User login
Jason Carris is director, Digital Media and Strategy, Society Partners, at Frontline Medical Communications. He previously worked in the newspaper industry as a writer and editor. He resides in Central New Jersey with his wife and three children. Email him at [email protected].
Analyze This
Editors note: This article features interactive region-by-region breakdowns and Team Hospitalist analysis of the latest compensation and productivity data from SHM and MGMA. Click here to open the interactive feature.
Every January, William “Tex” Landis, MD, FHM, sits in a conference room with key members of his hospital’s administration and presents what he affectionately refers to as the “state of the union” for his hospitalist group. The bar graphs, pie charts, and commentary have changed little in the past decade, Dr. Landis admits, but the information and analysis he has available to him as he begins crafting his 2011 presentation is better than ever.
Dr. Landis, medical director of Wellspan Hospitalists in York, Pa., and hospitalist group leaders across the country will have access to the State of Hospital Medicine: 2010 Report Based on 2009 Data this budget cycle. The new report, which will be available Sept. 10, offers new compensation and productivity information, new layers of detail, and new tools to help group leaders analyze the data.
“This data reflects the best numbers we have in our business,” says Dr. Landis, the chair of SHM’s Practice Analysis Committee. “We have better participation and better quality data analysis than we have ever had before. It’s a more standardized approach, and we are just going to be able to continue to build upon this. It sets the standard for moving forward, as far as I am concerned.”
The new report, which replaces SHM’s biannual survey, is the result of a partnership between SHM and the Medical Group Management Association (MGMA), an industry leader in practice-management resources. The report compiled data about 4,211 hospitalists in 443 groups, a 30% increase in survey respondents over SHM’s 2007-2008 report.
“The collaboration is really driven at providing a single set of benchmarks to the HM community,” says David Litzau, systems analyst at MGMA. “It provides a viewpoint of what’s happening elsewhere in the industry.”
What’s happening is that hospitalists continue to see increases in compensation. The new report, which uses some different data definitions and survey methodologies, and is based on a new population, shows that median compensation for adult hospitalists is $215,000 per year, a number that doesn’t take into account benefits. Hospitalist median compensation was $183,900, according to SHM’s 2007-2008 survey, and $171,000 in SHM’s 2005-2006 survey. MGMA’s 2009 report on physician compensation showed median compensation at $210,250 per internal medicine hospitalist.
And while the compensation numbers are higher than in previous surveys, the new report also shows adult hospitalists are increasing productivity, are seeing more patients per year (reversing a somewhat declining trend), and are collecting more per encounter.
The Numbers
Although compensation is the most popular survey metric, it’s not the only number worth investigating. A handful of key productivity measures seem to be on the rise, too, according to the new report.
The national median (the midpoint of all survey respondents) for work RVUs per adult hospitalist FTE is 4,107, according to the new data. SHM’s 2007-2008 survey reported wRVUs at 3,715 per adult hospitalist.
The national median for hospitalist wRVUs per encounter is 1.86. That same figure was reported at 1.53 wRVUs per encounter in 2008 and 1.37 in 2006.
Collections per wRVU is $45.57, according to the 2010 report. The 2008 survey showed collections at $44.97 per wRVU; the 2006 survey did not report the metric.
One thing the new metrics have in common is that they show hospitalists across the nation are becoming more efficient. “The numbers essentially reaffirm the overall trends for hospital medicine, in that the productivity continues to increase and the compensation paid to a provider continues to increase,” says Troy Ahlstrom, MD, FHM, CFO of Traverse City-based Hospitalists of Northern Michigan, which has nearly 50 hospitalists supporting three hospitals. “When you dig into the numbers, hospitalists are producing more work and more RVUs per encounter than they had been in the past.”
Financial support per hospitalist FTE, another key practice-management metric, parallels the compensation growth. Practices receive a median of $98,253 of support per hospitalist FTE, according to 2010 data. The 2008 report did not provide a median figure for support; instead, it published a mean figure of $97,375 of support per FTE. The 2010 mean (average) is $111,486.
Pediatric HM also shows signs of growth; median compensation is $160,038 in the new report. The 2008 report had pediatric hospitalist median compensation at $144,600.
The new data show a spike in HM groups providing “on site” care of patients 24 hours a day, seven days a week. More than 68% have on-site care with a physician, nurse practitioner, or physician assistant. Only 53% of groups had 24/7 coverage in the 2008 report; 51% had round-the-clock coverage in the 2006 report.
Dr. Ahlstrom, a veteran member of SHM’s Practice Analysis Committee, says he expects that trend to continue, especially with the large numbers of young hospitalists in the field interested in set schedules and work-life balance. “That’s the trend,” he says. “Younger physicians are more interested in seeing that split, where the days and nights are clearly set off. Older physicians are more than happy to have a nocturnist around, just as long as it’s not going to cost them a lot of money or productivity.”
A Word of Caution, and Unintended Benefits
The new report is based on a supplemental set of questions specifically directed at hospitalist practices in MGMA’s annual Physician Compensation and Productivity Survey. The survey is voluntary and is not audited, but it is the “best data” available for hospitalists, according to practice-management experts.
“So many people assume this data is what you should do,” says John Nelson, MD, MHM, co-founder and past president of SHM and a principal in hospitalist-consulting firm Nelson Flores Hospital Medicine Consultants. “It’s not. It is a survey of what’s happening. It’s a starting point, a frame of reference. It is the best data there is, no doubt. But you should not build your practice by trying to match the medians. You might have local data that deviates. You might be starting a program or be in a competitive situation.”
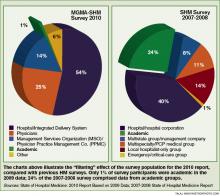
The same experts warn that the new survey population and methodologies will make it difficult to draw direct comparisons to data from previous surveys. For example, the 2007-2008 SHM survey included roughly a quarter of respondents from academic settings; the 2010 report has barely 1% of its respondents from academic settings (see Figure 1, p. 14). Traditionally, compensation and productivity levels for academic hospitalists are lower than nonacademic hospitalists. Most experts agree the “filtering” effect of the survey population factors heavily into the across- the-board increases in compensation and productivity in the 2010 report.
“The survey instrument that we use has been used historically for nonacademic physicians,” Litzau explains. “We also have an academic survey that is performed in the fall [Sept. 13 through Nov. 5], where we collect data specifically for academic faculty. We see very different trends within those two types of practice. It is difficult to draw clear comparisons between the two.”
Dr. Landis refers to the new report as a “baseline” and advises hospitalist leaders to review the caveats and cautions section (see “Survey Stipulation: Only Fools Rush In,” p. 16) before jumping right to the numbers. “This is a new set of numbers. Probably the more important comparison will be this set of numbers compared with the next set of data, next year,” he adds.
Even so, the “filtering” effect should provide nonacademic hospitalist groups a more accurate picture of compensation and productivity trends. One hospitalist leader says it’s a “win-win” for both academic and nonacademic practice leaders.
“As a community-based hospitalist, I always had to drill into those organizations that were similar to me. Being able to have more filtered information, it allows us to drill into the areas that are more important and then present that information to our CEO, CFO, VPMA,” says William D. Atchley Jr., MD, FACP, SFHM, chief of hospital medicine at Sentara Medical Group in Norfolk, Va., and a member of Team Hospitalist.
New Info, Deeper Analysis
In addition to a larger response rate and more filtered approach, the new report will offer greater frequency (annually), new data points, and in-depth breakdowns of key productivity metrics. Some of the new metrics reported include:
- Staff per FTE hospitalist physician;
- Staff turnover;
- Retirement benefits;
- Compensation to collections ratio;
- Compensation per encounter;
- Compensation per wRVU;
- Collections per encounter;
- Collections per wRVU; and
- Work RVUs per encounter.
The report will be available every fall, as compared to biannually for past SHM surveys. It also will offer more “cuts” of the data, including median, mean, 25th percentile, 75th percentile, and 90th percentile reports, along with regional breakdowns for many compensation and productivity metrics.
Practical Applications

—William “Tex” Landis, MD, FHM, medical director, Wellspan Hospitalists, York, Pa., SHM Practice Analysis Committee chair
Benchmarking data are used to set productivity goals and compensation levels in hospitalist practices throughout the country, and most administrators use multiple sources of data to make those decisions.
“If we are showing our hospitalists are generating 5,000 wRVUs per year, and the national median is 4,100, you can do the math. I can say, ‘We need to bring on another hospitalist. The timing is right, and we need to be recruiting,’ ” says Dr. Atchley, who has worked with benchmarking data for 15 years and currently supervises 45 full-time hospitalists who service five hospitals in southeast Virginia. “It’s always good to have national benchmarks to compare to, because that is always the question that is going to be asked. [Hospital administrators] want regional and national comparisons.”
Regional information and well-adapted data from national surveys guide James Gardner, MD, chief medical executive for Pro Health Care Inc., a two-hospital system just west of Milwaukee, when he’s hiring new hospitalists at 300-bed Waukesha Memorial Hospital or launching a new HM program at the system’s smaller, rural facility. In fact, Dr. Gardner currently is weighing options to expand the HM service at 80-bed Oconomowoc Hospital, less than a year after the program started.
“We like to look at a number of sources of data. The MGMA and SHM survey data, historically, have been two of our preferred sources,” Dr. Gardner says. “I think we tend to look at more regional data from the Midwest because the national data varies so much.
“We try to get a sense as to what our local market is.”
Dr. Gardner says he’d like to see a “couple years” to confirm the validity of the new SHM-MGMA report. That said, he says he knows how useful the data can be in regard to benchmarking hospitalist productivity.
“It’s been very helpful; it helps us know where we are at,” Dr. Gardner explains. “It’s one of the guideposts to decide when we are approaching the need for additional resources, whether that is midlevel providers or full-time hospitalists.”
Advice From a Numbers Guy
A self-described “numbers” guy, Dr. Ahlstrom agrees regional data is just as important as, if not more important than, the national numbers. He stresses knowing your market, your competitors, your hospital culture—and using that information along with the benchmarking data to formulate expectations for your group.
“Oftentimes you are measured against the guy next door,” Dr. Ahlstrom says. “You have to know the numbers, because [administrators] are going to know the numbers.”
Dr. Ahlstrom offers these tips for incorporating benchmarking data into your practice:
- Know your local market. “If you keep in mind your local needs, then you can look at the data and start to evaluate what parts are going to help you better formulate a practice that brings on the right people, does the right work, and continues to produce the amount of workload and compensation that makes sure they are happy in the future,” he says.
- Evaluate how applicable the data is. Pay attention to the total number of survey respondents in each category, and the standard deviation around the mean. “In other words, what is the central tendency of the data? You might find data in subsections that you find interesting, but it might not be data that has a central tendency,” he says. “Find data sets that are most applicable to your practice while assessing variations from the larger data sets. Consider how and why your practice might vary from the report as part of your evaluation.”
- Pick out trends and look at them in total. The key is to avoid looking at data points in isolation. “It’s important to look at trends in the data over time, and pick out where those trends are going to go,” he says.
- Involve your people. “I think that this data being available from the [provider] side and management side is a good thing,” Dr. Ahlstrom explains. “The more we are involved in understanding the trends in HM, the better we are going to plan where we are going in the future.” TH
Jason Carris is editor of The Hospitalist.
Editors note: This article features interactive region-by-region breakdowns and Team Hospitalist analysis of the latest compensation and productivity data from SHM and MGMA. Click here to open the interactive feature.
Every January, William “Tex” Landis, MD, FHM, sits in a conference room with key members of his hospital’s administration and presents what he affectionately refers to as the “state of the union” for his hospitalist group. The bar graphs, pie charts, and commentary have changed little in the past decade, Dr. Landis admits, but the information and analysis he has available to him as he begins crafting his 2011 presentation is better than ever.
Dr. Landis, medical director of Wellspan Hospitalists in York, Pa., and hospitalist group leaders across the country will have access to the State of Hospital Medicine: 2010 Report Based on 2009 Data this budget cycle. The new report, which will be available Sept. 10, offers new compensation and productivity information, new layers of detail, and new tools to help group leaders analyze the data.
“This data reflects the best numbers we have in our business,” says Dr. Landis, the chair of SHM’s Practice Analysis Committee. “We have better participation and better quality data analysis than we have ever had before. It’s a more standardized approach, and we are just going to be able to continue to build upon this. It sets the standard for moving forward, as far as I am concerned.”
The new report, which replaces SHM’s biannual survey, is the result of a partnership between SHM and the Medical Group Management Association (MGMA), an industry leader in practice-management resources. The report compiled data about 4,211 hospitalists in 443 groups, a 30% increase in survey respondents over SHM’s 2007-2008 report.
“The collaboration is really driven at providing a single set of benchmarks to the HM community,” says David Litzau, systems analyst at MGMA. “It provides a viewpoint of what’s happening elsewhere in the industry.”
What’s happening is that hospitalists continue to see increases in compensation. The new report, which uses some different data definitions and survey methodologies, and is based on a new population, shows that median compensation for adult hospitalists is $215,000 per year, a number that doesn’t take into account benefits. Hospitalist median compensation was $183,900, according to SHM’s 2007-2008 survey, and $171,000 in SHM’s 2005-2006 survey. MGMA’s 2009 report on physician compensation showed median compensation at $210,250 per internal medicine hospitalist.
And while the compensation numbers are higher than in previous surveys, the new report also shows adult hospitalists are increasing productivity, are seeing more patients per year (reversing a somewhat declining trend), and are collecting more per encounter.
