User login
Interventions Effective in Preventing Hospital Readmissions
Clinical question: Which interventions are most effective to prevent 30-day readmissions in medical or surgical patients?
Background: Preventing early readmissions has become a national priority. This study set out to determine which intervention had the largest impact on the prevention of early readmission.
Study design: Meta-analysis.
Setting: Forty-seven studies in multiple locations.
Synopsis: This study evaluated 47 randomized trials that assessed the effectiveness of peri-discharge interventions on the risk of all-cause or unplanned 30-day readmissions for medical and surgical patients. Outcomes included unplanned readmissions, all-cause readmissions, and a composite of unplanned and all-cause readmissions plus out-of-hospital deaths.
The included studies reported up to seven methods of preventing readmissions, including involvement of case management, home visits, education of patients, and self-care support. In 42 trials reporting readmission rates, the pooled relative risk of readmission was 0.82 (95 % CI, 0.73-0.91; P<0.001) within 30 days.
Multiple subgroup analyses noted that the most effective interventions on hospital readmission were those that were more complex and those that sought to augment patient capacity to access and enact dependable post-discharge care.
Limitations included single-center academic studies, lack of standard for dealing with missing data, existence of publication bias, and differing methods used to evaluate intervention effects.
Bottom line: This study was the largest of its kind, to date, and suggests that the interventions analyzed in this study, although complex (e.g. enhancing capacity for self-care at home), were efficacious in reducing 30-day readmissions.
Citation: Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107.
Clinical question: Which interventions are most effective to prevent 30-day readmissions in medical or surgical patients?
Background: Preventing early readmissions has become a national priority. This study set out to determine which intervention had the largest impact on the prevention of early readmission.
Study design: Meta-analysis.
Setting: Forty-seven studies in multiple locations.
Synopsis: This study evaluated 47 randomized trials that assessed the effectiveness of peri-discharge interventions on the risk of all-cause or unplanned 30-day readmissions for medical and surgical patients. Outcomes included unplanned readmissions, all-cause readmissions, and a composite of unplanned and all-cause readmissions plus out-of-hospital deaths.
The included studies reported up to seven methods of preventing readmissions, including involvement of case management, home visits, education of patients, and self-care support. In 42 trials reporting readmission rates, the pooled relative risk of readmission was 0.82 (95 % CI, 0.73-0.91; P<0.001) within 30 days.
Multiple subgroup analyses noted that the most effective interventions on hospital readmission were those that were more complex and those that sought to augment patient capacity to access and enact dependable post-discharge care.
Limitations included single-center academic studies, lack of standard for dealing with missing data, existence of publication bias, and differing methods used to evaluate intervention effects.
Bottom line: This study was the largest of its kind, to date, and suggests that the interventions analyzed in this study, although complex (e.g. enhancing capacity for self-care at home), were efficacious in reducing 30-day readmissions.
Citation: Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107.
Clinical question: Which interventions are most effective to prevent 30-day readmissions in medical or surgical patients?
Background: Preventing early readmissions has become a national priority. This study set out to determine which intervention had the largest impact on the prevention of early readmission.
Study design: Meta-analysis.
Setting: Forty-seven studies in multiple locations.
Synopsis: This study evaluated 47 randomized trials that assessed the effectiveness of peri-discharge interventions on the risk of all-cause or unplanned 30-day readmissions for medical and surgical patients. Outcomes included unplanned readmissions, all-cause readmissions, and a composite of unplanned and all-cause readmissions plus out-of-hospital deaths.
The included studies reported up to seven methods of preventing readmissions, including involvement of case management, home visits, education of patients, and self-care support. In 42 trials reporting readmission rates, the pooled relative risk of readmission was 0.82 (95 % CI, 0.73-0.91; P<0.001) within 30 days.
Multiple subgroup analyses noted that the most effective interventions on hospital readmission were those that were more complex and those that sought to augment patient capacity to access and enact dependable post-discharge care.
Limitations included single-center academic studies, lack of standard for dealing with missing data, existence of publication bias, and differing methods used to evaluate intervention effects.
Bottom line: This study was the largest of its kind, to date, and suggests that the interventions analyzed in this study, although complex (e.g. enhancing capacity for self-care at home), were efficacious in reducing 30-day readmissions.
Citation: Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-1107.
How Should Acute Alcoholic Hepatitis be Treated?
Case
A 53-year-old man with a history of daily alcohol use presents with one week of jaundice. His blood pressure is 95/60 mmHg, pulse 105/minute, and temperature 38.0°C. Examination discloses icterus, ascites, and an enlarged, tender liver. His bilirubin is 9 mg/dl, AST 250 IU/dL, ALT 115 IU/dL, prothromin time 22 seconds, INR 2.7, creatinine 0.9 mg/dL, and leukocyte count 15,000/cu mm with 70% neutrophils. He is admitted with a diagnosis of acute alcoholic hepatitis. How should he be treated?
