User login
Managing anxiety in patients with implanted cardiac defibrillators
Mr. W, age 51, received an implantable cardioverter defibrillator (ICD) after a diagnosis of ventricular tachycardia. He has lived more than 2 years without an ICD discharge and had been functioning well.
One evening, while watching his favorite football team lose a close, intense game on television, Mr. W receives his first ICD “shock.” He becomes extremely anxious and immediately associates the shock with the anger and frustration he was feeling while watching the game. He also suspects he might have caused the shock by using the remote control to change channels when he realized his team would lose.
Anxiety, depression, and feeling a “loss of control” are common among ICD patients. Although the devices provide cardiac patients with a better quality of life than the use of antiarrhythmia drugs,1 ICD recipients may live in fear of receiving a powerful shock at any moment.
This article explains how to break the “fear of fear” cycle that causes ICD patients to avoid activities they associate with ICD activation. To help you preserve ICD patients’ functioning, we describe:
- common psychiatric symptoms in ICD recipients
- when and how to assess for ICD-related anxiety
- cognitive-behavioral and pharmacotherapeutic options.
A psychological jolt
An ICD acts to prevent sudden cardiac death (Box 1)2-7 when a patient develops a sustained, potentially life-threatening arrhythmia. The device restores normal cardiac rhythm by delivering high-energy electrical pulses (shocks) to the appropriate chamber in the patient’s heart (Box 2).
Patients usually perceive ICD shocks as painful and unpleasant, which can cause fear, anger, anxiety, helplessness, and depression.8-11 The ICD recipient’s cardiac status, history of psychiatric illness, and other factors increase the risk of experiencing these symptoms (Table 1).8,9
Undergoing the implantation of an ICD may cause patients to feel a loss of personal, social, and material resources. The higher the ICD recipient’s sense of loss of financial or physical well-being, the higher the risk of depression and anxiety.9
Inadequate social support, poor physical functioning, a
history of depression, and greater length of time
since ICD implantation also may contribute
to emotional distress.9
Besides having undergone cardiac surgery, patients with newly implanted ICDs face other stressors, including:
- expensive medical bills
- possible disability
- driving restrictions.
Patients’ personal relationships may become strained because of changes in their ability to maintain previous physical, social, and sexual activity. Depression or anxiety can cause patients to be withdrawn or irritable.
Some ICD recipients become concerned with body image because the silhouette of the device may be visible under the skin. After ICD implantation, patients may become more aware that they may experience life-threatening arrhythmias.
Finally—and perhaps most important to the patient and psychiatrist—a recipient might be constantly afraid that the device is about to deliver a shock.8
Sudden cardiac death (SCD)—one of the leading causes of mortality in the United States2,3—is an unexpected death from cardiac causes that occurs in ≤1 hour. Causes include ventricular tachycardia, ventricular fibrillation, and bradycardia. Most SCD victims have coronary artery disease.2
Each year approximately 330,000 people die from SCD outside a hospital or emergency department.2 The incidence increases with age and is higher in men than women and in African-Americans than Caucasians.3
Implantable cardioverter defibrillators (ICDs) are a first-line prophylactic therapy for patients at risk for SCD.4,5 Annual ICD implants increased by 11-fold from 1990 to 2000, and this trend continues as the U.S. population ages.6 ICDs prevent sudden cardiac death in >90% of cardiac rhythm disturbances.7
Table 1
5 risk factors for ICD-related psychiatric symptoms
| Age <50 years |
| Limited social support |
| Poor cardiac status |
| History of psychiatric illness |
| Receiving frequent ICD discharges |
| Source: References 8,9 |
Fear impairs functioning
Experiencing an ICD discharge can affect patients’ appraisal of their situation and impair functioning.
CASE CONTINUED: Anxiety leads to avoidance
After receiving the ICD shock, Mr. W stops watching his favorite teams on television. He later ceases viewing sporting events, and over the next several months stops watching television altogether.
Mr. W continues to experience severe anxiety and ruminates about potential shocks. He believes that as long as he avoids becoming “excited” he can reduce his risk of shock. He comes to believe that his avoidance accounts for the absence of subsequent shocks and therefore continues to alter his lifestyle. Mr. W begins to eliminate other behaviors, including sex and exercise, that he fears might induce an ICD shock.
Avoiding activities. After receiving a shock, patients often develop fear that causes them to avoid the activity they were doing when the discharge occurred. This classical conditioning process often leads patients to continually avoid the activity, which may reduce anxiety but is negatively reinforcing (operant conditioning).
These fears and subsequent avoidance behaviors may increase with the number of shocks.8 Over time, fear and avoidance may adversely alter lifestyle and diminish quality of life.
Hypervigilance to physical sensations. Patients typically are troubled by ICDs’ uncontrollable, unpredictable nature and feel compelled to try to predict when the device will fire. Often patients become attuned to minor physical sensations and incorrectly interpret normal sympathetic sensations as precursors of an ICD discharge. Fearful assessment of these symptoms can activate anxiety-related sympathetic arousal, creating a “fear of fear” cycle that mimics the catastrophic interpretation of panic disorder patients.10
Cognitive distortions. After receiving an ICD discharge, patients commonly “catastrophize” about future events. They might overestimate the negative consequences of a discharge by, for example, thinking that if they are shocked during an important event, it will ruin the event for everyone.
“Overgeneralizing” occurs when patients believe a rare occurrence (an ICD discharge) will happen frequently, which may contribute to avoidance. For example, patients might think they should avoid the grocery store if they previously received a shock while shopping.
Phantom shocks. A patient with an ICD may insist he has experienced a shock even though the device provides no evidence of delivering one. Patients may report feeling kicked, shaken, or jolted out of sleep.
