User login
Malaria prevents hospitals from meeting blood demands
PHILADELPHIA—The demand for blood transfusions increases substantially during high malaria transmission season, according to a study of hospitals in Tanzania.
On average, blood demand increased about 24% from low transmission season to high transmission season.
And some hospitals could not meet the increased demand. Unmet demand was highest in government hospitals, followed by faith-based institutions and private facilities.
Bakary Drammeh, DrPH, of the Centers for Disease Control and Prevention in Atlanta, Georgia, and his colleagues presented these results in a poster (SP356) at the AABB Annual Meeting 2014.
The researchers analyzed 14,706 blood prescriptions at 42 Tanzanian hospitals—21 government, 9 private, and 12 faith-based institutions.
The team assessed the number of blood prescriptions according to high and low malaria transmission periods—June-July vs August-September.
On average, there were 130 monthly blood prescriptions written per 100 beds during high malaria transmission season and 107 written during low transmission season.
There were 189 and 153 units of blood or blood components requested per 100 beds during high and low seasons, respectively. And there were 159 and 127 units issued, respectively.
Ultimately, an average of 145 units were transfused per 100 beds during high malaria transmission season, and 122 were transfused during low transmission season.
Across all 42 hospitals, total blood prescriptions increased 29% from low malaria transmission season to high transmission season.
The number of units requested increased 26%, the number of units issued increased 34%, and the number of units transfused increased 28%.
So, on average, blood demand increased 23.5% at these 42 hospitals during high malaria transmission season. And some hospitals did not have enough blood to meet demand.
The unmet blood demand was highest in government hospitals, at 25%, compared to faith-based hospitals, at 11%, and private hospitals, at 5%.
The researchers said these results suggest blood services should monitor malaria transmission surveillance reports and revise or project blood collection targets to meet the anticipated demand. ![]()
PHILADELPHIA—The demand for blood transfusions increases substantially during high malaria transmission season, according to a study of hospitals in Tanzania.
On average, blood demand increased about 24% from low transmission season to high transmission season.
And some hospitals could not meet the increased demand. Unmet demand was highest in government hospitals, followed by faith-based institutions and private facilities.
Bakary Drammeh, DrPH, of the Centers for Disease Control and Prevention in Atlanta, Georgia, and his colleagues presented these results in a poster (SP356) at the AABB Annual Meeting 2014.
The researchers analyzed 14,706 blood prescriptions at 42 Tanzanian hospitals—21 government, 9 private, and 12 faith-based institutions.
The team assessed the number of blood prescriptions according to high and low malaria transmission periods—June-July vs August-September.
On average, there were 130 monthly blood prescriptions written per 100 beds during high malaria transmission season and 107 written during low transmission season.
There were 189 and 153 units of blood or blood components requested per 100 beds during high and low seasons, respectively. And there were 159 and 127 units issued, respectively.
Ultimately, an average of 145 units were transfused per 100 beds during high malaria transmission season, and 122 were transfused during low transmission season.
Across all 42 hospitals, total blood prescriptions increased 29% from low malaria transmission season to high transmission season.
The number of units requested increased 26%, the number of units issued increased 34%, and the number of units transfused increased 28%.
So, on average, blood demand increased 23.5% at these 42 hospitals during high malaria transmission season. And some hospitals did not have enough blood to meet demand.
The unmet blood demand was highest in government hospitals, at 25%, compared to faith-based hospitals, at 11%, and private hospitals, at 5%.
The researchers said these results suggest blood services should monitor malaria transmission surveillance reports and revise or project blood collection targets to meet the anticipated demand. ![]()
PHILADELPHIA—The demand for blood transfusions increases substantially during high malaria transmission season, according to a study of hospitals in Tanzania.
On average, blood demand increased about 24% from low transmission season to high transmission season.
And some hospitals could not meet the increased demand. Unmet demand was highest in government hospitals, followed by faith-based institutions and private facilities.
Bakary Drammeh, DrPH, of the Centers for Disease Control and Prevention in Atlanta, Georgia, and his colleagues presented these results in a poster (SP356) at the AABB Annual Meeting 2014.