Background
Hospitalists frequently encounter patients who use alcohol and have abnormal liver tests. Regular, heavy alcohol consumption is associated with a variety of forms of liver disease, including fatty liver, inflammation, hepatic fibrosis, and cirrhosis. The term “alcoholic hepatitis” describes a more severe form of alcohol-related liver disease associated with significant short-term mortality.
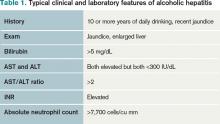
Alcoholic hepatitis typically occurs after more than 10 years of regular heavy alcohol use; average consumption in one study was 100 g/day (the equivalent of 10 drinks per day).1 The typical patient presents with recent onset of jaundice, ascites, and proximal muscle loss. Fever and leukocytosis also are common but should prompt an evaluation for infection, especially spontaneous bacterial peritonitis. Liver biopsy in these patients shows steatosis, swollen hepatocytes containing eosinophilic inclusion (Mallory) bodies, and a prominent neutrophilic inflammatory cell infiltrate. Because of the accuracy of clinical diagnosis, biopsy is rarely required, relying instead on clinical and laboratory features for diagnosis (see Table 1, below).
Prognosis can be determined with prediction models. The most common are Model for End-Stage Liver Disease (MELD) and Maddrey’s discriminate score (see Table 2). Several websites allow quick calculation of these scores and provide estimated 30-day or 90-day mortality. These scores can be used to guide therapy.
Review of the Data
How should hospitalists treat this serious illness? The evidence-based literature supporting the efficacy of treatments for alcoholic hepatitis is limited, and expert opinions sometimes conflict.
Abstinence has been shown to improve survival in all stages of alcohol-related liver disease.2 This can be accomplished by admitting this patient population to the hospital. A number of interventions and therapies are available to increase the chance of continued abstinence following discharge (see Table 3).
Nutritional support. Protein-calorie malnutrition is seen in up to 90% of patients with cirrhosis.3 The cause of malnutrition in these patients includes decreased caloric intake, metabolic derangements that accompany liver disease, and micronutrient and vitamin deficiencies. Many of these patients rely almost solely on alcohol for caloric intake; this contributes to potassium depletion, which is frequently seen. After admission, these patients are often evaluated for other conditions (such as gastrointestinal bleeding and altered mental status) that require them to be NPO overnight, thus further confounding their malnutrition. Enteral nutritional support was shown in a multicenter study to be associated with reduced infectious complications and improved one-year mortality.4
Little clinical data support specific recommendations for the amount of nutritional support. The American College of Gastroenterology (ACG) recommends 35 calories/kg to 40 calories/kg of body weight per day and a protein intake of 1.2 g/kg to 1.5g/kg per day.5 In an average, 70-kg patient, this is 2,450 to 2,800 calories a day. For patients who are not able to meet these nutritional needs by mouth, enteral feeding with a small-bore (Dobhoff) feeding tube can be used, even in patients with known esophageal varices.
Most of these patients have anorexia and nausea and do not meet these caloric recommendations by eating. Nutritional support is a low-risk intervention that can be provided on almost all inpatient medical care areas. Hospitalists should be attentive to nutritional support early in the hospitalization of these patients.
Corticosteroid therapy is recommended by the ACG for patients with alcoholic hepatitis and a Maddrey’s discriminant function greater than 32.5 There is much debate about this recommendation, as conflicting data about efficacy exist.
A 2008 Cochrane review included clinical trials published before July 2007 that examined corticosteroid use in patients with alcoholic hepatitis. A total of 15 trials with 721 randomized patients were included. The review concluded that corticosteroids did not statistically reduce mortality compared with placebo or no intervention; however, mortality was reduced in the subgroup of patients with Maddrey’s scores greater than 32 and hepatic encephalopathy.6 The review concluded that current evidence does not support the use of corticosteroids in alcoholic hepatitis, and more randomized trials were needed.
Another meta-analysis demonstrated a mortality benefit when the largest studies, which included 221 patients with high Maddrey’s scores, were analyzed separately.7 Contraindications to corticosteroid treatment include active infection, gastrointestinal bleeding, acute pancreatitis, and renal failure. Other concerns about corticosteroids include potential adverse reactions (hyperglycemia) and increased risk of infection. Prednisolone is preferred over prednisone because it is the active drug. The recommended dosage is 40 mg/day for 28 days followed by a taper (20 mg/day for one week, then 10 mg/day for one week).
