User login
Maternal Flu Vaccine Cuts Infants' Infection Risk
Major Finding: The incidence of influenza-like illness was 6.7 per 1,000 person-days for infants of mothers who had been vaccinated, compared with 7.2 per 1,000 person-days for infants of mothers who had not.
Data Source: A nonrandomized, prospective, observational cohort study involving 1,160 mother-infant pairs.
Disclosures: The study was funded by the U.S. Department of Health and Human Services' National Vaccine Program Office, the Office of Minority and Women's Health (now the Office of Health Disparities), the Centers for Disease Control and Prevention, Aventis-Pasteur, and Evans-Powderject. One of Dr. Eick's associates reported ties (unrelated to this study) with MedImmune, Pfizer, and Sanofi-Pasteur, all of which manufacture influenza vaccine.
Vaccinating pregnant women against seasonal influenza reduced the risk of laboratory-confirmed influenza infection in their infants by 41%, according to a study.
Maternal immunization similarly cut by 39% the risk that infants up to 6 months of age would be hospitalized for influenza-like illness, said Angelia A. Eick, Ph.D., of the Center for American Indian Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, and her associates.
Influenza vaccination is already recommended for pregnant women to reduce their risk of developing flu-related complications. “These findings provide support for the added benefit of protecting infants from influenza virus infection up to 6 months, the period when infants are not eligible for influenza vaccination but are at highest risk of severe influenza illness,” they noted.
Even though such immunization is recommended during pregnancy, it is not well accepted in the United States and many pregnant women do not get vaccinated. Since it would be unethical to perform a randomized, controlled study of maternal vaccination, Dr. Eick and her colleagues conducted a nonrandomized observational study to assess whether immunization during pregnancy conferred protection to infants.
The study subjects were 1,160 mother-infant pairs in which approximately half the mothers (573) had chosen to receive seasonal flu vaccine while pregnant and the other half (587) had declined the vaccine. All were enrolled after delivering healthy singleton infants at 7 hospitals serving the Navajo and White Mountain Apache Indian reservations in the southwestern United States during three flu seasons between 2002 and 2005.
A total of 605 infants developed influenza-like illness during the flu season following delivery. “We found a 41% reduction in the risk of laboratory-confirmed influenza virus infection for infants of influenza-vaccinated mothers compared with infants of unvaccinated mothers,” they said (Arch Pediatr. Adolesc. Med. 2010 [doi10.1001/archpediatrics.2010.192]).
The incidence of influenza-like illness was 6.7 per 1,000 person-days for infants of mothers who had been vaccinated, compared with 7.2 per 1,000 person-days for infants of mothers who had not. Among the infants whose mothers were vaccinated, there was a 41% reduction in the risk of laboratory-confirmed influenza virus infection compared with those whose mothers declined vaccination.
When the analysis was restricted only to cases of influenza that required hospitalization, a 39% reduction in risk was found for infants of women who had been vaccinated, compared with those of mothers who had not been vaccinated.
Cord blood samples or infant blood samples taken at 2–3 months of age were available for 160 study subjects. In this subgroup, the risk of influenza infection declined with increasing antibody titers.
The exact mechanism by which vaccination of the mother conferred protection to the infant is not certain. It may be due to maternal influenza antibodies being acquired transplacentally or through breastfeeding, or to reduced infant exposure to influenza in the mother.
It even could be due to residual confounding not accounted for in the statistical analyses, but the finding of significantly higher antibody titers in 2- to 3-month-old infants who did not develop illness argues against that possibility, they said.
View on the News
Barriers to Maternal Vaccination
This study confirms the potential for influenza vaccination of pregnant women to decrease newborn illness.
“In the United States, acceptance of vaccination during pregnancy is poor. Despite the fact that the U.S. Advisory Committee on Immunization Practices (ACIP) has recommended the use of influenza vaccine during pregnancy since 1997, there has been little appreciable change in vaccine use by the group from 1997 through 2009,” noted Dr. Justin R. Ortiz and Dr. Kathleen M. Neuzil.
Studies have indicated that some members of the public believe that influenza infection “is not serious” or hold misconceptions about vaccine safety during pregnancy. But decades of research have demonstrated substantial influenza-associated morbidity in pregnant women and have established the “excellent” safety profile of maternal trivalent inactivated influenza vaccination, they wrote.
JUSTIN R. ORTIZ, M.D., and KATHLEEN M. NEUZIL, M.D., and are both with the Vaccine Development Global Program at PATH, an international nonprofit organization dedicated to solving health care problems, and at the University of Washington, Seattle. They reported having no financial disclosures. These comments were summarized from their editorial (Arch. Pediatr. Adolesc. Med. 2010 [doi:10.1001/archpediatrics.2010.193]).
Major Finding: The incidence of influenza-like illness was 6.7 per 1,000 person-days for infants of mothers who had been vaccinated, compared with 7.2 per 1,000 person-days for infants of mothers who had not.
Data Source: A nonrandomized, prospective, observational cohort study involving 1,160 mother-infant pairs.
Disclosures: The study was funded by the U.S. Department of Health and Human Services' National Vaccine Program Office, the Office of Minority and Women's Health (now the Office of Health Disparities), the Centers for Disease Control and Prevention, Aventis-Pasteur, and Evans-Powderject. One of Dr. Eick's associates reported ties (unrelated to this study) with MedImmune, Pfizer, and Sanofi-Pasteur, all of which manufacture influenza vaccine.
Vaccinating pregnant women against seasonal influenza reduced the risk of laboratory-confirmed influenza infection in their infants by 41%, according to a study.
Maternal immunization similarly cut by 39% the risk that infants up to 6 months of age would be hospitalized for influenza-like illness, said Angelia A. Eick, Ph.D., of the Center for American Indian Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, and her associates.
Influenza vaccination is already recommended for pregnant women to reduce their risk of developing flu-related complications. “These findings provide support for the added benefit of protecting infants from influenza virus infection up to 6 months, the period when infants are not eligible for influenza vaccination but are at highest risk of severe influenza illness,” they noted.
Even though such immunization is recommended during pregnancy, it is not well accepted in the United States and many pregnant women do not get vaccinated. Since it would be unethical to perform a randomized, controlled study of maternal vaccination, Dr. Eick and her colleagues conducted a nonrandomized observational study to assess whether immunization during pregnancy conferred protection to infants.
The study subjects were 1,160 mother-infant pairs in which approximately half the mothers (573) had chosen to receive seasonal flu vaccine while pregnant and the other half (587) had declined the vaccine. All were enrolled after delivering healthy singleton infants at 7 hospitals serving the Navajo and White Mountain Apache Indian reservations in the southwestern United States during three flu seasons between 2002 and 2005.
A total of 605 infants developed influenza-like illness during the flu season following delivery. “We found a 41% reduction in the risk of laboratory-confirmed influenza virus infection for infants of influenza-vaccinated mothers compared with infants of unvaccinated mothers,” they said (Arch Pediatr. Adolesc. Med. 2010 [doi10.1001/archpediatrics.2010.192]).
The incidence of influenza-like illness was 6.7 per 1,000 person-days for infants of mothers who had been vaccinated, compared with 7.2 per 1,000 person-days for infants of mothers who had not. Among the infants whose mothers were vaccinated, there was a 41% reduction in the risk of laboratory-confirmed influenza virus infection compared with those whose mothers declined vaccination.
When the analysis was restricted only to cases of influenza that required hospitalization, a 39% reduction in risk was found for infants of women who had been vaccinated, compared with those of mothers who had not been vaccinated.
Cord blood samples or infant blood samples taken at 2–3 months of age were available for 160 study subjects. In this subgroup, the risk of influenza infection declined with increasing antibody titers.
The exact mechanism by which vaccination of the mother conferred protection to the infant is not certain. It may be due to maternal influenza antibodies being acquired transplacentally or through breastfeeding, or to reduced infant exposure to influenza in the mother.
It even could be due to residual confounding not accounted for in the statistical analyses, but the finding of significantly higher antibody titers in 2- to 3-month-old infants who did not develop illness argues against that possibility, they said.
View on the News
Barriers to Maternal Vaccination
This study confirms the potential for influenza vaccination of pregnant women to decrease newborn illness.
“In the United States, acceptance of vaccination during pregnancy is poor. Despite the fact that the U.S. Advisory Committee on Immunization Practices (ACIP) has recommended the use of influenza vaccine during pregnancy since 1997, there has been little appreciable change in vaccine use by the group from 1997 through 2009,” noted Dr. Justin R. Ortiz and Dr. Kathleen M. Neuzil.
Studies have indicated that some members of the public believe that influenza infection “is not serious” or hold misconceptions about vaccine safety during pregnancy. But decades of research have demonstrated substantial influenza-associated morbidity in pregnant women and have established the “excellent” safety profile of maternal trivalent inactivated influenza vaccination, they wrote.
JUSTIN R. ORTIZ, M.D., and KATHLEEN M. NEUZIL, M.D., and are both with the Vaccine Development Global Program at PATH, an international nonprofit organization dedicated to solving health care problems, and at the University of Washington, Seattle. They reported having no financial disclosures. These comments were summarized from their editorial (Arch. Pediatr. Adolesc. Med. 2010 [doi:10.1001/archpediatrics.2010.193]).
Major Finding: The incidence of influenza-like illness was 6.7 per 1,000 person-days for infants of mothers who had been vaccinated, compared with 7.2 per 1,000 person-days for infants of mothers who had not.
Data Source: A nonrandomized, prospective, observational cohort study involving 1,160 mother-infant pairs.
Disclosures: The study was funded by the U.S. Department of Health and Human Services' National Vaccine Program Office, the Office of Minority and Women's Health (now the Office of Health Disparities), the Centers for Disease Control and Prevention, Aventis-Pasteur, and Evans-Powderject. One of Dr. Eick's associates reported ties (unrelated to this study) with MedImmune, Pfizer, and Sanofi-Pasteur, all of which manufacture influenza vaccine.
Vaccinating pregnant women against seasonal influenza reduced the risk of laboratory-confirmed influenza infection in their infants by 41%, according to a study.
Maternal immunization similarly cut by 39% the risk that infants up to 6 months of age would be hospitalized for influenza-like illness, said Angelia A. Eick, Ph.D., of the Center for American Indian Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, and her associates.
Influenza vaccination is already recommended for pregnant women to reduce their risk of developing flu-related complications. “These findings provide support for the added benefit of protecting infants from influenza virus infection up to 6 months, the period when infants are not eligible for influenza vaccination but are at highest risk of severe influenza illness,” they noted.
Even though such immunization is recommended during pregnancy, it is not well accepted in the United States and many pregnant women do not get vaccinated. Since it would be unethical to perform a randomized, controlled study of maternal vaccination, Dr. Eick and her colleagues conducted a nonrandomized observational study to assess whether immunization during pregnancy conferred protection to infants.
The study subjects were 1,160 mother-infant pairs in which approximately half the mothers (573) had chosen to receive seasonal flu vaccine while pregnant and the other half (587) had declined the vaccine. All were enrolled after delivering healthy singleton infants at 7 hospitals serving the Navajo and White Mountain Apache Indian reservations in the southwestern United States during three flu seasons between 2002 and 2005.
A total of 605 infants developed influenza-like illness during the flu season following delivery. “We found a 41% reduction in the risk of laboratory-confirmed influenza virus infection for infants of influenza-vaccinated mothers compared with infants of unvaccinated mothers,” they said (Arch Pediatr. Adolesc. Med. 2010 [doi10.1001/archpediatrics.2010.192]).
The incidence of influenza-like illness was 6.7 per 1,000 person-days for infants of mothers who had been vaccinated, compared with 7.2 per 1,000 person-days for infants of mothers who had not. Among the infants whose mothers were vaccinated, there was a 41% reduction in the risk of laboratory-confirmed influenza virus infection compared with those whose mothers declined vaccination.
When the analysis was restricted only to cases of influenza that required hospitalization, a 39% reduction in risk was found for infants of women who had been vaccinated, compared with those of mothers who had not been vaccinated.
Cord blood samples or infant blood samples taken at 2–3 months of age were available for 160 study subjects. In this subgroup, the risk of influenza infection declined with increasing antibody titers.
The exact mechanism by which vaccination of the mother conferred protection to the infant is not certain. It may be due to maternal influenza antibodies being acquired transplacentally or through breastfeeding, or to reduced infant exposure to influenza in the mother.
It even could be due to residual confounding not accounted for in the statistical analyses, but the finding of significantly higher antibody titers in 2- to 3-month-old infants who did not develop illness argues against that possibility, they said.
View on the News
Barriers to Maternal Vaccination
This study confirms the potential for influenza vaccination of pregnant women to decrease newborn illness.
“In the United States, acceptance of vaccination during pregnancy is poor. Despite the fact that the U.S. Advisory Committee on Immunization Practices (ACIP) has recommended the use of influenza vaccine during pregnancy since 1997, there has been little appreciable change in vaccine use by the group from 1997 through 2009,” noted Dr. Justin R. Ortiz and Dr. Kathleen M. Neuzil.
Studies have indicated that some members of the public believe that influenza infection “is not serious” or hold misconceptions about vaccine safety during pregnancy. But decades of research have demonstrated substantial influenza-associated morbidity in pregnant women and have established the “excellent” safety profile of maternal trivalent inactivated influenza vaccination, they wrote.
JUSTIN R. ORTIZ, M.D., and KATHLEEN M. NEUZIL, M.D., and are both with the Vaccine Development Global Program at PATH, an international nonprofit organization dedicated to solving health care problems, and at the University of Washington, Seattle. They reported having no financial disclosures. These comments were summarized from their editorial (Arch. Pediatr. Adolesc. Med. 2010 [doi:10.1001/archpediatrics.2010.193]).
From the Archives of Pediatric and Adolescent Medicine
Web Tool Helps New Moms Shed Pounds
SEATTLE — A Web-based intervention that promotes physical activity and a better diet helps new mothers lose excess weight in the postpartum period, according to a randomized controlled trial.
In the trial, new mothers assigned to the intervention had about a 1.25-kg/m
“We saw a small differential effect on body mass index, not a dramatic effect, but in a fairly low-intensity intervention, we might not expect that,” lead investigator Karen J. Calfas, Ph.D., said at the meeting.
Weight gain over a person's lifespan is accelerated during certain periods, including pregnancy and the postpartum period for women, noted Dr. Calfas, who is an assistant clinical professor of family and preventive medicine at the University of California, San Diego.
“Women often don't return to their prepregnancy weight, and then maybe a second pregnancy comes and there is kind of a compounding effect of pregnancy weight over time for some women,” she said. Added to that, some women gain weight during the postpartum period because they are more sedentary and have readier access to food.
“Postpartum care is often focused really on the medical issues,” she further noted, “and the weight issues for the moms don't always get addressed.”
The investigators recruited women for the trial mainly by posting notices in community newspapers and obstetrician gynecologists' offices. To be eligible, women had to be 8 weeks to 12 months post partum and have a BMI placing them in the overweight to moderately obese category (25–35 kg/m
They were randomly assigned in nearly equal numbers to the 16-week Web-based intervention, called iMom, which encouraged increased physical activity and improved dietary intake with the goal of weight loss, or to a wait list control group.
The intervention entailed weekly Web-based educational content and behavior strategies, and monthly support phone calls. The mothers were encouraged to set goals, and they reported on their progress and received feedback online regarding weight, physical activity, and intakes of fat, fiber, and fruit and vegetables. The Web site also had a message board for connecting to other mothers.
“It's somewhat controversial to be recommending weight loss for women who might be breastfeeding,” Dr. Calfas acknowledged. However, the energy deficit recommended in the intervention was carefully tailored according to whether women were breastfeeding and how much. “The research shows that if calories are reduced slightly and weight is lost slowly over time, that it does not affect either the quantity or the quality of breast milk that is produced,” she noted.
Study results showed that mothers assigned to the intervention lost about 1.5 kg (3.3 lb) on average, whereas those assigned to the wait list lost about 0.5 kg (1.1 lb). The difference corresponded to a 1.21-kg (2.67-lb) greater loss for the former group. Similarly, BMI fell by about 1.25 kg/m
“The women, anecdotally, reported high satisfaction with [the intervention], and they especially appreciated the fact that they could do it whenever it was convenient for them,” commented Dr. Calfas.
Ongoing analyses will be looking for any dose-response relationship, evaluating how much the new mothers actually used the Web site, she said, noting that overall use was not as high as hoped.
Dr. Calfas is cofounder of and stockholder in Santech Inc., a company that uses mobile and Web technologies to promote behavior change.
SEATTLE — A Web-based intervention that promotes physical activity and a better diet helps new mothers lose excess weight in the postpartum period, according to a randomized controlled trial.
In the trial, new mothers assigned to the intervention had about a 1.25-kg/m
“We saw a small differential effect on body mass index, not a dramatic effect, but in a fairly low-intensity intervention, we might not expect that,” lead investigator Karen J. Calfas, Ph.D., said at the meeting.
Weight gain over a person's lifespan is accelerated during certain periods, including pregnancy and the postpartum period for women, noted Dr. Calfas, who is an assistant clinical professor of family and preventive medicine at the University of California, San Diego.
“Women often don't return to their prepregnancy weight, and then maybe a second pregnancy comes and there is kind of a compounding effect of pregnancy weight over time for some women,” she said. Added to that, some women gain weight during the postpartum period because they are more sedentary and have readier access to food.
“Postpartum care is often focused really on the medical issues,” she further noted, “and the weight issues for the moms don't always get addressed.”
The investigators recruited women for the trial mainly by posting notices in community newspapers and obstetrician gynecologists' offices. To be eligible, women had to be 8 weeks to 12 months post partum and have a BMI placing them in the overweight to moderately obese category (25–35 kg/m
They were randomly assigned in nearly equal numbers to the 16-week Web-based intervention, called iMom, which encouraged increased physical activity and improved dietary intake with the goal of weight loss, or to a wait list control group.
The intervention entailed weekly Web-based educational content and behavior strategies, and monthly support phone calls. The mothers were encouraged to set goals, and they reported on their progress and received feedback online regarding weight, physical activity, and intakes of fat, fiber, and fruit and vegetables. The Web site also had a message board for connecting to other mothers.
“It's somewhat controversial to be recommending weight loss for women who might be breastfeeding,” Dr. Calfas acknowledged. However, the energy deficit recommended in the intervention was carefully tailored according to whether women were breastfeeding and how much. “The research shows that if calories are reduced slightly and weight is lost slowly over time, that it does not affect either the quantity or the quality of breast milk that is produced,” she noted.
Study results showed that mothers assigned to the intervention lost about 1.5 kg (3.3 lb) on average, whereas those assigned to the wait list lost about 0.5 kg (1.1 lb). The difference corresponded to a 1.21-kg (2.67-lb) greater loss for the former group. Similarly, BMI fell by about 1.25 kg/m
“The women, anecdotally, reported high satisfaction with [the intervention], and they especially appreciated the fact that they could do it whenever it was convenient for them,” commented Dr. Calfas.
Ongoing analyses will be looking for any dose-response relationship, evaluating how much the new mothers actually used the Web site, she said, noting that overall use was not as high as hoped.
Dr. Calfas is cofounder of and stockholder in Santech Inc., a company that uses mobile and Web technologies to promote behavior change.
SEATTLE — A Web-based intervention that promotes physical activity and a better diet helps new mothers lose excess weight in the postpartum period, according to a randomized controlled trial.
In the trial, new mothers assigned to the intervention had about a 1.25-kg/m
“We saw a small differential effect on body mass index, not a dramatic effect, but in a fairly low-intensity intervention, we might not expect that,” lead investigator Karen J. Calfas, Ph.D., said at the meeting.
Weight gain over a person's lifespan is accelerated during certain periods, including pregnancy and the postpartum period for women, noted Dr. Calfas, who is an assistant clinical professor of family and preventive medicine at the University of California, San Diego.
“Women often don't return to their prepregnancy weight, and then maybe a second pregnancy comes and there is kind of a compounding effect of pregnancy weight over time for some women,” she said. Added to that, some women gain weight during the postpartum period because they are more sedentary and have readier access to food.
“Postpartum care is often focused really on the medical issues,” she further noted, “and the weight issues for the moms don't always get addressed.”
