User login
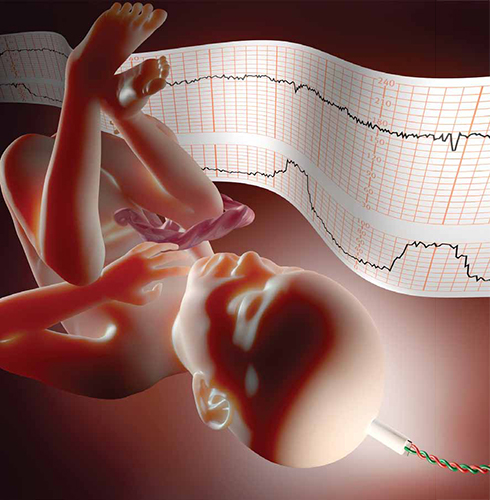
How can electronic fetal heart-rate monitoring best improve neonatal outcomes during induction of labor?
In this prospective cohort study of women undergoing induction of labor of a singleton fetus at term (≥37 weeks), Clark and colleagues examined each patient chart for adherence to 6 clinical practices:
- fetal weight estimated prior to induction
- clinical assessment of pelvic adequacy prior to induction
- completion of a safety checklist prior to induction
- completion of a safety checklist every 30 minutes during induction
- oxytocin infusion rate decreased if the fetal heart rate did not meet defined requirements
- oxytocin infusion rate decreased if uterine activity did not meet defined requirements.
Defined requirements for fetal heart rate included at least 1 acceleration of 15 bpm x 15 seconds in 30 minutes, or adequate variability for 10 of the previous 30 minutes. There should have been no more than 1 late deceleration in the previous 30 minutes. And there should have been no more than 2 variable decelerations exceeding 60 seconds and decreasing more than 60 bpm from baseline in the previous 30 minutes.
Defined requirements for uterine activity included no more than 5 contractions in 10 minutes for any 20-minute interval. There should have been no 2 contractions longer than 120 seconds in duration. In addition, the uterus should have been soft upon palpation between contractions. If an intrauterine pressure catheter was in place, measurement in Montevideo units should have been less than 300 mm Hg, with baseline resting tone of less than 25 mm Hg.
Outcome measures included admission to a neonatal intensive care unit (NICU), 1- and 5-minute Apgar scores of less than 7, and primary cesarean delivery.
Study findings underscore value of a checklist
The study found that completion of a safety checklist every 30 minutes during labor was associated with a significantly reduced rate of NICU admission and cesarean delivery. When the clinician stopped or reduced oxytocin for failure to meet specific uterine activity requirements, the rate of NICU admission also was reduced, but there were no differences in other outcomes. When the clinician stopped or reduced oxytocin for a failure to meet specific fetal heart-rate requirements, the rate of NICU admission was significantly reduced, as was the rate of low Apgar scores at birth, but there was a significantly higher rate of cesarean delivery (26.6% vs 17.5%).
Strengths include size of the study
This is a large study in a population with demographics that likely reflect those of the general US population. The study size permitted detection of relatively small differences in outcome.
The data clearly support the conclusions that “electronic fetal heart-rate monitoring improves neonatal outcomes when unambiguous definitions of abnormal fetal heart rate and tachysystole are coupled with specific interventions” and that “utilization of a checklist for oxytocin monitoring is associated with improved neonatal outcomes.” However, data were conflicting regarding the impact of a standard oxytocin checklist on the rate of cesarean delivery.
What this evidence means for practice
Implementation of a conservative intrapartum checklist has been shown to improve specific measures of newborn outcome. Further study is needed to define the impact on the rate of cesarean delivery.
—David A. Miller, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this prospective cohort study of women undergoing induction of labor of a singleton fetus at term (≥37 weeks), Clark and colleagues examined each patient chart for adherence to 6 clinical practices:
- fetal weight estimated prior to induction
- clinical assessment of pelvic adequacy prior to induction
- completion of a safety checklist prior to induction
- completion of a safety checklist every 30 minutes during induction
- oxytocin infusion rate decreased if the fetal heart rate did not meet defined requirements
- oxytocin infusion rate decreased if uterine activity did not meet defined requirements.
Defined requirements for fetal heart rate included at least 1 acceleration of 15 bpm x 15 seconds in 30 minutes, or adequate variability for 10 of the previous 30 minutes. There should have been no more than 1 late deceleration in the previous 30 minutes. And there should have been no more than 2 variable decelerations exceeding 60 seconds and decreasing more than 60 bpm from baseline in the previous 30 minutes.
Defined requirements for uterine activity included no more than 5 contractions in 10 minutes for any 20-minute interval. There should have been no 2 contractions longer than 120 seconds in duration. In addition, the uterus should have been soft upon palpation between contractions. If an intrauterine pressure catheter was in place, measurement in Montevideo units should have been less than 300 mm Hg, with baseline resting tone of less than 25 mm Hg.
Outcome measures included admission to a neonatal intensive care unit (NICU), 1- and 5-minute Apgar scores of less than 7, and primary cesarean delivery.
Study findings underscore value of a checklist
The study found that completion of a safety checklist every 30 minutes during labor was associated with a significantly reduced rate of NICU admission and cesarean delivery. When the clinician stopped or reduced oxytocin for failure to meet specific uterine activity requirements, the rate of NICU admission also was reduced, but there were no differences in other outcomes. When the clinician stopped or reduced oxytocin for a failure to meet specific fetal heart-rate requirements, the rate of NICU admission was significantly reduced, as was the rate of low Apgar scores at birth, but there was a significantly higher rate of cesarean delivery (26.6% vs 17.5%).
Strengths include size of the study
This is a large study in a population with demographics that likely reflect those of the general US population. The study size permitted detection of relatively small differences in outcome.
The data clearly support the conclusions that “electronic fetal heart-rate monitoring improves neonatal outcomes when unambiguous definitions of abnormal fetal heart rate and tachysystole are coupled with specific interventions” and that “utilization of a checklist for oxytocin monitoring is associated with improved neonatal outcomes.” However, data were conflicting regarding the impact of a standard oxytocin checklist on the rate of cesarean delivery.
What this evidence means for practice
Implementation of a conservative intrapartum checklist has been shown to improve specific measures of newborn outcome. Further study is needed to define the impact on the rate of cesarean delivery.