Some data suggest that if patients on corticosteroid therapy do not demonstrate a decrease in their bilirubin levels by Day 7, they are at higher risk of developing infections, have a poorer prognosis, and that corticosteroid therapy should be stopped.8 Some experts use the Lille model to decide whether to continue corticosteroids. In one study, patients who did not respond to prednisolone did not improve when switched to pentoxifyline.9
Patients discharged on corticosteroids require very careful coordination with outpatient providers as prolonged corticosteroid treatment courses can lead to serious complications and death. Critics of corticosteroid therapy in these patients often cite problems related to prolonged steroid use, especially in patients who do not respond to therapy.10
Pentoxifylline, an oral phosphodiesterase inhibitor, is recommended by the ACG, especially if corticosteroids are contraindicated.5 In 2008, 101 patients with alcoholic hepatitis were enrolled in a double-blind, placebo-controlled trial comparing pentoxifylline and placebo. This study demonstrated that patients who received pentoxifylline had decreased 28-day mortality (24.6% versus 46% receiving placebo). Of those patients who died during the study, only 50% (versus 91% in the placebo group) developed hepatorenal syndrome.11 However, a Cochrane review of all studies with pentoxifylline concluded that no firm conclusions could be drawn.12
One small, randomized trial comparing pentoxifylline with prednisolone demonstrated that pentoxifylline was superior.13 Pentoxifylline can be prescribed to patients who have contraindications to corticosteroid use (infection or gastrointestinal bleeding). The recommended dose is 400 mg orally three times daily (TID) for four weeks. Common side effects are nausea and vomiting. Pentoxifylline cannot be administered by nasogastric tubes and should not be used in patients with recent cerebral or retinal hemorrhage.
Other therapies. Several studies have examined vitamin E, N-acetylcystine, and other antioxidants as treatment for alcoholic hepatitis. No clear benefit has been demonstrated for any of these drugs. Tumor necrosis factor (TNF)-alpha inhibitors (e.g. infliximab) have been studied, but increased mortality was demonstrated and these studies were discontinued. Patients are not usually considered for liver transplantation until they have at least six months of abstinence from alcohol as recommended by the American Society of Transplantation.14
Discharge considerations. No clinical trials have studied optimal timing of discharge. Expert opinion based on clinical experience recommends that patients be kept in the hospital until they are eating, signs of alcohol withdrawal and encephalopathy are absent, and bilirubin is less than 10 mg/dL.14 These patients often are quite sick and hospitalization frequently exceeds 10 days. Careful outpatient follow-up and assistance with continued abstinence is very important.
Back to the Case
The patient fits the typical clinical picture of alcoholic hepatitis. Cessation of alcohol consumption is the most important treatment and is accomplished by admission to the hospital. Because of his daily alcohol consumption, folate, thiamine, multivitamins, and oral vitamin K are ordered. Though he has no symptoms of alcohol withdrawal, a note is added about potential withdrawal to the handoff report.
An infectious workup is completed by ordering blood and urine cultures, a chest X-ray, and performing paracentesis to exclude spontaneous bacterial peritonitis. A dietary consult with calorie count is given, along with a plan to discuss with the patient the importance of consuming at least 2,500 calories a day is made. Tube feedings will be considered if the patient does not meet this goal in 48 hours. Clinical calculators determine his Maddrey’s and MELD scores (50 and 25, respectively). If he is actively bleeding or infected, pentoxifylline (400 mg TID for 28 days) is favored due to its lower-side-effect profile.
His MELD score predicts a 90-day mortality of 43%; a meeting is planned to discuss code status and end-of-life issues with the patient and his family. Due to the severity of his illness, a gastroenterology consultation is recommended.
Bottom Line
Alcoholic hepatitis is a serious disease with significant short-term mortality. Treatment options are limited but include abstinence from alcohol, supplemental nutrition, and, for select patients, pentoxifylline or corticosteroids. Because most transplant centers require six months of abstinence, these patients usually are not eligible for urgent liver transplantation.
Dr. Parada is a clinical instructor and chief medical resident in the Department of Internal Medicine at the University of New Mexico School of Medicine and the University of New Mexico Hospital, Albuquerque. Dr. Pierce is associate professor in the Division of Hospital Medicine at the University of New Mexico School of Medicine and the University of New Mexico Hospital.
References
- Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology. 1997;25:108-111.
- Pessione F, Ramond MJ, Peters L, et al. Five-year survival predictive factors in patients with excessive alcohol intake and cirrhosis. Effect of alcoholic hepatitis, smoking and abstinence. Liver Int. 2003;23:45-53.
- Mendenhall CL, Anderson S, Weesner RE, Goldberg SJ, Crolic KA. Protein-calorie malnutrition associated with alcoholic hepatitis. Veterans Administration Cooperative Study Group on alcoholic hepatitis. Am J Med. 1984;76:211-222.
- Cabre E, Rodriguez-Iglesias P, Caballeria J, et al. Short- and long-term outcome of severe alcohol-induced hepatitis treated with steroids or enteral nutrition: a multicenter randomized trial. Hepatology. 2000;32:36-42.
- O’Shea RS, Dasarathy S, McCullough AJ, Practice Guideline Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology. 2010;51:307-328.
- Rambaldi A, Saconato HH, Christensen E, Thorlund K, Wetterslev J, Gluud C. Systematic review: Glucocorticosteroids for alcoholic hepatitis—a Cochrane hepato-biliary group systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. Aliment Pharmacol Ther. 2008;27:1167-1178.