The Numbers
Although compensation is the most popular survey metric, it’s not the only number worth investigating. A handful of key productivity measures seem to be on the rise, too, according to the new report.
The national median (the midpoint of all survey respondents) for work RVUs per adult hospitalist FTE is 4,107, according to the new data. SHM’s 2007-2008 survey reported wRVUs at 3,715 per adult hospitalist.
The national median for hospitalist wRVUs per encounter is 1.86. That same figure was reported at 1.53 wRVUs per encounter in 2008 and 1.37 in 2006.
Collections per wRVU is $45.57, according to the 2010 report. The 2008 survey showed collections at $44.97 per wRVU; the 2006 survey did not report the metric.
One thing the new metrics have in common is that they show hospitalists across the nation are becoming more efficient. “The numbers essentially reaffirm the overall trends for hospital medicine, in that the productivity continues to increase and the compensation paid to a provider continues to increase,” says Troy Ahlstrom, MD, FHM, CFO of Traverse City-based Hospitalists of Northern Michigan, which has nearly 50 hospitalists supporting three hospitals. “When you dig into the numbers, hospitalists are producing more work and more RVUs per encounter than they had been in the past.”
Financial support per hospitalist FTE, another key practice-management metric, parallels the compensation growth. Practices receive a median of $98,253 of support per hospitalist FTE, according to 2010 data. The 2008 report did not provide a median figure for support; instead, it published a mean figure of $97,375 of support per FTE. The 2010 mean (average) is $111,486.
Pediatric HM also shows signs of growth; median compensation is $160,038 in the new report. The 2008 report had pediatric hospitalist median compensation at $144,600.
The new data show a spike in HM groups providing “on site” care of patients 24 hours a day, seven days a week. More than 68% have on-site care with a physician, nurse practitioner, or physician assistant. Only 53% of groups had 24/7 coverage in the 2008 report; 51% had round-the-clock coverage in the 2006 report.
Dr. Ahlstrom, a veteran member of SHM’s Practice Analysis Committee, says he expects that trend to continue, especially with the large numbers of young hospitalists in the field interested in set schedules and work-life balance. “That’s the trend,” he says. “Younger physicians are more interested in seeing that split, where the days and nights are clearly set off. Older physicians are more than happy to have a nocturnist around, just as long as it’s not going to cost them a lot of money or productivity.”
A Word of Caution, and Unintended Benefits
The new report is based on a supplemental set of questions specifically directed at hospitalist practices in MGMA’s annual Physician Compensation and Productivity Survey. The survey is voluntary and is not audited, but it is the “best data” available for hospitalists, according to practice-management experts.
“So many people assume this data is what you should do,” says John Nelson, MD, MHM, co-founder and past president of SHM and a principal in hospitalist-consulting firm Nelson Flores Hospital Medicine Consultants. “It’s not. It is a survey of what’s happening. It’s a starting point, a frame of reference. It is the best data there is, no doubt. But you should not build your practice by trying to match the medians. You might have local data that deviates. You might be starting a program or be in a competitive situation.”
The same experts warn that the new survey population and methodologies will make it difficult to draw direct comparisons to data from previous surveys. For example, the 2007-2008 SHM survey included roughly a quarter of respondents from academic settings; the 2010 report has barely 1% of its respondents from academic settings (see Figure 1, p. 14). Traditionally, compensation and productivity levels for academic hospitalists are lower than nonacademic hospitalists. Most experts agree the “filtering” effect of the survey population factors heavily into the across- the-board increases in compensation and productivity in the 2010 report.
“The survey instrument that we use has been used historically for nonacademic physicians,” Litzau explains. “We also have an academic survey that is performed in the fall [Sept. 13 through Nov. 5], where we collect data specifically for academic faculty. We see very different trends within those two types of practice. It is difficult to draw clear comparisons between the two.”
Dr. Landis refers to the new report as a “baseline” and advises hospitalist leaders to review the caveats and cautions section (see “Survey Stipulation: Only Fools Rush In,” p. 16) before jumping right to the numbers. “This is a new set of numbers. Probably the more important comparison will be this set of numbers compared with the next set of data, next year,” he adds.
Even so, the “filtering” effect should provide nonacademic hospitalist groups a more accurate picture of compensation and productivity trends. One hospitalist leader says it’s a “win-win” for both academic and nonacademic practice leaders.
“As a community-based hospitalist, I always had to drill into those organizations that were similar to me. Being able to have more filtered information, it allows us to drill into the areas that are more important and then present that information to our CEO, CFO, VPMA,” says William D. Atchley Jr., MD, FACP, SFHM, chief of hospital medicine at Sentara Medical Group in Norfolk, Va., and a member of Team Hospitalist.
New Info, Deeper Analysis
In addition to a larger response rate and more filtered approach, the new report will offer greater frequency (annually), new data points, and in-depth breakdowns of key productivity metrics. Some of the new metrics reported include:
- Staff per FTE hospitalist physician;
- Staff turnover;
- Retirement benefits;
- Compensation to collections ratio;
- Compensation per encounter;
- Compensation per wRVU;
- Collections per encounter;
- Collections per wRVU; and
- Work RVUs per encounter.
The report will be available every fall, as compared to biannually for past SHM surveys. It also will offer more “cuts” of the data, including median, mean, 25th percentile, 75th percentile, and 90th percentile reports, along with regional breakdowns for many compensation and productivity metrics.
Practical Applications

—William “Tex” Landis, MD, FHM, medical director, Wellspan Hospitalists, York, Pa., SHM Practice Analysis Committee chair
Benchmarking data are used to set productivity goals and compensation levels in hospitalist practices throughout the country, and most administrators use multiple sources of data to make those decisions.
“If we are showing our hospitalists are generating 5,000 wRVUs per year, and the national median is 4,100, you can do the math. I can say, ‘We need to bring on another hospitalist. The timing is right, and we need to be recruiting,’ ” says Dr. Atchley, who has worked with benchmarking data for 15 years and currently supervises 45 full-time hospitalists who service five hospitals in southeast Virginia. “It’s always good to have national benchmarks to compare to, because that is always the question that is going to be asked. [Hospital administrators] want regional and national comparisons.”
Regional information and well-adapted data from national surveys guide James Gardner, MD, chief medical executive for Pro Health Care Inc., a two-hospital system just west of Milwaukee, when he’s hiring new hospitalists at 300-bed Waukesha Memorial Hospital or launching a new HM program at the system’s smaller, rural facility. In fact, Dr. Gardner currently is weighing options to expand the HM service at 80-bed Oconomowoc Hospital, less than a year after the program started.
“We like to look at a number of sources of data. The MGMA and SHM survey data, historically, have been two of our preferred sources,” Dr. Gardner says. “I think we tend to look at more regional data from the Midwest because the national data varies so much.
“We try to get a sense as to what our local market is.”
Dr. Gardner says he’d like to see a “couple years” to confirm the validity of the new SHM-MGMA report. That said, he says he knows how useful the data can be in regard to benchmarking hospitalist productivity.
“It’s been very helpful; it helps us know where we are at,” Dr. Gardner explains. “It’s one of the guideposts to decide when we are approaching the need for additional resources, whether that is midlevel providers or full-time hospitalists.”
Advice From a Numbers Guy
A self-described “numbers” guy, Dr. Ahlstrom agrees regional data is just as important as, if not more important than, the national numbers. He stresses knowing your market, your competitors, your hospital culture—and using that information along with the benchmarking data to formulate expectations for your group.
“Oftentimes you are measured against the guy next door,” Dr. Ahlstrom says. “You have to know the numbers, because [administrators] are going to know the numbers.”
Dr. Ahlstrom offers these tips for incorporating benchmarking data into your practice:
- Know your local market. “If you keep in mind your local needs, then you can look at the data and start to evaluate what parts are going to help you better formulate a practice that brings on the right people, does the right work, and continues to produce the amount of workload and compensation that makes sure they are happy in the future,” he says.
- Evaluate how applicable the data is. Pay attention to the total number of survey respondents in each category, and the standard deviation around the mean. “In other words, what is the central tendency of the data? You might find data in subsections that you find interesting, but it might not be data that has a central tendency,” he says. “Find data sets that are most applicable to your practice while assessing variations from the larger data sets. Consider how and why your practice might vary from the report as part of your evaluation.”
- Pick out trends and look at them in total. The key is to avoid looking at data points in isolation. “It’s important to look at trends in the data over time, and pick out where those trends are going to go,” he says.
- Involve your people. “I think that this data being available from the [provider] side and management side is a good thing,” Dr. Ahlstrom explains. “The more we are involved in understanding the trends in HM, the better we are going to plan where we are going in the future.” TH
Jason Carris is editor of The Hospitalist.
Editors note: This article features interactive region-by-region breakdowns and Team Hospitalist analysis of the latest compensation and productivity data from SHM and MGMA. Click here to open the interactive feature.
Every January, William “Tex” Landis, MD, FHM, sits in a conference room with key members of his hospital’s administration and presents what he affectionately refers to as the “state of the union” for his hospitalist group. The bar graphs, pie charts, and commentary have changed little in the past decade, Dr. Landis admits, but the information and analysis he has available to him as he begins crafting his 2011 presentation is better than ever.
Dr. Landis, medical director of Wellspan Hospitalists in York, Pa., and hospitalist group leaders across the country will have access to the State of Hospital Medicine: 2010 Report Based on 2009 Data this budget cycle. The new report, which will be available Sept. 10, offers new compensation and productivity information, new layers of detail, and new tools to help group leaders analyze the data.
“This data reflects the best numbers we have in our business,” says Dr. Landis, the chair of SHM’s Practice Analysis Committee. “We have better participation and better quality data analysis than we have ever had before. It’s a more standardized approach, and we are just going to be able to continue to build upon this. It sets the standard for moving forward, as far as I am concerned.”
The new report, which replaces SHM’s biannual survey, is the result of a partnership between SHM and the Medical Group Management Association (MGMA), an industry leader in practice-management resources. The report compiled data about 4,211 hospitalists in 443 groups, a 30% increase in survey respondents over SHM’s 2007-2008 report.
“The collaboration is really driven at providing a single set of benchmarks to the HM community,” says David Litzau, systems analyst at MGMA. “It provides a viewpoint of what’s happening elsewhere in the industry.”
What’s happening is that hospitalists continue to see increases in compensation. The new report, which uses some different data definitions and survey methodologies, and is based on a new population, shows that median compensation for adult hospitalists is $215,000 per year, a number that doesn’t take into account benefits. Hospitalist median compensation was $183,900, according to SHM’s 2007-2008 survey, and $171,000 in SHM’s 2005-2006 survey. MGMA’s 2009 report on physician compensation showed median compensation at $210,250 per internal medicine hospitalist.
And while the compensation numbers are higher than in previous surveys, the new report also shows adult hospitalists are increasing productivity, are seeing more patients per year (reversing a somewhat declining trend), and are collecting more per encounter.
The Numbers
Although compensation is the most popular survey metric, it’s not the only number worth investigating. A handful of key productivity measures seem to be on the rise, too, according to the new report.
The national median (the midpoint of all survey respondents) for work RVUs per adult hospitalist FTE is 4,107, according to the new data. SHM’s 2007-2008 survey reported wRVUs at 3,715 per adult hospitalist.
The national median for hospitalist wRVUs per encounter is 1.86. That same figure was reported at 1.53 wRVUs per encounter in 2008 and 1.37 in 2006.
Collections per wRVU is $45.57, according to the 2010 report. The 2008 survey showed collections at $44.97 per wRVU; the 2006 survey did not report the metric.
One thing the new metrics have in common is that they show hospitalists across the nation are becoming more efficient. “The numbers essentially reaffirm the overall trends for hospital medicine, in that the productivity continues to increase and the compensation paid to a provider continues to increase,” says Troy Ahlstrom, MD, FHM, CFO of Traverse City-based Hospitalists of Northern Michigan, which has nearly 50 hospitalists supporting three hospitals. “When you dig into the numbers, hospitalists are producing more work and more RVUs per encounter than they had been in the past.”
Financial support per hospitalist FTE, another key practice-management metric, parallels the compensation growth. Practices receive a median of $98,253 of support per hospitalist FTE, according to 2010 data. The 2008 report did not provide a median figure for support; instead, it published a mean figure of $97,375 of support per FTE. The 2010 mean (average) is $111,486.
Pediatric HM also shows signs of growth; median compensation is $160,038 in the new report. The 2008 report had pediatric hospitalist median compensation at $144,600.
The new data show a spike in HM groups providing “on site” care of patients 24 hours a day, seven days a week. More than 68% have on-site care with a physician, nurse practitioner, or physician assistant. Only 53% of groups had 24/7 coverage in the 2008 report; 51% had round-the-clock coverage in the 2006 report.
Dr. Ahlstrom, a veteran member of SHM’s Practice Analysis Committee, says he expects that trend to continue, especially with the large numbers of young hospitalists in the field interested in set schedules and work-life balance. “That’s the trend,” he says. “Younger physicians are more interested in seeing that split, where the days and nights are clearly set off. Older physicians are more than happy to have a nocturnist around, just as long as it’s not going to cost them a lot of money or productivity.”
A Word of Caution, and Unintended Benefits
The new report is based on a supplemental set of questions specifically directed at hospitalist practices in MGMA’s annual Physician Compensation and Productivity Survey. The survey is voluntary and is not audited, but it is the “best data” available for hospitalists, according to practice-management experts.
