User login
Hospitalists’ EMR frustrations continue: SHM report
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
LAS VEGAS – Ronald Schaefer, MD, a hospitalist with Hawaii Pacific Health who also works on creating digital templates for his hospital, can’t input hemoglobin A1c levels from three different labs into his electronic medical records (EMR) system the same way.
Hospitalist George Dimitriou, MD, FHM, who splits his time at Allegheny Health Network in Pittsburgh between clinical work and medical informatics, worries there are so many fields in his EMR that physicians can get distracted.
Yevgeniy “Eugene” Gitelman, MD, a clinical informatics manager at the Perelman School of Medicine at University of Pennsylvania Health in Philadelphia, wonders how good any systems can be with the privacy concerns related to HIPAA.
This was the nexus of IT and HM17, a time when hospitalists said they are stymied and frustrated by continuing issues of interoperability, functionality, and access. The meeting highlighted new smartphone and tablet applications, as well as medical devices available to hospitalists, but tech-focused physicians say the biggest issue remains the day-to-day workings of EMR.
“If you build something really good, people will use it. If you build something that makes their documentation process a lot easier and a lot faster and a lot better, they’ll use it,” said Dr. Schaefer. “The tools aren’t there yet. I don’t think the technology is mature enough.”
If the tech hasn’t yet come of full age, the concerns surely have. SHM unveiled a white paper at HM17 that codified hospitalists’ worries about the current state of IT. The report, “Hospitalist Perspectives on Electronic Medical Records,” found that “a staggering” 85% of providers said they spend more time interacting with their inpatient EMR than their actual inpatients.
Rupesh Prasad, MD, MPH, SFHM, chair of SHM’s Health IT Committee, says the report is meant to foster discussion about the issues surrounding EMRs. The data points, generated from 462 respondents, are stark. Just 40% said they were happy with their EMR. Some 52% would change vendors if they could. One-quarter of respondents would revert to using paper if given the option.
“By sharing these results, we hope to raise awareness of the unacceptable performance of existing systems,” the report states. “This continues to contribute to our slower than desired improvement in quality and safety, as well as increasing provider frustration. We strongly believe that we need a renewed focus on initial goals of technology adoption in health care.”
Dr. Prasad said that he hopes hospitalists heed that call to action and use the report in discussions with various stakeholders, including vendors, public policy officials, and their own bosses.
“We want to give hospitalists ammunition to go back to their systems and talk to their administrators to see if they can influence [it],” he said.
Dr. Prasad is pleased that the society is sensitive to the issues surrounding technology. He encourages hospitalists to actively participate in HMX, SHM’s online portal to discuss health IT issues and crowd-source potential solutions. Patrick Vulgamore, MPH, SHM’s director of governance and practice management, said the society is formulating a potential special-interest working group to further seek to solve problems.
Hospitalists were also urged to apply for American Board of Medical Specialties (ABMS) certification in clinical informatics. Physicians can grandfather into eligibility via the “practice pathway” through the end of the year, if they’ve been working in informatics professionally for at least 25% of their time during any three of the previous five years. Next year, only graduates of two-year Accreditation Council for Graduate Medical Education–accredited fellowships will be board eligible.
“As end users of technology, we understand the problems better than anybody else,” Dr. Prasad said. “Obviously, the next step would be try to solve the problems. And what better way then to get involved and become experts in what you do?”
While much of the meeting’s tech talk was frustration, both former National Coordinator for Health IT Karen DeSalvo, MD, MPH, MSc, and HM Dean Robert Wachter, MD, MHM, forecast a future when artificial intelligence and intuitive computers work alongside physicians. Imagine the user-friendliness of Apple’s Siri or Google’s Alexa married to the existing functionalities provided by firms such as Epic or Cerner.
But that’s years away, and hospitalists like Dr. Dimitriou want help now.
“The speed of medicine, the speed of what’s happening in real time, is still faster than what our electronic tools seem to be able to keep up with,” he said. “There are encouraging signs that we’ve definitely moved in the right direction. We’ve come a long way ... but again, the speed at which things are moving? We aren’t keeping up. We’ve got to do more.”
Nontraditional med student hopes to bridge common understanding gaps in health care
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ryan Gamlin, a nontraditional student at the University of Cincinnati College of Medicine. Ryan was chosen to present his scientific abstract at SHM’s annual meeting in 2016, and encourages medical students to utilize SHM’s resources.
Tell TH about your unique pathway to medical school. How did you become an SHM member?
After 10 years working for and consulting to large health insurance companies, I was increasingly disillusioned with my work and the insurance industry and began feeling restless. When I considered possible avenues to help improve health and the health care delivery system, nothing held more intellectual or professional appeal than working on problems from the inside as a physician.
This effort to bridge these constituencies was my introduction to SHM. I was fortunate enough to be selected for the Health Innovations Scholars Program (HISP), an incredible quality improvement (QI) and leadership development program run by the hospital medicine group at University of Colorado. Conceived by Jeff Glasheen, MD, and now led by Read Pierce, MD, and Emily Gottenborg, MD, among many others, HISP brings eight medical students together to grow their QI toolkit and build leadership skills while providing the opportunity to design and run a meaningful QI project at the University of Colorado’s Anschutz medical campus. Many involved with this program – and others within the hospital medicine group at the University of Colorado – are leaders within SHM. With their encouragement, I submitted an abstract based on our HISP project and had the good fortune to share our work as a podium presentation at Hospital Medicine 2016 in San Diego.
Describe your experience at your first annual meeting. Why would you encourage medical students to attend?
Hospital Medicine 2016 inspired me. As someone interested in the intersection of clinical care and the care system itself, I was amazed at the depth and breadth of forward-looking programming and the amount of similarly-inclined people!
I wish that every medical student – irrespective of their intended specialty – could attend an SHM meeting to witness firsthand how a progressive, thriving professional society integrates members at all levels (student, resident, early-career faculty, and beyond) into their work of improving health care.
As a medical student, why is SHM beneficial to your professional growth as a future physician?
I see SHM as a “big tent” professional society that values insights and expertise from all types of physicians, with tangible commitments to support them in the types of system-improving work that are important to me in my career. SHM’s member resources and commitment to students’ and residents’ professional development are incomparable.
What are the biggest opportunities you see for yourself and other future physicians in the changing health care landscape?
The days when a physician’s job was limited to doctoring are over. Our generation of physicians must be great clinicians and work to heal a sick health care system. Now more than ever, physicians must be systems thinkers, designers, and fixers, equipped with the tools of quality improvement, design thinking, finance, and health policy.
Opportunities for meaningful improvement exist at every level, from care teams to health systems, the health care industry, and policy at every level. I would encourage those at any stage of their careers to find an area that they’re excited about or interested in. Seek out information and mentors in that area at their institutions or within SHM, and just start working on something.
There is a tremendous amount of uncertainty in health care; reimbursement paradigms are changing, clinical expectations only grow, and the forces competing for every doctor’s limited time seem unlimited. Uncertainty is uncomfortable, but it also means opportunity. I’m excited to see the commitment to leadership from SHM and so many of its members. It has never been more necessary.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ryan Gamlin, a nontraditional student at the University of Cincinnati College of Medicine. Ryan was chosen to present his scientific abstract at SHM’s annual meeting in 2016, and encourages medical students to utilize SHM’s resources.
Tell TH about your unique pathway to medical school. How did you become an SHM member?
After 10 years working for and consulting to large health insurance companies, I was increasingly disillusioned with my work and the insurance industry and began feeling restless. When I considered possible avenues to help improve health and the health care delivery system, nothing held more intellectual or professional appeal than working on problems from the inside as a physician.