—David A. Miller, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this prospective cohort study of women undergoing induction of labor of a singleton fetus at term (≥37 weeks), Clark and colleagues examined each patient chart for adherence to 6 clinical practices:
- fetal weight estimated prior to induction
- clinical assessment of pelvic adequacy prior to induction
- completion of a safety checklist prior to induction
- completion of a safety checklist every 30 minutes during induction
- oxytocin infusion rate decreased if the fetal heart rate did not meet defined requirements
- oxytocin infusion rate decreased if uterine activity did not meet defined requirements.
Defined requirements for fetal heart rate included at least 1 acceleration of 15 bpm x 15 seconds in 30 minutes, or adequate variability for 10 of the previous 30 minutes. There should have been no more than 1 late deceleration in the previous 30 minutes. And there should have been no more than 2 variable decelerations exceeding 60 seconds and decreasing more than 60 bpm from baseline in the previous 30 minutes.
Defined requirements for uterine activity included no more than 5 contractions in 10 minutes for any 20-minute interval. There should have been no 2 contractions longer than 120 seconds in duration. In addition, the uterus should have been soft upon palpation between contractions. If an intrauterine pressure catheter was in place, measurement in Montevideo units should have been less than 300 mm Hg, with baseline resting tone of less than 25 mm Hg.
Outcome measures included admission to a neonatal intensive care unit (NICU), 1- and 5-minute Apgar scores of less than 7, and primary cesarean delivery.
Study findings underscore value of a checklist
The study found that completion of a safety checklist every 30 minutes during labor was associated with a significantly reduced rate of NICU admission and cesarean delivery. When the clinician stopped or reduced oxytocin for failure to meet specific uterine activity requirements, the rate of NICU admission also was reduced, but there were no differences in other outcomes. When the clinician stopped or reduced oxytocin for a failure to meet specific fetal heart-rate requirements, the rate of NICU admission was significantly reduced, as was the rate of low Apgar scores at birth, but there was a significantly higher rate of cesarean delivery (26.6% vs 17.5%).
Strengths include size of the study
This is a large study in a population with demographics that likely reflect those of the general US population. The study size permitted detection of relatively small differences in outcome.
The data clearly support the conclusions that “electronic fetal heart-rate monitoring improves neonatal outcomes when unambiguous definitions of abnormal fetal heart rate and tachysystole are coupled with specific interventions” and that “utilization of a checklist for oxytocin monitoring is associated with improved neonatal outcomes.” However, data were conflicting regarding the impact of a standard oxytocin checklist on the rate of cesarean delivery.
What this evidence means for practice
Implementation of a conservative intrapartum checklist has been shown to improve specific measures of newborn outcome. Further study is needed to define the impact on the rate of cesarean delivery.
—David A. Miller, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
A reasoned plan to manage a persistent Category-II FHR tracing
- Stop staring at that Category-II fetal heart-rate tracing…
Robert L. Barbieri, MD (Editorial, April 2011) - Guidelines on fetal monitoring aim to codify normal, abnormal FHR
Robert L. Barbieri, MD (Editorial, October 2008)
CASE An uncertain interlude during labor
An obstetrician checks on her laboring patient, only to discover that the fetal heart-rate (FHR) tracing has moved from Category I, a normal classification, into Category II—a gray zone. The OB decides to be proactive, not simply to wait for the tracing to return to normal. She has the patient move from a supine to a lateral position, provides oxygen, and administers a bolus of 500 to 1,000 mL of lactated Ringer’s solution over 20 minutes.
The tracing remains in Category II.
What should the OB do next?
When a fetal heart-rate tracing remains in Category II despite well-considered conservative corrective measures, a reasoned, rather than passive, approach is recommended.In 2008, the National Institute of Child Health and Human Development proposed a three-tier classification system for electronic FHR tracings (TABLE 1).1 Tracings in Category I are considered normal and can be managed routinely.1-3 Category-III tracings are considered abnormal and require additional attention; if corrective measures do not result in improvement, rapid delivery usually is warranted.1-3 Category II includes all FHR tracings that do not fit into either of the other categories. Because Category II encompasses such a wide range of FHR tracings, there are many options for management.
TABLE 1
3-tier fetal heart-rate classification system
| Category | Description |
|---|---|
| I | Fetal heart-rate (FHR) tracings include all of the following:
|
| II | Includes all FHR tracings not included in Category I or Category III |
| III | FHR tracings include:
|
| Source: Adapted from Macones GA, et al.1 | |
If the case described above sounds familiar, it may be that you read Editor in Chief Dr. Robert L. Barbieri’s editorial on Category-II FHR tracings in the April 2011 issue of OBG Management.4 That essay described a number of common conservative corrective measures applicable for Category-II tracings, including the three interventions the OB performed.
Other measures:
- reduce or stop infusion of oxytocin
- discontinue cervical ripening agents
- consider administering a tocolytic, such as terbutaline, if tachysystole is present or if uterine contractions are prolonged or coupled
- consider the option of amnioinfusion if variable decelerations are present.4,5
Systematic review of the oxygen pathway, from the environment to the fetus (maternal lungs, heart, vasculature, uterus, placenta, and umbilical cord), can facilitate recollection of all of these measures. In addition, a simplified “A-B-C-D” approach to the management of a Category-II FHR tracing is helpful (TABLES 2 and 3):
- Assess the oxygen pathway
- Begin conservative corrective measures
- Clear obstacles to rapid delivery
- Determine decision-to-delivery time.6,7
TABLE 2
Conservative corrective measures to improve fetal oxygenation
| “A” Assess oxygen pathway | “B” Begin corrective measures if indicated | |
|---|---|---|
| Lungs | Airway and breathing | Supplemental oxygen (10 L) using a tight-fitting, non-rebreather face mask for at least 15 minutes |
| Heart | Heart rate and rhythm | Position changes IV fluid bolus (500–1,000 cc of isotonic fluid over 20 min) Correct hypotension |
| Vasculature | Blood pressure Volume status | |
| Uterus | Contraction strength Contraction frequency Baseline uterine tone Exclude uterine rupture | Stop or reduce uterine stimulants (oxytocin, prostaglandin) Consider uterine relaxant (terbutaline) |
| Placenta | Placental separation Bleeding vasa previa | |
| Cord | Vaginal exam Exclude cord prolapse | Consider amnioinfusion |
| Courtesy of David A. Miller, MD | ||
As the obstetrician in the opening scenario knows all too well, conservative corrective measures do not always transform FHR tracings from Category II to Category I. In fact, it is extremely common for a Category-II tracing to remain in Category II despite every conservative corrective measure in the book. This article presents a practical, systematic, standardized approach to the management of a persistent Category-II FHR tracing.