Because re-experiencing an event (in this case, through phantom shocks), avoidance, and hyperarousal are part of DSM-IV-TR criteria for posttraumatic stress disorder (PTSD), some clinicians equate patients’ post-shock experience to PTSD.11 The more often patients are shocked, the more likely they will experience these outcomes.
CASE CONTINUED: Delayed diagnosis
As a result of his drastic lifestyle changes, Mr. W experiences considerable relationship, vocational, and financial problems. Unfortunately, Mr. W’s primary care physician doesn’t recognize the impact of these symptoms until Mr. W becomes severely depressed. Then Mr. W is referred for psychiatric treatment.
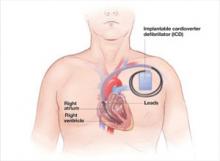
During implantation, the surgeon places the ICD under the skin in the upper chest beneath the patient’s collarbone or abdominal muscles. Each lead is threaded through the subclavian or cephalic vein, passed into the appropriate cardiac chamber, and anchored with a soft prong or screw.
Table 2
Self-rated Florida Shock Anxiety Scale for ICD patients*
| 1. | I am scared to exercise because I am scared that it will increase my heart rate and cause my device to fire. |
| 2. | I am afraid of being alone when the ICD fires and I will need help. |
| 3. | I do not get angry or upset because it may cause the ICD to fire. |
| 4. | It bothers me that I do not know when the ICD will fire. |
| 5. | I worry about the ICD not firing sometime when it should. |
| 6. | I am afraid to touch others for fear that I will shock them if the ICD fires. |
| 7. | I worry about the ICD firing and causing a scene. |
| 8. | When I note my heart beating rapidly, I worry that the ICD will fire. |
| 9. | I have unwanted thoughts of my ICD firing. |
| 10. | I do not engage in sexual activity because it will cause my ICD to fire. |
| *Patients rate each item as 1=Not at all; 2=Rarely; 3=Some of the time; 4=Most of the time; or 5=All of the time. A patient who scores 3 or higher on any item should be referred for further discussion of his specific concerns. | |
| Source: Adapted with permission of Blackwell Publishing Ltd. from Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8. | |
Frequent assessment is key
ICD patients should be assessed for psychiatric symptoms soon after the device is implanted and consistently as a part of routine medical care. At all follow-up visits, primary care clinicians should screen patients for anxiety, depression, and difficulty adjusting to receiving an ICD, and refer those who exhibit signs and symptoms of emotional distress to a mental health professional for evaluation and treatment.
ICD patients might not readily report psychiatric symptoms because of embarrassment, lack of insight, or the circumscribed nature of their symptoms. Because patients may have symptoms that do not meet diagnostic criteria for a specific DSM-IV-TR disorder but impair quality of life and functioning, assess for subclinical distress. Assess patients regularly even if they have not experienced a shock because device-related distress can occur in the absence of shock.
Frequently used screening instruments for anxiety and depression—such as the Beck Depression Inventory, Beck Anxiety Inventory, Brief Symptom Inventory-18 Item, and the Patient Health Questionnaire—can be helpful. Some patients’ distress is limited to their ICDs, however, and cannot be identified by more general measures.
As with Mr. W, traditional inventories might not detect the severity of ICD patients’ psychiatric symptoms until symptoms are severe. Moreover, initial symptoms can be very specific to the ICD and, to some clinicians, may seem relatively benign. Using an instrument designed specifically for assessing ICD patients can lead to earlier diagnosis and treatment.
ICD-specific tools. The Florida Shock Anxiety Scale (FSAS) is a 10-item questionnaire measuring ICD-specific fears about shock (Table 2).12 The FSAS contains statements, such as “I have unwanted thoughts of my ICD firing” and “When I note my heart beating rapidly, I worry that the ICD will fire,” that patients rate on a scale of 1 (Not at all) to 5 (All of the time). A patient who scores 3 or higher on any item should receive counseling related to his specific concerns.
Another useful instrument is the ICD Patient Concerns Questionnaire,13 a 20-item questionnaire to assess the number and severity of ICD recipients’ concerns. Both instruments can help identify targets for intervention.
Targeting underlying beliefs
The initial treatment goal is to relieve anxiety and depressive symptoms. These are likely to persist, however, if the patient’s irrational beliefs, avoidance, and conditioning are not addressed.
Treatment often involves a combination of medication, psychotherapy, and support. Anxiolytics and antidepressants may prove helpful. Choose medications—in collaboration with the patient’s electrophysiologist— based on the patient’s medical history, psychiatric history, and other factors.
Cognitive-behavioral therapy (CBT) often is used to identify and correct maladaptive or irrational beliefs about ICDs and shocks and to eliminate avoidance behaviors that serve as negative reinforcement. CBT typically begins with psychoeducation about the ICD to help patients realize their thoughts about the device might be irrational. Strategies include keeping a daily log of ICD-related thoughts and cognitive re-structuring. Exposure therapy can help patients re-engage in activities they have been avoiding because of irrational fears.
One study found that ICD patients who received CBT that included psychoeducation, stress management, addressing distorted cognitions and avoidance behavior, and resuming work and social activities had less depression and anxiety and better overall adjustment than those who did not get CBT, whether or not their ICD had ever delivered a shock.14
Smith et al15 demonstrated the effectiveness of CBT in patients with ICDs who suffer from panic disorder with agoraphobia and depression. This treatment included:
- interoceptive exposure to target somatic hypervigilance
- relaxation techniques
- cognitive restructuring.
