User login
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
Focused Practice in Hospital Medicine Track Helps Hospitalists Achieve ABIM Recertification
This is the year I complete my second recertification for the American Board of Internal Medicine (ABIM). Prior to 1990, the ABIM issued certificates that were good for life. Beginning in 1990 and through 2013, all certificates were issued for a 10-year duration. All those prior lifetime certificates were honored, so those holding them were deemed “grandfathered” and have not had to recertify. The rest of us are now on the recertification pathway, renewing every 10 years. Although the date has been set at 10 years, the recertification process has become more regimented since January 2014, when the ABIM moved to a continuous program requiring evidence of new learning and maintenance of quality in your practice every two years.
This ratcheting up of requirements and adding increased increments of progress hasn’t come without controversy. Last year a petition was started and signed by 19,000 physicians protesting the changes and arguing the ABIM should go back to the methodology of taking a test every 10 years. Even this was a moderate position; many were clamoring for the abolition of maintenance of certification (MOC) all together.
I represented the Society of Hospital Medicine (SHM) in July 2014 at a summit in Philadelphia called by the ABIM Foundation. Each of the medical subspecialties was given an opportunity to speak to the ABIM leadership and the audience of fellow representatives about the impact of MOC. As members of a relatively youthful field, hospitalists are less focused on how the “grandfathers” are being treated and more concerned about the confusing process and lack of opportunity to incorporate our daily hospitalist-focused work effort easily into the process.
As a result of that petition, many letters written to the board, and the outspoken representatives at the ABIM summit, the ABIM has responded with a plan to make elements of the process more friendly and open, as well as one to further plan and adapt.
Clearly, this is a process in evolution. Hospitalists are committed to lifelong learning. I think we can expect that with more transparency in all aspects of our lives, personal and professional, our patients, our hospitals, and payers…will all be expecting to see just exactly how committed we are to lifelong learning and self-improvement.
It’s our turn…
In 2009, some bold steps were taken with the announcement of the new Focused Practice in Hospital Medicine (FPHM) that, hopefully, will impact hospitalists for many years to come. SHM’s partnership with the ABIM began with work five years prior, creating a focused declaration of hospital medicine competence. Initially, this was set up as a pilot project to be evaluated for success along the way, to see if the concept would become permanent. The work was announced, and the inaugural class of 175 physicians entered the process. Since that time, 555 physicians have earned the FPHM certificate. What’s even more impressive is that we have seen a surge recently in the number of entrants. There are now 3,300 hospitalists enrolled in the pathway.
While this growth is great, we estimate that there are 44,000 hospitalists in the U.S. We know that many are newer hospitalists and not yet up for recertification. Our goal is to get every hospitalist entering the pathway when it is his or her time, just like I’m doing now. It is my time!
As we steadily progress in distinguishing and defining our field, we need as many hospitalists as possible to raise their hands and say that they proudly practice hospital medicine and have taken the steps to learn the special knowledge and gain the special skills needed to succeed in the hospital. The ABIM certification program is still in the pilot phase. One of the key markers of success to determine if it will be continued is the number of participants. I am writing this column as another way to encourage us all to stand up and be counted.
Practical Tips
So, we know things have changed, and we know things will be changing more, but what about now? What do we need to do to navigate the process to gain our FPHM certificate today?
1. Enter the process: You can’t win if you don’t play. Entering FPHM is easier than ever. The requirement for current active ACLS has been removed. Now it is a declaration that you see 1,000 patients a year or that you had 3,000 encounters in the last three years and pay the supplemental fee.
2. Earn 100 “points”: You have five years, with a mix of Part II and Part IV activities at least every two years, and the secure exam. You must have the patient voice and patient safety module credit as part of this every five years block.
2a. Medical Knowledge Self-Assessment (Part II): Show what you know or learn on an ongoing basis. You can do these at home, work, or with a buddy, or, even better, sign up for a group learning session, usually offered as a pre-course at society meetings. HM15 will be offering a pre-course that will offer Part II credit. SHM’s Hospital QI and Patient Safety Medical Knowledge Module is available at www.shmlearningportal.org.
2b. Practice Improvement (Part IV): Show that you are trying to improve your practice. Again, the ABIM website lists many possibilities for improvement activities that count and has a practice improvement module (PIM) selector tool (select “hospital medicine” and “inpatient”). Here are some of my favorite PIMs.
Team PIM. Complete a self-assessment of your team skills, get 10 members of your hospital multidisciplinary team to fill out an evaluation on you, and then review with a trusted colleague. This PIM also satisfies both patient voice and patient safety requirements (10 points).
SHM Project BOOST or SHM’s Glycemic Control Mentored Implementation Program. Do either of these at your hospital to earn 20 points.
Clinical Supervisor PIM. For those of you who work with residents or students. Observe 10 visits by learners, then follow up with a chart look-back, feedback to the learner, and a plan for improving learning (20 points).
3. Take a test! The secure exam is given every 10 years and counts for 20 points. What is great about this FPHM test is that it is focused on all the stuff you do every day in your job. It’s a hospitalist test, not an outpatient clinic doctor test. It focuses on inpatient clinical medicine and palliative care, plus patient safety and quality. You can use the current study materials (MedStudy, MKSAP [Medical Knowledge Self-Assessment Program], and the like); just skip the purely ambulatory material. Focused study materials will be available in the next year. Look for the HM15 exam preparation guide, which will direct you to HM15 sessions that cross over with the ABIM/ABFM [American Board of Family Medicine] Hospital Medicine exam.
If you would like other tools for studying for the consultative co-management and quality and patient safety sections of the exam, check out SHM Learning Portal.
Final Thoughts
It’s complicated, right? But each time I look at it or read one of these articles, it gets a bit simpler. The overall process for internal medicine certification now mirrors this one, with very few differences. Remember, the ABFM process is identical for hospitalists trained in family medicine. Hopefully, this column will help you get off the fence and come down on the side of representing what you do every day at work in the hospital.
Be proud, take the more pertinent path, be a hospitalist! Twenty points.

This is the year I complete my second recertification for the American Board of Internal Medicine (ABIM). Prior to 1990, the ABIM issued certificates that were good for life. Beginning in 1990 and through 2013, all certificates were issued for a 10-year duration. All those prior lifetime certificates were honored, so those holding them were deemed “grandfathered” and have not had to recertify. The rest of us are now on the recertification pathway, renewing every 10 years. Although the date has been set at 10 years, the recertification process has become more regimented since January 2014, when the ABIM moved to a continuous program requiring evidence of new learning and maintenance of quality in your practice every two years.
This ratcheting up of requirements and adding increased increments of progress hasn’t come without controversy. Last year a petition was started and signed by 19,000 physicians protesting the changes and arguing the ABIM should go back to the methodology of taking a test every 10 years. Even this was a moderate position; many were clamoring for the abolition of maintenance of certification (MOC) all together.
I represented the Society of Hospital Medicine (SHM) in July 2014 at a summit in Philadelphia called by the ABIM Foundation. Each of the medical subspecialties was given an opportunity to speak to the ABIM leadership and the audience of fellow representatives about the impact of MOC. As members of a relatively youthful field, hospitalists are less focused on how the “grandfathers” are being treated and more concerned about the confusing process and lack of opportunity to incorporate our daily hospitalist-focused work effort easily into the process.
As a result of that petition, many letters written to the board, and the outspoken representatives at the ABIM summit, the ABIM has responded with a plan to make elements of the process more friendly and open, as well as one to further plan and adapt.
Clearly, this is a process in evolution. Hospitalists are committed to lifelong learning. I think we can expect that with more transparency in all aspects of our lives, personal and professional, our patients, our hospitals, and payers…will all be expecting to see just exactly how committed we are to lifelong learning and self-improvement.
It’s our turn…
In 2009, some bold steps were taken with the announcement of the new Focused Practice in Hospital Medicine (FPHM) that, hopefully, will impact hospitalists for many years to come. SHM’s partnership with the ABIM began with work five years prior, creating a focused declaration of hospital medicine competence. Initially, this was set up as a pilot project to be evaluated for success along the way, to see if the concept would become permanent. The work was announced, and the inaugural class of 175 physicians entered the process. Since that time, 555 physicians have earned the FPHM certificate. What’s even more impressive is that we have seen a surge recently in the number of entrants. There are now 3,300 hospitalists enrolled in the pathway.
While this growth is great, we estimate that there are 44,000 hospitalists in the U.S. We know that many are newer hospitalists and not yet up for recertification. Our goal is to get every hospitalist entering the pathway when it is his or her time, just like I’m doing now. It is my time!
As we steadily progress in distinguishing and defining our field, we need as many hospitalists as possible to raise their hands and say that they proudly practice hospital medicine and have taken the steps to learn the special knowledge and gain the special skills needed to succeed in the hospital. The ABIM certification program is still in the pilot phase. One of the key markers of success to determine if it will be continued is the number of participants. I am writing this column as another way to encourage us all to stand up and be counted.
Practical Tips
So, we know things have changed, and we know things will be changing more, but what about now? What do we need to do to navigate the process to gain our FPHM certificate today?
1. Enter the process: You can’t win if you don’t play. Entering FPHM is easier than ever. The requirement for current active ACLS has been removed. Now it is a declaration that you see 1,000 patients a year or that you had 3,000 encounters in the last three years and pay the supplemental fee.
2. Earn 100 “points”: You have five years, with a mix of Part II and Part IV activities at least every two years, and the secure exam. You must have the patient voice and patient safety module credit as part of this every five years block.
2a. Medical Knowledge Self-Assessment (Part II): Show what you know or learn on an ongoing basis. You can do these at home, work, or with a buddy, or, even better, sign up for a group learning session, usually offered as a pre-course at society meetings. HM15 will be offering a pre-course that will offer Part II credit. SHM’s Hospital QI and Patient Safety Medical Knowledge Module is available at www.shmlearningportal.org.
2b. Practice Improvement (Part IV): Show that you are trying to improve your practice. Again, the ABIM website lists many possibilities for improvement activities that count and has a practice improvement module (PIM) selector tool (select “hospital medicine” and “inpatient”). Here are some of my favorite PIMs.
Team PIM. Complete a self-assessment of your team skills, get 10 members of your hospital multidisciplinary team to fill out an evaluation on you, and then review with a trusted colleague. This PIM also satisfies both patient voice and patient safety requirements (10 points).
SHM Project BOOST or SHM’s Glycemic Control Mentored Implementation Program. Do either of these at your hospital to earn 20 points.
Clinical Supervisor PIM. For those of you who work with residents or students. Observe 10 visits by learners, then follow up with a chart look-back, feedback to the learner, and a plan for improving learning (20 points).
3. Take a test! The secure exam is given every 10 years and counts for 20 points. What is great about this FPHM test is that it is focused on all the stuff you do every day in your job. It’s a hospitalist test, not an outpatient clinic doctor test. It focuses on inpatient clinical medicine and palliative care, plus patient safety and quality. You can use the current study materials (MedStudy, MKSAP [Medical Knowledge Self-Assessment Program], and the like); just skip the purely ambulatory material. Focused study materials will be available in the next year. Look for the HM15 exam preparation guide, which will direct you to HM15 sessions that cross over with the ABIM/ABFM [American Board of Family Medicine] Hospital Medicine exam.
If you would like other tools for studying for the consultative co-management and quality and patient safety sections of the exam, check out SHM Learning Portal.
Final Thoughts
It’s complicated, right? But each time I look at it or read one of these articles, it gets a bit simpler. The overall process for internal medicine certification now mirrors this one, with very few differences. Remember, the ABFM process is identical for hospitalists trained in family medicine. Hopefully, this column will help you get off the fence and come down on the side of representing what you do every day at work in the hospital.
Be proud, take the more pertinent path, be a hospitalist! Twenty points.

This is the year I complete my second recertification for the American Board of Internal Medicine (ABIM). Prior to 1990, the ABIM issued certificates that were good for life. Beginning in 1990 and through 2013, all certificates were issued for a 10-year duration. All those prior lifetime certificates were honored, so those holding them were deemed “grandfathered” and have not had to recertify. The rest of us are now on the recertification pathway, renewing every 10 years. Although the date has been set at 10 years, the recertification process has become more regimented since January 2014, when the ABIM moved to a continuous program requiring evidence of new learning and maintenance of quality in your practice every two years.
This ratcheting up of requirements and adding increased increments of progress hasn’t come without controversy. Last year a petition was started and signed by 19,000 physicians protesting the changes and arguing the ABIM should go back to the methodology of taking a test every 10 years. Even this was a moderate position; many were clamoring for the abolition of maintenance of certification (MOC) all together.
I represented the Society of Hospital Medicine (SHM) in July 2014 at a summit in Philadelphia called by the ABIM Foundation. Each of the medical subspecialties was given an opportunity to speak to the ABIM leadership and the audience of fellow representatives about the impact of MOC. As members of a relatively youthful field, hospitalists are less focused on how the “grandfathers” are being treated and more concerned about the confusing process and lack of opportunity to incorporate our daily hospitalist-focused work effort easily into the process.
As a result of that petition, many letters written to the board, and the outspoken representatives at the ABIM summit, the ABIM has responded with a plan to make elements of the process more friendly and open, as well as one to further plan and adapt.
Clearly, this is a process in evolution. Hospitalists are committed to lifelong learning. I think we can expect that with more transparency in all aspects of our lives, personal and professional, our patients, our hospitals, and payers…will all be expecting to see just exactly how committed we are to lifelong learning and self-improvement.
It’s our turn…
In 2009, some bold steps were taken with the announcement of the new Focused Practice in Hospital Medicine (FPHM) that, hopefully, will impact hospitalists for many years to come. SHM’s partnership with the ABIM began with work five years prior, creating a focused declaration of hospital medicine competence. Initially, this was set up as a pilot project to be evaluated for success along the way, to see if the concept would become permanent. The work was announced, and the inaugural class of 175 physicians entered the process. Since that time, 555 physicians have earned the FPHM certificate. What’s even more impressive is that we have seen a surge recently in the number of entrants. There are now 3,300 hospitalists enrolled in the pathway.