TABLE 3
Steps involved in preparing for delivery
| “C” Clear obstacles to rapid delivery | “D” Determine decision-to-delivery time | |
|---|---|---|
| Facility | Operating room availability Equipment | Facility response time |
| Staff | Notify: Obstetrician Surgical assistant Anesthesiologist Neonatologist Pediatrician Nursing staff | Consider staff: Availability Training Experience |
| Mother | Informed consent Anesthesia options Laboratory tests Blood products Intravenous access Urinary catheter Abdominal prep Transfer to OR | Surgical considerations (prior abdominal or uterine surgery) Medical considerations (obesity, hypertension, diabetes, SLE) Obstetric considerations (parity, pelvimetry, placental location) |
| Fetus | Confirm: Estimated fetal weight Gestational age Presentation Position | Consider factors such as: Estimated fetal weight Gestational age Presentation Position |
| Labor | Confirm adequate monitoring of uterine contractions | Consider factors such as: Arrest disorder Protracted labor Remote from delivery Poor expulsive efforts |
| Courtesy of David A. Miller, MD | ||
CASE Continued
When the OB’s preliminary interventions fail to nudge the FHR tracing back to Category I, she stops oxytocin and administers terbutaline. She even tries amnioinfusion. Still, the FHR tracing remains in Category II.
“What now?,” she wonders.
If conservative measures do not correct the FHR tracing to the satisfaction of the clinician, it is prudent to plan ahead for the possible need for rapid delivery. In a standardized “A-B-C-D” approach to FHR management, the next step is “C”: Clear obstacles to rapid delivery. This step does not constitute a commitment to a particular time or method of delivery. It simply serves as a reminder of common sources of unnecessary delay so that they can be addressed in a standardized, timely manner (FIGURE).

Decision model for management of intrapartum fetal heart rate (FHR)Standardization has long been recognized as an essential element of patient safety, and a growing body of contemporary evidence confirms that standardization can reduce adverse outcomes and malpractice claims.8-10 In FHR monitoring, standardization can help ensure that common obstacles to rapid delivery are not overlooked and that decisions are made in a timely fashion. TABLE 3 identifies common obstacles to rapid delivery, groups them in five major categories, and organizes them in non-random order. From largest to smallest, these categories include the facility, staff, mother, fetus, and labor.
Because many of these examples are viewed by clinicians as “common sense,” they do not always receive the serious, systematic attention they deserve. Instead, they are often left to the vagaries of random recall and are frequently overlooked, jeopardizing patient safety and inviting criticism. An easy way to minimize the error inherent in random recall is to use a simple checklist and to post it in a conspicuous location on the labor-and-delivery unit.
Next step: “D” – Determine the decision-to-delivery time
After appropriate conservative measures have been implemented and obstacles to rapid delivery have been cleared away, it is sensible to take a moment to estimate the time needed to accomplish delivery in the event of a sudden emergency. This step should be addressed by the clinician who is ultimately responsible for performing operative delivery, should it become necessary. The time between decision and delivery can be estimated systematically by considering individual characteristics of the facility, staff, mother, fetus, and labor. TABLE 3 summarizes examples of factors that can have an impact on this estimate.
Clinical judgment is required
Management steps A, B, C, and D are relatively uncontroversial, readily amenable to standardization, and represent the overwhelming majority of decisions that must be made during labor. These steps do not replace clinical judgment. On the contrary, they encourage the systematic, timely application of clinical judgment.
However, if the FHR tracing has not returned to Category I by the time A, B, C, and D are completed, the clinician must make a decision about whether to continue to wait for spontaneous vaginal delivery or to expedite delivery by other means. This decision balances the estimated time until vaginal delivery against the estimated time until the onset of metabolic acidemia and potential injury.
The estimate of the time until vaginal delivery is guided by the usual obstetric considerations, including the three “P’s”:
- Power – uterine contractions
- Passenger – the fetus
- Passage – the pelvis.
The estimate of the time until the onset of metabolic acidemia and potential injury is guided by limited data suggesting that metabolic acidemia usually does not appear suddenly, but can evolve gradually over a period of approximately 60 minutes.15 This general statement applies only to FHR tracings that are normal initially and subsequently develop minimal to absent variability with recurrent decelerations and no acute events.15 It does not constitute a “safe harbor.”
The inherent imprecision of these estimates can make the decision difficult. One of the most common preventable errors at this stage of FHR management is to postpone a difficult but clinically necessary decision in the hope that the situation will resolve on its own. Despite the difficulty, the standard of care mandates that a decision must be made using the best information available.
If a decision is made to expedite delivery, the rationale should be documented, and the plan should be implemented as rapidly and safely as feasible. If a decision is made to continue to wait, the rationale and plan should be documented, and the decision should be revisited after a reasonable period of time, usually in the range of 5 to 15 minutes in the second stage of labor.
“Deciding to wait” is distinctly different from “waiting to decide.” The former reflects the timely application of clinical judgment; the latter suggests procrastination.
CASE Resolved
The OB evaluates the patient again. The FHR tracing remains in Category II. The baseline rate is 150 bpm, variability is moderate, accelerations are present, and there are variable decelerations with every other contraction. The cervix remains dilated to 6 cm despite more than 2 hours of adequate contractions. Secondary arrest of dilatation is diagnosed, and cesarean delivery is recommended. Shortly thereafter, a vigorous baby is born. As the presence of moderate variability and accelerations predicted, the 5-minute Apgar score is normal. Assessment of the umbilical artery blood gas confirms the absence of metabolic acidemia, and the newborn course is uneventful.
