mutation in their epidermal growth factor receptor (EGFR) gene, specifically an exon 19 deletion.
Patients positive for erlotinib uptake on the PET scan also showed a tendency for better clinical responses to a therapeutic erlotinib regimen, reported Dr. Bahce, a pulmonologist at VU University, Amsterdam, during the World Conference on Lung Cancer.
Until now, the only way to identify advanced non–small cell lung cancer (NSCLC) tumors that are candidates for treatment with a tyrosine kinase inhibitor has been to biopsy the tumor and run an in vitro genetic analysis on the tumor cells. That can be challenging in some patients, such as when the tumor is not easy to biopsy, a limited amount of tissue is available, or the tumor is genetically heterogeneous. To get a reliable result from biopsy and testing, at least 30% of the specimen must contain malignant cells, Dr. Bahce said at the conference, sponsored by the International Association for the Study of Lung Cancer.
"It is a very early study, but ... it’s important because personalized treatment [for cancer] has gone to the next level, where we use new agents and match them to the right patients by doing biopsies," commented Dr. Roy S. Herbst, chief of medical oncology at the Yale Cancer Center in New Haven. "The PET method also allows physicians to assess the volume of cancer carrying the EGFR mutation following treatment, a way to track treatment efficacy," said Dr. Herbst in an interview.
"Instead of getting tissue at one point in time, you can image more frequently. It’s a way to track the course of treatment noninvasively," and in real time, he said.
He also predicted that the [11C]erlotinib PET test will become commercialized, although currently Dr. Bahce’s studies do not have any commercial funding.
"This is a proof of concept study," commented Dr. Luis Paz-Ares, chief of medical oncology at University Hospital Virgin del Rocio in Seville, Spain. "We need to define the positive predictive value and the negative predictive value" of the test, he added. The long-term future of a test like this may also be limited because future testing will probably need to look at multiple biomarkers, Dr. Paz-Ares said.
The study enrolled five patients with advanced NSCLC who had exon 19 deletion EGFR mutations, and five advanced NSCLC patients with wild-type EGFR genes. Each patient underwent a pair of [11C]erlotinib PET scans, each preceded by a [15O]water PET scan to assess blood perfusion of the tumors. A 4-hour interval separated the two sets of scans.
The scan results showed that the volume of distribution of the tagged erlotinib in the patients with EGFR mutations ran about 50% higher than in the patients with wild-type tumors, a difference that was significant (P = .03). Clinically, two of the five wild-type patients had nonetheless received erlotinib treatment prior to testing, and neither patient responded, with both showing progressive disease.
Three of the five patients with an EGFR mutation began receiving erlotinib treatment after testing and responded. In one of these patients, the tumor remained in check for 13 months. In a second patient, the tumor began to progress after 17 months of no progression on treatment. In the third patient, the tumor began to progress again after about 4 weeks of no progression on erlotinib treatment, Dr. Bahce said. A fourth patient went on erlotinib treatment before testing, and did not respond and continued to have progressive disease.
The two patient subgroups showed no difference in blood perfusion into the tumors or in EGFR expression in cell membranes.
Dr. Bahce said he had no disclosures.☐
Major Finding: Advanced non–small cell lung cancer tumors with an epidermal growth factor receptor (EGFR)–activating mutation bound significantly more radiolabeled erlotinib than did tumors with wild-type EGFR genes (P = .03).
Data Source: A pilot study in 10 patients.
Disclosures: Dr. Bahce said he had no disclosures.
Noninvasive Scan Has Promise For Lung Cancer Genotyping
AMSTERDAM – An experimental combination of PET scanning and a positron-emitting form of erlotinib appeared to work as a noninvasive way of identifying patients with advanced non–small cell lung cancer tumors that have the right genotype to receive erlotinib therapy.
"[11C]erlotinib PET shows promise as a noninvasive, in vivo means of selecting patients who may benefit from thymidine kinase inhibitor therapy," Dr. Idris Bahce said, reporting on a pilot study of 10 patients. Erlotinib (Tarceva) is from the thymidine kinase inhibitor drug class.
In his study, uptake of 11C-labeled erlotinib was significantly linked to the patients’ having an activating mutation in their epidermal growth factor receptor (EGFR) gene, specifically an exon 19 deletion.
Patients positive for erlotinib uptake on the PET scan also showed a tendency for better clinical responses to a therapeutic erlotinib regimen, reported Dr. Bahce, a pulmonologist at VU University, Amsterdam, during the World Conference on Lung Cancer.
Until now, the only way to identify advanced non–small cell lung cancer (NSCLC) tumors that are candidates for treatment with a tyrosine kinase inhibitor has been to biopsy the tumor and run an in vitro genetic analysis on the tumor cells. That can be challenging in some patients, such as when the tumor is not easy to biopsy, a limited amount of tissue is available, or the tumor is genetically heterogeneous. To get a reliable result from biopsy and testing, at least 30% of the specimen must contain malignant cells, Dr. Bahce said at the conference, sponsored by the International Association for the Study of Lung Cancer.
"It is a very early study, but ... it’s important because personalized treatment [for cancer] has gone to the next level, where we use new agents and match them to the right patients by doing biopsies," commented Dr. Roy S. Herbst, chief of medical oncology at the Yale Cancer Center in New Haven. "The PET method also allows physicians to assess the volume of cancer carrying the EGFR mutation following treatment, a way to track treatment efficacy," said Dr. Herbst in an interview.
"Instead of getting tissue at one point in time, you can image more frequently. It’s a way to track the course of treatment noninvasively," and in real time, he said.
He also predicted that the [11C]erlotinib PET test will become commercialized, although currently Dr. Bahce’s studies do not have any commercial funding.
"This is a proof of concept study," commented Dr. Luis Paz-Ares, chief of medical oncology at University Hospital Virgin del Rocio in Seville, Spain. "We need to define the positive predictive value and the negative predictive value" of the test, he added. The long-term future of a test like this may also be limited because future testing will probably need to look at multiple biomarkers, Dr. Paz-Ares said.
The study enrolled five patients with advanced NSCLC who had exon 19 deletion EGFR mutations, and five advanced NSCLC patients with wild-type EGFR genes. Each patient underwent a pair of [11C]erlotinib PET scans, each preceded by a [15O]water PET scan to assess blood perfusion of the tumors. A 4-hour interval separated the two sets of scans.
The scan results showed that the volume of distribution of the tagged erlotinib in the patients with EGFR mutations ran about 50% higher than in the patients with wild-type tumors, a difference that was significant (P = .03). Clinically, two of the five wild-type patients had nonetheless received erlotinib treatment prior to testing, and neither patient responded, with both showing progressive disease.
Three of the five patients with an EGFR mutation began receiving erlotinib treatment after testing and responded. In one of these patients, the tumor remained in check for 13 months. In a second patient, the tumor began to progress after 17 months of no progression on treatment. In the third patient, the tumor began to progress again after about 4 weeks of no progression on erlotinib treatment, Dr. Bahce said. A fourth patient went on erlotinib treatment before testing, and did not respond and continued to have progressive disease.
The two patient subgroups showed no difference in blood perfusion into the tumors or in EGFR expression in cell membranes.
Dr. Bahce said he had no disclosures.☐
AMSTERDAM – An experimental combination of PET scanning and a positron-emitting form of erlotinib appeared to work as a noninvasive way of identifying patients with advanced non–small cell lung cancer tumors that have the right genotype to receive erlotinib therapy.
"[11C]erlotinib PET shows promise as a noninvasive, in vivo means of selecting patients who may benefit from thymidine kinase inhibitor therapy," Dr. Idris Bahce said, reporting on a pilot study of 10 patients. Erlotinib (Tarceva) is from the thymidine kinase inhibitor drug class.
In his study, uptake of 11C-labeled erlotinib was significantly linked to the patients’ having an activating mutation in their epidermal growth factor receptor (EGFR) gene, specifically an exon 19 deletion.
Patients positive for erlotinib uptake on the PET scan also showed a tendency for better clinical responses to a therapeutic erlotinib regimen, reported Dr. Bahce, a pulmonologist at VU University, Amsterdam, during the World Conference on Lung Cancer.
Until now, the only way to identify advanced non–small cell lung cancer (NSCLC) tumors that are candidates for treatment with a tyrosine kinase inhibitor has been to biopsy the tumor and run an in vitro genetic analysis on the tumor cells. That can be challenging in some patients, such as when the tumor is not easy to biopsy, a limited amount of tissue is available, or the tumor is genetically heterogeneous. To get a reliable result from biopsy and testing, at least 30% of the specimen must contain malignant cells, Dr. Bahce said at the conference, sponsored by the International Association for the Study of Lung Cancer.
"It is a very early study, but ... it’s important because personalized treatment [for cancer] has gone to the next level, where we use new agents and match them to the right patients by doing biopsies," commented Dr. Roy S. Herbst, chief of medical oncology at the Yale Cancer Center in New Haven. "The PET method also allows physicians to assess the volume of cancer carrying the EGFR mutation following treatment, a way to track treatment efficacy," said Dr. Herbst in an interview.
"Instead of getting tissue at one point in time, you can image more frequently. It’s a way to track the course of treatment noninvasively," and in real time, he said.
He also predicted that the [11C]erlotinib PET test will become commercialized, although currently Dr. Bahce’s studies do not have any commercial funding.