While this growth is great, we estimate that there are 44,000 hospitalists in the U.S. We know that many are newer hospitalists and not yet up for recertification. Our goal is to get every hospitalist entering the pathway when it is his or her time, just like I’m doing now. It is my time!
As we steadily progress in distinguishing and defining our field, we need as many hospitalists as possible to raise their hands and say that they proudly practice hospital medicine and have taken the steps to learn the special knowledge and gain the special skills needed to succeed in the hospital. The ABIM certification program is still in the pilot phase. One of the key markers of success to determine if it will be continued is the number of participants. I am writing this column as another way to encourage us all to stand up and be counted.
Practical Tips
So, we know things have changed, and we know things will be changing more, but what about now? What do we need to do to navigate the process to gain our FPHM certificate today?
1. Enter the process: You can’t win if you don’t play. Entering FPHM is easier than ever. The requirement for current active ACLS has been removed. Now it is a declaration that you see 1,000 patients a year or that you had 3,000 encounters in the last three years and pay the supplemental fee.
2. Earn 100 “points”: You have five years, with a mix of Part II and Part IV activities at least every two years, and the secure exam. You must have the patient voice and patient safety module credit as part of this every five years block.
2a. Medical Knowledge Self-Assessment (Part II): Show what you know or learn on an ongoing basis. You can do these at home, work, or with a buddy, or, even better, sign up for a group learning session, usually offered as a pre-course at society meetings. HM15 will be offering a pre-course that will offer Part II credit. SHM’s Hospital QI and Patient Safety Medical Knowledge Module is available at www.shmlearningportal.org.
2b. Practice Improvement (Part IV): Show that you are trying to improve your practice. Again, the ABIM website lists many possibilities for improvement activities that count and has a practice improvement module (PIM) selector tool (select “hospital medicine” and “inpatient”). Here are some of my favorite PIMs.
Team PIM. Complete a self-assessment of your team skills, get 10 members of your hospital multidisciplinary team to fill out an evaluation on you, and then review with a trusted colleague. This PIM also satisfies both patient voice and patient safety requirements (10 points).
SHM Project BOOST or SHM’s Glycemic Control Mentored Implementation Program. Do either of these at your hospital to earn 20 points.
Clinical Supervisor PIM. For those of you who work with residents or students. Observe 10 visits by learners, then follow up with a chart look-back, feedback to the learner, and a plan for improving learning (20 points).
3. Take a test! The secure exam is given every 10 years and counts for 20 points. What is great about this FPHM test is that it is focused on all the stuff you do every day in your job. It’s a hospitalist test, not an outpatient clinic doctor test. It focuses on inpatient clinical medicine and palliative care, plus patient safety and quality. You can use the current study materials (MedStudy, MKSAP [Medical Knowledge Self-Assessment Program], and the like); just skip the purely ambulatory material. Focused study materials will be available in the next year. Look for the HM15 exam preparation guide, which will direct you to HM15 sessions that cross over with the ABIM/ABFM [American Board of Family Medicine] Hospital Medicine exam.
If you would like other tools for studying for the consultative co-management and quality and patient safety sections of the exam, check out SHM Learning Portal.
Final Thoughts
It’s complicated, right? But each time I look at it or read one of these articles, it gets a bit simpler. The overall process for internal medicine certification now mirrors this one, with very few differences. Remember, the ABFM process is identical for hospitalists trained in family medicine. Hopefully, this column will help you get off the fence and come down on the side of representing what you do every day at work in the hospital.
Be proud, take the more pertinent path, be a hospitalist! Twenty points.

Cut Costs, Improve Quality and Patient Experience
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
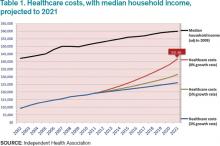
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
“Now that’s a fire!”
—Eddie Murphy
This is the final column in my five-part series tracing the history of the hospitalist movement and the factors that propelled it into becoming the fastest growing medical specialty in history and the mainstay of American medicine that it has become.
In the first column, “Tinder & Spark,” economic forces of the early 1990s pushed Baby Boomer physicians into creative ways of working in the hospital; a seminal article in the most famous journal in the world then sparked a revolution. In part two, “Fuel,” Generation X physicians aligned with the values of the HM movement and joined the field in record numbers. In part three, “Oxygen,” I explained how the patient safety and quality movement propelled hospitalist growth, through both inspiration and funding, to new heights throughout the late 90s and early 2000s. And in the October 2014 issue, I continued my journey through the first 20 years of hospital medicine as a field with the fourth installment, “Heat,” a focus on the rise in importance of patient experience and the Millennial generation’s arrival in our hospitalist workforce.
That brings us to the present and back to a factor that started our rise and is becoming more important than ever, both for us as a specialty and for our success as a country.
The Affordability Crisis
We have known for a long time how expensive healthcare is. If it wasn’t for managed care trying to control costs in the 80s and 90s, hospitalists might very well not even exist. But now, it isn’t just costly. It is unaffordable for the average family.
Table 1 shows projected healthcare costs and growth curves through 2021, with a median four-person household income overlaid.
In most scenarios, the two lines, income and healthcare costs, continue to get closer and closer—with healthcare costs almost $42,000 per family by 2021 in the most aggressive projection (8% growth). I am sure many of you have heard the phrase “bending the curve.” That simply means to try and bend that red line down to something approximating the blue line. It is slowing the growth, not actually decreasing the cost.
But it’s a step.
Only at that slowest healthcare growth rate projection (3%) does household income maintain pace. At the highest projection, two-thirds of family income will go toward healthcare. It simply won’t work. Affordability must be addressed.
Hospitalists are at the center of this storm. If you look at the various factors contributing to costs, we (and our keyboards) have great control and influence over inpatient, professional services, and pharmacy costs. To our credit, and to the credit of our teammates in the hospital, we actually seem to be bending the curve down toward the 5% range in inpatient care and professional services. Nevertheless, even at that level it is outpacing income growth.
In 2013, total healthcare costs for a family of four finally caught up with college costs. It is now just north of $22,000 per year for both healthcare costs and the annual cost of attending an in-state public college. Let’s not catch the private colleges as the biggest family budget buster.
The Triple Aim
So, over the course of five articles, I have talked about how we as hospitalists have faced and learned about key aspects of delivering care in a modern healthcare system. First, it was economics, then patient safety and quality, then patient experience, and now we’re back to economics as we consider patient affordability.
Wouldn’t it be great just to focus on one thing at a time? Unfortunately, life doesn’t work that way. In today’s world, hospitalists must give the best quality care while giving a great experience to their patients, all at an affordable cost. This concept of triple focus has given rise to a new term, “Triple Aim.”
The Institute for Healthcare Improvement (IHI) developed the phrase—and the idea—in 2006. It symbolizes an understanding that all three areas of quality MUST be joined together to achieve true success for our patients. As physicians and hospitalists, we have been taught to focus on health as the cornerstone of our profession. We know about cost pressures, and we now appreciate how important patient experience is. The problem has been that we tend to bounce back and forth in addressing these, silo to silo, depending on the circumstance—JCAHO [Joint Council on Accreditation of Healthcare Organizations] visit, publication of CMS core measures, Press-Ganey scores.
Payers and public data sites already have moved away from just reporting health measures. Experience is nearly as prominent in the discussion now. Affordability measures and transparent pricing are on the verge, especially as we arrive in a world with value-based purchasing and cost bundling.
It is easy to focus on just the crisis of the moment. Today, that might very well be the affordability crisis, but it’s important to understand that when delivering healthcare to real live human beings, with all their complexities and vulnerabilities, we have to tune in to our most creative selves to come up with solutions that don’t just address individual areas of care but that also integrate and synergize.
Into the Future
So why this long, five-column preamble into our history, our grand social movement? Because our society and specialty, even with almost 20 years under our belts, are still in the early days. Our members know this and stay connected and coordinated, either in person, at our annual meeting, or virtually using HMX, to better face the many challenges today and those coming down the road. When SHM surveyed its members last year about why they had attended the annual meeting, the overwhelming response was to “be part of the hospital medicine movement.”
Our specialty started out as a group of one-offs and experiments and then coalesced into a social movement, and although it has changed directions and gathered new areas of focus, we are charging ahead. Much social, cultural, and medical change is to come. It’s why our members have told us they keep coming back—to share in this great and glorious social movement called hospital medicine.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
Focus on Patient Experience Strengthens Hospital Medicine Movement
“People don’t always remember what you say or even what you do, but they always remember how you made them feel.”—Maya Angelou
When SHM surveyed its members last year about why they had attended the annual meeting, the single most common response was to “be part of the hospital medicine movement.”
In the first three of my presidential columns, I talked about what that meant for the first 15 years of our specialty. HM’s rise occurred in the mid 1990s, during a time of despair in medicine, when pressures from rising costs and the new managed care industry upended the usual way of doing things, and then, around the turn of the century, amid a growing awareness that the care we had been delivering was wildly variable in quality—and often unsafe. Our field, created by members of the Baby Boomer generation, ultimately proved highly attractive to Generation X’ers, and our growth was accelerated by this new supply of young doctors. Fueled by the influx of dollars and attention brought on by the patient safety and quality movement, HM became the fastest growing medical specialty in history.
So, now we know what being part of the hospitalist movement meant before, but what does it mean today? Are the issues and drivers the same? I left my last column in 2006, with the partnership between the Institute for Healthcare Improvement (IHI), SHM, and six other key organizations to create the 5 Million Lives Campaign. It was an important year in several other ways, as what it meant to be a hospitalist began to change.
Enter the Millenials
In 2006 a new generation, the Millenials, born between 1985 and 2000, began entering medical schools across the country. This group, raised on a diet of positive reinforcement and cooperation, is characterized by confidence and a desire to work in teams. Born after the introduction of the Macintosh computer, Millenials are not just tech savvy; they have grown up in the world of social media and are digital media savvy. Even more than Gen X, Millenials strive for work-life balance. It almost seems this was a generation born and raised to be hospitalists!
Not only is their life philosophy different than the Boomers and X’ers before them, but their medical training has been unlike any before. From the moment they entered medical school, they were taught about patient quality and safety. To them, doctors aren’t the isolated pillars of strength and sole possessors of sacred knowledge that they used to be. They intuitively get that medicine is a team sport. In fact, most of the attendings on their ward rotations have been hospitalists.
Rise of Experience
In the early days of medicine, we as physicians understood that patients might not have the best experience, but that was just part of the deal, right? It’s just not supposed to be fun to be hospitalized—and sometimes you had to go through hell to get better. Those were the days of pure, unadulterated paternalism. We did things to patients to make them get better.
In the late 1970s, Irwin Press, PhD, began to study and lecture on patient satisfaction. In 1985, he joined forces with statistician Rod Ganey, PhD, to found Press Ganey Inc.1 Patient experience as a concept began to enter the conversation of hospital administration, especially around the one-dimensional idea that better experience could contribute to the better financial health of an organization.
During the rise of the patient safety and quality movement in the late 1990s and early 2000s, our zeal to improve care led us to begin doing many things for patients. But a collateral idea began to rise in importance, too—the idea that a patient’s experience was critical to improving quality, not just a tool to attract more patients.
The entire national quality infrastructure I described in my last column (CMS, JCAHO, AHRQ, NQF) began to work on adding experience to the suite of measurements being developed. In 2006, CMS introduced the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey. This was a set of questions designed to be used at all hospitals nationwide, a significant development, because there was now a national standard for patient experience that could be compared over time and across hospitals anywhere in the country.2
In 2007, all hospitals subject to the Inpatient Prospective Payment System—pretty much all hospitals except critical access hospitals—were required to submit their HCAHPS survey data or face up to a 2% penalty. In 2008, this experience data was released publicly for the first time.2
And, of course, the Patient Protection and Affordable Care Act of 2010 (ACA) included HCAHPS results in calculating Hospital Value-Based Purchasing payments.3
The Institute of Medicine, in laying out a vision for better healthcare in 2012, called for more involvement of patients and families.
We are even seeing organizations creating leadership positions solely focused on patient experience. The Cleveland Clinic created the first physician leadership position dedicated to patient experience in the country, appointing Bridget Duffy, MD, a hospitalist, as its first chief experience officer in 2010. In 2012, Sound Physicians became the first hospitalist company to create such a position, to which it appointed Mark Rudolph, MD. Who would have imagined this 10 years ago?
Life for hospitalists has changed dramatically from the early 1990s to the Millenials now entering our workforce. The forces guiding our work and stimulating our growth have evolved, but the overarching theme of the last twenty years has been improvement. When the medical world took a cold hard look at the care being delivered, we suddenly saw a world of opportunities for improvement.
I talked before about how the rise of the patient safety and quality movement coincided perfectly with the emergence of hospitalists. Here I told you about how patient experience emerged in prominence as we, collectively, in becoming aware of our quality deficits, gained newfound empathy for what patients were going through. This focus on patient experience again plays into our strength and the opportunity we have as a specialty.
In the December issue of The Hospitalist, the final column in this five-part series will examine how to put it all together as we move toward the future of the field. But first I’ll introduce one last factor, a problem that helped launch our field and is now the greatest threat to our success.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Press Ganey Associates, Inc. A spark ignited nearly three decades ago. Available at: http://www.pressganey.com/aboutUs/ourHistory.aspx. Accessed August 31, 2014.
- Centers for Medicare and Medicaid Services. HCAHPS Fact Sheet. Available at: www.hcahpsonline.org. Accessed August 31, 2014.
- American Hospital Association. Inpatient PPS. Available at: http://www.aha.org/advocacy-issues/medicare/ipps/index.shtml. Accessed August 31, 2014.
“People don’t always remember what you say or even what you do, but they always remember how you made them feel.”—Maya Angelou
When SHM surveyed its members last year about why they had attended the annual meeting, the single most common response was to “be part of the hospital medicine movement.”
In the first three of my presidential columns, I talked about what that meant for the first 15 years of our specialty. HM’s rise occurred in the mid 1990s, during a time of despair in medicine, when pressures from rising costs and the new managed care industry upended the usual way of doing things, and then, around the turn of the century, amid a growing awareness that the care we had been delivering was wildly variable in quality—and often unsafe. Our field, created by members of the Baby Boomer generation, ultimately proved highly attractive to Generation X’ers, and our growth was accelerated by this new supply of young doctors. Fueled by the influx of dollars and attention brought on by the patient safety and quality movement, HM became the fastest growing medical specialty in history.