The paradox of FHR monitoring
The greatest strength of intrapartum FHR monitoring is the ability of moderate variability or accelerations, or both, to predict normal neurologic outcome with an extremely high degree of reliability.1,11,12 One of the greatest weaknesses of FHR monitoring is the inability of an “abnormal” tracing to predict abnormal neurologic outcome with any clinically relevant degree of accuracy. The false-positive rate of FHR monitoring for predicting cerebral palsy has been reported to exceed 99%, yielding a positive predictive value of less than 1%.1,13 This imprecision is explained in part by the relative rarity of intrapartum hypoxic neurologic injury, and in part by the mitigating interventions that are frequently prompted by FHR “abnormalities.”14 However, these explanations do not alter the fact that the positive predictive value of intrapartum FHR monitoring, as it is used in actual clinical practice, is essentially zero.
Reasonable management decisions simply cannot be based on the results of a test that is virtually always wrong. On the other hand, the negative predictive value of intrapartum FHR monitoring is nearly 100%. A test that is virtually always right is the ideal foundation for rational decision-making.
Standardization of intrapartum FHR monitoring promotes safety by reducing unnecessary complexity and minimizing the error inherent in random recall. However, the technology can achieve its potential only if it is used appropriately. Trying to use intrapartum FHR monitoring to diagnose neurologic injury is a recipe for failure. In contrast, relying on the presence of moderate variability or accelerations, or both, to confirm adequate fetal oxygenation allows the clinician to formulate and articulate a rational, evidence-based plan of management that reflects consensus in the literature.
We want to hear from you! Tell us what you think.
1. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions interpretation, and research guidelines. Obstet Gynecol. 2008;112(3):661-666.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin number 106: Intrapartum fetal heart rate monitoring: nomenclature interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192-202.
3. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116(5):1232-1240.
4. Barbieri RL. Stop staring at that Category-II fetal heart-rate tracing…and do something instead to improve fetal status! OBG Manage. 2011;23(4):6-9.
5. Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005;105(6):1362-1368.
6. Miller DA. Intrapartum fetal heart rate definitions and interpretation: evolving consensus. Clin Obstet Gynecol. 2011;54(1):16-21.
7. Miller DA. Intrapartum fetal heart monitoring: a standardized approach to management. Clin Obstet Gynecol. 2011;54(1):22-27.
8. To Err is Human: Building a Safer Health System. Kohn LT Corrigan JM, Donaldson MS, eds. Committee on Quality of Health Care in America. Institute of Medicine. Washington, DC: National Academy of Sciences;1999:14.
9. Pettker CM, Thung SF, Norwitz ER, et al. Impact of a comprehensive patient safety strategy on obstetric adverse events. Am J Obstet Gynecol. 2009;200(5):492.e1-8.
10. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
11. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ. 1999;319(7216):1054-1059.
12. American College of Obstetricians and Gynecologists. Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology. Washington DC: American College of Obstetricians and Gynecologists; 2003.
13. Nelson KB, Dambrosia JM, Ting TY, Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med. 1996;334(10):613-618.
14. Freeman RK, Nageotte MP. Comments on American College of Obstetricians and Gynecologists Practice Bulletin No. 106. Am J Obstet Gynecol. 2010;202(5):411-412.
15. Parer JT, King T, Flanders S, Fox M, Kilpatrick SJ. Fetal acidemia and electronic fetal heart rate patterns: is there evidence of an association? J Matern Fetal Neonatal Med. 2006;19(5):289-294.
- Stop staring at that Category-II fetal heart-rate tracing…
Robert L. Barbieri, MD (Editorial, April 2011) - Guidelines on fetal monitoring aim to codify normal, abnormal FHR
Robert L. Barbieri, MD (Editorial, October 2008)
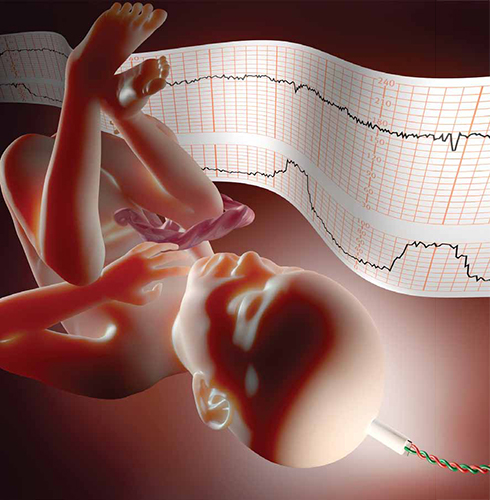
CASE An uncertain interlude during labor
An obstetrician checks on her laboring patient, only to discover that the fetal heart-rate (FHR) tracing has moved from Category I, a normal classification, into Category II—a gray zone. The OB decides to be proactive, not simply to wait for the tracing to return to normal. She has the patient move from a supine to a lateral position, provides oxygen, and administers a bolus of 500 to 1,000 mL of lactated Ringer’s solution over 20 minutes.
The tracing remains in Category II.
What should the OB do next?
When a fetal heart-rate tracing remains in Category II despite well-considered conservative corrective measures, a reasoned, rather than passive, approach is recommended.In 2008, the National Institute of Child Health and Human Development proposed a three-tier classification system for electronic FHR tracings (TABLE 1).1 Tracings in Category I are considered normal and can be managed routinely.1-3 Category-III tracings are considered abnormal and require additional attention; if corrective measures do not result in improvement, rapid delivery usually is warranted.1-3 Category II includes all FHR tracings that do not fit into either of the other categories. Because Category II encompasses such a wide range of FHR tracings, there are many options for management.
TABLE 1
3-tier fetal heart-rate classification system
| Category | Description |
|---|---|
| I | Fetal heart-rate (FHR) tracings include all of the following:
|
| II | Includes all FHR tracings not included in Category I or Category III |
| III | FHR tracings include:
|
| Source: Adapted from Macones GA, et al.1 | |
If the case described above sounds familiar, it may be that you read Editor in Chief Dr. Robert L. Barbieri’s editorial on Category-II FHR tracings in the April 2011 issue of OBG Management.4 That essay described a number of common conservative corrective measures applicable for Category-II tracings, including the three interventions the OB performed.
