User login
Will finding the depression−inflammation link lead to tailored treatments for MDD?
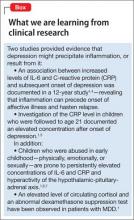
There is an association between inflammation and depression: Patients with a major depressive disorder (MDD) have elevated levels of pro-inflammatory cytokines interleukin (IL)-1, IL-6, tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP). Abnormal cell-mediated immunity and lymphocyte proliferation also have been reported in patients with MDD1-2 (Box).1,3-7
What remains unclear is whether inflammation is causative in affective illness,1-4 and how the association might be exploited for the benefit of a subset of MDD patients.
Underpinnings of pathophysiology
Immune system activation leads to production of cytokines, which 1) influences the synthesis, reuptake, and release of neurotransmitters and 2) stimulates the manifestations of depression.1,2 Interferon-γ and TNF-α are involved in neuronal degeneration and inhibition of neurogenesis in the brain, especially the hippocampus— thereby explaining observed cognitive deficits in depression.
Production of cytokines in serum and cerebrospinal fluid can be triggered by psychosocial stress, administration of interferon-α or IL-2, and acute stimulation of the immune system after vaccination; this production of cytokines is associated with development of MDD.1-3 Inflammatory disorders raise a person’s vulnerability to MDD; affective illness is the most common psychiatric condition seen in association with multiple sclerosis, for example.2
Principal receptor targets
Glucocorticoid receptors. Synchrony between the hypothalamic-pituitary-adrenal axis and adrenal function occurs during stressful circumstances.2 Down-regulation, or reduced activity, of glucocorticoid receptors in depression leads to glucocorticoid resistance, resulting in hyperactivity of this axis. TNF-α is associated with glucocorticoid resistance by its action in opposing the influx of the cortisol-glucocorticoid receptor complex into the nucleus and inhibiting its linkage with DNA. Cytokines increase levels of corticotropin-releasing hormone and adrenocorticotrophic hormone, leading to a higher-than-normal cortisol concentration in depressed patients.8
N-methyl-d-aspartate (NMDA) receptors are involved in the monoamine and glutamatergic pathways that are associated with depression.2 NMDA-receptor activation raises the intracellular calcium concentration, causing neuronal cell death. Inflammatory mediators, including TNF-α, induce activation of the kyneurin pathway. Thus, instead of serotonin production, tryptophan is diverted to the synthesis of the NMDA-receptor agonists kynurenine and quinolinic acid, which leads to apoptosis.
The glutamatergic pathway involves binding of IL-1β and IL-1R complexes to hippocampal NMDA receptors.2 Persistent activation of these receptors results in calcium toxicity and neuronal death. Reuptake inhibition of neurotransmitters is explained by the action of IL-1β on reuptake of glutamate, which enhances its availability to stimulate NMDA-receptor activation.
Any prospects for therapeutics?
As described, an association exists between inflammation and depression. Psychosocial stresses initiate inflammatory responses that might result in affective illness. In treating depression and preventing its relapse, the question is whether psychotherapy provides clinical efficacy through stress reduction, thereby leading to potential anti-inflammatory action.1
Inflammation has a detrimental influence in a subset of MDD cases.9 Identification of those patients through genetic research is ongoing, with the goal of establishing specific anti-inflammatory or antidepressant therapies.
Anti-inflammatory drugs such as aspirin, celecoxib, and etanercept do induce antidepressant effects and augment the antidepressant response to other therapies.1,3 In the future, anti-inflammatory treatments might become an option for select MDD patients.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Zunszain PA, Hepgul N, Pariante CM. Inflammation and depression. Curr Top Behav Neurosci. 2013;14:135-151.
2. Krishnadas R, Cavanagh J. Depression: an inflammatory illness? J Neurol Neurosurg Psychiatry. 2012;83(5):495-502.
3. Lotrich FE, El-Gabalawy H, Guenther LC, et al. The role of inflammation in the pathophysiology of depression: different treatments and their effects. J Rheumatol Suppl. 2011;88:48-54.