"This is a proof of concept study," commented Dr. Luis Paz-Ares, chief of medical oncology at University Hospital Virgin del Rocio in Seville, Spain. "We need to define the positive predictive value and the negative predictive value" of the test, he added. The long-term future of a test like this may also be limited because future testing will probably need to look at multiple biomarkers, Dr. Paz-Ares said.
The study enrolled five patients with advanced NSCLC who had exon 19 deletion EGFR mutations, and five advanced NSCLC patients with wild-type EGFR genes. Each patient underwent a pair of [11C]erlotinib PET scans, each preceded by a [15O]water PET scan to assess blood perfusion of the tumors. A 4-hour interval separated the two sets of scans.
The scan results showed that the volume of distribution of the tagged erlotinib in the patients with EGFR mutations ran about 50% higher than in the patients with wild-type tumors, a difference that was significant (P = .03). Clinically, two of the five wild-type patients had nonetheless received erlotinib treatment prior to testing, and neither patient responded, with both showing progressive disease.
Three of the five patients with an EGFR mutation began receiving erlotinib treatment after testing and responded. In one of these patients, the tumor remained in check for 13 months. In a second patient, the tumor began to progress after 17 months of no progression on treatment. In the third patient, the tumor began to progress again after about 4 weeks of no progression on erlotinib treatment, Dr. Bahce said. A fourth patient went on erlotinib treatment before testing, and did not respond and continued to have progressive disease.
The two patient subgroups showed no difference in blood perfusion into the tumors or in EGFR expression in cell membranes.
Dr. Bahce said he had no disclosures.☐
AMSTERDAM – An experimental combination of PET scanning and a positron-emitting form of erlotinib appeared to work as a noninvasive way of identifying patients with advanced non–small cell lung cancer tumors that have the right genotype to receive erlotinib therapy.
"[11C]erlotinib PET shows promise as a noninvasive, in vivo means of selecting patients who may benefit from thymidine kinase inhibitor therapy," Dr. Idris Bahce said, reporting on a pilot study of 10 patients. Erlotinib (Tarceva) is from the thymidine kinase inhibitor drug class.
In his study, uptake of 11C-labeled erlotinib was significantly linked to the patients’ having an activating mutation in their epidermal growth factor receptor (EGFR) gene, specifically an exon 19 deletion.
Patients positive for erlotinib uptake on the PET scan also showed a tendency for better clinical responses to a therapeutic erlotinib regimen, reported Dr. Bahce, a pulmonologist at VU University, Amsterdam, during the World Conference on Lung Cancer.
Until now, the only way to identify advanced non–small cell lung cancer (NSCLC) tumors that are candidates for treatment with a tyrosine kinase inhibitor has been to biopsy the tumor and run an in vitro genetic analysis on the tumor cells. That can be challenging in some patients, such as when the tumor is not easy to biopsy, a limited amount of tissue is available, or the tumor is genetically heterogeneous. To get a reliable result from biopsy and testing, at least 30% of the specimen must contain malignant cells, Dr. Bahce said at the conference, sponsored by the International Association for the Study of Lung Cancer.
"It is a very early study, but ... it’s important because personalized treatment [for cancer] has gone to the next level, where we use new agents and match them to the right patients by doing biopsies," commented Dr. Roy S. Herbst, chief of medical oncology at the Yale Cancer Center in New Haven. "The PET method also allows physicians to assess the volume of cancer carrying the EGFR mutation following treatment, a way to track treatment efficacy," said Dr. Herbst in an interview.
"Instead of getting tissue at one point in time, you can image more frequently. It’s a way to track the course of treatment noninvasively," and in real time, he said.
He also predicted that the [11C]erlotinib PET test will become commercialized, although currently Dr. Bahce’s studies do not have any commercial funding.
"This is a proof of concept study," commented Dr. Luis Paz-Ares, chief of medical oncology at University Hospital Virgin del Rocio in Seville, Spain. "We need to define the positive predictive value and the negative predictive value" of the test, he added. The long-term future of a test like this may also be limited because future testing will probably need to look at multiple biomarkers, Dr. Paz-Ares said.
The study enrolled five patients with advanced NSCLC who had exon 19 deletion EGFR mutations, and five advanced NSCLC patients with wild-type EGFR genes. Each patient underwent a pair of [11C]erlotinib PET scans, each preceded by a [15O]water PET scan to assess blood perfusion of the tumors. A 4-hour interval separated the two sets of scans.
The scan results showed that the volume of distribution of the tagged erlotinib in the patients with EGFR mutations ran about 50% higher than in the patients with wild-type tumors, a difference that was significant (P = .03). Clinically, two of the five wild-type patients had nonetheless received erlotinib treatment prior to testing, and neither patient responded, with both showing progressive disease.
Three of the five patients with an EGFR mutation began receiving erlotinib treatment after testing and responded. In one of these patients, the tumor remained in check for 13 months. In a second patient, the tumor began to progress after 17 months of no progression on treatment. In the third patient, the tumor began to progress again after about 4 weeks of no progression on erlotinib treatment, Dr. Bahce said. A fourth patient went on erlotinib treatment before testing, and did not respond and continued to have progressive disease.
The two patient subgroups showed no difference in blood perfusion into the tumors or in EGFR expression in cell membranes.
Dr. Bahce said he had no disclosures.☐
Major Finding: Advanced non–small cell lung cancer tumors with an epidermal growth factor receptor (EGFR)–activating mutation bound significantly more radiolabeled erlotinib than did tumors with wild-type EGFR genes (P = .03).
Data Source: A pilot study in 10 patients.
Disclosures: Dr. Bahce said he had no disclosures.
Alter Surveillance for Barrett's Esophagus?
The incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was only 1.2 cases per 1,000 person-years in a study of the entire population of Denmark reported in the New England Journal of Medicine.
That rate is four to five times lower than rates reported previously, said Dr. Frederik Hvid-Jensen of the department of surgical gastroenterology at Aarhus (Denmark) University and his associates.
"Our study provides solid evidence that esophageal adenocarcinoma will develop in very few patients with Barrett’s esophagus. Together with another recent study, as well as studies of cost-effectiveness and patients’ quality of life, the results of our study suggest that the risk of esophageal adenocarcinoma among patients with Barrett’s esophagus is so minor that in the absence of dysplasia, routine surveillance of such patients is of doubtful value," the investigators said.
The relevance of such surveillance programs has been questioned before because they have never been shown to improve survival and because an estimated 95% of patients with a new diagnosis of esophageal adenocarcinoma do not have a previous diagnosis of Barrett’s esophagus, they noted.
Dr. Hvid-Jensen and his colleagues used data from Denmark’s nationwide pathology and cancer registries to calculate the incidence of adenocarcinoma among patients with Barrett’s esophagus and compare it with the expected incidence in the general population of 5.4 million people.
A total of 11,028 patients underwent endoscopic biopsy and received a diagnosis of Barrett’s esophagus during 1992-2009. The median age at baseline was 63 years, and patients were followed for a median of 5.2 years.
During that time, 197 of these patients with Barrett’s esophagus developed new esophageal adenocarcinomas, which comprised 7.6% of all the 2,602 incident esophageal adenocarcinomas diagnosed in the general Danish population during 1992-2009.
After excluding cancer cases that developed in the first year after a diagnosis of Barrett’s esophagus, the incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was found to be 1.2 cases per 1,000 person-years, the investigators said (N. Engl. J. Med. 2011;365:1375-83).
The annual risk of developing the malignancy was only 0.12%, or one case of adenocarcinoma per 860 patient-years.
In contrast, there were four reviews of the literature published in the past decade that pooled the results of numerous small studies conducted throughout the United States and Europe. These studies calculated the esophageal adenocarcinoma incidence as ranging from 5.2 to 7.0 cases per 1,000 person-years. In addition, two previous registry studies calculated similar incidences of 4.0 and 5.0 cases of esophogeal cardinoma per 1,000 person-years.
Current surveillance guidelines are based upon these earlier studies, which appear to have overstated the risks, Dr. Hvid-Jensen and his associates stated.
Their population-based, nationwide study is one of the largest studies of the issue; it included patients of all ages and both sexes and had almost no loss to follow-up. Because of Denmark’s universal health care plan, this study also had no referral bias or diagnostic bias.
"The generalizability of our results is therefore high," they noted.
Moreover, a recent population-based study in Northern Ireland found remarkably similar results: an incidence of 1.3 cases of esophageal adenocarcinoma per 1,000 patient-years among people with Barrett’s esophagus.
And another recent study "in which Markov models were used to evaluate available data on the incidence of adenocarcinoma supports our findings ... [and suggests] that surveillance is not beneficial," the researchers added.
This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.☐
The "elegant" epidemiologic study by Dr. Hvid-Jensen and associates clearly shows that the relative risk of esophageal adenocarcinoma for a person with Barrett’s esophagus, as compared with the general population, is 11.3, "a substantial drop from the increase by a factor of 30 or 40 estimated in early reports," said Dr. Peter J. Kahrilas.
"As our knowledge of the biologic characteristics of Barrett’s esophagus has matured, the significance of the lesion has dwindled. In fact, patients with Barrett’s esophagus have the same life expectancy as does the general population, and esophageal cancer proves to be an uncommon cause of death in patients with Barrett’s esophagus regardless of surveillance," he noted.
Dr. Kahrilas is with the department of medicine at Northwestern University, Chicago. He reported ties to numerous industry sources. These remarks were taken from his editorial accompanying Dr. Hvid-Jensen’s report (N. Engl. J. Med. 2011;365:1437-8).