The investigators recruited women for the trial mainly by posting notices in community newspapers and obstetrician gynecologists' offices. To be eligible, women had to be 8 weeks to 12 months post partum and have a BMI placing them in the overweight to moderately obese category (25–35 kg/m
They were randomly assigned in nearly equal numbers to the 16-week Web-based intervention, called iMom, which encouraged increased physical activity and improved dietary intake with the goal of weight loss, or to a wait list control group.
The intervention entailed weekly Web-based educational content and behavior strategies, and monthly support phone calls. The mothers were encouraged to set goals, and they reported on their progress and received feedback online regarding weight, physical activity, and intakes of fat, fiber, and fruit and vegetables. The Web site also had a message board for connecting to other mothers.
“It's somewhat controversial to be recommending weight loss for women who might be breastfeeding,” Dr. Calfas acknowledged. However, the energy deficit recommended in the intervention was carefully tailored according to whether women were breastfeeding and how much. “The research shows that if calories are reduced slightly and weight is lost slowly over time, that it does not affect either the quantity or the quality of breast milk that is produced,” she noted.
Study results showed that mothers assigned to the intervention lost about 1.5 kg (3.3 lb) on average, whereas those assigned to the wait list lost about 0.5 kg (1.1 lb). The difference corresponded to a 1.21-kg (2.67-lb) greater loss for the former group. Similarly, BMI fell by about 1.25 kg/m
“The women, anecdotally, reported high satisfaction with [the intervention], and they especially appreciated the fact that they could do it whenever it was convenient for them,” commented Dr. Calfas.
Ongoing analyses will be looking for any dose-response relationship, evaluating how much the new mothers actually used the Web site, she said, noting that overall use was not as high as hoped.
Dr. Calfas is cofounder of and stockholder in Santech Inc., a company that uses mobile and Web technologies to promote behavior change.
The Annual Meeting of the Society of Behavioral Medicine
Ketamine Reduces Post C-Section Pain at 6 Weeks
Major Finding: Patients in the ketamine group reported significantly less pain at 6 weeks post partum, with scores of 1.3 vs. 2.3, but there were no significant differences at 6 weeks in depression or at 1 year in pain or depression.
Data Source: One-year follow-up of 82 parturients from an initial randomized, controlled trial of 188.
Disclosures: None was reported.
SAN ANTONIO — A single postpartum low dose of ketamine significantly and persistently reduced pain for up to 6 weeks after cesarean delivery compared with placebo, but there were no significant differences in chronic pain or depression between the two groups at 1 year, in a randomized, double-blind study of 82 women.
Low doses of the N-methyl-d-aspartate (NMDA) antagonist ketamine have been shown to decrease postoperative opioid requirements, and the drug has also been shown to have an antidepressive effect (Arch. Gen. Psychiatry 2006;63:856–64). hhose data led to the hypothesis that women who receive a single intravenous dose of ketamine might be less likely to develop postpartum depression or chronic pelvic pain, said Dr. Laurie Chalifoux of Northwestern University, Chicago.
A total of 188 women were randomized to receive either 10 mg IV ketamine or saline by a blinded anesthesiologist 5 minutes after cesarean delivery.
All received scheduled IV ketorolac 30 mg every 6 hours for 24 hours, along with 1 or 2 tablets of acetaminophen 325 mg/hydrocodone 10 mg every 4 hours as needed for breakthrough pain.
Among those 188 women, the group who received ketamine reported significantly lower numeric pain rating scores (on a scale of 1–10) than did those receiving saline.
However, there were no differences at any other time point, Dr. Chalifoux reported at the meeting.
The 82 patients who were available for an interview 1 year later were asked to report pain scores (1–10) and whether they had a self-diagnosis of depression at both 6 weeks and 1 year post partum. Patients in the ketamine group reported significantly less pain at 6 weeks post partum, with scores of 1.3 vs. 2.3.
Depression did not differ at 6 weeks, with just one woman (2%) from each group reporting that she was depressed at that point.
At 1 year, pain scores were nearly 0 in both groups and did not differ significantly (0.1 with ketamine vs. 0.0 with saline).
Depression also did not differ significantly, although there were two women (5%) who reported being depressed at 1 year in the saline group compared with none in the ketamine group.
It's possible that a higher dose than 10 mg might have had a greater impact, given that the previous studies showing analgesic and antidepressive effects used doses ranging from 0.15 to 1.0 mg/kg. However, the potential side effects of ketamine – including dysphoria, memory loss, hallucinations, seizures, nystagmus, hypertension, tachycardia, and nausea/vomiting – suggest that dosages should be kept in the lower ranges, Dr. Chalifoux noted.
Also, it's possible that ketamine might not have a large impact among healthy parturients, but it might among those who are at increased risk for depression or chronic pain, she said.
Major Finding: Patients in the ketamine group reported significantly less pain at 6 weeks post partum, with scores of 1.3 vs. 2.3, but there were no significant differences at 6 weeks in depression or at 1 year in pain or depression.
Data Source: One-year follow-up of 82 parturients from an initial randomized, controlled trial of 188.
Disclosures: None was reported.
SAN ANTONIO — A single postpartum low dose of ketamine significantly and persistently reduced pain for up to 6 weeks after cesarean delivery compared with placebo, but there were no significant differences in chronic pain or depression between the two groups at 1 year, in a randomized, double-blind study of 82 women.
Low doses of the N-methyl-d-aspartate (NMDA) antagonist ketamine have been shown to decrease postoperative opioid requirements, and the drug has also been shown to have an antidepressive effect (Arch. Gen. Psychiatry 2006;63:856–64). hhose data led to the hypothesis that women who receive a single intravenous dose of ketamine might be less likely to develop postpartum depression or chronic pelvic pain, said Dr. Laurie Chalifoux of Northwestern University, Chicago.
A total of 188 women were randomized to receive either 10 mg IV ketamine or saline by a blinded anesthesiologist 5 minutes after cesarean delivery.
All received scheduled IV ketorolac 30 mg every 6 hours for 24 hours, along with 1 or 2 tablets of acetaminophen 325 mg/hydrocodone 10 mg every 4 hours as needed for breakthrough pain.
Among those 188 women, the group who received ketamine reported significantly lower numeric pain rating scores (on a scale of 1–10) than did those receiving saline.
However, there were no differences at any other time point, Dr. Chalifoux reported at the meeting.
The 82 patients who were available for an interview 1 year later were asked to report pain scores (1–10) and whether they had a self-diagnosis of depression at both 6 weeks and 1 year post partum. Patients in the ketamine group reported significantly less pain at 6 weeks post partum, with scores of 1.3 vs. 2.3.
Depression did not differ at 6 weeks, with just one woman (2%) from each group reporting that she was depressed at that point.
At 1 year, pain scores were nearly 0 in both groups and did not differ significantly (0.1 with ketamine vs. 0.0 with saline).
Depression also did not differ significantly, although there were two women (5%) who reported being depressed at 1 year in the saline group compared with none in the ketamine group.
It's possible that a higher dose than 10 mg might have had a greater impact, given that the previous studies showing analgesic and antidepressive effects used doses ranging from 0.15 to 1.0 mg/kg. However, the potential side effects of ketamine – including dysphoria, memory loss, hallucinations, seizures, nystagmus, hypertension, tachycardia, and nausea/vomiting – suggest that dosages should be kept in the lower ranges, Dr. Chalifoux noted.
Also, it's possible that ketamine might not have a large impact among healthy parturients, but it might among those who are at increased risk for depression or chronic pain, she said.
Major Finding: Patients in the ketamine group reported significantly less pain at 6 weeks post partum, with scores of 1.3 vs. 2.3, but there were no significant differences at 6 weeks in depression or at 1 year in pain or depression.
Data Source: One-year follow-up of 82 parturients from an initial randomized, controlled trial of 188.
Disclosures: None was reported.
SAN ANTONIO — A single postpartum low dose of ketamine significantly and persistently reduced pain for up to 6 weeks after cesarean delivery compared with placebo, but there were no significant differences in chronic pain or depression between the two groups at 1 year, in a randomized, double-blind study of 82 women.
Low doses of the N-methyl-d-aspartate (NMDA) antagonist ketamine have been shown to decrease postoperative opioid requirements, and the drug has also been shown to have an antidepressive effect (Arch. Gen. Psychiatry 2006;63:856–64). hhose data led to the hypothesis that women who receive a single intravenous dose of ketamine might be less likely to develop postpartum depression or chronic pelvic pain, said Dr. Laurie Chalifoux of Northwestern University, Chicago.
A total of 188 women were randomized to receive either 10 mg IV ketamine or saline by a blinded anesthesiologist 5 minutes after cesarean delivery.
All received scheduled IV ketorolac 30 mg every 6 hours for 24 hours, along with 1 or 2 tablets of acetaminophen 325 mg/hydrocodone 10 mg every 4 hours as needed for breakthrough pain.
Among those 188 women, the group who received ketamine reported significantly lower numeric pain rating scores (on a scale of 1–10) than did those receiving saline.
However, there were no differences at any other time point, Dr. Chalifoux reported at the meeting.
The 82 patients who were available for an interview 1 year later were asked to report pain scores (1–10) and whether they had a self-diagnosis of depression at both 6 weeks and 1 year post partum. Patients in the ketamine group reported significantly less pain at 6 weeks post partum, with scores of 1.3 vs. 2.3.
Depression did not differ at 6 weeks, with just one woman (2%) from each group reporting that she was depressed at that point.
At 1 year, pain scores were nearly 0 in both groups and did not differ significantly (0.1 with ketamine vs. 0.0 with saline).
Depression also did not differ significantly, although there were two women (5%) who reported being depressed at 1 year in the saline group compared with none in the ketamine group.
It's possible that a higher dose than 10 mg might have had a greater impact, given that the previous studies showing analgesic and antidepressive effects used doses ranging from 0.15 to 1.0 mg/kg. However, the potential side effects of ketamine – including dysphoria, memory loss, hallucinations, seizures, nystagmus, hypertension, tachycardia, and nausea/vomiting – suggest that dosages should be kept in the lower ranges, Dr. Chalifoux noted.
Also, it's possible that ketamine might not have a large impact among healthy parturients, but it might among those who are at increased risk for depression or chronic pain, she said.
From the Annual Meeting of the Society for Obstetric Anesthesia and Perinatology
Select Criteria Denote High-Risk SLE Pregnancies
VANCOUVER, B.C. — Monthly monitoring by rheumatologists of every pregnancy in every woman with systemic lupus erythematosus may be unnecessary, according to Dr. Michelle Petri.
A relatively small list of criteria can distinguish high-risk pregnancies in women with systemic lupus erythematosus (SLE) – ones that carry a higher likelihood of miscarriage, extreme prematurity, and SLE flare – from others, and signal the need for intensive monitoring by obstetricians and rheumatologists, Dr. Petri said at the meeting.
At present, however, there is little effort to make such distinctions, so most SLE pregnancies are subjected to monthly visits to rheumatologists and obstetricians, and, starting at week 26, weekly monitoring by obstetricians.
That's not always necessary; women are subjected to needless anxiety and hospital resources are wasted, Dr. Petri said.
Based on the Hopkins Lupus Cohort, a database that has been tracking several thousand patients with SLE over the past 25 years, Dr. Petri and her colleague, Duke University rheumatologist Dr. Megan Clowse, have identified those factors that truly put women and fetuses at risk during SLE pregnancies.
Pregnancy and the postpartum period are hard on the kidneys of women with SLE, though organ involvement elsewhere in the body tends to lessen, said Dr. Petri, professor of rheumatology at Johns Hopkins University, Baltimore.
“Proteinuria from active lupus significantly increases, and this continues even after delivery,” she added.
Therefore, pregnant women with lupus nephritis truly do need close monitoring. Dr. Petri recommended monthly urine protein-creatinine ratios to detect a worsening of the condition and the need for treatment.
She noted that the ranges on urine dipsticks are too broad; the dipstick is not adequate as a monitoring tool for nephritis.
In terms of fetal health, the risk of miscarriage doubles if, at the first pregnancy visit, a woman is proteinuric, thrombocytopenic, or hypertensive, or has a history of antiphospholipid syndrome.
The risk triples if two or more of these conditions are present, Dr. Petri said. The presence of antithyroid antibodies also increases the risk of miscarriage.
In addition, active SLE, especially if accompanied by anti–double-stranded DNA antibody or low complement levels, predicts extreme prematurity. Autoimmune thyroid disease also appears to be associated with preterm birth.
Screening for the various factors, “we can predict at the first pregnancy visit if there's going to be a poor outcome,” Dr. Petri said.
If the risk factors are present, monthly monitoring by a high-risk obstetrician, followed by weekly monitoring at week 26, are appropriate to gauge if, and when, a rescue delivery is needed.
Otherwise, and absent renal involvement in the pregnant patient, SLE pregnancies may not need to be classified as high risk, Dr. Petri said.
“Since we can stratify women at risk for miscarriage and extreme prematurity, and know the only organ we have to worry about is the kidney, we can come closer to using our resources appropriately,” Dr. Petri said.
To reassure women, rheumatologists should “get the word out to patients that high-risk interventions are not necessary for every [SLE pregnancy],” she said.
Dr. Petri said she had no disclosures to report.
VANCOUVER, B.C. — Monthly monitoring by rheumatologists of every pregnancy in every woman with systemic lupus erythematosus may be unnecessary, according to Dr. Michelle Petri.
A relatively small list of criteria can distinguish high-risk pregnancies in women with systemic lupus erythematosus (SLE) – ones that carry a higher likelihood of miscarriage, extreme prematurity, and SLE flare – from others, and signal the need for intensive monitoring by obstetricians and rheumatologists, Dr. Petri said at the meeting.
At present, however, there is little effort to make such distinctions, so most SLE pregnancies are subjected to monthly visits to rheumatologists and obstetricians, and, starting at week 26, weekly monitoring by obstetricians.
That's not always necessary; women are subjected to needless anxiety and hospital resources are wasted, Dr. Petri said.
Based on the Hopkins Lupus Cohort, a database that has been tracking several thousand patients with SLE over the past 25 years, Dr. Petri and her colleague, Duke University rheumatologist Dr. Megan Clowse, have identified those factors that truly put women and fetuses at risk during SLE pregnancies.
Pregnancy and the postpartum period are hard on the kidneys of women with SLE, though organ involvement elsewhere in the body tends to lessen, said Dr. Petri, professor of rheumatology at Johns Hopkins University, Baltimore.
“Proteinuria from active lupus significantly increases, and this continues even after delivery,” she added.
Therefore, pregnant women with lupus nephritis truly do need close monitoring. Dr. Petri recommended monthly urine protein-creatinine ratios to detect a worsening of the condition and the need for treatment.
She noted that the ranges on urine dipsticks are too broad; the dipstick is not adequate as a monitoring tool for nephritis.
In terms of fetal health, the risk of miscarriage doubles if, at the first pregnancy visit, a woman is proteinuric, thrombocytopenic, or hypertensive, or has a history of antiphospholipid syndrome.
The risk triples if two or more of these conditions are present, Dr. Petri said. The presence of antithyroid antibodies also increases the risk of miscarriage.
In addition, active SLE, especially if accompanied by anti–double-stranded DNA antibody or low complement levels, predicts extreme prematurity. Autoimmune thyroid disease also appears to be associated with preterm birth.
Screening for the various factors, “we can predict at the first pregnancy visit if there's going to be a poor outcome,” Dr. Petri said.
If the risk factors are present, monthly monitoring by a high-risk obstetrician, followed by weekly monitoring at week 26, are appropriate to gauge if, and when, a rescue delivery is needed.
Otherwise, and absent renal involvement in the pregnant patient, SLE pregnancies may not need to be classified as high risk, Dr. Petri said.
“Since we can stratify women at risk for miscarriage and extreme prematurity, and know the only organ we have to worry about is the kidney, we can come closer to using our resources appropriately,” Dr. Petri said.
To reassure women, rheumatologists should “get the word out to patients that high-risk interventions are not necessary for every [SLE pregnancy],” she said.
Dr. Petri said she had no disclosures to report.
VANCOUVER, B.C. — Monthly monitoring by rheumatologists of every pregnancy in every woman with systemic lupus erythematosus may be unnecessary, according to Dr. Michelle Petri.
A relatively small list of criteria can distinguish high-risk pregnancies in women with systemic lupus erythematosus (SLE) – ones that carry a higher likelihood of miscarriage, extreme prematurity, and SLE flare – from others, and signal the need for intensive monitoring by obstetricians and rheumatologists, Dr. Petri said at the meeting.
At present, however, there is little effort to make such distinctions, so most SLE pregnancies are subjected to monthly visits to rheumatologists and obstetricians, and, starting at week 26, weekly monitoring by obstetricians.
That's not always necessary; women are subjected to needless anxiety and hospital resources are wasted, Dr. Petri said.
Based on the Hopkins Lupus Cohort, a database that has been tracking several thousand patients with SLE over the past 25 years, Dr. Petri and her colleague, Duke University rheumatologist Dr. Megan Clowse, have identified those factors that truly put women and fetuses at risk during SLE pregnancies.
Pregnancy and the postpartum period are hard on the kidneys of women with SLE, though organ involvement elsewhere in the body tends to lessen, said Dr. Petri, professor of rheumatology at Johns Hopkins University, Baltimore.
“Proteinuria from active lupus significantly increases, and this continues even after delivery,” she added.
Therefore, pregnant women with lupus nephritis truly do need close monitoring. Dr. Petri recommended monthly urine protein-creatinine ratios to detect a worsening of the condition and the need for treatment.
She noted that the ranges on urine dipsticks are too broad; the dipstick is not adequate as a monitoring tool for nephritis.
In terms of fetal health, the risk of miscarriage doubles if, at the first pregnancy visit, a woman is proteinuric, thrombocytopenic, or hypertensive, or has a history of antiphospholipid syndrome.
The risk triples if two or more of these conditions are present, Dr. Petri said. The presence of antithyroid antibodies also increases the risk of miscarriage.
In addition, active SLE, especially if accompanied by anti–double-stranded DNA antibody or low complement levels, predicts extreme prematurity. Autoimmune thyroid disease also appears to be associated with preterm birth.
Screening for the various factors, “we can predict at the first pregnancy visit if there's going to be a poor outcome,” Dr. Petri said.
If the risk factors are present, monthly monitoring by a high-risk obstetrician, followed by weekly monitoring at week 26, are appropriate to gauge if, and when, a rescue delivery is needed.
Otherwise, and absent renal involvement in the pregnant patient, SLE pregnancies may not need to be classified as high risk, Dr. Petri said.
“Since we can stratify women at risk for miscarriage and extreme prematurity, and know the only organ we have to worry about is the kidney, we can come closer to using our resources appropriately,” Dr. Petri said.
To reassure women, rheumatologists should “get the word out to patients that high-risk interventions are not necessary for every [SLE pregnancy],” she said.
Dr. Petri said she had no disclosures to report.
From the International Congress on Systemic Lupus Erythematosus
Why you should recommend flu vaccine to "every single patient"
OCTOBER 2010—ObGyns and other physicians who manage the care of pregnant women should routinely discuss the safety and benefits of seasonal influenza vaccination. That means raising the subject with “every single patient,” said Laura E. Riley, MD, who spoke on behalf of ACOG after a news conference sponsored by the National Foundation for Infectious Diseases (NFID) on October 7.
“That’s the job of providers, of doctors, to put it into perspective—for the patient’s sake as well as for the patient’s family,” said Dr. Riley, who is medical director of labor and delivery and director of ObGyn infectious disease at Massachusetts General Hospital in Boston.
Results of a recent consumer survey undertaken by NFID indicate that the advice of a physician strongly influences patient behavior. Among people who have already been vaccinated with the influenza vaccine or who plan to get vaccinated this season, 76% say they received a recommendation from a health-care provider; only 35% of those who do not plan to get vaccinated report receiving a recommendation from a health-care provider.
Expect flu to strike pregnant women hard
Vaccination against influenza is especially important for pregnant women, said Dr. Riley, for several reasons:
- Mortality from influenza is five times higher among pregnant women who have not been vaccinated than it is among nonpregnant counterparts
- Pregnant women who get the flu are more likely to be hospitalized for severe respiratory illness
- Influenza increases the risk of preterm delivery.
If a patient is concerned about risks associated with being vaccinated against influenza, she can be reassured that benefits far outweigh any potential risks, Dr. Riley said.
“The risks of getting vaccinated in pregnancy aren’t any different than vaccination outside of pregnancy,” she said. “We’ve been giving millions of doses of seasonal flu vaccine to pregnant women for years—at least 10 years. And there’s never been any increase in concern over safety in terms of maternal disease.” The vaccine also is safe for babies, she added.
