User login
Conference highlights growing HAI concerns
The Fifth Decennial International Conference on Healthcare-Associated Infections 2010, held in March in Atlanta, featured experts from several different fields discussing the significant prevalence of healthcare-associated infections (HAIs) and strategies that may be implemented to reduce their occurrence.
HAIs precipitated by the use of such devices as central venous catheters (CVCs), mechanical ventilators, and indwelling urinary catheters received special emphasis as important sources of patient morbidity and mortality.
Naomi O’Grady of the National Institutes of Health (NIH) summarized the current available knowledge regarding the prevention of central-line-associated bloodstream infections (CLABSIs). Strategies targeting appropriate line maintenance include:
- Chlorhexidine sponge dressings at the CVC insertion site in patients with short-term catheters;
- Cleanse catheter hubs and connectors with alcoholic-chlorhexidine (rather than alcohol alone) after each use; and
- Consider daily bathing of patients with chlorhexidine soap.
Speakers stressed that novel technologies, such as antimicrobial lock solutions and antiseptic- or antibiotic-impregnated catheters, should be considered when CLABSI rates remain high. Mark Shelly, MD, of Rochester, N.Y., emphasized awareness that CLABSIs occur frequently outside the ICU. “If you are only looking for CLABSI in the ICU, then you are missing more than half of the story,” Dr. Shelly said. Researchers from the National Health Safety Network (NHSN) provided more information about the substantial numbers of CLABSIs that occur on general medical wards.
Carolyn Gould, MD, MS, of the Centers for Disease Control and Prevention (CDC) confirmed that catheter-associated urinary tract infections (CAUTIs) are the most common type of HAI. CAUTIs occur at a frequency of >560,000 infections per year and cost as much as $500 million per year, she explained. Strategies to prevent CAUTIs include inserting urinary catheters only for appropriate indications and leaving them in place for the shortest possible duration.
In recent years, concern has grown about the prevalence of healthcare-associated Clostridium difficile infection (HA-CDI), which can lead to uncomplicated diarrhea, sepsis, or even death. Several speakers described strategies that reduce HA-CDI development, including the identification and removal of environmental sources of C. diff, accommodating CDI patients in a private room with contact precautions, and minimizing both the frequency and duration of antimicrobial therapy.
Uncertainty about the most reliable tests to confirm CDI was a topic of focus. Enzyme immunoassay (EIA) testing, cell cytotoxin assays, and polymerase chain reaction (PCR) testing are readily available in most U.S. hospitals; however, PCR testing might prove to be the most advantageous since it is rapid, sensitive, and specific.
Neil Fishman, MD, of the University of Pennsylvania School of Medicine in Philadelphia was one of several speakers to address the important role of antimicrobial stewardship program (ASP) development. According to Dr. Fishman, ASP goals should be to “ensure the proper use of antimicrobials” and to “promote cost-effectiveness.” By taking actions that promote the appropriate use of antimicrobials, the following positive consequences can be anticipated:
- Improved clinical outcomes;
- Reduced risk of adverse drug effects; and
- A reduction in, or stabilization of, the rate of antimicrobial resistance.
Multidrug-resistant (MDR) gram-negative Bacillus is a major challenge for hospitals worldwide. The CDC offers two guidelines for the optimal management and isolation of MDR organisms (MDRO): HICPAC 2006 (a management guideline) and HICPAC 2007 (MDRO isolation precaution guidelines). Consistent utilization of these guidelines is crucial to control the spread of MDRO.
The CDC’s Alexander Killen, MD, discussed the increasing proportion of MDR Acinetobacter and Enterobacteriaceae. Emerging issues among these organisms include the development of highly resistant strains, the incidence of which is increasing in nonacute-care settings.
The CDC’s Karen Anderson reported laboratory data on carbapenem-resistant Enterobacteriaceae (CRE) in a long-term-care facility. Her team demonstrated that CRE colonization can persist for up to six months. She speculated that the transfer of resistance between different species occurs, as does patient-to-patient transmission.
The CDC recommends the use of surveillance cultures as part of enhanced precautions. Surveillance is to continue until no new cases are detected.
Karen Clarke, MD, MS, MPH
Ketino Kobaidze, MD, PhD
Mohamad Moussa, MD
Sheri Tejedor, MD
Emory University
School of Medicine, Atlanta
The Fifth Decennial International Conference on Healthcare-Associated Infections 2010, held in March in Atlanta, featured experts from several different fields discussing the significant prevalence of healthcare-associated infections (HAIs) and strategies that may be implemented to reduce their occurrence.
HAIs precipitated by the use of such devices as central venous catheters (CVCs), mechanical ventilators, and indwelling urinary catheters received special emphasis as important sources of patient morbidity and mortality.
Naomi O’Grady of the National Institutes of Health (NIH) summarized the current available knowledge regarding the prevention of central-line-associated bloodstream infections (CLABSIs). Strategies targeting appropriate line maintenance include:
- Chlorhexidine sponge dressings at the CVC insertion site in patients with short-term catheters;
- Cleanse catheter hubs and connectors with alcoholic-chlorhexidine (rather than alcohol alone) after each use; and
- Consider daily bathing of patients with chlorhexidine soap.