The researchers analyzed 14,706 blood prescriptions at 42 Tanzanian hospitals—21 government, 9 private, and 12 faith-based institutions.
The team assessed the number of blood prescriptions according to high and low malaria transmission periods—June-July vs August-September.
On average, there were 130 monthly blood prescriptions written per 100 beds during high malaria transmission season and 107 written during low transmission season.
There were 189 and 153 units of blood or blood components requested per 100 beds during high and low seasons, respectively. And there were 159 and 127 units issued, respectively.
Ultimately, an average of 145 units were transfused per 100 beds during high malaria transmission season, and 122 were transfused during low transmission season.
Across all 42 hospitals, total blood prescriptions increased 29% from low malaria transmission season to high transmission season.
The number of units requested increased 26%, the number of units issued increased 34%, and the number of units transfused increased 28%.
So, on average, blood demand increased 23.5% at these 42 hospitals during high malaria transmission season. And some hospitals did not have enough blood to meet demand.
The unmet blood demand was highest in government hospitals, at 25%, compared to faith-based hospitals, at 11%, and private hospitals, at 5%.
The researchers said these results suggest blood services should monitor malaria transmission surveillance reports and revise or project blood collection targets to meet the anticipated demand. ![]()
Study reveals gap in patient blood management
PHILADELPHIA—Healthcare professionals may not be using blood management interventions in a majority of patients receiving red blood cell (RBC) transfusions, a large study suggests.
The research showed that 72 US hospitals have made strides in reducing the use of RBCs in patients undergoing orthopedic and cardiac surgery.
And smaller reductions have occurred in patients with gastrointestinal bleeding, obstetric patients, and those receiving bone marrow transplants or inpatient chemotherapy.
However, more than 60% of the transfusions studied were given to patients who did not belong to any of the aforementioned groups.
“So when we target our [patient blood management] interventions to these kind of surgical procedures, in fact, we’re looking at only about 40% of the red cell use, and 60% goes to a myriad of other patients,” said Robert L. Thurer, MD, of Haemonetics in Braintree, Massachusetts.
He added that the groups of specific patient populations within that 60% were so small—“2% of patients here and 3% of patients there”—that it was too difficult to examine them individually in this study.
Dr Thurer presented this research at the AABB Annual Meeting 2014 (abstract S65-030K).
He and his colleagues wanted to determine which specific groups of patients have been most affected by patient blood management, understand further opportunities for decreasing transfusion use, and project future blood needs.
So the researchers analyzed data from 3,946,428 inpatients at 72 US hospitals, comparing the use of RBC transfusions in 2009/2010 to use in 2013.
In 2009/2010, there were 1,378,581 patients admitted to the hospitals, the RBC transfusion rate was 11.5.%, and the utilization (total units/total patients) was 0.41. In 2013, there were 861,804 patients, the transfusion rate was 10%, and the utilization was 0.34.
So from 2009/2010 to 2013, there was a 13% reduction in transfusion rate and a 17% reduction in utilization.
The greatest decrease was in orthopedic surgery patients. In those undergoing hip and knee joint replacement surgery, there was a 45% reduction in transfusion rate and a 43% reduction in utilization. In patients with a hip fracture, there was a 20% decrease in transfusion rate and a 20% decrease in utilization.
There was a smaller, though still sizable, reduction in transfusion use among patients undergoing cardiac surgery—a 15% decrease in transfusion rate and an 18% decrease in utilization.
“My personal thoughts about this is that it represents, certainly, lower transfusion triggers, which are becoming more widely adopted, [and] the use of antifibrinolytic drugs, particularly in orthopedic surgeries,” Dr Thurer said.
“We like to think that comprehensive coagulation testing and better matching of coagulation abnormalities contributes to this. Perhaps correction of preoperative anemia [contributes] for elective patients. And, clearly, surgical techniques have evolved, and, as they do, blood loss goes down.”
Reductions in RBC use were also seen in patients with gastrointestinal bleeding, where there was a 3% decrease in transfusion rate and a 13% decrease in utilization.
“For gastrointestinal bleeding, I think the lower transfusion triggers [have made an impact], but there’s also . . . more interest in timely interventions to stop bleeding,” Dr Thurer said.