So, now we know what being part of the hospitalist movement meant before, but what does it mean today? Are the issues and drivers the same? I left my last column in 2006, with the partnership between the Institute for Healthcare Improvement (IHI), SHM, and six other key organizations to create the 5 Million Lives Campaign. It was an important year in several other ways, as what it meant to be a hospitalist began to change.
Enter the Millenials
In 2006 a new generation, the Millenials, born between 1985 and 2000, began entering medical schools across the country. This group, raised on a diet of positive reinforcement and cooperation, is characterized by confidence and a desire to work in teams. Born after the introduction of the Macintosh computer, Millenials are not just tech savvy; they have grown up in the world of social media and are digital media savvy. Even more than Gen X, Millenials strive for work-life balance. It almost seems this was a generation born and raised to be hospitalists!
Not only is their life philosophy different than the Boomers and X’ers before them, but their medical training has been unlike any before. From the moment they entered medical school, they were taught about patient quality and safety. To them, doctors aren’t the isolated pillars of strength and sole possessors of sacred knowledge that they used to be. They intuitively get that medicine is a team sport. In fact, most of the attendings on their ward rotations have been hospitalists.
Rise of Experience
In the early days of medicine, we as physicians understood that patients might not have the best experience, but that was just part of the deal, right? It’s just not supposed to be fun to be hospitalized—and sometimes you had to go through hell to get better. Those were the days of pure, unadulterated paternalism. We did things to patients to make them get better.
In the late 1970s, Irwin Press, PhD, began to study and lecture on patient satisfaction. In 1985, he joined forces with statistician Rod Ganey, PhD, to found Press Ganey Inc.1 Patient experience as a concept began to enter the conversation of hospital administration, especially around the one-dimensional idea that better experience could contribute to the better financial health of an organization.
During the rise of the patient safety and quality movement in the late 1990s and early 2000s, our zeal to improve care led us to begin doing many things for patients. But a collateral idea began to rise in importance, too—the idea that a patient’s experience was critical to improving quality, not just a tool to attract more patients.
The entire national quality infrastructure I described in my last column (CMS, JCAHO, AHRQ, NQF) began to work on adding experience to the suite of measurements being developed. In 2006, CMS introduced the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey. This was a set of questions designed to be used at all hospitals nationwide, a significant development, because there was now a national standard for patient experience that could be compared over time and across hospitals anywhere in the country.2
In 2007, all hospitals subject to the Inpatient Prospective Payment System—pretty much all hospitals except critical access hospitals—were required to submit their HCAHPS survey data or face up to a 2% penalty. In 2008, this experience data was released publicly for the first time.2
And, of course, the Patient Protection and Affordable Care Act of 2010 (ACA) included HCAHPS results in calculating Hospital Value-Based Purchasing payments.3
The Institute of Medicine, in laying out a vision for better healthcare in 2012, called for more involvement of patients and families.
We are even seeing organizations creating leadership positions solely focused on patient experience. The Cleveland Clinic created the first physician leadership position dedicated to patient experience in the country, appointing Bridget Duffy, MD, a hospitalist, as its first chief experience officer in 2010. In 2012, Sound Physicians became the first hospitalist company to create such a position, to which it appointed Mark Rudolph, MD. Who would have imagined this 10 years ago?
Life for hospitalists has changed dramatically from the early 1990s to the Millenials now entering our workforce. The forces guiding our work and stimulating our growth have evolved, but the overarching theme of the last twenty years has been improvement. When the medical world took a cold hard look at the care being delivered, we suddenly saw a world of opportunities for improvement.
I talked before about how the rise of the patient safety and quality movement coincided perfectly with the emergence of hospitalists. Here I told you about how patient experience emerged in prominence as we, collectively, in becoming aware of our quality deficits, gained newfound empathy for what patients were going through. This focus on patient experience again plays into our strength and the opportunity we have as a specialty.
In the December issue of The Hospitalist, the final column in this five-part series will examine how to put it all together as we move toward the future of the field. But first I’ll introduce one last factor, a problem that helped launch our field and is now the greatest threat to our success.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Press Ganey Associates, Inc. A spark ignited nearly three decades ago. Available at: http://www.pressganey.com/aboutUs/ourHistory.aspx. Accessed August 31, 2014.
- Centers for Medicare and Medicaid Services. HCAHPS Fact Sheet. Available at: www.hcahpsonline.org. Accessed August 31, 2014.
- American Hospital Association. Inpatient PPS. Available at: http://www.aha.org/advocacy-issues/medicare/ipps/index.shtml. Accessed August 31, 2014.
“People don’t always remember what you say or even what you do, but they always remember how you made them feel.”—Maya Angelou
When SHM surveyed its members last year about why they had attended the annual meeting, the single most common response was to “be part of the hospital medicine movement.”
In the first three of my presidential columns, I talked about what that meant for the first 15 years of our specialty. HM’s rise occurred in the mid 1990s, during a time of despair in medicine, when pressures from rising costs and the new managed care industry upended the usual way of doing things, and then, around the turn of the century, amid a growing awareness that the care we had been delivering was wildly variable in quality—and often unsafe. Our field, created by members of the Baby Boomer generation, ultimately proved highly attractive to Generation X’ers, and our growth was accelerated by this new supply of young doctors. Fueled by the influx of dollars and attention brought on by the patient safety and quality movement, HM became the fastest growing medical specialty in history.
So, now we know what being part of the hospitalist movement meant before, but what does it mean today? Are the issues and drivers the same? I left my last column in 2006, with the partnership between the Institute for Healthcare Improvement (IHI), SHM, and six other key organizations to create the 5 Million Lives Campaign. It was an important year in several other ways, as what it meant to be a hospitalist began to change.
Enter the Millenials
In 2006 a new generation, the Millenials, born between 1985 and 2000, began entering medical schools across the country. This group, raised on a diet of positive reinforcement and cooperation, is characterized by confidence and a desire to work in teams. Born after the introduction of the Macintosh computer, Millenials are not just tech savvy; they have grown up in the world of social media and are digital media savvy. Even more than Gen X, Millenials strive for work-life balance. It almost seems this was a generation born and raised to be hospitalists!
Not only is their life philosophy different than the Boomers and X’ers before them, but their medical training has been unlike any before. From the moment they entered medical school, they were taught about patient quality and safety. To them, doctors aren’t the isolated pillars of strength and sole possessors of sacred knowledge that they used to be. They intuitively get that medicine is a team sport. In fact, most of the attendings on their ward rotations have been hospitalists.
Rise of Experience
In the early days of medicine, we as physicians understood that patients might not have the best experience, but that was just part of the deal, right? It’s just not supposed to be fun to be hospitalized—and sometimes you had to go through hell to get better. Those were the days of pure, unadulterated paternalism. We did things to patients to make them get better.
In the late 1970s, Irwin Press, PhD, began to study and lecture on patient satisfaction. In 1985, he joined forces with statistician Rod Ganey, PhD, to found Press Ganey Inc.1 Patient experience as a concept began to enter the conversation of hospital administration, especially around the one-dimensional idea that better experience could contribute to the better financial health of an organization.
During the rise of the patient safety and quality movement in the late 1990s and early 2000s, our zeal to improve care led us to begin doing many things for patients. But a collateral idea began to rise in importance, too—the idea that a patient’s experience was critical to improving quality, not just a tool to attract more patients.
The entire national quality infrastructure I described in my last column (CMS, JCAHO, AHRQ, NQF) began to work on adding experience to the suite of measurements being developed. In 2006, CMS introduced the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey. This was a set of questions designed to be used at all hospitals nationwide, a significant development, because there was now a national standard for patient experience that could be compared over time and across hospitals anywhere in the country.2
In 2007, all hospitals subject to the Inpatient Prospective Payment System—pretty much all hospitals except critical access hospitals—were required to submit their HCAHPS survey data or face up to a 2% penalty. In 2008, this experience data was released publicly for the first time.2
And, of course, the Patient Protection and Affordable Care Act of 2010 (ACA) included HCAHPS results in calculating Hospital Value-Based Purchasing payments.3
The Institute of Medicine, in laying out a vision for better healthcare in 2012, called for more involvement of patients and families.
We are even seeing organizations creating leadership positions solely focused on patient experience. The Cleveland Clinic created the first physician leadership position dedicated to patient experience in the country, appointing Bridget Duffy, MD, a hospitalist, as its first chief experience officer in 2010. In 2012, Sound Physicians became the first hospitalist company to create such a position, to which it appointed Mark Rudolph, MD. Who would have imagined this 10 years ago?
Life for hospitalists has changed dramatically from the early 1990s to the Millenials now entering our workforce. The forces guiding our work and stimulating our growth have evolved, but the overarching theme of the last twenty years has been improvement. When the medical world took a cold hard look at the care being delivered, we suddenly saw a world of opportunities for improvement.
I talked before about how the rise of the patient safety and quality movement coincided perfectly with the emergence of hospitalists. Here I told you about how patient experience emerged in prominence as we, collectively, in becoming aware of our quality deficits, gained newfound empathy for what patients were going through. This focus on patient experience again plays into our strength and the opportunity we have as a specialty.
In the December issue of The Hospitalist, the final column in this five-part series will examine how to put it all together as we move toward the future of the field. But first I’ll introduce one last factor, a problem that helped launch our field and is now the greatest threat to our success.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Press Ganey Associates, Inc. A spark ignited nearly three decades ago. Available at: http://www.pressganey.com/aboutUs/ourHistory.aspx. Accessed August 31, 2014.
- Centers for Medicare and Medicaid Services. HCAHPS Fact Sheet. Available at: www.hcahpsonline.org. Accessed August 31, 2014.
- American Hospital Association. Inpatient PPS. Available at: http://www.aha.org/advocacy-issues/medicare/ipps/index.shtml. Accessed August 31, 2014.
Hospital Patient Safety, Quality Movement Helped Propel Hospitalists
Hippocrates, Epidemics.“The Physician must be able to do good or to do no harm.”
This is part three of my ongoing series on the journey of hospital medicine and how we are poised for greater things yet. In part one, “Tinder and Spark,” macro changes in the American healthcare landscape pressured primary care physicians to get creative with new ways to practice, the most prominent result being the creation of hospitalist practices. Wachter and Goldman provided the spark that gave the field its name and cohesiveness. In part two, “Fuel,” the Baby Boomers shaped the field, setting the stage for the Generation X physicians who fueled HM’s early growth.
But the field might have stagnated there, the fire attenuated, if not for the rise of something new, something that stoked our growth to new heights.
Orlando, Fla., December 2006.
SHM President-Elect Rusty Holman, MD, MHM, was on stage representing hospitalists at the annual Institute for Healthcare Improvement (IHI) National Forum in front of more than 5,000 enthusiastic attendees representing every discipline of clinical care from hundreds of healthcare organizations across the country and internationally. This was a special event. Two years earlier, IHI President Don Berwick, MD, MPP, had launched an audacious campaign, called the 100,000 Lives Campaign, that aimed to prevent the deaths of 100,000 patients in our nation’s hospitals in the following 18 months, not by utilizing some great new technological advance but by changing the culture around safety and quality in our nation’s hospitals and enacting proven safety methods and processes.1 Out of this plan came widespread use of terms and programs that weren’t widely adopted then but are familiar to all of us now: rapid response teams, medicine reconciliation, surgical site infection prevention, and ventilator-acquired pneumonia.
That program estimated that it saved 122,000 lives.1
IHI was looking to build on the safety and quality infrastructure that had been built up to make the 100,000 Lives Campaign a success and to launch an even bigger program. The 5 Million Lives Campaign’s goal was to reduce incidents of harm in five million patients over the next two years. For this campaign, IHI understood that success could only be achieved with partners. SHM and the field of hospital medicine, which had grown in size and influence, was seen as a critical and influential partner in achieving the goal of reducing harm in our nation’s hospitals. Thus, Dr. Holman was standing on that stage for SHM at the launch of the biggest safety and quality initiative in our nation’s history. SHM was among seven partner organizations, including the American Nurses Association, the Centers for Medicare and Medicaid Services (CMS), the American Heart Association, and the CDC. SHM was the only medical society represented. Pretty heady stuff for a field barely 10 years old. How did we get there? For that story, we need to go back a few years.
In 1984, Libby Zion, an 18-year-old college student, died from serotonin syndrome. A contributing factor was felt to be overworked residents not getting enough sleep. In his landmark 1990 article, “Human Factors in Hazardous Situations,” James Reason, PhD, introduced the world to some key concepts: active versus latent errors and the Swiss cheese model of errors.2 These concepts influence our thinking to this day. In 1994, Betsy Lehman, a health reporter for the Boston Globe, died from a massive chemotherapy overdose. That same year Lucian Leape, MD, a Harvard pediatric surgeon, published his influential article in JAMA, “Errors in Medicine,” which called for a systems approach to improving patient safety.3
These key moments in safety and quality, all of which occurred in the years leading up to hospitalists gaining their identity, were but a prelude to the widespread patient safety and quality movement. Like our own social movement, “Patient Safety and Quality” was born with an influential publication. This was the 1999 release of the Institute of Medicine’s “To Err is Human,” a report that reiterated claims that up to 98,000 U.S. patients per year were dying from medical errors.4 It also supported Dr. Leape’s earlier work calling for systems changes. In 2001, the Institute of Medicine published a second report, “Crossing the Quality Chasm: A New Health System for the 21st Century,” which introduced the six aims for healthcare improvement: safe, timely, effective, efficient, equitable, and patient-centered.5
Before 1999, hospitalists were just getting their feet on the ground. Groups were experimenting with practice models and recruiting young talent, mostly with a pitch for a new way to practice with freedom to design their day and often an interesting work schedule.
After the publication of “To Err is Human” in 1999, changes in patient safety and quality began to accelerate. Taking one of the recommendations from “To Err is Human,” which suggested that employers should use their market power to improve quality and safety, the Leapfrog Group, a consortium of large employers, organized in 2000. Leapfrog began rewarding and recognizing hospitals that put accepted safety measures in place.6 Suddenly, hospital CEOs began to see tangible rewards for improving quality in their hospitals.