The "elegant" epidemiologic study by Dr. Hvid-Jensen and associates clearly shows that the relative risk of esophageal adenocarcinoma for a person with Barrett’s esophagus, as compared with the general population, is 11.3, "a substantial drop from the increase by a factor of 30 or 40 estimated in early reports," said Dr. Peter J. Kahrilas.
"As our knowledge of the biologic characteristics of Barrett’s esophagus has matured, the significance of the lesion has dwindled. In fact, patients with Barrett’s esophagus have the same life expectancy as does the general population, and esophageal cancer proves to be an uncommon cause of death in patients with Barrett’s esophagus regardless of surveillance," he noted.
Dr. Kahrilas is with the department of medicine at Northwestern University, Chicago. He reported ties to numerous industry sources. These remarks were taken from his editorial accompanying Dr. Hvid-Jensen’s report (N. Engl. J. Med. 2011;365:1437-8).
The "elegant" epidemiologic study by Dr. Hvid-Jensen and associates clearly shows that the relative risk of esophageal adenocarcinoma for a person with Barrett’s esophagus, as compared with the general population, is 11.3, "a substantial drop from the increase by a factor of 30 or 40 estimated in early reports," said Dr. Peter J. Kahrilas.
"As our knowledge of the biologic characteristics of Barrett’s esophagus has matured, the significance of the lesion has dwindled. In fact, patients with Barrett’s esophagus have the same life expectancy as does the general population, and esophageal cancer proves to be an uncommon cause of death in patients with Barrett’s esophagus regardless of surveillance," he noted.
Dr. Kahrilas is with the department of medicine at Northwestern University, Chicago. He reported ties to numerous industry sources. These remarks were taken from his editorial accompanying Dr. Hvid-Jensen’s report (N. Engl. J. Med. 2011;365:1437-8).
The incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was only 1.2 cases per 1,000 person-years in a study of the entire population of Denmark reported in the New England Journal of Medicine.
That rate is four to five times lower than rates reported previously, said Dr. Frederik Hvid-Jensen of the department of surgical gastroenterology at Aarhus (Denmark) University and his associates.
"Our study provides solid evidence that esophageal adenocarcinoma will develop in very few patients with Barrett’s esophagus. Together with another recent study, as well as studies of cost-effectiveness and patients’ quality of life, the results of our study suggest that the risk of esophageal adenocarcinoma among patients with Barrett’s esophagus is so minor that in the absence of dysplasia, routine surveillance of such patients is of doubtful value," the investigators said.
The relevance of such surveillance programs has been questioned before because they have never been shown to improve survival and because an estimated 95% of patients with a new diagnosis of esophageal adenocarcinoma do not have a previous diagnosis of Barrett’s esophagus, they noted.
Dr. Hvid-Jensen and his colleagues used data from Denmark’s nationwide pathology and cancer registries to calculate the incidence of adenocarcinoma among patients with Barrett’s esophagus and compare it with the expected incidence in the general population of 5.4 million people.
A total of 11,028 patients underwent endoscopic biopsy and received a diagnosis of Barrett’s esophagus during 1992-2009. The median age at baseline was 63 years, and patients were followed for a median of 5.2 years.
During that time, 197 of these patients with Barrett’s esophagus developed new esophageal adenocarcinomas, which comprised 7.6% of all the 2,602 incident esophageal adenocarcinomas diagnosed in the general Danish population during 1992-2009.
After excluding cancer cases that developed in the first year after a diagnosis of Barrett’s esophagus, the incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was found to be 1.2 cases per 1,000 person-years, the investigators said (N. Engl. J. Med. 2011;365:1375-83).
The annual risk of developing the malignancy was only 0.12%, or one case of adenocarcinoma per 860 patient-years.
In contrast, there were four reviews of the literature published in the past decade that pooled the results of numerous small studies conducted throughout the United States and Europe. These studies calculated the esophageal adenocarcinoma incidence as ranging from 5.2 to 7.0 cases per 1,000 person-years. In addition, two previous registry studies calculated similar incidences of 4.0 and 5.0 cases of esophogeal cardinoma per 1,000 person-years.
Current surveillance guidelines are based upon these earlier studies, which appear to have overstated the risks, Dr. Hvid-Jensen and his associates stated.
Their population-based, nationwide study is one of the largest studies of the issue; it included patients of all ages and both sexes and had almost no loss to follow-up. Because of Denmark’s universal health care plan, this study also had no referral bias or diagnostic bias.
"The generalizability of our results is therefore high," they noted.
Moreover, a recent population-based study in Northern Ireland found remarkably similar results: an incidence of 1.3 cases of esophageal adenocarcinoma per 1,000 patient-years among people with Barrett’s esophagus.
And another recent study "in which Markov models were used to evaluate available data on the incidence of adenocarcinoma supports our findings ... [and suggests] that surveillance is not beneficial," the researchers added.
This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.☐
The incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was only 1.2 cases per 1,000 person-years in a study of the entire population of Denmark reported in the New England Journal of Medicine.
That rate is four to five times lower than rates reported previously, said Dr. Frederik Hvid-Jensen of the department of surgical gastroenterology at Aarhus (Denmark) University and his associates.
"Our study provides solid evidence that esophageal adenocarcinoma will develop in very few patients with Barrett’s esophagus. Together with another recent study, as well as studies of cost-effectiveness and patients’ quality of life, the results of our study suggest that the risk of esophageal adenocarcinoma among patients with Barrett’s esophagus is so minor that in the absence of dysplasia, routine surveillance of such patients is of doubtful value," the investigators said.
The relevance of such surveillance programs has been questioned before because they have never been shown to improve survival and because an estimated 95% of patients with a new diagnosis of esophageal adenocarcinoma do not have a previous diagnosis of Barrett’s esophagus, they noted.
Dr. Hvid-Jensen and his colleagues used data from Denmark’s nationwide pathology and cancer registries to calculate the incidence of adenocarcinoma among patients with Barrett’s esophagus and compare it with the expected incidence in the general population of 5.4 million people.
A total of 11,028 patients underwent endoscopic biopsy and received a diagnosis of Barrett’s esophagus during 1992-2009. The median age at baseline was 63 years, and patients were followed for a median of 5.2 years.
During that time, 197 of these patients with Barrett’s esophagus developed new esophageal adenocarcinomas, which comprised 7.6% of all the 2,602 incident esophageal adenocarcinomas diagnosed in the general Danish population during 1992-2009.
After excluding cancer cases that developed in the first year after a diagnosis of Barrett’s esophagus, the incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was found to be 1.2 cases per 1,000 person-years, the investigators said (N. Engl. J. Med. 2011;365:1375-83).
The annual risk of developing the malignancy was only 0.12%, or one case of adenocarcinoma per 860 patient-years.
In contrast, there were four reviews of the literature published in the past decade that pooled the results of numerous small studies conducted throughout the United States and Europe. These studies calculated the esophageal adenocarcinoma incidence as ranging from 5.2 to 7.0 cases per 1,000 person-years. In addition, two previous registry studies calculated similar incidences of 4.0 and 5.0 cases of esophogeal cardinoma per 1,000 person-years.
Current surveillance guidelines are based upon these earlier studies, which appear to have overstated the risks, Dr. Hvid-Jensen and his associates stated.
Their population-based, nationwide study is one of the largest studies of the issue; it included patients of all ages and both sexes and had almost no loss to follow-up. Because of Denmark’s universal health care plan, this study also had no referral bias or diagnostic bias.
"The generalizability of our results is therefore high," they noted.
Moreover, a recent population-based study in Northern Ireland found remarkably similar results: an incidence of 1.3 cases of esophageal adenocarcinoma per 1,000 patient-years among people with Barrett’s esophagus.
And another recent study "in which Markov models were used to evaluate available data on the incidence of adenocarcinoma supports our findings ... [and suggests] that surveillance is not beneficial," the researchers added.
This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.☐
Major Finding: The incidence of esophageal adenocarcinoma among all patients in Denmark with Barrett’s esophagus was 1.2 cases per 1,000 person-years, which is four to five times lower than estimated in previous, smaller studies.
Data Source: An epidemiologic cohort study of esophageal adenocarcinoma among the 5.4 million residents of Denmark, including 11,028 with Barrett’s esophagus followed for a median of 5.2 years.
Disclosures: This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.
Alter Surveillance for Barrett's Esophagus?
The incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was only 1.2 cases per 1,000 person-years in a study of the entire population of Denmark reported in the New England Journal of Medicine.
That rate is four to five times lower than rates reported previously, said Dr. Frederik Hvid-Jensen of the department of surgical gastroenterology at Aarhus (Denmark) University and his associates.
"Our study provides solid evidence that esophageal adenocarcinoma will develop in very few patients with Barrett’s esophagus. Together with another recent study, as well as studies of cost-effectiveness and patients’ quality of life, the results of our study suggest that the risk of esophageal adenocarcinoma among patients with Barrett’s esophagus is so minor that in the absence of dysplasia, routine surveillance of such patients is of doubtful value," the investigators said.
The relevance of such surveillance programs has been questioned before because they have never been shown to improve survival and because an estimated 95% of patients with a new diagnosis of esophageal adenocarcinoma do not have a previous diagnosis of Barrett’s esophagus, they noted.