“So rather than the gastroenterologist saying, ‘Correct the hematocrit and the coagulation factors, and I’ll stop the bleeding in the morning,’ we’re seeing now much more interest in very prompt endoscopy to stop bleeding. And as you know, the way to stop giving transfusions is to stop the patient from bleeding.”
Obstetric patients saw a 5% reduction in transfusion rate and an 8% reduction in utilization. And patients undergoing bone marrow transplant or inpatient chemotherapy saw a 6% decrease in transfusion rate and an 8% decrease in utilization.
Other transplant patients actually saw an increase in RBC transfusions. In liver transplant recipients, there was a 2.2% increase in transfusion rate and a 6% increase in utilization. And in kidney transplant recipients, there was a 0.2% increase in transfusion rate and a 19% increase in utilization.
However, Dr Thurer noted that the majority of RBC transfusions are administered to patients outside of these groups. In 2013, 60.6% of transfusions went to patients who did not fit into any of the aforementioned categories.
“So clearly,” he concluded, “further studies are needed to determine whether these reductions that we’ve seen in some areas can be implemented in a wider variety of patients.” ![]()
PHILADELPHIA—Healthcare professionals may not be using blood management interventions in a majority of patients receiving red blood cell (RBC) transfusions, a large study suggests.
The research showed that 72 US hospitals have made strides in reducing the use of RBCs in patients undergoing orthopedic and cardiac surgery.
And smaller reductions have occurred in patients with gastrointestinal bleeding, obstetric patients, and those receiving bone marrow transplants or inpatient chemotherapy.
However, more than 60% of the transfusions studied were given to patients who did not belong to any of the aforementioned groups.
“So when we target our [patient blood management] interventions to these kind of surgical procedures, in fact, we’re looking at only about 40% of the red cell use, and 60% goes to a myriad of other patients,” said Robert L. Thurer, MD, of Haemonetics in Braintree, Massachusetts.
He added that the groups of specific patient populations within that 60% were so small—“2% of patients here and 3% of patients there”—that it was too difficult to examine them individually in this study.
Dr Thurer presented this research at the AABB Annual Meeting 2014 (abstract S65-030K).
He and his colleagues wanted to determine which specific groups of patients have been most affected by patient blood management, understand further opportunities for decreasing transfusion use, and project future blood needs.
So the researchers analyzed data from 3,946,428 inpatients at 72 US hospitals, comparing the use of RBC transfusions in 2009/2010 to use in 2013.
In 2009/2010, there were 1,378,581 patients admitted to the hospitals, the RBC transfusion rate was 11.5.%, and the utilization (total units/total patients) was 0.41. In 2013, there were 861,804 patients, the transfusion rate was 10%, and the utilization was 0.34.
So from 2009/2010 to 2013, there was a 13% reduction in transfusion rate and a 17% reduction in utilization.
The greatest decrease was in orthopedic surgery patients. In those undergoing hip and knee joint replacement surgery, there was a 45% reduction in transfusion rate and a 43% reduction in utilization. In patients with a hip fracture, there was a 20% decrease in transfusion rate and a 20% decrease in utilization.
There was a smaller, though still sizable, reduction in transfusion use among patients undergoing cardiac surgery—a 15% decrease in transfusion rate and an 18% decrease in utilization.
“My personal thoughts about this is that it represents, certainly, lower transfusion triggers, which are becoming more widely adopted, [and] the use of antifibrinolytic drugs, particularly in orthopedic surgeries,” Dr Thurer said.
“We like to think that comprehensive coagulation testing and better matching of coagulation abnormalities contributes to this. Perhaps correction of preoperative anemia [contributes] for elective patients. And, clearly, surgical techniques have evolved, and, as they do, blood loss goes down.”
Reductions in RBC use were also seen in patients with gastrointestinal bleeding, where there was a 3% decrease in transfusion rate and a 13% decrease in utilization.
“For gastrointestinal bleeding, I think the lower transfusion triggers [have made an impact], but there’s also . . . more interest in timely interventions to stop bleeding,” Dr Thurer said.
“So rather than the gastroenterologist saying, ‘Correct the hematocrit and the coagulation factors, and I’ll stop the bleeding in the morning,’ we’re seeing now much more interest in very prompt endoscopy to stop bleeding. And as you know, the way to stop giving transfusions is to stop the patient from bleeding.”