4. Gimeno D, Marmot MG, Singh-Manoux A. Inflammatory markers and cognitive function in middle-aged adults: the Whitehall II study. Psychoneuroendocrinology. 2008; 33(10):1322-1334.
5. Copeland WE, Shanahan L, Worthman C, et al. Cumulative depression episodes predict later C-reactive protein levels: a prospective analysis. Biol Psychiatry. 2012;71(1):15-21.
6. Chida Y, Sudo N, Sonoda J, et al. Early-life psychological stress exacerbates adult mouse asthma via the hypothalamus-pituitary-adrenal axis. Am J Respir Crit Care Med. 2007;175(4):316-322.
7. Carpenter LL, Gawuga CE, Tyrka AR, et al. Association between plasma IL-6 response to acute stress and early-life adversity in healthy adults. Neuropsychopharmacology. 2010;35(13):2617-2623.
8. Messay B, Lim A, Marsland AL. Current understanding of the bi-directional relationship of major depression with inflammation. Biol Mood Anxiety Disord. 2012;2(1):4.
9. Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011;7(6):323-331.
There is an association between inflammation and depression: Patients with a major depressive disorder (MDD) have elevated levels of pro-inflammatory cytokines interleukin (IL)-1, IL-6, tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP). Abnormal cell-mediated immunity and lymphocyte proliferation also have been reported in patients with MDD1-2 (Box).1,3-7
What remains unclear is whether inflammation is causative in affective illness,1-4 and how the association might be exploited for the benefit of a subset of MDD patients.
Underpinnings of pathophysiology
Immune system activation leads to production of cytokines, which 1) influences the synthesis, reuptake, and release of neurotransmitters and 2) stimulates the manifestations of depression.1,2 Interferon-γ and TNF-α are involved in neuronal degeneration and inhibition of neurogenesis in the brain, especially the hippocampus— thereby explaining observed cognitive deficits in depression.
Production of cytokines in serum and cerebrospinal fluid can be triggered by psychosocial stress, administration of interferon-α or IL-2, and acute stimulation of the immune system after vaccination; this production of cytokines is associated with development of MDD.1-3 Inflammatory disorders raise a person’s vulnerability to MDD; affective illness is the most common psychiatric condition seen in association with multiple sclerosis, for example.2
Principal receptor targets
Glucocorticoid receptors. Synchrony between the hypothalamic-pituitary-adrenal axis and adrenal function occurs during stressful circumstances.2 Down-regulation, or reduced activity, of glucocorticoid receptors in depression leads to glucocorticoid resistance, resulting in hyperactivity of this axis. TNF-α is associated with glucocorticoid resistance by its action in opposing the influx of the cortisol-glucocorticoid receptor complex into the nucleus and inhibiting its linkage with DNA. Cytokines increase levels of corticotropin-releasing hormone and adrenocorticotrophic hormone, leading to a higher-than-normal cortisol concentration in depressed patients.8
N-methyl-d-aspartate (NMDA) receptors are involved in the monoamine and glutamatergic pathways that are associated with depression.2 NMDA-receptor activation raises the intracellular calcium concentration, causing neuronal cell death. Inflammatory mediators, including TNF-α, induce activation of the kyneurin pathway. Thus, instead of serotonin production, tryptophan is diverted to the synthesis of the NMDA-receptor agonists kynurenine and quinolinic acid, which leads to apoptosis.
The glutamatergic pathway involves binding of IL-1β and IL-1R complexes to hippocampal NMDA receptors.2 Persistent activation of these receptors results in calcium toxicity and neuronal death. Reuptake inhibition of neurotransmitters is explained by the action of IL-1β on reuptake of glutamate, which enhances its availability to stimulate NMDA-receptor activation.
Any prospects for therapeutics?
As described, an association exists between inflammation and depression. Psychosocial stresses initiate inflammatory responses that might result in affective illness. In treating depression and preventing its relapse, the question is whether psychotherapy provides clinical efficacy through stress reduction, thereby leading to potential anti-inflammatory action.1
Inflammation has a detrimental influence in a subset of MDD cases.9 Identification of those patients through genetic research is ongoing, with the goal of establishing specific anti-inflammatory or antidepressant therapies.