Other measures:
- reduce or stop infusion of oxytocin
- discontinue cervical ripening agents
- consider administering a tocolytic, such as terbutaline, if tachysystole is present or if uterine contractions are prolonged or coupled
- consider the option of amnioinfusion if variable decelerations are present.4,5
Systematic review of the oxygen pathway, from the environment to the fetus (maternal lungs, heart, vasculature, uterus, placenta, and umbilical cord), can facilitate recollection of all of these measures. In addition, a simplified “A-B-C-D” approach to the management of a Category-II FHR tracing is helpful (TABLES 2 and 3):
- Assess the oxygen pathway
- Begin conservative corrective measures
- Clear obstacles to rapid delivery
- Determine decision-to-delivery time.6,7
TABLE 2
Conservative corrective measures to improve fetal oxygenation
| “A” Assess oxygen pathway | “B” Begin corrective measures if indicated | |
|---|---|---|
| Lungs | Airway and breathing | Supplemental oxygen (10 L) using a tight-fitting, non-rebreather face mask for at least 15 minutes |
| Heart | Heart rate and rhythm | Position changes IV fluid bolus (500–1,000 cc of isotonic fluid over 20 min) Correct hypotension |
| Vasculature | Blood pressure Volume status | |
| Uterus | Contraction strength Contraction frequency Baseline uterine tone Exclude uterine rupture | Stop or reduce uterine stimulants (oxytocin, prostaglandin) Consider uterine relaxant (terbutaline) |
| Placenta | Placental separation Bleeding vasa previa | |
| Cord | Vaginal exam Exclude cord prolapse | Consider amnioinfusion |
| Courtesy of David A. Miller, MD | ||
As the obstetrician in the opening scenario knows all too well, conservative corrective measures do not always transform FHR tracings from Category II to Category I. In fact, it is extremely common for a Category-II tracing to remain in Category II despite every conservative corrective measure in the book. This article presents a practical, systematic, standardized approach to the management of a persistent Category-II FHR tracing.
TABLE 3
Steps involved in preparing for delivery
| “C” Clear obstacles to rapid delivery | “D” Determine decision-to-delivery time | |
|---|---|---|
| Facility | Operating room availability Equipment | Facility response time |
| Staff | Notify: Obstetrician Surgical assistant Anesthesiologist Neonatologist Pediatrician Nursing staff | Consider staff: Availability Training Experience |
| Mother | Informed consent Anesthesia options Laboratory tests Blood products Intravenous access Urinary catheter Abdominal prep Transfer to OR | Surgical considerations (prior abdominal or uterine surgery) Medical considerations (obesity, hypertension, diabetes, SLE) Obstetric considerations (parity, pelvimetry, placental location) |
| Fetus | Confirm: Estimated fetal weight Gestational age Presentation Position | Consider factors such as: Estimated fetal weight Gestational age Presentation Position |
| Labor | Confirm adequate monitoring of uterine contractions | Consider factors such as: Arrest disorder Protracted labor Remote from delivery Poor expulsive efforts |
| Courtesy of David A. Miller, MD | ||
CASE Continued
When the OB’s preliminary interventions fail to nudge the FHR tracing back to Category I, she stops oxytocin and administers terbutaline. She even tries amnioinfusion. Still, the FHR tracing remains in Category II.
“What now?,” she wonders.
If conservative measures do not correct the FHR tracing to the satisfaction of the clinician, it is prudent to plan ahead for the possible need for rapid delivery. In a standardized “A-B-C-D” approach to FHR management, the next step is “C”: Clear obstacles to rapid delivery. This step does not constitute a commitment to a particular time or method of delivery. It simply serves as a reminder of common sources of unnecessary delay so that they can be addressed in a standardized, timely manner (FIGURE).

Decision model for management of intrapartum fetal heart rate (FHR)Standardization has long been recognized as an essential element of patient safety, and a growing body of contemporary evidence confirms that standardization can reduce adverse outcomes and malpractice claims.8-10 In FHR monitoring, standardization can help ensure that common obstacles to rapid delivery are not overlooked and that decisions are made in a timely fashion. TABLE 3 identifies common obstacles to rapid delivery, groups them in five major categories, and organizes them in non-random order. From largest to smallest, these categories include the facility, staff, mother, fetus, and labor.
Because many of these examples are viewed by clinicians as “common sense,” they do not always receive the serious, systematic attention they deserve. Instead, they are often left to the vagaries of random recall and are frequently overlooked, jeopardizing patient safety and inviting criticism. An easy way to minimize the error inherent in random recall is to use a simple checklist and to post it in a conspicuous location on the labor-and-delivery unit.
Next step: “D” – Determine the decision-to-delivery time
After appropriate conservative measures have been implemented and obstacles to rapid delivery have been cleared away, it is sensible to take a moment to estimate the time needed to accomplish delivery in the event of a sudden emergency. This step should be addressed by the clinician who is ultimately responsible for performing operative delivery, should it become necessary. The time between decision and delivery can be estimated systematically by considering individual characteristics of the facility, staff, mother, fetus, and labor. TABLE 3 summarizes examples of factors that can have an impact on this estimate.
Clinical judgment is required
Management steps A, B, C, and D are relatively uncontroversial, readily amenable to standardization, and represent the overwhelming majority of decisions that must be made during labor. These steps do not replace clinical judgment. On the contrary, they encourage the systematic, timely application of clinical judgment.
However, if the FHR tracing has not returned to Category I by the time A, B, C, and D are completed, the clinician must make a decision about whether to continue to wait for spontaneous vaginal delivery or to expedite delivery by other means. This decision balances the estimated time until vaginal delivery against the estimated time until the onset of metabolic acidemia and potential injury.
The estimate of the time until vaginal delivery is guided by the usual obstetric considerations, including the three “P’s”:
- Power – uterine contractions
- Passenger – the fetus
- Passage – the pelvis.
The estimate of the time until the onset of metabolic acidemia and potential injury is guided by limited data suggesting that metabolic acidemia usually does not appear suddenly, but can evolve gradually over a period of approximately 60 minutes.15 This general statement applies only to FHR tracings that are normal initially and subsequently develop minimal to absent variability with recurrent decelerations and no acute events.15 It does not constitute a “safe harbor.”