Obstetric patients saw a 5% reduction in transfusion rate and an 8% reduction in utilization. And patients undergoing bone marrow transplant or inpatient chemotherapy saw a 6% decrease in transfusion rate and an 8% decrease in utilization.
Other transplant patients actually saw an increase in RBC transfusions. In liver transplant recipients, there was a 2.2% increase in transfusion rate and a 6% increase in utilization. And in kidney transplant recipients, there was a 0.2% increase in transfusion rate and a 19% increase in utilization.
However, Dr Thurer noted that the majority of RBC transfusions are administered to patients outside of these groups. In 2013, 60.6% of transfusions went to patients who did not fit into any of the aforementioned categories.
“So clearly,” he concluded, “further studies are needed to determine whether these reductions that we’ve seen in some areas can be implemented in a wider variety of patients.” ![]()
PHILADELPHIA—Healthcare professionals may not be using blood management interventions in a majority of patients receiving red blood cell (RBC) transfusions, a large study suggests.
The research showed that 72 US hospitals have made strides in reducing the use of RBCs in patients undergoing orthopedic and cardiac surgery.
And smaller reductions have occurred in patients with gastrointestinal bleeding, obstetric patients, and those receiving bone marrow transplants or inpatient chemotherapy.
However, more than 60% of the transfusions studied were given to patients who did not belong to any of the aforementioned groups.
“So when we target our [patient blood management] interventions to these kind of surgical procedures, in fact, we’re looking at only about 40% of the red cell use, and 60% goes to a myriad of other patients,” said Robert L. Thurer, MD, of Haemonetics in Braintree, Massachusetts.
He added that the groups of specific patient populations within that 60% were so small—“2% of patients here and 3% of patients there”—that it was too difficult to examine them individually in this study.
Dr Thurer presented this research at the AABB Annual Meeting 2014 (abstract S65-030K).
He and his colleagues wanted to determine which specific groups of patients have been most affected by patient blood management, understand further opportunities for decreasing transfusion use, and project future blood needs.
So the researchers analyzed data from 3,946,428 inpatients at 72 US hospitals, comparing the use of RBC transfusions in 2009/2010 to use in 2013.
In 2009/2010, there were 1,378,581 patients admitted to the hospitals, the RBC transfusion rate was 11.5.%, and the utilization (total units/total patients) was 0.41. In 2013, there were 861,804 patients, the transfusion rate was 10%, and the utilization was 0.34.
So from 2009/2010 to 2013, there was a 13% reduction in transfusion rate and a 17% reduction in utilization.
The greatest decrease was in orthopedic surgery patients. In those undergoing hip and knee joint replacement surgery, there was a 45% reduction in transfusion rate and a 43% reduction in utilization. In patients with a hip fracture, there was a 20% decrease in transfusion rate and a 20% decrease in utilization.
There was a smaller, though still sizable, reduction in transfusion use among patients undergoing cardiac surgery—a 15% decrease in transfusion rate and an 18% decrease in utilization.
“My personal thoughts about this is that it represents, certainly, lower transfusion triggers, which are becoming more widely adopted, [and] the use of antifibrinolytic drugs, particularly in orthopedic surgeries,” Dr Thurer said.
“We like to think that comprehensive coagulation testing and better matching of coagulation abnormalities contributes to this. Perhaps correction of preoperative anemia [contributes] for elective patients. And, clearly, surgical techniques have evolved, and, as they do, blood loss goes down.”
Reductions in RBC use were also seen in patients with gastrointestinal bleeding, where there was a 3% decrease in transfusion rate and a 13% decrease in utilization.
“For gastrointestinal bleeding, I think the lower transfusion triggers [have made an impact], but there’s also . . . more interest in timely interventions to stop bleeding,” Dr Thurer said.
“So rather than the gastroenterologist saying, ‘Correct the hematocrit and the coagulation factors, and I’ll stop the bleeding in the morning,’ we’re seeing now much more interest in very prompt endoscopy to stop bleeding. And as you know, the way to stop giving transfusions is to stop the patient from bleeding.”