Other therapeutic interventions that can help patients cope and improve their quality of life include support groups, relaxation training, biofeedback, and couples’ counseling.16-19
CASE CONTINUED: CBT helps patient resume activities CBT helps patient resume activities
During 8 CBT sessions, Mr. W learns to identify and challenge the irrational and maladaptive beliefs that were leading him to avoid numerous activities. He eventually accepts that watching television is not likely by itself to trigger an ICD discharge. Through a combination of exposure therapy and relaxation training, Mr. W can resume most activities, which improves his personal relationships and quality of life.
Related resources
- Frizelle D, Lewin B, Kaye G, Moniz-Cook E. Development of a measure of the concerns held by people with implanted cardioverter defibrillators: the ICDC. Br J Health Psychol 2006;11:293-301.
- Hecksel KA, Bostwick JM. Getting to the heart of his 'shocking' trauma. Current Psychiatry 2007;6(6):84-95.
- Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8.
- Thomas S, Friedmann E, Kao C, et al. Quality of life and psychological status of patients with implantable cardioverter defibrillators. Am J Crit Care 2006;15(4):389-98.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. American Heart Association Sudden cardiac death 2007. Available at: http://www.americanheart.org/presenter.jhtml?identifier=14. Accessed April 16, 2007.
2. Zheng Z, Croft J, Giles W, Mehsah G. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001;104:2158-63.
3. The Antiarrhythmic versus Implantable Defibrillator Study (AVID) Investigators. A comparison of antiarrhythmicdrug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. Circulation 1997;337:1576-83.
4. Moss A, Zareba W, Hall W, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877-83.
5. Kadish A, Dyer A, Daubert J, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004;350:2151-8.
6. Maisel W, Sweeney M, Stevenson W, et al. Recalls and safety alerts involving pacemakers and implantable cardioverter defibrillator generators. JAMA 2001;286(7):793-9.
7. Groeneveld P, Matta M, Suh J, et al. Costs and quality-of-life effects of implantable cardioverter-defibrillators. Am J Cardiol 2006;98:1409-14.
8. Sears S, Kovacs A, Azzarello L, et al. Innovations in health psychology: the psychosocial care of adults with implantable cardioverter defibrillators. Prof Psychol Res Pr 2004;35:520-6.
9. Luyster F, Hughes J, Waechter D, Josephson R. Resource loss predicts depression and anxiety among patients treated with an implantable cardioverter defibrillator. Psychosom Med 2006;68:794-800.
10. Pauli P, Wiedemannn G, Dengler W, et al. Anxiety in patients with an automatic implantable cardioverter defibrillator: what differentiates them from panic patients? Psychosom Med 1999;61:69-76.
11. Hamner M, Hunt N, Gee J, et al. PTSD and automatic implantable cardioverter defibrillators. Psychosomatics 1999;40:82-5.
12. Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8.
13. Frizelle D, Lewin B, Kaye G, Moniz-Cook E. Development of a measure of the concerns held by people with implanted cardioverter defibrillators: the ICDC. Br J Health Psychol 2006;11:293-301.
14. Kohn C, Petrucci R, Baessler C, et al. The effect of psychological intervention on patients’ long-term adjustment to the ICD: a prospective study. Pacing Clin Electrophysiol 2000;23(4):450-6.
15. Smith LC, Fogel D, Friedman S. Cognitive-behavioral treatment of panic disorder with agoraphobia triggered by AICD implant activity. Psychosomatics 1999;39(5):474-7.
16. Fitchet A, Doherty PJ, Bundy C, et al. Comprehensive cardiac rehabilitation program for implantable cardioverter-defibrillator patients: a randomized controlled trial. Heart 2003;89:155-60.
17. Sears SF, Conti JB. Quality of life and psychological functioning of ICD patients. Heart 2002;87:488-93.
18. Kranitz L, Lehrer P. Biofeedback applications in the treatment of cardiovascular diseases. Cardiol Rev 2004;12(3):177-81.
19. O’Brien MC, Langberg J, Valderrama AL, et al. Implantable cardioverter defibrillator storm nursing care issues for patients and families. Crit Care Nurs Clin North Am 2005;17:9-6.
Mr. W, age 51, received an implantable cardioverter defibrillator (ICD) after a diagnosis of ventricular tachycardia. He has lived more than 2 years without an ICD discharge and had been functioning well.
One evening, while watching his favorite football team lose a close, intense game on television, Mr. W receives his first ICD “shock.” He becomes extremely anxious and immediately associates the shock with the anger and frustration he was feeling while watching the game. He also suspects he might have caused the shock by using the remote control to change channels when he realized his team would lose.
Anxiety, depression, and feeling a “loss of control” are common among ICD patients. Although the devices provide cardiac patients with a better quality of life than the use of antiarrhythmia drugs,1 ICD recipients may live in fear of receiving a powerful shock at any moment.
This article explains how to break the “fear of fear” cycle that causes ICD patients to avoid activities they associate with ICD activation. To help you preserve ICD patients’ functioning, we describe:
- common psychiatric symptoms in ICD recipients
- when and how to assess for ICD-related anxiety
- cognitive-behavioral and pharmacotherapeutic options.
A psychological jolt
An ICD acts to prevent sudden cardiac death (Box 1)2-7 when a patient develops a sustained, potentially life-threatening arrhythmia. The device restores normal cardiac rhythm by delivering high-energy electrical pulses (shocks) to the appropriate chamber in the patient’s heart (Box 2).
Patients usually perceive ICD shocks as painful and unpleasant, which can cause fear, anger, anxiety, helplessness, and depression.8-11 The ICD recipient’s cardiac status, history of psychiatric illness, and other factors increase the risk of experiencing these symptoms (Table 1).8,9
Undergoing the implantation of an ICD may cause patients to feel a loss of personal, social, and material resources. The higher the ICD recipient’s sense of loss of financial or physical well-being, the higher the risk of depression and anxiety.9
Inadequate social support, poor physical functioning, a
history of depression, and greater length of time
since ICD implantation also may contribute
to emotional distress.9
Besides having undergone cardiac surgery, patients with newly implanted ICDs face other stressors, including:
- expensive medical bills
- possible disability
- driving restrictions.