A new year, a new protocol
This year, for the first time, influenza vaccine is recommended for everyone 6 months of age and older. Infants younger than 6 months cannot be vaccinated, but they can benefit from the antibodies they receive from their vaccinated mothers (if the mothers were vaccinated during pregnancy, or if the infant is breastfeeding).
This year’s vaccine is an “all-in-one” product; patients do not need to get a separate H1N1 vaccine. The 2010 vaccine provides coverage against three strains of virus:
- influenza B virus
- influenza A H3N2
- influenza A H1N1 (2009 variant).
These strains were chosen for inclusion in the vaccine because they are very similar to the viruses circulating in the United States and abroad,” said Daniel Jernigan, MD, MPH, who spoke at the news conference. Dr. Jernigan is deputy director of the influenza division at the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention.
The fact that the vaccine provides coverage so specific to what is happening in the community is “very good news,” he added. “We also know that the viruses that we’re seeing are susceptible to antiviral drugs.”
Don’t forget about pertussis
Although pertussis typically is not life-threatening in adults, adults and adolescents who have the disease can pass it to infants who have not been immunized—among whom it can be especially severe. In recent years, 91% of all deaths from pertussis have been in infants 6 months and younger. In addition, more than 50% of infants younger than 1 year who contract pertussis must be hospitalized.
For that reason, it is important that every woman be immunized with Tdap immediately postpartum if her last tetanus-diphtheria booster was more than 2 years earlier.
We want to hear from you! Tell us what you think.
OCTOBER 2010—ObGyns and other physicians who manage the care of pregnant women should routinely discuss the safety and benefits of seasonal influenza vaccination. That means raising the subject with “every single patient,” said Laura E. Riley, MD, who spoke on behalf of ACOG after a news conference sponsored by the National Foundation for Infectious Diseases (NFID) on October 7.
“That’s the job of providers, of doctors, to put it into perspective—for the patient’s sake as well as for the patient’s family,” said Dr. Riley, who is medical director of labor and delivery and director of ObGyn infectious disease at Massachusetts General Hospital in Boston.
Results of a recent consumer survey undertaken by NFID indicate that the advice of a physician strongly influences patient behavior. Among people who have already been vaccinated with the influenza vaccine or who plan to get vaccinated this season, 76% say they received a recommendation from a health-care provider; only 35% of those who do not plan to get vaccinated report receiving a recommendation from a health-care provider.
Expect flu to strike pregnant women hard
Vaccination against influenza is especially important for pregnant women, said Dr. Riley, for several reasons:
- Mortality from influenza is five times higher among pregnant women who have not been vaccinated than it is among nonpregnant counterparts
- Pregnant women who get the flu are more likely to be hospitalized for severe respiratory illness
- Influenza increases the risk of preterm delivery.
If a patient is concerned about risks associated with being vaccinated against influenza, she can be reassured that benefits far outweigh any potential risks, Dr. Riley said.
“The risks of getting vaccinated in pregnancy aren’t any different than vaccination outside of pregnancy,” she said. “We’ve been giving millions of doses of seasonal flu vaccine to pregnant women for years—at least 10 years. And there’s never been any increase in concern over safety in terms of maternal disease.” The vaccine also is safe for babies, she added.
A new year, a new protocol
This year, for the first time, influenza vaccine is recommended for everyone 6 months of age and older. Infants younger than 6 months cannot be vaccinated, but they can benefit from the antibodies they receive from their vaccinated mothers (if the mothers were vaccinated during pregnancy, or if the infant is breastfeeding).
This year’s vaccine is an “all-in-one” product; patients do not need to get a separate H1N1 vaccine. The 2010 vaccine provides coverage against three strains of virus:
- influenza B virus
- influenza A H3N2
- influenza A H1N1 (2009 variant).
These strains were chosen for inclusion in the vaccine because they are very similar to the viruses circulating in the United States and abroad,” said Daniel Jernigan, MD, MPH, who spoke at the news conference. Dr. Jernigan is deputy director of the influenza division at the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention.
The fact that the vaccine provides coverage so specific to what is happening in the community is “very good news,” he added. “We also know that the viruses that we’re seeing are susceptible to antiviral drugs.”
Don’t forget about pertussis
Although pertussis typically is not life-threatening in adults, adults and adolescents who have the disease can pass it to infants who have not been immunized—among whom it can be especially severe. In recent years, 91% of all deaths from pertussis have been in infants 6 months and younger. In addition, more than 50% of infants younger than 1 year who contract pertussis must be hospitalized.
For that reason, it is important that every woman be immunized with Tdap immediately postpartum if her last tetanus-diphtheria booster was more than 2 years earlier.
We want to hear from you! Tell us what you think.
OCTOBER 2010—ObGyns and other physicians who manage the care of pregnant women should routinely discuss the safety and benefits of seasonal influenza vaccination. That means raising the subject with “every single patient,” said Laura E. Riley, MD, who spoke on behalf of ACOG after a news conference sponsored by the National Foundation for Infectious Diseases (NFID) on October 7.
“That’s the job of providers, of doctors, to put it into perspective—for the patient’s sake as well as for the patient’s family,” said Dr. Riley, who is medical director of labor and delivery and director of ObGyn infectious disease at Massachusetts General Hospital in Boston.
Results of a recent consumer survey undertaken by NFID indicate that the advice of a physician strongly influences patient behavior. Among people who have already been vaccinated with the influenza vaccine or who plan to get vaccinated this season, 76% say they received a recommendation from a health-care provider; only 35% of those who do not plan to get vaccinated report receiving a recommendation from a health-care provider.
Expect flu to strike pregnant women hard
Vaccination against influenza is especially important for pregnant women, said Dr. Riley, for several reasons:
- Mortality from influenza is five times higher among pregnant women who have not been vaccinated than it is among nonpregnant counterparts
- Pregnant women who get the flu are more likely to be hospitalized for severe respiratory illness
- Influenza increases the risk of preterm delivery.
If a patient is concerned about risks associated with being vaccinated against influenza, she can be reassured that benefits far outweigh any potential risks, Dr. Riley said.
“The risks of getting vaccinated in pregnancy aren’t any different than vaccination outside of pregnancy,” she said. “We’ve been giving millions of doses of seasonal flu vaccine to pregnant women for years—at least 10 years. And there’s never been any increase in concern over safety in terms of maternal disease.” The vaccine also is safe for babies, she added.
A new year, a new protocol
This year, for the first time, influenza vaccine is recommended for everyone 6 months of age and older. Infants younger than 6 months cannot be vaccinated, but they can benefit from the antibodies they receive from their vaccinated mothers (if the mothers were vaccinated during pregnancy, or if the infant is breastfeeding).
This year’s vaccine is an “all-in-one” product; patients do not need to get a separate H1N1 vaccine. The 2010 vaccine provides coverage against three strains of virus:
- influenza B virus
- influenza A H3N2
- influenza A H1N1 (2009 variant).
These strains were chosen for inclusion in the vaccine because they are very similar to the viruses circulating in the United States and abroad,” said Daniel Jernigan, MD, MPH, who spoke at the news conference. Dr. Jernigan is deputy director of the influenza division at the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention.
The fact that the vaccine provides coverage so specific to what is happening in the community is “very good news,” he added. “We also know that the viruses that we’re seeing are susceptible to antiviral drugs.”
Don’t forget about pertussis
Although pertussis typically is not life-threatening in adults, adults and adolescents who have the disease can pass it to infants who have not been immunized—among whom it can be especially severe. In recent years, 91% of all deaths from pertussis have been in infants 6 months and younger. In addition, more than 50% of infants younger than 1 year who contract pertussis must be hospitalized.
For that reason, it is important that every woman be immunized with Tdap immediately postpartum if her last tetanus-diphtheria booster was more than 2 years earlier.
We want to hear from you! Tell us what you think.
CP Risks Are Higher at 'Early' and 'Late' Term
Among births that occur during the term and postterm range of 37-44 weeks' gestation, the risk of cerebral palsy is lowest at 40 weeks and highest at the “early” extreme of 37-38 weeks and the “late” extreme of 42 weeks or more, said Dr. Dag Moster of the University of Bergen, Norway, and his associates.
Preterm delivery is a well-established risk factor for CP, but there is scant information on CP risk within the term range, even though most cases of CP occur in children born at term. Dr. Moster and his colleagues examined the issue using data in a nationwide Norwegian registry covering 1,682,441 singleton live births at 37-44 weeks that took place between 1967 and 2001, as well as a medical registry of all the disabled people in the country born during the same period.
There were 1,938 infants in this cohort who were eventually diagnosed as having CP, for an overall prevalence of 1.15 cases per 1,000 live births (JAMA 2010;304:976-82). Delivery at 40 weeks was associated with the lowest CP risk, with a prevalence of 0.99 cases per 1,000 live births.
In comparison, the prevalence of CP at 37 weeks' gestation was 1.91 per 1,000 (for a relative risk of 1.9) and at 38 weeks was 1.25 per 1,000 (for a relative risk of 1.3). Similarly, the prevalence of CP at 42 weeks was 1.36 per 1,000 live births (for a relative risk of 1.4) and after 42 weeks was 1.44 per 1,000 live births (for a relative risk of 1.4).
Children with CP had lower mean birth weights (3,437 g) compared with children without CP (3,585 g) and smaller head circumferences (35.1 cm) compared with children without CP (35.3 cm). Children with CP were 82 times more likely to have had low Apgar scores (less than 4) and were eight times more likely to have been transferred to pediatric units after delivery. Results were essentially the same in a further analysis of the data after adjustment for possible confounders such as maternal age, marital status, and education level.
“One possible interpretation is that delivery too early or too late, even within the limited range of term and postterm births, increases the risk of CP.
“However, an equally plausible interpretation is that fetuses predisposed to CP have a disturbance in the timing of their delivery, which causes them to be more often delivered early or late,” Dr. Moster and his associates said.
“This apparently happens with other fetal conditions: There is a U-shaped pattern in the risk of congenital anomalies with gestational age after 37 weeks. Since congenital anomalies are not caused by the timing of delivery, the most plausible explanation is reverse causation: Malformed infants experience disruptions in their time of delivery, with increased chance of delivery either earlier or later than 40 weeks,” the researchers said.
“Although the forces that regulate timing of a normal delivery are poorly understood, it appears that the types of malformations most likely to disrupt the timing of delivery often involve cerebral function.
For example, anencephalic fetuses have a tendency to be born post term, children with Trisomy 18 to be born preterm or post term, and children with Down syndrome to be born early.
“It is possible that cerebral damage later expressed as CP similarly disrupts time of delivery,” Dr. Moster and his associates said.
The lower birth weight and smaller head circumference among CP cases in this cohort “suggest that these children differ from non-CP infants even before birth,” they added.
Dr. Moster and his associates emphasized that it would be incorrect to extrapolate from these study findings that intervening to alter the time of delivery could reduce the rate of CP.
Disclosures: This study was sponsored by the National Institutes of Health, the National Institute of Environmental Health Sciences, the Unger-Vetlesen Charitable Fund, the U.S.-Norway Fulbright Foundation, the Norwegian Society of Pediatricians, the University of Bergen, and the Research Council of Norway. No financial conflicts of interest were reported.
Among births that occur during the term and postterm range of 37-44 weeks' gestation, the risk of cerebral palsy is lowest at 40 weeks and highest at the “early” extreme of 37-38 weeks and the “late” extreme of 42 weeks or more, said Dr. Dag Moster of the University of Bergen, Norway, and his associates.
Preterm delivery is a well-established risk factor for CP, but there is scant information on CP risk within the term range, even though most cases of CP occur in children born at term. Dr. Moster and his colleagues examined the issue using data in a nationwide Norwegian registry covering 1,682,441 singleton live births at 37-44 weeks that took place between 1967 and 2001, as well as a medical registry of all the disabled people in the country born during the same period.
There were 1,938 infants in this cohort who were eventually diagnosed as having CP, for an overall prevalence of 1.15 cases per 1,000 live births (JAMA 2010;304:976-82). Delivery at 40 weeks was associated with the lowest CP risk, with a prevalence of 0.99 cases per 1,000 live births.
In comparison, the prevalence of CP at 37 weeks' gestation was 1.91 per 1,000 (for a relative risk of 1.9) and at 38 weeks was 1.25 per 1,000 (for a relative risk of 1.3). Similarly, the prevalence of CP at 42 weeks was 1.36 per 1,000 live births (for a relative risk of 1.4) and after 42 weeks was 1.44 per 1,000 live births (for a relative risk of 1.4).
Children with CP had lower mean birth weights (3,437 g) compared with children without CP (3,585 g) and smaller head circumferences (35.1 cm) compared with children without CP (35.3 cm). Children with CP were 82 times more likely to have had low Apgar scores (less than 4) and were eight times more likely to have been transferred to pediatric units after delivery. Results were essentially the same in a further analysis of the data after adjustment for possible confounders such as maternal age, marital status, and education level.
“One possible interpretation is that delivery too early or too late, even within the limited range of term and postterm births, increases the risk of CP.
“However, an equally plausible interpretation is that fetuses predisposed to CP have a disturbance in the timing of their delivery, which causes them to be more often delivered early or late,” Dr. Moster and his associates said.
“This apparently happens with other fetal conditions: There is a U-shaped pattern in the risk of congenital anomalies with gestational age after 37 weeks. Since congenital anomalies are not caused by the timing of delivery, the most plausible explanation is reverse causation: Malformed infants experience disruptions in their time of delivery, with increased chance of delivery either earlier or later than 40 weeks,” the researchers said.
“Although the forces that regulate timing of a normal delivery are poorly understood, it appears that the types of malformations most likely to disrupt the timing of delivery often involve cerebral function.
For example, anencephalic fetuses have a tendency to be born post term, children with Trisomy 18 to be born preterm or post term, and children with Down syndrome to be born early.
“It is possible that cerebral damage later expressed as CP similarly disrupts time of delivery,” Dr. Moster and his associates said.
The lower birth weight and smaller head circumference among CP cases in this cohort “suggest that these children differ from non-CP infants even before birth,” they added.
Dr. Moster and his associates emphasized that it would be incorrect to extrapolate from these study findings that intervening to alter the time of delivery could reduce the rate of CP.
Disclosures: This study was sponsored by the National Institutes of Health, the National Institute of Environmental Health Sciences, the Unger-Vetlesen Charitable Fund, the U.S.-Norway Fulbright Foundation, the Norwegian Society of Pediatricians, the University of Bergen, and the Research Council of Norway. No financial conflicts of interest were reported.
Among births that occur during the term and postterm range of 37-44 weeks' gestation, the risk of cerebral palsy is lowest at 40 weeks and highest at the “early” extreme of 37-38 weeks and the “late” extreme of 42 weeks or more, said Dr. Dag Moster of the University of Bergen, Norway, and his associates.
Preterm delivery is a well-established risk factor for CP, but there is scant information on CP risk within the term range, even though most cases of CP occur in children born at term. Dr. Moster and his colleagues examined the issue using data in a nationwide Norwegian registry covering 1,682,441 singleton live births at 37-44 weeks that took place between 1967 and 2001, as well as a medical registry of all the disabled people in the country born during the same period.
There were 1,938 infants in this cohort who were eventually diagnosed as having CP, for an overall prevalence of 1.15 cases per 1,000 live births (JAMA 2010;304:976-82). Delivery at 40 weeks was associated with the lowest CP risk, with a prevalence of 0.99 cases per 1,000 live births.
In comparison, the prevalence of CP at 37 weeks' gestation was 1.91 per 1,000 (for a relative risk of 1.9) and at 38 weeks was 1.25 per 1,000 (for a relative risk of 1.3). Similarly, the prevalence of CP at 42 weeks was 1.36 per 1,000 live births (for a relative risk of 1.4) and after 42 weeks was 1.44 per 1,000 live births (for a relative risk of 1.4).
Children with CP had lower mean birth weights (3,437 g) compared with children without CP (3,585 g) and smaller head circumferences (35.1 cm) compared with children without CP (35.3 cm). Children with CP were 82 times more likely to have had low Apgar scores (less than 4) and were eight times more likely to have been transferred to pediatric units after delivery. Results were essentially the same in a further analysis of the data after adjustment for possible confounders such as maternal age, marital status, and education level.
“One possible interpretation is that delivery too early or too late, even within the limited range of term and postterm births, increases the risk of CP.
“However, an equally plausible interpretation is that fetuses predisposed to CP have a disturbance in the timing of their delivery, which causes them to be more often delivered early or late,” Dr. Moster and his associates said.
“This apparently happens with other fetal conditions: There is a U-shaped pattern in the risk of congenital anomalies with gestational age after 37 weeks. Since congenital anomalies are not caused by the timing of delivery, the most plausible explanation is reverse causation: Malformed infants experience disruptions in their time of delivery, with increased chance of delivery either earlier or later than 40 weeks,” the researchers said.
“Although the forces that regulate timing of a normal delivery are poorly understood, it appears that the types of malformations most likely to disrupt the timing of delivery often involve cerebral function.
For example, anencephalic fetuses have a tendency to be born post term, children with Trisomy 18 to be born preterm or post term, and children with Down syndrome to be born early.
“It is possible that cerebral damage later expressed as CP similarly disrupts time of delivery,” Dr. Moster and his associates said.
The lower birth weight and smaller head circumference among CP cases in this cohort “suggest that these children differ from non-CP infants even before birth,” they added.
Dr. Moster and his associates emphasized that it would be incorrect to extrapolate from these study findings that intervening to alter the time of delivery could reduce the rate of CP.
Disclosures: This study was sponsored by the National Institutes of Health, the National Institute of Environmental Health Sciences, the Unger-Vetlesen Charitable Fund, the U.S.-Norway Fulbright Foundation, the Norwegian Society of Pediatricians, the University of Bergen, and the Research Council of Norway. No financial conflicts of interest were reported.
From JAMA
External Cephalic Version: No Drop in C-Sections
Major Finding: Women randomized to early or late external cephalic version had nonsignificant differences in cesarean section rate (52% vs. 56%), with a trend toward more preterm deliveries in the early-version group.
Data Source: A study that randomized 1,532 women with breech presentations to either an early external cephalic version or a later version performed at 37 weeks.
Disclosures: Dr. Carson said he had no relevant disclosures. The trial was funded by the Canadian Institutes of Health Research.
MONTREAL — Early external cephalic version increases the likelihood of cephalic presentation at birth, but does not result in fewer cesarean sections compared with later cephalic version, based on the results of an international, multicenter, randomized controlled trial.
In addition, there was a trend toward greater risk of preterm birth when the procedure was done early, defined as between the 34th and 35th weeks, reported Dr. George Carson, one of the investigators on the Early External Cephalic Version 2 (ECV2) Trial.
“This is actually very disappointing,” he said in an interview at the meeting.
“It is worth trying to investigate why turning the baby didn't result in a reduction in cesarean sections. Obviously the purpose of this was not to turn the baby – it was to reduce cesarean sections – and that didn't happen, and that's disappointing.”
The study randomized 1,532 women with breech presentations to either an early version or a later version performed at 37 weeks. The primary end point was the rate of cesarean section, with a secondary end point of preterm birth.
“The concern was that in performing version one might precipitate preterm birth, and so this could be the adverse effect of the attempt to turn the baby,” noted Dr. Carson, director of maternal-fetal medicine at Regina (Sask.) General Hospital.
Baseline characteristics including parity, types of breech presentation, and anterior placenta were similar in both groups.
Cephalic presentation at the time of delivery, due to either successful external version or spontaneous version, was higher in the early-version group (59% vs. 51%), and the difference reached statistical significance, said Dr. Carson. However, there was not a statistically significant difference in the cesarean section rate: 52% in the early group and 56% in the late group.
“More women delivered vaginally than was anticipated in the delayed group – due to spontaneous conversion and a small number of women who decided to deliver vaginally even though their baby was still breech,” he said, adding that overall, the cesarean section rate was high.
“Very few of these were done for nonreassuring monitoring. They were done in places that do a lot of sections anyway, so being cephalic was not in any way a guarantee that one wouldn't have a section done,” he said.
The increased rate of preterm delivery in the early-version group (6.5% vs. 4.4% in the late group) was not statistically significant, but it strengthens the argument against attempting an early cephalic version, said Dr. Carson.