“So many people assume this data is what you should do,” says John Nelson, MD, MHM, co-founder and past president of SHM and a principal in hospitalist-consulting firm Nelson Flores Hospital Medicine Consultants. “It’s not. It is a survey of what’s happening. It’s a starting point, a frame of reference. It is the best data there is, no doubt. But you should not build your practice by trying to match the medians. You might have local data that deviates. You might be starting a program or be in a competitive situation.”
The same experts warn that the new survey population and methodologies will make it difficult to draw direct comparisons to data from previous surveys. For example, the 2007-2008 SHM survey included roughly a quarter of respondents from academic settings; the 2010 report has barely 1% of its respondents from academic settings (see Figure 1, p. 14). Traditionally, compensation and productivity levels for academic hospitalists are lower than nonacademic hospitalists. Most experts agree the “filtering” effect of the survey population factors heavily into the across- the-board increases in compensation and productivity in the 2010 report.
“The survey instrument that we use has been used historically for nonacademic physicians,” Litzau explains. “We also have an academic survey that is performed in the fall [Sept. 13 through Nov. 5], where we collect data specifically for academic faculty. We see very different trends within those two types of practice. It is difficult to draw clear comparisons between the two.”
Dr. Landis refers to the new report as a “baseline” and advises hospitalist leaders to review the caveats and cautions section (see “Survey Stipulation: Only Fools Rush In,” p. 16) before jumping right to the numbers. “This is a new set of numbers. Probably the more important comparison will be this set of numbers compared with the next set of data, next year,” he adds.
Even so, the “filtering” effect should provide nonacademic hospitalist groups a more accurate picture of compensation and productivity trends. One hospitalist leader says it’s a “win-win” for both academic and nonacademic practice leaders.
“As a community-based hospitalist, I always had to drill into those organizations that were similar to me. Being able to have more filtered information, it allows us to drill into the areas that are more important and then present that information to our CEO, CFO, VPMA,” says William D. Atchley Jr., MD, FACP, SFHM, chief of hospital medicine at Sentara Medical Group in Norfolk, Va., and a member of Team Hospitalist.
New Info, Deeper Analysis
In addition to a larger response rate and more filtered approach, the new report will offer greater frequency (annually), new data points, and in-depth breakdowns of key productivity metrics. Some of the new metrics reported include:
- Staff per FTE hospitalist physician;
- Staff turnover;
- Retirement benefits;
- Compensation to collections ratio;
- Compensation per encounter;
- Compensation per wRVU;
- Collections per encounter;
- Collections per wRVU; and
- Work RVUs per encounter.
The report will be available every fall, as compared to biannually for past SHM surveys. It also will offer more “cuts” of the data, including median, mean, 25th percentile, 75th percentile, and 90th percentile reports, along with regional breakdowns for many compensation and productivity metrics.
Practical Applications

—William “Tex” Landis, MD, FHM, medical director, Wellspan Hospitalists, York, Pa., SHM Practice Analysis Committee chair
Benchmarking data are used to set productivity goals and compensation levels in hospitalist practices throughout the country, and most administrators use multiple sources of data to make those decisions.
“If we are showing our hospitalists are generating 5,000 wRVUs per year, and the national median is 4,100, you can do the math. I can say, ‘We need to bring on another hospitalist. The timing is right, and we need to be recruiting,’ ” says Dr. Atchley, who has worked with benchmarking data for 15 years and currently supervises 45 full-time hospitalists who service five hospitals in southeast Virginia. “It’s always good to have national benchmarks to compare to, because that is always the question that is going to be asked. [Hospital administrators] want regional and national comparisons.”
Regional information and well-adapted data from national surveys guide James Gardner, MD, chief medical executive for Pro Health Care Inc., a two-hospital system just west of Milwaukee, when he’s hiring new hospitalists at 300-bed Waukesha Memorial Hospital or launching a new HM program at the system’s smaller, rural facility. In fact, Dr. Gardner currently is weighing options to expand the HM service at 80-bed Oconomowoc Hospital, less than a year after the program started.
“We like to look at a number of sources of data. The MGMA and SHM survey data, historically, have been two of our preferred sources,” Dr. Gardner says. “I think we tend to look at more regional data from the Midwest because the national data varies so much.
“We try to get a sense as to what our local market is.”
Dr. Gardner says he’d like to see a “couple years” to confirm the validity of the new SHM-MGMA report. That said, he says he knows how useful the data can be in regard to benchmarking hospitalist productivity.
“It’s been very helpful; it helps us know where we are at,” Dr. Gardner explains. “It’s one of the guideposts to decide when we are approaching the need for additional resources, whether that is midlevel providers or full-time hospitalists.”
Advice From a Numbers Guy
A self-described “numbers” guy, Dr. Ahlstrom agrees regional data is just as important as, if not more important than, the national numbers. He stresses knowing your market, your competitors, your hospital culture—and using that information along with the benchmarking data to formulate expectations for your group.
“Oftentimes you are measured against the guy next door,” Dr. Ahlstrom says. “You have to know the numbers, because [administrators] are going to know the numbers.”
Dr. Ahlstrom offers these tips for incorporating benchmarking data into your practice:
- Know your local market. “If you keep in mind your local needs, then you can look at the data and start to evaluate what parts are going to help you better formulate a practice that brings on the right people, does the right work, and continues to produce the amount of workload and compensation that makes sure they are happy in the future,” he says.
- Evaluate how applicable the data is. Pay attention to the total number of survey respondents in each category, and the standard deviation around the mean. “In other words, what is the central tendency of the data? You might find data in subsections that you find interesting, but it might not be data that has a central tendency,” he says. “Find data sets that are most applicable to your practice while assessing variations from the larger data sets. Consider how and why your practice might vary from the report as part of your evaluation.”
- Pick out trends and look at them in total. The key is to avoid looking at data points in isolation. “It’s important to look at trends in the data over time, and pick out where those trends are going to go,” he says.
- Involve your people. “I think that this data being available from the [provider] side and management side is a good thing,” Dr. Ahlstrom explains. “The more we are involved in understanding the trends in HM, the better we are going to plan where we are going in the future.” TH
Jason Carris is editor of The Hospitalist.
ONLINE EXCLUSIVE: Audio interview with Troy Ahlstrom, MD, FHM, CFO of Hospitalists of Northern Michigan
SHM Practice Analysis Committee member Troy Ahlstrom, MD, FHM, discusses the new compensation and productivity report, and gives advice on how best to use benchmarking data in your practice.
SHM Practice Analysis Committee member Troy Ahlstrom, MD, FHM, discusses the new compensation and productivity report, and gives advice on how best to use benchmarking data in your practice.
SHM Practice Analysis Committee member Troy Ahlstrom, MD, FHM, discusses the new compensation and productivity report, and gives advice on how best to use benchmarking data in your practice.
Mentorship Matters
As you begin the next phase in your career, whether starting residency, a fellowship, or a new faculty position, it’s likely you have dozens of questions. How do I survive the rigors of residency? What do I need to make the most of my fellowship? What do I need to do to become more efficient in my clinical productivity? How do I succeed in academics? There are many more questions we could add to this list.
While some lessons in life are learned through trial and error, it rarely is the best way. This is especially true when considering your professional future. An essential first step at any phase in your career is finding yourself a mentor. There are many benefits to having someone help you navigate through many of the challenges you will face. A mentor’s experience is invaluable in avoiding potential pitfalls that set many physicians back in their careers, and in giving you the best opportunity to succeed as you begin your desired path.
This might seem like a new idea, but the concept of mentoring has been around for centuries. All of us have been mentored at some point in our lives; you probably just haven’t realized it. It could have been a parent, coach, guidance counselor, or teacher. Mentorship is a mutually beneficial relationship that applies to many areas of life, including your career development in medicine.
Finding a mentor is easier said than done. Many physicians are not sure where to begin. How do you choose? Where do you start? These are common questions, among many others. Some institutions assign mentors for this very reason. However, this is not always an ideal solution, as the mentor/mentee relationship might not be a perfect match.
Here are some ideas to help get you started in your mentor search:
1) Know Thyself: As you begin your search, start by reflecting on yourself. What do you need? What are your current skills? What are your career aspirations? This initial step of introspection is essential in becoming more aware of your own mentoring needs. The more specific you can be in defining your needs and goals, the better equipped you will be to seek out someone who can help guide you on the path to achieve them.
2) Know What to Look for: Having established what you are looking for as a mentee, it is important to consider what makes for a good mentor. A good mentor is experienced, successful, and has the proper skill sets, but also should have the following basic qualities:
- A willingness to mentor. They should want to invest in you and be interested in your career success;
- A commitment to the mentoring relationship. They will spend the time, energy, and resources necessary to help you achieve your goals;
- Availability. They must not be too busy with other responsibilities or other mentees;
- Good communications skills. They need to be a sounding board, and provide honest and constructive advice that is specific to your needs; and
- Professionalism. You should trust them to maintain confidentiality.
3) Start the Search: Now that you understand your needs and the desired qualities in a mentor, start thinking about potential options. You might already have someone in mind based on his or her success or reputation as a mentor. However, by asking around, you might also find other, lesser-known mentors that might be an even better fit for you in the long run.
Don’t limit yourself to your current institution. You might find that the mentors you are looking for are at other institutions. These opportunities are usually found through networking, either through local channels or through regional/national meetings. Although these kinds of mentorship relationships are more difficult to initiate and maintain, the opportunity to collaborate among members at various institutions can end up being more fruitful in the long term.
4) Meet and Greet: After assembling a short list of potential mentors, schedule a meeting with each of them. This may be cumbersome at first, but it is essential in finding out if this is someone you can see working with and learning from over the next few months or years. Finding this natural “fit” is what helps make for a lasting relationship.
At the same time, think of the meetings as interviews for a “position,” which is important to your future. This is the time for communicating your intentions, for making mutual expectations clear, and refining them further. Keep your professional goals in mind, as this will help in narrowing down your list.
5) One Size Does Not Fit All: As you consider potential mentors, keep in mind that it is OK to branch out. You might have many areas (research, education, quality improvement, work-life balance, leadership, clinical productivity, etc.) of interest that need mentoring. One mentor is unlikely to be able to meet all of your needs. This is where developing a core group of mentors could be helpful, each providing their unique insight.
Once you find a good mentor, remember to value their time and respect their expectations for you as a mentee. You are to be as committed to the partnership as you expect them to be. As you develop this mentorship, you will realize that it can become more than a professional relationship—it also can become a lasting alliance that strengthens with time. TH
Dr. LaBrin is an academic hospitalist at Vanderbilt University School of Medicine in Nashville, Tenn.
As you begin the next phase in your career, whether starting residency, a fellowship, or a new faculty position, it’s likely you have dozens of questions. How do I survive the rigors of residency? What do I need to make the most of my fellowship? What do I need to do to become more efficient in my clinical productivity? How do I succeed in academics? There are many more questions we could add to this list.
While some lessons in life are learned through trial and error, it rarely is the best way. This is especially true when considering your professional future. An essential first step at any phase in your career is finding yourself a mentor. There are many benefits to having someone help you navigate through many of the challenges you will face. A mentor’s experience is invaluable in avoiding potential pitfalls that set many physicians back in their careers, and in giving you the best opportunity to succeed as you begin your desired path.
This might seem like a new idea, but the concept of mentoring has been around for centuries. All of us have been mentored at some point in our lives; you probably just haven’t realized it. It could have been a parent, coach, guidance counselor, or teacher. Mentorship is a mutually beneficial relationship that applies to many areas of life, including your career development in medicine.
Finding a mentor is easier said than done. Many physicians are not sure where to begin. How do you choose? Where do you start? These are common questions, among many others. Some institutions assign mentors for this very reason. However, this is not always an ideal solution, as the mentor/mentee relationship might not be a perfect match.
Here are some ideas to help get you started in your mentor search:
1) Know Thyself: As you begin your search, start by reflecting on yourself. What do you need? What are your current skills? What are your career aspirations? This initial step of introspection is essential in becoming more aware of your own mentoring needs. The more specific you can be in defining your needs and goals, the better equipped you will be to seek out someone who can help guide you on the path to achieve them.
2) Know What to Look for: Having established what you are looking for as a mentee, it is important to consider what makes for a good mentor. A good mentor is experienced, successful, and has the proper skill sets, but also should have the following basic qualities:
- A willingness to mentor. They should want to invest in you and be interested in your career success;
- A commitment to the mentoring relationship. They will spend the time, energy, and resources necessary to help you achieve your goals;
- Availability. They must not be too busy with other responsibilities or other mentees;
- Good communications skills. They need to be a sounding board, and provide honest and constructive advice that is specific to your needs; and
- Professionalism. You should trust them to maintain confidentiality.
3) Start the Search: Now that you understand your needs and the desired qualities in a mentor, start thinking about potential options. You might already have someone in mind based on his or her success or reputation as a mentor. However, by asking around, you might also find other, lesser-known mentors that might be an even better fit for you in the long run.
Don’t limit yourself to your current institution. You might find that the mentors you are looking for are at other institutions. These opportunities are usually found through networking, either through local channels or through regional/national meetings. Although these kinds of mentorship relationships are more difficult to initiate and maintain, the opportunity to collaborate among members at various institutions can end up being more fruitful in the long term.