This effort to bridge these constituencies was my introduction to SHM. I was fortunate enough to be selected for the Health Innovations Scholars Program (HISP), an incredible quality improvement (QI) and leadership development program run by the hospital medicine group at University of Colorado. Conceived by Jeff Glasheen, MD, and now led by Read Pierce, MD, and Emily Gottenborg, MD, among many others, HISP brings eight medical students together to grow their QI toolkit and build leadership skills while providing the opportunity to design and run a meaningful QI project at the University of Colorado’s Anschutz medical campus. Many involved with this program – and others within the hospital medicine group at the University of Colorado – are leaders within SHM. With their encouragement, I submitted an abstract based on our HISP project and had the good fortune to share our work as a podium presentation at Hospital Medicine 2016 in San Diego.
Describe your experience at your first annual meeting. Why would you encourage medical students to attend?
Hospital Medicine 2016 inspired me. As someone interested in the intersection of clinical care and the care system itself, I was amazed at the depth and breadth of forward-looking programming and the amount of similarly-inclined people!
I wish that every medical student – irrespective of their intended specialty – could attend an SHM meeting to witness firsthand how a progressive, thriving professional society integrates members at all levels (student, resident, early-career faculty, and beyond) into their work of improving health care.
As a medical student, why is SHM beneficial to your professional growth as a future physician?
I see SHM as a “big tent” professional society that values insights and expertise from all types of physicians, with tangible commitments to support them in the types of system-improving work that are important to me in my career. SHM’s member resources and commitment to students’ and residents’ professional development are incomparable.
What are the biggest opportunities you see for yourself and other future physicians in the changing health care landscape?
The days when a physician’s job was limited to doctoring are over. Our generation of physicians must be great clinicians and work to heal a sick health care system. Now more than ever, physicians must be systems thinkers, designers, and fixers, equipped with the tools of quality improvement, design thinking, finance, and health policy.
Opportunities for meaningful improvement exist at every level, from care teams to health systems, the health care industry, and policy at every level. I would encourage those at any stage of their careers to find an area that they’re excited about or interested in. Seek out information and mentors in that area at their institutions or within SHM, and just start working on something.
There is a tremendous amount of uncertainty in health care; reimbursement paradigms are changing, clinical expectations only grow, and the forces competing for every doctor’s limited time seem unlimited. Uncertainty is uncomfortable, but it also means opportunity. I’m excited to see the commitment to leadership from SHM and so many of its members. It has never been more necessary.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ryan Gamlin, a nontraditional student at the University of Cincinnati College of Medicine. Ryan was chosen to present his scientific abstract at SHM’s annual meeting in 2016, and encourages medical students to utilize SHM’s resources.
Tell TH about your unique pathway to medical school. How did you become an SHM member?
After 10 years working for and consulting to large health insurance companies, I was increasingly disillusioned with my work and the insurance industry and began feeling restless. When I considered possible avenues to help improve health and the health care delivery system, nothing held more intellectual or professional appeal than working on problems from the inside as a physician.
This effort to bridge these constituencies was my introduction to SHM. I was fortunate enough to be selected for the Health Innovations Scholars Program (HISP), an incredible quality improvement (QI) and leadership development program run by the hospital medicine group at University of Colorado. Conceived by Jeff Glasheen, MD, and now led by Read Pierce, MD, and Emily Gottenborg, MD, among many others, HISP brings eight medical students together to grow their QI toolkit and build leadership skills while providing the opportunity to design and run a meaningful QI project at the University of Colorado’s Anschutz medical campus. Many involved with this program – and others within the hospital medicine group at the University of Colorado – are leaders within SHM. With their encouragement, I submitted an abstract based on our HISP project and had the good fortune to share our work as a podium presentation at Hospital Medicine 2016 in San Diego.
Describe your experience at your first annual meeting. Why would you encourage medical students to attend?
Hospital Medicine 2016 inspired me. As someone interested in the intersection of clinical care and the care system itself, I was amazed at the depth and breadth of forward-looking programming and the amount of similarly-inclined people!
I wish that every medical student – irrespective of their intended specialty – could attend an SHM meeting to witness firsthand how a progressive, thriving professional society integrates members at all levels (student, resident, early-career faculty, and beyond) into their work of improving health care.
As a medical student, why is SHM beneficial to your professional growth as a future physician?
I see SHM as a “big tent” professional society that values insights and expertise from all types of physicians, with tangible commitments to support them in the types of system-improving work that are important to me in my career. SHM’s member resources and commitment to students’ and residents’ professional development are incomparable.
What are the biggest opportunities you see for yourself and other future physicians in the changing health care landscape?
The days when a physician’s job was limited to doctoring are over. Our generation of physicians must be great clinicians and work to heal a sick health care system. Now more than ever, physicians must be systems thinkers, designers, and fixers, equipped with the tools of quality improvement, design thinking, finance, and health policy.
Opportunities for meaningful improvement exist at every level, from care teams to health systems, the health care industry, and policy at every level. I would encourage those at any stage of their careers to find an area that they’re excited about or interested in. Seek out information and mentors in that area at their institutions or within SHM, and just start working on something.
There is a tremendous amount of uncertainty in health care; reimbursement paradigms are changing, clinical expectations only grow, and the forces competing for every doctor’s limited time seem unlimited. Uncertainty is uncomfortable, but it also means opportunity. I’m excited to see the commitment to leadership from SHM and so many of its members. It has never been more necessary.
Felicia Steele is SHM’s communications coordinator.
VIDEO: NPs, PAs weigh common issues in hospitalist practice
Practicing at the top of your license, billing and reimbursement, recruiting and orientation – Those were some of the hot topics discussed by more than 50 attendees of HM17’s Special Interest Forum for nurse practitioners (NPs) and physician assistants (PAs).
“Every year, we are seeing more and more HM groups integrating NPs and PAs into their practice,” said forum moderator Emilie Thornhill, PA-C, a certified PA, who works for Oschner Health in New Orleans, La.
Ms. Thornhill emphasized that a common issue among attendees is restrictive HM policies in dictating the scope of practice for NP/PAs in hospitalist groups.
“That seems to be the thing that is holding us back the most,” she said. “SHM is really going to be the home for these individuals to find the resources they need to address these issues.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Practicing at the top of your license, billing and reimbursement, recruiting and orientation – Those were some of the hot topics discussed by more than 50 attendees of HM17’s Special Interest Forum for nurse practitioners (NPs) and physician assistants (PAs).
“Every year, we are seeing more and more HM groups integrating NPs and PAs into their practice,” said forum moderator Emilie Thornhill, PA-C, a certified PA, who works for Oschner Health in New Orleans, La.
Ms. Thornhill emphasized that a common issue among attendees is restrictive HM policies in dictating the scope of practice for NP/PAs in hospitalist groups.
“That seems to be the thing that is holding us back the most,” she said. “SHM is really going to be the home for these individuals to find the resources they need to address these issues.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Practicing at the top of your license, billing and reimbursement, recruiting and orientation – Those were some of the hot topics discussed by more than 50 attendees of HM17’s Special Interest Forum for nurse practitioners (NPs) and physician assistants (PAs).
“Every year, we are seeing more and more HM groups integrating NPs and PAs into their practice,” said forum moderator Emilie Thornhill, PA-C, a certified PA, who works for Oschner Health in New Orleans, La.
Ms. Thornhill emphasized that a common issue among attendees is restrictive HM policies in dictating the scope of practice for NP/PAs in hospitalist groups.
“That seems to be the thing that is holding us back the most,” she said. “SHM is really going to be the home for these individuals to find the resources they need to address these issues.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Connect: Community hospitalists brainstorm ways to be stronger as a group
Coping with disjointed administrative goals, demonstrating value to hospital leadership, and strengthening support networks for one another were hot-button topics during the Special Interest Group for Community Hospitalists at this year’s HM17.