Anti-inflammatory drugs such as aspirin, celecoxib, and etanercept do induce antidepressant effects and augment the antidepressant response to other therapies.1,3 In the future, anti-inflammatory treatments might become an option for select MDD patients.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
There is an association between inflammation and depression: Patients with a major depressive disorder (MDD) have elevated levels of pro-inflammatory cytokines interleukin (IL)-1, IL-6, tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP). Abnormal cell-mediated immunity and lymphocyte proliferation also have been reported in patients with MDD1-2 (Box).1,3-7
What remains unclear is whether inflammation is causative in affective illness,1-4 and how the association might be exploited for the benefit of a subset of MDD patients.
Underpinnings of pathophysiology
Immune system activation leads to production of cytokines, which 1) influences the synthesis, reuptake, and release of neurotransmitters and 2) stimulates the manifestations of depression.1,2 Interferon-γ and TNF-α are involved in neuronal degeneration and inhibition of neurogenesis in the brain, especially the hippocampus— thereby explaining observed cognitive deficits in depression.
Production of cytokines in serum and cerebrospinal fluid can be triggered by psychosocial stress, administration of interferon-α or IL-2, and acute stimulation of the immune system after vaccination; this production of cytokines is associated with development of MDD.1-3 Inflammatory disorders raise a person’s vulnerability to MDD; affective illness is the most common psychiatric condition seen in association with multiple sclerosis, for example.2
Principal receptor targets
Glucocorticoid receptors. Synchrony between the hypothalamic-pituitary-adrenal axis and adrenal function occurs during stressful circumstances.2 Down-regulation, or reduced activity, of glucocorticoid receptors in depression leads to glucocorticoid resistance, resulting in hyperactivity of this axis. TNF-α is associated with glucocorticoid resistance by its action in opposing the influx of the cortisol-glucocorticoid receptor complex into the nucleus and inhibiting its linkage with DNA. Cytokines increase levels of corticotropin-releasing hormone and adrenocorticotrophic hormone, leading to a higher-than-normal cortisol concentration in depressed patients.8
N-methyl-d-aspartate (NMDA) receptors are involved in the monoamine and glutamatergic pathways that are associated with depression.2 NMDA-receptor activation raises the intracellular calcium concentration, causing neuronal cell death. Inflammatory mediators, including TNF-α, induce activation of the kyneurin pathway. Thus, instead of serotonin production, tryptophan is diverted to the synthesis of the NMDA-receptor agonists kynurenine and quinolinic acid, which leads to apoptosis.
The glutamatergic pathway involves binding of IL-1β and IL-1R complexes to hippocampal NMDA receptors.2 Persistent activation of these receptors results in calcium toxicity and neuronal death. Reuptake inhibition of neurotransmitters is explained by the action of IL-1β on reuptake of glutamate, which enhances its availability to stimulate NMDA-receptor activation.
Any prospects for therapeutics?
As described, an association exists between inflammation and depression. Psychosocial stresses initiate inflammatory responses that might result in affective illness. In treating depression and preventing its relapse, the question is whether psychotherapy provides clinical efficacy through stress reduction, thereby leading to potential anti-inflammatory action.1
Inflammation has a detrimental influence in a subset of MDD cases.9 Identification of those patients through genetic research is ongoing, with the goal of establishing specific anti-inflammatory or antidepressant therapies.
Anti-inflammatory drugs such as aspirin, celecoxib, and etanercept do induce antidepressant effects and augment the antidepressant response to other therapies.1,3 In the future, anti-inflammatory treatments might become an option for select MDD patients.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Zunszain PA, Hepgul N, Pariante CM. Inflammation and depression. Curr Top Behav Neurosci. 2013;14:135-151.