4) Meet and Greet: After assembling a short list of potential mentors, schedule a meeting with each of them. This may be cumbersome at first, but it is essential in finding out if this is someone you can see working with and learning from over the next few months or years. Finding this natural “fit” is what helps make for a lasting relationship.
At the same time, think of the meetings as interviews for a “position,” which is important to your future. This is the time for communicating your intentions, for making mutual expectations clear, and refining them further. Keep your professional goals in mind, as this will help in narrowing down your list.
5) One Size Does Not Fit All: As you consider potential mentors, keep in mind that it is OK to branch out. You might have many areas (research, education, quality improvement, work-life balance, leadership, clinical productivity, etc.) of interest that need mentoring. One mentor is unlikely to be able to meet all of your needs. This is where developing a core group of mentors could be helpful, each providing their unique insight.
Once you find a good mentor, remember to value their time and respect their expectations for you as a mentee. You are to be as committed to the partnership as you expect them to be. As you develop this mentorship, you will realize that it can become more than a professional relationship—it also can become a lasting alliance that strengthens with time. TH
Dr. LaBrin is an academic hospitalist at Vanderbilt University School of Medicine in Nashville, Tenn.
As you begin the next phase in your career, whether starting residency, a fellowship, or a new faculty position, it’s likely you have dozens of questions. How do I survive the rigors of residency? What do I need to make the most of my fellowship? What do I need to do to become more efficient in my clinical productivity? How do I succeed in academics? There are many more questions we could add to this list.
While some lessons in life are learned through trial and error, it rarely is the best way. This is especially true when considering your professional future. An essential first step at any phase in your career is finding yourself a mentor. There are many benefits to having someone help you navigate through many of the challenges you will face. A mentor’s experience is invaluable in avoiding potential pitfalls that set many physicians back in their careers, and in giving you the best opportunity to succeed as you begin your desired path.
This might seem like a new idea, but the concept of mentoring has been around for centuries. All of us have been mentored at some point in our lives; you probably just haven’t realized it. It could have been a parent, coach, guidance counselor, or teacher. Mentorship is a mutually beneficial relationship that applies to many areas of life, including your career development in medicine.
Finding a mentor is easier said than done. Many physicians are not sure where to begin. How do you choose? Where do you start? These are common questions, among many others. Some institutions assign mentors for this very reason. However, this is not always an ideal solution, as the mentor/mentee relationship might not be a perfect match.
Here are some ideas to help get you started in your mentor search:
1) Know Thyself: As you begin your search, start by reflecting on yourself. What do you need? What are your current skills? What are your career aspirations? This initial step of introspection is essential in becoming more aware of your own mentoring needs. The more specific you can be in defining your needs and goals, the better equipped you will be to seek out someone who can help guide you on the path to achieve them.
2) Know What to Look for: Having established what you are looking for as a mentee, it is important to consider what makes for a good mentor. A good mentor is experienced, successful, and has the proper skill sets, but also should have the following basic qualities:
- A willingness to mentor. They should want to invest in you and be interested in your career success;
- A commitment to the mentoring relationship. They will spend the time, energy, and resources necessary to help you achieve your goals;
- Availability. They must not be too busy with other responsibilities or other mentees;
- Good communications skills. They need to be a sounding board, and provide honest and constructive advice that is specific to your needs; and
- Professionalism. You should trust them to maintain confidentiality.
3) Start the Search: Now that you understand your needs and the desired qualities in a mentor, start thinking about potential options. You might already have someone in mind based on his or her success or reputation as a mentor. However, by asking around, you might also find other, lesser-known mentors that might be an even better fit for you in the long run.
Don’t limit yourself to your current institution. You might find that the mentors you are looking for are at other institutions. These opportunities are usually found through networking, either through local channels or through regional/national meetings. Although these kinds of mentorship relationships are more difficult to initiate and maintain, the opportunity to collaborate among members at various institutions can end up being more fruitful in the long term.
4) Meet and Greet: After assembling a short list of potential mentors, schedule a meeting with each of them. This may be cumbersome at first, but it is essential in finding out if this is someone you can see working with and learning from over the next few months or years. Finding this natural “fit” is what helps make for a lasting relationship.
At the same time, think of the meetings as interviews for a “position,” which is important to your future. This is the time for communicating your intentions, for making mutual expectations clear, and refining them further. Keep your professional goals in mind, as this will help in narrowing down your list.
5) One Size Does Not Fit All: As you consider potential mentors, keep in mind that it is OK to branch out. You might have many areas (research, education, quality improvement, work-life balance, leadership, clinical productivity, etc.) of interest that need mentoring. One mentor is unlikely to be able to meet all of your needs. This is where developing a core group of mentors could be helpful, each providing their unique insight.
Once you find a good mentor, remember to value their time and respect their expectations for you as a mentee. You are to be as committed to the partnership as you expect them to be. As you develop this mentorship, you will realize that it can become more than a professional relationship—it also can become a lasting alliance that strengthens with time. TH
Dr. LaBrin is an academic hospitalist at Vanderbilt University School of Medicine in Nashville, Tenn.
MGMA Releases Compensation and Productivity Data
New hospitalist compensation and productivity information is available via the 2010 Physician Compensation and Production Survey Report, the Medical Group Management Association’s (MGMA) annual survey. However, HM leaders are urging restraint to group directors and individual hospitalists pining for the latest industry benchmarks.
“We want to be careful not to read too much into trends at this point. This is a new set of data,” says William “Tex” Landis, MD, FHM, medical director of Wellspan Hospitalists in York, Pa., and chair of SHM’s Practice Analysis Committee. “I think the trending might be beneficial, but I think it should be done with great caution.”
The report, which surveyed 4,211 hospitalists from 443 groups, shows median hospitalist compensation at $215,000 annually. That’s an increase of about $20,000 per year compared with SHM’s 2007-2008 survey data.
The report also shows the median number of work RVUs at 4,107 per hospitalist per year.
SHM, which collaborated on the survey with MGMA, will release a more detailed compensation and productivity report in September. That report replaces SHM’s biannual survey, and will break down such hospitalist-specific data as night coverage, financial support, and staffing models.
The MGMA survey adds new layers of detail, as compared with past SHM surveys. In addition to mean and median values, the MGMA report breaks down production and compensation values to 25th-, 75th-, and 90th-percentile ranges. “It provides a lot more ways to cut the data than [SHM] has traditionally done,” says Leslie Flores, SHM senior advisor of practice management.
Although he warns of taking the MGMA survey information too literally, Dr. Landis knows his peers are anxiously awaiting the new numbers. “It provides the best possible data to help with optimal decision-making, especially as it pertains to resourcing hospitalist programs,” he says. “What will be more important, however, will be what next year’s numbers show; then, we will be comparing like with like.”
New hospitalist compensation and productivity information is available via the 2010 Physician Compensation and Production Survey Report, the Medical Group Management Association’s (MGMA) annual survey. However, HM leaders are urging restraint to group directors and individual hospitalists pining for the latest industry benchmarks.
“We want to be careful not to read too much into trends at this point. This is a new set of data,” says William “Tex” Landis, MD, FHM, medical director of Wellspan Hospitalists in York, Pa., and chair of SHM’s Practice Analysis Committee. “I think the trending might be beneficial, but I think it should be done with great caution.”
The report, which surveyed 4,211 hospitalists from 443 groups, shows median hospitalist compensation at $215,000 annually. That’s an increase of about $20,000 per year compared with SHM’s 2007-2008 survey data.
The report also shows the median number of work RVUs at 4,107 per hospitalist per year.
SHM, which collaborated on the survey with MGMA, will release a more detailed compensation and productivity report in September. That report replaces SHM’s biannual survey, and will break down such hospitalist-specific data as night coverage, financial support, and staffing models.
The MGMA survey adds new layers of detail, as compared with past SHM surveys. In addition to mean and median values, the MGMA report breaks down production and compensation values to 25th-, 75th-, and 90th-percentile ranges. “It provides a lot more ways to cut the data than [SHM] has traditionally done,” says Leslie Flores, SHM senior advisor of practice management.
Although he warns of taking the MGMA survey information too literally, Dr. Landis knows his peers are anxiously awaiting the new numbers. “It provides the best possible data to help with optimal decision-making, especially as it pertains to resourcing hospitalist programs,” he says. “What will be more important, however, will be what next year’s numbers show; then, we will be comparing like with like.”
New hospitalist compensation and productivity information is available via the 2010 Physician Compensation and Production Survey Report, the Medical Group Management Association’s (MGMA) annual survey. However, HM leaders are urging restraint to group directors and individual hospitalists pining for the latest industry benchmarks.
“We want to be careful not to read too much into trends at this point. This is a new set of data,” says William “Tex” Landis, MD, FHM, medical director of Wellspan Hospitalists in York, Pa., and chair of SHM’s Practice Analysis Committee. “I think the trending might be beneficial, but I think it should be done with great caution.”
The report, which surveyed 4,211 hospitalists from 443 groups, shows median hospitalist compensation at $215,000 annually. That’s an increase of about $20,000 per year compared with SHM’s 2007-2008 survey data.
The report also shows the median number of work RVUs at 4,107 per hospitalist per year.
SHM, which collaborated on the survey with MGMA, will release a more detailed compensation and productivity report in September. That report replaces SHM’s biannual survey, and will break down such hospitalist-specific data as night coverage, financial support, and staffing models.
The MGMA survey adds new layers of detail, as compared with past SHM surveys. In addition to mean and median values, the MGMA report breaks down production and compensation values to 25th-, 75th-, and 90th-percentile ranges. “It provides a lot more ways to cut the data than [SHM] has traditionally done,” says Leslie Flores, SHM senior advisor of practice management.
Although he warns of taking the MGMA survey information too literally, Dr. Landis knows his peers are anxiously awaiting the new numbers. “It provides the best possible data to help with optimal decision-making, especially as it pertains to resourcing hospitalist programs,” he says. “What will be more important, however, will be what next year’s numbers show; then, we will be comparing like with like.”
ONLINE EXCLUSIVE: Quick Response
Jitendra Dassani, MD, is a hospitalist who works for Advocate Medical Group at Illinois Masonic Hospital in Chicago. He passed the American Board of Internal Medicine’s (ABIM) traditional internal-medicine Maintenance of Certification (MOC) examination in 2008. According to current guidelines, he won’t have to recertify until 2018.
But Dr. Dassani is more than a veteran hospitalist. He’s practiced hospital-based medicine for well over a decade, and is planning on a long and prosperous HM career. In fact, he’s so dedicated to the field that he is planning to recertify through ABIM’s new Focused Practice in Hospital Medicine (FPHM) MOC next year—or, at the very latest, in 2012.
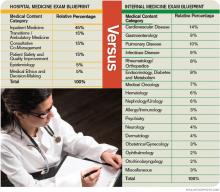
“I’ve been a hospitalist for 13 years, and I think it’s important to have something that can assess your knowledge and abilities as a hospitalist,” says Dr. Dassani, one of nearly 200 hospitalists who have signed up for the FPHM pathway. The first secure exam will be administered in October. “I took the general IM exam in 2008. That’s the traditional ABIM boards; I felt some of the questions were not related to my practice. That’s why I think the [FPHM] is really good and really important.”
He’s not alone. SHM and ABIM are anxious to see where this new MOC pathway goes. SHM leaders think the FPHM offers career validation and a customized MOC process to the 30,000 hospitalists practicing nationwide. ABIM is planning an extensive research effort to analyze a focused-practice MOC, using hospitalists as the test subjects.
One area in which the FPHM varies from the traditional MOC is its every-three-year requirement to complete practice-improvement modules (PIMs). Dr. Dassani likens the higher standard to the kind of continuing education and training programs other specialized fields require.
“I think it’s a good idea. It’s more work, but I support it,” he says. “Every time you get onto a plane, you hope the pilot is certified every six months, versus no one has evaluated the pilot in two years. Your safety is in his hands. Take that same analogy to medicine.
“You will have time,” he adds. “It’s 60 points over three years. One PIM is 40 points, so it’s not overwhelming.”—JC
Jitendra Dassani, MD, is a hospitalist who works for Advocate Medical Group at Illinois Masonic Hospital in Chicago. He passed the American Board of Internal Medicine’s (ABIM) traditional internal-medicine Maintenance of Certification (MOC) examination in 2008. According to current guidelines, he won’t have to recertify until 2018.
But Dr. Dassani is more than a veteran hospitalist. He’s practiced hospital-based medicine for well over a decade, and is planning on a long and prosperous HM career. In fact, he’s so dedicated to the field that he is planning to recertify through ABIM’s new Focused Practice in Hospital Medicine (FPHM) MOC next year—or, at the very latest, in 2012.
“I’ve been a hospitalist for 13 years, and I think it’s important to have something that can assess your knowledge and abilities as a hospitalist,” says Dr. Dassani, one of nearly 200 hospitalists who have signed up for the FPHM pathway. The first secure exam will be administered in October. “I took the general IM exam in 2008. That’s the traditional ABIM boards; I felt some of the questions were not related to my practice. That’s why I think the [FPHM] is really good and really important.”
He’s not alone. SHM and ABIM are anxious to see where this new MOC pathway goes. SHM leaders think the FPHM offers career validation and a customized MOC process to the 30,000 hospitalists practicing nationwide. ABIM is planning an extensive research effort to analyze a focused-practice MOC, using hospitalists as the test subjects.