Speakers stressed that novel technologies, such as antimicrobial lock solutions and antiseptic- or antibiotic-impregnated catheters, should be considered when CLABSI rates remain high. Mark Shelly, MD, of Rochester, N.Y., emphasized awareness that CLABSIs occur frequently outside the ICU. “If you are only looking for CLABSI in the ICU, then you are missing more than half of the story,” Dr. Shelly said. Researchers from the National Health Safety Network (NHSN) provided more information about the substantial numbers of CLABSIs that occur on general medical wards.
Carolyn Gould, MD, MS, of the Centers for Disease Control and Prevention (CDC) confirmed that catheter-associated urinary tract infections (CAUTIs) are the most common type of HAI. CAUTIs occur at a frequency of >560,000 infections per year and cost as much as $500 million per year, she explained. Strategies to prevent CAUTIs include inserting urinary catheters only for appropriate indications and leaving them in place for the shortest possible duration.
In recent years, concern has grown about the prevalence of healthcare-associated Clostridium difficile infection (HA-CDI), which can lead to uncomplicated diarrhea, sepsis, or even death. Several speakers described strategies that reduce HA-CDI development, including the identification and removal of environmental sources of C. diff, accommodating CDI patients in a private room with contact precautions, and minimizing both the frequency and duration of antimicrobial therapy.
Uncertainty about the most reliable tests to confirm CDI was a topic of focus. Enzyme immunoassay (EIA) testing, cell cytotoxin assays, and polymerase chain reaction (PCR) testing are readily available in most U.S. hospitals; however, PCR testing might prove to be the most advantageous since it is rapid, sensitive, and specific.
Neil Fishman, MD, of the University of Pennsylvania School of Medicine in Philadelphia was one of several speakers to address the important role of antimicrobial stewardship program (ASP) development. According to Dr. Fishman, ASP goals should be to “ensure the proper use of antimicrobials” and to “promote cost-effectiveness.” By taking actions that promote the appropriate use of antimicrobials, the following positive consequences can be anticipated:
- Improved clinical outcomes;
- Reduced risk of adverse drug effects; and
- A reduction in, or stabilization of, the rate of antimicrobial resistance.
Multidrug-resistant (MDR) gram-negative Bacillus is a major challenge for hospitals worldwide. The CDC offers two guidelines for the optimal management and isolation of MDR organisms (MDRO): HICPAC 2006 (a management guideline) and HICPAC 2007 (MDRO isolation precaution guidelines). Consistent utilization of these guidelines is crucial to control the spread of MDRO.
The CDC’s Alexander Killen, MD, discussed the increasing proportion of MDR Acinetobacter and Enterobacteriaceae. Emerging issues among these organisms include the development of highly resistant strains, the incidence of which is increasing in nonacute-care settings.
The CDC’s Karen Anderson reported laboratory data on carbapenem-resistant Enterobacteriaceae (CRE) in a long-term-care facility. Her team demonstrated that CRE colonization can persist for up to six months. She speculated that the transfer of resistance between different species occurs, as does patient-to-patient transmission.
The CDC recommends the use of surveillance cultures as part of enhanced precautions. Surveillance is to continue until no new cases are detected.
Karen Clarke, MD, MS, MPH
Ketino Kobaidze, MD, PhD
Mohamad Moussa, MD
Sheri Tejedor, MD
Emory University
School of Medicine, Atlanta
The Fifth Decennial International Conference on Healthcare-Associated Infections 2010, held in March in Atlanta, featured experts from several different fields discussing the significant prevalence of healthcare-associated infections (HAIs) and strategies that may be implemented to reduce their occurrence.
HAIs precipitated by the use of such devices as central venous catheters (CVCs), mechanical ventilators, and indwelling urinary catheters received special emphasis as important sources of patient morbidity and mortality.
Naomi O’Grady of the National Institutes of Health (NIH) summarized the current available knowledge regarding the prevention of central-line-associated bloodstream infections (CLABSIs). Strategies targeting appropriate line maintenance include:
- Chlorhexidine sponge dressings at the CVC insertion site in patients with short-term catheters;
- Cleanse catheter hubs and connectors with alcoholic-chlorhexidine (rather than alcohol alone) after each use; and
- Consider daily bathing of patients with chlorhexidine soap.
Speakers stressed that novel technologies, such as antimicrobial lock solutions and antiseptic- or antibiotic-impregnated catheters, should be considered when CLABSI rates remain high. Mark Shelly, MD, of Rochester, N.Y., emphasized awareness that CLABSIs occur frequently outside the ICU. “If you are only looking for CLABSI in the ICU, then you are missing more than half of the story,” Dr. Shelly said. Researchers from the National Health Safety Network (NHSN) provided more information about the substantial numbers of CLABSIs that occur on general medical wards.
Carolyn Gould, MD, MS, of the Centers for Disease Control and Prevention (CDC) confirmed that catheter-associated urinary tract infections (CAUTIs) are the most common type of HAI. CAUTIs occur at a frequency of >560,000 infections per year and cost as much as $500 million per year, she explained. Strategies to prevent CAUTIs include inserting urinary catheters only for appropriate indications and leaving them in place for the shortest possible duration.