- Mathurin P, Mendenhall CL, Carithers RL Jr., et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol. 2002;36:480-487.
- Louvet A, Naveau S, Abdelnour M, et al. The Lille model: A new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology. 2007;45:1348-1354.
- Louvet A, Diaz E, Dharancy S, et al. Early switch topentoxifylline in patients with severe alcoholic hepatitis is inefficient in non-responders to corticosteroids. J Hepatol. 2008;48:465-470.
- Amini M, Runyon BA. Alcoholic hepatitis 2010: A clinician’s guide to diagnosis and therapy. World J Gastroenterol. 2010;16:4905-4912.
- Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: A double-blind, placebo-controlled trial. Gastroenterology. 2000;119:1637-1648.
- Whitfield K, Rambaldi A, Wetterslev J, Gluud C. Pentoxifylline for alcoholic hepatitis. Cochrane Database Syst Rev. 2009;(4):CD007339.
- De BK, Gangopadhyay S, Dutta D, Baksi SD, Pani A, Ghosh P. Pentoxifylline versus prednisolone for severe alcoholic hepatitis: A randomized controlled trial. World J Gastroenterol. 2009;15:1613-1619.
- Lucey MR, Brown KA, Everson GT, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997;3:628-637.
Case
A 53-year-old man with a history of daily alcohol use presents with one week of jaundice. His blood pressure is 95/60 mmHg, pulse 105/minute, and temperature 38.0°C. Examination discloses icterus, ascites, and an enlarged, tender liver. His bilirubin is 9 mg/dl, AST 250 IU/dL, ALT 115 IU/dL, prothromin time 22 seconds, INR 2.7, creatinine 0.9 mg/dL, and leukocyte count 15,000/cu mm with 70% neutrophils. He is admitted with a diagnosis of acute alcoholic hepatitis. How should he be treated?
Background
Hospitalists frequently encounter patients who use alcohol and have abnormal liver tests. Regular, heavy alcohol consumption is associated with a variety of forms of liver disease, including fatty liver, inflammation, hepatic fibrosis, and cirrhosis. The term “alcoholic hepatitis” describes a more severe form of alcohol-related liver disease associated with significant short-term mortality.
Alcoholic hepatitis typically occurs after more than 10 years of regular heavy alcohol use; average consumption in one study was 100 g/day (the equivalent of 10 drinks per day).1 The typical patient presents with recent onset of jaundice, ascites, and proximal muscle loss. Fever and leukocytosis also are common but should prompt an evaluation for infection, especially spontaneous bacterial peritonitis. Liver biopsy in these patients shows steatosis, swollen hepatocytes containing eosinophilic inclusion (Mallory) bodies, and a prominent neutrophilic inflammatory cell infiltrate. Because of the accuracy of clinical diagnosis, biopsy is rarely required, relying instead on clinical and laboratory features for diagnosis (see Table 1, below).
Prognosis can be determined with prediction models. The most common are Model for End-Stage Liver Disease (MELD) and Maddrey’s discriminate score (see Table 2). Several websites allow quick calculation of these scores and provide estimated 30-day or 90-day mortality. These scores can be used to guide therapy.
Review of the Data
How should hospitalists treat this serious illness? The evidence-based literature supporting the efficacy of treatments for alcoholic hepatitis is limited, and expert opinions sometimes conflict.
Abstinence has been shown to improve survival in all stages of alcohol-related liver disease.2 This can be accomplished by admitting this patient population to the hospital. A number of interventions and therapies are available to increase the chance of continued abstinence following discharge (see Table 3).
Nutritional support. Protein-calorie malnutrition is seen in up to 90% of patients with cirrhosis.3 The cause of malnutrition in these patients includes decreased caloric intake, metabolic derangements that accompany liver disease, and micronutrient and vitamin deficiencies. Many of these patients rely almost solely on alcohol for caloric intake; this contributes to potassium depletion, which is frequently seen. After admission, these patients are often evaluated for other conditions (such as gastrointestinal bleeding and altered mental status) that require them to be NPO overnight, thus further confounding their malnutrition. Enteral nutritional support was shown in a multicenter study to be associated with reduced infectious complications and improved one-year mortality.4
Little clinical data support specific recommendations for the amount of nutritional support. The American College of Gastroenterology (ACG) recommends 35 calories/kg to 40 calories/kg of body weight per day and a protein intake of 1.2 g/kg to 1.5g/kg per day.5 In an average, 70-kg patient, this is 2,450 to 2,800 calories a day. For patients who are not able to meet these nutritional needs by mouth, enteral feeding with a small-bore (Dobhoff) feeding tube can be used, even in patients with known esophageal varices.
Most of these patients have anorexia and nausea and do not meet these caloric recommendations by eating. Nutritional support is a low-risk intervention that can be provided on almost all inpatient medical care areas. Hospitalists should be attentive to nutritional support early in the hospitalization of these patients.