Here is where the hospitalist movement and the patient safety and quality movement began to intersect.
Shift to Quality and Safety
In 2001, the same year “Crossing the Quality Chasm” was published, Congress created the Center for Quality Improvement and Patient Safety within the Agency for Healthcare Research and Quality. Significant funding was suddenly available for quality and safety research, and a more organized reporting mechanism for quality would soon be available.
In 2002, the Joint Commission released its first set of National Patient Safety Goals. There were seven, and key goals for hospitalists included improving the effectiveness of communication among caregivers, reducing the risk of healthcare-acquired infections, and reconciling medications.
And, lastly, as if that weren’t enough activity in the patient safety and quality world, the Joint Commission and CMS released in 2003 the first joint, aligned set of core measures, with which we are all now very familiar, around acute myocardial infarction, congestive heart failure, and pneumonia.
Hospital executives were trying to get a handle on the meaning of this flurry of activity for their hospitals. It certainly meant new regulatory requirements. It probably meant greater visibility to the public around what happened behind the walls of their facilities. No doubt dollars on the line wouldn’t be too far behind. They needed help, and they needed it fast.
No longer were hospitalists a small group of young docs roaming the halls; now, instead of just taking care of one patient at a time, they were reaching the threshold of size—and even status in some organizations—where they could leverage their working knowledge of the system and presence on site to affect the various facets of quality now being measured and incented. Additionally, as the information technology (IT) revolution rolled out, hospitalists, mostly tech-savvy Gen X’ers, looked to ease the transition into the new world of EHRs, which promised to serve as a new base for improving quality.
As the C-suite continued making value calculations in their heads, they saw that, in addition to helping them manage the many facets of the transition of primary care and specialty teaching attendings out of the hospital, hospitalists could now be a powerful weapon in helping them stay competitive in the looming patient safety and quality revolution. They pulled out their checkbooks.
When SHM first started gathering data to explore this gap, we discovered that in 2003 the reported median support per FTE of an adult hospitalist in this country was $60,000.7 With an estimated 11,000 hospitalists in the country at that time, C-suite funders paid out over $600 million to help overcome the deficit between hospitalist professional billings and salary and benefits. By the time SHM partnered with IHI on the 5 Million Lives Campaign in 2006, the figure stood at well over $2 billion. The 2011 SHM/Medical Group Management Association survey data showed $139,090 support per FTE. With 31,000 U.S. hospitalists estimated at the time, that figure had doubled to over $4 billion in just five years’ time.
The new generation of doctors had come along in the late 1990s looking for a practice that fit their wants and needs. HM gave them what they were looking for: autonomy, the promise of work-life balance, and the ability to help patients in their most vulnerable time. The traditional E&M [evaluation and management]-based funding mechanisms simply weren’t designed to account for physicians who spend all of their time doing the critical cognitive and coordinating clinical work. To account for this, hospitals and medical groups, seeing the value to their organizations in this new specialty, anteed up to cover the difference. That gave us a great beginning.
But it was the convergence of the early hospitalist movement and the emergent patient safety and quality movement that created a synergy that propelled both movements forward. Boosted by the influx of funding directly and indirectly related to patient safety and quality, hospitalists grew in number from an estimated 5,000 physicians at the 1999 publication of “To Err is Human” to north of 40,000 today.
The synergy was evident when SHM President-Elect Dr. Holman, representing our fledgling specialty and society, faced that cheering throng in Orlando alongside Dr. Don Berwick, the face of the patient safety and quality movement.
But that’s not quite the end of the story.
To get us up to the present and on to our bright future, there will be a few more additions to the quality story and an all-new generation arriving on the scene to shake things up.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Institute for Healthcare Improvement. Overview of the 100,000 Lives Campaign. Available at: http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Documents/Overview%20of%20the%20100K%20Campaign.pdf. Accessed July 6, 2014.
- Broadbent DE, Reason J, Baddeley A, eds. Human Factors in Hazardous Situations: Proceedings of a Royal Society Discussion Meeting Held on 28 and 29 June 1989. Gloucestershire, England: Clarendon Press; 1990:475-484.
- Leape LL. Error in medicine JAMA.1994;272(23):1851-1857.
- Institute of Medicine. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: The National Academy Press; 2000.
- Institute of Medicine. Committee on Quality of Healthcare in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: The National Academy Press; 2001.
- The Leapfrog Group. About Leapfrog. Available at: http://www.leapfroggroup.org/about_leapfrog. Accessed July 6, 2014.
- Society of Hospital Medicine. SHM’s State of Hospital Medicine Surveys 2003-2012. Available at: www.hospitalmedicine.org/survey. Accessed July 3, 2014.
Hippocrates, Epidemics.“The Physician must be able to do good or to do no harm.”
This is part three of my ongoing series on the journey of hospital medicine and how we are poised for greater things yet. In part one, “Tinder and Spark,” macro changes in the American healthcare landscape pressured primary care physicians to get creative with new ways to practice, the most prominent result being the creation of hospitalist practices. Wachter and Goldman provided the spark that gave the field its name and cohesiveness. In part two, “Fuel,” the Baby Boomers shaped the field, setting the stage for the Generation X physicians who fueled HM’s early growth.
But the field might have stagnated there, the fire attenuated, if not for the rise of something new, something that stoked our growth to new heights.
Orlando, Fla., December 2006.
SHM President-Elect Rusty Holman, MD, MHM, was on stage representing hospitalists at the annual Institute for Healthcare Improvement (IHI) National Forum in front of more than 5,000 enthusiastic attendees representing every discipline of clinical care from hundreds of healthcare organizations across the country and internationally. This was a special event. Two years earlier, IHI President Don Berwick, MD, MPP, had launched an audacious campaign, called the 100,000 Lives Campaign, that aimed to prevent the deaths of 100,000 patients in our nation’s hospitals in the following 18 months, not by utilizing some great new technological advance but by changing the culture around safety and quality in our nation’s hospitals and enacting proven safety methods and processes.1 Out of this plan came widespread use of terms and programs that weren’t widely adopted then but are familiar to all of us now: rapid response teams, medicine reconciliation, surgical site infection prevention, and ventilator-acquired pneumonia.
That program estimated that it saved 122,000 lives.1
IHI was looking to build on the safety and quality infrastructure that had been built up to make the 100,000 Lives Campaign a success and to launch an even bigger program. The 5 Million Lives Campaign’s goal was to reduce incidents of harm in five million patients over the next two years. For this campaign, IHI understood that success could only be achieved with partners. SHM and the field of hospital medicine, which had grown in size and influence, was seen as a critical and influential partner in achieving the goal of reducing harm in our nation’s hospitals. Thus, Dr. Holman was standing on that stage for SHM at the launch of the biggest safety and quality initiative in our nation’s history. SHM was among seven partner organizations, including the American Nurses Association, the Centers for Medicare and Medicaid Services (CMS), the American Heart Association, and the CDC. SHM was the only medical society represented. Pretty heady stuff for a field barely 10 years old. How did we get there? For that story, we need to go back a few years.
In 1984, Libby Zion, an 18-year-old college student, died from serotonin syndrome. A contributing factor was felt to be overworked residents not getting enough sleep. In his landmark 1990 article, “Human Factors in Hazardous Situations,” James Reason, PhD, introduced the world to some key concepts: active versus latent errors and the Swiss cheese model of errors.2 These concepts influence our thinking to this day. In 1994, Betsy Lehman, a health reporter for the Boston Globe, died from a massive chemotherapy overdose. That same year Lucian Leape, MD, a Harvard pediatric surgeon, published his influential article in JAMA, “Errors in Medicine,” which called for a systems approach to improving patient safety.3
These key moments in safety and quality, all of which occurred in the years leading up to hospitalists gaining their identity, were but a prelude to the widespread patient safety and quality movement. Like our own social movement, “Patient Safety and Quality” was born with an influential publication. This was the 1999 release of the Institute of Medicine’s “To Err is Human,” a report that reiterated claims that up to 98,000 U.S. patients per year were dying from medical errors.4 It also supported Dr. Leape’s earlier work calling for systems changes. In 2001, the Institute of Medicine published a second report, “Crossing the Quality Chasm: A New Health System for the 21st Century,” which introduced the six aims for healthcare improvement: safe, timely, effective, efficient, equitable, and patient-centered.5
Before 1999, hospitalists were just getting their feet on the ground. Groups were experimenting with practice models and recruiting young talent, mostly with a pitch for a new way to practice with freedom to design their day and often an interesting work schedule.
After the publication of “To Err is Human” in 1999, changes in patient safety and quality began to accelerate. Taking one of the recommendations from “To Err is Human,” which suggested that employers should use their market power to improve quality and safety, the Leapfrog Group, a consortium of large employers, organized in 2000. Leapfrog began rewarding and recognizing hospitals that put accepted safety measures in place.6 Suddenly, hospital CEOs began to see tangible rewards for improving quality in their hospitals.
Here is where the hospitalist movement and the patient safety and quality movement began to intersect.
Shift to Quality and Safety
In 2001, the same year “Crossing the Quality Chasm” was published, Congress created the Center for Quality Improvement and Patient Safety within the Agency for Healthcare Research and Quality. Significant funding was suddenly available for quality and safety research, and a more organized reporting mechanism for quality would soon be available.
In 2002, the Joint Commission released its first set of National Patient Safety Goals. There were seven, and key goals for hospitalists included improving the effectiveness of communication among caregivers, reducing the risk of healthcare-acquired infections, and reconciling medications.
And, lastly, as if that weren’t enough activity in the patient safety and quality world, the Joint Commission and CMS released in 2003 the first joint, aligned set of core measures, with which we are all now very familiar, around acute myocardial infarction, congestive heart failure, and pneumonia.
Hospital executives were trying to get a handle on the meaning of this flurry of activity for their hospitals. It certainly meant new regulatory requirements. It probably meant greater visibility to the public around what happened behind the walls of their facilities. No doubt dollars on the line wouldn’t be too far behind. They needed help, and they needed it fast.
No longer were hospitalists a small group of young docs roaming the halls; now, instead of just taking care of one patient at a time, they were reaching the threshold of size—and even status in some organizations—where they could leverage their working knowledge of the system and presence on site to affect the various facets of quality now being measured and incented. Additionally, as the information technology (IT) revolution rolled out, hospitalists, mostly tech-savvy Gen X’ers, looked to ease the transition into the new world of EHRs, which promised to serve as a new base for improving quality.
As the C-suite continued making value calculations in their heads, they saw that, in addition to helping them manage the many facets of the transition of primary care and specialty teaching attendings out of the hospital, hospitalists could now be a powerful weapon in helping them stay competitive in the looming patient safety and quality revolution. They pulled out their checkbooks.
When SHM first started gathering data to explore this gap, we discovered that in 2003 the reported median support per FTE of an adult hospitalist in this country was $60,000.7 With an estimated 11,000 hospitalists in the country at that time, C-suite funders paid out over $600 million to help overcome the deficit between hospitalist professional billings and salary and benefits. By the time SHM partnered with IHI on the 5 Million Lives Campaign in 2006, the figure stood at well over $2 billion. The 2011 SHM/Medical Group Management Association survey data showed $139,090 support per FTE. With 31,000 U.S. hospitalists estimated at the time, that figure had doubled to over $4 billion in just five years’ time.
The new generation of doctors had come along in the late 1990s looking for a practice that fit their wants and needs. HM gave them what they were looking for: autonomy, the promise of work-life balance, and the ability to help patients in their most vulnerable time. The traditional E&M [evaluation and management]-based funding mechanisms simply weren’t designed to account for physicians who spend all of their time doing the critical cognitive and coordinating clinical work. To account for this, hospitals and medical groups, seeing the value to their organizations in this new specialty, anteed up to cover the difference. That gave us a great beginning.
But it was the convergence of the early hospitalist movement and the emergent patient safety and quality movement that created a synergy that propelled both movements forward. Boosted by the influx of funding directly and indirectly related to patient safety and quality, hospitalists grew in number from an estimated 5,000 physicians at the 1999 publication of “To Err is Human” to north of 40,000 today.
The synergy was evident when SHM President-Elect Dr. Holman, representing our fledgling specialty and society, faced that cheering throng in Orlando alongside Dr. Don Berwick, the face of the patient safety and quality movement.
But that’s not quite the end of the story.
To get us up to the present and on to our bright future, there will be a few more additions to the quality story and an all-new generation arriving on the scene to shake things up.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Institute for Healthcare Improvement. Overview of the 100,000 Lives Campaign. Available at: http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Documents/Overview%20of%20the%20100K%20Campaign.pdf. Accessed July 6, 2014.
- Broadbent DE, Reason J, Baddeley A, eds. Human Factors in Hazardous Situations: Proceedings of a Royal Society Discussion Meeting Held on 28 and 29 June 1989. Gloucestershire, England: Clarendon Press; 1990:475-484.
- Leape LL. Error in medicine JAMA.1994;272(23):1851-1857.
- Institute of Medicine. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: The National Academy Press; 2000.
- Institute of Medicine. Committee on Quality of Healthcare in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: The National Academy Press; 2001.
- The Leapfrog Group. About Leapfrog. Available at: http://www.leapfroggroup.org/about_leapfrog. Accessed July 6, 2014.
- Society of Hospital Medicine. SHM’s State of Hospital Medicine Surveys 2003-2012. Available at: www.hospitalmedicine.org/survey. Accessed July 3, 2014.
Hippocrates, Epidemics.“The Physician must be able to do good or to do no harm.”
This is part three of my ongoing series on the journey of hospital medicine and how we are poised for greater things yet. In part one, “Tinder and Spark,” macro changes in the American healthcare landscape pressured primary care physicians to get creative with new ways to practice, the most prominent result being the creation of hospitalist practices. Wachter and Goldman provided the spark that gave the field its name and cohesiveness. In part two, “Fuel,” the Baby Boomers shaped the field, setting the stage for the Generation X physicians who fueled HM’s early growth.
But the field might have stagnated there, the fire attenuated, if not for the rise of something new, something that stoked our growth to new heights.
Orlando, Fla., December 2006.