One area in which the FPHM varies from the traditional MOC is its every-three-year requirement to complete practice-improvement modules (PIMs). Dr. Dassani likens the higher standard to the kind of continuing education and training programs other specialized fields require.
“I think it’s a good idea. It’s more work, but I support it,” he says. “Every time you get onto a plane, you hope the pilot is certified every six months, versus no one has evaluated the pilot in two years. Your safety is in his hands. Take that same analogy to medicine.
“You will have time,” he adds. “It’s 60 points over three years. One PIM is 40 points, so it’s not overwhelming.”—JC
Jitendra Dassani, MD, is a hospitalist who works for Advocate Medical Group at Illinois Masonic Hospital in Chicago. He passed the American Board of Internal Medicine’s (ABIM) traditional internal-medicine Maintenance of Certification (MOC) examination in 2008. According to current guidelines, he won’t have to recertify until 2018.
But Dr. Dassani is more than a veteran hospitalist. He’s practiced hospital-based medicine for well over a decade, and is planning on a long and prosperous HM career. In fact, he’s so dedicated to the field that he is planning to recertify through ABIM’s new Focused Practice in Hospital Medicine (FPHM) MOC next year—or, at the very latest, in 2012.
“I’ve been a hospitalist for 13 years, and I think it’s important to have something that can assess your knowledge and abilities as a hospitalist,” says Dr. Dassani, one of nearly 200 hospitalists who have signed up for the FPHM pathway. The first secure exam will be administered in October. “I took the general IM exam in 2008. That’s the traditional ABIM boards; I felt some of the questions were not related to my practice. That’s why I think the [FPHM] is really good and really important.”
He’s not alone. SHM and ABIM are anxious to see where this new MOC pathway goes. SHM leaders think the FPHM offers career validation and a customized MOC process to the 30,000 hospitalists practicing nationwide. ABIM is planning an extensive research effort to analyze a focused-practice MOC, using hospitalists as the test subjects.
One area in which the FPHM varies from the traditional MOC is its every-three-year requirement to complete practice-improvement modules (PIMs). Dr. Dassani likens the higher standard to the kind of continuing education and training programs other specialized fields require.
“I think it’s a good idea. It’s more work, but I support it,” he says. “Every time you get onto a plane, you hope the pilot is certified every six months, versus no one has evaluated the pilot in two years. Your safety is in his hands. Take that same analogy to medicine.
“You will have time,” he adds. “It’s 60 points over three years. One PIM is 40 points, so it’s not overwhelming.”—JC
ONLINE EXCLUSIVE: Focused Practice in Hospital Medicine audio interview with SHM President Jeff Wiese, MD, FACP, SFHM
2010 HM Awards Winners
Awards of Excellence
Award for Excellence in Teamwork in Quality Improvement
The Emory University Hospital Healthcare Team, co-led by Jason Stein, MD, FHM, Carolyn Hill, RN, Laura Phillips, and Dee Cantrell, received the award for excellence in QI teamwork for their groundbreaking work on VTE prophylaxis, a key indicator of hospital quality.
Award for Clinical Excellence
Jennifer Myers, MD, FHM, for leading the “rapid root cause analysis” process that convenes medical error reviews with front-line clinicians and staff.
Award for Excellence in Teaching
Amir Jaffer, MD, FHM
Award for Outstanding Service in Hospital Medicine
Mitchell Wilson, MD, FHM
Award for Excellence in Research
Margaret C. Fang MD, MPH, FHM
Research, Innovation, and Clinical Vignettes Winners
2010 Innovation Poster Winner: Aaron Farberg, BS, Andrew Lin, BS, Latoya Kuhn, MPH, Scott Flanders, MD, SFHM, Christopher Kim, MD, MBA, University of Michigan Medical School, “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication.”
2010 Adult Vignette Winner: Jennie Wei, MD, and Patrick Kneeland, MD, University of California at San Francisco, “A Case of Skin Ulcers and Neutropenia: Definitely Not a Helminth Problem.”
2010 Research Winner: Will Southern, MD, MS, and Julia Arnsten, MD, MPH, Montefiore Medical Center, Bronx, N.Y.: “Increased Mortality and Readmission Among Patients Discharged against Medical Advice.”
2010 Pediatric Vignette Winner: Harry Hoar, MD, Baystate Children’s Hospitalist, Springfield, Mass., “A Teen with Varices: An Uncommon Presentation of a Familiar Disease.”
Researchers Earn First SHM Junior Faculty Development Awards
Two-year, $50,000 commitment bolsters academic pursuits for young hospitalists
By Jason Carris
NATIONAL HARBOR, Md.– Kirsten Kangelaris, MD, and Evan Fieldston, MD, MBA, MSHP, were presented $50,000 Junior Faculty Development Awards at HM10. The first-year awards are part of SHM’s commitment to helping the “generation of new knowledge,” said Scott Flanders, SHM’s outgoing president.
Dr. Kangelaris, a fellow in internal medicine at the University of California at San Francisco, focuses her research on continued clinical and biologic genetic risk-prediction algorithms that will improve the triage and early-management strategies for hospitalized patients with inflammatory illness.
Dr. Fieldston, an assistant professor in pediatrics at the University of Pennsylvania School of Medicine and Children’s Hospital of Philadelphia, plans to use his award to examine the association between dynamic aspects of workload, workforce, and quality of care at children’s hospitals.
SHM also handed out its annual Awards of Excellence (above left) and announced winners from the Research, Innovation, and Clinical Vignette competition (below left). Judges scored more than 400 posters; some of the winning project teams included medical students.
“I am particularly proud to see that we had medical students as award winners,” said Flanders, chief of the hospital medicine division at the University of Michigan Health System in Ann Arbor. “That gives me great hope for the future of HM.”
Awards of Excellence
Award for Excellence in Teamwork in Quality Improvement
The Emory University Hospital Healthcare Team, co-led by Jason Stein, MD, FHM, Carolyn Hill, RN, Laura Phillips, and Dee Cantrell, received the award for excellence in QI teamwork for their groundbreaking work on VTE prophylaxis, a key indicator of hospital quality.
Award for Clinical Excellence
Jennifer Myers, MD, FHM, for leading the “rapid root cause analysis” process that convenes medical error reviews with front-line clinicians and staff.
Award for Excellence in Teaching
Amir Jaffer, MD, FHM
Award for Outstanding Service in Hospital Medicine
Mitchell Wilson, MD, FHM
Award for Excellence in Research
Margaret C. Fang MD, MPH, FHM
Research, Innovation, and Clinical Vignettes Winners
2010 Innovation Poster Winner: Aaron Farberg, BS, Andrew Lin, BS, Latoya Kuhn, MPH, Scott Flanders, MD, SFHM, Christopher Kim, MD, MBA, University of Michigan Medical School, “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication.”
2010 Adult Vignette Winner: Jennie Wei, MD, and Patrick Kneeland, MD, University of California at San Francisco, “A Case of Skin Ulcers and Neutropenia: Definitely Not a Helminth Problem.”
2010 Research Winner: Will Southern, MD, MS, and Julia Arnsten, MD, MPH, Montefiore Medical Center, Bronx, N.Y.: “Increased Mortality and Readmission Among Patients Discharged against Medical Advice.”
2010 Pediatric Vignette Winner: Harry Hoar, MD, Baystate Children’s Hospitalist, Springfield, Mass., “A Teen with Varices: An Uncommon Presentation of a Familiar Disease.”
Researchers Earn First SHM Junior Faculty Development Awards
Two-year, $50,000 commitment bolsters academic pursuits for young hospitalists
By Jason Carris
NATIONAL HARBOR, Md.– Kirsten Kangelaris, MD, and Evan Fieldston, MD, MBA, MSHP, were presented $50,000 Junior Faculty Development Awards at HM10. The first-year awards are part of SHM’s commitment to helping the “generation of new knowledge,” said Scott Flanders, SHM’s outgoing president.
Dr. Kangelaris, a fellow in internal medicine at the University of California at San Francisco, focuses her research on continued clinical and biologic genetic risk-prediction algorithms that will improve the triage and early-management strategies for hospitalized patients with inflammatory illness.
Dr. Fieldston, an assistant professor in pediatrics at the University of Pennsylvania School of Medicine and Children’s Hospital of Philadelphia, plans to use his award to examine the association between dynamic aspects of workload, workforce, and quality of care at children’s hospitals.
SHM also handed out its annual Awards of Excellence (above left) and announced winners from the Research, Innovation, and Clinical Vignette competition (below left). Judges scored more than 400 posters; some of the winning project teams included medical students.
“I am particularly proud to see that we had medical students as award winners,” said Flanders, chief of the hospital medicine division at the University of Michigan Health System in Ann Arbor. “That gives me great hope for the future of HM.”
Awards of Excellence
Award for Excellence in Teamwork in Quality Improvement
The Emory University Hospital Healthcare Team, co-led by Jason Stein, MD, FHM, Carolyn Hill, RN, Laura Phillips, and Dee Cantrell, received the award for excellence in QI teamwork for their groundbreaking work on VTE prophylaxis, a key indicator of hospital quality.
Award for Clinical Excellence
Jennifer Myers, MD, FHM, for leading the “rapid root cause analysis” process that convenes medical error reviews with front-line clinicians and staff.
Award for Excellence in Teaching
Amir Jaffer, MD, FHM
Award for Outstanding Service in Hospital Medicine
Mitchell Wilson, MD, FHM
Award for Excellence in Research
Margaret C. Fang MD, MPH, FHM
Research, Innovation, and Clinical Vignettes Winners
2010 Innovation Poster Winner: Aaron Farberg, BS, Andrew Lin, BS, Latoya Kuhn, MPH, Scott Flanders, MD, SFHM, Christopher Kim, MD, MBA, University of Michigan Medical School, “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication.”
2010 Adult Vignette Winner: Jennie Wei, MD, and Patrick Kneeland, MD, University of California at San Francisco, “A Case of Skin Ulcers and Neutropenia: Definitely Not a Helminth Problem.”
2010 Research Winner: Will Southern, MD, MS, and Julia Arnsten, MD, MPH, Montefiore Medical Center, Bronx, N.Y.: “Increased Mortality and Readmission Among Patients Discharged against Medical Advice.”
2010 Pediatric Vignette Winner: Harry Hoar, MD, Baystate Children’s Hospitalist, Springfield, Mass., “A Teen with Varices: An Uncommon Presentation of a Familiar Disease.”
Researchers Earn First SHM Junior Faculty Development Awards
Two-year, $50,000 commitment bolsters academic pursuits for young hospitalists
By Jason Carris
NATIONAL HARBOR, Md.– Kirsten Kangelaris, MD, and Evan Fieldston, MD, MBA, MSHP, were presented $50,000 Junior Faculty Development Awards at HM10. The first-year awards are part of SHM’s commitment to helping the “generation of new knowledge,” said Scott Flanders, SHM’s outgoing president.
Dr. Kangelaris, a fellow in internal medicine at the University of California at San Francisco, focuses her research on continued clinical and biologic genetic risk-prediction algorithms that will improve the triage and early-management strategies for hospitalized patients with inflammatory illness.
Dr. Fieldston, an assistant professor in pediatrics at the University of Pennsylvania School of Medicine and Children’s Hospital of Philadelphia, plans to use his award to examine the association between dynamic aspects of workload, workforce, and quality of care at children’s hospitals.
SHM also handed out its annual Awards of Excellence (above left) and announced winners from the Research, Innovation, and Clinical Vignette competition (below left). Judges scored more than 400 posters; some of the winning project teams included medical students.
“I am particularly proud to see that we had medical students as award winners,” said Flanders, chief of the hospital medicine division at the University of Michigan Health System in Ann Arbor. “That gives me great hope for the future of HM.”
Focused Practice in Hospital Medicine
Some in her HM group think Cathleen Ammann, MD, is the guinea pig. Dr. Ammann, the medical director of the hospital medicine division at Wentworth-Douglass Hospital in Dover, N.H., will be one of the first to complete her American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) through the new Focused Practice in Hospital Medicine (FPHM) pathway. Dr. Ammann—and the hospital administration—sees things a little differently.
“Am I the guinea pig or a pioneer?” a hospitalist in Dr. Ammann’s group asked her recently. “I definitely see it as being a pioneer. When you look back in another 10 years, hospital medicine might be a specialty with its own certification. I know it’s a little corny, but I look forward to getting in on that at the ground floor.”
Dr. Ammann is one of about 175 hospitalists who have signed up to recertify through FPHM. Her internal-medicine (IM) certification expires at the end of the year, so she will be taking the recertification exam Oct. 25.
“I hope the test focuses more on what I’m doing … stroke, quality measures,” she says. “Hospitalists know that stuff like the back of our hand. … I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine. It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Dr. Ammann sums up the thinking of many HM leaders who’ve been working with ABIM and the American Board of Medical Specialties to launch the MOC pathway for hospitalists: Not only does a focused practice certification allow the more than 30,000 hospitalists in the U.S. to define themselves as different, it also provides hospitalists an MOC process and secured examination more acutely tailored to their skill sets and daily practice. The new pathway also requires ACLS certification and stresses continued “maintenance of competency,” according to SHM leaders, through a triennial self-evaluation requirement (60 self-evaluation points, with at least 20 points from medical knowledge modules and 40 points from completion of practice performance modules). The traditional IM MOC requires a practice-improvement module (PIM) every 10 years.