Corticosteroid therapy is recommended by the ACG for patients with alcoholic hepatitis and a Maddrey’s discriminant function greater than 32.5 There is much debate about this recommendation, as conflicting data about efficacy exist.
A 2008 Cochrane review included clinical trials published before July 2007 that examined corticosteroid use in patients with alcoholic hepatitis. A total of 15 trials with 721 randomized patients were included. The review concluded that corticosteroids did not statistically reduce mortality compared with placebo or no intervention; however, mortality was reduced in the subgroup of patients with Maddrey’s scores greater than 32 and hepatic encephalopathy.6 The review concluded that current evidence does not support the use of corticosteroids in alcoholic hepatitis, and more randomized trials were needed.
Another meta-analysis demonstrated a mortality benefit when the largest studies, which included 221 patients with high Maddrey’s scores, were analyzed separately.7 Contraindications to corticosteroid treatment include active infection, gastrointestinal bleeding, acute pancreatitis, and renal failure. Other concerns about corticosteroids include potential adverse reactions (hyperglycemia) and increased risk of infection. Prednisolone is preferred over prednisone because it is the active drug. The recommended dosage is 40 mg/day for 28 days followed by a taper (20 mg/day for one week, then 10 mg/day for one week).
Some data suggest that if patients on corticosteroid therapy do not demonstrate a decrease in their bilirubin levels by Day 7, they are at higher risk of developing infections, have a poorer prognosis, and that corticosteroid therapy should be stopped.8 Some experts use the Lille model to decide whether to continue corticosteroids. In one study, patients who did not respond to prednisolone did not improve when switched to pentoxifyline.9
Patients discharged on corticosteroids require very careful coordination with outpatient providers as prolonged corticosteroid treatment courses can lead to serious complications and death. Critics of corticosteroid therapy in these patients often cite problems related to prolonged steroid use, especially in patients who do not respond to therapy.10
Pentoxifylline, an oral phosphodiesterase inhibitor, is recommended by the ACG, especially if corticosteroids are contraindicated.5 In 2008, 101 patients with alcoholic hepatitis were enrolled in a double-blind, placebo-controlled trial comparing pentoxifylline and placebo. This study demonstrated that patients who received pentoxifylline had decreased 28-day mortality (24.6% versus 46% receiving placebo). Of those patients who died during the study, only 50% (versus 91% in the placebo group) developed hepatorenal syndrome.11 However, a Cochrane review of all studies with pentoxifylline concluded that no firm conclusions could be drawn.12
One small, randomized trial comparing pentoxifylline with prednisolone demonstrated that pentoxifylline was superior.13 Pentoxifylline can be prescribed to patients who have contraindications to corticosteroid use (infection or gastrointestinal bleeding). The recommended dose is 400 mg orally three times daily (TID) for four weeks. Common side effects are nausea and vomiting. Pentoxifylline cannot be administered by nasogastric tubes and should not be used in patients with recent cerebral or retinal hemorrhage.
Other therapies. Several studies have examined vitamin E, N-acetylcystine, and other antioxidants as treatment for alcoholic hepatitis. No clear benefit has been demonstrated for any of these drugs. Tumor necrosis factor (TNF)-alpha inhibitors (e.g. infliximab) have been studied, but increased mortality was demonstrated and these studies were discontinued. Patients are not usually considered for liver transplantation until they have at least six months of abstinence from alcohol as recommended by the American Society of Transplantation.14
Discharge considerations. No clinical trials have studied optimal timing of discharge. Expert opinion based on clinical experience recommends that patients be kept in the hospital until they are eating, signs of alcohol withdrawal and encephalopathy are absent, and bilirubin is less than 10 mg/dL.14 These patients often are quite sick and hospitalization frequently exceeds 10 days. Careful outpatient follow-up and assistance with continued abstinence is very important.
Back to the Case
The patient fits the typical clinical picture of alcoholic hepatitis. Cessation of alcohol consumption is the most important treatment and is accomplished by admission to the hospital. Because of his daily alcohol consumption, folate, thiamine, multivitamins, and oral vitamin K are ordered. Though he has no symptoms of alcohol withdrawal, a note is added about potential withdrawal to the handoff report.
An infectious workup is completed by ordering blood and urine cultures, a chest X-ray, and performing paracentesis to exclude spontaneous bacterial peritonitis. A dietary consult with calorie count is given, along with a plan to discuss with the patient the importance of consuming at least 2,500 calories a day is made. Tube feedings will be considered if the patient does not meet this goal in 48 hours. Clinical calculators determine his Maddrey’s and MELD scores (50 and 25, respectively). If he is actively bleeding or infected, pentoxifylline (400 mg TID for 28 days) is favored due to its lower-side-effect profile.
His MELD score predicts a 90-day mortality of 43%; a meeting is planned to discuss code status and end-of-life issues with the patient and his family. Due to the severity of his illness, a gastroenterology consultation is recommended.