In recent years, concern has grown about the prevalence of healthcare-associated Clostridium difficile infection (HA-CDI), which can lead to uncomplicated diarrhea, sepsis, or even death. Several speakers described strategies that reduce HA-CDI development, including the identification and removal of environmental sources of C. diff, accommodating CDI patients in a private room with contact precautions, and minimizing both the frequency and duration of antimicrobial therapy.
Uncertainty about the most reliable tests to confirm CDI was a topic of focus. Enzyme immunoassay (EIA) testing, cell cytotoxin assays, and polymerase chain reaction (PCR) testing are readily available in most U.S. hospitals; however, PCR testing might prove to be the most advantageous since it is rapid, sensitive, and specific.
Neil Fishman, MD, of the University of Pennsylvania School of Medicine in Philadelphia was one of several speakers to address the important role of antimicrobial stewardship program (ASP) development. According to Dr. Fishman, ASP goals should be to “ensure the proper use of antimicrobials” and to “promote cost-effectiveness.” By taking actions that promote the appropriate use of antimicrobials, the following positive consequences can be anticipated:
- Improved clinical outcomes;
- Reduced risk of adverse drug effects; and
- A reduction in, or stabilization of, the rate of antimicrobial resistance.
Multidrug-resistant (MDR) gram-negative Bacillus is a major challenge for hospitals worldwide. The CDC offers two guidelines for the optimal management and isolation of MDR organisms (MDRO): HICPAC 2006 (a management guideline) and HICPAC 2007 (MDRO isolation precaution guidelines). Consistent utilization of these guidelines is crucial to control the spread of MDRO.
The CDC’s Alexander Killen, MD, discussed the increasing proportion of MDR Acinetobacter and Enterobacteriaceae. Emerging issues among these organisms include the development of highly resistant strains, the incidence of which is increasing in nonacute-care settings.
The CDC’s Karen Anderson reported laboratory data on carbapenem-resistant Enterobacteriaceae (CRE) in a long-term-care facility. Her team demonstrated that CRE colonization can persist for up to six months. She speculated that the transfer of resistance between different species occurs, as does patient-to-patient transmission.
The CDC recommends the use of surveillance cultures as part of enhanced precautions. Surveillance is to continue until no new cases are detected.
Karen Clarke, MD, MS, MPH
Ketino Kobaidze, MD, PhD
Mohamad Moussa, MD
Sheri Tejedor, MD
Emory University
School of Medicine, Atlanta
How should a patient with a new-onset seizure be managed?
Case
A 42-year-old man is brought to the hospital by his family after a reported seizure. The patient was found on the floor, unresponsive, and suffering convulsions lasting less than a minute. He suffered no apparent trauma before or during the event. He has no history of seizures. His mental status quickly improved; he experienced oriented lucidity with slight drowsiness. His neurological exam is nonfocal, and his vital signs and laboratory values are normal. A noncontrast head computed tomogram (CT) is normal.
What is the appropriate approach to diagnosis and management for this patient with a new-onset seizure?
Overview
A patient with a first seizure presents a dilemma. Underlying causes for seizure are potentially life-threatening, and must be identified if present. A patient whose first seizure is unprovoked is at risk for future seizures (i.e., epilepsy). However, long-term therapy with anticonvulsant medication has morbidity, side effects, and expense. Advising a patient on whether to drive has public safety and legal implications, as well as major lifestyle changes for the patient.
Seizures may be focal (limited to one area of the brain) or generalized (involving both hemispheres). For the most part, focal (also known as partial) seizures do not impair consciousness; generalized seizures do. Approximately 70% of first seizures are partial focal seizures.1 Such provoking causes as head trauma, stroke, alcohol withdrawal, brain tumors, and infections can be identified in about one-third of cases.1
Electroencephalogram (EEG) and computed tomogram (CT) of the brain should be obtained, but insufficient evidence exists to recommend other testing, which should be pursued according to the clinical context.2
Unprovoked seizures recur in about 25% to 50% of patients, resulting in a diagnosis of epilepsy.1,2,4-7
Therapy is unnecessary in patients whose seizures will not recur, but reliably identifying these patients is a challenge. Whether antiepileptic drug (AED) therapy should be initiated in patients with a first unprovoked seizure is controversial and will be reviewed below.
Review of the Data
History: No test or finding can reliably differentiate unwitnessed seizures from other events (e.g., syncope).2 History from a reliable observer often is necessary to determine whether the event actually was a seizure.2 In as many as 50% of patients with a “first” seizure, thorough history will likely reveal previously unrecognized seizures.1 Although most epilepsy syndromes begin in childhood or adolescence, a significant number of patients will experience their first seizure in adulthood.2
A thorough neurologic examination should be performed. In a minority of cases, an exam will suggest a focal lesion. An impaired level of consciousness might represent a post-ictal state or delirium.2
Diagnostic evaluation: If the history suggests a seizure, an EEG should be obtained. Although the EEG will be normal in 50% of patients following a first seizure, an abnormal EEG provides useful information about seizure type and the likelihood of recurrence.2 In nearly a quarter of patients, the EEG will show epileptiform abnormalities that predict future seizures.2
Generally, an EEG should be obtained as soon as feasible, once a seizure is suspected. Some evidence in children suggests that EEG yield is higher in the 24 hours after a first seizure.