SHM President-Elect Rusty Holman, MD, MHM, was on stage representing hospitalists at the annual Institute for Healthcare Improvement (IHI) National Forum in front of more than 5,000 enthusiastic attendees representing every discipline of clinical care from hundreds of healthcare organizations across the country and internationally. This was a special event. Two years earlier, IHI President Don Berwick, MD, MPP, had launched an audacious campaign, called the 100,000 Lives Campaign, that aimed to prevent the deaths of 100,000 patients in our nation’s hospitals in the following 18 months, not by utilizing some great new technological advance but by changing the culture around safety and quality in our nation’s hospitals and enacting proven safety methods and processes.1 Out of this plan came widespread use of terms and programs that weren’t widely adopted then but are familiar to all of us now: rapid response teams, medicine reconciliation, surgical site infection prevention, and ventilator-acquired pneumonia.
That program estimated that it saved 122,000 lives.1
IHI was looking to build on the safety and quality infrastructure that had been built up to make the 100,000 Lives Campaign a success and to launch an even bigger program. The 5 Million Lives Campaign’s goal was to reduce incidents of harm in five million patients over the next two years. For this campaign, IHI understood that success could only be achieved with partners. SHM and the field of hospital medicine, which had grown in size and influence, was seen as a critical and influential partner in achieving the goal of reducing harm in our nation’s hospitals. Thus, Dr. Holman was standing on that stage for SHM at the launch of the biggest safety and quality initiative in our nation’s history. SHM was among seven partner organizations, including the American Nurses Association, the Centers for Medicare and Medicaid Services (CMS), the American Heart Association, and the CDC. SHM was the only medical society represented. Pretty heady stuff for a field barely 10 years old. How did we get there? For that story, we need to go back a few years.
In 1984, Libby Zion, an 18-year-old college student, died from serotonin syndrome. A contributing factor was felt to be overworked residents not getting enough sleep. In his landmark 1990 article, “Human Factors in Hazardous Situations,” James Reason, PhD, introduced the world to some key concepts: active versus latent errors and the Swiss cheese model of errors.2 These concepts influence our thinking to this day. In 1994, Betsy Lehman, a health reporter for the Boston Globe, died from a massive chemotherapy overdose. That same year Lucian Leape, MD, a Harvard pediatric surgeon, published his influential article in JAMA, “Errors in Medicine,” which called for a systems approach to improving patient safety.3
These key moments in safety and quality, all of which occurred in the years leading up to hospitalists gaining their identity, were but a prelude to the widespread patient safety and quality movement. Like our own social movement, “Patient Safety and Quality” was born with an influential publication. This was the 1999 release of the Institute of Medicine’s “To Err is Human,” a report that reiterated claims that up to 98,000 U.S. patients per year were dying from medical errors.4 It also supported Dr. Leape’s earlier work calling for systems changes. In 2001, the Institute of Medicine published a second report, “Crossing the Quality Chasm: A New Health System for the 21st Century,” which introduced the six aims for healthcare improvement: safe, timely, effective, efficient, equitable, and patient-centered.5
Before 1999, hospitalists were just getting their feet on the ground. Groups were experimenting with practice models and recruiting young talent, mostly with a pitch for a new way to practice with freedom to design their day and often an interesting work schedule.
After the publication of “To Err is Human” in 1999, changes in patient safety and quality began to accelerate. Taking one of the recommendations from “To Err is Human,” which suggested that employers should use their market power to improve quality and safety, the Leapfrog Group, a consortium of large employers, organized in 2000. Leapfrog began rewarding and recognizing hospitals that put accepted safety measures in place.6 Suddenly, hospital CEOs began to see tangible rewards for improving quality in their hospitals.
Here is where the hospitalist movement and the patient safety and quality movement began to intersect.
Shift to Quality and Safety
In 2001, the same year “Crossing the Quality Chasm” was published, Congress created the Center for Quality Improvement and Patient Safety within the Agency for Healthcare Research and Quality. Significant funding was suddenly available for quality and safety research, and a more organized reporting mechanism for quality would soon be available.
In 2002, the Joint Commission released its first set of National Patient Safety Goals. There were seven, and key goals for hospitalists included improving the effectiveness of communication among caregivers, reducing the risk of healthcare-acquired infections, and reconciling medications.
And, lastly, as if that weren’t enough activity in the patient safety and quality world, the Joint Commission and CMS released in 2003 the first joint, aligned set of core measures, with which we are all now very familiar, around acute myocardial infarction, congestive heart failure, and pneumonia.
Hospital executives were trying to get a handle on the meaning of this flurry of activity for their hospitals. It certainly meant new regulatory requirements. It probably meant greater visibility to the public around what happened behind the walls of their facilities. No doubt dollars on the line wouldn’t be too far behind. They needed help, and they needed it fast.
No longer were hospitalists a small group of young docs roaming the halls; now, instead of just taking care of one patient at a time, they were reaching the threshold of size—and even status in some organizations—where they could leverage their working knowledge of the system and presence on site to affect the various facets of quality now being measured and incented. Additionally, as the information technology (IT) revolution rolled out, hospitalists, mostly tech-savvy Gen X’ers, looked to ease the transition into the new world of EHRs, which promised to serve as a new base for improving quality.
As the C-suite continued making value calculations in their heads, they saw that, in addition to helping them manage the many facets of the transition of primary care and specialty teaching attendings out of the hospital, hospitalists could now be a powerful weapon in helping them stay competitive in the looming patient safety and quality revolution. They pulled out their checkbooks.
When SHM first started gathering data to explore this gap, we discovered that in 2003 the reported median support per FTE of an adult hospitalist in this country was $60,000.7 With an estimated 11,000 hospitalists in the country at that time, C-suite funders paid out over $600 million to help overcome the deficit between hospitalist professional billings and salary and benefits. By the time SHM partnered with IHI on the 5 Million Lives Campaign in 2006, the figure stood at well over $2 billion. The 2011 SHM/Medical Group Management Association survey data showed $139,090 support per FTE. With 31,000 U.S. hospitalists estimated at the time, that figure had doubled to over $4 billion in just five years’ time.
The new generation of doctors had come along in the late 1990s looking for a practice that fit their wants and needs. HM gave them what they were looking for: autonomy, the promise of work-life balance, and the ability to help patients in their most vulnerable time. The traditional E&M [evaluation and management]-based funding mechanisms simply weren’t designed to account for physicians who spend all of their time doing the critical cognitive and coordinating clinical work. To account for this, hospitals and medical groups, seeing the value to their organizations in this new specialty, anteed up to cover the difference. That gave us a great beginning.
But it was the convergence of the early hospitalist movement and the emergent patient safety and quality movement that created a synergy that propelled both movements forward. Boosted by the influx of funding directly and indirectly related to patient safety and quality, hospitalists grew in number from an estimated 5,000 physicians at the 1999 publication of “To Err is Human” to north of 40,000 today.
The synergy was evident when SHM President-Elect Dr. Holman, representing our fledgling specialty and society, faced that cheering throng in Orlando alongside Dr. Don Berwick, the face of the patient safety and quality movement.
But that’s not quite the end of the story.
To get us up to the present and on to our bright future, there will be a few more additions to the quality story and an all-new generation arriving on the scene to shake things up.
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Institute for Healthcare Improvement. Overview of the 100,000 Lives Campaign. Available at: http://www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign/Documents/Overview%20of%20the%20100K%20Campaign.pdf. Accessed July 6, 2014.
- Broadbent DE, Reason J, Baddeley A, eds. Human Factors in Hazardous Situations: Proceedings of a Royal Society Discussion Meeting Held on 28 and 29 June 1989. Gloucestershire, England: Clarendon Press; 1990:475-484.
- Leape LL. Error in medicine JAMA.1994;272(23):1851-1857.
- Institute of Medicine. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, D.C.: The National Academy Press; 2000.
- Institute of Medicine. Committee on Quality of Healthcare in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: The National Academy Press; 2001.
- The Leapfrog Group. About Leapfrog. Available at: http://www.leapfroggroup.org/about_leapfrog. Accessed July 6, 2014.
- Society of Hospital Medicine. SHM’s State of Hospital Medicine Surveys 2003-2012. Available at: www.hospitalmedicine.org/survey. Accessed July 3, 2014.
How Generation X-Era Physicians Have Energized Hospital Medicine
“Each generation goes further than the generation preceding it, because it stands on the shoulders of that generation. You will have opportunities beyond anything we've ever known.”
—Former U.S. President Ronald Reagan
In the April 2014 issue of The Hospitalist, I began the tale of our specialty and the beginning of our evolution into a social movement. A social movement occurs when a large number of agents take coordinated action simultaneously.1 In the early days, managed care and other factors began driving doctors to try new, more efficient ways to practice, including early hospitalist practices, but usually these practices were one-offs and uncoordinated in their actions. Additionally, small numbers of doctors, perhaps a few hundred, focused their practice in the hospital. Drs. Wachter and Goldman published their “Sounding Board” article in the New England Journal of Medicine and, suddenly, hospital doctors across the country had a common identity: hospitalists.2 The specialty was poised for growth, but who would fill the need to come?
We should back up a few years to the dawn of the hospitalist movement in the late 1980s and early 1990s. For 20 years, Baby Boomers had been matriculating and graduating from medical school. The last Baby Boomers would graduate as the 1990s were just beginning. Baby Boomers were raised in the post-war era, largely by intact families with working fathers and stay-at-home mothers. They grew up in a competitive school environment—fueled by Sputnik—with a focus on success and working hard as the means to achieve that success. They were raised to be idealists and to question authority—remember Vietnam protests? These traits served the Baby Boomers well when managed care began to exert its pressure on physician practices. It was these physicians who figured out a new way to succeed in an altered landscape. It was either them or the big payers; their competitive nature was funneled into trying new, efficient practice models, to maintain income and control over their practices. Hospitalist systems were the most visible new practice model created in this era.
Fast forward a few years to the mid 1990s. A demographic shift was occurring. A new generation of Americans arrived on the scene of modern medicine—Generation X. The first Gen-X physicians graduated from medical school in 1991 and began moving into internship. They would graduate from residency in 1994, just as the early HM groups were starting to build a quiet but critical mass. This was a generation raised as latchkey kids in a time of rising divorce rates and working mothers. These kids were often home alone and grew up with more freedom and independence than any recent generation in history. Gen-X kids learned how to function on their own. Resourceful and self-reliant, they took on responsibility, but, conversely, did not appreciate being watched over. They liked to work at their own pace and valued work-life balance in a way that was foreign to the Baby Boomers. They weren’t born with keyboards in their cradles, but this was the first generation raised with technology—and they embraced it.
As these Generation X’ers came out of residency looking for the right fit in a specialty, trying creative ways of doing things, and seeking balance in their lives, they saw the early hospitalist programs the Boomer pioneers had created and started to join. They saw in these early hospitalist programs all that they were looking for in a practice. In many programs, the first hospitalists were lonely souls—but lonely by choice, usually left to their own devices. Their partners in the clinic stopped coming to the hospital, and their administrative leaders focused on the engine of running the clinic and managing the capitated and non-capitated costs of care.
Hospitalist practices became bastions of independence and freedom. No longer were these physicians chained down to their small area in one hallway of the clinic, nor did they cling to the metaphor of the fast-moving production line. Hospitalists could roam the hospital at will, from inpatient unit to ED to ICU. Hospitalists could eat lunch when they wanted to! Gen-X physicians flocked to this model of independence that so aligned with their own inner desire to work at their own pace and in their own way.
These early hospitalist programs, still trying to find their way in a complicated and changing healthcare environment, necessitated continued resourcefulness. We saw creative approaches to scheduling that favored continuity (seven on/seven off), transitions to hospitalists as teaching attendings, and early attempts at night coverage. The transition from at-home call or coverage by residents to in-house shifts to nocturnists could fill its own column. The creative opportunities offered by these early practices strongly appealed to the Gen-X sensibilities and values.3
Lastly, work-life balance strongly resonated with Gen-X physicians. Many of the Boomer physicians of the time were content to stay in the clinic and “run faster” to keep up with the demands of managed care; however, the Boomers who migrated to the hospital and the early Gen-X physicians seemed to have a different mindset. They relished the opportunity to work in the new hybrid model. I say hybrid because it certainly wasn’t the ongoing continuity model that it originated from in primary care, but neither was it pure shift work like in the ED. It had the element of daily shifts—but clustered together in five to 14 day runs, often with an equal amount of time away from work. Additionally, nobody was taking work home—at least not until EMR. Work-life balance was the recruiting “pitch” during the late 90s and early 2000s.
So, after the creation of the field by Baby Boomers, the Gen-X doctors were the fuel needed to grow the specialty at a pace never before seen in medicine. Wachter and Goldman’s article opened the floodgates. Between 1997 and 2006, the number of hospitalists grew by 29%—not in total, but 29% per year!
Gen-X physicians latched onto the idea created and publicized by the Boomers, but the movement needed more to sustain, even accelerate, that early growth than just an interesting new idea for how to see hospital patients. What was the oxygen? What gave the HM social movement its purpose?
In my August column, I will explore what came next to propel HM from a new area of practice, an offshoot of primary care, into a full-fledged movement. It was that next thing that made our field “go viral.”
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Lancaster LC, Stillman D. When Generations Collide. Who They Are. Why They Clash. How to Solve the Generational Puzzle at Work. New York: HarperCollins; 2002.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. New Engl J Med. 1996;335(7):514-517.
- Wachter R. Today’s NEJM hospitalist study: what’s the news? Available at: http://community.the-hospitalist.org/2009/03/13/today-s-nejm-hospitalist-study-what-s-the-news/. Accessed May 11, 2014.
“Each generation goes further than the generation preceding it, because it stands on the shoulders of that generation. You will have opportunities beyond anything we've ever known.”
—Former U.S. President Ronald Reagan
In the April 2014 issue of The Hospitalist, I began the tale of our specialty and the beginning of our evolution into a social movement. A social movement occurs when a large number of agents take coordinated action simultaneously.1 In the early days, managed care and other factors began driving doctors to try new, more efficient ways to practice, including early hospitalist practices, but usually these practices were one-offs and uncoordinated in their actions. Additionally, small numbers of doctors, perhaps a few hundred, focused their practice in the hospital. Drs. Wachter and Goldman published their “Sounding Board” article in the New England Journal of Medicine and, suddenly, hospital doctors across the country had a common identity: hospitalists.2 The specialty was poised for growth, but who would fill the need to come?