2. Krishnadas R, Cavanagh J. Depression: an inflammatory illness? J Neurol Neurosurg Psychiatry. 2012;83(5):495-502.
3. Lotrich FE, El-Gabalawy H, Guenther LC, et al. The role of inflammation in the pathophysiology of depression: different treatments and their effects. J Rheumatol Suppl. 2011;88:48-54.
4. Gimeno D, Marmot MG, Singh-Manoux A. Inflammatory markers and cognitive function in middle-aged adults: the Whitehall II study. Psychoneuroendocrinology. 2008; 33(10):1322-1334.
5. Copeland WE, Shanahan L, Worthman C, et al. Cumulative depression episodes predict later C-reactive protein levels: a prospective analysis. Biol Psychiatry. 2012;71(1):15-21.
6. Chida Y, Sudo N, Sonoda J, et al. Early-life psychological stress exacerbates adult mouse asthma via the hypothalamus-pituitary-adrenal axis. Am J Respir Crit Care Med. 2007;175(4):316-322.
7. Carpenter LL, Gawuga CE, Tyrka AR, et al. Association between plasma IL-6 response to acute stress and early-life adversity in healthy adults. Neuropsychopharmacology. 2010;35(13):2617-2623.
8. Messay B, Lim A, Marsland AL. Current understanding of the bi-directional relationship of major depression with inflammation. Biol Mood Anxiety Disord. 2012;2(1):4.
9. Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011;7(6):323-331.
1. Zunszain PA, Hepgul N, Pariante CM. Inflammation and depression. Curr Top Behav Neurosci. 2013;14:135-151.
2. Krishnadas R, Cavanagh J. Depression: an inflammatory illness? J Neurol Neurosurg Psychiatry. 2012;83(5):495-502.
3. Lotrich FE, El-Gabalawy H, Guenther LC, et al. The role of inflammation in the pathophysiology of depression: different treatments and their effects. J Rheumatol Suppl. 2011;88:48-54.
4. Gimeno D, Marmot MG, Singh-Manoux A. Inflammatory markers and cognitive function in middle-aged adults: the Whitehall II study. Psychoneuroendocrinology. 2008; 33(10):1322-1334.
5. Copeland WE, Shanahan L, Worthman C, et al. Cumulative depression episodes predict later C-reactive protein levels: a prospective analysis. Biol Psychiatry. 2012;71(1):15-21.
6. Chida Y, Sudo N, Sonoda J, et al. Early-life psychological stress exacerbates adult mouse asthma via the hypothalamus-pituitary-adrenal axis. Am J Respir Crit Care Med. 2007;175(4):316-322.
7. Carpenter LL, Gawuga CE, Tyrka AR, et al. Association between plasma IL-6 response to acute stress and early-life adversity in healthy adults. Neuropsychopharmacology. 2010;35(13):2617-2623.
8. Messay B, Lim A, Marsland AL. Current understanding of the bi-directional relationship of major depression with inflammation. Biol Mood Anxiety Disord. 2012;2(1):4.
9. Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011;7(6):323-331.
Dihydropyridine calcium channel blockers in dementia and hypertension
Dementia affects 34 million people globally, with the most common cause of dementia, Alzheimer’s disease (AD), affecting 5.5 million Americans.1,2 The connection between cerebrovascular disorders and AD means that antihypertensive agents may play a role in dementia prophylaxis and management.1,2
Hypertension increases the risk of intellectual dysfunction by increasing susceptibility to heart disease, ischemic brain injury, and cerebrovascular pathology.1 In addition to senile plaques, ischemic brain lesions are observed in autopsies of AD patients,1 and brain infarctions are more common among AD patients than among controls.2 Brain pathology suggestive of AD was found in 30% to 50% of postmortem examinations of patients with vascular dementia.1
It is useful to note that dihydropyridines, a subgroup of calcium channel blockers, may inhibit amyloidogenesis.3
Hypertension and cognition
Hypertension-induced hyperdense lesions in cerebral white matter reflect pathology in small vessels, inflammatory change, and disruption of the blood-brain barrier, which may precede cognitive decline.1 Even subclinical ischemic changes may increase the probability of developing dementia.2 Hypertension also reduces cerebral perfusion, especially in the hippocampus, which may promote degeneration of memory function.1 Prolonged cerebral hypoxia increases amyloid precursor protein production and β-secretase activity.1,2 Patients who died of brain ischemia show prominent β-amyloid protein and apolipoprotein E in histopathologic analysis of the hippocampus.1 Compression of vessels by â-amyloid protein further augments this degenerative process.1
Inhibition of amyloidogenesis
Long-term administration of antihypertensive medications in patients age <75 decreases the probability of dementia by 8% each year.1 Calcium channel blockers protect neurons by lowering blood pressure and reversing cellular-level calcium channel dysfunction that occurs with age, cerebral infarction, and AD.