“The process will ask diplomates to participate in practice improvement every three years, which will focus on the ongoing need for performance improvement,” says Jeff Wiese, MD, FACP, SFHM, SHM president and chair of the ABIM Hospital Medicine MOC Question Writing Committee. “It will separate out the authentic hospitalist who is representing the goals and virtues that we are espousing as a society, particularly with regards to quality healthcare and safe healthcare. But I also think there are unique benefits for the patient that will be receiving the healthcare, because through this process, I believe, every diplomate will be a better hospitalist as a product of having done it.”
Here’s a brief look at what hospitalists interested in the FPHM MOC can expect:
The Process and Timeline
ABIM and SHM began working toward an HM-focused pathway about five years ago, and the two groups announced the FPHM program in September 2009. ABIM is in the process of retooling its website for the new MOC pathway. The entry system—to sign up and begin the MOC’s attestation process—was made public in March. The registration interface for the secure exam opened to the hospitalist community May 1, says Eric Holmboe, MD, ABIM’s chief medical officer.
“Diplomates can signify their interest and start the attestation process, which will allow them to get formal entry into the pathway,” Dr. Holmboe says. “Once they receive the attestation confirmation back, they can start doing the requirements around the medical knowledge and performance and practice requirements. Those are all available on the website. … We’re excited. The first phase of the project is live. This is a brand-new pathway for MOC, and we’re really hopeful people will find it valuable and useful.”
Board recertification is no easy task, and prospective diplomates should organize a plan of attack based upon individual workloads and regular involvement in performance-improvement programs. Some hospitalists will only need six to nine months to complete all the requirements and take the exam; others might take a conservative approach and need one to two years.
“Eighteen months is very reasonable,” Dr. Holmboe says. “Because of the 40-point requirement for the evaluation of performance and practice, that means you have to do the hospital-based PIM or self-directed PIM, or some combination thereof, twice. So if you haven’t been active in QI projects in your hospital, you really need to get going.”
Some hospitalists and HM groups work on quality-improvement (QI) projects regularly. Dr. Ammann plans to use a recent QI project looking at her group’s compliance with antibiotic selection for pneumonia to satisfy one of her required PIMs.
“[The three-year] requirement should be easy for directors because we’re always doing that kind of work anyway,” she says. “We just finished a project where we had to improve our compliance with antibiotic selection. We looked at our processes and found that our pathway wasn’t clear, and it could be interpreted a couple different ways. So our chief of medicine and I just changed the pathway, put it out there, and since then, our compliance has consistently been 100%.
We have two quarters of data, and I’m going to use that for my PIM, which is nice, because it’s done.”
For hospitalists whose certification runs out in 2011 or beyond, Dr. Holmboe suggests the following timeline:
Now through end of 2010
- Register for the Focused Practice in Hospital Medicine MOC pathway on ABIM’ website (www.abim.org/moc/policies. aspx);
- Complete the attestation process;
- Get involved in an appropriate (hospital-based) performance-improvement activity; and
- Complete Update in Hospital Medicine using ABIM or ACP medical education modules.

—Cathleen Ammann, MD, medical director, hospital medicine division, Wentworth-Douglass Hospital, Dover, N.H.
First six months of 2011
- Complete the next yearly Update in HM module;
- Develop a strategy to prepare for the exam, which is given in the fall; and
- Plan and complete your second performance improvement activity.
Second half of 2011
- Prepare for the exam; and
- Pass the exam.
Start Process Now, Start Earning Points
ABIM is encouraging prospective FPHM diplomates to begin working on medical-knowledge modules. Most are designed to “stretch folks and to get them to look things up.”
“ACP, to their credit, also has hospital-based modules,” Dr. Holmboe says. “So if somebody is a dual member, they can certainly use the ACP’s MKSAP (Medical Knowledge Self-Assessment Program) hospital-based modules as well. We’re also working with SHM, looking for areas they might fill in around knowledge and updates—things that could be brought into the program over time.”
In regard to the evaluation and performance modules, ABIM offers three main pathways, including the Hospital-Based PIM, which targets core measure sets like community-acquired pneumonia and congestive heart failure and DVT prophylaxis. “Hospitalists can use those PIMs to start a quality-improvement program, or they can use it to report on one they are working on,” Dr. Holmboe says, adding the Hospital Based PIM’s online module will be redesigned this summer to improve the user experience.
Two other approaches are the Self-Directed PIM and the Accepted Quality Improvement programs. “That would be for hospitalists who may not be working on the core measure sets in the hospital-based PIM, but are still important,” he says. “They can use that module to report on those activities and get the points they need.”
Dr. Holmboe also points out that diplomates do not have to complete all the other requirements before they take the exam. “Some people get confused; you don’t have to cram in the 100 points before the exam,” Dr. Holmboe explains. He notes that the exam can, for example, be taken this year and the remainder of the requirements completed at a later date.
“If it was up to me, you should do a [PIM] every year,” says Larry Wellikson, MD, SFHM, CEO of SHM and one of the architects of the new FPHM pathway. “If you are a real hospitalist, completing a PIM every three years shouldn’t be a big deal. You should be able to say, ‘I’ve looked at 10 things: how I’m doing in pneumonia, how I’m doing in DVT, how I’m doing in glycemic control. This isn’t work for me; it’s part of my workflow.’ It’s like asking a salesman how many sales calls have you made, how many miles have you driven, and how many sales have you closed.”
The Examination
Dr. Wiese, associate dean of Graduate Medical Education and professor of medicine at Tulane University in New Orleans, completed his 10-year MOC in 2008, and he says the process made him “a better physician.” As president of SHM and chair of the FPHM test-writing committee, he envisions that the new MOC pathway will help “ramp up the quality of care for the hospitalized patient.”
“The FPHM MOC process is much more than just a different exam,” he says. “It is true the secure examination will have a lot more hospital-medicine-patient content focus, but not to the exclusion of ambulatory content.”

—Jeff Wiese, SHM president, ABIM Focused Practice in Hospital Medicine Test Writing Committee chair
The content-area blueprint (see “Traditional IM Test vs. Focused Practice in HM Test” below) for the FPHM exam includes 15% of questions in the areas of quality and patient safety, along with another 15% in consultative and comanagement topics. Transitions of care and ambulatory questions make up another 15% of the exam.
“If there is one component of the exam that will [be HM-focused], it’s the questions of the exam that are focusing on the core principles of quality and patient safety,” Dr. Wiese says.
That’s music to the ears of many hospitalists—including Dr. Ammann—who know questions about managing cholesterol aren’t relevant to hospitalists. Dr. Ammann was an office-based physician before becoming a hospitalist in 2005. One year later, she was promoted to director of her group, which includes 14 physicians and two nonphysician providers.
“I was really hoping I would be able to [MOC] through the focused practice in HM,” she says. “I did practice office medicine, so I probably have a little advantage. But I was not looking forward to spending time learning and brushing up on things that I am not doing anymore—not only because I’m not doing it anymore, but it would be a waste of time because I’m not going to be doing it, either.”
One of her hospitalist colleagues is taking the traditional IM pathway to MOC, Dr. Ammann says, because “she doesn’t want to limit her scope.” But that’s not how Dr. Ammann sees the FPHM. She is committed to HM and doesn’t have “any problems kissing office medicine goodbye.”
“I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine,” she says. “It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Educational Efforts
Vikas Parekh, MD, FHM, is in his second year as the chair of SHM’s Education Committee, and says the first task at hand is to educate hospitalists about the new FPHM pathway to MOC. The University of Michigan hospitalist says his committee, working with ABIM and SHM staff, is focused on two major educational efforts: developing the SHM strategy to assist hospitalists with the new FPHM MOC pathway, and “fulfilling the needs of hospitalists, in terms of the resources they have for the MOC process.”
“We’ve already started down this route, in terms of developing resources,” Dr. Parekh says. “We’ve done a few things that have been easy. One is the ABIM learning session pre-course at the annual meeting. … It earns you points toward the medical-knowledge component.”
ABIM and ACP are the traditional avenues for medical-knowledge and practice-improvement requirements for the MOC process. SHM and ABIM currently are working to develop medical-knowledge modules in the domains of patient safety and quality improvement, areas most relevant to HM. Dr. Parekh expects those components to be available in early 2011.
“Practice improvement is likely to be our second main effort,” Dr. Parekh says. “SHM has a lot of resources within our resource rooms that have the shell of what you would really need to meet ABIM requirements for a PIM but aren’t quite complete or thorough enough, or have all the bells and whistles that ABIM wants them to have. … We think we can do a much better job focusing the PIMs to hospitalists.”
At a more granular level, Dr. Wellikson envisions a “suite of products” to assist members in the MOC process. “What we are trying to do is develop resources that help people practice better medicine,” he says, “and while we are helping you practice better medicine, you can also use that to prove to [ABIM] that you have done it.
“So if you log onto the website today and downloaded and completed any of those SHM resource rooms, somewhere in the next several months you will be able to click on a form, enter the results, send it to ABIM, and you’ll have satisfied a PIM,” Dr. Wellikson says. “You can do the work today.”
SHM’s Project BOOST (Better Outcomes for Older Adults through Safer Transitions) and Glycemic Control Mentored Implementation programs are prime candidates for Web-based PIMs, according to Dr. Holmboe.
“I think it is still very early, but we are very excited about this,” Dr. Parekh says. “I think a lot of people still have questions about what exactly this mean to me, and why should I recertify through this focused practice as opposed to the traditional general pathway? We hope to change that by making the resources focused to their practice.” TH
Jason Carris is editor of The Hospitalist.
Some in her HM group think Cathleen Ammann, MD, is the guinea pig. Dr. Ammann, the medical director of the hospital medicine division at Wentworth-Douglass Hospital in Dover, N.H., will be one of the first to complete her American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) through the new Focused Practice in Hospital Medicine (FPHM) pathway. Dr. Ammann—and the hospital administration—sees things a little differently.
“Am I the guinea pig or a pioneer?” a hospitalist in Dr. Ammann’s group asked her recently. “I definitely see it as being a pioneer. When you look back in another 10 years, hospital medicine might be a specialty with its own certification. I know it’s a little corny, but I look forward to getting in on that at the ground floor.”
Dr. Ammann is one of about 175 hospitalists who have signed up to recertify through FPHM. Her internal-medicine (IM) certification expires at the end of the year, so she will be taking the recertification exam Oct. 25.
“I hope the test focuses more on what I’m doing … stroke, quality measures,” she says. “Hospitalists know that stuff like the back of our hand. … I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine. It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Dr. Ammann sums up the thinking of many HM leaders who’ve been working with ABIM and the American Board of Medical Specialties to launch the MOC pathway for hospitalists: Not only does a focused practice certification allow the more than 30,000 hospitalists in the U.S. to define themselves as different, it also provides hospitalists an MOC process and secured examination more acutely tailored to their skill sets and daily practice. The new pathway also requires ACLS certification and stresses continued “maintenance of competency,” according to SHM leaders, through a triennial self-evaluation requirement (60 self-evaluation points, with at least 20 points from medical knowledge modules and 40 points from completion of practice performance modules). The traditional IM MOC requires a practice-improvement module (PIM) every 10 years.
“The process will ask diplomates to participate in practice improvement every three years, which will focus on the ongoing need for performance improvement,” says Jeff Wiese, MD, FACP, SFHM, SHM president and chair of the ABIM Hospital Medicine MOC Question Writing Committee. “It will separate out the authentic hospitalist who is representing the goals and virtues that we are espousing as a society, particularly with regards to quality healthcare and safe healthcare. But I also think there are unique benefits for the patient that will be receiving the healthcare, because through this process, I believe, every diplomate will be a better hospitalist as a product of having done it.”
Here’s a brief look at what hospitalists interested in the FPHM MOC can expect:
The Process and Timeline
ABIM and SHM began working toward an HM-focused pathway about five years ago, and the two groups announced the FPHM program in September 2009. ABIM is in the process of retooling its website for the new MOC pathway. The entry system—to sign up and begin the MOC’s attestation process—was made public in March. The registration interface for the secure exam opened to the hospitalist community May 1, says Eric Holmboe, MD, ABIM’s chief medical officer.
“Diplomates can signify their interest and start the attestation process, which will allow them to get formal entry into the pathway,” Dr. Holmboe says. “Once they receive the attestation confirmation back, they can start doing the requirements around the medical knowledge and performance and practice requirements. Those are all available on the website. … We’re excited. The first phase of the project is live. This is a brand-new pathway for MOC, and we’re really hopeful people will find it valuable and useful.”
Board recertification is no easy task, and prospective diplomates should organize a plan of attack based upon individual workloads and regular involvement in performance-improvement programs. Some hospitalists will only need six to nine months to complete all the requirements and take the exam; others might take a conservative approach and need one to two years.
“Eighteen months is very reasonable,” Dr. Holmboe says. “Because of the 40-point requirement for the evaluation of performance and practice, that means you have to do the hospital-based PIM or self-directed PIM, or some combination thereof, twice. So if you haven’t been active in QI projects in your hospital, you really need to get going.”
Some hospitalists and HM groups work on quality-improvement (QI) projects regularly. Dr. Ammann plans to use a recent QI project looking at her group’s compliance with antibiotic selection for pneumonia to satisfy one of her required PIMs.
“[The three-year] requirement should be easy for directors because we’re always doing that kind of work anyway,” she says. “We just finished a project where we had to improve our compliance with antibiotic selection. We looked at our processes and found that our pathway wasn’t clear, and it could be interpreted a couple different ways. So our chief of medicine and I just changed the pathway, put it out there, and since then, our compliance has consistently been 100%.