The inherent imprecision of these estimates can make the decision difficult. One of the most common preventable errors at this stage of FHR management is to postpone a difficult but clinically necessary decision in the hope that the situation will resolve on its own. Despite the difficulty, the standard of care mandates that a decision must be made using the best information available.
If a decision is made to expedite delivery, the rationale should be documented, and the plan should be implemented as rapidly and safely as feasible. If a decision is made to continue to wait, the rationale and plan should be documented, and the decision should be revisited after a reasonable period of time, usually in the range of 5 to 15 minutes in the second stage of labor.
“Deciding to wait” is distinctly different from “waiting to decide.” The former reflects the timely application of clinical judgment; the latter suggests procrastination.
CASE Resolved
The OB evaluates the patient again. The FHR tracing remains in Category II. The baseline rate is 150 bpm, variability is moderate, accelerations are present, and there are variable decelerations with every other contraction. The cervix remains dilated to 6 cm despite more than 2 hours of adequate contractions. Secondary arrest of dilatation is diagnosed, and cesarean delivery is recommended. Shortly thereafter, a vigorous baby is born. As the presence of moderate variability and accelerations predicted, the 5-minute Apgar score is normal. Assessment of the umbilical artery blood gas confirms the absence of metabolic acidemia, and the newborn course is uneventful.
The paradox of FHR monitoring
The greatest strength of intrapartum FHR monitoring is the ability of moderate variability or accelerations, or both, to predict normal neurologic outcome with an extremely high degree of reliability.1,11,12 One of the greatest weaknesses of FHR monitoring is the inability of an “abnormal” tracing to predict abnormal neurologic outcome with any clinically relevant degree of accuracy. The false-positive rate of FHR monitoring for predicting cerebral palsy has been reported to exceed 99%, yielding a positive predictive value of less than 1%.1,13 This imprecision is explained in part by the relative rarity of intrapartum hypoxic neurologic injury, and in part by the mitigating interventions that are frequently prompted by FHR “abnormalities.”14 However, these explanations do not alter the fact that the positive predictive value of intrapartum FHR monitoring, as it is used in actual clinical practice, is essentially zero.
Reasonable management decisions simply cannot be based on the results of a test that is virtually always wrong. On the other hand, the negative predictive value of intrapartum FHR monitoring is nearly 100%. A test that is virtually always right is the ideal foundation for rational decision-making.
Standardization of intrapartum FHR monitoring promotes safety by reducing unnecessary complexity and minimizing the error inherent in random recall. However, the technology can achieve its potential only if it is used appropriately. Trying to use intrapartum FHR monitoring to diagnose neurologic injury is a recipe for failure. In contrast, relying on the presence of moderate variability or accelerations, or both, to confirm adequate fetal oxygenation allows the clinician to formulate and articulate a rational, evidence-based plan of management that reflects consensus in the literature.
We want to hear from you! Tell us what you think.
- Stop staring at that Category-II fetal heart-rate tracing…
Robert L. Barbieri, MD (Editorial, April 2011) - Guidelines on fetal monitoring aim to codify normal, abnormal FHR
Robert L. Barbieri, MD (Editorial, October 2008)
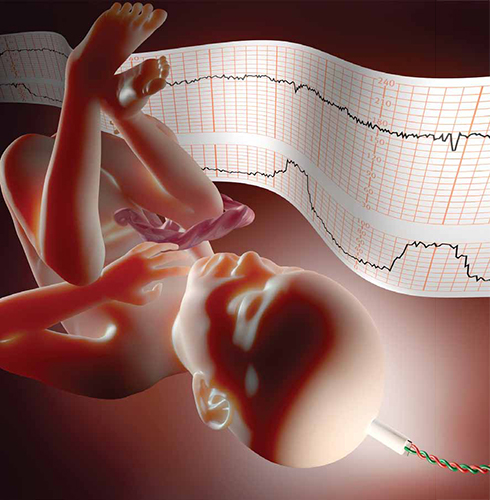
CASE An uncertain interlude during labor
An obstetrician checks on her laboring patient, only to discover that the fetal heart-rate (FHR) tracing has moved from Category I, a normal classification, into Category II—a gray zone. The OB decides to be proactive, not simply to wait for the tracing to return to normal. She has the patient move from a supine to a lateral position, provides oxygen, and administers a bolus of 500 to 1,000 mL of lactated Ringer’s solution over 20 minutes.
The tracing remains in Category II.
What should the OB do next?
When a fetal heart-rate tracing remains in Category II despite well-considered conservative corrective measures, a reasoned, rather than passive, approach is recommended.In 2008, the National Institute of Child Health and Human Development proposed a three-tier classification system for electronic FHR tracings (TABLE 1).1 Tracings in Category I are considered normal and can be managed routinely.1-3 Category-III tracings are considered abnormal and require additional attention; if corrective measures do not result in improvement, rapid delivery usually is warranted.1-3 Category II includes all FHR tracings that do not fit into either of the other categories. Because Category II encompasses such a wide range of FHR tracings, there are many options for management.
TABLE 1
3-tier fetal heart-rate classification system
| Category | Description |
|---|---|
| I | Fetal heart-rate (FHR) tracings include all of the following:
|
| II | Includes all FHR tracings not included in Category I or Category III |
| III | FHR tracings include:
|
| Source: Adapted from Macones GA, et al.1 | |
If the case described above sounds familiar, it may be that you read Editor in Chief Dr. Robert L. Barbieri’s editorial on Category-II FHR tracings in the April 2011 issue of OBG Management.4 That essay described a number of common conservative corrective measures applicable for Category-II tracings, including the three interventions the OB performed.