Bottom Line
Alcoholic hepatitis is a serious disease with significant short-term mortality. Treatment options are limited but include abstinence from alcohol, supplemental nutrition, and, for select patients, pentoxifylline or corticosteroids. Because most transplant centers require six months of abstinence, these patients usually are not eligible for urgent liver transplantation.
Dr. Parada is a clinical instructor and chief medical resident in the Department of Internal Medicine at the University of New Mexico School of Medicine and the University of New Mexico Hospital, Albuquerque. Dr. Pierce is associate professor in the Division of Hospital Medicine at the University of New Mexico School of Medicine and the University of New Mexico Hospital.
References
- Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology. 1997;25:108-111.
- Pessione F, Ramond MJ, Peters L, et al. Five-year survival predictive factors in patients with excessive alcohol intake and cirrhosis. Effect of alcoholic hepatitis, smoking and abstinence. Liver Int. 2003;23:45-53.
- Mendenhall CL, Anderson S, Weesner RE, Goldberg SJ, Crolic KA. Protein-calorie malnutrition associated with alcoholic hepatitis. Veterans Administration Cooperative Study Group on alcoholic hepatitis. Am J Med. 1984;76:211-222.
- Cabre E, Rodriguez-Iglesias P, Caballeria J, et al. Short- and long-term outcome of severe alcohol-induced hepatitis treated with steroids or enteral nutrition: a multicenter randomized trial. Hepatology. 2000;32:36-42.
- O’Shea RS, Dasarathy S, McCullough AJ, Practice Guideline Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology. 2010;51:307-328.
- Rambaldi A, Saconato HH, Christensen E, Thorlund K, Wetterslev J, Gluud C. Systematic review: Glucocorticosteroids for alcoholic hepatitis—a Cochrane hepato-biliary group systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. Aliment Pharmacol Ther. 2008;27:1167-1178.
- Mathurin P, Mendenhall CL, Carithers RL Jr., et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol. 2002;36:480-487.
- Louvet A, Naveau S, Abdelnour M, et al. The Lille model: A new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology. 2007;45:1348-1354.
- Louvet A, Diaz E, Dharancy S, et al. Early switch topentoxifylline in patients with severe alcoholic hepatitis is inefficient in non-responders to corticosteroids. J Hepatol. 2008;48:465-470.
- Amini M, Runyon BA. Alcoholic hepatitis 2010: A clinician’s guide to diagnosis and therapy. World J Gastroenterol. 2010;16:4905-4912.
- Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: A double-blind, placebo-controlled trial. Gastroenterology. 2000;119:1637-1648.
- Whitfield K, Rambaldi A, Wetterslev J, Gluud C. Pentoxifylline for alcoholic hepatitis. Cochrane Database Syst Rev. 2009;(4):CD007339.
- De BK, Gangopadhyay S, Dutta D, Baksi SD, Pani A, Ghosh P. Pentoxifylline versus prednisolone for severe alcoholic hepatitis: A randomized controlled trial. World J Gastroenterol. 2009;15:1613-1619.
- Lucey MR, Brown KA, Everson GT, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997;3:628-637.
Case
A 53-year-old man with a history of daily alcohol use presents with one week of jaundice. His blood pressure is 95/60 mmHg, pulse 105/minute, and temperature 38.0°C. Examination discloses icterus, ascites, and an enlarged, tender liver. His bilirubin is 9 mg/dl, AST 250 IU/dL, ALT 115 IU/dL, prothromin time 22 seconds, INR 2.7, creatinine 0.9 mg/dL, and leukocyte count 15,000/cu mm with 70% neutrophils. He is admitted with a diagnosis of acute alcoholic hepatitis. How should he be treated?
Background
Hospitalists frequently encounter patients who use alcohol and have abnormal liver tests. Regular, heavy alcohol consumption is associated with a variety of forms of liver disease, including fatty liver, inflammation, hepatic fibrosis, and cirrhosis. The term “alcoholic hepatitis” describes a more severe form of alcohol-related liver disease associated with significant short-term mortality.
Alcoholic hepatitis typically occurs after more than 10 years of regular heavy alcohol use; average consumption in one study was 100 g/day (the equivalent of 10 drinks per day).1 The typical patient presents with recent onset of jaundice, ascites, and proximal muscle loss. Fever and leukocytosis also are common but should prompt an evaluation for infection, especially spontaneous bacterial peritonitis. Liver biopsy in these patients shows steatosis, swollen hepatocytes containing eosinophilic inclusion (Mallory) bodies, and a prominent neutrophilic inflammatory cell infiltrate. Because of the accuracy of clinical diagnosis, biopsy is rarely required, relying instead on clinical and laboratory features for diagnosis (see Table 1, below).
Prognosis can be determined with prediction models. The most common are Model for End-Stage Liver Disease (MELD) and Maddrey’s discriminate score (see Table 2). Several websites allow quick calculation of these scores and provide estimated 30-day or 90-day mortality. These scores can be used to guide therapy.