We should back up a few years to the dawn of the hospitalist movement in the late 1980s and early 1990s. For 20 years, Baby Boomers had been matriculating and graduating from medical school. The last Baby Boomers would graduate as the 1990s were just beginning. Baby Boomers were raised in the post-war era, largely by intact families with working fathers and stay-at-home mothers. They grew up in a competitive school environment—fueled by Sputnik—with a focus on success and working hard as the means to achieve that success. They were raised to be idealists and to question authority—remember Vietnam protests? These traits served the Baby Boomers well when managed care began to exert its pressure on physician practices. It was these physicians who figured out a new way to succeed in an altered landscape. It was either them or the big payers; their competitive nature was funneled into trying new, efficient practice models, to maintain income and control over their practices. Hospitalist systems were the most visible new practice model created in this era.
Fast forward a few years to the mid 1990s. A demographic shift was occurring. A new generation of Americans arrived on the scene of modern medicine—Generation X. The first Gen-X physicians graduated from medical school in 1991 and began moving into internship. They would graduate from residency in 1994, just as the early HM groups were starting to build a quiet but critical mass. This was a generation raised as latchkey kids in a time of rising divorce rates and working mothers. These kids were often home alone and grew up with more freedom and independence than any recent generation in history. Gen-X kids learned how to function on their own. Resourceful and self-reliant, they took on responsibility, but, conversely, did not appreciate being watched over. They liked to work at their own pace and valued work-life balance in a way that was foreign to the Baby Boomers. They weren’t born with keyboards in their cradles, but this was the first generation raised with technology—and they embraced it.
As these Generation X’ers came out of residency looking for the right fit in a specialty, trying creative ways of doing things, and seeking balance in their lives, they saw the early hospitalist programs the Boomer pioneers had created and started to join. They saw in these early hospitalist programs all that they were looking for in a practice. In many programs, the first hospitalists were lonely souls—but lonely by choice, usually left to their own devices. Their partners in the clinic stopped coming to the hospital, and their administrative leaders focused on the engine of running the clinic and managing the capitated and non-capitated costs of care.
Hospitalist practices became bastions of independence and freedom. No longer were these physicians chained down to their small area in one hallway of the clinic, nor did they cling to the metaphor of the fast-moving production line. Hospitalists could roam the hospital at will, from inpatient unit to ED to ICU. Hospitalists could eat lunch when they wanted to! Gen-X physicians flocked to this model of independence that so aligned with their own inner desire to work at their own pace and in their own way.
These early hospitalist programs, still trying to find their way in a complicated and changing healthcare environment, necessitated continued resourcefulness. We saw creative approaches to scheduling that favored continuity (seven on/seven off), transitions to hospitalists as teaching attendings, and early attempts at night coverage. The transition from at-home call or coverage by residents to in-house shifts to nocturnists could fill its own column. The creative opportunities offered by these early practices strongly appealed to the Gen-X sensibilities and values.3
Lastly, work-life balance strongly resonated with Gen-X physicians. Many of the Boomer physicians of the time were content to stay in the clinic and “run faster” to keep up with the demands of managed care; however, the Boomers who migrated to the hospital and the early Gen-X physicians seemed to have a different mindset. They relished the opportunity to work in the new hybrid model. I say hybrid because it certainly wasn’t the ongoing continuity model that it originated from in primary care, but neither was it pure shift work like in the ED. It had the element of daily shifts—but clustered together in five to 14 day runs, often with an equal amount of time away from work. Additionally, nobody was taking work home—at least not until EMR. Work-life balance was the recruiting “pitch” during the late 90s and early 2000s.
So, after the creation of the field by Baby Boomers, the Gen-X doctors were the fuel needed to grow the specialty at a pace never before seen in medicine. Wachter and Goldman’s article opened the floodgates. Between 1997 and 2006, the number of hospitalists grew by 29%—not in total, but 29% per year!
Gen-X physicians latched onto the idea created and publicized by the Boomers, but the movement needed more to sustain, even accelerate, that early growth than just an interesting new idea for how to see hospital patients. What was the oxygen? What gave the HM social movement its purpose?
In my August column, I will explore what came next to propel HM from a new area of practice, an offshoot of primary care, into a full-fledged movement. It was that next thing that made our field “go viral.”
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Lancaster LC, Stillman D. When Generations Collide. Who They Are. Why They Clash. How to Solve the Generational Puzzle at Work. New York: HarperCollins; 2002.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. New Engl J Med. 1996;335(7):514-517.
- Wachter R. Today’s NEJM hospitalist study: what’s the news? Available at: http://community.the-hospitalist.org/2009/03/13/today-s-nejm-hospitalist-study-what-s-the-news/. Accessed May 11, 2014.
“Each generation goes further than the generation preceding it, because it stands on the shoulders of that generation. You will have opportunities beyond anything we've ever known.”
—Former U.S. President Ronald Reagan
In the April 2014 issue of The Hospitalist, I began the tale of our specialty and the beginning of our evolution into a social movement. A social movement occurs when a large number of agents take coordinated action simultaneously.1 In the early days, managed care and other factors began driving doctors to try new, more efficient ways to practice, including early hospitalist practices, but usually these practices were one-offs and uncoordinated in their actions. Additionally, small numbers of doctors, perhaps a few hundred, focused their practice in the hospital. Drs. Wachter and Goldman published their “Sounding Board” article in the New England Journal of Medicine and, suddenly, hospital doctors across the country had a common identity: hospitalists.2 The specialty was poised for growth, but who would fill the need to come?
We should back up a few years to the dawn of the hospitalist movement in the late 1980s and early 1990s. For 20 years, Baby Boomers had been matriculating and graduating from medical school. The last Baby Boomers would graduate as the 1990s were just beginning. Baby Boomers were raised in the post-war era, largely by intact families with working fathers and stay-at-home mothers. They grew up in a competitive school environment—fueled by Sputnik—with a focus on success and working hard as the means to achieve that success. They were raised to be idealists and to question authority—remember Vietnam protests? These traits served the Baby Boomers well when managed care began to exert its pressure on physician practices. It was these physicians who figured out a new way to succeed in an altered landscape. It was either them or the big payers; their competitive nature was funneled into trying new, efficient practice models, to maintain income and control over their practices. Hospitalist systems were the most visible new practice model created in this era.
Fast forward a few years to the mid 1990s. A demographic shift was occurring. A new generation of Americans arrived on the scene of modern medicine—Generation X. The first Gen-X physicians graduated from medical school in 1991 and began moving into internship. They would graduate from residency in 1994, just as the early HM groups were starting to build a quiet but critical mass. This was a generation raised as latchkey kids in a time of rising divorce rates and working mothers. These kids were often home alone and grew up with more freedom and independence than any recent generation in history. Gen-X kids learned how to function on their own. Resourceful and self-reliant, they took on responsibility, but, conversely, did not appreciate being watched over. They liked to work at their own pace and valued work-life balance in a way that was foreign to the Baby Boomers. They weren’t born with keyboards in their cradles, but this was the first generation raised with technology—and they embraced it.
As these Generation X’ers came out of residency looking for the right fit in a specialty, trying creative ways of doing things, and seeking balance in their lives, they saw the early hospitalist programs the Boomer pioneers had created and started to join. They saw in these early hospitalist programs all that they were looking for in a practice. In many programs, the first hospitalists were lonely souls—but lonely by choice, usually left to their own devices. Their partners in the clinic stopped coming to the hospital, and their administrative leaders focused on the engine of running the clinic and managing the capitated and non-capitated costs of care.
Hospitalist practices became bastions of independence and freedom. No longer were these physicians chained down to their small area in one hallway of the clinic, nor did they cling to the metaphor of the fast-moving production line. Hospitalists could roam the hospital at will, from inpatient unit to ED to ICU. Hospitalists could eat lunch when they wanted to! Gen-X physicians flocked to this model of independence that so aligned with their own inner desire to work at their own pace and in their own way.
These early hospitalist programs, still trying to find their way in a complicated and changing healthcare environment, necessitated continued resourcefulness. We saw creative approaches to scheduling that favored continuity (seven on/seven off), transitions to hospitalists as teaching attendings, and early attempts at night coverage. The transition from at-home call or coverage by residents to in-house shifts to nocturnists could fill its own column. The creative opportunities offered by these early practices strongly appealed to the Gen-X sensibilities and values.3
Lastly, work-life balance strongly resonated with Gen-X physicians. Many of the Boomer physicians of the time were content to stay in the clinic and “run faster” to keep up with the demands of managed care; however, the Boomers who migrated to the hospital and the early Gen-X physicians seemed to have a different mindset. They relished the opportunity to work in the new hybrid model. I say hybrid because it certainly wasn’t the ongoing continuity model that it originated from in primary care, but neither was it pure shift work like in the ED. It had the element of daily shifts—but clustered together in five to 14 day runs, often with an equal amount of time away from work. Additionally, nobody was taking work home—at least not until EMR. Work-life balance was the recruiting “pitch” during the late 90s and early 2000s.
So, after the creation of the field by Baby Boomers, the Gen-X doctors were the fuel needed to grow the specialty at a pace never before seen in medicine. Wachter and Goldman’s article opened the floodgates. Between 1997 and 2006, the number of hospitalists grew by 29%—not in total, but 29% per year!
Gen-X physicians latched onto the idea created and publicized by the Boomers, but the movement needed more to sustain, even accelerate, that early growth than just an interesting new idea for how to see hospital patients. What was the oxygen? What gave the HM social movement its purpose?
In my August column, I will explore what came next to propel HM from a new area of practice, an offshoot of primary care, into a full-fledged movement. It was that next thing that made our field “go viral.”
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Lancaster LC, Stillman D. When Generations Collide. Who They Are. Why They Clash. How to Solve the Generational Puzzle at Work. New York: HarperCollins; 2002.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. New Engl J Med. 1996;335(7):514-517.
- Wachter R. Today’s NEJM hospitalist study: what’s the news? Available at: http://community.the-hospitalist.org/2009/03/13/today-s-nejm-hospitalist-study-what-s-the-news/. Accessed May 11, 2014.
The Rise, Evolution of Hospital-Based Practice
“When the time is ripe for certain things, they appear at different places in the manner of violets coming to light in early spring.” —Farkas Bolyai, to his son, Janos, urging him to claim the invention of non-Euclidean geometry without delay.
In February, I was at a 20th anniversary party for the hospital medicine program from Park Nicollet Methodist Hospital in St Louis Park, Minn., listening to the original founders of the group giving speeches and telling stories of how their program began. For them, it all began at an internal medicine retreat in 1993, with ideas being tossed about on how to be more efficient and deliver better care for their patients. This was three years before Bob Wachter and Lee Goldman delivered their sounding board article to the New England Journal of Medicine describing some early programs and, more importantly, giving those new practitioners a name: “hospitalist.”1 The very same Park Nicollet program I was now helping to celebrate 20 years of success was called out in that article as one of four early groups in our country experimenting with hospitalists.
As I listened to the speeches, it occurred to me that the hospitalists standing up at the front of the room telling their war stories and reminiscing about the early days weren’t actually hospitalists at all back when they were thinking this new model up. They were primary care physicians struggling to meet the demands of the care environment at the time, coming up with unique solutions to the problems of the times without anyone telling them how or showing them the way. Back then, a few brave souls in the group stepped forward and said they would take on the majority of inpatient coverage, and suddenly, just like that, there were hospitalists, their given name still three years in the future, but hospitalists nevertheless.
Now this early program wasn’t the very first program, but it was part of a trend repeating at hospitals and within medical groups all over America. Slowly growing, slowly spreading, and under the radar, a social movement was afoot.
What Is a Social Movement?
Wikipedia says: Social movements are a type of group action. In sociology, a group action is a situation in which a large number of agents take action simultaneously in order to achieve a common goal; their actions are usually coordinated.
In those early days, the proto-hospitalists around the country were not coordinated or acting together, but that would come soon enough.
What were the factors that gave birth to this nascent social movement? Why was the same solution beginning to pop up all over the country in seemingly unconnected instances? The zeitgeist of the times had a lot to do with this, and it can all be boiled down to three things: time, money, and the “X” factor.
In the late 1980s and early 90s, managed care was making inroads into healthcare as a struggling country tried to wrestle with exploding costs. Capitated managed care systems attempted to control costs and improve health by managing cases preferentially, using PCPs with a directive to limit resource utilization.2 They were the “gatekeepers” to more expensive care options like specialists and hospitalization. They were tasked with managing larger panels of patients, conducting shorter visits, and seeing more patients per day. In the other type of managed care of the time (non-capitated), physician practices, to stay in the game, were negotiating large discounts for their services. Then, to maintain their income, they had to see larger numbers of patients, either in the same amount of time or, as was usually the case, in time added to their workday.2
Just when the country was starting to count on primary care to be the lynchpin for the new healthcare model, medical students were turning away from primary care in record numbers. Internal-medicine matches were near all-time lows. PCPs in practice were facing growing time and money crunches, and the medical students they were counting on to help out were choosing other fields. The cavalry of new doctors needed to bolster the ranks of those already struggling to keep up simply wasn’t coming.
Finally, unassigned care for hospitalized patients, which had always been a responsibility of local doctors, had frequently been a condition of hospital privileging, and was often seen by the doctors as a way to give back to their hospital and community, was now something that added even more time, work, and financial pressure to their growing burdens.
So, these doctors, just like the doctors in the Park Nicollet Medical Group, began to brainstorm new ways to improve efficiency and see if they could get on top of the changes happening around them. One such idea was to create rounder systems. These systems would have each doctor in the practice take a week away from clinic and care for all of the practice’s patients in the hospital. This way, only one doctor would have to spend time away from those ever-busier clinic practices during the week. By giving up the continuity of the individual rounder and trading it for the continuity of the group, these groups gained efficiencies for everyone in the practice. This was the first small, but critical, step toward hospital medicine. It would have been hard to get to hospitalists without PCPs taking that first mental leap.