Dr. Hvid-Jensen and his colleagues used data from Denmark’s nationwide pathology and cancer registries to calculate the incidence of adenocarcinoma among patients with Barrett’s esophagus and compare it with the expected incidence in the general population of 5.4 million people.
A total of 11,028 patients underwent endoscopic biopsy and received a diagnosis of Barrett’s esophagus during 1992-2009. The median age at baseline was 63 years, and patients were followed for a median of 5.2 years.
During that time, 197 of these patients with Barrett’s esophagus developed new esophageal adenocarcinomas, which comprised 7.6% of all the 2,602 incident esophageal adenocarcinomas diagnosed in the general Danish population during 1992-2009.
After excluding cancer cases that developed in the first year after a diagnosis of Barrett’s esophagus, the incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was found to be 1.2 cases per 1,000 person-years, the investigators said (N. Engl. J. Med. 2011;365:1375-83).
The annual risk of developing the malignancy was only 0.12%, or one case of adenocarcinoma per 860 patient-years.
In contrast, there were four reviews of the literature published in the past decade that pooled the results of numerous small studies conducted throughout the United States and Europe. These studies calculated the esophageal adenocarcinoma incidence as ranging from 5.2 to 7.0 cases per 1,000 person-years. In addition, two previous registry studies calculated similar incidences of 4.0 and 5.0 cases of esophogeal cardinoma per 1,000 person-years.
Current surveillance guidelines are based upon these earlier studies, which appear to have overstated the risks, Dr. Hvid-Jensen and his associates stated.
Their population-based, nationwide study is one of the largest studies of the issue; it included patients of all ages and both sexes and had almost no loss to follow-up. Because of Denmark’s universal health care plan, this study also had no referral bias or diagnostic bias.
"The generalizability of our results is therefore high," they noted.
Moreover, a recent population-based study in Northern Ireland found remarkably similar results: an incidence of 1.3 cases of esophageal adenocarcinoma per 1,000 patient-years among people with Barrett’s esophagus.
And another recent study "in which Markov models were used to evaluate available data on the incidence of adenocarcinoma supports our findings ... [and suggests] that surveillance is not beneficial," the researchers added.
This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.☐
The "elegant" epidemiologic study by Dr. Hvid-Jensen and associates clearly shows that the relative risk of esophageal adenocarcinoma for a person with Barrett’s esophagus, as compared with the general population, is 11.3, "a substantial drop from the increase by a factor of 30 or 40 estimated in early reports," said Dr. Peter J. Kahrilas.
"As our knowledge of the biologic characteristics of Barrett’s esophagus has matured, the significance of the lesion has dwindled. In fact, patients with Barrett’s esophagus have the same life expectancy as does the general population, and esophageal cancer proves to be an uncommon cause of death in patients with Barrett’s esophagus regardless of surveillance," he noted.
Dr. Kahrilas is with the department of medicine at Northwestern University, Chicago. He reported ties to numerous industry sources. These remarks were taken from his editorial accompanying Dr. Hvid-Jensen’s report (N. Engl. J. Med. 2011;365:1437-8).
The "elegant" epidemiologic study by Dr. Hvid-Jensen and associates clearly shows that the relative risk of esophageal adenocarcinoma for a person with Barrett’s esophagus, as compared with the general population, is 11.3, "a substantial drop from the increase by a factor of 30 or 40 estimated in early reports," said Dr. Peter J. Kahrilas.
"As our knowledge of the biologic characteristics of Barrett’s esophagus has matured, the significance of the lesion has dwindled. In fact, patients with Barrett’s esophagus have the same life expectancy as does the general population, and esophageal cancer proves to be an uncommon cause of death in patients with Barrett’s esophagus regardless of surveillance," he noted.
Dr. Kahrilas is with the department of medicine at Northwestern University, Chicago. He reported ties to numerous industry sources. These remarks were taken from his editorial accompanying Dr. Hvid-Jensen’s report (N. Engl. J. Med. 2011;365:1437-8).
The "elegant" epidemiologic study by Dr. Hvid-Jensen and associates clearly shows that the relative risk of esophageal adenocarcinoma for a person with Barrett’s esophagus, as compared with the general population, is 11.3, "a substantial drop from the increase by a factor of 30 or 40 estimated in early reports," said Dr. Peter J. Kahrilas.
"As our knowledge of the biologic characteristics of Barrett’s esophagus has matured, the significance of the lesion has dwindled. In fact, patients with Barrett’s esophagus have the same life expectancy as does the general population, and esophageal cancer proves to be an uncommon cause of death in patients with Barrett’s esophagus regardless of surveillance," he noted.
Dr. Kahrilas is with the department of medicine at Northwestern University, Chicago. He reported ties to numerous industry sources. These remarks were taken from his editorial accompanying Dr. Hvid-Jensen’s report (N. Engl. J. Med. 2011;365:1437-8).
The incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was only 1.2 cases per 1,000 person-years in a study of the entire population of Denmark reported in the New England Journal of Medicine.
That rate is four to five times lower than rates reported previously, said Dr. Frederik Hvid-Jensen of the department of surgical gastroenterology at Aarhus (Denmark) University and his associates.
"Our study provides solid evidence that esophageal adenocarcinoma will develop in very few patients with Barrett’s esophagus. Together with another recent study, as well as studies of cost-effectiveness and patients’ quality of life, the results of our study suggest that the risk of esophageal adenocarcinoma among patients with Barrett’s esophagus is so minor that in the absence of dysplasia, routine surveillance of such patients is of doubtful value," the investigators said.
The relevance of such surveillance programs has been questioned before because they have never been shown to improve survival and because an estimated 95% of patients with a new diagnosis of esophageal adenocarcinoma do not have a previous diagnosis of Barrett’s esophagus, they noted.
Dr. Hvid-Jensen and his colleagues used data from Denmark’s nationwide pathology and cancer registries to calculate the incidence of adenocarcinoma among patients with Barrett’s esophagus and compare it with the expected incidence in the general population of 5.4 million people.
A total of 11,028 patients underwent endoscopic biopsy and received a diagnosis of Barrett’s esophagus during 1992-2009. The median age at baseline was 63 years, and patients were followed for a median of 5.2 years.
During that time, 197 of these patients with Barrett’s esophagus developed new esophageal adenocarcinomas, which comprised 7.6% of all the 2,602 incident esophageal adenocarcinomas diagnosed in the general Danish population during 1992-2009.
After excluding cancer cases that developed in the first year after a diagnosis of Barrett’s esophagus, the incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was found to be 1.2 cases per 1,000 person-years, the investigators said (N. Engl. J. Med. 2011;365:1375-83).
The annual risk of developing the malignancy was only 0.12%, or one case of adenocarcinoma per 860 patient-years.
In contrast, there were four reviews of the literature published in the past decade that pooled the results of numerous small studies conducted throughout the United States and Europe. These studies calculated the esophageal adenocarcinoma incidence as ranging from 5.2 to 7.0 cases per 1,000 person-years. In addition, two previous registry studies calculated similar incidences of 4.0 and 5.0 cases of esophogeal cardinoma per 1,000 person-years.
Current surveillance guidelines are based upon these earlier studies, which appear to have overstated the risks, Dr. Hvid-Jensen and his associates stated.
Their population-based, nationwide study is one of the largest studies of the issue; it included patients of all ages and both sexes and had almost no loss to follow-up. Because of Denmark’s universal health care plan, this study also had no referral bias or diagnostic bias.
"The generalizability of our results is therefore high," they noted.
Moreover, a recent population-based study in Northern Ireland found remarkably similar results: an incidence of 1.3 cases of esophageal adenocarcinoma per 1,000 patient-years among people with Barrett’s esophagus.
And another recent study "in which Markov models were used to evaluate available data on the incidence of adenocarcinoma supports our findings ... [and suggests] that surveillance is not beneficial," the researchers added.
This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.☐
The incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was only 1.2 cases per 1,000 person-years in a study of the entire population of Denmark reported in the New England Journal of Medicine.
That rate is four to five times lower than rates reported previously, said Dr. Frederik Hvid-Jensen of the department of surgical gastroenterology at Aarhus (Denmark) University and his associates.
"Our study provides solid evidence that esophageal adenocarcinoma will develop in very few patients with Barrett’s esophagus. Together with another recent study, as well as studies of cost-effectiveness and patients’ quality of life, the results of our study suggest that the risk of esophageal adenocarcinoma among patients with Barrett’s esophagus is so minor that in the absence of dysplasia, routine surveillance of such patients is of doubtful value," the investigators said.
The relevance of such surveillance programs has been questioned before because they have never been shown to improve survival and because an estimated 95% of patients with a new diagnosis of esophageal adenocarcinoma do not have a previous diagnosis of Barrett’s esophagus, they noted.
Dr. Hvid-Jensen and his colleagues used data from Denmark’s nationwide pathology and cancer registries to calculate the incidence of adenocarcinoma among patients with Barrett’s esophagus and compare it with the expected incidence in the general population of 5.4 million people.
A total of 11,028 patients underwent endoscopic biopsy and received a diagnosis of Barrett’s esophagus during 1992-2009. The median age at baseline was 63 years, and patients were followed for a median of 5.2 years.
During that time, 197 of these patients with Barrett’s esophagus developed new esophageal adenocarcinomas, which comprised 7.6% of all the 2,602 incident esophageal adenocarcinomas diagnosed in the general Danish population during 1992-2009.