“What I tell the women that I am trying to do a version on is, if we don't do it … they've got about a 70% chance of a cesarean section. If we do it, that could be reduced to about 50%. But my chance of getting the fetus around is only about 50%.
“And if we push hard on the uterus, maybe we could make them deliver prematurely. It won't be very premature, but it's still better to be term than 35 weeks,” he said.
Major Finding: Women randomized to early or late external cephalic version had nonsignificant differences in cesarean section rate (52% vs. 56%), with a trend toward more preterm deliveries in the early-version group.
Data Source: A study that randomized 1,532 women with breech presentations to either an early external cephalic version or a later version performed at 37 weeks.
Disclosures: Dr. Carson said he had no relevant disclosures. The trial was funded by the Canadian Institutes of Health Research.
MONTREAL — Early external cephalic version increases the likelihood of cephalic presentation at birth, but does not result in fewer cesarean sections compared with later cephalic version, based on the results of an international, multicenter, randomized controlled trial.
In addition, there was a trend toward greater risk of preterm birth when the procedure was done early, defined as between the 34th and 35th weeks, reported Dr. George Carson, one of the investigators on the Early External Cephalic Version 2 (ECV2) Trial.
“This is actually very disappointing,” he said in an interview at the meeting.
“It is worth trying to investigate why turning the baby didn't result in a reduction in cesarean sections. Obviously the purpose of this was not to turn the baby – it was to reduce cesarean sections – and that didn't happen, and that's disappointing.”
The study randomized 1,532 women with breech presentations to either an early version or a later version performed at 37 weeks. The primary end point was the rate of cesarean section, with a secondary end point of preterm birth.
“The concern was that in performing version one might precipitate preterm birth, and so this could be the adverse effect of the attempt to turn the baby,” noted Dr. Carson, director of maternal-fetal medicine at Regina (Sask.) General Hospital.
Baseline characteristics including parity, types of breech presentation, and anterior placenta were similar in both groups.
Cephalic presentation at the time of delivery, due to either successful external version or spontaneous version, was higher in the early-version group (59% vs. 51%), and the difference reached statistical significance, said Dr. Carson. However, there was not a statistically significant difference in the cesarean section rate: 52% in the early group and 56% in the late group.
“More women delivered vaginally than was anticipated in the delayed group – due to spontaneous conversion and a small number of women who decided to deliver vaginally even though their baby was still breech,” he said, adding that overall, the cesarean section rate was high.
“Very few of these were done for nonreassuring monitoring. They were done in places that do a lot of sections anyway, so being cephalic was not in any way a guarantee that one wouldn't have a section done,” he said.
The increased rate of preterm delivery in the early-version group (6.5% vs. 4.4% in the late group) was not statistically significant, but it strengthens the argument against attempting an early cephalic version, said Dr. Carson.
“What I tell the women that I am trying to do a version on is, if we don't do it … they've got about a 70% chance of a cesarean section. If we do it, that could be reduced to about 50%. But my chance of getting the fetus around is only about 50%.
“And if we push hard on the uterus, maybe we could make them deliver prematurely. It won't be very premature, but it's still better to be term than 35 weeks,” he said.
Major Finding: Women randomized to early or late external cephalic version had nonsignificant differences in cesarean section rate (52% vs. 56%), with a trend toward more preterm deliveries in the early-version group.
Data Source: A study that randomized 1,532 women with breech presentations to either an early external cephalic version or a later version performed at 37 weeks.
Disclosures: Dr. Carson said he had no relevant disclosures. The trial was funded by the Canadian Institutes of Health Research.
MONTREAL — Early external cephalic version increases the likelihood of cephalic presentation at birth, but does not result in fewer cesarean sections compared with later cephalic version, based on the results of an international, multicenter, randomized controlled trial.
In addition, there was a trend toward greater risk of preterm birth when the procedure was done early, defined as between the 34th and 35th weeks, reported Dr. George Carson, one of the investigators on the Early External Cephalic Version 2 (ECV2) Trial.
“This is actually very disappointing,” he said in an interview at the meeting.
“It is worth trying to investigate why turning the baby didn't result in a reduction in cesarean sections. Obviously the purpose of this was not to turn the baby – it was to reduce cesarean sections – and that didn't happen, and that's disappointing.”
The study randomized 1,532 women with breech presentations to either an early version or a later version performed at 37 weeks. The primary end point was the rate of cesarean section, with a secondary end point of preterm birth.
“The concern was that in performing version one might precipitate preterm birth, and so this could be the adverse effect of the attempt to turn the baby,” noted Dr. Carson, director of maternal-fetal medicine at Regina (Sask.) General Hospital.
Baseline characteristics including parity, types of breech presentation, and anterior placenta were similar in both groups.
Cephalic presentation at the time of delivery, due to either successful external version or spontaneous version, was higher in the early-version group (59% vs. 51%), and the difference reached statistical significance, said Dr. Carson. However, there was not a statistically significant difference in the cesarean section rate: 52% in the early group and 56% in the late group.
“More women delivered vaginally than was anticipated in the delayed group – due to spontaneous conversion and a small number of women who decided to deliver vaginally even though their baby was still breech,” he said, adding that overall, the cesarean section rate was high.
“Very few of these were done for nonreassuring monitoring. They were done in places that do a lot of sections anyway, so being cephalic was not in any way a guarantee that one wouldn't have a section done,” he said.
The increased rate of preterm delivery in the early-version group (6.5% vs. 4.4% in the late group) was not statistically significant, but it strengthens the argument against attempting an early cephalic version, said Dr. Carson.
“What I tell the women that I am trying to do a version on is, if we don't do it … they've got about a 70% chance of a cesarean section. If we do it, that could be reduced to about 50%. But my chance of getting the fetus around is only about 50%.
“And if we push hard on the uterus, maybe we could make them deliver prematurely. It won't be very premature, but it's still better to be term than 35 weeks,” he said.
From the Annual Meeting of the Society of Obstetricians and Gynaecologists of Canada
Monitor Newer Antiepileptics Closely
SAN FRANCISCO — Third-generation antiepileptic drugs such as lamotrigine and oxcarbazepine are less likely than earlier treatments to cause congenital malformations, but serum levels of the newer drugs must be monitored more closely during pregnancy to avoid other problems.
“The good news is that the third-generation drugs seem to have a spectrum of safety that we did not see with earlier generations,” said Dr. Yasser Y. El-Sayed. “It took awhile for this to be evaluated, as many of these third-generation drugs were part of polytherapy. They were add-on treatments. It seems that with these newer drugs, the incidence of congenital malformation is within the expected range for the general population.”
The risk of birth defects with older antiepileptics has been reported to be 4%-9%, double to triple the 2%-3% rate of birth defects in the general population. Therapy with four or more antiepileptic drugs boosts the risk for malformations to as high as 25%, said Dr. El-Sayed, professor of maternal-fetal medicine and obstetrics at Stanford (Calif.) University. High peak serum levels of the drugs also increase risk, he said.
Valproic acid, in particular, stands out among older antiepileptics for elevating risk of congenital malformations. A 2009 report by the quality standards subcommittee of the American Academy of Neurology and the American Epilepsy Society recommended that physicians avoid valproic acid and polytherapy for women in their first trimesters of pregnancy, if possible, to reduce overall risk of congenital malformations.
The report also said to avoid phenytoin, carbamazepine, and phenobarbital during the first trimester to reduce risks of specific anomalies, Dr. El-Sayed said at the meeting, which was sponsored by the University of California, San Francisco.”
“Having said that, the majority of women on these drugs will not have malformations, so if that's the drug you need to use to control the seizure, then so be it,” he added. Many women hear about the teratogenic potential of antiepileptics and decide to stop epilepsy treatment entirely. “The problem is that seizure activity is hugely problematic” in pregnancy, with potentially grave consequences for both mother and baby.
The most practical approach to treating pregnant women with epilepsy is to pick the single most effective drug and use it at the lowest possible dose, Dr. El-Sayed suggested.
Unlike the older drugs, third-generation antiepileptics have not shown their risks for anomalies to be dose dependent, he added. It's important with the older antiepileptics to keep the whole clinical picture in mind and not respond only to changes in serum levels.
The story is very different with the newer agents. “Their management in pregnancy is much more problematic. The drop in serum levels can be dramatic, and unlike with the older drugs, we tend to see an increase in seizures,” he said. “They require much more stringent monitoring in pregnancy and a much more reactionary approach to lower serum levels.”
Assessing a patient's therapeutic serum level for a drug before conception helps guide treatment during pregnancy. At a minimum, check serum levels at the beginning of each trimester, or monthly for lamotrigine or oxcarbazepine, Dr. El-Sayed advised. Check levels again in the last month of pregnancy and through postpartum week 8, with close attention to third-generation agents because “there tends to be a reactive toxicity post partum. If you've increased the dose during pregnancy, post partum you may run into some toxicity.” Get free fraction levels, if available, and not just total fraction measurements, he said.
Besides sticking to monotherapy and more closely monitoring newer antiepileptic drug levels, good management involves partnering between obstetricians and neurologists in the care of these patients, Dr. El-Sayed added.
Most women with epilepsy give birth safely and successfully, but 1%-2% will develop tonic-clonic seizure during labor, and another 1%-2% will do so during the 24 hours after delivery.
“This can be from stress or lack of sleep, but also from failure to continue adequate administration of antiepileptic drugs during labor,” Dr. El-Sayed said.
Don't forget to give medicine in labor, and consider intravenous or intramuscular administration if needed, he noted.
Disclosures: Dr. El-Sayed said he has no relevant conflicts of interest.
SAN FRANCISCO — Third-generation antiepileptic drugs such as lamotrigine and oxcarbazepine are less likely than earlier treatments to cause congenital malformations, but serum levels of the newer drugs must be monitored more closely during pregnancy to avoid other problems.
“The good news is that the third-generation drugs seem to have a spectrum of safety that we did not see with earlier generations,” said Dr. Yasser Y. El-Sayed. “It took awhile for this to be evaluated, as many of these third-generation drugs were part of polytherapy. They were add-on treatments. It seems that with these newer drugs, the incidence of congenital malformation is within the expected range for the general population.”
The risk of birth defects with older antiepileptics has been reported to be 4%-9%, double to triple the 2%-3% rate of birth defects in the general population. Therapy with four or more antiepileptic drugs boosts the risk for malformations to as high as 25%, said Dr. El-Sayed, professor of maternal-fetal medicine and obstetrics at Stanford (Calif.) University. High peak serum levels of the drugs also increase risk, he said.
Valproic acid, in particular, stands out among older antiepileptics for elevating risk of congenital malformations. A 2009 report by the quality standards subcommittee of the American Academy of Neurology and the American Epilepsy Society recommended that physicians avoid valproic acid and polytherapy for women in their first trimesters of pregnancy, if possible, to reduce overall risk of congenital malformations.
The report also said to avoid phenytoin, carbamazepine, and phenobarbital during the first trimester to reduce risks of specific anomalies, Dr. El-Sayed said at the meeting, which was sponsored by the University of California, San Francisco.”
“Having said that, the majority of women on these drugs will not have malformations, so if that's the drug you need to use to control the seizure, then so be it,” he added. Many women hear about the teratogenic potential of antiepileptics and decide to stop epilepsy treatment entirely. “The problem is that seizure activity is hugely problematic” in pregnancy, with potentially grave consequences for both mother and baby.
The most practical approach to treating pregnant women with epilepsy is to pick the single most effective drug and use it at the lowest possible dose, Dr. El-Sayed suggested.
Unlike the older drugs, third-generation antiepileptics have not shown their risks for anomalies to be dose dependent, he added. It's important with the older antiepileptics to keep the whole clinical picture in mind and not respond only to changes in serum levels.
The story is very different with the newer agents. “Their management in pregnancy is much more problematic. The drop in serum levels can be dramatic, and unlike with the older drugs, we tend to see an increase in seizures,” he said. “They require much more stringent monitoring in pregnancy and a much more reactionary approach to lower serum levels.”
Assessing a patient's therapeutic serum level for a drug before conception helps guide treatment during pregnancy. At a minimum, check serum levels at the beginning of each trimester, or monthly for lamotrigine or oxcarbazepine, Dr. El-Sayed advised. Check levels again in the last month of pregnancy and through postpartum week 8, with close attention to third-generation agents because “there tends to be a reactive toxicity post partum. If you've increased the dose during pregnancy, post partum you may run into some toxicity.” Get free fraction levels, if available, and not just total fraction measurements, he said.
Besides sticking to monotherapy and more closely monitoring newer antiepileptic drug levels, good management involves partnering between obstetricians and neurologists in the care of these patients, Dr. El-Sayed added.
Most women with epilepsy give birth safely and successfully, but 1%-2% will develop tonic-clonic seizure during labor, and another 1%-2% will do so during the 24 hours after delivery.
“This can be from stress or lack of sleep, but also from failure to continue adequate administration of antiepileptic drugs during labor,” Dr. El-Sayed said.
Don't forget to give medicine in labor, and consider intravenous or intramuscular administration if needed, he noted.
Disclosures: Dr. El-Sayed said he has no relevant conflicts of interest.
SAN FRANCISCO — Third-generation antiepileptic drugs such as lamotrigine and oxcarbazepine are less likely than earlier treatments to cause congenital malformations, but serum levels of the newer drugs must be monitored more closely during pregnancy to avoid other problems.
“The good news is that the third-generation drugs seem to have a spectrum of safety that we did not see with earlier generations,” said Dr. Yasser Y. El-Sayed. “It took awhile for this to be evaluated, as many of these third-generation drugs were part of polytherapy. They were add-on treatments. It seems that with these newer drugs, the incidence of congenital malformation is within the expected range for the general population.”
The risk of birth defects with older antiepileptics has been reported to be 4%-9%, double to triple the 2%-3% rate of birth defects in the general population. Therapy with four or more antiepileptic drugs boosts the risk for malformations to as high as 25%, said Dr. El-Sayed, professor of maternal-fetal medicine and obstetrics at Stanford (Calif.) University. High peak serum levels of the drugs also increase risk, he said.
Valproic acid, in particular, stands out among older antiepileptics for elevating risk of congenital malformations. A 2009 report by the quality standards subcommittee of the American Academy of Neurology and the American Epilepsy Society recommended that physicians avoid valproic acid and polytherapy for women in their first trimesters of pregnancy, if possible, to reduce overall risk of congenital malformations.
The report also said to avoid phenytoin, carbamazepine, and phenobarbital during the first trimester to reduce risks of specific anomalies, Dr. El-Sayed said at the meeting, which was sponsored by the University of California, San Francisco.”
“Having said that, the majority of women on these drugs will not have malformations, so if that's the drug you need to use to control the seizure, then so be it,” he added. Many women hear about the teratogenic potential of antiepileptics and decide to stop epilepsy treatment entirely. “The problem is that seizure activity is hugely problematic” in pregnancy, with potentially grave consequences for both mother and baby.
The most practical approach to treating pregnant women with epilepsy is to pick the single most effective drug and use it at the lowest possible dose, Dr. El-Sayed suggested.
Unlike the older drugs, third-generation antiepileptics have not shown their risks for anomalies to be dose dependent, he added. It's important with the older antiepileptics to keep the whole clinical picture in mind and not respond only to changes in serum levels.
The story is very different with the newer agents. “Their management in pregnancy is much more problematic. The drop in serum levels can be dramatic, and unlike with the older drugs, we tend to see an increase in seizures,” he said. “They require much more stringent monitoring in pregnancy and a much more reactionary approach to lower serum levels.”
Assessing a patient's therapeutic serum level for a drug before conception helps guide treatment during pregnancy. At a minimum, check serum levels at the beginning of each trimester, or monthly for lamotrigine or oxcarbazepine, Dr. El-Sayed advised. Check levels again in the last month of pregnancy and through postpartum week 8, with close attention to third-generation agents because “there tends to be a reactive toxicity post partum. If you've increased the dose during pregnancy, post partum you may run into some toxicity.” Get free fraction levels, if available, and not just total fraction measurements, he said.
Besides sticking to monotherapy and more closely monitoring newer antiepileptic drug levels, good management involves partnering between obstetricians and neurologists in the care of these patients, Dr. El-Sayed added.
Most women with epilepsy give birth safely and successfully, but 1%-2% will develop tonic-clonic seizure during labor, and another 1%-2% will do so during the 24 hours after delivery.
“This can be from stress or lack of sleep, but also from failure to continue adequate administration of antiepileptic drugs during labor,” Dr. El-Sayed said.
Don't forget to give medicine in labor, and consider intravenous or intramuscular administration if needed, he noted.
Disclosures: Dr. El-Sayed said he has no relevant conflicts of interest.
From a Meeting on Antepartum and Intrapartum Management
Are ObGyns offering the range of treatment options for early pregnancy failure?
One in every four women experiences EPF. Although office uterine evacuation and misoprostol administration are less invasive and less expensive alternatives to traditional OR evacuation, it is not clear how extensively clinicians employ these options in the United States.1,2
In 2008, Dalton and colleagues surveyed ObGyns, certified nurse midwives (CNMs), and family physicians (FPs) in the United States who had evaluated or treated, or both, a woman for EPF in the preceding 6 months. They achieved response rates of 51.0%, 70.9%, and 53.5%, respectively. Evaluable respondents had a mean age of 49 to 50 years and included 309 ObGyns (46.9% of whom were female), 368 CNMs (97.8% female), and 299 FPs (43.6% female).
Overall, approximately one third of respondents believe that office evacuation is riskier than OR evacuation. In addition, 65.7% of ObGyns believe that most patients prefer OR evacuation, compared with 46.2% and 43.1% of CNMs and FPs, respectively (P < .001). Among ObGyns, an adjusted analysis estimated the likelihood of providing office evacuation to be five times higher among those who have undergone training in induced abortion (P < .05). As for misoprostol for EPF, about two thirds of respondents overall believe that it is safe.
Dalton and associates posit that providers “perceive that their personal treatment preferences are different than their patients’. Whether this discordance results in women undergoing operating room uterine evacuation more often than is necessary or preferred could not be assessed by this study.” However, the authors also assert that, “given that providers affect treatment choice greatly, it is plausible that provider treatment preferences are an important influence on current treatment patterns.”
Certainly, women have diverse preferences for how EPF is managed, but many do find office evacuation and misoprostol to be acceptable methods. Accordingly, we should offer all options to them. As the investigators in this study suggest, we may need to focus on correcting inaccurate beliefs about these modalities among providers to increase their willingness to offer them.
The findings of this survey also underscore the fact that training programs that do not teach induced abortion—or that allow trainees to opt out of such training—can compromise the care provided to women who have EPF.—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Zhang J, Gilles JM, Barnhart K, et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
2. Harris LH, Dalton VK, Johnson TR. Surgical management of early pregnancy failure: history, politics, and safe, cost-effective care. Am J Obstet Gynecol. 2007;196(5):445.e1–e5.-
One in every four women experiences EPF. Although office uterine evacuation and misoprostol administration are less invasive and less expensive alternatives to traditional OR evacuation, it is not clear how extensively clinicians employ these options in the United States.1,2
In 2008, Dalton and colleagues surveyed ObGyns, certified nurse midwives (CNMs), and family physicians (FPs) in the United States who had evaluated or treated, or both, a woman for EPF in the preceding 6 months. They achieved response rates of 51.0%, 70.9%, and 53.5%, respectively. Evaluable respondents had a mean age of 49 to 50 years and included 309 ObGyns (46.9% of whom were female), 368 CNMs (97.8% female), and 299 FPs (43.6% female).
Overall, approximately one third of respondents believe that office evacuation is riskier than OR evacuation. In addition, 65.7% of ObGyns believe that most patients prefer OR evacuation, compared with 46.2% and 43.1% of CNMs and FPs, respectively (P < .001). Among ObGyns, an adjusted analysis estimated the likelihood of providing office evacuation to be five times higher among those who have undergone training in induced abortion (P < .05). As for misoprostol for EPF, about two thirds of respondents overall believe that it is safe.
Dalton and associates posit that providers “perceive that their personal treatment preferences are different than their patients’. Whether this discordance results in women undergoing operating room uterine evacuation more often than is necessary or preferred could not be assessed by this study.” However, the authors also assert that, “given that providers affect treatment choice greatly, it is plausible that provider treatment preferences are an important influence on current treatment patterns.”