A mix of hospitalists from rural, urban, and suburban facilities with an average 200-500 beds joined in the discussion, moderated by Stephen Behnke, MD, an internist and president of MedOne in Columbus, Ohio, and Jason Robertson, MD, an internist with HealthPartners in Bloomington, Minn.
Burnout was seen by several in the crowd of about two dozen physicians as being related in part to poor staffing and scheduling decisions at the administrative level, and not allocating clerical work to other staff, often forcing hospitalists to perform tasks not at the top of their license. One solution offered was to amortize the cost of physicians doing paperwork according to their salaries, and to bring those numbers to the attention of hospital leadership.
The group called on the Society of Hospital Medicine to create and disseminate evidence-based resources to help demonstrate their value to hospital administration. Many in the group expressed interest in learning how to communicate their value effectively to their respective C-suites to underscore the essential nature HM has to the core business. In an interview directly after the session, Dr. Behnke explained that hospital leaders often underfund HM programs, only to find that the decision ends up costing them more in the long run.
Lots of upset was vented by session attendees over patient discharge protocols that often resulted in higher lengths of stay or increased readmissions, which then reflected poorly on the hospitalist. The group agreed that since there was no one-size-fits-all approach to this, it would be helpful to start a listserv of community hospitalists in the SHM that was organized by hospital size, location, and types of staffing, so it would be easier to find solutions by connecting with others with similar concerns.
Many in the group also shared how their respective facilities promoted wellness through togetherness activities: staff retreats, movie nights, book clubs, group family outings, and forming alliances with hospitalists at other local hospitals. The general consensus was that this helped improve staff morale.
Coping with disjointed administrative goals, demonstrating value to hospital leadership, and strengthening support networks for one another were hot-button topics during the Special Interest Group for Community Hospitalists at this year’s HM17.
A mix of hospitalists from rural, urban, and suburban facilities with an average 200-500 beds joined in the discussion, moderated by Stephen Behnke, MD, an internist and president of MedOne in Columbus, Ohio, and Jason Robertson, MD, an internist with HealthPartners in Bloomington, Minn.
Burnout was seen by several in the crowd of about two dozen physicians as being related in part to poor staffing and scheduling decisions at the administrative level, and not allocating clerical work to other staff, often forcing hospitalists to perform tasks not at the top of their license. One solution offered was to amortize the cost of physicians doing paperwork according to their salaries, and to bring those numbers to the attention of hospital leadership.
The group called on the Society of Hospital Medicine to create and disseminate evidence-based resources to help demonstrate their value to hospital administration. Many in the group expressed interest in learning how to communicate their value effectively to their respective C-suites to underscore the essential nature HM has to the core business. In an interview directly after the session, Dr. Behnke explained that hospital leaders often underfund HM programs, only to find that the decision ends up costing them more in the long run.
Lots of upset was vented by session attendees over patient discharge protocols that often resulted in higher lengths of stay or increased readmissions, which then reflected poorly on the hospitalist. The group agreed that since there was no one-size-fits-all approach to this, it would be helpful to start a listserv of community hospitalists in the SHM that was organized by hospital size, location, and types of staffing, so it would be easier to find solutions by connecting with others with similar concerns.
Many in the group also shared how their respective facilities promoted wellness through togetherness activities: staff retreats, movie nights, book clubs, group family outings, and forming alliances with hospitalists at other local hospitals. The general consensus was that this helped improve staff morale.
Coping with disjointed administrative goals, demonstrating value to hospital leadership, and strengthening support networks for one another were hot-button topics during the Special Interest Group for Community Hospitalists at this year’s HM17.
A mix of hospitalists from rural, urban, and suburban facilities with an average 200-500 beds joined in the discussion, moderated by Stephen Behnke, MD, an internist and president of MedOne in Columbus, Ohio, and Jason Robertson, MD, an internist with HealthPartners in Bloomington, Minn.
Burnout was seen by several in the crowd of about two dozen physicians as being related in part to poor staffing and scheduling decisions at the administrative level, and not allocating clerical work to other staff, often forcing hospitalists to perform tasks not at the top of their license. One solution offered was to amortize the cost of physicians doing paperwork according to their salaries, and to bring those numbers to the attention of hospital leadership.
The group called on the Society of Hospital Medicine to create and disseminate evidence-based resources to help demonstrate their value to hospital administration. Many in the group expressed interest in learning how to communicate their value effectively to their respective C-suites to underscore the essential nature HM has to the core business. In an interview directly after the session, Dr. Behnke explained that hospital leaders often underfund HM programs, only to find that the decision ends up costing them more in the long run.
Lots of upset was vented by session attendees over patient discharge protocols that often resulted in higher lengths of stay or increased readmissions, which then reflected poorly on the hospitalist. The group agreed that since there was no one-size-fits-all approach to this, it would be helpful to start a listserv of community hospitalists in the SHM that was organized by hospital size, location, and types of staffing, so it would be easier to find solutions by connecting with others with similar concerns.
Many in the group also shared how their respective facilities promoted wellness through togetherness activities: staff retreats, movie nights, book clubs, group family outings, and forming alliances with hospitalists at other local hospitals. The general consensus was that this helped improve staff morale.
Highlights of Day 4
Sometimes the final day of a convention is nothing more than the “getaway day.”
But not at HM17. Not this year.
The finale of the 2017 annual meeting is capped off, as has become tradition, by a speech from the dean of hospital medicine: Robert Wachter, MD, MHM. The last time Dr. Wachter gave his address from a Vegas stage, it ended with him in head-to-toe Elton John regalia. While there’s no guarantee of a wardrobe reprisal, the annual address from the man who helped name the specialty promises to entertain and inform, said HM17 course director Lenny Feldman, MD, SFHM.
However, Dr. Wachter’s words – this year titled “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” – aren’t the final day’s only lure.
Two of this year’s newest educational tracks – Health Policy and Medical Education – debut today and offer five courses focusing on niche areas interesting to many hospitalists. Also today is the annual Potpurri track, which highlights off-beat topics such as “Case-Based Approach to Difficult Conversations” and “The History of Medicine: Discoveries that Shaped Our Profession.”
“These sessions are unique but have a wide range of appeal,” Dr. Feldman said. “Attendees are going to have a great time delving into these topics.”
Sometimes the final day of a convention is nothing more than the “getaway day.”
But not at HM17. Not this year.
The finale of the 2017 annual meeting is capped off, as has become tradition, by a speech from the dean of hospital medicine: Robert Wachter, MD, MHM. The last time Dr. Wachter gave his address from a Vegas stage, it ended with him in head-to-toe Elton John regalia. While there’s no guarantee of a wardrobe reprisal, the annual address from the man who helped name the specialty promises to entertain and inform, said HM17 course director Lenny Feldman, MD, SFHM.
However, Dr. Wachter’s words – this year titled “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” – aren’t the final day’s only lure.
Two of this year’s newest educational tracks – Health Policy and Medical Education – debut today and offer five courses focusing on niche areas interesting to many hospitalists. Also today is the annual Potpurri track, which highlights off-beat topics such as “Case-Based Approach to Difficult Conversations” and “The History of Medicine: Discoveries that Shaped Our Profession.”
“These sessions are unique but have a wide range of appeal,” Dr. Feldman said. “Attendees are going to have a great time delving into these topics.”
Sometimes the final day of a convention is nothing more than the “getaway day.”
But not at HM17. Not this year.
The finale of the 2017 annual meeting is capped off, as has become tradition, by a speech from the dean of hospital medicine: Robert Wachter, MD, MHM. The last time Dr. Wachter gave his address from a Vegas stage, it ended with him in head-to-toe Elton John regalia. While there’s no guarantee of a wardrobe reprisal, the annual address from the man who helped name the specialty promises to entertain and inform, said HM17 course director Lenny Feldman, MD, SFHM.