After excluding cancer cases that developed in the first year after a diagnosis of Barrett’s esophagus, the incidence of esophageal adenocarcinoma among patients with Barrett’s esophagus was found to be 1.2 cases per 1,000 person-years, the investigators said (N. Engl. J. Med. 2011;365:1375-83).
The annual risk of developing the malignancy was only 0.12%, or one case of adenocarcinoma per 860 patient-years.
In contrast, there were four reviews of the literature published in the past decade that pooled the results of numerous small studies conducted throughout the United States and Europe. These studies calculated the esophageal adenocarcinoma incidence as ranging from 5.2 to 7.0 cases per 1,000 person-years. In addition, two previous registry studies calculated similar incidences of 4.0 and 5.0 cases of esophogeal cardinoma per 1,000 person-years.
Current surveillance guidelines are based upon these earlier studies, which appear to have overstated the risks, Dr. Hvid-Jensen and his associates stated.
Their population-based, nationwide study is one of the largest studies of the issue; it included patients of all ages and both sexes and had almost no loss to follow-up. Because of Denmark’s universal health care plan, this study also had no referral bias or diagnostic bias.
"The generalizability of our results is therefore high," they noted.
Moreover, a recent population-based study in Northern Ireland found remarkably similar results: an incidence of 1.3 cases of esophageal adenocarcinoma per 1,000 patient-years among people with Barrett’s esophagus.
And another recent study "in which Markov models were used to evaluate available data on the incidence of adenocarcinoma supports our findings ... [and suggests] that surveillance is not beneficial," the researchers added.
This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.☐
Major Finding: The incidence of esophageal adenocarcinoma among all patients in Denmark with Barrett’s esophagus was 1.2 cases per 1,000 person-years, which is four to five times lower than estimated in previous, smaller studies.
Data Source: An epidemiologic cohort study of esophageal adenocarcinoma among the 5.4 million residents of Denmark, including 11,028 with Barrett’s esophagus followed for a median of 5.2 years.
Disclosures: This study was supported by the University of Aarhus Clinical Institute. No financial conflicts of interest were reported.
Lower Radiation Dose Improves Lung Cancer Survival
MIAMI BEACH – Less turned out to be better in a large clinical trial comparing radiation doses in patients treated with radiation and chemotherapy for stage III non–small cell lung cancer, investigators reported here.
The median overall survival rate at 1 year was 81% for patients treated with standard-dose (60 Gy) radiation, compared with 70.4% for those who received the high dose (74 Gy), according to preliminary findings from the radiation-dose arm of the ongoing phase III Radiation Therapy Oncology Group (RTOG) 0617 trial. The respective median survival rates were 21.7 months and 20.7 months (P = .02).
A planned interim analysis from the trial showed that the radiation comparison had crossed the prespecified boundary for futility, and the high-dose arm was stopped in June 2011, reported Dr. Jeffrey Bradley from Washington University in St. Louis at the annual meeting of the American Society for Radiation Oncology.
"I think this changes practice: If [cancer centers] weren’t using 60 Gray before, perhaps they should go back to using 60 Gray, because it does not appear that a higher dose is better," Dr. Bradley commented at the annual meeting of the American Society of Radiation Oncology (ASTRO).
Dr. Tim R. Williams, from the Lynn Cancer Institute at Boca Raton (Fla.) Regional Hospital, the immediate-past chairman of ASTRO, noted that his center has used high-dose radiation in stage III non–small cell lung cancer (NSCLC) patients for about 5 years. Although practice patterns vary, it’s likely that many treatment centers currently use the higher dose, he said.
In RTOG 0617, a total of 500 patients with stage IIIA/IIIB NSCLC were scheduled for randomization to one of four arms in a 2 x 2 factorial design with each patient assigned to receive either 74 Gy or 60 Gy radiation with or without cetuximab (Erbitux), on a background chemotherapy regimen of weekly paclitaxel (45 mg/m2) and carboplatin (titrated to an area-under-the-curve of 2).
The radiation was delivered in 2-Gy fractions over 30-37 fractions.
The analysis was performed on 426 patients who had been enrolled in the study before June 17, 2011.
Seeking to understand why the higher radiation dose was not better – the investigators had originally hypothesized that 74 Gy would result in a 7-month improvement in overall survival vs. 64 Gy – they performed univariate analyses, and found that significant predictors for better outcomes included continuous therapy, nonsquamous histology, and, female gender. In multivariate analysis, radiation dose (60 Gy vs. 74 Gy) was associated with a hazard ratio for overall survival of 1.48 (P = .038), nonsquamous histology versus squamous was associated with an HR of 1.52 (P = .025), and gross or internal tumor volume had a small but significant HR of 1.002 (P = .011).
Dr. Benjamin Movsas, chair of radiation oncology at the Henry Ford Health System in Detroit, the invited discussant, said that "as of 2011, level I evidence demonstrates no role for dose escalation in stage III non–small cell lung cancer."
He noted that although there were small differences between the radiation dose groups in terms of tumor histology, gross tumor volume, and other factors, they were not large enough to explain the differences in outcomes.
Citing the advice of his late father, also a physician, Dr. Movsas reminded the audience that "More is not always better."
The trial is continuing, but with patients assigned to 60 Gy radiation only, with the goal of evaluating the secondary study end point of overall survival of patients with or without cetuximab added to concurrent chemoradiotherapy.
The RTOG 0617 trial is supported by grants from the U.S. National Cancer Institute, with additional support from Bristol-Myers Squibb and ImClone.
Dr. Bradley and Dr. Williams had no disclosures. Dr. Movsas disclosed departmental research support from Varian and Philips. He also has served as a chair of an RTOG committee, but was not involved in the 0617 study.
MIAMI BEACH – Less turned out to be better in a large clinical trial comparing radiation doses in patients treated with radiation and chemotherapy for stage III non–small cell lung cancer, investigators reported here.
The median overall survival rate at 1 year was 81% for patients treated with standard-dose (60 Gy) radiation, compared with 70.4% for those who received the high dose (74 Gy), according to preliminary findings from the radiation-dose arm of the ongoing phase III Radiation Therapy Oncology Group (RTOG) 0617 trial. The respective median survival rates were 21.7 months and 20.7 months (P = .02).
A planned interim analysis from the trial showed that the radiation comparison had crossed the prespecified boundary for futility, and the high-dose arm was stopped in June 2011, reported Dr. Jeffrey Bradley from Washington University in St. Louis at the annual meeting of the American Society for Radiation Oncology.
"I think this changes practice: If [cancer centers] weren’t using 60 Gray before, perhaps they should go back to using 60 Gray, because it does not appear that a higher dose is better," Dr. Bradley commented at the annual meeting of the American Society of Radiation Oncology (ASTRO).
Dr. Tim R. Williams, from the Lynn Cancer Institute at Boca Raton (Fla.) Regional Hospital, the immediate-past chairman of ASTRO, noted that his center has used high-dose radiation in stage III non–small cell lung cancer (NSCLC) patients for about 5 years. Although practice patterns vary, it’s likely that many treatment centers currently use the higher dose, he said.
In RTOG 0617, a total of 500 patients with stage IIIA/IIIB NSCLC were scheduled for randomization to one of four arms in a 2 x 2 factorial design with each patient assigned to receive either 74 Gy or 60 Gy radiation with or without cetuximab (Erbitux), on a background chemotherapy regimen of weekly paclitaxel (45 mg/m2) and carboplatin (titrated to an area-under-the-curve of 2).
The radiation was delivered in 2-Gy fractions over 30-37 fractions.
The analysis was performed on 426 patients who had been enrolled in the study before June 17, 2011.
Seeking to understand why the higher radiation dose was not better – the investigators had originally hypothesized that 74 Gy would result in a 7-month improvement in overall survival vs. 64 Gy – they performed univariate analyses, and found that significant predictors for better outcomes included continuous therapy, nonsquamous histology, and, female gender. In multivariate analysis, radiation dose (60 Gy vs. 74 Gy) was associated with a hazard ratio for overall survival of 1.48 (P = .038), nonsquamous histology versus squamous was associated with an HR of 1.52 (P = .025), and gross or internal tumor volume had a small but significant HR of 1.002 (P = .011).
Dr. Benjamin Movsas, chair of radiation oncology at the Henry Ford Health System in Detroit, the invited discussant, said that "as of 2011, level I evidence demonstrates no role for dose escalation in stage III non–small cell lung cancer."
He noted that although there were small differences between the radiation dose groups in terms of tumor histology, gross tumor volume, and other factors, they were not large enough to explain the differences in outcomes.
Citing the advice of his late father, also a physician, Dr. Movsas reminded the audience that "More is not always better."
The trial is continuing, but with patients assigned to 60 Gy radiation only, with the goal of evaluating the secondary study end point of overall survival of patients with or without cetuximab added to concurrent chemoradiotherapy.
The RTOG 0617 trial is supported by grants from the U.S. National Cancer Institute, with additional support from Bristol-Myers Squibb and ImClone.
Dr. Bradley and Dr. Williams had no disclosures. Dr. Movsas disclosed departmental research support from Varian and Philips. He also has served as a chair of an RTOG committee, but was not involved in the 0617 study.
MIAMI BEACH – Less turned out to be better in a large clinical trial comparing radiation doses in patients treated with radiation and chemotherapy for stage III non–small cell lung cancer, investigators reported here.