Other measures:
- reduce or stop infusion of oxytocin
- discontinue cervical ripening agents
- consider administering a tocolytic, such as terbutaline, if tachysystole is present or if uterine contractions are prolonged or coupled
- consider the option of amnioinfusion if variable decelerations are present.4,5
Systematic review of the oxygen pathway, from the environment to the fetus (maternal lungs, heart, vasculature, uterus, placenta, and umbilical cord), can facilitate recollection of all of these measures. In addition, a simplified “A-B-C-D” approach to the management of a Category-II FHR tracing is helpful (TABLES 2 and 3):
- Assess the oxygen pathway
- Begin conservative corrective measures
- Clear obstacles to rapid delivery
- Determine decision-to-delivery time.6,7
TABLE 2
Conservative corrective measures to improve fetal oxygenation
| “A” Assess oxygen pathway | “B” Begin corrective measures if indicated | |
|---|---|---|
| Lungs | Airway and breathing | Supplemental oxygen (10 L) using a tight-fitting, non-rebreather face mask for at least 15 minutes |
| Heart | Heart rate and rhythm | Position changes IV fluid bolus (500–1,000 cc of isotonic fluid over 20 min) Correct hypotension |
| Vasculature | Blood pressure Volume status | |
| Uterus | Contraction strength Contraction frequency Baseline uterine tone Exclude uterine rupture | Stop or reduce uterine stimulants (oxytocin, prostaglandin) Consider uterine relaxant (terbutaline) |
| Placenta | Placental separation Bleeding vasa previa | |
| Cord | Vaginal exam Exclude cord prolapse | Consider amnioinfusion |
| Courtesy of David A. Miller, MD | ||
As the obstetrician in the opening scenario knows all too well, conservative corrective measures do not always transform FHR tracings from Category II to Category I. In fact, it is extremely common for a Category-II tracing to remain in Category II despite every conservative corrective measure in the book. This article presents a practical, systematic, standardized approach to the management of a persistent Category-II FHR tracing.
TABLE 3
Steps involved in preparing for delivery
| “C” Clear obstacles to rapid delivery | “D” Determine decision-to-delivery time | |
|---|---|---|
| Facility | Operating room availability Equipment | Facility response time |
| Staff | Notify: Obstetrician Surgical assistant Anesthesiologist Neonatologist Pediatrician Nursing staff | Consider staff: Availability Training Experience |
| Mother | Informed consent Anesthesia options Laboratory tests Blood products Intravenous access Urinary catheter Abdominal prep Transfer to OR | Surgical considerations (prior abdominal or uterine surgery) Medical considerations (obesity, hypertension, diabetes, SLE) Obstetric considerations (parity, pelvimetry, placental location) |
| Fetus | Confirm: Estimated fetal weight Gestational age Presentation Position | Consider factors such as: Estimated fetal weight Gestational age Presentation Position |
| Labor | Confirm adequate monitoring of uterine contractions | Consider factors such as: Arrest disorder Protracted labor Remote from delivery Poor expulsive efforts |
| Courtesy of David A. Miller, MD | ||
CASE Continued
When the OB’s preliminary interventions fail to nudge the FHR tracing back to Category I, she stops oxytocin and administers terbutaline. She even tries amnioinfusion. Still, the FHR tracing remains in Category II.
“What now?,” she wonders.
If conservative measures do not correct the FHR tracing to the satisfaction of the clinician, it is prudent to plan ahead for the possible need for rapid delivery. In a standardized “A-B-C-D” approach to FHR management, the next step is “C”: Clear obstacles to rapid delivery. This step does not constitute a commitment to a particular time or method of delivery. It simply serves as a reminder of common sources of unnecessary delay so that they can be addressed in a standardized, timely manner (FIGURE).

Decision model for management of intrapartum fetal heart rate (FHR)Standardization has long been recognized as an essential element of patient safety, and a growing body of contemporary evidence confirms that standardization can reduce adverse outcomes and malpractice claims.8-10 In FHR monitoring, standardization can help ensure that common obstacles to rapid delivery are not overlooked and that decisions are made in a timely fashion. TABLE 3 identifies common obstacles to rapid delivery, groups them in five major categories, and organizes them in non-random order. From largest to smallest, these categories include the facility, staff, mother, fetus, and labor.
Because many of these examples are viewed by clinicians as “common sense,” they do not always receive the serious, systematic attention they deserve. Instead, they are often left to the vagaries of random recall and are frequently overlooked, jeopardizing patient safety and inviting criticism. An easy way to minimize the error inherent in random recall is to use a simple checklist and to post it in a conspicuous location on the labor-and-delivery unit.
Next step: “D” – Determine the decision-to-delivery time
After appropriate conservative measures have been implemented and obstacles to rapid delivery have been cleared away, it is sensible to take a moment to estimate the time needed to accomplish delivery in the event of a sudden emergency. This step should be addressed by the clinician who is ultimately responsible for performing operative delivery, should it become necessary. The time between decision and delivery can be estimated systematically by considering individual characteristics of the facility, staff, mother, fetus, and labor. TABLE 3 summarizes examples of factors that can have an impact on this estimate.
Clinical judgment is required
Management steps A, B, C, and D are relatively uncontroversial, readily amenable to standardization, and represent the overwhelming majority of decisions that must be made during labor. These steps do not replace clinical judgment. On the contrary, they encourage the systematic, timely application of clinical judgment.
However, if the FHR tracing has not returned to Category I by the time A, B, C, and D are completed, the clinician must make a decision about whether to continue to wait for spontaneous vaginal delivery or to expedite delivery by other means. This decision balances the estimated time until vaginal delivery against the estimated time until the onset of metabolic acidemia and potential injury.
The estimate of the time until vaginal delivery is guided by the usual obstetric considerations, including the three “P’s”:
- Power – uterine contractions
- Passenger – the fetus
- Passage – the pelvis.
The estimate of the time until the onset of metabolic acidemia and potential injury is guided by limited data suggesting that metabolic acidemia usually does not appear suddenly, but can evolve gradually over a period of approximately 60 minutes.15 This general statement applies only to FHR tracings that are normal initially and subsequently develop minimal to absent variability with recurrent decelerations and no acute events.15 It does not constitute a “safe harbor.”
The inherent imprecision of these estimates can make the decision difficult. One of the most common preventable errors at this stage of FHR management is to postpone a difficult but clinically necessary decision in the hope that the situation will resolve on its own. Despite the difficulty, the standard of care mandates that a decision must be made using the best information available.
If a decision is made to expedite delivery, the rationale should be documented, and the plan should be implemented as rapidly and safely as feasible. If a decision is made to continue to wait, the rationale and plan should be documented, and the decision should be revisited after a reasonable period of time, usually in the range of 5 to 15 minutes in the second stage of labor.
“Deciding to wait” is distinctly different from “waiting to decide.” The former reflects the timely application of clinical judgment; the latter suggests procrastination.