However, Dr. Wachter’s words – this year titled “Planning for the Future in a World of Constant Change: What Should Hospitalists Do?” – aren’t the final day’s only lure.
Two of this year’s newest educational tracks – Health Policy and Medical Education – debut today and offer five courses focusing on niche areas interesting to many hospitalists. Also today is the annual Potpurri track, which highlights off-beat topics such as “Case-Based Approach to Difficult Conversations” and “The History of Medicine: Discoveries that Shaped Our Profession.”
“These sessions are unique but have a wide range of appeal,” Dr. Feldman said. “Attendees are going to have a great time delving into these topics.”
Hospitalist movers and shakers
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Andrew Auerbach, MD, MPH, SFHM, and Vineet Arora, MD, MPP, MHM, recently were elected to the new member class of American Society for Clinical Investigation (ASCI) for 2017. Members must have “accomplished meritorious, original, creative, and independent investigations in the clinical or allied sciences of medicine and enjoy an unimpeachable moral standing in the medical profession.”
Dr. Auerbach and Dr. Arora are just the third and fourth hospitalists to become ASCI members. Dr. Auerbach is the professor of medicine in residence and director of the research division of hospital medicine at the University of California, San Francisco. Dr. Aurora is associate professor of medicine, assistant dean for scholarship and discovery, and director of graduate medical education’s clinical learning environment innovation at the University of Chicago.
Mark V. Williams, MD, FACP, MHM, director of the University of Kentucky’s Center for Health Services Research (CHSR), recently presented at the International Conference of Hospital Medicine held in Taiwan.
Olevia M. Pitts, MD, SFHM, made history at Research Medical Center in Kansas City, becoming the first woman and the first person of color to be named the facility’s chief medical officer. Dr. Pitts assumed her role at the 131-year-old RMC on January 30.
Greta Boynton, MD, SFHM, was promoted to the role of associate chief medical officer of Sound Physicians’ northeast region. She was elevated from her position as regional medical director for Sound Physicians, a health care organization that serves as a provider practice in 225 hospitals in 38 states.
Dr. Boynton will be charged with overseeing clinical operation of 13 programs, 120 providers, and a team of regional medical directors. She joined Sound Physicians in 2013 as chief hospitalist and divisional chief at Baystate Medical Center in Springfield, Mass. She was, previously, chief of hospital medicine for Eastern Connecticut Health Network, Manchester, from 2008-2013.
Business Moves
Sound Physicians, Tacoma, Wash., added to its list of partners on March 1, when Eagle Hospital Medicine Practices, Atlanta, joined the Sound group’s organization. Eagle’s 150 providers in 16 hospitals across the United States raises Sound’s resume to more than 2,500 providers.
Eagle will continue to run its own Locum Connections and Telemedicine divisions.
The Society of Hospital Medicine’s Center for Quality Improvement recently was recognized and honored by the Centers for Medicare & Medicaid Services (CMS) for its patient-safety partnership with CMS. The two entities have maintained a relationship since August 2016.
SHM’s Center for QI has participated in weekly CMS webinars to generate strategies intended to limit opioid use, including SHM’s pilot RADEO – Reducing Adverse Drug Events Related to Opioids – program. In January 2017, CMS contacted SHM to provide best practices for patients receiving opioids and better use data to monitor those patients.
University of Iowa Health Care, Iowa City, and Van Buren County Hospital, Keosauqua, Iowa, have created a partnership, allowing patients at VBCH access to UI hospitalists through a telemedicine connection. The relationship will allow VBCH patients to remain at their local hospital – located 90 minutes from Iowa City – while getting care and treatment advice from UI hospitalists through videoconferencing and a shared electronic health record.
With their VBCH provider bedside, patients meet face-to–virtual face with the UI hospitalist during twice-daily virtual rounding.
Unity Medical Center, Manchester, Tenn., recently partnered with physician-owned and -operated Concord Medical Group, Knoxville, Tenn., to provide hospitalist services at its facility in Manchester. Unity now will have hospitalists on duty 24 hours per day thanks to the relationship with Concord, a hospital management and staffing specialist group.
Here’s what’s trending at SHM
SHM gives QI a new look
SHM is proud to announce that its Center for Hospital Innovation & Improvement has a fresh look and name: SHM’s Center for Quality Improvement. While the name may have changed, SHM’s Center for QI will remain your partner in quality and patient safety.
“SHM’s Center for QI provides a comprehensive set of resources and programs to support hospitalists and other hospital clinicians as they work to improve quality and safety in their hospitals,” says Eric E. Howell, MD, MHM, senior physician advisor for SHM’s Center for QI.
SHM’s Center for QI’s mentored implementation programs are deployed in hundreds of hospitals and have been recognized with the John M. Eisenberg Award. More recently, its opioid-safety program (RADEO) was recognized by the CMS for its efforts to enhance patient safety.
Visit http://www.hospitalmedicine.org/QI to learn more about SHM’s Center for QI and about opportunities for partnerships, solutions, and tools to address your QI needs.
PHM 2017 is coming! Book your ticket to Nashville today
Pediatric Hospital Medicine (PHM) 2017 is the largest, leading educational event for health care professionals who specialize in the care of hospitalized children. This year’s meeting will be held July 20-23 at the Omni Nashville in Tennessee.
Attendees will have the opportunity to network with colleagues from across the nation, learn from renowned faculty from throughout the discipline, and acquire skills, tools, and resources to directly benefit their patients and practice.
PHM 2017 has been designed to provide participants with tools to improve clinical skills and practice, address management issues, lead change and innovation within their institutions, and network with thought leaders to collaborate and learn about new innovations.
View the full meeting schedule, educational objectives, and more at www.peds2017.org.
Benchmark your HMG appropriately with the State of Hospital Medicine Report
The State of Hospital Medicine Report continues to be the best source of detail regarding the configuration and operation of hospital medicine groups. The biennial report provides current data on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
“We’ve used data from the report to hold more informed discussions with the group that provides our note-coding services and to determine how to benchmark our nocturnists’ workloads and pay,” said Andrew White, MD, SFHM, director of the Hospital Medicine Service at the University of Washington in Seattle. “The results are broken into region and academic practice type, which gives me the confidence that I’m looking at results from groups like mine, rather than comparing to the country-wide average.”
The report is designed for hospital medicine leaders (both physician leaders and nonphysician practice administrators and executives), as well as frontline hospitalists, nurse practitioners, physician assistants, pediatricians, and internal and family medicine physicians.
In addition to the print version, the 2016 State of Hospital Medicine Report is also available in an enhanced, fully searchable digital version. To order your copy in either print or digital, visit www.hospitalmedicine.org/survey.
Learn how to drive change as a leader in hospital medicine
A successful hospitalist program requires strong leadership from the floor to the C-suite. SHM’s Leadership Academy prepares clinical and academic leaders with vital skills that, traditionally, are not taught in medical school or typical residency programs. This year’s meeting will be held October 23-26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees, regardless of previous attendance. SHM provides recommendations for interested registrants so they can determine which course fits them best in their leadership journey.
Take the Strategic Essentials course to evaluate your personal leadership strengths and weaknesses, understand key hospital drivers, and more.
If you are looking to learn skills needed to drive culture change through specific leadership behaviors as well as financial storytelling, then Leadership: Influential Management would be a great course for you.
The third course, Leadership: Mastering Teamwork, will help attendees learn to critically assess program growth opportunities, lead and motivate teams, and design effective communication strategies. Learn more at www.shmleadershipacademy.org.
Stay ahead of the MACRA curve with SHM
The Medicare Access and CHIP Reauthorization Act (MACRA) put into motion the new Quality Payment Program, which replaces past pay-for-performance programs, such as the Physician Quality Reporting System and physician value-based modifier. The new program has many complicated requirements, and hospitalists will be impacted.