Review of the Data
How should hospitalists treat this serious illness? The evidence-based literature supporting the efficacy of treatments for alcoholic hepatitis is limited, and expert opinions sometimes conflict.
Abstinence has been shown to improve survival in all stages of alcohol-related liver disease.2 This can be accomplished by admitting this patient population to the hospital. A number of interventions and therapies are available to increase the chance of continued abstinence following discharge (see Table 3).
Nutritional support. Protein-calorie malnutrition is seen in up to 90% of patients with cirrhosis.3 The cause of malnutrition in these patients includes decreased caloric intake, metabolic derangements that accompany liver disease, and micronutrient and vitamin deficiencies. Many of these patients rely almost solely on alcohol for caloric intake; this contributes to potassium depletion, which is frequently seen. After admission, these patients are often evaluated for other conditions (such as gastrointestinal bleeding and altered mental status) that require them to be NPO overnight, thus further confounding their malnutrition. Enteral nutritional support was shown in a multicenter study to be associated with reduced infectious complications and improved one-year mortality.4
Little clinical data support specific recommendations for the amount of nutritional support. The American College of Gastroenterology (ACG) recommends 35 calories/kg to 40 calories/kg of body weight per day and a protein intake of 1.2 g/kg to 1.5g/kg per day.5 In an average, 70-kg patient, this is 2,450 to 2,800 calories a day. For patients who are not able to meet these nutritional needs by mouth, enteral feeding with a small-bore (Dobhoff) feeding tube can be used, even in patients with known esophageal varices.
Most of these patients have anorexia and nausea and do not meet these caloric recommendations by eating. Nutritional support is a low-risk intervention that can be provided on almost all inpatient medical care areas. Hospitalists should be attentive to nutritional support early in the hospitalization of these patients.
Corticosteroid therapy is recommended by the ACG for patients with alcoholic hepatitis and a Maddrey’s discriminant function greater than 32.5 There is much debate about this recommendation, as conflicting data about efficacy exist.
A 2008 Cochrane review included clinical trials published before July 2007 that examined corticosteroid use in patients with alcoholic hepatitis. A total of 15 trials with 721 randomized patients were included. The review concluded that corticosteroids did not statistically reduce mortality compared with placebo or no intervention; however, mortality was reduced in the subgroup of patients with Maddrey’s scores greater than 32 and hepatic encephalopathy.6 The review concluded that current evidence does not support the use of corticosteroids in alcoholic hepatitis, and more randomized trials were needed.
Another meta-analysis demonstrated a mortality benefit when the largest studies, which included 221 patients with high Maddrey’s scores, were analyzed separately.7 Contraindications to corticosteroid treatment include active infection, gastrointestinal bleeding, acute pancreatitis, and renal failure. Other concerns about corticosteroids include potential adverse reactions (hyperglycemia) and increased risk of infection. Prednisolone is preferred over prednisone because it is the active drug. The recommended dosage is 40 mg/day for 28 days followed by a taper (20 mg/day for one week, then 10 mg/day for one week).
Some data suggest that if patients on corticosteroid therapy do not demonstrate a decrease in their bilirubin levels by Day 7, they are at higher risk of developing infections, have a poorer prognosis, and that corticosteroid therapy should be stopped.8 Some experts use the Lille model to decide whether to continue corticosteroids. In one study, patients who did not respond to prednisolone did not improve when switched to pentoxifyline.9
Patients discharged on corticosteroids require very careful coordination with outpatient providers as prolonged corticosteroid treatment courses can lead to serious complications and death. Critics of corticosteroid therapy in these patients often cite problems related to prolonged steroid use, especially in patients who do not respond to therapy.10
Pentoxifylline, an oral phosphodiesterase inhibitor, is recommended by the ACG, especially if corticosteroids are contraindicated.5 In 2008, 101 patients with alcoholic hepatitis were enrolled in a double-blind, placebo-controlled trial comparing pentoxifylline and placebo. This study demonstrated that patients who received pentoxifylline had decreased 28-day mortality (24.6% versus 46% receiving placebo). Of those patients who died during the study, only 50% (versus 91% in the placebo group) developed hepatorenal syndrome.11 However, a Cochrane review of all studies with pentoxifylline concluded that no firm conclusions could be drawn.12
One small, randomized trial comparing pentoxifylline with prednisolone demonstrated that pentoxifylline was superior.13 Pentoxifylline can be prescribed to patients who have contraindications to corticosteroid use (infection or gastrointestinal bleeding). The recommended dose is 400 mg orally three times daily (TID) for four weeks. Common side effects are nausea and vomiting. Pentoxifylline cannot be administered by nasogastric tubes and should not be used in patients with recent cerebral or retinal hemorrhage.