Select dihydropyridines may inhibit amyloidogenesis in apolipoprotein E carriers:
• amlodipine and nilvadipine reduce β-secretase activity and amyloid precursor protein-β production3
• nilvadipine and nitrendipine limit β-amyloid protein synthesis in the brain and promote their clearance through the blood-brain barrier3
• nilvadipine-treated apolipoprotein E carriers experience cognitive stabilization compared with cognitive decreases seen in non-treated subjects.
Dihydropyridines can produce therapeutic effects for both AD and cerebrovascular dementia patients, indicating the potential that certain agents in this class have for treating both conditions.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Valenzuela M, Esler M, Ritchie K, et al. Antihypertensives for combating dementia? A perspective on candidate molecular mechanisms and population-based prevention. Transl Psychiatry. 2012;2:e107.
2. Pimentel-Coelho PM, Rivest S. The early contribution of cerebrovascular factors to the pathogenesis of Alzheimer’s disease. Eur J Neurosci. 2012;35(12):1917-1937.
3. Paris D, Bachmeier C, Patel N, et al. Selective antihypertensive dihydropyridines lower Aβ accumulation by targeting both the production and the clearance of Aβ across the blood-brain barrier. Mol Med. 2011;17(3-4):149-162.
Dementia affects 34 million people globally, with the most common cause of dementia, Alzheimer’s disease (AD), affecting 5.5 million Americans.1,2 The connection between cerebrovascular disorders and AD means that antihypertensive agents may play a role in dementia prophylaxis and management.1,2
Hypertension increases the risk of intellectual dysfunction by increasing susceptibility to heart disease, ischemic brain injury, and cerebrovascular pathology.1 In addition to senile plaques, ischemic brain lesions are observed in autopsies of AD patients,1 and brain infarctions are more common among AD patients than among controls.2 Brain pathology suggestive of AD was found in 30% to 50% of postmortem examinations of patients with vascular dementia.1
It is useful to note that dihydropyridines, a subgroup of calcium channel blockers, may inhibit amyloidogenesis.3
Hypertension and cognition
Hypertension-induced hyperdense lesions in cerebral white matter reflect pathology in small vessels, inflammatory change, and disruption of the blood-brain barrier, which may precede cognitive decline.1 Even subclinical ischemic changes may increase the probability of developing dementia.2 Hypertension also reduces cerebral perfusion, especially in the hippocampus, which may promote degeneration of memory function.1 Prolonged cerebral hypoxia increases amyloid precursor protein production and β-secretase activity.1,2 Patients who died of brain ischemia show prominent β-amyloid protein and apolipoprotein E in histopathologic analysis of the hippocampus.1 Compression of vessels by â-amyloid protein further augments this degenerative process.1
Inhibition of amyloidogenesis
Long-term administration of antihypertensive medications in patients age <75 decreases the probability of dementia by 8% each year.1 Calcium channel blockers protect neurons by lowering blood pressure and reversing cellular-level calcium channel dysfunction that occurs with age, cerebral infarction, and AD.
Select dihydropyridines may inhibit amyloidogenesis in apolipoprotein E carriers:
• amlodipine and nilvadipine reduce β-secretase activity and amyloid precursor protein-β production3
• nilvadipine and nitrendipine limit β-amyloid protein synthesis in the brain and promote their clearance through the blood-brain barrier3
• nilvadipine-treated apolipoprotein E carriers experience cognitive stabilization compared with cognitive decreases seen in non-treated subjects.