A noncontrast head CT or magnetic resonance imaging (MRI) reveals a significant abnormality about 10% of the time.2 A CT or MRI should be obtained. Few studies have compared CT to MRI in terms of yield in determining first seizure etiology, and those that do compare the two suffer from selection bias.2 Although CT or MRI are appropriate in evaluating a patient with a first seizure, the MRI’s greater resolution might provide a higher diagnostic yield in terms of seizure etiology, and, therefore, some experts recommend MRI over CT in nonemergent cases.2
Insufficient data exist to support or refute diagnostic testing beyond brain imaging and EEG. Although electrolyte abnormalities, hypoglycemia, and infections might infrequently cause seizures, such routine blood tests as complete blood count (CBC) and chemistry panels are rarely helpful.
As many as 15% of patients with a seizure will have minor abnormalities on routine lab tests, but the abnormalities do not appear to be the cause of the seizure.2
Lumbar puncture (LP) is categorically recommended only in patients in whom there is a clinical suspicion for infection as a seizure etiology. Reviews suggest that signs and symptoms of infection are typically present in patients with meningitis or another infectious cause for seizure; LP generally has limited utility in other noninfectious causes of seizure.2
The utility of toxicology testing in a first seizure has not been studied widely. Testing urine or blood for the presence of alcohol, cocaine, methamphetamines, benzodiazepines, or drug metabolites could be useful in the appropriate clinical setting.2
It is unclear whether a patient with a first seizure requires hospitalization. If initial testing in the ED rules out serious causes of seizures, the yield for hospitalization is likely to be low. In clinical practice, however, hospitalization is common and often necessary to complete such diagnostic testing as EEG and MRI.
Medical therapy: Patients with suspected epilepsy (e.g., those whose presenting seizure is, in retrospect, not their first seizure) should begin antiepileptic drug therapy (AED).1
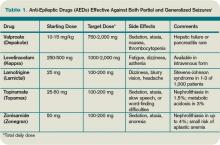
Typically, a broad-spectrum AED—one that is effective against both partial and generalized seizures—should be used as initial therapy for epilepsy. These include valproate, lamotrigine, topiramate, zonisamide, and levetiracetam (see Table 1, above). Valproate has the longest history of effectiveness; levetiracetam has fewer drug interactions, and randomized trials support its efficacy.1
Checking blood electrolytes and liver enzymes is recommended before beginning AED treatment. Significant hepatic or renal dysfunction might necessitate dosing adjustments in many AEDs.2
Inpatient consultation with a neurologist might be helpful, although insufficient evidence exists that such consultation improves patient outcomes or makes care more cost-efficient. A neurologist should follow up on patients with a first seizure after hospital discharge.2
Patients with a first seizure that likely was provoked by a reversible condition (e.g., hypotension, hypoglycemia, infection) should generally not begin AED therapy. This also includes patients with multiple seizures in a brief period of time (less than 24 hours), all attributed to the same reversible cause.1
The decision to begin AED therapy after a first unprovoked seizure is controversial. Estimates of the likelihood of seizure recurrence range from 25% at two years to 50% at one year (in the absence of AED therapy).1-2,4-7 The decision to start AED therapy after a first seizure must therefore be individualized for each patient.
Patients at high risk for recurrent seizures should begin AED therapy.1 However, no test or prognostic tool reliably identifies these patients, and initiating therapy carries side effects and places psychological, financial, and social burdens on the patient. The prevailing clinical practice, therefore, has been watchful waiting, with a second seizure constituting proof of high risk for recurrence—and need for AED therapy. Three-quarters of patients with two or more unprovoked seizures likely will go on to have recurrent seizures.6
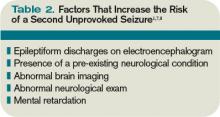
On the other hand, in patients believed to be at high risk for seizure recurrence, a more aggressive approach of initiating AED therapy after the first seizure is reasonable. A number of risk factors increasing risk for seizure recurrence have been identified (see Table 2, left).1,2 It is justified to initiate AED therapy if any of these factors are present, even after a single seizure. Still, it’s important to note that most people with risk factors will not benefit from AEDs, as only about 40% will have a seizure in the following two years.1
Early initiation of AED therapy might be appropriate for patients with occupations or hobbies in which seizures could be life-threatening (e.g., scuba divers, truck drivers).2
Low-risk patients still have a roughly 20% to 30% risk of seizure recurrence within three years.1 A second seizure that occurs while driving or while engaged in any hazardous activity could lead to serious injury.
Patients should be advised of this small but inescapable risk and instructed to contact their department of motor vehicles for specific legal restrictions, which vary by state. Once three seizure-free years have passed after a patient’s initial seizure, the chance of a recurrence falls to around 10% to 20%.6-7
Back to the Case
Our 42-year-old patient with a first seizure had normal findings on examination, laboratory studies, and brain imaging. An EEG showed epileptiform discharges in a spike and wave pattern. The attending hospitalist counseled him on his elevated risk of future seizures; the patient then elected to begin AED therapy, citing a fear of losing his driving privileges. Levetiracetam was started, which he tolerated despite mild sedation.