Certainly, women have diverse preferences for how EPF is managed, but many do find office evacuation and misoprostol to be acceptable methods. Accordingly, we should offer all options to them. As the investigators in this study suggest, we may need to focus on correcting inaccurate beliefs about these modalities among providers to increase their willingness to offer them.
The findings of this survey also underscore the fact that training programs that do not teach induced abortion—or that allow trainees to opt out of such training—can compromise the care provided to women who have EPF.—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
One in every four women experiences EPF. Although office uterine evacuation and misoprostol administration are less invasive and less expensive alternatives to traditional OR evacuation, it is not clear how extensively clinicians employ these options in the United States.1,2
In 2008, Dalton and colleagues surveyed ObGyns, certified nurse midwives (CNMs), and family physicians (FPs) in the United States who had evaluated or treated, or both, a woman for EPF in the preceding 6 months. They achieved response rates of 51.0%, 70.9%, and 53.5%, respectively. Evaluable respondents had a mean age of 49 to 50 years and included 309 ObGyns (46.9% of whom were female), 368 CNMs (97.8% female), and 299 FPs (43.6% female).
Overall, approximately one third of respondents believe that office evacuation is riskier than OR evacuation. In addition, 65.7% of ObGyns believe that most patients prefer OR evacuation, compared with 46.2% and 43.1% of CNMs and FPs, respectively (P < .001). Among ObGyns, an adjusted analysis estimated the likelihood of providing office evacuation to be five times higher among those who have undergone training in induced abortion (P < .05). As for misoprostol for EPF, about two thirds of respondents overall believe that it is safe.
Dalton and associates posit that providers “perceive that their personal treatment preferences are different than their patients’. Whether this discordance results in women undergoing operating room uterine evacuation more often than is necessary or preferred could not be assessed by this study.” However, the authors also assert that, “given that providers affect treatment choice greatly, it is plausible that provider treatment preferences are an important influence on current treatment patterns.”
Certainly, women have diverse preferences for how EPF is managed, but many do find office evacuation and misoprostol to be acceptable methods. Accordingly, we should offer all options to them. As the investigators in this study suggest, we may need to focus on correcting inaccurate beliefs about these modalities among providers to increase their willingness to offer them.
The findings of this survey also underscore the fact that training programs that do not teach induced abortion—or that allow trainees to opt out of such training—can compromise the care provided to women who have EPF.—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Zhang J, Gilles JM, Barnhart K, et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
2. Harris LH, Dalton VK, Johnson TR. Surgical management of early pregnancy failure: history, politics, and safe, cost-effective care. Am J Obstet Gynecol. 2007;196(5):445.e1–e5.-
1. Zhang J, Gilles JM, Barnhart K, et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
2. Harris LH, Dalton VK, Johnson TR. Surgical management of early pregnancy failure: history, politics, and safe, cost-effective care. Am J Obstet Gynecol. 2007;196(5):445.e1–e5.-
ENT complaints in pregnancy: The ear and the throat
Ear, nose, and throat complaints are common even before you superimpose the transformations and demands of pregnancy. Take gastroesophageal reflux disease (GERD), for example. Experts estimate that one third of the US population suffers from this condition.1 In pregnancy, endocrine and anatomic factors converge to exacerbate acid reflux disorders in 30% to 50% of women.2
Other complaints, too, surface or worsen during gestation. In Part 1 of this series (August 2010), we discussed sinonasal disease in pregnancy: specifically, pregnancy rhinitis, allergic rhinitis, vasomotor rhinitis, rhinitis medicamentosa, sinusitis, epistaxis, and sleep-disordered breathing. In Part 2, our focus is:
- laryngologic complaints
- – GERD
– laryngopharyngeal reflux
– laryngopathia gravidarum
- otologic disorders
- – eustachian tube dysfunction
– facial paralysis (Bell’s palsy)
– otosclerosis
– sudden sensorineural hearing loss
- endocrine abnormalities
- – thyroid nodules
- dermatologic complaints
- – melasma
– pyogenic granuloma.
Mapping the head and neck, and the spectrum of disease there in pregnancy
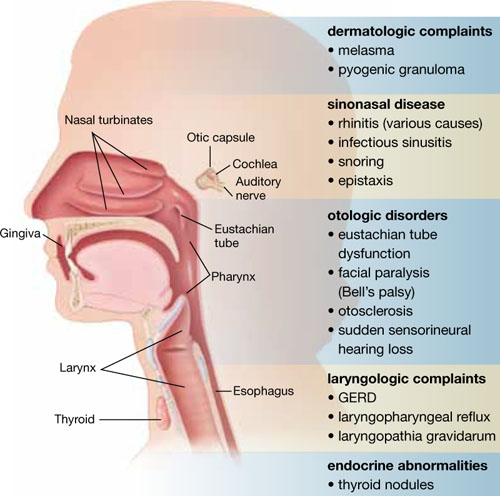
This list includes diseases and problems reviewed in the first part of this article, August 2010.
Why does GERD increase in pregnancy?
The smooth muscle–relaxing effects of progesterone and estrogen are likely responsible for the decreased tone of both the upper esophageal and gastroesophageal sphincters. This reduced tone may lead to increased reflux of stomach contents into the esophagus, larynx, and pharynx. Decreased gastric emptying and increased intestinal transit time may also play a role. Reflux of gastric contents may also be exacerbated by compression from the gravid uterus.
Gastroesophageal reflux is physiologic, occurring in healthy people as often as 50 times a day. It becomes GERD when reflux into the esophagus is excessive, causing tissue damage (esophagitis) and clinical symptoms (heartburn). Recent studies suggest that, in addition to the traditional symptoms, GERD is associated with increased severity of nausea and vomiting in pregnancy.3
Ultimately, refluxed gastric contents cause mucosal injury to the upper aerodigestive tract. The location of injury and subsequent clinical manifestations are believed to correspond to the pattern of reflux.4
Some refluxers do it in the daytime
Laryngopharyngeal reflux (LPR), widely viewed as a separate clinical entity from GERD, is backflow of stomach contents into the laryngopharynx (FIGURE).5 Fewer than 40% of patients who have LPR experience heartburn, and fewer than 25% have evidence of esophagitis.6 LPR patients are predominantly upright, daytime refluxers, whereas GERD patients are predominantly supine or nocturnal refluxers. The threshold for reflux-related injury of the laryngeal epithelium is significantly lower than the threshold for injury to epithelium of the esophagus.7 As a result, even brief reflux exposures can injure the laryngeal epithelium.8
Injury in LPR manifests clinically as posterior laryngeal edema and erythema, obliteration of the laryngeal ventricles, and interarytenoid hypertrophy.5 These changes produce symptoms of chronic throat clearing, hoarseness, cough, and the sensation that something is caught in the throat (globus sensation). History and physical examination are typically sufficient to diagnose LPR.
Lifestyle changes can make a difference in GERD and LPR
Start with simple measures. Advise the patient to elevate the head of her bed 6 to 8 inches. Our patients report that it is usually easier to tolerate books under the legs of the head end of the bed than it is to sleep with extra pillows, especially when a side position is desired.
The patient also should be advised to avoid lying down within 3 hours after eating and to avoid smoking tobacco; drinking beer, wine, coffee, soda, caffeinated tea, and citrus juice; eating foods that are fried, high in fat, or spicy; and using drugs that promote reflux (i.e., calcium channel blockers, sedatives, and nitrates).
An interesting tip: Chewing gum increases salivary bicarbonate production and may neutralize acid.9
Pharmacologic options include H2 blockers and PPIs
Antacids, such as sucralfate, neutralize acid already in the stomach and may have a role in the treatment of acute symptoms.
Histamine 2 (H2) blockers such as cimetidine (Tagamet), ranitidine (Zantac), and famotidine (Pepcid) block the histamine receptor in the stomach and reduce acid secretion by as much as 50%. These medications are typically taken two to three times daily. They all fall into Pregnancy Category B, except for nizatidine (Axid), which is Category C.
Proton pump inhibitors (PPIs). Recently, utilization of H2 blockers has given way to the newer class of PPIs, including lansoprazole (Prevacid), pantoprazole (Protonix), and esomeprazole (Nexium). These drugs target the parietal cell hydrogen potassium ATPase, reducing acid secretion by 80% to 90%. Treatment is typically once daily for uncomplicated GERD and twice daily for LPR. Patients who have LPR also require higher dosages to achieve complete acid suppression and heal the delicate laryngeal tissue. Tissue injury in LPR may take 6 months to reverse once adequate therapy has been initiated. Severe, complicated cases may require the addition of an H2 blocker or even a third daily dose of the PPI.
Patients should not discontinue a PPI abruptly because of the risk of rebound hypersecretion of gastric acid. Rather, these drugs should be stopped gradually over several weeks. They are best taken 30 minutes before a meal, as that is when they reach maximum blood concentration.
PPIs are generally considered safe for use after the first trimester of pregnancy. All are Category B drugs, except for omeprazole (Prilosec), which is a Category C drug.
The human voice is extremely sensitive to the endocrinologic changes of pregnancy. Many of these changes manifest as alterations in fluid content of the lamina propria just beneath the laryngeal mucosa.27 Collectively, the voice changes of pregnancy are known as laryngopathia gravidarum. Abdominal distension during pregnancy also interferes with abdominal muscle function, altering the mechanics of phonation and creating overuse injuries.
Symptoms include hoarseness and voice loss. Singers, in particular, notice a deeper voice and a diminished range of pitch.28 Treatment is largely supportive, with hydration, and singers should be advised to refrain from singing until abdominal muscle function resolves.
Laryngopathia gravidarum typically resolves postpartum as endocrinologic alterations return to baseline and abdominal support returns.
Eustachian tube dysfunction usually resolves postpartum
This disorder affects between 5% and 30% of pregnant women. Symptoms usually begin after the first trimester and consist of tubal obstruction or patulous Eustachian tubes. Women who have tubal obstruction report a clogged or popping sensation in their ears, with muffling of sounds. In severe cases, serous effusion may develop.
Tubal obstruction is related to edema of the respiratory mucosa. In cases in which symptoms are more distressing to the patient, increased humidity, treatment of rhinitis, and frequent Valsalva maneuvers have had variable success in providing relief. For recalcitrant cases, pressure-equalization tubes can be placed (in an otolaryngology clinic).
Women who have patulous tubes usually report intermittent symptoms that consist of autophony and a roaring sensation in their ears that is synchronous with breathing and is worse when they are in an upright position or exercising (or both). The cause of patulous Eustachian tubes is not well defined. Weight loss and hormonal variables are believed to play a role.
This condition typically resolves postpartum.
Treatment is largely supportive, including humidification, reassurance, and instructions on how to perform a forceful inspiratory nasal sniff.
Incidence of Bell’s palsy in pregnancy is uncertain
A possible association between pregnancy and idiopathic facial paralysis (Bell’s palsy) was first noted by Sir Charles Bell in 1830. Retrospective literature at first suggested a 3.3-fold increased risk of Bell’s palsy during pregnancy, with the incidence peaking during the third trimester of gestation.10 Subsequent re-analysis found no significant difference in the incidence of Bell’s palsy between pregnant and nonpregnant women of childbearing age.11 Prospective studies are sorely needed to definitively establish the incidence of Bell’s palsy in pregnancy.
Bell’s palsy typically appears during the third trimester
A unique aspect of Bell’s palsy in pregnancy is its tendency to manifest during the third trimester and postpartum. The most widely accepted theory for this phenomenon is the reactivation of latent herpes simplex virus within the geniculate ganglion.12 A large body of scientific work supports this theory.
The maternal immune system undergoes complex alterations during pregnancy, although the mechanisms for these changes are not completely understood. The most pronounced change is a shift from cell-mediated immune responses toward humoral and innate immune responses as pregnancy progresses.13 Such a shift likely reduces the maternal cytotoxic potential against fetal antigens.14 Clinically, the decrease in cellular immunity manifests as an increased susceptibility to intracellular pathogens such as herpes simplex virus later in pregnancy.15
Sudden facial weakness is the usual presenting symptom
This weakness develops over 24 to 48 hours, progressing to complete or near-complete paralysis within 1 week. Associated symptoms often include pain, fever, dry eye, a change in taste and salivation, and sensitivity to noise.11
Diagnosis of Bell’s palsy requires the exclusion of other causes, accomplished primarily by taking a thorough history and performing a physical examination. Between 14% and 21% of pregnant patients who have acute facial paralysis have causes other than Bell’s palsy.16
Among the other causes of facial paralysis are herpes zoster oticus (Ramsay Hunt syndrome), in which varicella zoster virus reactivates at the geniculate ganglion.10 The patient with this disorder experiences facial nerve paralysis, skin eruption in the auricular canal, and cochleovestibular symptoms. Ramsay Hunt syndrome generally has a worse prognosis than Bell’s palsy for return of facial function.
Recurrent facial nerve paralysis can also be seen in Lyme disease, and prolonged paralysis may occur in Guillain-Barré syndrome.
When facial paralysis is accompanied by ear pain and purulent otorrhea, the cause may be acute otitis media. Cholesteatoma, trauma, neoplasm, myasthenia gravis, arteriovenous malformation, and mumps can all produce facial paralysis.
Treatment in pregnancy resembles treatment in the general population
Topical eye care, oral corticosteroids, and antiviral medications are the standard of care for Bell’s palsy. Surgical decompression may be utilized in the nonpregnant population, but reports of facial nerve decompression during pregnancy are extremely rare.
Eye care involves the use of preservative-free artificial tears, a viscous ocular ointment (Lacri-Lube) that must be applied at bedtime, with taping of the eyelids (shut) indicated at night for severe paralysis. Eye care plays a critical role in the prevention of ocular complications such as corneal abrasion.
Steroid treatment (i.e., prednisone at a dosage of 1 mg/kg for 5 days, followed by tapering) improves recovery in Bell’s palsy when it is initiated within 14 days after the onset of facial paralysis.17 However, use of steroids during the first trimester of pregnancy has been associated with an increased risk of cleft palate, and infants born to mothers who received exogenous steroids during gestation should be watched for adrenal hypofunction.
Antiviral medications represent another adjunctive treatment for Bell’s palsy. Nucleoside analogues, including valacyclovir (Valtrex) and famciclovir (Famvir) (both Category B), pose little risk to mother and fetus. In fact, these agents are commonly used to prevent outbreaks of herpes simplex virus late in pregnancy. Two double-blind, randomized, controlled trials in nonpregnant patients have demonstrated improved outcomes when Bell’s palsy is treated with steroids and antiviral agents within 3 days after onset of the paralysis, compared with steroids alone.18,19
Rapid diagnosis and treatment are critical for a good outcome. The potential benefits of treatment likely outweigh the limited fetal risks posed by these medications. Although there are conflicting reports, in general, pregnant patients who experience incomplete paralysis do extremely well, recovering with minimal residual deficits. The prognosis is less optimistic for patients who have complete paralysis, with persistent deficits observed in as many as 50% of cases.
Diffuse thyroid gland enlargement during pregnancy is common, occurring to varying degrees in nearly 50% of pregnant women. Pregnancy is also thought to promote the growth of existing thyroid nodules and induce the formation of new nodules.29 In both pregnant and nonpregnant patients, the majority (more than 90%) of these nodules are benign, although pregnant women appear to have a slightly higher likelihood that a solitary nodule is malignant.30
Diagnosis is straightforward
When a thyroid nodule is detected in a pregnant patient, the workup begins with a thorough history, noting age, family history of thyroid or endocrine disease, personal history of low-dosage head and neck radiation, and any recent hoarseness, dysphagia, and symptoms of hypermetabolism.
The physical exam should focus on the size and location of the thyroid abnormality, the degree of firmness of the nodule, the presence of any other nodules in the thyroid, any palpable cervical lymph nodes, and any vocal cord dysfunction.
US imaging is recommended
Because ultrasonography (US) of the thyroid is noninvasive, it is the initial imaging modality of choice. It can establish the size of any nodule (and serve as an objective baseline measurement) and identify any characteristics that suggest malignancy, such as microcalcifications, hypoechogenicity, and solid structure.
Consider fine-needle aspiration (FNA)
This technique, guided by US, is recommended when a nodule is discovered during the first trimester. However, when a nodule is discovered after 20 weeks’ gestation, the FNA option is not required. FNA can be deferred until after delivery because, even with a histologically confirmed, well-differentiated thyroid cancer, we would not operate during the third trimester—the elevated risk of preterm labor precludes that option.
When the diagnosis is cancer
The nonpregnant patient has several therapeutic options for management of thyroid cancer, but pregnancy restricts these options to close observation and surgical resection. The optimal timing of surgical management (either the second trimester or postpartum) remains unresolved.
Thyroid cancer is somewhat unique among malignancies. The majority of cancers are well-differentiated and exhibit indolent tumor biology. In one prospective study of nonpregnant patients who had small, papillary, thyroid cancers, more than 70% of those who bypassed surgical intervention had no tumor growth after 5 years of follow-up.31
Given that pregnancy is an independent risk factor for surgical complications, prolonged hospitalization, and higher hospital costs after thyroidectomy, it seems reasonable to carefully monitor, by serial US, pregnant women who have been given a diagnosis of small, well-differentiated thyroid cancer.32
In general, if a nodule is discovered during the first trimester and is larger than 1.5 cm, and if the diagnosis is cytology-proven, differentiated thyroid cancer, we would consider surgery during the second trimester if the patient were adamant. Other authors recommend second-trimester surgery more strongly.33 Regardless of the timing of resection, adjunctive treatment with radioactive iodine ablation (RIA) 3 to 6 months after delivery is an accepted component of complete oncologic therapy. Breastfeeding is prohibited with RIA, and patients are advised to wait 1 year after RIA before conceiving again.
If the patient chooses to undergo surgical resection of the thyroid during the second trimester, be aware of the transient hypothyroid state that immediately follows surgery (before the patient becomes euthyroid on replacement hormone). Because the fetus begins to synthesize its own thyroid hormone around the 18th week of gestation, we agree with the contention that the optimal time to operate is between week 19 and week 22 of gestation.34 Operating before 24 weeks also reduces the concerns related to fetal viability.
If a nodule is cytology-proven to be differentiated thyroid cancer and is smaller than 1.5 cm or is discovered late in the second trimester or beyond, most authors recommend delaying surgery until after delivery.
Outcomes are not worse in pregnancy
Pregnant women who have well-differentiated thyroid cancer and their nonpregnant counterparts have statistically identical outcomes. Moosa and Mazzaferri demonstrated no significant differences in the rate of recurrence, distant spread, or mortality.35 Their findings have been replicated in a larger, population-based study.36 There also appears to be no significant differences in maternal survival or fetal outcome between women who undergo surgical intervention during the second trimester and those who delay surgery to the postpartum period.35,37,38 After treatment, the risk of recurrence does not increase in subsequent pregnancies.35
Otosclerosis may lead to hearing loss
The primary disease of the otic capsule, otosclerosis is characterized by alternating phases of absorption of compact bony tissue and replacement with spongy bone. The most common location of this disorder is the oval window, and it can lead to stapedial ankylosis and subsequent conductive hearing loss. The disease can eventually progress to cochlear otosclerosis with sensorineural hearing loss.
Otosclerosis is multifactorial in origin, with contributors that include genetics, fluoridated water, exposure to measles, and vitamin D deficiency.
Pregnancy probably does not accelerate otosclerosis
Early reports, based on subjective, self-reported hearing endpoints, suggested that pregnancy might cause or accelerate the process of otosclerosis.20 In the 1950s, some authors even advocated termination of pregnancy and sterilization as treatment in progressive cases.21 The likely source of this idea was a paper written by Greifenstein in 1939, which stated the official policy of the German Reichsgutacherstelle (Agency of Expert Opinion of the German Reich) in regard to abortion and sterilization in women who had genetic disease.22 As a result of this guideline, in 1939, of 69 women who had otosclerosis in Germany, 43 underwent abortion and 23 were sterilized.23
Recent research argues strongly against an association between pregnancy and accelerated otosclerosis. Rigorous audiometry found no adverse effect on hearing in otosclerotic women who had children, compared with women without children. Nor were air conduction, bone conduction, and discrimination worse in women who had children, compared with childless women. No significant correlation was found between the number of children and hearing loss, or between lactation and hearing loss.24
Treatment of otosclerosis entails amplification throughout the pregnancy. Postpartum, an elective stapedectomy, in which the sclerotic stapes bone is replaced with a micro-prosthesis, frequently provides a clinically significant increase in hearing.