The median overall survival rate at 1 year was 81% for patients treated with standard-dose (60 Gy) radiation, compared with 70.4% for those who received the high dose (74 Gy), according to preliminary findings from the radiation-dose arm of the ongoing phase III Radiation Therapy Oncology Group (RTOG) 0617 trial. The respective median survival rates were 21.7 months and 20.7 months (P = .02).
A planned interim analysis from the trial showed that the radiation comparison had crossed the prespecified boundary for futility, and the high-dose arm was stopped in June 2011, reported Dr. Jeffrey Bradley from Washington University in St. Louis at the annual meeting of the American Society for Radiation Oncology.
"I think this changes practice: If [cancer centers] weren’t using 60 Gray before, perhaps they should go back to using 60 Gray, because it does not appear that a higher dose is better," Dr. Bradley commented at the annual meeting of the American Society of Radiation Oncology (ASTRO).
Dr. Tim R. Williams, from the Lynn Cancer Institute at Boca Raton (Fla.) Regional Hospital, the immediate-past chairman of ASTRO, noted that his center has used high-dose radiation in stage III non–small cell lung cancer (NSCLC) patients for about 5 years. Although practice patterns vary, it’s likely that many treatment centers currently use the higher dose, he said.
In RTOG 0617, a total of 500 patients with stage IIIA/IIIB NSCLC were scheduled for randomization to one of four arms in a 2 x 2 factorial design with each patient assigned to receive either 74 Gy or 60 Gy radiation with or without cetuximab (Erbitux), on a background chemotherapy regimen of weekly paclitaxel (45 mg/m2) and carboplatin (titrated to an area-under-the-curve of 2).
The radiation was delivered in 2-Gy fractions over 30-37 fractions.
The analysis was performed on 426 patients who had been enrolled in the study before June 17, 2011.
Seeking to understand why the higher radiation dose was not better – the investigators had originally hypothesized that 74 Gy would result in a 7-month improvement in overall survival vs. 64 Gy – they performed univariate analyses, and found that significant predictors for better outcomes included continuous therapy, nonsquamous histology, and, female gender. In multivariate analysis, radiation dose (60 Gy vs. 74 Gy) was associated with a hazard ratio for overall survival of 1.48 (P = .038), nonsquamous histology versus squamous was associated with an HR of 1.52 (P = .025), and gross or internal tumor volume had a small but significant HR of 1.002 (P = .011).
Dr. Benjamin Movsas, chair of radiation oncology at the Henry Ford Health System in Detroit, the invited discussant, said that "as of 2011, level I evidence demonstrates no role for dose escalation in stage III non–small cell lung cancer."
He noted that although there were small differences between the radiation dose groups in terms of tumor histology, gross tumor volume, and other factors, they were not large enough to explain the differences in outcomes.
Citing the advice of his late father, also a physician, Dr. Movsas reminded the audience that "More is not always better."
The trial is continuing, but with patients assigned to 60 Gy radiation only, with the goal of evaluating the secondary study end point of overall survival of patients with or without cetuximab added to concurrent chemoradiotherapy.
The RTOG 0617 trial is supported by grants from the U.S. National Cancer Institute, with additional support from Bristol-Myers Squibb and ImClone.
Dr. Bradley and Dr. Williams had no disclosures. Dr. Movsas disclosed departmental research support from Varian and Philips. He also has served as a chair of an RTOG committee, but was not involved in the 0617 study.
Major Finding: Median overall survival among patients with stage III NSCLC treated with chemotherapy was 20.7 months with high-dose radiation (74 Gy), vs. 21.7 months with standard-dose radiation (60 Gy; P =.02).
Data Source: 426 patients enrolled in the randomized controlled RTOG 0617 trial.
Disclosures: Dr. Bradley and Dr. Williams had no disclosures. Dr. Movsas disclosed departmental research support from Varian and Philips. He also has served as a chair of an RTOG committee, but was not involved in the 0617 study.
Reflux Surgery Redos Safe, Outcomes Not Always Optimal
Reoperation for failed antireflux surgery can be performed safely in experienced centers, but outcomes are not as good as with primary operations, according to the results of two new analyses.
Dr. Nicholas R.A. Symons of Imperial College, London, and his associates performed a systematic literature review of 20 studies comprising 930 operations in 922 patients. "We can conclude that laparoscopic revision antireflux surgery, when performed in units with an interest in this type of surgery, is feasible and safe but subject to somewhat greater risk of conversion, higher morbidity, longer hospital stay, and poorer outcomes than primary laparoscopic fundoplication," the researchers said (Am. J. Surg. 2011;202:336-43).
Similarly, based on their retrospective study of 275 patients, Dr. Omar Awais of the University of Pittsburgh and his associates said, "Redo antireflux surgery can be performed safely in experienced centers, and as expected, the outcomes after redo antireflux surgery are not as good as [those of] first-time procedures. The operative approach depends on the underlying cause of failure" (Ann. Thorac. Surg. 2011;92:1083-90).
Between 2.8% and 4.4% of patients who undergo laparoscopic fundoplication at a specialist center will require late reoperation for persistent or recurrent symptoms, and there may be an increased revision rate after primary laparoscopic antireflux surgery compared with an initial open approach. Revision of failed antireflux surgery increasingly is being performed laparoscopically, but data about this approach are limited, Dr. Symons and his associates noted.
Their analysis included 19 case-control series and one prospective case-control study. Patients ranged in age from 13 to 83 years, and 57% were female. Of the eight articles in which the mean time between initial fundoplication and revision was given, the mean interval was 45.5 months (range 2-360 months). Of 12 studies noting the number of previous fundoplications the patients had undergone, 47 procedures (6.9%) were second reoperations and 9 (1.3%) were third reoperations.
Of the 18 studies documenting the type of initial surgery, 62% were laparoscopic, 35% were performed via laparotomy, 3% via thoracotomy, and 0.2% using video-assisted thoracoscopic surgery. Nissen fundoplication and Toupet partial fundoplication were the most common initial and revision procedures. Reflux/heartburn, experienced by 61% of patients, and dysphagia in 31% were the most common indications for laparoscopic reoperation, the investigators reported. Surgical duration, reported in 13 of the case series had an overall mean of 166 minutes for 721 patients.
The overall rate of conversion from laparoscopic reoperation to open surgery – reported in all the studies – was 7.2%, while the rate for patients who had more than one previous fundoplication was 19%. The most common reason for conversion, reported in 16 studies, was adhesions from previous surgery. The overall 7.2% conversion rate is higher than that noted for primary surgery (3.7%), "but is not excessive given the increased complexity of revision surgery," they commented.
Postoperative complications, reported from 18 studies, occurred in 14%, ranging from 0% to 44%. There were two deaths, both occurring in the same study. Pneumothorax was the most common complication, in 2% (14/810). Mean length of stay, reported in 18 studies, ranged from 1.2 to 6 days. Satisfactory to excellent results were reported for 84% of the operations; 5% of patients had a further antireflux procedure.
While revision laparoscopic fundoplication does not confer excessive morbidity, evidence for the efficacy of this procedure "is far less convincing, mainly owing to the mixture of reporting time points, inconsistency of end point definitions, and methods of assessment between studies. There appears to be a larger proportion of patients undergoing a re-revision surgery than after primary fundoplication," Dr. Symons commented.
The University of Pittsburgh study included patients who underwent minimally invasive reoperative surgery after failed fundoplication from 1996 to 2008. The 275 patients had a median age of 52 years (range 17-88 years), and 11.3% had had more than one prior antireflux surgery. As with the systematic review, the most common presenting symptoms were heartburn (64%) and dysphagia (49.5%). The median time from the prior operation to the redo operation was 36 months.
Transmediastinal migration of the wrap or a recurrent hiatal hernia (64%) were the most common causes of failure of the prior antireflux operation. Esophageal shortening was noted in 43% of patients, and a defect in the crural repair was identified in 4.4%. The most common procedure during reoperation was a Nissen fundoplication with or without a Collis gastroplasty. Nearly all of the redo procedures (93%) were done with a minimally invasive approach. There were eight conversions to open surgery due to extensive adhesions or a recognized intraoperative perforation, Dr. Awais and his associates reported.
Major complications included postoperative leaks in 3.3%; atrial fibrillation in 2%; and bleeding, pulmonary embolism, and Clostridium difficile colitis, each in less than 1%. Reexploration was required in 1.4%, for complications related to leak or bleeding. There was no perioperative mortality. Length of stay ranged from 1 to 75 days (median 3 days).
During follow-up of up to 14.5 years (median 3.3 years), 11.3% had a failure of the redo operation, requiring surgical intervention. An esophagectomy was required in four patients. The estimated probability of freedom from failure was 95% at 1 year, 93% at 2 years, and 84% at 5 years. Age and partial fundoplication were significantly associated with failure of the redo operation. and there was a trend for multiple redo operations to be associated with failure, Dr. Awais and his associates said.
Dysphagia decreased significantly after the redo procedure in 135 patients, with dysphagia scores declining from 2.7 to 1.4. Scores on the GERD-Health Related Quality of Life questionnaire, available in 186 patients, were excellent in 52% and satisfactory in 33%.
Both Dr. Symons and Dr. Awais stated that they had no disclosures.
Reoperation for failed antireflux surgery can be performed safely in experienced centers, but outcomes are not as good as with primary operations, according to the results of two new analyses.