A year later, he suffered another seizure at his home. With regular followup and titration of his AED, he remained seizure-free for the next five years.
Bottom Line
Most patients with a single unprovoked seizure can be managed with watchful waiting, counseling, and neurological followup. Initiation of AED therapy is appropriate for patients with a high risk of seizure recurrence, or for whom another seizure could pose personal or social harm. TH
Dr. Hoffman is a hospitalist at Emory University School of Medicine in Atlanta.
References
- French JA, Pedley TA. Clinical practice: Initial management of epilepsy. N Engl J Med. 2008;359:166-176.
- Krumholz A, Wiebe S, Gronseth G, et al. Practice Parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007;69:1996-2007.
- Schachter SC. Antiepileptic drug therapy: general treatment principles and application for special patient populations. Epilepsia. 1999;40(9):S20-25.
- Hauser WA, Rich SS, Annegers JF, et al. Seizure recurrence after a first unprovoked seizure: an extended follow-up. Neurology. 1990;40:1163-1170.
- Marson A, Jacoby A, Johnson A, et al. Immediate versus deferred antiepileptic drug treatment for epilepsy and single seizures: a randomized controlled trial. Lancet. 2005;365: 2007-2013.
- Hauser WA, Rich SS, Lee JR, Annegers JF, Anderson VE. Risk of recurrent seizures after two unprovoked seizures. N Engl J Med. 1998;338:429-434.
- Berg AT. Risk of recurrence after a first unprovoked seizure. Epilepsia. 2008;49:S13-18.
- Kim LG, Johnson TL, Marson AG, et al. Prediction of risk of seizure recurrence after a single seizure and early epilepsy: further results from the MESS trial. Lancet Neurology. 2006;5(4):317-322.
Case
A 42-year-old man is brought to the hospital by his family after a reported seizure. The patient was found on the floor, unresponsive, and suffering convulsions lasting less than a minute. He suffered no apparent trauma before or during the event. He has no history of seizures. His mental status quickly improved; he experienced oriented lucidity with slight drowsiness. His neurological exam is nonfocal, and his vital signs and laboratory values are normal. A noncontrast head computed tomogram (CT) is normal.
What is the appropriate approach to diagnosis and management for this patient with a new-onset seizure?
Overview
A patient with a first seizure presents a dilemma. Underlying causes for seizure are potentially life-threatening, and must be identified if present. A patient whose first seizure is unprovoked is at risk for future seizures (i.e., epilepsy). However, long-term therapy with anticonvulsant medication has morbidity, side effects, and expense. Advising a patient on whether to drive has public safety and legal implications, as well as major lifestyle changes for the patient.
Seizures may be focal (limited to one area of the brain) or generalized (involving both hemispheres). For the most part, focal (also known as partial) seizures do not impair consciousness; generalized seizures do. Approximately 70% of first seizures are partial focal seizures.1 Such provoking causes as head trauma, stroke, alcohol withdrawal, brain tumors, and infections can be identified in about one-third of cases.1
Electroencephalogram (EEG) and computed tomogram (CT) of the brain should be obtained, but insufficient evidence exists to recommend other testing, which should be pursued according to the clinical context.2
Unprovoked seizures recur in about 25% to 50% of patients, resulting in a diagnosis of epilepsy.1,2,4-7
Therapy is unnecessary in patients whose seizures will not recur, but reliably identifying these patients is a challenge. Whether antiepileptic drug (AED) therapy should be initiated in patients with a first unprovoked seizure is controversial and will be reviewed below.
Review of the Data
History: No test or finding can reliably differentiate unwitnessed seizures from other events (e.g., syncope).2 History from a reliable observer often is necessary to determine whether the event actually was a seizure.2 In as many as 50% of patients with a “first” seizure, thorough history will likely reveal previously unrecognized seizures.1 Although most epilepsy syndromes begin in childhood or adolescence, a significant number of patients will experience their first seizure in adulthood.2
A thorough neurologic examination should be performed. In a minority of cases, an exam will suggest a focal lesion. An impaired level of consciousness might represent a post-ictal state or delirium.2
Diagnostic evaluation: If the history suggests a seizure, an EEG should be obtained. Although the EEG will be normal in 50% of patients following a first seizure, an abnormal EEG provides useful information about seizure type and the likelihood of recurrence.2 In nearly a quarter of patients, the EEG will show epileptiform abnormalities that predict future seizures.2
Generally, an EEG should be obtained as soon as feasible, once a seizure is suspected. Some evidence in children suggests that EEG yield is higher in the 24 hours after a first seizure.
A noncontrast head CT or magnetic resonance imaging (MRI) reveals a significant abnormality about 10% of the time.2 A CT or MRI should be obtained. Few studies have compared CT to MRI in terms of yield in determining first seizure etiology, and those that do compare the two suffer from selection bias.2 Although CT or MRI are appropriate in evaluating a patient with a first seizure, the MRI’s greater resolution might provide a higher diagnostic yield in terms of seizure etiology, and, therefore, some experts recommend MRI over CT in nonemergent cases.2
Insufficient data exist to support or refute diagnostic testing beyond brain imaging and EEG. Although electrolyte abnormalities, hypoglycemia, and infections might infrequently cause seizures, such routine blood tests as complete blood count (CBC) and chemistry panels are rarely helpful.