Sudden sensorineural hearing loss is rare
Although it is uncommon during pregnancy, sudden sensorineural hearing loss has been associated with hypertension and toxemia of pregnancy, presumably due to microemboli-mediated vascular occlusion of the microcirculation of the cochlea and auditory nerve. Complete otologic and audiologic evaluation, as well as treatment of the toxemia, is the standard of care.
Melasma affects almost 75% of gravidas
The “mask of pregnancy” is one of the most frequently encountered changes of pregnancy. The condition is thought to be driven by sun exposure and concomitant increases in the levels of melanocyte-stimulating hormone, serum estrogen, and progesterone. Well-delineated areas of hypermelanosis affect the face and neck. These lesions can begin during pregnancy, or become worse if they were present before conception. The most frequently involved sites are the cheeks, nose, and chin.
Avoidance of sunlight is the treatment for melasma
Topical sunscreens are recommended. Melasma typically regresses after delivery but persists in fewer than 10% of cases. Persistent hyperpigmentation can be treated with a variety of topical agents, including hydroquinone, tretinoin, kojic acid, and vitamin C, among others.25 Treatment is not always effective, however. Extensive pigmentary changes predict a poor response to topical therapy.
Pyogenic granuloma usually regresses postpartum
Granuloma gravidarum, or pyogenic granuloma of pregnancy, consists of soft, pedunculated, vascular proliferations, most commonly arising from the gingiva and nasal mucosa in 2% of pregnant women.25 These proliferations are thought to be triggered by the myriad hormonal changes of pregnancy superimposed on local tissue trauma. These lesions rarely exceed 2 cm in size, but they can ulcerate and cause pain. They frequently regress 1 to 2 months postpartum. Surgical resection is utilized only to stanch recalcitrant bleeding. When lesions recur after surgical excision, inadequate resection is thought to be the cause. A recent report described the Nd:YAG laser as an effective tool for treatment of these lesions.26
Part 1 of this series focuses on sinonasal disease in pregnancy.
We want to hear from you! Tell us what you think.
1. American Gastroenterological Association. The burden of chronic gastrointestinal diseases study. Bethesda, Md: AGA; 2001.
2. Cappell MS, Garcia A. Gastric and duodenal ulcers during pregnancy. Gastroenterol Clin North Am. 1998;27(1):169-195.
3. Gill SK, Maltepe C, Koren G. The effect of heartburn and acid reflux on the severity of nausea and vomiting of pregnancy. Can J Gastroenterol. 2009;23(4):270-272.
4. Wiener GJ, Koufman JA, Wu WC, Cooper JB, Richter JE, Castell DO. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84(12):1503-1508.
5. Gupta R, Sataloff RT. Laryngopharyngeal reflux: current concepts and questions. Curr Opin Otolaryngol Head Neck Surg. 2009;17(3):143-148.
6. Koufman JA, Belafsky PC, Bach KK, Daniel E, Postma GN. Prevalence of esophagitis in patients with pH-documented laryngopharyngeal reflux. Laryngoscope. 2002;112(9):1606-1609.
7. Johnston N, Bulmer D, Gill GA, Panetti M, et al. Cell biology of laryngeal epithelial defenses in health and disease: further studies. Ann Otol Rhinol Laryngol. 2003;112(6):481-491.
8. Gill GA, Johnston N, Buda A, et al. Laryngeal epithelial defenses against laryngopharyngeal reflux: investigations of E-cadherin, carbonic anhydrase isoenzyme III, and pepsin. Ann Otol Rhinol Laryngol. 2005;114(12):913-921.
9. Smoak BR, Koufman JA. Effects of gum chewing on pharyngeal and esophageal pH. Ann Otol Rhinol Laryngol. 2001;110(12):1117-1119.
10. Hilsinger RL, Jr, Adour KK, Doty HE. Idiopathic facial paralysis, pregnancy, and the menstrual cycle. Ann Otol Rhinol Laryngol. 1975;84(4 Pt 1):433-442.
11. Vrabec JT, Isaacson B, Van Hook JW. Bell’s palsy and pregnancy. Otolaryngol Head Neck Surg. 2007;137(6):858-861.
12. Murakami S, Mizobuchi M, Nakashiro Y, Doi T, Hato N, Yanagihara N. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med. 1996;124(1 Pt 1):27-30.
13. Sacks G, Sargent I, Redman C. An innate view of human pregnancy. Immunol Today. 1999;20(3):114-118.
14. Wegmann TG, Lin H, Guilbert L, Mosmann TR. Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol Today. 1993;14(7):353-356.
15. Stirrat GM. Pregnancy and immunity. BMJ. 1994;308(6941):1385-1386.
16. Gillman GS, Schaitkin BM, May M, Klein SR. Bell’s palsy in pregnancy: a study of recovery outcomes. Otolaryngol Head Neck Surg. 2002;126(1):26-30.
17. Ramsey MJ, DerSimonian R, Holtel MR, Burgess LP. Corticosteroid treatment for idiopathic facial nerve paralysis: a meta-analysis. Laryngoscope. 2000;110(3 Pt 1):335-341.
18. Adour KK, Ruboyianes JM, Von Doersten PG, et al. Bell’s palsy treatment with acyclovir and prednisone compared with prednisone alone: a double-blind, randomized, controlled trial. Ann Otol Rhinol Laryngol. 1996;105(5):371-378.
19. Hato N, Yamada H, Kohno H, et al. Valacyclovir and prednisolone treatment for Bell’s palsy: a multicenter, randomized, placebo-controlled study. Otol Neurotol. 2007;28(3):408-413.
20. Gristwood RE, Venables WN. Pregnancy and otosclerosis. Clin Otolaryngol Allied Sci. 1983;8(3):205-210.
21. Pearson E. The effect of pregnancy on otosclerosis. Ann West Med Surg. 1951;5(5):477-482.
22. Greifenstein. Schwangerschaftsunterbrechung und unfruchtbarmachung aus gesundheitlichen Grunden bei Otosklerose. Zeitschrift fur halsnasen und ohrenheilkunde 1939;46:344-362.
23. Markou K, Goudakos J. An overview of the etiology of otosclerosis. Eur Arch Otorhinolaryngol. 2009;266(1):25-35.
24. Lippy WH, Berenholz LP, Schuring AG, et al. Does pregnancy affect otosclerosis? Laryngoscope. 2005;115(10):1833-1836.
25. Muallem MM, Rubeiz NG. Physiological and biological skin changes in pregnancy. Clin Dermatol. 2006;24(2):80-83.
26. Powell JL, Bailey CL, Coopland AT, Otis CN, Frank JL, Meyer I. Nd:YAG laser excision of a giant gingival pyogenic granuloma of pregnancy. Lasers Surg Med. 1994;14(2):178-183.
27. Brodnitz FS. Hormones and the human voice. Bull NY Acad Med. 1971;47(2):183-191.
28. Sataloff RT, Hoover CA. Endocrine dysfunction. In: Sataloff RT, ed. Professional voice: the science and art of clinical care. 2nd ed. San Diego, CA: Singular Publishing Group, Inc. 1997;293-295.
29. Kung AW, Chau MT, Lao TT, Tam SC, Low LC. The effect of pregnancy on thyroid nodule formation. J Clin Endocrinol Metab. 2002;87(3):1010-1014.
30. Smith LH, Danielsen B, Allen ME, Cress R. Cancer associated with obstetric delivery: results of linkage with the California cancer registry. Am J Obstet Gynecol. 2003;189(4):1128-1135.
31. Ito Y, Uruno T, Nakano K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid. 2003;13(4):381-387.
32. Kuy S, Roman SA, Desai R, Sosa JA. Outcomes following thyroid and parathyroid surgery in pregnant women. Arch Surg. 2009;144(5):399-406.
33. Rosen IB, Korman M, Walfish PG. Thyroid nodular disease in pregnancy: current diagnosis and management. Clin Obstet Gynecol. 1997;40(1):81-89.
34. Fanarjian N, Athavale SM, Herrero N, et al. Thyroid cancer in pregnancy. Laryngoscope. 2007;117(10):1777-1781.
35. Moosa M, Mazzaferri EL. Outcome of differentiated thyroid cancer diagnosed in pregnant women. J Clin Endocrinol Metab. 1997;82(9):2862-2866.
36. Yasmeen S, Cress R, Romano PS, et al. Thyroid cancer in pregnancy. Int J Gynaecol Obstet. 2005;91(1):15-20.
37. Nam KH, Yoon JH, Chang HS, Park CS. Optimal timing of surgery in well-differentiated thyroid carcinoma detected during pregnancy. J Surg Oncol. 2005;91(3):199-203.
38. Doherty CM, Shindo ML, et al. Management of thyroid nodules during pregnancy. Laryngoscope. 1995;105(3 Pt 1):251-255.
Ear, nose, and throat complaints are common even before you superimpose the transformations and demands of pregnancy. Take gastroesophageal reflux disease (GERD), for example. Experts estimate that one third of the US population suffers from this condition.1 In pregnancy, endocrine and anatomic factors converge to exacerbate acid reflux disorders in 30% to 50% of women.2
Other complaints, too, surface or worsen during gestation. In Part 1 of this series (August 2010), we discussed sinonasal disease in pregnancy: specifically, pregnancy rhinitis, allergic rhinitis, vasomotor rhinitis, rhinitis medicamentosa, sinusitis, epistaxis, and sleep-disordered breathing. In Part 2, our focus is:
- laryngologic complaints
- – GERD
– laryngopharyngeal reflux
– laryngopathia gravidarum
- otologic disorders
- – eustachian tube dysfunction
– facial paralysis (Bell’s palsy)
– otosclerosis
– sudden sensorineural hearing loss
- endocrine abnormalities
- – thyroid nodules
- dermatologic complaints
- – melasma
– pyogenic granuloma.
Mapping the head and neck, and the spectrum of disease there in pregnancy
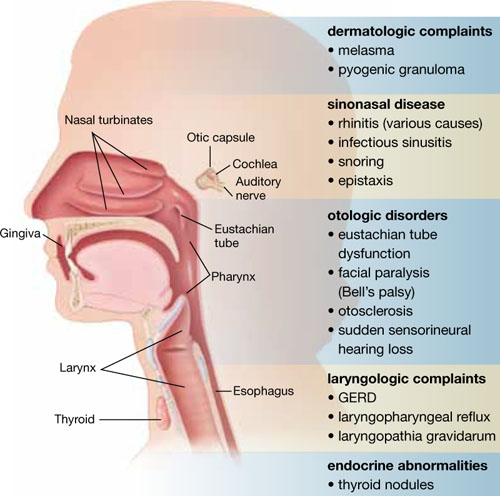
This list includes diseases and problems reviewed in the first part of this article, August 2010.
Why does GERD increase in pregnancy?
The smooth muscle–relaxing effects of progesterone and estrogen are likely responsible for the decreased tone of both the upper esophageal and gastroesophageal sphincters. This reduced tone may lead to increased reflux of stomach contents into the esophagus, larynx, and pharynx. Decreased gastric emptying and increased intestinal transit time may also play a role. Reflux of gastric contents may also be exacerbated by compression from the gravid uterus.
Gastroesophageal reflux is physiologic, occurring in healthy people as often as 50 times a day. It becomes GERD when reflux into the esophagus is excessive, causing tissue damage (esophagitis) and clinical symptoms (heartburn). Recent studies suggest that, in addition to the traditional symptoms, GERD is associated with increased severity of nausea and vomiting in pregnancy.3
Ultimately, refluxed gastric contents cause mucosal injury to the upper aerodigestive tract. The location of injury and subsequent clinical manifestations are believed to correspond to the pattern of reflux.4
Some refluxers do it in the daytime
Laryngopharyngeal reflux (LPR), widely viewed as a separate clinical entity from GERD, is backflow of stomach contents into the laryngopharynx (FIGURE).5 Fewer than 40% of patients who have LPR experience heartburn, and fewer than 25% have evidence of esophagitis.6 LPR patients are predominantly upright, daytime refluxers, whereas GERD patients are predominantly supine or nocturnal refluxers. The threshold for reflux-related injury of the laryngeal epithelium is significantly lower than the threshold for injury to epithelium of the esophagus.7 As a result, even brief reflux exposures can injure the laryngeal epithelium.8
Injury in LPR manifests clinically as posterior laryngeal edema and erythema, obliteration of the laryngeal ventricles, and interarytenoid hypertrophy.5 These changes produce symptoms of chronic throat clearing, hoarseness, cough, and the sensation that something is caught in the throat (globus sensation). History and physical examination are typically sufficient to diagnose LPR.
Lifestyle changes can make a difference in GERD and LPR
Start with simple measures. Advise the patient to elevate the head of her bed 6 to 8 inches. Our patients report that it is usually easier to tolerate books under the legs of the head end of the bed than it is to sleep with extra pillows, especially when a side position is desired.
The patient also should be advised to avoid lying down within 3 hours after eating and to avoid smoking tobacco; drinking beer, wine, coffee, soda, caffeinated tea, and citrus juice; eating foods that are fried, high in fat, or spicy; and using drugs that promote reflux (i.e., calcium channel blockers, sedatives, and nitrates).
An interesting tip: Chewing gum increases salivary bicarbonate production and may neutralize acid.9
Pharmacologic options include H2 blockers and PPIs
Antacids, such as sucralfate, neutralize acid already in the stomach and may have a role in the treatment of acute symptoms.
Histamine 2 (H2) blockers such as cimetidine (Tagamet), ranitidine (Zantac), and famotidine (Pepcid) block the histamine receptor in the stomach and reduce acid secretion by as much as 50%. These medications are typically taken two to three times daily. They all fall into Pregnancy Category B, except for nizatidine (Axid), which is Category C.
Proton pump inhibitors (PPIs). Recently, utilization of H2 blockers has given way to the newer class of PPIs, including lansoprazole (Prevacid), pantoprazole (Protonix), and esomeprazole (Nexium). These drugs target the parietal cell hydrogen potassium ATPase, reducing acid secretion by 80% to 90%. Treatment is typically once daily for uncomplicated GERD and twice daily for LPR. Patients who have LPR also require higher dosages to achieve complete acid suppression and heal the delicate laryngeal tissue. Tissue injury in LPR may take 6 months to reverse once adequate therapy has been initiated. Severe, complicated cases may require the addition of an H2 blocker or even a third daily dose of the PPI.
Patients should not discontinue a PPI abruptly because of the risk of rebound hypersecretion of gastric acid. Rather, these drugs should be stopped gradually over several weeks. They are best taken 30 minutes before a meal, as that is when they reach maximum blood concentration.
PPIs are generally considered safe for use after the first trimester of pregnancy. All are Category B drugs, except for omeprazole (Prilosec), which is a Category C drug.
The human voice is extremely sensitive to the endocrinologic changes of pregnancy. Many of these changes manifest as alterations in fluid content of the lamina propria just beneath the laryngeal mucosa.27 Collectively, the voice changes of pregnancy are known as laryngopathia gravidarum. Abdominal distension during pregnancy also interferes with abdominal muscle function, altering the mechanics of phonation and creating overuse injuries.
Symptoms include hoarseness and voice loss. Singers, in particular, notice a deeper voice and a diminished range of pitch.28 Treatment is largely supportive, with hydration, and singers should be advised to refrain from singing until abdominal muscle function resolves.
Laryngopathia gravidarum typically resolves postpartum as endocrinologic alterations return to baseline and abdominal support returns.
Eustachian tube dysfunction usually resolves postpartum
This disorder affects between 5% and 30% of pregnant women. Symptoms usually begin after the first trimester and consist of tubal obstruction or patulous Eustachian tubes. Women who have tubal obstruction report a clogged or popping sensation in their ears, with muffling of sounds. In severe cases, serous effusion may develop.
Tubal obstruction is related to edema of the respiratory mucosa. In cases in which symptoms are more distressing to the patient, increased humidity, treatment of rhinitis, and frequent Valsalva maneuvers have had variable success in providing relief. For recalcitrant cases, pressure-equalization tubes can be placed (in an otolaryngology clinic).
Women who have patulous tubes usually report intermittent symptoms that consist of autophony and a roaring sensation in their ears that is synchronous with breathing and is worse when they are in an upright position or exercising (or both). The cause of patulous Eustachian tubes is not well defined. Weight loss and hormonal variables are believed to play a role.
This condition typically resolves postpartum.
Treatment is largely supportive, including humidification, reassurance, and instructions on how to perform a forceful inspiratory nasal sniff.
Incidence of Bell’s palsy in pregnancy is uncertain
A possible association between pregnancy and idiopathic facial paralysis (Bell’s palsy) was first noted by Sir Charles Bell in 1830. Retrospective literature at first suggested a 3.3-fold increased risk of Bell’s palsy during pregnancy, with the incidence peaking during the third trimester of gestation.10 Subsequent re-analysis found no significant difference in the incidence of Bell’s palsy between pregnant and nonpregnant women of childbearing age.11 Prospective studies are sorely needed to definitively establish the incidence of Bell’s palsy in pregnancy.
Bell’s palsy typically appears during the third trimester
A unique aspect of Bell’s palsy in pregnancy is its tendency to manifest during the third trimester and postpartum. The most widely accepted theory for this phenomenon is the reactivation of latent herpes simplex virus within the geniculate ganglion.12 A large body of scientific work supports this theory.
The maternal immune system undergoes complex alterations during pregnancy, although the mechanisms for these changes are not completely understood. The most pronounced change is a shift from cell-mediated immune responses toward humoral and innate immune responses as pregnancy progresses.13 Such a shift likely reduces the maternal cytotoxic potential against fetal antigens.14 Clinically, the decrease in cellular immunity manifests as an increased susceptibility to intracellular pathogens such as herpes simplex virus later in pregnancy.15
Sudden facial weakness is the usual presenting symptom
This weakness develops over 24 to 48 hours, progressing to complete or near-complete paralysis within 1 week. Associated symptoms often include pain, fever, dry eye, a change in taste and salivation, and sensitivity to noise.11
Diagnosis of Bell’s palsy requires the exclusion of other causes, accomplished primarily by taking a thorough history and performing a physical examination. Between 14% and 21% of pregnant patients who have acute facial paralysis have causes other than Bell’s palsy.16
Among the other causes of facial paralysis are herpes zoster oticus (Ramsay Hunt syndrome), in which varicella zoster virus reactivates at the geniculate ganglion.10 The patient with this disorder experiences facial nerve paralysis, skin eruption in the auricular canal, and cochleovestibular symptoms. Ramsay Hunt syndrome generally has a worse prognosis than Bell’s palsy for return of facial function.
Recurrent facial nerve paralysis can also be seen in Lyme disease, and prolonged paralysis may occur in Guillain-Barré syndrome.
When facial paralysis is accompanied by ear pain and purulent otorrhea, the cause may be acute otitis media. Cholesteatoma, trauma, neoplasm, myasthenia gravis, arteriovenous malformation, and mumps can all produce facial paralysis.
Treatment in pregnancy resembles treatment in the general population
Topical eye care, oral corticosteroids, and antiviral medications are the standard of care for Bell’s palsy. Surgical decompression may be utilized in the nonpregnant population, but reports of facial nerve decompression during pregnancy are extremely rare.
Eye care involves the use of preservative-free artificial tears, a viscous ocular ointment (Lacri-Lube) that must be applied at bedtime, with taping of the eyelids (shut) indicated at night for severe paralysis. Eye care plays a critical role in the prevention of ocular complications such as corneal abrasion.
Steroid treatment (i.e., prednisone at a dosage of 1 mg/kg for 5 days, followed by tapering) improves recovery in Bell’s palsy when it is initiated within 14 days after the onset of facial paralysis.17 However, use of steroids during the first trimester of pregnancy has been associated with an increased risk of cleft palate, and infants born to mothers who received exogenous steroids during gestation should be watched for adrenal hypofunction.
Antiviral medications represent another adjunctive treatment for Bell’s palsy. Nucleoside analogues, including valacyclovir (Valtrex) and famciclovir (Famvir) (both Category B), pose little risk to mother and fetus. In fact, these agents are commonly used to prevent outbreaks of herpes simplex virus late in pregnancy. Two double-blind, randomized, controlled trials in nonpregnant patients have demonstrated improved outcomes when Bell’s palsy is treated with steroids and antiviral agents within 3 days after onset of the paralysis, compared with steroids alone.18,19
Rapid diagnosis and treatment are critical for a good outcome. The potential benefits of treatment likely outweigh the limited fetal risks posed by these medications. Although there are conflicting reports, in general, pregnant patients who experience incomplete paralysis do extremely well, recovering with minimal residual deficits. The prognosis is less optimistic for patients who have complete paralysis, with persistent deficits observed in as many as 50% of cases.