Patients’ personal relationships may become strained because of changes in their ability to maintain previous physical, social, and sexual activity. Depression or anxiety can cause patients to be withdrawn or irritable.
Some ICD recipients become concerned with body image because the silhouette of the device may be visible under the skin. After ICD implantation, patients may become more aware that they may experience life-threatening arrhythmias.
Finally—and perhaps most important to the patient and psychiatrist—a recipient might be constantly afraid that the device is about to deliver a shock.8
Sudden cardiac death (SCD)—one of the leading causes of mortality in the United States2,3—is an unexpected death from cardiac causes that occurs in ≤1 hour. Causes include ventricular tachycardia, ventricular fibrillation, and bradycardia. Most SCD victims have coronary artery disease.2
Each year approximately 330,000 people die from SCD outside a hospital or emergency department.2 The incidence increases with age and is higher in men than women and in African-Americans than Caucasians.3
Implantable cardioverter defibrillators (ICDs) are a first-line prophylactic therapy for patients at risk for SCD.4,5 Annual ICD implants increased by 11-fold from 1990 to 2000, and this trend continues as the U.S. population ages.6 ICDs prevent sudden cardiac death in >90% of cardiac rhythm disturbances.7
Table 1
5 risk factors for ICD-related psychiatric symptoms
| Age <50 years |
| Limited social support |
| Poor cardiac status |
| History of psychiatric illness |
| Receiving frequent ICD discharges |
| Source: References 8,9 |
Fear impairs functioning
Experiencing an ICD discharge can affect patients’ appraisal of their situation and impair functioning.
CASE CONTINUED: Anxiety leads to avoidance
After receiving the ICD shock, Mr. W stops watching his favorite teams on television. He later ceases viewing sporting events, and over the next several months stops watching television altogether.
Mr. W continues to experience severe anxiety and ruminates about potential shocks. He believes that as long as he avoids becoming “excited” he can reduce his risk of shock. He comes to believe that his avoidance accounts for the absence of subsequent shocks and therefore continues to alter his lifestyle. Mr. W begins to eliminate other behaviors, including sex and exercise, that he fears might induce an ICD shock.
Avoiding activities. After receiving a shock, patients often develop fear that causes them to avoid the activity they were doing when the discharge occurred. This classical conditioning process often leads patients to continually avoid the activity, which may reduce anxiety but is negatively reinforcing (operant conditioning).
These fears and subsequent avoidance behaviors may increase with the number of shocks.8 Over time, fear and avoidance may adversely alter lifestyle and diminish quality of life.
Hypervigilance to physical sensations. Patients typically are troubled by ICDs’ uncontrollable, unpredictable nature and feel compelled to try to predict when the device will fire. Often patients become attuned to minor physical sensations and incorrectly interpret normal sympathetic sensations as precursors of an ICD discharge. Fearful assessment of these symptoms can activate anxiety-related sympathetic arousal, creating a “fear of fear” cycle that mimics the catastrophic interpretation of panic disorder patients.10
Cognitive distortions. After receiving an ICD discharge, patients commonly “catastrophize” about future events. They might overestimate the negative consequences of a discharge by, for example, thinking that if they are shocked during an important event, it will ruin the event for everyone.
“Overgeneralizing” occurs when patients believe a rare occurrence (an ICD discharge) will happen frequently, which may contribute to avoidance. For example, patients might think they should avoid the grocery store if they previously received a shock while shopping.
Phantom shocks. A patient with an ICD may insist he has experienced a shock even though the device provides no evidence of delivering one. Patients may report feeling kicked, shaken, or jolted out of sleep.
Because re-experiencing an event (in this case, through phantom shocks), avoidance, and hyperarousal are part of DSM-IV-TR criteria for posttraumatic stress disorder (PTSD), some clinicians equate patients’ post-shock experience to PTSD.11 The more often patients are shocked, the more likely they will experience these outcomes.
CASE CONTINUED: Delayed diagnosis
As a result of his drastic lifestyle changes, Mr. W experiences considerable relationship, vocational, and financial problems. Unfortunately, Mr. W’s primary care physician doesn’t recognize the impact of these symptoms until Mr. W becomes severely depressed. Then Mr. W is referred for psychiatric treatment.
During implantation, the surgeon places the ICD under the skin in the upper chest beneath the patient’s collarbone or abdominal muscles. Each lead is threaded through the subclavian or cephalic vein, passed into the appropriate cardiac chamber, and anchored with a soft prong or screw.
Table 2
Self-rated Florida Shock Anxiety Scale for ICD patients*
| 1. | I am scared to exercise because I am scared that it will increase my heart rate and cause my device to fire. |
| 2. | I am afraid of being alone when the ICD fires and I will need help. |
| 3. | I do not get angry or upset because it may cause the ICD to fire. |
| 4. | It bothers me that I do not know when the ICD will fire. |
| 5. | I worry about the ICD not firing sometime when it should. |
| 6. | I am afraid to touch others for fear that I will shock them if the ICD fires. |
| 7. | I worry about the ICD firing and causing a scene. |
| 8. | When I note my heart beating rapidly, I worry that the ICD will fire. |
| 9. | I have unwanted thoughts of my ICD firing. |
| 10. | I do not engage in sexual activity because it will cause my ICD to fire. |
| *Patients rate each item as 1=Not at all; 2=Rarely; 3=Some of the time; 4=Most of the time; or 5=All of the time. A patient who scores 3 or higher on any item should be referred for further discussion of his specific concerns. | |
| Source: Adapted with permission of Blackwell Publishing Ltd. from Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8. | |
Frequent assessment is key
ICD patients should be assessed for psychiatric symptoms soon after the device is implanted and consistently as a part of routine medical care. At all follow-up visits, primary care clinicians should screen patients for anxiety, depression, and difficulty adjusting to receiving an ICD, and refer those who exhibit signs and symptoms of emotional distress to a mental health professional for evaluation and treatment.