We have two quarters of data, and I’m going to use that for my PIM, which is nice, because it’s done.”
For hospitalists whose certification runs out in 2011 or beyond, Dr. Holmboe suggests the following timeline:
Now through end of 2010
- Register for the Focused Practice in Hospital Medicine MOC pathway on ABIM’ website (www.abim.org/moc/policies. aspx);
- Complete the attestation process;
- Get involved in an appropriate (hospital-based) performance-improvement activity; and
- Complete Update in Hospital Medicine using ABIM or ACP medical education modules.

—Cathleen Ammann, MD, medical director, hospital medicine division, Wentworth-Douglass Hospital, Dover, N.H.
First six months of 2011
- Complete the next yearly Update in HM module;
- Develop a strategy to prepare for the exam, which is given in the fall; and
- Plan and complete your second performance improvement activity.
Second half of 2011
- Prepare for the exam; and
- Pass the exam.
Start Process Now, Start Earning Points
ABIM is encouraging prospective FPHM diplomates to begin working on medical-knowledge modules. Most are designed to “stretch folks and to get them to look things up.”
“ACP, to their credit, also has hospital-based modules,” Dr. Holmboe says. “So if somebody is a dual member, they can certainly use the ACP’s MKSAP (Medical Knowledge Self-Assessment Program) hospital-based modules as well. We’re also working with SHM, looking for areas they might fill in around knowledge and updates—things that could be brought into the program over time.”
In regard to the evaluation and performance modules, ABIM offers three main pathways, including the Hospital-Based PIM, which targets core measure sets like community-acquired pneumonia and congestive heart failure and DVT prophylaxis. “Hospitalists can use those PIMs to start a quality-improvement program, or they can use it to report on one they are working on,” Dr. Holmboe says, adding the Hospital Based PIM’s online module will be redesigned this summer to improve the user experience.
Two other approaches are the Self-Directed PIM and the Accepted Quality Improvement programs. “That would be for hospitalists who may not be working on the core measure sets in the hospital-based PIM, but are still important,” he says. “They can use that module to report on those activities and get the points they need.”
Dr. Holmboe also points out that diplomates do not have to complete all the other requirements before they take the exam. “Some people get confused; you don’t have to cram in the 100 points before the exam,” Dr. Holmboe explains. He notes that the exam can, for example, be taken this year and the remainder of the requirements completed at a later date.
“If it was up to me, you should do a [PIM] every year,” says Larry Wellikson, MD, SFHM, CEO of SHM and one of the architects of the new FPHM pathway. “If you are a real hospitalist, completing a PIM every three years shouldn’t be a big deal. You should be able to say, ‘I’ve looked at 10 things: how I’m doing in pneumonia, how I’m doing in DVT, how I’m doing in glycemic control. This isn’t work for me; it’s part of my workflow.’ It’s like asking a salesman how many sales calls have you made, how many miles have you driven, and how many sales have you closed.”
The Examination
Dr. Wiese, associate dean of Graduate Medical Education and professor of medicine at Tulane University in New Orleans, completed his 10-year MOC in 2008, and he says the process made him “a better physician.” As president of SHM and chair of the FPHM test-writing committee, he envisions that the new MOC pathway will help “ramp up the quality of care for the hospitalized patient.”
“The FPHM MOC process is much more than just a different exam,” he says. “It is true the secure examination will have a lot more hospital-medicine-patient content focus, but not to the exclusion of ambulatory content.”

—Jeff Wiese, SHM president, ABIM Focused Practice in Hospital Medicine Test Writing Committee chair
The content-area blueprint (see “Traditional IM Test vs. Focused Practice in HM Test” below) for the FPHM exam includes 15% of questions in the areas of quality and patient safety, along with another 15% in consultative and comanagement topics. Transitions of care and ambulatory questions make up another 15% of the exam.
“If there is one component of the exam that will [be HM-focused], it’s the questions of the exam that are focusing on the core principles of quality and patient safety,” Dr. Wiese says.
That’s music to the ears of many hospitalists—including Dr. Ammann—who know questions about managing cholesterol aren’t relevant to hospitalists. Dr. Ammann was an office-based physician before becoming a hospitalist in 2005. One year later, she was promoted to director of her group, which includes 14 physicians and two nonphysician providers.
“I was really hoping I would be able to [MOC] through the focused practice in HM,” she says. “I did practice office medicine, so I probably have a little advantage. But I was not looking forward to spending time learning and brushing up on things that I am not doing anymore—not only because I’m not doing it anymore, but it would be a waste of time because I’m not going to be doing it, either.”
One of her hospitalist colleagues is taking the traditional IM pathway to MOC, Dr. Ammann says, because “she doesn’t want to limit her scope.” But that’s not how Dr. Ammann sees the FPHM. She is committed to HM and doesn’t have “any problems kissing office medicine goodbye.”
“I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine,” she says. “It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Educational Efforts
Vikas Parekh, MD, FHM, is in his second year as the chair of SHM’s Education Committee, and says the first task at hand is to educate hospitalists about the new FPHM pathway to MOC. The University of Michigan hospitalist says his committee, working with ABIM and SHM staff, is focused on two major educational efforts: developing the SHM strategy to assist hospitalists with the new FPHM MOC pathway, and “fulfilling the needs of hospitalists, in terms of the resources they have for the MOC process.”
“We’ve already started down this route, in terms of developing resources,” Dr. Parekh says. “We’ve done a few things that have been easy. One is the ABIM learning session pre-course at the annual meeting. … It earns you points toward the medical-knowledge component.”
ABIM and ACP are the traditional avenues for medical-knowledge and practice-improvement requirements for the MOC process. SHM and ABIM currently are working to develop medical-knowledge modules in the domains of patient safety and quality improvement, areas most relevant to HM. Dr. Parekh expects those components to be available in early 2011.
“Practice improvement is likely to be our second main effort,” Dr. Parekh says. “SHM has a lot of resources within our resource rooms that have the shell of what you would really need to meet ABIM requirements for a PIM but aren’t quite complete or thorough enough, or have all the bells and whistles that ABIM wants them to have. … We think we can do a much better job focusing the PIMs to hospitalists.”
At a more granular level, Dr. Wellikson envisions a “suite of products” to assist members in the MOC process. “What we are trying to do is develop resources that help people practice better medicine,” he says, “and while we are helping you practice better medicine, you can also use that to prove to [ABIM] that you have done it.
“So if you log onto the website today and downloaded and completed any of those SHM resource rooms, somewhere in the next several months you will be able to click on a form, enter the results, send it to ABIM, and you’ll have satisfied a PIM,” Dr. Wellikson says. “You can do the work today.”
SHM’s Project BOOST (Better Outcomes for Older Adults through Safer Transitions) and Glycemic Control Mentored Implementation programs are prime candidates for Web-based PIMs, according to Dr. Holmboe.
“I think it is still very early, but we are very excited about this,” Dr. Parekh says. “I think a lot of people still have questions about what exactly this mean to me, and why should I recertify through this focused practice as opposed to the traditional general pathway? We hope to change that by making the resources focused to their practice.” TH
Jason Carris is editor of The Hospitalist.
Some in her HM group think Cathleen Ammann, MD, is the guinea pig. Dr. Ammann, the medical director of the hospital medicine division at Wentworth-Douglass Hospital in Dover, N.H., will be one of the first to complete her American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) through the new Focused Practice in Hospital Medicine (FPHM) pathway. Dr. Ammann—and the hospital administration—sees things a little differently.
“Am I the guinea pig or a pioneer?” a hospitalist in Dr. Ammann’s group asked her recently. “I definitely see it as being a pioneer. When you look back in another 10 years, hospital medicine might be a specialty with its own certification. I know it’s a little corny, but I look forward to getting in on that at the ground floor.”
Dr. Ammann is one of about 175 hospitalists who have signed up to recertify through FPHM. Her internal-medicine (IM) certification expires at the end of the year, so she will be taking the recertification exam Oct. 25.
“I hope the test focuses more on what I’m doing … stroke, quality measures,” she says. “Hospitalists know that stuff like the back of our hand. … I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine. It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Dr. Ammann sums up the thinking of many HM leaders who’ve been working with ABIM and the American Board of Medical Specialties to launch the MOC pathway for hospitalists: Not only does a focused practice certification allow the more than 30,000 hospitalists in the U.S. to define themselves as different, it also provides hospitalists an MOC process and secured examination more acutely tailored to their skill sets and daily practice. The new pathway also requires ACLS certification and stresses continued “maintenance of competency,” according to SHM leaders, through a triennial self-evaluation requirement (60 self-evaluation points, with at least 20 points from medical knowledge modules and 40 points from completion of practice performance modules). The traditional IM MOC requires a practice-improvement module (PIM) every 10 years.
“The process will ask diplomates to participate in practice improvement every three years, which will focus on the ongoing need for performance improvement,” says Jeff Wiese, MD, FACP, SFHM, SHM president and chair of the ABIM Hospital Medicine MOC Question Writing Committee. “It will separate out the authentic hospitalist who is representing the goals and virtues that we are espousing as a society, particularly with regards to quality healthcare and safe healthcare. But I also think there are unique benefits for the patient that will be receiving the healthcare, because through this process, I believe, every diplomate will be a better hospitalist as a product of having done it.”
Here’s a brief look at what hospitalists interested in the FPHM MOC can expect:
The Process and Timeline
ABIM and SHM began working toward an HM-focused pathway about five years ago, and the two groups announced the FPHM program in September 2009. ABIM is in the process of retooling its website for the new MOC pathway. The entry system—to sign up and begin the MOC’s attestation process—was made public in March. The registration interface for the secure exam opened to the hospitalist community May 1, says Eric Holmboe, MD, ABIM’s chief medical officer.
“Diplomates can signify their interest and start the attestation process, which will allow them to get formal entry into the pathway,” Dr. Holmboe says. “Once they receive the attestation confirmation back, they can start doing the requirements around the medical knowledge and performance and practice requirements. Those are all available on the website. … We’re excited. The first phase of the project is live. This is a brand-new pathway for MOC, and we’re really hopeful people will find it valuable and useful.”
Board recertification is no easy task, and prospective diplomates should organize a plan of attack based upon individual workloads and regular involvement in performance-improvement programs. Some hospitalists will only need six to nine months to complete all the requirements and take the exam; others might take a conservative approach and need one to two years.
“Eighteen months is very reasonable,” Dr. Holmboe says. “Because of the 40-point requirement for the evaluation of performance and practice, that means you have to do the hospital-based PIM or self-directed PIM, or some combination thereof, twice. So if you haven’t been active in QI projects in your hospital, you really need to get going.”
Some hospitalists and HM groups work on quality-improvement (QI) projects regularly. Dr. Ammann plans to use a recent QI project looking at her group’s compliance with antibiotic selection for pneumonia to satisfy one of her required PIMs.
“[The three-year] requirement should be easy for directors because we’re always doing that kind of work anyway,” she says. “We just finished a project where we had to improve our compliance with antibiotic selection. We looked at our processes and found that our pathway wasn’t clear, and it could be interpreted a couple different ways. So our chief of medicine and I just changed the pathway, put it out there, and since then, our compliance has consistently been 100%.
We have two quarters of data, and I’m going to use that for my PIM, which is nice, because it’s done.”
For hospitalists whose certification runs out in 2011 or beyond, Dr. Holmboe suggests the following timeline:
Now through end of 2010
- Register for the Focused Practice in Hospital Medicine MOC pathway on ABIM’ website (www.abim.org/moc/policies. aspx);
- Complete the attestation process;
- Get involved in an appropriate (hospital-based) performance-improvement activity; and
- Complete Update in Hospital Medicine using ABIM or ACP medical education modules.

—Cathleen Ammann, MD, medical director, hospital medicine division, Wentworth-Douglass Hospital, Dover, N.H.
First six months of 2011
- Complete the next yearly Update in HM module;
- Develop a strategy to prepare for the exam, which is given in the fall; and
- Plan and complete your second performance improvement activity.
Second half of 2011
- Prepare for the exam; and
- Pass the exam.
Start Process Now, Start Earning Points
ABIM is encouraging prospective FPHM diplomates to begin working on medical-knowledge modules. Most are designed to “stretch folks and to get them to look things up.”
“ACP, to their credit, also has hospital-based modules,” Dr. Holmboe says. “So if somebody is a dual member, they can certainly use the ACP’s MKSAP (Medical Knowledge Self-Assessment Program) hospital-based modules as well. We’re also working with SHM, looking for areas they might fill in around knowledge and updates—things that could be brought into the program over time.”
In regard to the evaluation and performance modules, ABIM offers three main pathways, including the Hospital-Based PIM, which targets core measure sets like community-acquired pneumonia and congestive heart failure and DVT prophylaxis. “Hospitalists can use those PIMs to start a quality-improvement program, or they can use it to report on one they are working on,” Dr. Holmboe says, adding the Hospital Based PIM’s online module will be redesigned this summer to improve the user experience.
Two other approaches are the Self-Directed PIM and the Accepted Quality Improvement programs. “That would be for hospitalists who may not be working on the core measure sets in the hospital-based PIM, but are still important,” he says. “They can use that module to report on those activities and get the points they need.”