Dihydropyridines can produce therapeutic effects for both AD and cerebrovascular dementia patients, indicating the potential that certain agents in this class have for treating both conditions.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dementia affects 34 million people globally, with the most common cause of dementia, Alzheimer’s disease (AD), affecting 5.5 million Americans.1,2 The connection between cerebrovascular disorders and AD means that antihypertensive agents may play a role in dementia prophylaxis and management.1,2
Hypertension increases the risk of intellectual dysfunction by increasing susceptibility to heart disease, ischemic brain injury, and cerebrovascular pathology.1 In addition to senile plaques, ischemic brain lesions are observed in autopsies of AD patients,1 and brain infarctions are more common among AD patients than among controls.2 Brain pathology suggestive of AD was found in 30% to 50% of postmortem examinations of patients with vascular dementia.1
It is useful to note that dihydropyridines, a subgroup of calcium channel blockers, may inhibit amyloidogenesis.3
Hypertension and cognition
Hypertension-induced hyperdense lesions in cerebral white matter reflect pathology in small vessels, inflammatory change, and disruption of the blood-brain barrier, which may precede cognitive decline.1 Even subclinical ischemic changes may increase the probability of developing dementia.2 Hypertension also reduces cerebral perfusion, especially in the hippocampus, which may promote degeneration of memory function.1 Prolonged cerebral hypoxia increases amyloid precursor protein production and β-secretase activity.1,2 Patients who died of brain ischemia show prominent β-amyloid protein and apolipoprotein E in histopathologic analysis of the hippocampus.1 Compression of vessels by â-amyloid protein further augments this degenerative process.1
Inhibition of amyloidogenesis
Long-term administration of antihypertensive medications in patients age <75 decreases the probability of dementia by 8% each year.1 Calcium channel blockers protect neurons by lowering blood pressure and reversing cellular-level calcium channel dysfunction that occurs with age, cerebral infarction, and AD.
Select dihydropyridines may inhibit amyloidogenesis in apolipoprotein E carriers:
• amlodipine and nilvadipine reduce β-secretase activity and amyloid precursor protein-β production3
• nilvadipine and nitrendipine limit β-amyloid protein synthesis in the brain and promote their clearance through the blood-brain barrier3
• nilvadipine-treated apolipoprotein E carriers experience cognitive stabilization compared with cognitive decreases seen in non-treated subjects.
Dihydropyridines can produce therapeutic effects for both AD and cerebrovascular dementia patients, indicating the potential that certain agents in this class have for treating both conditions.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Valenzuela M, Esler M, Ritchie K, et al. Antihypertensives for combating dementia? A perspective on candidate molecular mechanisms and population-based prevention. Transl Psychiatry. 2012;2:e107.
2. Pimentel-Coelho PM, Rivest S. The early contribution of cerebrovascular factors to the pathogenesis of Alzheimer’s disease. Eur J Neurosci. 2012;35(12):1917-1937.
3. Paris D, Bachmeier C, Patel N, et al. Selective antihypertensive dihydropyridines lower Aβ accumulation by targeting both the production and the clearance of Aβ across the blood-brain barrier. Mol Med. 2011;17(3-4):149-162.
1. Valenzuela M, Esler M, Ritchie K, et al. Antihypertensives for combating dementia? A perspective on candidate molecular mechanisms and population-based prevention. Transl Psychiatry. 2012;2:e107.
2. Pimentel-Coelho PM, Rivest S. The early contribution of cerebrovascular factors to the pathogenesis of Alzheimer’s disease. Eur J Neurosci. 2012;35(12):1917-1937.
3. Paris D, Bachmeier C, Patel N, et al. Selective antihypertensive dihydropyridines lower Aβ accumulation by targeting both the production and the clearance of Aβ across the blood-brain barrier. Mol Med. 2011;17(3-4):149-162.