Other therapies. Several studies have examined vitamin E, N-acetylcystine, and other antioxidants as treatment for alcoholic hepatitis. No clear benefit has been demonstrated for any of these drugs. Tumor necrosis factor (TNF)-alpha inhibitors (e.g. infliximab) have been studied, but increased mortality was demonstrated and these studies were discontinued. Patients are not usually considered for liver transplantation until they have at least six months of abstinence from alcohol as recommended by the American Society of Transplantation.14
Discharge considerations. No clinical trials have studied optimal timing of discharge. Expert opinion based on clinical experience recommends that patients be kept in the hospital until they are eating, signs of alcohol withdrawal and encephalopathy are absent, and bilirubin is less than 10 mg/dL.14 These patients often are quite sick and hospitalization frequently exceeds 10 days. Careful outpatient follow-up and assistance with continued abstinence is very important.
Back to the Case
The patient fits the typical clinical picture of alcoholic hepatitis. Cessation of alcohol consumption is the most important treatment and is accomplished by admission to the hospital. Because of his daily alcohol consumption, folate, thiamine, multivitamins, and oral vitamin K are ordered. Though he has no symptoms of alcohol withdrawal, a note is added about potential withdrawal to the handoff report.
An infectious workup is completed by ordering blood and urine cultures, a chest X-ray, and performing paracentesis to exclude spontaneous bacterial peritonitis. A dietary consult with calorie count is given, along with a plan to discuss with the patient the importance of consuming at least 2,500 calories a day is made. Tube feedings will be considered if the patient does not meet this goal in 48 hours. Clinical calculators determine his Maddrey’s and MELD scores (50 and 25, respectively). If he is actively bleeding or infected, pentoxifylline (400 mg TID for 28 days) is favored due to its lower-side-effect profile.
His MELD score predicts a 90-day mortality of 43%; a meeting is planned to discuss code status and end-of-life issues with the patient and his family. Due to the severity of his illness, a gastroenterology consultation is recommended.
Bottom Line
Alcoholic hepatitis is a serious disease with significant short-term mortality. Treatment options are limited but include abstinence from alcohol, supplemental nutrition, and, for select patients, pentoxifylline or corticosteroids. Because most transplant centers require six months of abstinence, these patients usually are not eligible for urgent liver transplantation.
Dr. Parada is a clinical instructor and chief medical resident in the Department of Internal Medicine at the University of New Mexico School of Medicine and the University of New Mexico Hospital, Albuquerque. Dr. Pierce is associate professor in the Division of Hospital Medicine at the University of New Mexico School of Medicine and the University of New Mexico Hospital.
References
- Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology. 1997;25:108-111.
- Pessione F, Ramond MJ, Peters L, et al. Five-year survival predictive factors in patients with excessive alcohol intake and cirrhosis. Effect of alcoholic hepatitis, smoking and abstinence. Liver Int. 2003;23:45-53.
- Mendenhall CL, Anderson S, Weesner RE, Goldberg SJ, Crolic KA. Protein-calorie malnutrition associated with alcoholic hepatitis. Veterans Administration Cooperative Study Group on alcoholic hepatitis. Am J Med. 1984;76:211-222.
- Cabre E, Rodriguez-Iglesias P, Caballeria J, et al. Short- and long-term outcome of severe alcohol-induced hepatitis treated with steroids or enteral nutrition: a multicenter randomized trial. Hepatology. 2000;32:36-42.
- O’Shea RS, Dasarathy S, McCullough AJ, Practice Guideline Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology. 2010;51:307-328.
- Rambaldi A, Saconato HH, Christensen E, Thorlund K, Wetterslev J, Gluud C. Systematic review: Glucocorticosteroids for alcoholic hepatitis—a Cochrane hepato-biliary group systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. Aliment Pharmacol Ther. 2008;27:1167-1178.
- Mathurin P, Mendenhall CL, Carithers RL Jr., et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol. 2002;36:480-487.
- Louvet A, Naveau S, Abdelnour M, et al. The Lille model: A new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology. 2007;45:1348-1354.
- Louvet A, Diaz E, Dharancy S, et al. Early switch topentoxifylline in patients with severe alcoholic hepatitis is inefficient in non-responders to corticosteroids. J Hepatol. 2008;48:465-470.
- Amini M, Runyon BA. Alcoholic hepatitis 2010: A clinician’s guide to diagnosis and therapy. World J Gastroenterol. 2010;16:4905-4912.
- Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: A double-blind, placebo-controlled trial. Gastroenterology. 2000;119:1637-1648.
- Whitfield K, Rambaldi A, Wetterslev J, Gluud C. Pentoxifylline for alcoholic hepatitis. Cochrane Database Syst Rev. 2009;(4):CD007339.
- De BK, Gangopadhyay S, Dutta D, Baksi SD, Pani A, Ghosh P. Pentoxifylline versus prednisolone for severe alcoholic hepatitis: A randomized controlled trial. World J Gastroenterol. 2009;15:1613-1619.
- Lucey MR, Brown KA, Everson GT, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997;3:628-637.