CASE Resolved
The OB evaluates the patient again. The FHR tracing remains in Category II. The baseline rate is 150 bpm, variability is moderate, accelerations are present, and there are variable decelerations with every other contraction. The cervix remains dilated to 6 cm despite more than 2 hours of adequate contractions. Secondary arrest of dilatation is diagnosed, and cesarean delivery is recommended. Shortly thereafter, a vigorous baby is born. As the presence of moderate variability and accelerations predicted, the 5-minute Apgar score is normal. Assessment of the umbilical artery blood gas confirms the absence of metabolic acidemia, and the newborn course is uneventful.
The paradox of FHR monitoring
The greatest strength of intrapartum FHR monitoring is the ability of moderate variability or accelerations, or both, to predict normal neurologic outcome with an extremely high degree of reliability.1,11,12 One of the greatest weaknesses of FHR monitoring is the inability of an “abnormal” tracing to predict abnormal neurologic outcome with any clinically relevant degree of accuracy. The false-positive rate of FHR monitoring for predicting cerebral palsy has been reported to exceed 99%, yielding a positive predictive value of less than 1%.1,13 This imprecision is explained in part by the relative rarity of intrapartum hypoxic neurologic injury, and in part by the mitigating interventions that are frequently prompted by FHR “abnormalities.”14 However, these explanations do not alter the fact that the positive predictive value of intrapartum FHR monitoring, as it is used in actual clinical practice, is essentially zero.
Reasonable management decisions simply cannot be based on the results of a test that is virtually always wrong. On the other hand, the negative predictive value of intrapartum FHR monitoring is nearly 100%. A test that is virtually always right is the ideal foundation for rational decision-making.
Standardization of intrapartum FHR monitoring promotes safety by reducing unnecessary complexity and minimizing the error inherent in random recall. However, the technology can achieve its potential only if it is used appropriately. Trying to use intrapartum FHR monitoring to diagnose neurologic injury is a recipe for failure. In contrast, relying on the presence of moderate variability or accelerations, or both, to confirm adequate fetal oxygenation allows the clinician to formulate and articulate a rational, evidence-based plan of management that reflects consensus in the literature.
We want to hear from you! Tell us what you think.
1. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions interpretation, and research guidelines. Obstet Gynecol. 2008;112(3):661-666.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin number 106: Intrapartum fetal heart rate monitoring: nomenclature interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192-202.
3. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116(5):1232-1240.
4. Barbieri RL. Stop staring at that Category-II fetal heart-rate tracing…and do something instead to improve fetal status! OBG Manage. 2011;23(4):6-9.
5. Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005;105(6):1362-1368.
6. Miller DA. Intrapartum fetal heart rate definitions and interpretation: evolving consensus. Clin Obstet Gynecol. 2011;54(1):16-21.
7. Miller DA. Intrapartum fetal heart monitoring: a standardized approach to management. Clin Obstet Gynecol. 2011;54(1):22-27.
8. To Err is Human: Building a Safer Health System. Kohn LT Corrigan JM, Donaldson MS, eds. Committee on Quality of Health Care in America. Institute of Medicine. Washington, DC: National Academy of Sciences;1999:14.
9. Pettker CM, Thung SF, Norwitz ER, et al. Impact of a comprehensive patient safety strategy on obstetric adverse events. Am J Obstet Gynecol. 2009;200(5):492.e1-8.
10. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
11. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ. 1999;319(7216):1054-1059.
12. American College of Obstetricians and Gynecologists. Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology. Washington DC: American College of Obstetricians and Gynecologists; 2003.
13. Nelson KB, Dambrosia JM, Ting TY, Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med. 1996;334(10):613-618.
14. Freeman RK, Nageotte MP. Comments on American College of Obstetricians and Gynecologists Practice Bulletin No. 106. Am J Obstet Gynecol. 2010;202(5):411-412.
15. Parer JT, King T, Flanders S, Fox M, Kilpatrick SJ. Fetal acidemia and electronic fetal heart rate patterns: is there evidence of an association? J Matern Fetal Neonatal Med. 2006;19(5):289-294.
1. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions interpretation, and research guidelines. Obstet Gynecol. 2008;112(3):661-666.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin number 106: Intrapartum fetal heart rate monitoring: nomenclature interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192-202.
3. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116(5):1232-1240.
4. Barbieri RL. Stop staring at that Category-II fetal heart-rate tracing…and do something instead to improve fetal status! OBG Manage. 2011;23(4):6-9.
5. Simpson KR, James DC. Efficacy of intrauterine resuscitation techniques in improving fetal oxygen status during labor. Obstet Gynecol. 2005;105(6):1362-1368.
6. Miller DA. Intrapartum fetal heart rate definitions and interpretation: evolving consensus. Clin Obstet Gynecol. 2011;54(1):16-21.
7. Miller DA. Intrapartum fetal heart monitoring: a standardized approach to management. Clin Obstet Gynecol. 2011;54(1):22-27.
8. To Err is Human: Building a Safer Health System. Kohn LT Corrigan JM, Donaldson MS, eds. Committee on Quality of Health Care in America. Institute of Medicine. Washington, DC: National Academy of Sciences;1999:14.
9. Pettker CM, Thung SF, Norwitz ER, et al. Impact of a comprehensive patient safety strategy on obstetric adverse events. Am J Obstet Gynecol. 2009;200(5):492.e1-8.
10. Clark SL, Belfort MA, Dildy GA, Meyers JA. Reducing obstetric litigation through alterations in practice patterns. Obstet Gynecol. 2008;112(6):1279-1283.
11. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ. 1999;319(7216):1054-1059.
12. American College of Obstetricians and Gynecologists. Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology. Washington DC: American College of Obstetricians and Gynecologists; 2003.
13. Nelson KB, Dambrosia JM, Ting TY, Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med. 1996;334(10):613-618.
14. Freeman RK, Nageotte MP. Comments on American College of Obstetricians and Gynecologists Practice Bulletin No. 106. Am J Obstet Gynecol. 2010;202(5):411-412.
15. Parer JT, King T, Flanders S, Fox M, Kilpatrick SJ. Fetal acidemia and electronic fetal heart rate patterns: is there evidence of an association? J Matern Fetal Neonatal Med. 2006;19(5):289-294.