Often, it was one or more of these rounders who decided, for various reasons—boredom with ambulatory care, dislike of the more frantic pace of clinic, or simply a realization that they enjoyed or excelled at hospital care—that maybe they would just take on all of the hospital care for their group. This is what happened at Park Nicollet, and what started happening all across the country. The tinder was assembled and stacked, ready for something else to happen.
The Spark
Word of these new types of models and practices began to spread and was even talked about inside the pages of some journals. It took a few years, but somebody noticed and finally put it all together into an article that was published in the most famous medical journal in the world. In that 1996 New England Journal of Medicine article, “The Emerging Role of ‘Hospitalists’ in the American Health Care System,” Wachter and Goldman gave a name to the strange creatures willingly giving up half of what they had been trained to do and devoting all their time to an inpatient practice.1 “Hospitalists,” they called them, and when the rest of the country read that article, the movement was no longer under the radar; it had a name. The spark had been ignited. What would become the fastest growing medical specialty in history was ready to take off.
But a spark needs more than tinder to truly ignite. Fuel and oxygen are necessary to give it life.
I’ll talk about that in my next column…
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. New Engl J Med. 1996;335(7):514-517.
- Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999;14(Suppl 1):S34-S40.
“When the time is ripe for certain things, they appear at different places in the manner of violets coming to light in early spring.” —Farkas Bolyai, to his son, Janos, urging him to claim the invention of non-Euclidean geometry without delay.
In February, I was at a 20th anniversary party for the hospital medicine program from Park Nicollet Methodist Hospital in St Louis Park, Minn., listening to the original founders of the group giving speeches and telling stories of how their program began. For them, it all began at an internal medicine retreat in 1993, with ideas being tossed about on how to be more efficient and deliver better care for their patients. This was three years before Bob Wachter and Lee Goldman delivered their sounding board article to the New England Journal of Medicine describing some early programs and, more importantly, giving those new practitioners a name: “hospitalist.”1 The very same Park Nicollet program I was now helping to celebrate 20 years of success was called out in that article as one of four early groups in our country experimenting with hospitalists.
As I listened to the speeches, it occurred to me that the hospitalists standing up at the front of the room telling their war stories and reminiscing about the early days weren’t actually hospitalists at all back when they were thinking this new model up. They were primary care physicians struggling to meet the demands of the care environment at the time, coming up with unique solutions to the problems of the times without anyone telling them how or showing them the way. Back then, a few brave souls in the group stepped forward and said they would take on the majority of inpatient coverage, and suddenly, just like that, there were hospitalists, their given name still three years in the future, but hospitalists nevertheless.
Now this early program wasn’t the very first program, but it was part of a trend repeating at hospitals and within medical groups all over America. Slowly growing, slowly spreading, and under the radar, a social movement was afoot.
What Is a Social Movement?
Wikipedia says: Social movements are a type of group action. In sociology, a group action is a situation in which a large number of agents take action simultaneously in order to achieve a common goal; their actions are usually coordinated.
In those early days, the proto-hospitalists around the country were not coordinated or acting together, but that would come soon enough.
What were the factors that gave birth to this nascent social movement? Why was the same solution beginning to pop up all over the country in seemingly unconnected instances? The zeitgeist of the times had a lot to do with this, and it can all be boiled down to three things: time, money, and the “X” factor.
In the late 1980s and early 90s, managed care was making inroads into healthcare as a struggling country tried to wrestle with exploding costs. Capitated managed care systems attempted to control costs and improve health by managing cases preferentially, using PCPs with a directive to limit resource utilization.2 They were the “gatekeepers” to more expensive care options like specialists and hospitalization. They were tasked with managing larger panels of patients, conducting shorter visits, and seeing more patients per day. In the other type of managed care of the time (non-capitated), physician practices, to stay in the game, were negotiating large discounts for their services. Then, to maintain their income, they had to see larger numbers of patients, either in the same amount of time or, as was usually the case, in time added to their workday.2
Just when the country was starting to count on primary care to be the lynchpin for the new healthcare model, medical students were turning away from primary care in record numbers. Internal-medicine matches were near all-time lows. PCPs in practice were facing growing time and money crunches, and the medical students they were counting on to help out were choosing other fields. The cavalry of new doctors needed to bolster the ranks of those already struggling to keep up simply wasn’t coming.
Finally, unassigned care for hospitalized patients, which had always been a responsibility of local doctors, had frequently been a condition of hospital privileging, and was often seen by the doctors as a way to give back to their hospital and community, was now something that added even more time, work, and financial pressure to their growing burdens.
So, these doctors, just like the doctors in the Park Nicollet Medical Group, began to brainstorm new ways to improve efficiency and see if they could get on top of the changes happening around them. One such idea was to create rounder systems. These systems would have each doctor in the practice take a week away from clinic and care for all of the practice’s patients in the hospital. This way, only one doctor would have to spend time away from those ever-busier clinic practices during the week. By giving up the continuity of the individual rounder and trading it for the continuity of the group, these groups gained efficiencies for everyone in the practice. This was the first small, but critical, step toward hospital medicine. It would have been hard to get to hospitalists without PCPs taking that first mental leap.
Often, it was one or more of these rounders who decided, for various reasons—boredom with ambulatory care, dislike of the more frantic pace of clinic, or simply a realization that they enjoyed or excelled at hospital care—that maybe they would just take on all of the hospital care for their group. This is what happened at Park Nicollet, and what started happening all across the country. The tinder was assembled and stacked, ready for something else to happen.
The Spark
Word of these new types of models and practices began to spread and was even talked about inside the pages of some journals. It took a few years, but somebody noticed and finally put it all together into an article that was published in the most famous medical journal in the world. In that 1996 New England Journal of Medicine article, “The Emerging Role of ‘Hospitalists’ in the American Health Care System,” Wachter and Goldman gave a name to the strange creatures willingly giving up half of what they had been trained to do and devoting all their time to an inpatient practice.1 “Hospitalists,” they called them, and when the rest of the country read that article, the movement was no longer under the radar; it had a name. The spark had been ignited. What would become the fastest growing medical specialty in history was ready to take off.
But a spark needs more than tinder to truly ignite. Fuel and oxygen are necessary to give it life.
I’ll talk about that in my next column…
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. New Engl J Med. 1996;335(7):514-517.
- Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999;14(Suppl 1):S34-S40.
“When the time is ripe for certain things, they appear at different places in the manner of violets coming to light in early spring.” —Farkas Bolyai, to his son, Janos, urging him to claim the invention of non-Euclidean geometry without delay.
In February, I was at a 20th anniversary party for the hospital medicine program from Park Nicollet Methodist Hospital in St Louis Park, Minn., listening to the original founders of the group giving speeches and telling stories of how their program began. For them, it all began at an internal medicine retreat in 1993, with ideas being tossed about on how to be more efficient and deliver better care for their patients. This was three years before Bob Wachter and Lee Goldman delivered their sounding board article to the New England Journal of Medicine describing some early programs and, more importantly, giving those new practitioners a name: “hospitalist.”1 The very same Park Nicollet program I was now helping to celebrate 20 years of success was called out in that article as one of four early groups in our country experimenting with hospitalists.
As I listened to the speeches, it occurred to me that the hospitalists standing up at the front of the room telling their war stories and reminiscing about the early days weren’t actually hospitalists at all back when they were thinking this new model up. They were primary care physicians struggling to meet the demands of the care environment at the time, coming up with unique solutions to the problems of the times without anyone telling them how or showing them the way. Back then, a few brave souls in the group stepped forward and said they would take on the majority of inpatient coverage, and suddenly, just like that, there were hospitalists, their given name still three years in the future, but hospitalists nevertheless.
Now this early program wasn’t the very first program, but it was part of a trend repeating at hospitals and within medical groups all over America. Slowly growing, slowly spreading, and under the radar, a social movement was afoot.
What Is a Social Movement?
Wikipedia says: Social movements are a type of group action. In sociology, a group action is a situation in which a large number of agents take action simultaneously in order to achieve a common goal; their actions are usually coordinated.
In those early days, the proto-hospitalists around the country were not coordinated or acting together, but that would come soon enough.
What were the factors that gave birth to this nascent social movement? Why was the same solution beginning to pop up all over the country in seemingly unconnected instances? The zeitgeist of the times had a lot to do with this, and it can all be boiled down to three things: time, money, and the “X” factor.
In the late 1980s and early 90s, managed care was making inroads into healthcare as a struggling country tried to wrestle with exploding costs. Capitated managed care systems attempted to control costs and improve health by managing cases preferentially, using PCPs with a directive to limit resource utilization.2 They were the “gatekeepers” to more expensive care options like specialists and hospitalization. They were tasked with managing larger panels of patients, conducting shorter visits, and seeing more patients per day. In the other type of managed care of the time (non-capitated), physician practices, to stay in the game, were negotiating large discounts for their services. Then, to maintain their income, they had to see larger numbers of patients, either in the same amount of time or, as was usually the case, in time added to their workday.2
Just when the country was starting to count on primary care to be the lynchpin for the new healthcare model, medical students were turning away from primary care in record numbers. Internal-medicine matches were near all-time lows. PCPs in practice were facing growing time and money crunches, and the medical students they were counting on to help out were choosing other fields. The cavalry of new doctors needed to bolster the ranks of those already struggling to keep up simply wasn’t coming.
Finally, unassigned care for hospitalized patients, which had always been a responsibility of local doctors, had frequently been a condition of hospital privileging, and was often seen by the doctors as a way to give back to their hospital and community, was now something that added even more time, work, and financial pressure to their growing burdens.
So, these doctors, just like the doctors in the Park Nicollet Medical Group, began to brainstorm new ways to improve efficiency and see if they could get on top of the changes happening around them. One such idea was to create rounder systems. These systems would have each doctor in the practice take a week away from clinic and care for all of the practice’s patients in the hospital. This way, only one doctor would have to spend time away from those ever-busier clinic practices during the week. By giving up the continuity of the individual rounder and trading it for the continuity of the group, these groups gained efficiencies for everyone in the practice. This was the first small, but critical, step toward hospital medicine. It would have been hard to get to hospitalists without PCPs taking that first mental leap.
Often, it was one or more of these rounders who decided, for various reasons—boredom with ambulatory care, dislike of the more frantic pace of clinic, or simply a realization that they enjoyed or excelled at hospital care—that maybe they would just take on all of the hospital care for their group. This is what happened at Park Nicollet, and what started happening all across the country. The tinder was assembled and stacked, ready for something else to happen.
The Spark
Word of these new types of models and practices began to spread and was even talked about inside the pages of some journals. It took a few years, but somebody noticed and finally put it all together into an article that was published in the most famous medical journal in the world. In that 1996 New England Journal of Medicine article, “The Emerging Role of ‘Hospitalists’ in the American Health Care System,” Wachter and Goldman gave a name to the strange creatures willingly giving up half of what they had been trained to do and devoting all their time to an inpatient practice.1 “Hospitalists,” they called them, and when the rest of the country read that article, the movement was no longer under the radar; it had a name. The spark had been ignited. What would become the fastest growing medical specialty in history was ready to take off.
But a spark needs more than tinder to truly ignite. Fuel and oxygen are necessary to give it life.
I’ll talk about that in my next column…
Dr. Kealey is SHM president and medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. New Engl J Med. 1996;335(7):514-517.
- Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999;14(Suppl 1):S34-S40.
Empathy Can Help Hospitalists Improve Patient Experience, Outcomes
Empathy: ability to understand and share the feelings of another.
In today’s increasingly hyper-measured healthcare world, we are looking more and more at measures of patient outcomes. The Institute for Healthcare Improvement (IHI) touts the Triple Aim principle as the lens through which we should be approaching our work. The Triple Aim is the three-part goal and simultaneous focus of improving the health of the community and our patients, improving affordability of care, and finally and perhaps most elusively, improving the patient experience. Who wouldn’t want to hit on these admirable goals? How do we do it?
In approaching the health aspect of the Triple Aim, we, as hospitalists, have tried-and-true frameworks of process improvement. Clinical research and peer-reviewed publication advance the knowledge of what medicines and procedures can improve care. Although powerful and generally truthful, this system results in a slow diffusion of practice improvement, not to mention idiosyncratic and nonstandardized care. This has led to a new toolkit of improvement techniques: continuous quality improvement, Lean, and Six Sigma. We learn and adopt these and watch our scores go up at a steady pace.
Improving affordability has its challenges, some huge, like our basic cultural ethos that “more is better.” Yet affordability is still something we can grasp. It is rooted in systems we are all familiar with, from basic personal finance to resource allocation to generally accepted accounting principles. We all can grasp that the current system of pay for widgets is teetering at the edge, just waiting for a shove from CMS to send it to its doom. Once this happens, affordability likely will become something we can start to make serious headway against.
Improving the experience of patients and families is perhaps the toughest of the three and where I would like to focus.
Patients First
First, a question: Are experience scores reflective of the true experience of a patient?
Two weeks after discharge, when patients receive their HCAHPS questionnaire in the mail, do they remember the details of their stay? And who was their doctor anyway? The cardiologist who placed a stent? The on-call doctor? The hospitalist who visited them every morning? If all we focus on is the scores, and we lack faith that the scores represent the true experience of patients, then how can we ever truly create a more satisfying experience for our patients?
I believe that the answer lies with empathy. What’s unique about this part of the Triple Aim is that many of the answers are within us. Gaining empathy with our patients requires us to ask questions of them and also to ask questions of ourselves. It requires us to invoke ancient methods of learning and thinking, like walking in another’s shoes for a day or using the Golden Rule. Experience doesn’t lend itself to being taught by PowerPoint. It must be lived and channeled back and out through our emotional selves as empathy.
Using the wisdom of patients themselves is one way to understand their needs and develop the empathy to motivate us to change how we do things in health care. Many organizations around the country have used some form of patient focus group to help learn from patients. Park Nicollet, a large health system in Minnesota, has incorporated family councils in nearly every clinic and care area. They usually are patients or caregivers from the area, bound together by a common disease or location. They dedicate their time, often meeting monthly, to share their stories, give opinions on care processes, and even to shape the design of a care area. Currently, there are more than 100 patient councils in the system, and the number continues to grow.