Obstetric patients saw a 5% reduction in transfusion rate and an 8% reduction in utilization. And patients undergoing bone marrow transplant or inpatient chemotherapy saw a 6% decrease in transfusion rate and an 8% decrease in utilization.
Other transplant patients actually saw an increase in RBC transfusions. In liver transplant recipients, there was a 2.2% increase in transfusion rate and a 6% increase in utilization. And in kidney transplant recipients, there was a 0.2% increase in transfusion rate and a 19% increase in utilization.
However, Dr Thurer noted that the majority of RBC transfusions are administered to patients outside of these groups. In 2013, 60.6% of transfusions went to patients who did not fit into any of the aforementioned categories.
“So clearly,” he concluded, “further studies are needed to determine whether these reductions that we’ve seen in some areas can be implemented in a wider variety of patients.” ![]()
Results support transfusing with caution in TTP, HIT
PHILADELPHIA—Results of a large study support the recommendation that patients with platelet consumptive disorders only receive platelet transfusions if they exhibit severe or life-threatening bleeding that is refractory to other therapies.
The research indicated that platelet transfusions may increase the risk of arterial thrombosis and mortality among hospitalized patients with thrombotic thrombocytopenic purpura (TTP) and those with heparin-induced thrombocytopenia (HIT).
Platelet transfusions were also associated with a greater risk of acute myocardial infarction in TTP patients.
However, transfused patients with immune thrombocytopenia (ITP) did not have an increased risk of such complications.
The study did not establish a causal link between transfusions and complications, as it was retrospective and the researchers did not know the exact timing of events.
However, the complications and the transfusions did occur during the same hospital admission, noted Ruchika Goel, MD, of Johns Hopkins University in Baltimore, Maryland. She presented these findings at the AABB Annual Meeting 2014 (abstract S41-030G).
Dr Goel and her colleagues conducted this study to assess current platelet transfusion practices in the US in hospitalized patients with TTP, HIT, and ITP. The team wanted to explore any associations between transfusions and bleeding, venous and arterial thrombotic events, acute myocardial infarction, stroke, and in-hospital mortality in these patients.
“Currently, very little data are available on the risks and benefits associated with platelet transfusions in various platelet consumptive or disruptive disorders,” Dr Goel said. “Thus, evidence-based platelet transfusion guidelines in these disorders are either non-existent or they’re based on consensus statements, with not much supportive data.”
With this in mind, the researchers analyzed data from the Nationwide Inpatient Sample, a stratified probability sample of 20% of all discharges at community hospitals in the US, which covers more than 1100 hospitals across 47 states. The team looked at 5 years of data spanning the period from 2007 through 2011.
They included patients in whom TTP and ITP were the primary admitting diagnoses and patients in whom HIT was 1 of the top 3 diagnoses. Hospitalizations in which patients had a prior history of thrombosis were excluded, as were hospitalizations with any thrombosis/thromboembolism listed as the primary admitting diagnosis (implying that it was already present at admission).
So the analysis included 10,624 patients with TTP, 6332 with HIT, and 79,980 with ITP. The median ages were 47.4, 61.8, and 47.5, respectively. And platelet transfusions were given to 10.1%, 7.1%, and 25.8% of patients, respectively.
When the researchers adjusted their analysis for age and gender, they discovered a significantly increased risk of bleeding among all transfused patients. The odds ratios (ORs) were 2.3 for TTP, 5.5 for HIT, and 5.1 for ITP patients.
“The odds of platelet transfusion were significantly higher in patients who had bleeding, thus implying that . . . that was the indication for the transfusion—an actual bleeding complication,” Dr Goel said.
The results also showed that none of the transfused patients had a significantly increased risk of venous thrombosis or stroke. The ORs for venous thrombosis were 1.1 for TTP, 0.8 for HIT, and 1.3 for ITP patients. And the ORs for stroke were 1.6, 0.5, and 1.3, respectively.
However, both TTP patients and HIT patients had a significantly increased risk of arterial thrombosis. The ORs were 5.8 for TTP, 3.4 for HIT, and 0.3 for ITP patients.
TTP patients also had a significantly increased risk of acute myocardial infarction. The ORs were 2.0 for TTP, 1.9 for HIT, and 1.3 for ITP patients.