The first year of the program has flexible participation, yet hospitalists need to do at least one thing (report one quality measure, attest to one improvement activity) in the program in order to avoid a 4% penalty to Medicare payments. 2017 is the first reporting year, so now is the time for providers to familiarize themselves with the requirements.
To support hospitalists who are looking for hospital medicine–specific ways to participate and avoid penalties, SHM hosted a webinar that is now available at www.macraforhm.org under “Resources.” SHM’s policy staff broke down the program requirements and went into detail on ways in which hospitalists can and should participate in the new program. Updates and other resources are also available at www.macraforhm.org.
Looking to be a speaker at Hospital Medicine 2018?
The Society of Hospital Medicine reminds you to submit your workshop proposal for the 2018 Annual Meeting to be held April 8-11, 2018, at the Orlando World Center Marriott. Workshops should involve topics in one of ten categories: clinical, career development, research, academic, patient experience/communication, perioperative, information technology, practice management, quality and patient safety, and evidence‐based medicine/high‐value care. Each workshop should last 90 minutes.
Proposals that are the most likely to be accepted will be innovative as well as highly interactive, utilizing small groups and limiting didactic/lecture content. Workshops previously presented at national or regional meetings will be considered. Four faculty members from each workshop that is accepted will receive 50% off their annual meeting registration, although workshops may include a maximum of six additional facilitators.
The submission deadline is Friday, May 12, 2017 at 8:00 a.m. EST. Visit www.hospitalmedicine2018.org for more information.
Brett Radler is SHM’s communications specialist.
SHM gives QI a new look
SHM is proud to announce that its Center for Hospital Innovation & Improvement has a fresh look and name: SHM’s Center for Quality Improvement. While the name may have changed, SHM’s Center for QI will remain your partner in quality and patient safety.
“SHM’s Center for QI provides a comprehensive set of resources and programs to support hospitalists and other hospital clinicians as they work to improve quality and safety in their hospitals,” says Eric E. Howell, MD, MHM, senior physician advisor for SHM’s Center for QI.
SHM’s Center for QI’s mentored implementation programs are deployed in hundreds of hospitals and have been recognized with the John M. Eisenberg Award. More recently, its opioid-safety program (RADEO) was recognized by the CMS for its efforts to enhance patient safety.
Visit http://www.hospitalmedicine.org/QI to learn more about SHM’s Center for QI and about opportunities for partnerships, solutions, and tools to address your QI needs.
PHM 2017 is coming! Book your ticket to Nashville today
Pediatric Hospital Medicine (PHM) 2017 is the largest, leading educational event for health care professionals who specialize in the care of hospitalized children. This year’s meeting will be held July 20-23 at the Omni Nashville in Tennessee.
Attendees will have the opportunity to network with colleagues from across the nation, learn from renowned faculty from throughout the discipline, and acquire skills, tools, and resources to directly benefit their patients and practice.
PHM 2017 has been designed to provide participants with tools to improve clinical skills and practice, address management issues, lead change and innovation within their institutions, and network with thought leaders to collaborate and learn about new innovations.
View the full meeting schedule, educational objectives, and more at www.peds2017.org.
Benchmark your HMG appropriately with the State of Hospital Medicine Report
The State of Hospital Medicine Report continues to be the best source of detail regarding the configuration and operation of hospital medicine groups. The biennial report provides current data on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
“We’ve used data from the report to hold more informed discussions with the group that provides our note-coding services and to determine how to benchmark our nocturnists’ workloads and pay,” said Andrew White, MD, SFHM, director of the Hospital Medicine Service at the University of Washington in Seattle. “The results are broken into region and academic practice type, which gives me the confidence that I’m looking at results from groups like mine, rather than comparing to the country-wide average.”
The report is designed for hospital medicine leaders (both physician leaders and nonphysician practice administrators and executives), as well as frontline hospitalists, nurse practitioners, physician assistants, pediatricians, and internal and family medicine physicians.
In addition to the print version, the 2016 State of Hospital Medicine Report is also available in an enhanced, fully searchable digital version. To order your copy in either print or digital, visit www.hospitalmedicine.org/survey.
Learn how to drive change as a leader in hospital medicine
A successful hospitalist program requires strong leadership from the floor to the C-suite. SHM’s Leadership Academy prepares clinical and academic leaders with vital skills that, traditionally, are not taught in medical school or typical residency programs. This year’s meeting will be held October 23-26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees, regardless of previous attendance. SHM provides recommendations for interested registrants so they can determine which course fits them best in their leadership journey.
Take the Strategic Essentials course to evaluate your personal leadership strengths and weaknesses, understand key hospital drivers, and more.
If you are looking to learn skills needed to drive culture change through specific leadership behaviors as well as financial storytelling, then Leadership: Influential Management would be a great course for you.
The third course, Leadership: Mastering Teamwork, will help attendees learn to critically assess program growth opportunities, lead and motivate teams, and design effective communication strategies. Learn more at www.shmleadershipacademy.org.
Stay ahead of the MACRA curve with SHM
The Medicare Access and CHIP Reauthorization Act (MACRA) put into motion the new Quality Payment Program, which replaces past pay-for-performance programs, such as the Physician Quality Reporting System and physician value-based modifier. The new program has many complicated requirements, and hospitalists will be impacted.
The first year of the program has flexible participation, yet hospitalists need to do at least one thing (report one quality measure, attest to one improvement activity) in the program in order to avoid a 4% penalty to Medicare payments. 2017 is the first reporting year, so now is the time for providers to familiarize themselves with the requirements.
To support hospitalists who are looking for hospital medicine–specific ways to participate and avoid penalties, SHM hosted a webinar that is now available at www.macraforhm.org under “Resources.” SHM’s policy staff broke down the program requirements and went into detail on ways in which hospitalists can and should participate in the new program. Updates and other resources are also available at www.macraforhm.org.
Looking to be a speaker at Hospital Medicine 2018?
The Society of Hospital Medicine reminds you to submit your workshop proposal for the 2018 Annual Meeting to be held April 8-11, 2018, at the Orlando World Center Marriott. Workshops should involve topics in one of ten categories: clinical, career development, research, academic, patient experience/communication, perioperative, information technology, practice management, quality and patient safety, and evidence‐based medicine/high‐value care. Each workshop should last 90 minutes.
Proposals that are the most likely to be accepted will be innovative as well as highly interactive, utilizing small groups and limiting didactic/lecture content. Workshops previously presented at national or regional meetings will be considered. Four faculty members from each workshop that is accepted will receive 50% off their annual meeting registration, although workshops may include a maximum of six additional facilitators.
The submission deadline is Friday, May 12, 2017 at 8:00 a.m. EST. Visit www.hospitalmedicine2018.org for more information.
Brett Radler is SHM’s communications specialist.
SHM gives QI a new look
SHM is proud to announce that its Center for Hospital Innovation & Improvement has a fresh look and name: SHM’s Center for Quality Improvement. While the name may have changed, SHM’s Center for QI will remain your partner in quality and patient safety.
“SHM’s Center for QI provides a comprehensive set of resources and programs to support hospitalists and other hospital clinicians as they work to improve quality and safety in their hospitals,” says Eric E. Howell, MD, MHM, senior physician advisor for SHM’s Center for QI.
SHM’s Center for QI’s mentored implementation programs are deployed in hundreds of hospitals and have been recognized with the John M. Eisenberg Award. More recently, its opioid-safety program (RADEO) was recognized by the CMS for its efforts to enhance patient safety.
Visit http://www.hospitalmedicine.org/QI to learn more about SHM’s Center for QI and about opportunities for partnerships, solutions, and tools to address your QI needs.