Diffuse thyroid gland enlargement during pregnancy is common, occurring to varying degrees in nearly 50% of pregnant women. Pregnancy is also thought to promote the growth of existing thyroid nodules and induce the formation of new nodules.29 In both pregnant and nonpregnant patients, the majority (more than 90%) of these nodules are benign, although pregnant women appear to have a slightly higher likelihood that a solitary nodule is malignant.30
Diagnosis is straightforward
When a thyroid nodule is detected in a pregnant patient, the workup begins with a thorough history, noting age, family history of thyroid or endocrine disease, personal history of low-dosage head and neck radiation, and any recent hoarseness, dysphagia, and symptoms of hypermetabolism.
The physical exam should focus on the size and location of the thyroid abnormality, the degree of firmness of the nodule, the presence of any other nodules in the thyroid, any palpable cervical lymph nodes, and any vocal cord dysfunction.
US imaging is recommended
Because ultrasonography (US) of the thyroid is noninvasive, it is the initial imaging modality of choice. It can establish the size of any nodule (and serve as an objective baseline measurement) and identify any characteristics that suggest malignancy, such as microcalcifications, hypoechogenicity, and solid structure.
Consider fine-needle aspiration (FNA)
This technique, guided by US, is recommended when a nodule is discovered during the first trimester. However, when a nodule is discovered after 20 weeks’ gestation, the FNA option is not required. FNA can be deferred until after delivery because, even with a histologically confirmed, well-differentiated thyroid cancer, we would not operate during the third trimester—the elevated risk of preterm labor precludes that option.
When the diagnosis is cancer
The nonpregnant patient has several therapeutic options for management of thyroid cancer, but pregnancy restricts these options to close observation and surgical resection. The optimal timing of surgical management (either the second trimester or postpartum) remains unresolved.
Thyroid cancer is somewhat unique among malignancies. The majority of cancers are well-differentiated and exhibit indolent tumor biology. In one prospective study of nonpregnant patients who had small, papillary, thyroid cancers, more than 70% of those who bypassed surgical intervention had no tumor growth after 5 years of follow-up.31
Given that pregnancy is an independent risk factor for surgical complications, prolonged hospitalization, and higher hospital costs after thyroidectomy, it seems reasonable to carefully monitor, by serial US, pregnant women who have been given a diagnosis of small, well-differentiated thyroid cancer.32
In general, if a nodule is discovered during the first trimester and is larger than 1.5 cm, and if the diagnosis is cytology-proven, differentiated thyroid cancer, we would consider surgery during the second trimester if the patient were adamant. Other authors recommend second-trimester surgery more strongly.33 Regardless of the timing of resection, adjunctive treatment with radioactive iodine ablation (RIA) 3 to 6 months after delivery is an accepted component of complete oncologic therapy. Breastfeeding is prohibited with RIA, and patients are advised to wait 1 year after RIA before conceiving again.
If the patient chooses to undergo surgical resection of the thyroid during the second trimester, be aware of the transient hypothyroid state that immediately follows surgery (before the patient becomes euthyroid on replacement hormone). Because the fetus begins to synthesize its own thyroid hormone around the 18th week of gestation, we agree with the contention that the optimal time to operate is between week 19 and week 22 of gestation.34 Operating before 24 weeks also reduces the concerns related to fetal viability.
If a nodule is cytology-proven to be differentiated thyroid cancer and is smaller than 1.5 cm or is discovered late in the second trimester or beyond, most authors recommend delaying surgery until after delivery.
Outcomes are not worse in pregnancy
Pregnant women who have well-differentiated thyroid cancer and their nonpregnant counterparts have statistically identical outcomes. Moosa and Mazzaferri demonstrated no significant differences in the rate of recurrence, distant spread, or mortality.35 Their findings have been replicated in a larger, population-based study.36 There also appears to be no significant differences in maternal survival or fetal outcome between women who undergo surgical intervention during the second trimester and those who delay surgery to the postpartum period.35,37,38 After treatment, the risk of recurrence does not increase in subsequent pregnancies.35
Otosclerosis may lead to hearing loss
The primary disease of the otic capsule, otosclerosis is characterized by alternating phases of absorption of compact bony tissue and replacement with spongy bone. The most common location of this disorder is the oval window, and it can lead to stapedial ankylosis and subsequent conductive hearing loss. The disease can eventually progress to cochlear otosclerosis with sensorineural hearing loss.
Otosclerosis is multifactorial in origin, with contributors that include genetics, fluoridated water, exposure to measles, and vitamin D deficiency.
Pregnancy probably does not accelerate otosclerosis
Early reports, based on subjective, self-reported hearing endpoints, suggested that pregnancy might cause or accelerate the process of otosclerosis.20 In the 1950s, some authors even advocated termination of pregnancy and sterilization as treatment in progressive cases.21 The likely source of this idea was a paper written by Greifenstein in 1939, which stated the official policy of the German Reichsgutacherstelle (Agency of Expert Opinion of the German Reich) in regard to abortion and sterilization in women who had genetic disease.22 As a result of this guideline, in 1939, of 69 women who had otosclerosis in Germany, 43 underwent abortion and 23 were sterilized.23
Recent research argues strongly against an association between pregnancy and accelerated otosclerosis. Rigorous audiometry found no adverse effect on hearing in otosclerotic women who had children, compared with women without children. Nor were air conduction, bone conduction, and discrimination worse in women who had children, compared with childless women. No significant correlation was found between the number of children and hearing loss, or between lactation and hearing loss.24
Treatment of otosclerosis entails amplification throughout the pregnancy. Postpartum, an elective stapedectomy, in which the sclerotic stapes bone is replaced with a micro-prosthesis, frequently provides a clinically significant increase in hearing.
Sudden sensorineural hearing loss is rare
Although it is uncommon during pregnancy, sudden sensorineural hearing loss has been associated with hypertension and toxemia of pregnancy, presumably due to microemboli-mediated vascular occlusion of the microcirculation of the cochlea and auditory nerve. Complete otologic and audiologic evaluation, as well as treatment of the toxemia, is the standard of care.
Melasma affects almost 75% of gravidas
The “mask of pregnancy” is one of the most frequently encountered changes of pregnancy. The condition is thought to be driven by sun exposure and concomitant increases in the levels of melanocyte-stimulating hormone, serum estrogen, and progesterone. Well-delineated areas of hypermelanosis affect the face and neck. These lesions can begin during pregnancy, or become worse if they were present before conception. The most frequently involved sites are the cheeks, nose, and chin.
Avoidance of sunlight is the treatment for melasma
Topical sunscreens are recommended. Melasma typically regresses after delivery but persists in fewer than 10% of cases. Persistent hyperpigmentation can be treated with a variety of topical agents, including hydroquinone, tretinoin, kojic acid, and vitamin C, among others.25 Treatment is not always effective, however. Extensive pigmentary changes predict a poor response to topical therapy.
Pyogenic granuloma usually regresses postpartum
Granuloma gravidarum, or pyogenic granuloma of pregnancy, consists of soft, pedunculated, vascular proliferations, most commonly arising from the gingiva and nasal mucosa in 2% of pregnant women.25 These proliferations are thought to be triggered by the myriad hormonal changes of pregnancy superimposed on local tissue trauma. These lesions rarely exceed 2 cm in size, but they can ulcerate and cause pain. They frequently regress 1 to 2 months postpartum. Surgical resection is utilized only to stanch recalcitrant bleeding. When lesions recur after surgical excision, inadequate resection is thought to be the cause. A recent report described the Nd:YAG laser as an effective tool for treatment of these lesions.26
Part 1 of this series focuses on sinonasal disease in pregnancy.
We want to hear from you! Tell us what you think.
Ear, nose, and throat complaints are common even before you superimpose the transformations and demands of pregnancy. Take gastroesophageal reflux disease (GERD), for example. Experts estimate that one third of the US population suffers from this condition.1 In pregnancy, endocrine and anatomic factors converge to exacerbate acid reflux disorders in 30% to 50% of women.2
Other complaints, too, surface or worsen during gestation. In Part 1 of this series (August 2010), we discussed sinonasal disease in pregnancy: specifically, pregnancy rhinitis, allergic rhinitis, vasomotor rhinitis, rhinitis medicamentosa, sinusitis, epistaxis, and sleep-disordered breathing. In Part 2, our focus is:
- laryngologic complaints
- – GERD
– laryngopharyngeal reflux
– laryngopathia gravidarum
- otologic disorders
- – eustachian tube dysfunction
– facial paralysis (Bell’s palsy)
– otosclerosis
– sudden sensorineural hearing loss
- endocrine abnormalities
- – thyroid nodules
- dermatologic complaints
- – melasma
– pyogenic granuloma.
Mapping the head and neck, and the spectrum of disease there in pregnancy
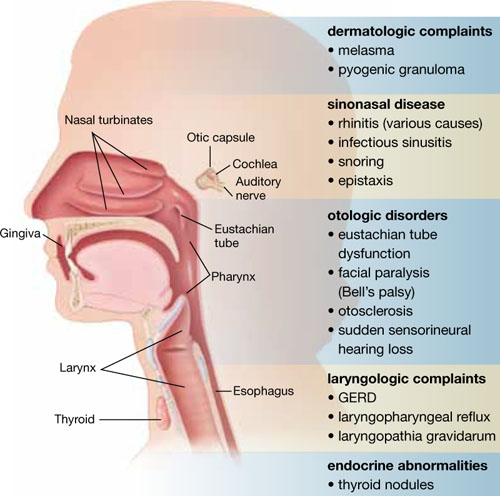
This list includes diseases and problems reviewed in the first part of this article, August 2010.
Why does GERD increase in pregnancy?
The smooth muscle–relaxing effects of progesterone and estrogen are likely responsible for the decreased tone of both the upper esophageal and gastroesophageal sphincters. This reduced tone may lead to increased reflux of stomach contents into the esophagus, larynx, and pharynx. Decreased gastric emptying and increased intestinal transit time may also play a role. Reflux of gastric contents may also be exacerbated by compression from the gravid uterus.
Gastroesophageal reflux is physiologic, occurring in healthy people as often as 50 times a day. It becomes GERD when reflux into the esophagus is excessive, causing tissue damage (esophagitis) and clinical symptoms (heartburn). Recent studies suggest that, in addition to the traditional symptoms, GERD is associated with increased severity of nausea and vomiting in pregnancy.3
Ultimately, refluxed gastric contents cause mucosal injury to the upper aerodigestive tract. The location of injury and subsequent clinical manifestations are believed to correspond to the pattern of reflux.4
Some refluxers do it in the daytime
Laryngopharyngeal reflux (LPR), widely viewed as a separate clinical entity from GERD, is backflow of stomach contents into the laryngopharynx (FIGURE).5 Fewer than 40% of patients who have LPR experience heartburn, and fewer than 25% have evidence of esophagitis.6 LPR patients are predominantly upright, daytime refluxers, whereas GERD patients are predominantly supine or nocturnal refluxers. The threshold for reflux-related injury of the laryngeal epithelium is significantly lower than the threshold for injury to epithelium of the esophagus.7 As a result, even brief reflux exposures can injure the laryngeal epithelium.8
Injury in LPR manifests clinically as posterior laryngeal edema and erythema, obliteration of the laryngeal ventricles, and interarytenoid hypertrophy.5 These changes produce symptoms of chronic throat clearing, hoarseness, cough, and the sensation that something is caught in the throat (globus sensation). History and physical examination are typically sufficient to diagnose LPR.
Lifestyle changes can make a difference in GERD and LPR
Start with simple measures. Advise the patient to elevate the head of her bed 6 to 8 inches. Our patients report that it is usually easier to tolerate books under the legs of the head end of the bed than it is to sleep with extra pillows, especially when a side position is desired.
The patient also should be advised to avoid lying down within 3 hours after eating and to avoid smoking tobacco; drinking beer, wine, coffee, soda, caffeinated tea, and citrus juice; eating foods that are fried, high in fat, or spicy; and using drugs that promote reflux (i.e., calcium channel blockers, sedatives, and nitrates).
An interesting tip: Chewing gum increases salivary bicarbonate production and may neutralize acid.9
Pharmacologic options include H2 blockers and PPIs
Antacids, such as sucralfate, neutralize acid already in the stomach and may have a role in the treatment of acute symptoms.
Histamine 2 (H2) blockers such as cimetidine (Tagamet), ranitidine (Zantac), and famotidine (Pepcid) block the histamine receptor in the stomach and reduce acid secretion by as much as 50%. These medications are typically taken two to three times daily. They all fall into Pregnancy Category B, except for nizatidine (Axid), which is Category C.
Proton pump inhibitors (PPIs). Recently, utilization of H2 blockers has given way to the newer class of PPIs, including lansoprazole (Prevacid), pantoprazole (Protonix), and esomeprazole (Nexium). These drugs target the parietal cell hydrogen potassium ATPase, reducing acid secretion by 80% to 90%. Treatment is typically once daily for uncomplicated GERD and twice daily for LPR. Patients who have LPR also require higher dosages to achieve complete acid suppression and heal the delicate laryngeal tissue. Tissue injury in LPR may take 6 months to reverse once adequate therapy has been initiated. Severe, complicated cases may require the addition of an H2 blocker or even a third daily dose of the PPI.
Patients should not discontinue a PPI abruptly because of the risk of rebound hypersecretion of gastric acid. Rather, these drugs should be stopped gradually over several weeks. They are best taken 30 minutes before a meal, as that is when they reach maximum blood concentration.
PPIs are generally considered safe for use after the first trimester of pregnancy. All are Category B drugs, except for omeprazole (Prilosec), which is a Category C drug.
The human voice is extremely sensitive to the endocrinologic changes of pregnancy. Many of these changes manifest as alterations in fluid content of the lamina propria just beneath the laryngeal mucosa.27 Collectively, the voice changes of pregnancy are known as laryngopathia gravidarum. Abdominal distension during pregnancy also interferes with abdominal muscle function, altering the mechanics of phonation and creating overuse injuries.
Symptoms include hoarseness and voice loss. Singers, in particular, notice a deeper voice and a diminished range of pitch.28 Treatment is largely supportive, with hydration, and singers should be advised to refrain from singing until abdominal muscle function resolves.
Laryngopathia gravidarum typically resolves postpartum as endocrinologic alterations return to baseline and abdominal support returns.
Eustachian tube dysfunction usually resolves postpartum
This disorder affects between 5% and 30% of pregnant women. Symptoms usually begin after the first trimester and consist of tubal obstruction or patulous Eustachian tubes. Women who have tubal obstruction report a clogged or popping sensation in their ears, with muffling of sounds. In severe cases, serous effusion may develop.
Tubal obstruction is related to edema of the respiratory mucosa. In cases in which symptoms are more distressing to the patient, increased humidity, treatment of rhinitis, and frequent Valsalva maneuvers have had variable success in providing relief. For recalcitrant cases, pressure-equalization tubes can be placed (in an otolaryngology clinic).
Women who have patulous tubes usually report intermittent symptoms that consist of autophony and a roaring sensation in their ears that is synchronous with breathing and is worse when they are in an upright position or exercising (or both). The cause of patulous Eustachian tubes is not well defined. Weight loss and hormonal variables are believed to play a role.
This condition typically resolves postpartum.
Treatment is largely supportive, including humidification, reassurance, and instructions on how to perform a forceful inspiratory nasal sniff.
Incidence of Bell’s palsy in pregnancy is uncertain
A possible association between pregnancy and idiopathic facial paralysis (Bell’s palsy) was first noted by Sir Charles Bell in 1830. Retrospective literature at first suggested a 3.3-fold increased risk of Bell’s palsy during pregnancy, with the incidence peaking during the third trimester of gestation.10 Subsequent re-analysis found no significant difference in the incidence of Bell’s palsy between pregnant and nonpregnant women of childbearing age.11 Prospective studies are sorely needed to definitively establish the incidence of Bell’s palsy in pregnancy.
Bell’s palsy typically appears during the third trimester
A unique aspect of Bell’s palsy in pregnancy is its tendency to manifest during the third trimester and postpartum. The most widely accepted theory for this phenomenon is the reactivation of latent herpes simplex virus within the geniculate ganglion.12 A large body of scientific work supports this theory.
The maternal immune system undergoes complex alterations during pregnancy, although the mechanisms for these changes are not completely understood. The most pronounced change is a shift from cell-mediated immune responses toward humoral and innate immune responses as pregnancy progresses.13 Such a shift likely reduces the maternal cytotoxic potential against fetal antigens.14 Clinically, the decrease in cellular immunity manifests as an increased susceptibility to intracellular pathogens such as herpes simplex virus later in pregnancy.15
Sudden facial weakness is the usual presenting symptom
This weakness develops over 24 to 48 hours, progressing to complete or near-complete paralysis within 1 week. Associated symptoms often include pain, fever, dry eye, a change in taste and salivation, and sensitivity to noise.11
Diagnosis of Bell’s palsy requires the exclusion of other causes, accomplished primarily by taking a thorough history and performing a physical examination. Between 14% and 21% of pregnant patients who have acute facial paralysis have causes other than Bell’s palsy.16
Among the other causes of facial paralysis are herpes zoster oticus (Ramsay Hunt syndrome), in which varicella zoster virus reactivates at the geniculate ganglion.10 The patient with this disorder experiences facial nerve paralysis, skin eruption in the auricular canal, and cochleovestibular symptoms. Ramsay Hunt syndrome generally has a worse prognosis than Bell’s palsy for return of facial function.
Recurrent facial nerve paralysis can also be seen in Lyme disease, and prolonged paralysis may occur in Guillain-Barré syndrome.
When facial paralysis is accompanied by ear pain and purulent otorrhea, the cause may be acute otitis media. Cholesteatoma, trauma, neoplasm, myasthenia gravis, arteriovenous malformation, and mumps can all produce facial paralysis.
Treatment in pregnancy resembles treatment in the general population
Topical eye care, oral corticosteroids, and antiviral medications are the standard of care for Bell’s palsy. Surgical decompression may be utilized in the nonpregnant population, but reports of facial nerve decompression during pregnancy are extremely rare.
Eye care involves the use of preservative-free artificial tears, a viscous ocular ointment (Lacri-Lube) that must be applied at bedtime, with taping of the eyelids (shut) indicated at night for severe paralysis. Eye care plays a critical role in the prevention of ocular complications such as corneal abrasion.
Steroid treatment (i.e., prednisone at a dosage of 1 mg/kg for 5 days, followed by tapering) improves recovery in Bell’s palsy when it is initiated within 14 days after the onset of facial paralysis.17 However, use of steroids during the first trimester of pregnancy has been associated with an increased risk of cleft palate, and infants born to mothers who received exogenous steroids during gestation should be watched for adrenal hypofunction.
Antiviral medications represent another adjunctive treatment for Bell’s palsy. Nucleoside analogues, including valacyclovir (Valtrex) and famciclovir (Famvir) (both Category B), pose little risk to mother and fetus. In fact, these agents are commonly used to prevent outbreaks of herpes simplex virus late in pregnancy. Two double-blind, randomized, controlled trials in nonpregnant patients have demonstrated improved outcomes when Bell’s palsy is treated with steroids and antiviral agents within 3 days after onset of the paralysis, compared with steroids alone.18,19
Rapid diagnosis and treatment are critical for a good outcome. The potential benefits of treatment likely outweigh the limited fetal risks posed by these medications. Although there are conflicting reports, in general, pregnant patients who experience incomplete paralysis do extremely well, recovering with minimal residual deficits. The prognosis is less optimistic for patients who have complete paralysis, with persistent deficits observed in as many as 50% of cases.
Diffuse thyroid gland enlargement during pregnancy is common, occurring to varying degrees in nearly 50% of pregnant women. Pregnancy is also thought to promote the growth of existing thyroid nodules and induce the formation of new nodules.29 In both pregnant and nonpregnant patients, the majority (more than 90%) of these nodules are benign, although pregnant women appear to have a slightly higher likelihood that a solitary nodule is malignant.30
Diagnosis is straightforward
When a thyroid nodule is detected in a pregnant patient, the workup begins with a thorough history, noting age, family history of thyroid or endocrine disease, personal history of low-dosage head and neck radiation, and any recent hoarseness, dysphagia, and symptoms of hypermetabolism.