As many as 15% of patients with a seizure will have minor abnormalities on routine lab tests, but the abnormalities do not appear to be the cause of the seizure.2
Lumbar puncture (LP) is categorically recommended only in patients in whom there is a clinical suspicion for infection as a seizure etiology. Reviews suggest that signs and symptoms of infection are typically present in patients with meningitis or another infectious cause for seizure; LP generally has limited utility in other noninfectious causes of seizure.2
The utility of toxicology testing in a first seizure has not been studied widely. Testing urine or blood for the presence of alcohol, cocaine, methamphetamines, benzodiazepines, or drug metabolites could be useful in the appropriate clinical setting.2
It is unclear whether a patient with a first seizure requires hospitalization. If initial testing in the ED rules out serious causes of seizures, the yield for hospitalization is likely to be low. In clinical practice, however, hospitalization is common and often necessary to complete such diagnostic testing as EEG and MRI.
Medical therapy: Patients with suspected epilepsy (e.g., those whose presenting seizure is, in retrospect, not their first seizure) should begin antiepileptic drug therapy (AED).1
Typically, a broad-spectrum AED—one that is effective against both partial and generalized seizures—should be used as initial therapy for epilepsy. These include valproate, lamotrigine, topiramate, zonisamide, and levetiracetam (see Table 1, above). Valproate has the longest history of effectiveness; levetiracetam has fewer drug interactions, and randomized trials support its efficacy.1
Checking blood electrolytes and liver enzymes is recommended before beginning AED treatment. Significant hepatic or renal dysfunction might necessitate dosing adjustments in many AEDs.2
Inpatient consultation with a neurologist might be helpful, although insufficient evidence exists that such consultation improves patient outcomes or makes care more cost-efficient. A neurologist should follow up on patients with a first seizure after hospital discharge.2
Patients with a first seizure that likely was provoked by a reversible condition (e.g., hypotension, hypoglycemia, infection) should generally not begin AED therapy. This also includes patients with multiple seizures in a brief period of time (less than 24 hours), all attributed to the same reversible cause.1
The decision to begin AED therapy after a first unprovoked seizure is controversial. Estimates of the likelihood of seizure recurrence range from 25% at two years to 50% at one year (in the absence of AED therapy).1-2,4-7 The decision to start AED therapy after a first seizure must therefore be individualized for each patient.
Patients at high risk for recurrent seizures should begin AED therapy.1 However, no test or prognostic tool reliably identifies these patients, and initiating therapy carries side effects and places psychological, financial, and social burdens on the patient. The prevailing clinical practice, therefore, has been watchful waiting, with a second seizure constituting proof of high risk for recurrence—and need for AED therapy. Three-quarters of patients with two or more unprovoked seizures likely will go on to have recurrent seizures.6
On the other hand, in patients believed to be at high risk for seizure recurrence, a more aggressive approach of initiating AED therapy after the first seizure is reasonable. A number of risk factors increasing risk for seizure recurrence have been identified (see Table 2, left).1,2 It is justified to initiate AED therapy if any of these factors are present, even after a single seizure. Still, it’s important to note that most people with risk factors will not benefit from AEDs, as only about 40% will have a seizure in the following two years.1
Early initiation of AED therapy might be appropriate for patients with occupations or hobbies in which seizures could be life-threatening (e.g., scuba divers, truck drivers).2
Low-risk patients still have a roughly 20% to 30% risk of seizure recurrence within three years.1 A second seizure that occurs while driving or while engaged in any hazardous activity could lead to serious injury.
Patients should be advised of this small but inescapable risk and instructed to contact their department of motor vehicles for specific legal restrictions, which vary by state. Once three seizure-free years have passed after a patient’s initial seizure, the chance of a recurrence falls to around 10% to 20%.6-7
Back to the Case
Our 42-year-old patient with a first seizure had normal findings on examination, laboratory studies, and brain imaging. An EEG showed epileptiform discharges in a spike and wave pattern. The attending hospitalist counseled him on his elevated risk of future seizures; the patient then elected to begin AED therapy, citing a fear of losing his driving privileges. Levetiracetam was started, which he tolerated despite mild sedation.
A year later, he suffered another seizure at his home. With regular followup and titration of his AED, he remained seizure-free for the next five years.
Bottom Line
Most patients with a single unprovoked seizure can be managed with watchful waiting, counseling, and neurological followup. Initiation of AED therapy is appropriate for patients with a high risk of seizure recurrence, or for whom another seizure could pose personal or social harm. TH
Dr. Hoffman is a hospitalist at Emory University School of Medicine in Atlanta.
References
- French JA, Pedley TA. Clinical practice: Initial management of epilepsy. N Engl J Med. 2008;359:166-176.
- Krumholz A, Wiebe S, Gronseth G, et al. Practice Parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007;69:1996-2007.
- Schachter SC. Antiepileptic drug therapy: general treatment principles and application for special patient populations. Epilepsia. 1999;40(9):S20-25.