PHM 2017 is coming! Book your ticket to Nashville today
Pediatric Hospital Medicine (PHM) 2017 is the largest, leading educational event for health care professionals who specialize in the care of hospitalized children. This year’s meeting will be held July 20-23 at the Omni Nashville in Tennessee.
Attendees will have the opportunity to network with colleagues from across the nation, learn from renowned faculty from throughout the discipline, and acquire skills, tools, and resources to directly benefit their patients and practice.
PHM 2017 has been designed to provide participants with tools to improve clinical skills and practice, address management issues, lead change and innovation within their institutions, and network with thought leaders to collaborate and learn about new innovations.
View the full meeting schedule, educational objectives, and more at www.peds2017.org.
Benchmark your HMG appropriately with the State of Hospital Medicine Report
The State of Hospital Medicine Report continues to be the best source of detail regarding the configuration and operation of hospital medicine groups. The biennial report provides current data on hospitalist compensation and production, in addition to cutting-edge knowledge covering practice demographics, staffing levels, turnover, staff growth, compensation methods, and financial support for solid, evidence-based management decisions.
“We’ve used data from the report to hold more informed discussions with the group that provides our note-coding services and to determine how to benchmark our nocturnists’ workloads and pay,” said Andrew White, MD, SFHM, director of the Hospital Medicine Service at the University of Washington in Seattle. “The results are broken into region and academic practice type, which gives me the confidence that I’m looking at results from groups like mine, rather than comparing to the country-wide average.”
The report is designed for hospital medicine leaders (both physician leaders and nonphysician practice administrators and executives), as well as frontline hospitalists, nurse practitioners, physician assistants, pediatricians, and internal and family medicine physicians.
In addition to the print version, the 2016 State of Hospital Medicine Report is also available in an enhanced, fully searchable digital version. To order your copy in either print or digital, visit www.hospitalmedicine.org/survey.
Learn how to drive change as a leader in hospital medicine
A successful hospitalist program requires strong leadership from the floor to the C-suite. SHM’s Leadership Academy prepares clinical and academic leaders with vital skills that, traditionally, are not taught in medical school or typical residency programs. This year’s meeting will be held October 23-26 at the JW Marriott Camelback Inn in Scottsdale, Ariz.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees, regardless of previous attendance. SHM provides recommendations for interested registrants so they can determine which course fits them best in their leadership journey.
Take the Strategic Essentials course to evaluate your personal leadership strengths and weaknesses, understand key hospital drivers, and more.
If you are looking to learn skills needed to drive culture change through specific leadership behaviors as well as financial storytelling, then Leadership: Influential Management would be a great course for you.
The third course, Leadership: Mastering Teamwork, will help attendees learn to critically assess program growth opportunities, lead and motivate teams, and design effective communication strategies. Learn more at www.shmleadershipacademy.org.
Stay ahead of the MACRA curve with SHM
The Medicare Access and CHIP Reauthorization Act (MACRA) put into motion the new Quality Payment Program, which replaces past pay-for-performance programs, such as the Physician Quality Reporting System and physician value-based modifier. The new program has many complicated requirements, and hospitalists will be impacted.
The first year of the program has flexible participation, yet hospitalists need to do at least one thing (report one quality measure, attest to one improvement activity) in the program in order to avoid a 4% penalty to Medicare payments. 2017 is the first reporting year, so now is the time for providers to familiarize themselves with the requirements.
To support hospitalists who are looking for hospital medicine–specific ways to participate and avoid penalties, SHM hosted a webinar that is now available at www.macraforhm.org under “Resources.” SHM’s policy staff broke down the program requirements and went into detail on ways in which hospitalists can and should participate in the new program. Updates and other resources are also available at www.macraforhm.org.
Looking to be a speaker at Hospital Medicine 2018?
The Society of Hospital Medicine reminds you to submit your workshop proposal for the 2018 Annual Meeting to be held April 8-11, 2018, at the Orlando World Center Marriott. Workshops should involve topics in one of ten categories: clinical, career development, research, academic, patient experience/communication, perioperative, information technology, practice management, quality and patient safety, and evidence‐based medicine/high‐value care. Each workshop should last 90 minutes.
Proposals that are the most likely to be accepted will be innovative as well as highly interactive, utilizing small groups and limiting didactic/lecture content. Workshops previously presented at national or regional meetings will be considered. Four faculty members from each workshop that is accepted will receive 50% off their annual meeting registration, although workshops may include a maximum of six additional facilitators.
The submission deadline is Friday, May 12, 2017 at 8:00 a.m. EST. Visit www.hospitalmedicine2018.org for more information.
Brett Radler is SHM’s communications specialist.
Hospitalists: Leading health care innovation
As I begin my year as SHM president, I continue to be energized by the opportunity to be part of an organization that has such a positive impact on our nation’s health care system. From the beginning of my medical career to now, never have I witnessed a health care movement quite like hospital medicine.
Even when I first arrived in Southern California as a pulmonary/critical-care physician in 1987, there were groups of physicians who had taken financial risk on populations of managed-care patients and were paid using an “alternative payment model” called capitation. One of the innovations they had utilized since the early ’80s to successfully manage their risk – and their patients’ – was to have dedicated inpatient physicians caring for their hospitalized patients 24/7, while most of their primary care partners managed the group’s patients in the outpatient setting.
This year will see a continued reshaping of our delivery system, driven by emerging federal policy like the Medicare Access and CHIP Reauthorization Act (MACRA). All of this policy is designed to create a health care system that delivers high-quality care in a much more cost effective way. Many of these policies will result in groups of providers being pushed away from fee-for-service payment toward alternative payment models that involve higher levels of risk and opportunity. If we, as providers, are going to be successful in managing our “at risk” populations, we are going to have to be as innovative as our managed care forefathers. If we are not, we, as a society, are not going to be able to afford to deliver high-quality care to our nations sickest citizens.
At the center of much of this innovation will be hospitalists. After all, by its very nature, our model is a delivery system reform. The drive to deliver more-efficient quality care is in the very DNA of our specialty.
As decisions are made, they will have a significant impact on our patients and our careers. It will continue to be a priority for SHM to make sure that the voice of hospital medicine is heard loud and clear. We will continue to ask our members to ensure that the hospital medicine community has a prominent place in these conversations. Those who step up in this effort will lead us as we insist on having a prominent seat at the table and as new models of care emerge and new incentives are created for the provider community. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen SHM’s system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them with their colleagues at the local level. In our attempts to further connect our members with others who share similar interests and focuses, we will be rolling out a new structure of special interest groups. These local chapters and these interest groups will fuel new ideas that will continue to improve our specialty and the effectiveness of the society to speak for hospital medicine with a strong voice.
Of course, SHM will continue to be the only organization that was created to represent our nation’s hospitalists and will be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy. I look forward to serving you and helping you get the most from your SHM experience. Together, we will continue to move the hospital medicine movement forward, shaping our health care system and improving patient care.
Dr. Greeno is the incoming president of the Society of Hospital Medicine and senior adviser for medical affairs at TeamHealth.
As I begin my year as SHM president, I continue to be energized by the opportunity to be part of an organization that has such a positive impact on our nation’s health care system. From the beginning of my medical career to now, never have I witnessed a health care movement quite like hospital medicine.
Even when I first arrived in Southern California as a pulmonary/critical-care physician in 1987, there were groups of physicians who had taken financial risk on populations of managed-care patients and were paid using an “alternative payment model” called capitation. One of the innovations they had utilized since the early ’80s to successfully manage their risk – and their patients’ – was to have dedicated inpatient physicians caring for their hospitalized patients 24/7, while most of their primary care partners managed the group’s patients in the outpatient setting.