Dr. Nicholas R.A. Symons of Imperial College, London, and his associates performed a systematic literature review of 20 studies comprising 930 operations in 922 patients. "We can conclude that laparoscopic revision antireflux surgery, when performed in units with an interest in this type of surgery, is feasible and safe but subject to somewhat greater risk of conversion, higher morbidity, longer hospital stay, and poorer outcomes than primary laparoscopic fundoplication," the researchers said (Am. J. Surg. 2011;202:336-43).
Similarly, based on their retrospective study of 275 patients, Dr. Omar Awais of the University of Pittsburgh and his associates said, "Redo antireflux surgery can be performed safely in experienced centers, and as expected, the outcomes after redo antireflux surgery are not as good as [those of] first-time procedures. The operative approach depends on the underlying cause of failure" (Ann. Thorac. Surg. 2011;92:1083-90).
Between 2.8% and 4.4% of patients who undergo laparoscopic fundoplication at a specialist center will require late reoperation for persistent or recurrent symptoms, and there may be an increased revision rate after primary laparoscopic antireflux surgery compared with an initial open approach. Revision of failed antireflux surgery increasingly is being performed laparoscopically, but data about this approach are limited, Dr. Symons and his associates noted.
Their analysis included 19 case-control series and one prospective case-control study. Patients ranged in age from 13 to 83 years, and 57% were female. Of the eight articles in which the mean time between initial fundoplication and revision was given, the mean interval was 45.5 months (range 2-360 months). Of 12 studies noting the number of previous fundoplications the patients had undergone, 47 procedures (6.9%) were second reoperations and 9 (1.3%) were third reoperations.
Of the 18 studies documenting the type of initial surgery, 62% were laparoscopic, 35% were performed via laparotomy, 3% via thoracotomy, and 0.2% using video-assisted thoracoscopic surgery. Nissen fundoplication and Toupet partial fundoplication were the most common initial and revision procedures. Reflux/heartburn, experienced by 61% of patients, and dysphagia in 31% were the most common indications for laparoscopic reoperation, the investigators reported. Surgical duration, reported in 13 of the case series had an overall mean of 166 minutes for 721 patients.
The overall rate of conversion from laparoscopic reoperation to open surgery – reported in all the studies – was 7.2%, while the rate for patients who had more than one previous fundoplication was 19%. The most common reason for conversion, reported in 16 studies, was adhesions from previous surgery. The overall 7.2% conversion rate is higher than that noted for primary surgery (3.7%), "but is not excessive given the increased complexity of revision surgery," they commented.
Postoperative complications, reported from 18 studies, occurred in 14%, ranging from 0% to 44%. There were two deaths, both occurring in the same study. Pneumothorax was the most common complication, in 2% (14/810). Mean length of stay, reported in 18 studies, ranged from 1.2 to 6 days. Satisfactory to excellent results were reported for 84% of the operations; 5% of patients had a further antireflux procedure.
While revision laparoscopic fundoplication does not confer excessive morbidity, evidence for the efficacy of this procedure "is far less convincing, mainly owing to the mixture of reporting time points, inconsistency of end point definitions, and methods of assessment between studies. There appears to be a larger proportion of patients undergoing a re-revision surgery than after primary fundoplication," Dr. Symons commented.
The University of Pittsburgh study included patients who underwent minimally invasive reoperative surgery after failed fundoplication from 1996 to 2008. The 275 patients had a median age of 52 years (range 17-88 years), and 11.3% had had more than one prior antireflux surgery. As with the systematic review, the most common presenting symptoms were heartburn (64%) and dysphagia (49.5%). The median time from the prior operation to the redo operation was 36 months.
Transmediastinal migration of the wrap or a recurrent hiatal hernia (64%) were the most common causes of failure of the prior antireflux operation. Esophageal shortening was noted in 43% of patients, and a defect in the crural repair was identified in 4.4%. The most common procedure during reoperation was a Nissen fundoplication with or without a Collis gastroplasty. Nearly all of the redo procedures (93%) were done with a minimally invasive approach. There were eight conversions to open surgery due to extensive adhesions or a recognized intraoperative perforation, Dr. Awais and his associates reported.
Major complications included postoperative leaks in 3.3%; atrial fibrillation in 2%; and bleeding, pulmonary embolism, and Clostridium difficile colitis, each in less than 1%. Reexploration was required in 1.4%, for complications related to leak or bleeding. There was no perioperative mortality. Length of stay ranged from 1 to 75 days (median 3 days).
During follow-up of up to 14.5 years (median 3.3 years), 11.3% had a failure of the redo operation, requiring surgical intervention. An esophagectomy was required in four patients. The estimated probability of freedom from failure was 95% at 1 year, 93% at 2 years, and 84% at 5 years. Age and partial fundoplication were significantly associated with failure of the redo operation. and there was a trend for multiple redo operations to be associated with failure, Dr. Awais and his associates said.
Dysphagia decreased significantly after the redo procedure in 135 patients, with dysphagia scores declining from 2.7 to 1.4. Scores on the GERD-Health Related Quality of Life questionnaire, available in 186 patients, were excellent in 52% and satisfactory in 33%.
Both Dr. Symons and Dr. Awais stated that they had no disclosures.
Reoperation for failed antireflux surgery can be performed safely in experienced centers, but outcomes are not as good as with primary operations, according to the results of two new analyses.
Dr. Nicholas R.A. Symons of Imperial College, London, and his associates performed a systematic literature review of 20 studies comprising 930 operations in 922 patients. "We can conclude that laparoscopic revision antireflux surgery, when performed in units with an interest in this type of surgery, is feasible and safe but subject to somewhat greater risk of conversion, higher morbidity, longer hospital stay, and poorer outcomes than primary laparoscopic fundoplication," the researchers said (Am. J. Surg. 2011;202:336-43).
Similarly, based on their retrospective study of 275 patients, Dr. Omar Awais of the University of Pittsburgh and his associates said, "Redo antireflux surgery can be performed safely in experienced centers, and as expected, the outcomes after redo antireflux surgery are not as good as [those of] first-time procedures. The operative approach depends on the underlying cause of failure" (Ann. Thorac. Surg. 2011;92:1083-90).
Between 2.8% and 4.4% of patients who undergo laparoscopic fundoplication at a specialist center will require late reoperation for persistent or recurrent symptoms, and there may be an increased revision rate after primary laparoscopic antireflux surgery compared with an initial open approach. Revision of failed antireflux surgery increasingly is being performed laparoscopically, but data about this approach are limited, Dr. Symons and his associates noted.
Their analysis included 19 case-control series and one prospective case-control study. Patients ranged in age from 13 to 83 years, and 57% were female. Of the eight articles in which the mean time between initial fundoplication and revision was given, the mean interval was 45.5 months (range 2-360 months). Of 12 studies noting the number of previous fundoplications the patients had undergone, 47 procedures (6.9%) were second reoperations and 9 (1.3%) were third reoperations.
Of the 18 studies documenting the type of initial surgery, 62% were laparoscopic, 35% were performed via laparotomy, 3% via thoracotomy, and 0.2% using video-assisted thoracoscopic surgery. Nissen fundoplication and Toupet partial fundoplication were the most common initial and revision procedures. Reflux/heartburn, experienced by 61% of patients, and dysphagia in 31% were the most common indications for laparoscopic reoperation, the investigators reported. Surgical duration, reported in 13 of the case series had an overall mean of 166 minutes for 721 patients.
The overall rate of conversion from laparoscopic reoperation to open surgery – reported in all the studies – was 7.2%, while the rate for patients who had more than one previous fundoplication was 19%. The most common reason for conversion, reported in 16 studies, was adhesions from previous surgery. The overall 7.2% conversion rate is higher than that noted for primary surgery (3.7%), "but is not excessive given the increased complexity of revision surgery," they commented.
Postoperative complications, reported from 18 studies, occurred in 14%, ranging from 0% to 44%. There were two deaths, both occurring in the same study. Pneumothorax was the most common complication, in 2% (14/810). Mean length of stay, reported in 18 studies, ranged from 1.2 to 6 days. Satisfactory to excellent results were reported for 84% of the operations; 5% of patients had a further antireflux procedure.
While revision laparoscopic fundoplication does not confer excessive morbidity, evidence for the efficacy of this procedure "is far less convincing, mainly owing to the mixture of reporting time points, inconsistency of end point definitions, and methods of assessment between studies. There appears to be a larger proportion of patients undergoing a re-revision surgery than after primary fundoplication," Dr. Symons commented.
The University of Pittsburgh study included patients who underwent minimally invasive reoperative surgery after failed fundoplication from 1996 to 2008. The 275 patients had a median age of 52 years (range 17-88 years), and 11.3% had had more than one prior antireflux surgery. As with the systematic review, the most common presenting symptoms were heartburn (64%) and dysphagia (49.5%). The median time from the prior operation to the redo operation was 36 months.
Transmediastinal migration of the wrap or a recurrent hiatal hernia (64%) were the most common causes of failure of the prior antireflux operation. Esophageal shortening was noted in 43% of patients, and a defect in the crural repair was identified in 4.4%. The most common procedure during reoperation was a Nissen fundoplication with or without a Collis gastroplasty. Nearly all of the redo procedures (93%) were done with a minimally invasive approach. There were eight conversions to open surgery due to extensive adhesions or a recognized intraoperative perforation, Dr. Awais and his associates reported.
Major complications included postoperative leaks in 3.3%; atrial fibrillation in 2%; and bleeding, pulmonary embolism, and Clostridium difficile colitis, each in less than 1%. Reexploration was required in 1.4%, for complications related to leak or bleeding. There was no perioperative mortality. Length of stay ranged from 1 to 75 days (median 3 days).