ICD patients might not readily report psychiatric symptoms because of embarrassment, lack of insight, or the circumscribed nature of their symptoms. Because patients may have symptoms that do not meet diagnostic criteria for a specific DSM-IV-TR disorder but impair quality of life and functioning, assess for subclinical distress. Assess patients regularly even if they have not experienced a shock because device-related distress can occur in the absence of shock.
Frequently used screening instruments for anxiety and depression—such as the Beck Depression Inventory, Beck Anxiety Inventory, Brief Symptom Inventory-18 Item, and the Patient Health Questionnaire—can be helpful. Some patients’ distress is limited to their ICDs, however, and cannot be identified by more general measures.
As with Mr. W, traditional inventories might not detect the severity of ICD patients’ psychiatric symptoms until symptoms are severe. Moreover, initial symptoms can be very specific to the ICD and, to some clinicians, may seem relatively benign. Using an instrument designed specifically for assessing ICD patients can lead to earlier diagnosis and treatment.
ICD-specific tools. The Florida Shock Anxiety Scale (FSAS) is a 10-item questionnaire measuring ICD-specific fears about shock (Table 2).12 The FSAS contains statements, such as “I have unwanted thoughts of my ICD firing” and “When I note my heart beating rapidly, I worry that the ICD will fire,” that patients rate on a scale of 1 (Not at all) to 5 (All of the time). A patient who scores 3 or higher on any item should receive counseling related to his specific concerns.
Another useful instrument is the ICD Patient Concerns Questionnaire,13 a 20-item questionnaire to assess the number and severity of ICD recipients’ concerns. Both instruments can help identify targets for intervention.
Targeting underlying beliefs
The initial treatment goal is to relieve anxiety and depressive symptoms. These are likely to persist, however, if the patient’s irrational beliefs, avoidance, and conditioning are not addressed.
Treatment often involves a combination of medication, psychotherapy, and support. Anxiolytics and antidepressants may prove helpful. Choose medications—in collaboration with the patient’s electrophysiologist— based on the patient’s medical history, psychiatric history, and other factors.
Cognitive-behavioral therapy (CBT) often is used to identify and correct maladaptive or irrational beliefs about ICDs and shocks and to eliminate avoidance behaviors that serve as negative reinforcement. CBT typically begins with psychoeducation about the ICD to help patients realize their thoughts about the device might be irrational. Strategies include keeping a daily log of ICD-related thoughts and cognitive re-structuring. Exposure therapy can help patients re-engage in activities they have been avoiding because of irrational fears.
One study found that ICD patients who received CBT that included psychoeducation, stress management, addressing distorted cognitions and avoidance behavior, and resuming work and social activities had less depression and anxiety and better overall adjustment than those who did not get CBT, whether or not their ICD had ever delivered a shock.14
Smith et al15 demonstrated the effectiveness of CBT in patients with ICDs who suffer from panic disorder with agoraphobia and depression. This treatment included:
- interoceptive exposure to target somatic hypervigilance
- relaxation techniques
- cognitive restructuring.
Other therapeutic interventions that can help patients cope and improve their quality of life include support groups, relaxation training, biofeedback, and couples’ counseling.16-19
CASE CONTINUED: CBT helps patient resume activities CBT helps patient resume activities
During 8 CBT sessions, Mr. W learns to identify and challenge the irrational and maladaptive beliefs that were leading him to avoid numerous activities. He eventually accepts that watching television is not likely by itself to trigger an ICD discharge. Through a combination of exposure therapy and relaxation training, Mr. W can resume most activities, which improves his personal relationships and quality of life.
Related resources
- Frizelle D, Lewin B, Kaye G, Moniz-Cook E. Development of a measure of the concerns held by people with implanted cardioverter defibrillators: the ICDC. Br J Health Psychol 2006;11:293-301.
- Hecksel KA, Bostwick JM. Getting to the heart of his 'shocking' trauma. Current Psychiatry 2007;6(6):84-95.
- Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8.
- Thomas S, Friedmann E, Kao C, et al. Quality of life and psychological status of patients with implantable cardioverter defibrillators. Am J Crit Care 2006;15(4):389-98.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Mr. W, age 51, received an implantable cardioverter defibrillator (ICD) after a diagnosis of ventricular tachycardia. He has lived more than 2 years without an ICD discharge and had been functioning well.
One evening, while watching his favorite football team lose a close, intense game on television, Mr. W receives his first ICD “shock.” He becomes extremely anxious and immediately associates the shock with the anger and frustration he was feeling while watching the game. He also suspects he might have caused the shock by using the remote control to change channels when he realized his team would lose.
Anxiety, depression, and feeling a “loss of control” are common among ICD patients. Although the devices provide cardiac patients with a better quality of life than the use of antiarrhythmia drugs,1 ICD recipients may live in fear of receiving a powerful shock at any moment.
This article explains how to break the “fear of fear” cycle that causes ICD patients to avoid activities they associate with ICD activation. To help you preserve ICD patients’ functioning, we describe:
- common psychiatric symptoms in ICD recipients
- when and how to assess for ICD-related anxiety
- cognitive-behavioral and pharmacotherapeutic options.
A psychological jolt
An ICD acts to prevent sudden cardiac death (Box 1)2-7 when a patient develops a sustained, potentially life-threatening arrhythmia. The device restores normal cardiac rhythm by delivering high-energy electrical pulses (shocks) to the appropriate chamber in the patient’s heart (Box 2).