This year will see a continued reshaping of our delivery system, driven by emerging federal policy like the Medicare Access and CHIP Reauthorization Act (MACRA). All of this policy is designed to create a health care system that delivers high-quality care in a much more cost effective way. Many of these policies will result in groups of providers being pushed away from fee-for-service payment toward alternative payment models that involve higher levels of risk and opportunity. If we, as providers, are going to be successful in managing our “at risk” populations, we are going to have to be as innovative as our managed care forefathers. If we are not, we, as a society, are not going to be able to afford to deliver high-quality care to our nations sickest citizens.
At the center of much of this innovation will be hospitalists. After all, by its very nature, our model is a delivery system reform. The drive to deliver more-efficient quality care is in the very DNA of our specialty.
As decisions are made, they will have a significant impact on our patients and our careers. It will continue to be a priority for SHM to make sure that the voice of hospital medicine is heard loud and clear. We will continue to ask our members to ensure that the hospital medicine community has a prominent place in these conversations. Those who step up in this effort will lead us as we insist on having a prominent seat at the table and as new models of care emerge and new incentives are created for the provider community. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen SHM’s system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them with their colleagues at the local level. In our attempts to further connect our members with others who share similar interests and focuses, we will be rolling out a new structure of special interest groups. These local chapters and these interest groups will fuel new ideas that will continue to improve our specialty and the effectiveness of the society to speak for hospital medicine with a strong voice.
Of course, SHM will continue to be the only organization that was created to represent our nation’s hospitalists and will be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy. I look forward to serving you and helping you get the most from your SHM experience. Together, we will continue to move the hospital medicine movement forward, shaping our health care system and improving patient care.
Dr. Greeno is the incoming president of the Society of Hospital Medicine and senior adviser for medical affairs at TeamHealth.
As I begin my year as SHM president, I continue to be energized by the opportunity to be part of an organization that has such a positive impact on our nation’s health care system. From the beginning of my medical career to now, never have I witnessed a health care movement quite like hospital medicine.
Even when I first arrived in Southern California as a pulmonary/critical-care physician in 1987, there were groups of physicians who had taken financial risk on populations of managed-care patients and were paid using an “alternative payment model” called capitation. One of the innovations they had utilized since the early ’80s to successfully manage their risk – and their patients’ – was to have dedicated inpatient physicians caring for their hospitalized patients 24/7, while most of their primary care partners managed the group’s patients in the outpatient setting.