- Hauser WA, Rich SS, Annegers JF, et al. Seizure recurrence after a first unprovoked seizure: an extended follow-up. Neurology. 1990;40:1163-1170.
- Marson A, Jacoby A, Johnson A, et al. Immediate versus deferred antiepileptic drug treatment for epilepsy and single seizures: a randomized controlled trial. Lancet. 2005;365: 2007-2013.
- Hauser WA, Rich SS, Lee JR, Annegers JF, Anderson VE. Risk of recurrent seizures after two unprovoked seizures. N Engl J Med. 1998;338:429-434.
- Berg AT. Risk of recurrence after a first unprovoked seizure. Epilepsia. 2008;49:S13-18.
- Kim LG, Johnson TL, Marson AG, et al. Prediction of risk of seizure recurrence after a single seizure and early epilepsy: further results from the MESS trial. Lancet Neurology. 2006;5(4):317-322.
Case
A 42-year-old man is brought to the hospital by his family after a reported seizure. The patient was found on the floor, unresponsive, and suffering convulsions lasting less than a minute. He suffered no apparent trauma before or during the event. He has no history of seizures. His mental status quickly improved; he experienced oriented lucidity with slight drowsiness. His neurological exam is nonfocal, and his vital signs and laboratory values are normal. A noncontrast head computed tomogram (CT) is normal.
What is the appropriate approach to diagnosis and management for this patient with a new-onset seizure?
Overview
A patient with a first seizure presents a dilemma. Underlying causes for seizure are potentially life-threatening, and must be identified if present. A patient whose first seizure is unprovoked is at risk for future seizures (i.e., epilepsy). However, long-term therapy with anticonvulsant medication has morbidity, side effects, and expense. Advising a patient on whether to drive has public safety and legal implications, as well as major lifestyle changes for the patient.
Seizures may be focal (limited to one area of the brain) or generalized (involving both hemispheres). For the most part, focal (also known as partial) seizures do not impair consciousness; generalized seizures do. Approximately 70% of first seizures are partial focal seizures.1 Such provoking causes as head trauma, stroke, alcohol withdrawal, brain tumors, and infections can be identified in about one-third of cases.1
Electroencephalogram (EEG) and computed tomogram (CT) of the brain should be obtained, but insufficient evidence exists to recommend other testing, which should be pursued according to the clinical context.2
Unprovoked seizures recur in about 25% to 50% of patients, resulting in a diagnosis of epilepsy.1,2,4-7
Therapy is unnecessary in patients whose seizures will not recur, but reliably identifying these patients is a challenge. Whether antiepileptic drug (AED) therapy should be initiated in patients with a first unprovoked seizure is controversial and will be reviewed below.
Review of the Data
History: No test or finding can reliably differentiate unwitnessed seizures from other events (e.g., syncope).2 History from a reliable observer often is necessary to determine whether the event actually was a seizure.2 In as many as 50% of patients with a “first” seizure, thorough history will likely reveal previously unrecognized seizures.1 Although most epilepsy syndromes begin in childhood or adolescence, a significant number of patients will experience their first seizure in adulthood.2
A thorough neurologic examination should be performed. In a minority of cases, an exam will suggest a focal lesion. An impaired level of consciousness might represent a post-ictal state or delirium.2
Diagnostic evaluation: If the history suggests a seizure, an EEG should be obtained. Although the EEG will be normal in 50% of patients following a first seizure, an abnormal EEG provides useful information about seizure type and the likelihood of recurrence.2 In nearly a quarter of patients, the EEG will show epileptiform abnormalities that predict future seizures.2
Generally, an EEG should be obtained as soon as feasible, once a seizure is suspected. Some evidence in children suggests that EEG yield is higher in the 24 hours after a first seizure.
A noncontrast head CT or magnetic resonance imaging (MRI) reveals a significant abnormality about 10% of the time.2 A CT or MRI should be obtained. Few studies have compared CT to MRI in terms of yield in determining first seizure etiology, and those that do compare the two suffer from selection bias.2 Although CT or MRI are appropriate in evaluating a patient with a first seizure, the MRI’s greater resolution might provide a higher diagnostic yield in terms of seizure etiology, and, therefore, some experts recommend MRI over CT in nonemergent cases.2
Insufficient data exist to support or refute diagnostic testing beyond brain imaging and EEG. Although electrolyte abnormalities, hypoglycemia, and infections might infrequently cause seizures, such routine blood tests as complete blood count (CBC) and chemistry panels are rarely helpful.
As many as 15% of patients with a seizure will have minor abnormalities on routine lab tests, but the abnormalities do not appear to be the cause of the seizure.2
Lumbar puncture (LP) is categorically recommended only in patients in whom there is a clinical suspicion for infection as a seizure etiology. Reviews suggest that signs and symptoms of infection are typically present in patients with meningitis or another infectious cause for seizure; LP generally has limited utility in other noninfectious causes of seizure.2
The utility of toxicology testing in a first seizure has not been studied widely. Testing urine or blood for the presence of alcohol, cocaine, methamphetamines, benzodiazepines, or drug metabolites could be useful in the appropriate clinical setting.2
It is unclear whether a patient with a first seizure requires hospitalization. If initial testing in the ED rules out serious causes of seizures, the yield for hospitalization is likely to be low. In clinical practice, however, hospitalization is common and often necessary to complete such diagnostic testing as EEG and MRI.