Patients usually perceive ICD shocks as painful and unpleasant, which can cause fear, anger, anxiety, helplessness, and depression.8-11 The ICD recipient’s cardiac status, history of psychiatric illness, and other factors increase the risk of experiencing these symptoms (Table 1).8,9
Undergoing the implantation of an ICD may cause patients to feel a loss of personal, social, and material resources. The higher the ICD recipient’s sense of loss of financial or physical well-being, the higher the risk of depression and anxiety.9
Inadequate social support, poor physical functioning, a
history of depression, and greater length of time
since ICD implantation also may contribute
to emotional distress.9
Besides having undergone cardiac surgery, patients with newly implanted ICDs face other stressors, including:
- expensive medical bills
- possible disability
- driving restrictions.
Patients’ personal relationships may become strained because of changes in their ability to maintain previous physical, social, and sexual activity. Depression or anxiety can cause patients to be withdrawn or irritable.
Some ICD recipients become concerned with body image because the silhouette of the device may be visible under the skin. After ICD implantation, patients may become more aware that they may experience life-threatening arrhythmias.
Finally—and perhaps most important to the patient and psychiatrist—a recipient might be constantly afraid that the device is about to deliver a shock.8
Sudden cardiac death (SCD)—one of the leading causes of mortality in the United States2,3—is an unexpected death from cardiac causes that occurs in ≤1 hour. Causes include ventricular tachycardia, ventricular fibrillation, and bradycardia. Most SCD victims have coronary artery disease.2
Each year approximately 330,000 people die from SCD outside a hospital or emergency department.2 The incidence increases with age and is higher in men than women and in African-Americans than Caucasians.3
Implantable cardioverter defibrillators (ICDs) are a first-line prophylactic therapy for patients at risk for SCD.4,5 Annual ICD implants increased by 11-fold from 1990 to 2000, and this trend continues as the U.S. population ages.6 ICDs prevent sudden cardiac death in >90% of cardiac rhythm disturbances.7
Table 1
5 risk factors for ICD-related psychiatric symptoms
| Age <50 years |
| Limited social support |
| Poor cardiac status |
| History of psychiatric illness |
| Receiving frequent ICD discharges |
| Source: References 8,9 |
Fear impairs functioning
Experiencing an ICD discharge can affect patients’ appraisal of their situation and impair functioning.
CASE CONTINUED: Anxiety leads to avoidance
After receiving the ICD shock, Mr. W stops watching his favorite teams on television. He later ceases viewing sporting events, and over the next several months stops watching television altogether.
Mr. W continues to experience severe anxiety and ruminates about potential shocks. He believes that as long as he avoids becoming “excited” he can reduce his risk of shock. He comes to believe that his avoidance accounts for the absence of subsequent shocks and therefore continues to alter his lifestyle. Mr. W begins to eliminate other behaviors, including sex and exercise, that he fears might induce an ICD shock.
Avoiding activities. After receiving a shock, patients often develop fear that causes them to avoid the activity they were doing when the discharge occurred. This classical conditioning process often leads patients to continually avoid the activity, which may reduce anxiety but is negatively reinforcing (operant conditioning).
These fears and subsequent avoidance behaviors may increase with the number of shocks.8 Over time, fear and avoidance may adversely alter lifestyle and diminish quality of life.
Hypervigilance to physical sensations. Patients typically are troubled by ICDs’ uncontrollable, unpredictable nature and feel compelled to try to predict when the device will fire. Often patients become attuned to minor physical sensations and incorrectly interpret normal sympathetic sensations as precursors of an ICD discharge. Fearful assessment of these symptoms can activate anxiety-related sympathetic arousal, creating a “fear of fear” cycle that mimics the catastrophic interpretation of panic disorder patients.10
Cognitive distortions. After receiving an ICD discharge, patients commonly “catastrophize” about future events. They might overestimate the negative consequences of a discharge by, for example, thinking that if they are shocked during an important event, it will ruin the event for everyone.
“Overgeneralizing” occurs when patients believe a rare occurrence (an ICD discharge) will happen frequently, which may contribute to avoidance. For example, patients might think they should avoid the grocery store if they previously received a shock while shopping.
Phantom shocks. A patient with an ICD may insist he has experienced a shock even though the device provides no evidence of delivering one. Patients may report feeling kicked, shaken, or jolted out of sleep.
Because re-experiencing an event (in this case, through phantom shocks), avoidance, and hyperarousal are part of DSM-IV-TR criteria for posttraumatic stress disorder (PTSD), some clinicians equate patients’ post-shock experience to PTSD.11 The more often patients are shocked, the more likely they will experience these outcomes.
CASE CONTINUED: Delayed diagnosis
As a result of his drastic lifestyle changes, Mr. W experiences considerable relationship, vocational, and financial problems. Unfortunately, Mr. W’s primary care physician doesn’t recognize the impact of these symptoms until Mr. W becomes severely depressed. Then Mr. W is referred for psychiatric treatment.
During implantation, the surgeon places the ICD under the skin in the upper chest beneath the patient’s collarbone or abdominal muscles. Each lead is threaded through the subclavian or cephalic vein, passed into the appropriate cardiac chamber, and anchored with a soft prong or screw.