This year will see a continued reshaping of our delivery system, driven by emerging federal policy like the Medicare Access and CHIP Reauthorization Act (MACRA). All of this policy is designed to create a health care system that delivers high-quality care in a much more cost effective way. Many of these policies will result in groups of providers being pushed away from fee-for-service payment toward alternative payment models that involve higher levels of risk and opportunity. If we, as providers, are going to be successful in managing our “at risk” populations, we are going to have to be as innovative as our managed care forefathers. If we are not, we, as a society, are not going to be able to afford to deliver high-quality care to our nations sickest citizens.
At the center of much of this innovation will be hospitalists. After all, by its very nature, our model is a delivery system reform. The drive to deliver more-efficient quality care is in the very DNA of our specialty.
As decisions are made, they will have a significant impact on our patients and our careers. It will continue to be a priority for SHM to make sure that the voice of hospital medicine is heard loud and clear. We will continue to ask our members to ensure that the hospital medicine community has a prominent place in these conversations. Those who step up in this effort will lead us as we insist on having a prominent seat at the table and as new models of care emerge and new incentives are created for the provider community. We will continue to strive to make sure that our patients get the care they deserve and that we continue to help build a sustainable health care delivery system.
This year, you will also see a focused effort to strengthen SHM’s system of state and local chapters. The vitality of these local organizations is important to our efforts to effectively serve our members by engaging them with their colleagues at the local level. In our attempts to further connect our members with others who share similar interests and focuses, we will be rolling out a new structure of special interest groups. These local chapters and these interest groups will fuel new ideas that will continue to improve our specialty and the effectiveness of the society to speak for hospital medicine with a strong voice.
Of course, SHM will continue to be the only organization that was created to represent our nation’s hospitalists and will be totally committed to providing our members with clinical and administrative education, dedicated publications, leadership training, research opportunities, and advocacy. I look forward to serving you and helping you get the most from your SHM experience. Together, we will continue to move the hospital medicine movement forward, shaping our health care system and improving patient care.
Dr. Greeno is the incoming president of the Society of Hospital Medicine and senior adviser for medical affairs at TeamHealth.
RIV poster contest a meeting highlight
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
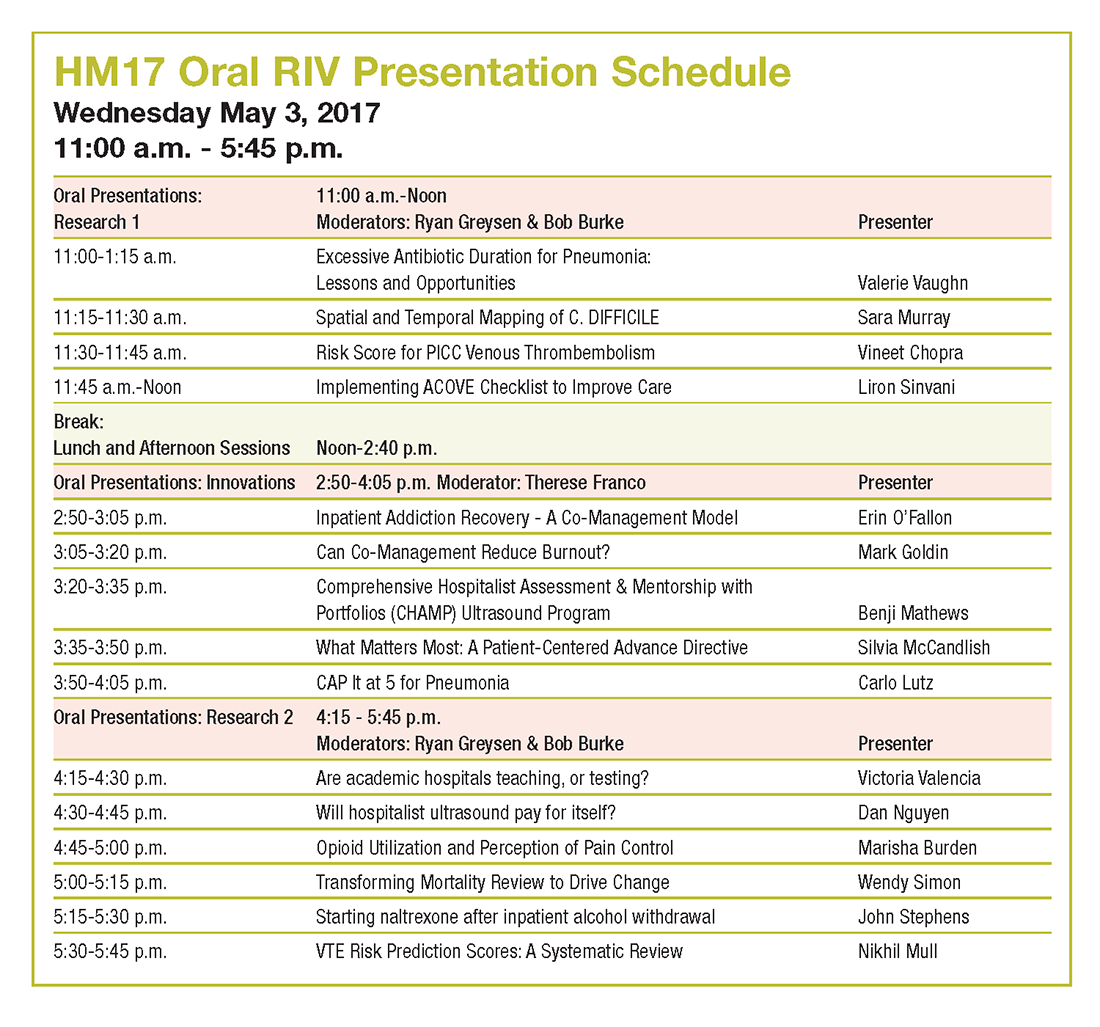
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
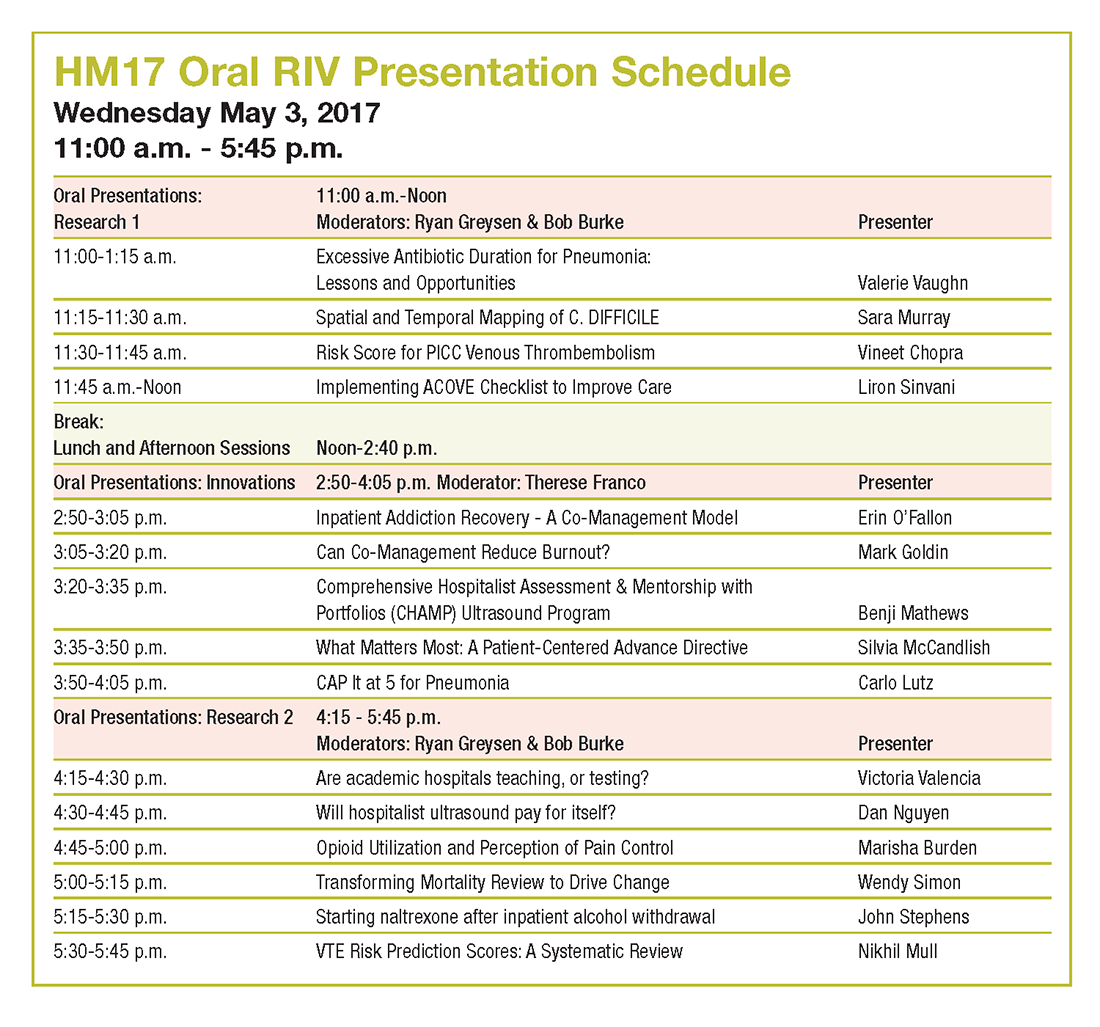
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
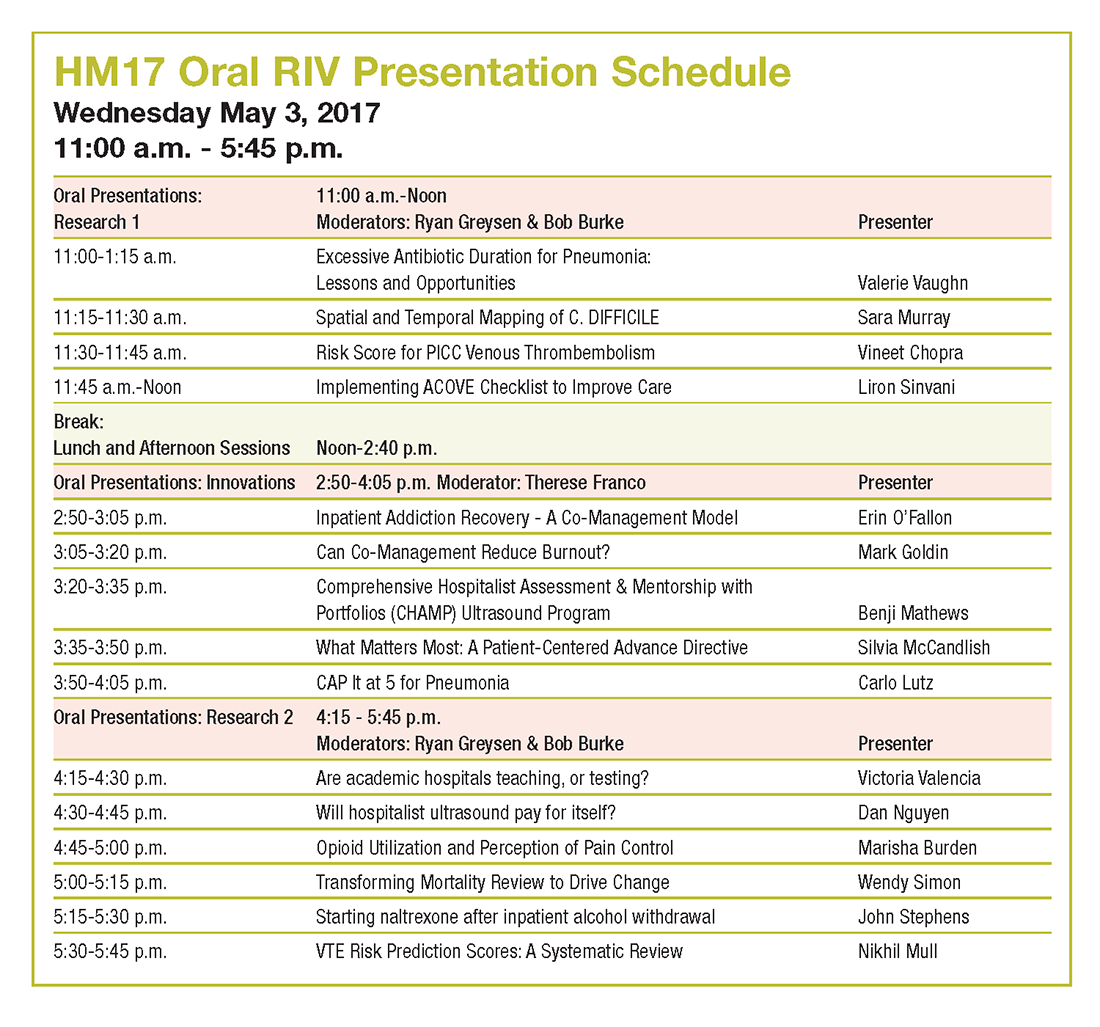
Crossing the personal quality chasm: QI enthusiast to QI leader
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.