Dr. Holmboe also points out that diplomates do not have to complete all the other requirements before they take the exam. “Some people get confused; you don’t have to cram in the 100 points before the exam,” Dr. Holmboe explains. He notes that the exam can, for example, be taken this year and the remainder of the requirements completed at a later date.
“If it was up to me, you should do a [PIM] every year,” says Larry Wellikson, MD, SFHM, CEO of SHM and one of the architects of the new FPHM pathway. “If you are a real hospitalist, completing a PIM every three years shouldn’t be a big deal. You should be able to say, ‘I’ve looked at 10 things: how I’m doing in pneumonia, how I’m doing in DVT, how I’m doing in glycemic control. This isn’t work for me; it’s part of my workflow.’ It’s like asking a salesman how many sales calls have you made, how many miles have you driven, and how many sales have you closed.”
The Examination
Dr. Wiese, associate dean of Graduate Medical Education and professor of medicine at Tulane University in New Orleans, completed his 10-year MOC in 2008, and he says the process made him “a better physician.” As president of SHM and chair of the FPHM test-writing committee, he envisions that the new MOC pathway will help “ramp up the quality of care for the hospitalized patient.”
“The FPHM MOC process is much more than just a different exam,” he says. “It is true the secure examination will have a lot more hospital-medicine-patient content focus, but not to the exclusion of ambulatory content.”

—Jeff Wiese, SHM president, ABIM Focused Practice in Hospital Medicine Test Writing Committee chair
The content-area blueprint (see “Traditional IM Test vs. Focused Practice in HM Test” below) for the FPHM exam includes 15% of questions in the areas of quality and patient safety, along with another 15% in consultative and comanagement topics. Transitions of care and ambulatory questions make up another 15% of the exam.
“If there is one component of the exam that will [be HM-focused], it’s the questions of the exam that are focusing on the core principles of quality and patient safety,” Dr. Wiese says.
That’s music to the ears of many hospitalists—including Dr. Ammann—who know questions about managing cholesterol aren’t relevant to hospitalists. Dr. Ammann was an office-based physician before becoming a hospitalist in 2005. One year later, she was promoted to director of her group, which includes 14 physicians and two nonphysician providers.
“I was really hoping I would be able to [MOC] through the focused practice in HM,” she says. “I did practice office medicine, so I probably have a little advantage. But I was not looking forward to spending time learning and brushing up on things that I am not doing anymore—not only because I’m not doing it anymore, but it would be a waste of time because I’m not going to be doing it, either.”
One of her hospitalist colleagues is taking the traditional IM pathway to MOC, Dr. Ammann says, because “she doesn’t want to limit her scope.” But that’s not how Dr. Ammann sees the FPHM. She is committed to HM and doesn’t have “any problems kissing office medicine goodbye.”
“I think it will work out well for me, but I also think it will be great for our program to have a director who has a Focused Practice in Hospital Medicine,” she says. “It shows my commitment, and we can hold that up to the rest of the organization and say we really have someone who is concentrated in this field.”
Educational Efforts
Vikas Parekh, MD, FHM, is in his second year as the chair of SHM’s Education Committee, and says the first task at hand is to educate hospitalists about the new FPHM pathway to MOC. The University of Michigan hospitalist says his committee, working with ABIM and SHM staff, is focused on two major educational efforts: developing the SHM strategy to assist hospitalists with the new FPHM MOC pathway, and “fulfilling the needs of hospitalists, in terms of the resources they have for the MOC process.”
“We’ve already started down this route, in terms of developing resources,” Dr. Parekh says. “We’ve done a few things that have been easy. One is the ABIM learning session pre-course at the annual meeting. … It earns you points toward the medical-knowledge component.”
ABIM and ACP are the traditional avenues for medical-knowledge and practice-improvement requirements for the MOC process. SHM and ABIM currently are working to develop medical-knowledge modules in the domains of patient safety and quality improvement, areas most relevant to HM. Dr. Parekh expects those components to be available in early 2011.
“Practice improvement is likely to be our second main effort,” Dr. Parekh says. “SHM has a lot of resources within our resource rooms that have the shell of what you would really need to meet ABIM requirements for a PIM but aren’t quite complete or thorough enough, or have all the bells and whistles that ABIM wants them to have. … We think we can do a much better job focusing the PIMs to hospitalists.”
At a more granular level, Dr. Wellikson envisions a “suite of products” to assist members in the MOC process. “What we are trying to do is develop resources that help people practice better medicine,” he says, “and while we are helping you practice better medicine, you can also use that to prove to [ABIM] that you have done it.
“So if you log onto the website today and downloaded and completed any of those SHM resource rooms, somewhere in the next several months you will be able to click on a form, enter the results, send it to ABIM, and you’ll have satisfied a PIM,” Dr. Wellikson says. “You can do the work today.”
SHM’s Project BOOST (Better Outcomes for Older Adults through Safer Transitions) and Glycemic Control Mentored Implementation programs are prime candidates for Web-based PIMs, according to Dr. Holmboe.
“I think it is still very early, but we are very excited about this,” Dr. Parekh says. “I think a lot of people still have questions about what exactly this mean to me, and why should I recertify through this focused practice as opposed to the traditional general pathway? We hope to change that by making the resources focused to their practice.” TH
Jason Carris is editor of The Hospitalist.
Clinical Session: “The New C. Diff”
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
JOHN G. BARTLETT, MD, professor of medicine in the Department of Infectious Diseases at Johns Hopkins University School of Medicine in Baltimore, mesmerized a standing-room-only crowd of more than 500 at his lecture about the increase of Clostridium difficile in U.S. hospitals.
C. diff incidence has more than doubled since the mid-1990s, to more than 160 cases per 100,000 patients, and currently outnumbers the annual total of MRSA cases in the U.S., according to Dr. Bartlett, one of the foremost scholars on the subject. For hospitalists encountering patients with questions about the disease and where it comes from, Dr. Bartlett encouraged providers to punt that question: “The fact is, we don’t know most of the time.”
Most patients acquire C. diff during a hospital stay (74%) or a previous hospital stay (21%), and research shows the longer patients stay in the hospital, the more likely they are to acquire the disease.
—John G. Bartlett, professor, Department of Infectious Diseases, Johns Hopkins University School of Medicine, Baltimore
“It’s embedded in the fabric of hospitals,” Dr. Bartlett said. “The longer you are in the hospital, the more likely you are to get colonized.”
Prevention guidelines include:
- Hand hygiene;
- Advocate gloves and gowns;
- Patients with C. diff should be in single rooms;
- Maintain precautions until diarrhea resolves; and
- Clean with chlorine antiseptic.
Dr. Bartlett was excited to share his experience with RT-PCR testing, which he termed the “new, slick, fast” testing option for C. diff. In trials, it has been shown to be 99% sensitive and 98% specific. “If your lab does PCR, it is the best test currently available,” Dr. Bartlett said, although he cautioned that “this test detects the bug, not the toxin.”
Treatment of C. diff disease happens in the colon, and medications must make it there to be effective. The most common treatments, vancomycin and metronidazole, have pluses and minuses, Dr. Bartlett explained. Vancomycin is FDA-approved and unbeaten in clinical trials; however, it is the more expensive choice. Metronidazole is cheaper ($5 per day) and proven to be effective in mild to moderate cases, but is not FDA-approved and is unproven in severe cases.
Dr. Bartlett’s guidelines for C. diff treatment:
- Mild cases: no treatment;
- Moderate: metronidazole 250 mg four times a day for 10 to 14 days; and
- Serious: vancomycin 125 mg four times a day for 10 to 14 days.
“If metro doesn’t work, switch to oral vanco,” Dr. Bartlett said. HM10
Quality Initiative
Janet Nagamine, MD, SFHM, a hospitalist at Kaiser Permanente Medical Center in Santa Clara, Calif., has an affinity for patient safety and the West Coast.
“I’m a California girl through and through. Any sunshine or beach works for me,” says the new SHM board member, a former assistant chief of quality and former patient safety officer. “I see quality and safety as part of my clinical care. I started out saying I don’t like the way my glucoses are documented in these charts, and so I started creating graphs to help physicians understand the information better.”
Dr. Nagamine didn’t start her career as a hospitalist: She was an ICU nurse for 23 years. She also didn’t jump onto the quality-improvement (QI) bandwagon until she became a hospitalist 10 years ago. A charter SHM member, she has been a member of the Healthcare Quality and Patient Safety Committee since 2002, serving as chair the past three years.
“I began [my quality career] by addressing the obstacles that get in the way of caring for patients,” Dr. Nagamine says. “And back then, there was no shortage of opportunity to make things better.”
So it’s no surprise her professional passion will be at the forefront of her service to SHM’s board and members. “What is exciting is that we’ve really raised the bar the past five to 10 years,” she says. “We have a ways to go, but HM really is front and center to the solutions.”
One area in which Dr. Nagamine plans to be a driving force is SHM’s mentored implementation programs: Project BOOST, Glycemic Control, and VTE Prevention.
“We can all go to a seminar, take a course, but who do we turn to when we’re back in the trenches?” she says. “That’s the hard part. It helps to have someone who has been there before, made the mistakes before, to talk to. That can shave a couple years off the learning curve.”
Dr. Nagamine joins Eric Siegal, MD, SFHM, a critical-care fellow at the University of Wisconsin School of Medicine and Public Health in Madison, as the board’s newest members. Incumbent board members Joseph Ming Wah Li, MD, SFHM, assistant professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, and Mahalakshmi K. Halasymani, MD, SFHM, vice president for quality and systems improvement at Saint Joseph Mercy Health System in Ann Arbor, Mich., were re-elected for three-year terms.
Janet Nagamine, MD, SFHM, a hospitalist at Kaiser Permanente Medical Center in Santa Clara, Calif., has an affinity for patient safety and the West Coast.
“I’m a California girl through and through. Any sunshine or beach works for me,” says the new SHM board member, a former assistant chief of quality and former patient safety officer. “I see quality and safety as part of my clinical care. I started out saying I don’t like the way my glucoses are documented in these charts, and so I started creating graphs to help physicians understand the information better.”
Dr. Nagamine didn’t start her career as a hospitalist: She was an ICU nurse for 23 years. She also didn’t jump onto the quality-improvement (QI) bandwagon until she became a hospitalist 10 years ago. A charter SHM member, she has been a member of the Healthcare Quality and Patient Safety Committee since 2002, serving as chair the past three years.
“I began [my quality career] by addressing the obstacles that get in the way of caring for patients,” Dr. Nagamine says. “And back then, there was no shortage of opportunity to make things better.”
So it’s no surprise her professional passion will be at the forefront of her service to SHM’s board and members. “What is exciting is that we’ve really raised the bar the past five to 10 years,” she says. “We have a ways to go, but HM really is front and center to the solutions.”
One area in which Dr. Nagamine plans to be a driving force is SHM’s mentored implementation programs: Project BOOST, Glycemic Control, and VTE Prevention.
“We can all go to a seminar, take a course, but who do we turn to when we’re back in the trenches?” she says. “That’s the hard part. It helps to have someone who has been there before, made the mistakes before, to talk to. That can shave a couple years off the learning curve.”
Dr. Nagamine joins Eric Siegal, MD, SFHM, a critical-care fellow at the University of Wisconsin School of Medicine and Public Health in Madison, as the board’s newest members. Incumbent board members Joseph Ming Wah Li, MD, SFHM, assistant professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, and Mahalakshmi K. Halasymani, MD, SFHM, vice president for quality and systems improvement at Saint Joseph Mercy Health System in Ann Arbor, Mich., were re-elected for three-year terms.
Janet Nagamine, MD, SFHM, a hospitalist at Kaiser Permanente Medical Center in Santa Clara, Calif., has an affinity for patient safety and the West Coast.
“I’m a California girl through and through. Any sunshine or beach works for me,” says the new SHM board member, a former assistant chief of quality and former patient safety officer. “I see quality and safety as part of my clinical care. I started out saying I don’t like the way my glucoses are documented in these charts, and so I started creating graphs to help physicians understand the information better.”
Dr. Nagamine didn’t start her career as a hospitalist: She was an ICU nurse for 23 years. She also didn’t jump onto the quality-improvement (QI) bandwagon until she became a hospitalist 10 years ago. A charter SHM member, she has been a member of the Healthcare Quality and Patient Safety Committee since 2002, serving as chair the past three years.
“I began [my quality career] by addressing the obstacles that get in the way of caring for patients,” Dr. Nagamine says. “And back then, there was no shortage of opportunity to make things better.”
So it’s no surprise her professional passion will be at the forefront of her service to SHM’s board and members. “What is exciting is that we’ve really raised the bar the past five to 10 years,” she says. “We have a ways to go, but HM really is front and center to the solutions.”
One area in which Dr. Nagamine plans to be a driving force is SHM’s mentored implementation programs: Project BOOST, Glycemic Control, and VTE Prevention.
“We can all go to a seminar, take a course, but who do we turn to when we’re back in the trenches?” she says. “That’s the hard part. It helps to have someone who has been there before, made the mistakes before, to talk to. That can shave a couple years off the learning curve.”
Dr. Nagamine joins Eric Siegal, MD, SFHM, a critical-care fellow at the University of Wisconsin School of Medicine and Public Health in Madison, as the board’s newest members. Incumbent board members Joseph Ming Wah Li, MD, SFHM, assistant professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, and Mahalakshmi K. Halasymani, MD, SFHM, vice president for quality and systems improvement at Saint Joseph Mercy Health System in Ann Arbor, Mich., were re-elected for three-year terms.