Table 2
Self-rated Florida Shock Anxiety Scale for ICD patients*
| 1. | I am scared to exercise because I am scared that it will increase my heart rate and cause my device to fire. |
| 2. | I am afraid of being alone when the ICD fires and I will need help. |
| 3. | I do not get angry or upset because it may cause the ICD to fire. |
| 4. | It bothers me that I do not know when the ICD will fire. |
| 5. | I worry about the ICD not firing sometime when it should. |
| 6. | I am afraid to touch others for fear that I will shock them if the ICD fires. |
| 7. | I worry about the ICD firing and causing a scene. |
| 8. | When I note my heart beating rapidly, I worry that the ICD will fire. |
| 9. | I have unwanted thoughts of my ICD firing. |
| 10. | I do not engage in sexual activity because it will cause my ICD to fire. |
| *Patients rate each item as 1=Not at all; 2=Rarely; 3=Some of the time; 4=Most of the time; or 5=All of the time. A patient who scores 3 or higher on any item should be referred for further discussion of his specific concerns. | |
| Source: Adapted with permission of Blackwell Publishing Ltd. from Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8. | |
Frequent assessment is key
ICD patients should be assessed for psychiatric symptoms soon after the device is implanted and consistently as a part of routine medical care. At all follow-up visits, primary care clinicians should screen patients for anxiety, depression, and difficulty adjusting to receiving an ICD, and refer those who exhibit signs and symptoms of emotional distress to a mental health professional for evaluation and treatment.
ICD patients might not readily report psychiatric symptoms because of embarrassment, lack of insight, or the circumscribed nature of their symptoms. Because patients may have symptoms that do not meet diagnostic criteria for a specific DSM-IV-TR disorder but impair quality of life and functioning, assess for subclinical distress. Assess patients regularly even if they have not experienced a shock because device-related distress can occur in the absence of shock.
Frequently used screening instruments for anxiety and depression—such as the Beck Depression Inventory, Beck Anxiety Inventory, Brief Symptom Inventory-18 Item, and the Patient Health Questionnaire—can be helpful. Some patients’ distress is limited to their ICDs, however, and cannot be identified by more general measures.
As with Mr. W, traditional inventories might not detect the severity of ICD patients’ psychiatric symptoms until symptoms are severe. Moreover, initial symptoms can be very specific to the ICD and, to some clinicians, may seem relatively benign. Using an instrument designed specifically for assessing ICD patients can lead to earlier diagnosis and treatment.
ICD-specific tools. The Florida Shock Anxiety Scale (FSAS) is a 10-item questionnaire measuring ICD-specific fears about shock (Table 2).12 The FSAS contains statements, such as “I have unwanted thoughts of my ICD firing” and “When I note my heart beating rapidly, I worry that the ICD will fire,” that patients rate on a scale of 1 (Not at all) to 5 (All of the time). A patient who scores 3 or higher on any item should receive counseling related to his specific concerns.
Another useful instrument is the ICD Patient Concerns Questionnaire,13 a 20-item questionnaire to assess the number and severity of ICD recipients’ concerns. Both instruments can help identify targets for intervention.
Targeting underlying beliefs
The initial treatment goal is to relieve anxiety and depressive symptoms. These are likely to persist, however, if the patient’s irrational beliefs, avoidance, and conditioning are not addressed.
Treatment often involves a combination of medication, psychotherapy, and support. Anxiolytics and antidepressants may prove helpful. Choose medications—in collaboration with the patient’s electrophysiologist— based on the patient’s medical history, psychiatric history, and other factors.
Cognitive-behavioral therapy (CBT) often is used to identify and correct maladaptive or irrational beliefs about ICDs and shocks and to eliminate avoidance behaviors that serve as negative reinforcement. CBT typically begins with psychoeducation about the ICD to help patients realize their thoughts about the device might be irrational. Strategies include keeping a daily log of ICD-related thoughts and cognitive re-structuring. Exposure therapy can help patients re-engage in activities they have been avoiding because of irrational fears.
One study found that ICD patients who received CBT that included psychoeducation, stress management, addressing distorted cognitions and avoidance behavior, and resuming work and social activities had less depression and anxiety and better overall adjustment than those who did not get CBT, whether or not their ICD had ever delivered a shock.14
Smith et al15 demonstrated the effectiveness of CBT in patients with ICDs who suffer from panic disorder with agoraphobia and depression. This treatment included:
- interoceptive exposure to target somatic hypervigilance
- relaxation techniques
- cognitive restructuring.
Other therapeutic interventions that can help patients cope and improve their quality of life include support groups, relaxation training, biofeedback, and couples’ counseling.16-19
CASE CONTINUED: CBT helps patient resume activities CBT helps patient resume activities
During 8 CBT sessions, Mr. W learns to identify and challenge the irrational and maladaptive beliefs that were leading him to avoid numerous activities. He eventually accepts that watching television is not likely by itself to trigger an ICD discharge. Through a combination of exposure therapy and relaxation training, Mr. W can resume most activities, which improves his personal relationships and quality of life.
Related resources
- Frizelle D, Lewin B, Kaye G, Moniz-Cook E. Development of a measure of the concerns held by people with implanted cardioverter defibrillators: the ICDC. Br J Health Psychol 2006;11:293-301.
- Hecksel KA, Bostwick JM. Getting to the heart of his 'shocking' trauma. Current Psychiatry 2007;6(6):84-95.
- Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8.
- Thomas S, Friedmann E, Kao C, et al. Quality of life and psychological status of patients with implantable cardioverter defibrillators. Am J Crit Care 2006;15(4):389-98.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
1. American Heart Association Sudden cardiac death 2007. Available at: http://www.americanheart.org/presenter.jhtml?identifier=14. Accessed April 16, 2007.
2. Zheng Z, Croft J, Giles W, Mehsah G. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001;104:2158-63.
3. The Antiarrhythmic versus Implantable Defibrillator Study (AVID) Investigators. A comparison of antiarrhythmicdrug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. Circulation 1997;337:1576-83.