The physical exam should focus on the size and location of the thyroid abnormality, the degree of firmness of the nodule, the presence of any other nodules in the thyroid, any palpable cervical lymph nodes, and any vocal cord dysfunction.
US imaging is recommended
Because ultrasonography (US) of the thyroid is noninvasive, it is the initial imaging modality of choice. It can establish the size of any nodule (and serve as an objective baseline measurement) and identify any characteristics that suggest malignancy, such as microcalcifications, hypoechogenicity, and solid structure.
Consider fine-needle aspiration (FNA)
This technique, guided by US, is recommended when a nodule is discovered during the first trimester. However, when a nodule is discovered after 20 weeks’ gestation, the FNA option is not required. FNA can be deferred until after delivery because, even with a histologically confirmed, well-differentiated thyroid cancer, we would not operate during the third trimester—the elevated risk of preterm labor precludes that option.
When the diagnosis is cancer
The nonpregnant patient has several therapeutic options for management of thyroid cancer, but pregnancy restricts these options to close observation and surgical resection. The optimal timing of surgical management (either the second trimester or postpartum) remains unresolved.
Thyroid cancer is somewhat unique among malignancies. The majority of cancers are well-differentiated and exhibit indolent tumor biology. In one prospective study of nonpregnant patients who had small, papillary, thyroid cancers, more than 70% of those who bypassed surgical intervention had no tumor growth after 5 years of follow-up.31
Given that pregnancy is an independent risk factor for surgical complications, prolonged hospitalization, and higher hospital costs after thyroidectomy, it seems reasonable to carefully monitor, by serial US, pregnant women who have been given a diagnosis of small, well-differentiated thyroid cancer.32
In general, if a nodule is discovered during the first trimester and is larger than 1.5 cm, and if the diagnosis is cytology-proven, differentiated thyroid cancer, we would consider surgery during the second trimester if the patient were adamant. Other authors recommend second-trimester surgery more strongly.33 Regardless of the timing of resection, adjunctive treatment with radioactive iodine ablation (RIA) 3 to 6 months after delivery is an accepted component of complete oncologic therapy. Breastfeeding is prohibited with RIA, and patients are advised to wait 1 year after RIA before conceiving again.
If the patient chooses to undergo surgical resection of the thyroid during the second trimester, be aware of the transient hypothyroid state that immediately follows surgery (before the patient becomes euthyroid on replacement hormone). Because the fetus begins to synthesize its own thyroid hormone around the 18th week of gestation, we agree with the contention that the optimal time to operate is between week 19 and week 22 of gestation.34 Operating before 24 weeks also reduces the concerns related to fetal viability.
If a nodule is cytology-proven to be differentiated thyroid cancer and is smaller than 1.5 cm or is discovered late in the second trimester or beyond, most authors recommend delaying surgery until after delivery.
Outcomes are not worse in pregnancy
Pregnant women who have well-differentiated thyroid cancer and their nonpregnant counterparts have statistically identical outcomes. Moosa and Mazzaferri demonstrated no significant differences in the rate of recurrence, distant spread, or mortality.35 Their findings have been replicated in a larger, population-based study.36 There also appears to be no significant differences in maternal survival or fetal outcome between women who undergo surgical intervention during the second trimester and those who delay surgery to the postpartum period.35,37,38 After treatment, the risk of recurrence does not increase in subsequent pregnancies.35
Otosclerosis may lead to hearing loss
The primary disease of the otic capsule, otosclerosis is characterized by alternating phases of absorption of compact bony tissue and replacement with spongy bone. The most common location of this disorder is the oval window, and it can lead to stapedial ankylosis and subsequent conductive hearing loss. The disease can eventually progress to cochlear otosclerosis with sensorineural hearing loss.
Otosclerosis is multifactorial in origin, with contributors that include genetics, fluoridated water, exposure to measles, and vitamin D deficiency.
Pregnancy probably does not accelerate otosclerosis
Early reports, based on subjective, self-reported hearing endpoints, suggested that pregnancy might cause or accelerate the process of otosclerosis.20 In the 1950s, some authors even advocated termination of pregnancy and sterilization as treatment in progressive cases.21 The likely source of this idea was a paper written by Greifenstein in 1939, which stated the official policy of the German Reichsgutacherstelle (Agency of Expert Opinion of the German Reich) in regard to abortion and sterilization in women who had genetic disease.22 As a result of this guideline, in 1939, of 69 women who had otosclerosis in Germany, 43 underwent abortion and 23 were sterilized.23
Recent research argues strongly against an association between pregnancy and accelerated otosclerosis. Rigorous audiometry found no adverse effect on hearing in otosclerotic women who had children, compared with women without children. Nor were air conduction, bone conduction, and discrimination worse in women who had children, compared with childless women. No significant correlation was found between the number of children and hearing loss, or between lactation and hearing loss.24
Treatment of otosclerosis entails amplification throughout the pregnancy. Postpartum, an elective stapedectomy, in which the sclerotic stapes bone is replaced with a micro-prosthesis, frequently provides a clinically significant increase in hearing.
Sudden sensorineural hearing loss is rare
Although it is uncommon during pregnancy, sudden sensorineural hearing loss has been associated with hypertension and toxemia of pregnancy, presumably due to microemboli-mediated vascular occlusion of the microcirculation of the cochlea and auditory nerve. Complete otologic and audiologic evaluation, as well as treatment of the toxemia, is the standard of care.
Melasma affects almost 75% of gravidas
The “mask of pregnancy” is one of the most frequently encountered changes of pregnancy. The condition is thought to be driven by sun exposure and concomitant increases in the levels of melanocyte-stimulating hormone, serum estrogen, and progesterone. Well-delineated areas of hypermelanosis affect the face and neck. These lesions can begin during pregnancy, or become worse if they were present before conception. The most frequently involved sites are the cheeks, nose, and chin.
Avoidance of sunlight is the treatment for melasma
Topical sunscreens are recommended. Melasma typically regresses after delivery but persists in fewer than 10% of cases. Persistent hyperpigmentation can be treated with a variety of topical agents, including hydroquinone, tretinoin, kojic acid, and vitamin C, among others.25 Treatment is not always effective, however. Extensive pigmentary changes predict a poor response to topical therapy.
Pyogenic granuloma usually regresses postpartum
Granuloma gravidarum, or pyogenic granuloma of pregnancy, consists of soft, pedunculated, vascular proliferations, most commonly arising from the gingiva and nasal mucosa in 2% of pregnant women.25 These proliferations are thought to be triggered by the myriad hormonal changes of pregnancy superimposed on local tissue trauma. These lesions rarely exceed 2 cm in size, but they can ulcerate and cause pain. They frequently regress 1 to 2 months postpartum. Surgical resection is utilized only to stanch recalcitrant bleeding. When lesions recur after surgical excision, inadequate resection is thought to be the cause. A recent report described the Nd:YAG laser as an effective tool for treatment of these lesions.26
Part 1 of this series focuses on sinonasal disease in pregnancy.
We want to hear from you! Tell us what you think.
1. American Gastroenterological Association. The burden of chronic gastrointestinal diseases study. Bethesda, Md: AGA; 2001.
2. Cappell MS, Garcia A. Gastric and duodenal ulcers during pregnancy. Gastroenterol Clin North Am. 1998;27(1):169-195.
3. Gill SK, Maltepe C, Koren G. The effect of heartburn and acid reflux on the severity of nausea and vomiting of pregnancy. Can J Gastroenterol. 2009;23(4):270-272.
4. Wiener GJ, Koufman JA, Wu WC, Cooper JB, Richter JE, Castell DO. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84(12):1503-1508.
5. Gupta R, Sataloff RT. Laryngopharyngeal reflux: current concepts and questions. Curr Opin Otolaryngol Head Neck Surg. 2009;17(3):143-148.
6. Koufman JA, Belafsky PC, Bach KK, Daniel E, Postma GN. Prevalence of esophagitis in patients with pH-documented laryngopharyngeal reflux. Laryngoscope. 2002;112(9):1606-1609.
7. Johnston N, Bulmer D, Gill GA, Panetti M, et al. Cell biology of laryngeal epithelial defenses in health and disease: further studies. Ann Otol Rhinol Laryngol. 2003;112(6):481-491.
8. Gill GA, Johnston N, Buda A, et al. Laryngeal epithelial defenses against laryngopharyngeal reflux: investigations of E-cadherin, carbonic anhydrase isoenzyme III, and pepsin. Ann Otol Rhinol Laryngol. 2005;114(12):913-921.
9. Smoak BR, Koufman JA. Effects of gum chewing on pharyngeal and esophageal pH. Ann Otol Rhinol Laryngol. 2001;110(12):1117-1119.
10. Hilsinger RL, Jr, Adour KK, Doty HE. Idiopathic facial paralysis, pregnancy, and the menstrual cycle. Ann Otol Rhinol Laryngol. 1975;84(4 Pt 1):433-442.
11. Vrabec JT, Isaacson B, Van Hook JW. Bell’s palsy and pregnancy. Otolaryngol Head Neck Surg. 2007;137(6):858-861.
12. Murakami S, Mizobuchi M, Nakashiro Y, Doi T, Hato N, Yanagihara N. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med. 1996;124(1 Pt 1):27-30.
13. Sacks G, Sargent I, Redman C. An innate view of human pregnancy. Immunol Today. 1999;20(3):114-118.
14. Wegmann TG, Lin H, Guilbert L, Mosmann TR. Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol Today. 1993;14(7):353-356.
15. Stirrat GM. Pregnancy and immunity. BMJ. 1994;308(6941):1385-1386.
16. Gillman GS, Schaitkin BM, May M, Klein SR. Bell’s palsy in pregnancy: a study of recovery outcomes. Otolaryngol Head Neck Surg. 2002;126(1):26-30.
17. Ramsey MJ, DerSimonian R, Holtel MR, Burgess LP. Corticosteroid treatment for idiopathic facial nerve paralysis: a meta-analysis. Laryngoscope. 2000;110(3 Pt 1):335-341.
18. Adour KK, Ruboyianes JM, Von Doersten PG, et al. Bell’s palsy treatment with acyclovir and prednisone compared with prednisone alone: a double-blind, randomized, controlled trial. Ann Otol Rhinol Laryngol. 1996;105(5):371-378.
19. Hato N, Yamada H, Kohno H, et al. Valacyclovir and prednisolone treatment for Bell’s palsy: a multicenter, randomized, placebo-controlled study. Otol Neurotol. 2007;28(3):408-413.
20. Gristwood RE, Venables WN. Pregnancy and otosclerosis. Clin Otolaryngol Allied Sci. 1983;8(3):205-210.
21. Pearson E. The effect of pregnancy on otosclerosis. Ann West Med Surg. 1951;5(5):477-482.
22. Greifenstein. Schwangerschaftsunterbrechung und unfruchtbarmachung aus gesundheitlichen Grunden bei Otosklerose. Zeitschrift fur halsnasen und ohrenheilkunde 1939;46:344-362.
23. Markou K, Goudakos J. An overview of the etiology of otosclerosis. Eur Arch Otorhinolaryngol. 2009;266(1):25-35.
24. Lippy WH, Berenholz LP, Schuring AG, et al. Does pregnancy affect otosclerosis? Laryngoscope. 2005;115(10):1833-1836.
25. Muallem MM, Rubeiz NG. Physiological and biological skin changes in pregnancy. Clin Dermatol. 2006;24(2):80-83.
26. Powell JL, Bailey CL, Coopland AT, Otis CN, Frank JL, Meyer I. Nd:YAG laser excision of a giant gingival pyogenic granuloma of pregnancy. Lasers Surg Med. 1994;14(2):178-183.
27. Brodnitz FS. Hormones and the human voice. Bull NY Acad Med. 1971;47(2):183-191.
28. Sataloff RT, Hoover CA. Endocrine dysfunction. In: Sataloff RT, ed. Professional voice: the science and art of clinical care. 2nd ed. San Diego, CA: Singular Publishing Group, Inc. 1997;293-295.
29. Kung AW, Chau MT, Lao TT, Tam SC, Low LC. The effect of pregnancy on thyroid nodule formation. J Clin Endocrinol Metab. 2002;87(3):1010-1014.
30. Smith LH, Danielsen B, Allen ME, Cress R. Cancer associated with obstetric delivery: results of linkage with the California cancer registry. Am J Obstet Gynecol. 2003;189(4):1128-1135.
31. Ito Y, Uruno T, Nakano K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid. 2003;13(4):381-387.
32. Kuy S, Roman SA, Desai R, Sosa JA. Outcomes following thyroid and parathyroid surgery in pregnant women. Arch Surg. 2009;144(5):399-406.
33. Rosen IB, Korman M, Walfish PG. Thyroid nodular disease in pregnancy: current diagnosis and management. Clin Obstet Gynecol. 1997;40(1):81-89.
34. Fanarjian N, Athavale SM, Herrero N, et al. Thyroid cancer in pregnancy. Laryngoscope. 2007;117(10):1777-1781.
35. Moosa M, Mazzaferri EL. Outcome of differentiated thyroid cancer diagnosed in pregnant women. J Clin Endocrinol Metab. 1997;82(9):2862-2866.
36. Yasmeen S, Cress R, Romano PS, et al. Thyroid cancer in pregnancy. Int J Gynaecol Obstet. 2005;91(1):15-20.
37. Nam KH, Yoon JH, Chang HS, Park CS. Optimal timing of surgery in well-differentiated thyroid carcinoma detected during pregnancy. J Surg Oncol. 2005;91(3):199-203.
38. Doherty CM, Shindo ML, et al. Management of thyroid nodules during pregnancy. Laryngoscope. 1995;105(3 Pt 1):251-255.
1. American Gastroenterological Association. The burden of chronic gastrointestinal diseases study. Bethesda, Md: AGA; 2001.
2. Cappell MS, Garcia A. Gastric and duodenal ulcers during pregnancy. Gastroenterol Clin North Am. 1998;27(1):169-195.
3. Gill SK, Maltepe C, Koren G. The effect of heartburn and acid reflux on the severity of nausea and vomiting of pregnancy. Can J Gastroenterol. 2009;23(4):270-272.
4. Wiener GJ, Koufman JA, Wu WC, Cooper JB, Richter JE, Castell DO. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84(12):1503-1508.
5. Gupta R, Sataloff RT. Laryngopharyngeal reflux: current concepts and questions. Curr Opin Otolaryngol Head Neck Surg. 2009;17(3):143-148.
6. Koufman JA, Belafsky PC, Bach KK, Daniel E, Postma GN. Prevalence of esophagitis in patients with pH-documented laryngopharyngeal reflux. Laryngoscope. 2002;112(9):1606-1609.
7. Johnston N, Bulmer D, Gill GA, Panetti M, et al. Cell biology of laryngeal epithelial defenses in health and disease: further studies. Ann Otol Rhinol Laryngol. 2003;112(6):481-491.
8. Gill GA, Johnston N, Buda A, et al. Laryngeal epithelial defenses against laryngopharyngeal reflux: investigations of E-cadherin, carbonic anhydrase isoenzyme III, and pepsin. Ann Otol Rhinol Laryngol. 2005;114(12):913-921.
9. Smoak BR, Koufman JA. Effects of gum chewing on pharyngeal and esophageal pH. Ann Otol Rhinol Laryngol. 2001;110(12):1117-1119.
10. Hilsinger RL, Jr, Adour KK, Doty HE. Idiopathic facial paralysis, pregnancy, and the menstrual cycle. Ann Otol Rhinol Laryngol. 1975;84(4 Pt 1):433-442.
11. Vrabec JT, Isaacson B, Van Hook JW. Bell’s palsy and pregnancy. Otolaryngol Head Neck Surg. 2007;137(6):858-861.
12. Murakami S, Mizobuchi M, Nakashiro Y, Doi T, Hato N, Yanagihara N. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med. 1996;124(1 Pt 1):27-30.
13. Sacks G, Sargent I, Redman C. An innate view of human pregnancy. Immunol Today. 1999;20(3):114-118.
14. Wegmann TG, Lin H, Guilbert L, Mosmann TR. Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol Today. 1993;14(7):353-356.
15. Stirrat GM. Pregnancy and immunity. BMJ. 1994;308(6941):1385-1386.
16. Gillman GS, Schaitkin BM, May M, Klein SR. Bell’s palsy in pregnancy: a study of recovery outcomes. Otolaryngol Head Neck Surg. 2002;126(1):26-30.
17. Ramsey MJ, DerSimonian R, Holtel MR, Burgess LP. Corticosteroid treatment for idiopathic facial nerve paralysis: a meta-analysis. Laryngoscope. 2000;110(3 Pt 1):335-341.
18. Adour KK, Ruboyianes JM, Von Doersten PG, et al. Bell’s palsy treatment with acyclovir and prednisone compared with prednisone alone: a double-blind, randomized, controlled trial. Ann Otol Rhinol Laryngol. 1996;105(5):371-378.
19. Hato N, Yamada H, Kohno H, et al. Valacyclovir and prednisolone treatment for Bell’s palsy: a multicenter, randomized, placebo-controlled study. Otol Neurotol. 2007;28(3):408-413.
20. Gristwood RE, Venables WN. Pregnancy and otosclerosis. Clin Otolaryngol Allied Sci. 1983;8(3):205-210.
21. Pearson E. The effect of pregnancy on otosclerosis. Ann West Med Surg. 1951;5(5):477-482.
22. Greifenstein. Schwangerschaftsunterbrechung und unfruchtbarmachung aus gesundheitlichen Grunden bei Otosklerose. Zeitschrift fur halsnasen und ohrenheilkunde 1939;46:344-362.
23. Markou K, Goudakos J. An overview of the etiology of otosclerosis. Eur Arch Otorhinolaryngol. 2009;266(1):25-35.
24. Lippy WH, Berenholz LP, Schuring AG, et al. Does pregnancy affect otosclerosis? Laryngoscope. 2005;115(10):1833-1836.
25. Muallem MM, Rubeiz NG. Physiological and biological skin changes in pregnancy. Clin Dermatol. 2006;24(2):80-83.
26. Powell JL, Bailey CL, Coopland AT, Otis CN, Frank JL, Meyer I. Nd:YAG laser excision of a giant gingival pyogenic granuloma of pregnancy. Lasers Surg Med. 1994;14(2):178-183.
27. Brodnitz FS. Hormones and the human voice. Bull NY Acad Med. 1971;47(2):183-191.
28. Sataloff RT, Hoover CA. Endocrine dysfunction. In: Sataloff RT, ed. Professional voice: the science and art of clinical care. 2nd ed. San Diego, CA: Singular Publishing Group, Inc. 1997;293-295.
29. Kung AW, Chau MT, Lao TT, Tam SC, Low LC. The effect of pregnancy on thyroid nodule formation. J Clin Endocrinol Metab. 2002;87(3):1010-1014.
30. Smith LH, Danielsen B, Allen ME, Cress R. Cancer associated with obstetric delivery: results of linkage with the California cancer registry. Am J Obstet Gynecol. 2003;189(4):1128-1135.
31. Ito Y, Uruno T, Nakano K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid. 2003;13(4):381-387.
32. Kuy S, Roman SA, Desai R, Sosa JA. Outcomes following thyroid and parathyroid surgery in pregnant women. Arch Surg. 2009;144(5):399-406.
33. Rosen IB, Korman M, Walfish PG. Thyroid nodular disease in pregnancy: current diagnosis and management. Clin Obstet Gynecol. 1997;40(1):81-89.
34. Fanarjian N, Athavale SM, Herrero N, et al. Thyroid cancer in pregnancy. Laryngoscope. 2007;117(10):1777-1781.
35. Moosa M, Mazzaferri EL. Outcome of differentiated thyroid cancer diagnosed in pregnant women. J Clin Endocrinol Metab. 1997;82(9):2862-2866.
36. Yasmeen S, Cress R, Romano PS, et al. Thyroid cancer in pregnancy. Int J Gynaecol Obstet. 2005;91(1):15-20.
37. Nam KH, Yoon JH, Chang HS, Park CS. Optimal timing of surgery in well-differentiated thyroid carcinoma detected during pregnancy. J Surg Oncol. 2005;91(3):199-203.
38. Doherty CM, Shindo ML, et al. Management of thyroid nodules during pregnancy. Laryngoscope. 1995;105(3 Pt 1):251-255.