Film, when done skillfully, is a powerful tool in helping us gain empathy. The Cleveland Clinic has produced an amazing short film called “Empathy: The Human Connection to Patient Care.” It follows patients, families, and staff through the care system. As the camera focuses on each person, floating text appears near them, explaining their situation, inner thoughts, or fears, all overlaid by an emotional piano score. Tears will flow. Understanding follows.
Jim Merlino, MD, Cleveland Clinic’s chief experience officer, explains, “We need to understand that being on the other side of health care is frightening, and our job, our responsibility as people responsible for other people, is to help ease that fear.” Cleveland Clinic has done a remarkable job in reminding us why we went in to health care.
Morgan Spurlock of “Super Size Me” fame produced a reality series called “30 Days.” In each episode, a participant spent 30 days in the shoes of another. In the “Life in a Wheelchair” episode, Super Bowl-winning football player Ray Crockett lives in a wheelchair for 30 days and explores what it is like going through recovery and the healthcare system. He meets several rehabbing paraplegics and quadriplegics and accompanies them through their daily lives at home and the hospital. Viewers gain empathy directly in seeing these patients struggle to get better and work with the healthcare system. We also gain empathy watching Crockett gain empathy. The combination is powerful.
In Patients’ Shoes
In addition to listening and observation, we can begin to literally walk in the shoes of our patients.
I recently attended IHI’s International Forum in London. The National Health Service (NHS) in England is using a new tool to help providers understand what it is like for geriatric patients who must navigate the healthcare system with diminished senses and capabilities. Providers put on an age-simulation suit (www.age-simulation-suit.com) that mimics the impairments of aging. Special goggles fog the vision and narrow the visual field. Head mobility is reduced so that it becomes difficult to see beyond the field cuts. Earmuffs reduce high-frequency hearing and the ability to understand speech clearly. The overall suit impedes motion and reduces strength. Thick gloves make it difficult to coordinate fine motions. Wearing this suit and trying to go through a hospital or clinic setting instantly makes the wearer gain empathy for our patients’ needs.
Most important, be a patient. SHM immediate past president Shaun Frost, MD, SFHM, whose personal mission during his tenure was to help the society understand patient experience, explained it best to me. “In one episode in the hospital with a family member, I learned more about patient experience than all the reading and self-educating I have been doing for the last year.”
I think any of us who have been a patient in the hospital, or accompanied a loved one, comes out frustrated that the healthcare system is so convoluted and lacking in clarity for patients. Then there is often a sense of renewal, hopefully,followed by evangelism to spread their newfound empathy to others in the system.
In our busy work lives as hospitalists, it isn’t easy turning our daily focus away from efficiency and productivity. Yet we must always remain mindful of that core idea every one of us wrote down as the heart of our personal statements on our applications to medical school. Do you remember writing something like this? “I want to help people and relieve suffering in their time of need.”
Empathy is the start of our work.
Dr. Kealey is medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. He is an SHM board member and SHM president-elect.
Empathy: ability to understand and share the feelings of another.
In today’s increasingly hyper-measured healthcare world, we are looking more and more at measures of patient outcomes. The Institute for Healthcare Improvement (IHI) touts the Triple Aim principle as the lens through which we should be approaching our work. The Triple Aim is the three-part goal and simultaneous focus of improving the health of the community and our patients, improving affordability of care, and finally and perhaps most elusively, improving the patient experience. Who wouldn’t want to hit on these admirable goals? How do we do it?
In approaching the health aspect of the Triple Aim, we, as hospitalists, have tried-and-true frameworks of process improvement. Clinical research and peer-reviewed publication advance the knowledge of what medicines and procedures can improve care. Although powerful and generally truthful, this system results in a slow diffusion of practice improvement, not to mention idiosyncratic and nonstandardized care. This has led to a new toolkit of improvement techniques: continuous quality improvement, Lean, and Six Sigma. We learn and adopt these and watch our scores go up at a steady pace.
Improving affordability has its challenges, some huge, like our basic cultural ethos that “more is better.” Yet affordability is still something we can grasp. It is rooted in systems we are all familiar with, from basic personal finance to resource allocation to generally accepted accounting principles. We all can grasp that the current system of pay for widgets is teetering at the edge, just waiting for a shove from CMS to send it to its doom. Once this happens, affordability likely will become something we can start to make serious headway against.
Improving the experience of patients and families is perhaps the toughest of the three and where I would like to focus.
Patients First
First, a question: Are experience scores reflective of the true experience of a patient?
Two weeks after discharge, when patients receive their HCAHPS questionnaire in the mail, do they remember the details of their stay? And who was their doctor anyway? The cardiologist who placed a stent? The on-call doctor? The hospitalist who visited them every morning? If all we focus on is the scores, and we lack faith that the scores represent the true experience of patients, then how can we ever truly create a more satisfying experience for our patients?
I believe that the answer lies with empathy. What’s unique about this part of the Triple Aim is that many of the answers are within us. Gaining empathy with our patients requires us to ask questions of them and also to ask questions of ourselves. It requires us to invoke ancient methods of learning and thinking, like walking in another’s shoes for a day or using the Golden Rule. Experience doesn’t lend itself to being taught by PowerPoint. It must be lived and channeled back and out through our emotional selves as empathy.
Using the wisdom of patients themselves is one way to understand their needs and develop the empathy to motivate us to change how we do things in health care. Many organizations around the country have used some form of patient focus group to help learn from patients. Park Nicollet, a large health system in Minnesota, has incorporated family councils in nearly every clinic and care area. They usually are patients or caregivers from the area, bound together by a common disease or location. They dedicate their time, often meeting monthly, to share their stories, give opinions on care processes, and even to shape the design of a care area. Currently, there are more than 100 patient councils in the system, and the number continues to grow.
Film, when done skillfully, is a powerful tool in helping us gain empathy. The Cleveland Clinic has produced an amazing short film called “Empathy: The Human Connection to Patient Care.” It follows patients, families, and staff through the care system. As the camera focuses on each person, floating text appears near them, explaining their situation, inner thoughts, or fears, all overlaid by an emotional piano score. Tears will flow. Understanding follows.
Jim Merlino, MD, Cleveland Clinic’s chief experience officer, explains, “We need to understand that being on the other side of health care is frightening, and our job, our responsibility as people responsible for other people, is to help ease that fear.” Cleveland Clinic has done a remarkable job in reminding us why we went in to health care.
Morgan Spurlock of “Super Size Me” fame produced a reality series called “30 Days.” In each episode, a participant spent 30 days in the shoes of another. In the “Life in a Wheelchair” episode, Super Bowl-winning football player Ray Crockett lives in a wheelchair for 30 days and explores what it is like going through recovery and the healthcare system. He meets several rehabbing paraplegics and quadriplegics and accompanies them through their daily lives at home and the hospital. Viewers gain empathy directly in seeing these patients struggle to get better and work with the healthcare system. We also gain empathy watching Crockett gain empathy. The combination is powerful.
In Patients’ Shoes
In addition to listening and observation, we can begin to literally walk in the shoes of our patients.
I recently attended IHI’s International Forum in London. The National Health Service (NHS) in England is using a new tool to help providers understand what it is like for geriatric patients who must navigate the healthcare system with diminished senses and capabilities. Providers put on an age-simulation suit (www.age-simulation-suit.com) that mimics the impairments of aging. Special goggles fog the vision and narrow the visual field. Head mobility is reduced so that it becomes difficult to see beyond the field cuts. Earmuffs reduce high-frequency hearing and the ability to understand speech clearly. The overall suit impedes motion and reduces strength. Thick gloves make it difficult to coordinate fine motions. Wearing this suit and trying to go through a hospital or clinic setting instantly makes the wearer gain empathy for our patients’ needs.
Most important, be a patient. SHM immediate past president Shaun Frost, MD, SFHM, whose personal mission during his tenure was to help the society understand patient experience, explained it best to me. “In one episode in the hospital with a family member, I learned more about patient experience than all the reading and self-educating I have been doing for the last year.”
I think any of us who have been a patient in the hospital, or accompanied a loved one, comes out frustrated that the healthcare system is so convoluted and lacking in clarity for patients. Then there is often a sense of renewal, hopefully,followed by evangelism to spread their newfound empathy to others in the system.
In our busy work lives as hospitalists, it isn’t easy turning our daily focus away from efficiency and productivity. Yet we must always remain mindful of that core idea every one of us wrote down as the heart of our personal statements on our applications to medical school. Do you remember writing something like this? “I want to help people and relieve suffering in their time of need.”
Empathy is the start of our work.
Dr. Kealey is medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. He is an SHM board member and SHM president-elect.
Empathy: ability to understand and share the feelings of another.
In today’s increasingly hyper-measured healthcare world, we are looking more and more at measures of patient outcomes. The Institute for Healthcare Improvement (IHI) touts the Triple Aim principle as the lens through which we should be approaching our work. The Triple Aim is the three-part goal and simultaneous focus of improving the health of the community and our patients, improving affordability of care, and finally and perhaps most elusively, improving the patient experience. Who wouldn’t want to hit on these admirable goals? How do we do it?
In approaching the health aspect of the Triple Aim, we, as hospitalists, have tried-and-true frameworks of process improvement. Clinical research and peer-reviewed publication advance the knowledge of what medicines and procedures can improve care. Although powerful and generally truthful, this system results in a slow diffusion of practice improvement, not to mention idiosyncratic and nonstandardized care. This has led to a new toolkit of improvement techniques: continuous quality improvement, Lean, and Six Sigma. We learn and adopt these and watch our scores go up at a steady pace.
Improving affordability has its challenges, some huge, like our basic cultural ethos that “more is better.” Yet affordability is still something we can grasp. It is rooted in systems we are all familiar with, from basic personal finance to resource allocation to generally accepted accounting principles. We all can grasp that the current system of pay for widgets is teetering at the edge, just waiting for a shove from CMS to send it to its doom. Once this happens, affordability likely will become something we can start to make serious headway against.
Improving the experience of patients and families is perhaps the toughest of the three and where I would like to focus.
Patients First
First, a question: Are experience scores reflective of the true experience of a patient?
Two weeks after discharge, when patients receive their HCAHPS questionnaire in the mail, do they remember the details of their stay? And who was their doctor anyway? The cardiologist who placed a stent? The on-call doctor? The hospitalist who visited them every morning? If all we focus on is the scores, and we lack faith that the scores represent the true experience of patients, then how can we ever truly create a more satisfying experience for our patients?
I believe that the answer lies with empathy. What’s unique about this part of the Triple Aim is that many of the answers are within us. Gaining empathy with our patients requires us to ask questions of them and also to ask questions of ourselves. It requires us to invoke ancient methods of learning and thinking, like walking in another’s shoes for a day or using the Golden Rule. Experience doesn’t lend itself to being taught by PowerPoint. It must be lived and channeled back and out through our emotional selves as empathy.
Using the wisdom of patients themselves is one way to understand their needs and develop the empathy to motivate us to change how we do things in health care. Many organizations around the country have used some form of patient focus group to help learn from patients. Park Nicollet, a large health system in Minnesota, has incorporated family councils in nearly every clinic and care area. They usually are patients or caregivers from the area, bound together by a common disease or location. They dedicate their time, often meeting monthly, to share their stories, give opinions on care processes, and even to shape the design of a care area. Currently, there are more than 100 patient councils in the system, and the number continues to grow.
Film, when done skillfully, is a powerful tool in helping us gain empathy. The Cleveland Clinic has produced an amazing short film called “Empathy: The Human Connection to Patient Care.” It follows patients, families, and staff through the care system. As the camera focuses on each person, floating text appears near them, explaining their situation, inner thoughts, or fears, all overlaid by an emotional piano score. Tears will flow. Understanding follows.
Jim Merlino, MD, Cleveland Clinic’s chief experience officer, explains, “We need to understand that being on the other side of health care is frightening, and our job, our responsibility as people responsible for other people, is to help ease that fear.” Cleveland Clinic has done a remarkable job in reminding us why we went in to health care.
Morgan Spurlock of “Super Size Me” fame produced a reality series called “30 Days.” In each episode, a participant spent 30 days in the shoes of another. In the “Life in a Wheelchair” episode, Super Bowl-winning football player Ray Crockett lives in a wheelchair for 30 days and explores what it is like going through recovery and the healthcare system. He meets several rehabbing paraplegics and quadriplegics and accompanies them through their daily lives at home and the hospital. Viewers gain empathy directly in seeing these patients struggle to get better and work with the healthcare system. We also gain empathy watching Crockett gain empathy. The combination is powerful.
In Patients’ Shoes
In addition to listening and observation, we can begin to literally walk in the shoes of our patients.
I recently attended IHI’s International Forum in London. The National Health Service (NHS) in England is using a new tool to help providers understand what it is like for geriatric patients who must navigate the healthcare system with diminished senses and capabilities. Providers put on an age-simulation suit (www.age-simulation-suit.com) that mimics the impairments of aging. Special goggles fog the vision and narrow the visual field. Head mobility is reduced so that it becomes difficult to see beyond the field cuts. Earmuffs reduce high-frequency hearing and the ability to understand speech clearly. The overall suit impedes motion and reduces strength. Thick gloves make it difficult to coordinate fine motions. Wearing this suit and trying to go through a hospital or clinic setting instantly makes the wearer gain empathy for our patients’ needs.
Most important, be a patient. SHM immediate past president Shaun Frost, MD, SFHM, whose personal mission during his tenure was to help the society understand patient experience, explained it best to me. “In one episode in the hospital with a family member, I learned more about patient experience than all the reading and self-educating I have been doing for the last year.”
I think any of us who have been a patient in the hospital, or accompanied a loved one, comes out frustrated that the healthcare system is so convoluted and lacking in clarity for patients. Then there is often a sense of renewal, hopefully,followed by evangelism to spread their newfound empathy to others in the system.
In our busy work lives as hospitalists, it isn’t easy turning our daily focus away from efficiency and productivity. Yet we must always remain mindful of that core idea every one of us wrote down as the heart of our personal statements on our applications to medical school. Do you remember writing something like this? “I want to help people and relieve suffering in their time of need.”
Empathy is the start of our work.
Dr. Kealey is medical director of hospital specialties at HealthPartners Medical Group in St. Paul, Minn. He is an SHM board member and SHM president-elect.