During follow-up of up to 14.5 years (median 3.3 years), 11.3% had a failure of the redo operation, requiring surgical intervention. An esophagectomy was required in four patients. The estimated probability of freedom from failure was 95% at 1 year, 93% at 2 years, and 84% at 5 years. Age and partial fundoplication were significantly associated with failure of the redo operation. and there was a trend for multiple redo operations to be associated with failure, Dr. Awais and his associates said.
Dysphagia decreased significantly after the redo procedure in 135 patients, with dysphagia scores declining from 2.7 to 1.4. Scores on the GERD-Health Related Quality of Life questionnaire, available in 186 patients, were excellent in 52% and satisfactory in 33%.
Both Dr. Symons and Dr. Awais stated that they had no disclosures.
Rigid Plating Speeds Sternal Healing
COLORADO SPRINGS – Rigid fixation with sternal plates resulted in superior sternal bone healing post sternotomy, compared with conventional wire cerclage in a randomized trial.
This was the first-ever randomized study to utilize CT scans to objectively assess sternal union. The results at 6 months of follow-up showed a striking advantage for rigid plate fixation using the proprietary SternaLock system, Dr. Jaishankar Raman said at the annual meeting of the Western Thoracic Surgical Association.
Most cardiac surgeons will be surprised, as was he, at how low the sternal union rates were 3 months poststernotomy. In fact, the sternal union rate then with conventional wire closure was zero, while for sternal plating it was 17%, added Dr. Raman of the University of Chicago.
He reported on 141 randomized cardiac surgery patients at six centers in the United States and Germany. All were at high risk for sternal wound complications, mostly due to multiple comorbid diseases. Their multilevel CT scans obtained at 3 or 6 months post surgery were independently scored in structured fashion by two independent radiologists at a core imaging center.
At 6 months, sternal union, or osteosynthesis – as defined by a CT score of 3 or more – was achieved in 70% of the rigid plate fixation group, compared with 20% of those with conventional wire cerclage.
There were no significant differences between the two study arms in rates of wound dehiscence or other adverse events.
Asked about the cost of SternaLock fixation, Dr. Raman replied, "That’s the biggest stumbling block in developing this technology."
The wire for conventional cerclage costs less than $50 per patient. In contrast, the SternaLock system costs about $1,000 per patient. It could be argued that if rigid plate fixation reduces the incidence of sternal wound complications in high-risk patients, the advanced technology would be cost effective. However, the randomized trial wasn’t powered to show a significant difference in such complications.
Dr. Raman observed that wire cerclage has been accepted as the time-honored and most widely employed means of sternal closure ever since the modern era of cardiac surgery began back in the 1950s, even though it is a crude method.
"Even though we may not like it, we in cardiac surgery do more bone approximation and bone fixation than most other bone-handling surgeons. Yet all other bone-handling surgeons have moved on to plate and screw fixation. Biomechanical studies show that plate fixation is significantly better than wire closure," according to the surgeon.
Discussant Dr. Matthew S. Slater, clinical director of adult cardiac surgery at Oregon Health & Sciences Center, Portland, said that based on the assumption that rigid plate fixation is a better method than conventional wire cerclage, what he’d really like to see next is a comparative study pitting the SternaLock system against other novel fixation technologies on the market, such as KLS Martin’s Sternal Talon and ACUTE Innovations’ AcuTie.
Dr. Raman agreed that would be a logical next step, adding that it’s his strong impression the industry is not interested in funding comparative trials.
He declared that he received a research grant from Biomet Microfixation, which markets the SternaLock and funded the randomized trial.
COLORADO SPRINGS – Rigid fixation with sternal plates resulted in superior sternal bone healing post sternotomy, compared with conventional wire cerclage in a randomized trial.
This was the first-ever randomized study to utilize CT scans to objectively assess sternal union. The results at 6 months of follow-up showed a striking advantage for rigid plate fixation using the proprietary SternaLock system, Dr. Jaishankar Raman said at the annual meeting of the Western Thoracic Surgical Association.
Most cardiac surgeons will be surprised, as was he, at how low the sternal union rates were 3 months poststernotomy. In fact, the sternal union rate then with conventional wire closure was zero, while for sternal plating it was 17%, added Dr. Raman of the University of Chicago.
He reported on 141 randomized cardiac surgery patients at six centers in the United States and Germany. All were at high risk for sternal wound complications, mostly due to multiple comorbid diseases. Their multilevel CT scans obtained at 3 or 6 months post surgery were independently scored in structured fashion by two independent radiologists at a core imaging center.
At 6 months, sternal union, or osteosynthesis – as defined by a CT score of 3 or more – was achieved in 70% of the rigid plate fixation group, compared with 20% of those with conventional wire cerclage.
There were no significant differences between the two study arms in rates of wound dehiscence or other adverse events.
Asked about the cost of SternaLock fixation, Dr. Raman replied, "That’s the biggest stumbling block in developing this technology."
The wire for conventional cerclage costs less than $50 per patient. In contrast, the SternaLock system costs about $1,000 per patient. It could be argued that if rigid plate fixation reduces the incidence of sternal wound complications in high-risk patients, the advanced technology would be cost effective. However, the randomized trial wasn’t powered to show a significant difference in such complications.
Dr. Raman observed that wire cerclage has been accepted as the time-honored and most widely employed means of sternal closure ever since the modern era of cardiac surgery began back in the 1950s, even though it is a crude method.
"Even though we may not like it, we in cardiac surgery do more bone approximation and bone fixation than most other bone-handling surgeons. Yet all other bone-handling surgeons have moved on to plate and screw fixation. Biomechanical studies show that plate fixation is significantly better than wire closure," according to the surgeon.
Discussant Dr. Matthew S. Slater, clinical director of adult cardiac surgery at Oregon Health & Sciences Center, Portland, said that based on the assumption that rigid plate fixation is a better method than conventional wire cerclage, what he’d really like to see next is a comparative study pitting the SternaLock system against other novel fixation technologies on the market, such as KLS Martin’s Sternal Talon and ACUTE Innovations’ AcuTie.
Dr. Raman agreed that would be a logical next step, adding that it’s his strong impression the industry is not interested in funding comparative trials.
He declared that he received a research grant from Biomet Microfixation, which markets the SternaLock and funded the randomized trial.
COLORADO SPRINGS – Rigid fixation with sternal plates resulted in superior sternal bone healing post sternotomy, compared with conventional wire cerclage in a randomized trial.
This was the first-ever randomized study to utilize CT scans to objectively assess sternal union. The results at 6 months of follow-up showed a striking advantage for rigid plate fixation using the proprietary SternaLock system, Dr. Jaishankar Raman said at the annual meeting of the Western Thoracic Surgical Association.
Most cardiac surgeons will be surprised, as was he, at how low the sternal union rates were 3 months poststernotomy. In fact, the sternal union rate then with conventional wire closure was zero, while for sternal plating it was 17%, added Dr. Raman of the University of Chicago.
He reported on 141 randomized cardiac surgery patients at six centers in the United States and Germany. All were at high risk for sternal wound complications, mostly due to multiple comorbid diseases. Their multilevel CT scans obtained at 3 or 6 months post surgery were independently scored in structured fashion by two independent radiologists at a core imaging center.
At 6 months, sternal union, or osteosynthesis – as defined by a CT score of 3 or more – was achieved in 70% of the rigid plate fixation group, compared with 20% of those with conventional wire cerclage.
There were no significant differences between the two study arms in rates of wound dehiscence or other adverse events.
Asked about the cost of SternaLock fixation, Dr. Raman replied, "That’s the biggest stumbling block in developing this technology."
The wire for conventional cerclage costs less than $50 per patient. In contrast, the SternaLock system costs about $1,000 per patient. It could be argued that if rigid plate fixation reduces the incidence of sternal wound complications in high-risk patients, the advanced technology would be cost effective. However, the randomized trial wasn’t powered to show a significant difference in such complications.
Dr. Raman observed that wire cerclage has been accepted as the time-honored and most widely employed means of sternal closure ever since the modern era of cardiac surgery began back in the 1950s, even though it is a crude method.
"Even though we may not like it, we in cardiac surgery do more bone approximation and bone fixation than most other bone-handling surgeons. Yet all other bone-handling surgeons have moved on to plate and screw fixation. Biomechanical studies show that plate fixation is significantly better than wire closure," according to the surgeon.
Discussant Dr. Matthew S. Slater, clinical director of adult cardiac surgery at Oregon Health & Sciences Center, Portland, said that based on the assumption that rigid plate fixation is a better method than conventional wire cerclage, what he’d really like to see next is a comparative study pitting the SternaLock system against other novel fixation technologies on the market, such as KLS Martin’s Sternal Talon and ACUTE Innovations’ AcuTie.
Dr. Raman agreed that would be a logical next step, adding that it’s his strong impression the industry is not interested in funding comparative trials.
He declared that he received a research grant from Biomet Microfixation, which markets the SternaLock and funded the randomized trial.
Major Finding: At 6 months, sternal union, or osteosynthesis – as defined by a CT score of 3 or more – was achieved in 70% of the rigid plate fixation group, compared with 20% who had conventional wire cerclage.
Data Source: A 141-patient multicenter randomized trial.
Disclosures: Dr. Raman received a research grant from Biomet Microfixation, which markets the SternaLock and funded the randomized trial.