4. Moss A, Zareba W, Hall W, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877-83.
5. Kadish A, Dyer A, Daubert J, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004;350:2151-8.
6. Maisel W, Sweeney M, Stevenson W, et al. Recalls and safety alerts involving pacemakers and implantable cardioverter defibrillator generators. JAMA 2001;286(7):793-9.
7. Groeneveld P, Matta M, Suh J, et al. Costs and quality-of-life effects of implantable cardioverter-defibrillators. Am J Cardiol 2006;98:1409-14.
8. Sears S, Kovacs A, Azzarello L, et al. Innovations in health psychology: the psychosocial care of adults with implantable cardioverter defibrillators. Prof Psychol Res Pr 2004;35:520-6.
9. Luyster F, Hughes J, Waechter D, Josephson R. Resource loss predicts depression and anxiety among patients treated with an implantable cardioverter defibrillator. Psychosom Med 2006;68:794-800.
10. Pauli P, Wiedemannn G, Dengler W, et al. Anxiety in patients with an automatic implantable cardioverter defibrillator: what differentiates them from panic patients? Psychosom Med 1999;61:69-76.
11. Hamner M, Hunt N, Gee J, et al. PTSD and automatic implantable cardioverter defibrillators. Psychosomatics 1999;40:82-5.
12. Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8.
13. Frizelle D, Lewin B, Kaye G, Moniz-Cook E. Development of a measure of the concerns held by people with implanted cardioverter defibrillators: the ICDC. Br J Health Psychol 2006;11:293-301.
14. Kohn C, Petrucci R, Baessler C, et al. The effect of psychological intervention on patients’ long-term adjustment to the ICD: a prospective study. Pacing Clin Electrophysiol 2000;23(4):450-6.
15. Smith LC, Fogel D, Friedman S. Cognitive-behavioral treatment of panic disorder with agoraphobia triggered by AICD implant activity. Psychosomatics 1999;39(5):474-7.
16. Fitchet A, Doherty PJ, Bundy C, et al. Comprehensive cardiac rehabilitation program for implantable cardioverter-defibrillator patients: a randomized controlled trial. Heart 2003;89:155-60.
17. Sears SF, Conti JB. Quality of life and psychological functioning of ICD patients. Heart 2002;87:488-93.
18. Kranitz L, Lehrer P. Biofeedback applications in the treatment of cardiovascular diseases. Cardiol Rev 2004;12(3):177-81.
19. O’Brien MC, Langberg J, Valderrama AL, et al. Implantable cardioverter defibrillator storm nursing care issues for patients and families. Crit Care Nurs Clin North Am 2005;17:9-6.
1. American Heart Association Sudden cardiac death 2007. Available at: http://www.americanheart.org/presenter.jhtml?identifier=14. Accessed April 16, 2007.
2. Zheng Z, Croft J, Giles W, Mehsah G. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001;104:2158-63.
3. The Antiarrhythmic versus Implantable Defibrillator Study (AVID) Investigators. A comparison of antiarrhythmicdrug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. Circulation 1997;337:1576-83.
4. Moss A, Zareba W, Hall W, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877-83.
5. Kadish A, Dyer A, Daubert J, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004;350:2151-8.
6. Maisel W, Sweeney M, Stevenson W, et al. Recalls and safety alerts involving pacemakers and implantable cardioverter defibrillator generators. JAMA 2001;286(7):793-9.
7. Groeneveld P, Matta M, Suh J, et al. Costs and quality-of-life effects of implantable cardioverter-defibrillators. Am J Cardiol 2006;98:1409-14.
8. Sears S, Kovacs A, Azzarello L, et al. Innovations in health psychology: the psychosocial care of adults with implantable cardioverter defibrillators. Prof Psychol Res Pr 2004;35:520-6.
9. Luyster F, Hughes J, Waechter D, Josephson R. Resource loss predicts depression and anxiety among patients treated with an implantable cardioverter defibrillator. Psychosom Med 2006;68:794-800.
10. Pauli P, Wiedemannn G, Dengler W, et al. Anxiety in patients with an automatic implantable cardioverter defibrillator: what differentiates them from panic patients? Psychosom Med 1999;61:69-76.
11. Hamner M, Hunt N, Gee J, et al. PTSD and automatic implantable cardioverter defibrillators. Psychosomatics 1999;40:82-5.
12. Kuhl E, Dixit N, Walker R, et al. Measurement of patient fears about implantable cardioverter defibrillator shock: an initial evaluation of the Florida Shock Anxiety Scale. Pacing Clin Electrophysiol 2006;29:614-8.
13. Frizelle D, Lewin B, Kaye G, Moniz-Cook E. Development of a measure of the concerns held by people with implanted cardioverter defibrillators: the ICDC. Br J Health Psychol 2006;11:293-301.
14. Kohn C, Petrucci R, Baessler C, et al. The effect of psychological intervention on patients’ long-term adjustment to the ICD: a prospective study. Pacing Clin Electrophysiol 2000;23(4):450-6.
15. Smith LC, Fogel D, Friedman S. Cognitive-behavioral treatment of panic disorder with agoraphobia triggered by AICD implant activity. Psychosomatics 1999;39(5):474-7.
16. Fitchet A, Doherty PJ, Bundy C, et al. Comprehensive cardiac rehabilitation program for implantable cardioverter-defibrillator patients: a randomized controlled trial. Heart 2003;89:155-60.
17. Sears SF, Conti JB. Quality of life and psychological functioning of ICD patients. Heart 2002;87:488-93.
18. Kranitz L, Lehrer P. Biofeedback applications in the treatment of cardiovascular diseases. Cardiol Rev 2004;12(3):177-81.
19. O’Brien MC, Langberg J, Valderrama AL, et al. Implantable cardioverter defibrillator storm nursing care issues for patients and families. Crit Care Nurs Clin North Am 2005;17:9-6.