Medical therapy: Patients with suspected epilepsy (e.g., those whose presenting seizure is, in retrospect, not their first seizure) should begin antiepileptic drug therapy (AED).1
Typically, a broad-spectrum AED—one that is effective against both partial and generalized seizures—should be used as initial therapy for epilepsy. These include valproate, lamotrigine, topiramate, zonisamide, and levetiracetam (see Table 1, above). Valproate has the longest history of effectiveness; levetiracetam has fewer drug interactions, and randomized trials support its efficacy.1
Checking blood electrolytes and liver enzymes is recommended before beginning AED treatment. Significant hepatic or renal dysfunction might necessitate dosing adjustments in many AEDs.2
Inpatient consultation with a neurologist might be helpful, although insufficient evidence exists that such consultation improves patient outcomes or makes care more cost-efficient. A neurologist should follow up on patients with a first seizure after hospital discharge.2
Patients with a first seizure that likely was provoked by a reversible condition (e.g., hypotension, hypoglycemia, infection) should generally not begin AED therapy. This also includes patients with multiple seizures in a brief period of time (less than 24 hours), all attributed to the same reversible cause.1
The decision to begin AED therapy after a first unprovoked seizure is controversial. Estimates of the likelihood of seizure recurrence range from 25% at two years to 50% at one year (in the absence of AED therapy).1-2,4-7 The decision to start AED therapy after a first seizure must therefore be individualized for each patient.
Patients at high risk for recurrent seizures should begin AED therapy.1 However, no test or prognostic tool reliably identifies these patients, and initiating therapy carries side effects and places psychological, financial, and social burdens on the patient. The prevailing clinical practice, therefore, has been watchful waiting, with a second seizure constituting proof of high risk for recurrence—and need for AED therapy. Three-quarters of patients with two or more unprovoked seizures likely will go on to have recurrent seizures.6
On the other hand, in patients believed to be at high risk for seizure recurrence, a more aggressive approach of initiating AED therapy after the first seizure is reasonable. A number of risk factors increasing risk for seizure recurrence have been identified (see Table 2, left).1,2 It is justified to initiate AED therapy if any of these factors are present, even after a single seizure. Still, it’s important to note that most people with risk factors will not benefit from AEDs, as only about 40% will have a seizure in the following two years.1
Early initiation of AED therapy might be appropriate for patients with occupations or hobbies in which seizures could be life-threatening (e.g., scuba divers, truck drivers).2
Low-risk patients still have a roughly 20% to 30% risk of seizure recurrence within three years.1 A second seizure that occurs while driving or while engaged in any hazardous activity could lead to serious injury.
Patients should be advised of this small but inescapable risk and instructed to contact their department of motor vehicles for specific legal restrictions, which vary by state. Once three seizure-free years have passed after a patient’s initial seizure, the chance of a recurrence falls to around 10% to 20%.6-7
Back to the Case
Our 42-year-old patient with a first seizure had normal findings on examination, laboratory studies, and brain imaging. An EEG showed epileptiform discharges in a spike and wave pattern. The attending hospitalist counseled him on his elevated risk of future seizures; the patient then elected to begin AED therapy, citing a fear of losing his driving privileges. Levetiracetam was started, which he tolerated despite mild sedation.
A year later, he suffered another seizure at his home. With regular followup and titration of his AED, he remained seizure-free for the next five years.
Bottom Line
Most patients with a single unprovoked seizure can be managed with watchful waiting, counseling, and neurological followup. Initiation of AED therapy is appropriate for patients with a high risk of seizure recurrence, or for whom another seizure could pose personal or social harm. TH
Dr. Hoffman is a hospitalist at Emory University School of Medicine in Atlanta.
References
- French JA, Pedley TA. Clinical practice: Initial management of epilepsy. N Engl J Med. 2008;359:166-176.
- Krumholz A, Wiebe S, Gronseth G, et al. Practice Parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007;69:1996-2007.
- Schachter SC. Antiepileptic drug therapy: general treatment principles and application for special patient populations. Epilepsia. 1999;40(9):S20-25.
- Hauser WA, Rich SS, Annegers JF, et al. Seizure recurrence after a first unprovoked seizure: an extended follow-up. Neurology. 1990;40:1163-1170.
- Marson A, Jacoby A, Johnson A, et al. Immediate versus deferred antiepileptic drug treatment for epilepsy and single seizures: a randomized controlled trial. Lancet. 2005;365: 2007-2013.
- Hauser WA, Rich SS, Lee JR, Annegers JF, Anderson VE. Risk of recurrent seizures after two unprovoked seizures. N Engl J Med. 1998;338:429-434.
- Berg AT. Risk of recurrence after a first unprovoked seizure. Epilepsia. 2008;49:S13-18.
- Kim LG, Johnson TL, Marson AG, et al. Prediction of risk of seizure recurrence after a single seizure and early epilepsy: further results from the MESS trial. Lancet Neurology. 2006;5(4):317-322.