And patients with TTP and HIT had a significantly increased risk of in-hospital mortality. The ORs were 2.0 for TTP, 5.2 for HIT, and 1.1 for ITP patients.
Dr Goel noted that this study had several limitations. The temporality of events was not reported, there was no information on platelet thresholds for transfusion or disease severity and the effect on outcomes, and accuracy was limited by the precision of discharge coding.
Therefore, further studies are needed to assess whether platelet transfusions are directly responsible for complications or if they serve as a surrogate marker for the severity of illness.
“We propose that, until such studies or trials are indeed available, which are very hard [to conduct in] these rare disorders, platelets should continue to be considered relatively contraindicated and used only for severe or life-threatening bleeding which is refractory to other therapies,” Dr Goel concluded. ![]()
PHILADELPHIA—Results of a large study support the recommendation that patients with platelet consumptive disorders only receive platelet transfusions if they exhibit severe or life-threatening bleeding that is refractory to other therapies.
The research indicated that platelet transfusions may increase the risk of arterial thrombosis and mortality among hospitalized patients with thrombotic thrombocytopenic purpura (TTP) and those with heparin-induced thrombocytopenia (HIT).
Platelet transfusions were also associated with a greater risk of acute myocardial infarction in TTP patients.
However, transfused patients with immune thrombocytopenia (ITP) did not have an increased risk of such complications.
The study did not establish a causal link between transfusions and complications, as it was retrospective and the researchers did not know the exact timing of events.
However, the complications and the transfusions did occur during the same hospital admission, noted Ruchika Goel, MD, of Johns Hopkins University in Baltimore, Maryland. She presented these findings at the AABB Annual Meeting 2014 (abstract S41-030G).
Dr Goel and her colleagues conducted this study to assess current platelet transfusion practices in the US in hospitalized patients with TTP, HIT, and ITP. The team wanted to explore any associations between transfusions and bleeding, venous and arterial thrombotic events, acute myocardial infarction, stroke, and in-hospital mortality in these patients.
“Currently, very little data are available on the risks and benefits associated with platelet transfusions in various platelet consumptive or disruptive disorders,” Dr Goel said. “Thus, evidence-based platelet transfusion guidelines in these disorders are either non-existent or they’re based on consensus statements, with not much supportive data.”
With this in mind, the researchers analyzed data from the Nationwide Inpatient Sample, a stratified probability sample of 20% of all discharges at community hospitals in the US, which covers more than 1100 hospitals across 47 states. The team looked at 5 years of data spanning the period from 2007 through 2011.
They included patients in whom TTP and ITP were the primary admitting diagnoses and patients in whom HIT was 1 of the top 3 diagnoses. Hospitalizations in which patients had a prior history of thrombosis were excluded, as were hospitalizations with any thrombosis/thromboembolism listed as the primary admitting diagnosis (implying that it was already present at admission).
So the analysis included 10,624 patients with TTP, 6332 with HIT, and 79,980 with ITP. The median ages were 47.4, 61.8, and 47.5, respectively. And platelet transfusions were given to 10.1%, 7.1%, and 25.8% of patients, respectively.
When the researchers adjusted their analysis for age and gender, they discovered a significantly increased risk of bleeding among all transfused patients. The odds ratios (ORs) were 2.3 for TTP, 5.5 for HIT, and 5.1 for ITP patients.
“The odds of platelet transfusion were significantly higher in patients who had bleeding, thus implying that . . . that was the indication for the transfusion—an actual bleeding complication,” Dr Goel said.
The results also showed that none of the transfused patients had a significantly increased risk of venous thrombosis or stroke. The ORs for venous thrombosis were 1.1 for TTP, 0.8 for HIT, and 1.3 for ITP patients. And the ORs for stroke were 1.6, 0.5, and 1.3, respectively.
However, both TTP patients and HIT patients had a significantly increased risk of arterial thrombosis. The ORs were 5.8 for TTP, 3.4 for HIT, and 0.3 for ITP patients.
TTP patients also had a significantly increased risk of acute myocardial infarction. The ORs were 2.0 for TTP, 1.9 for HIT, and 1.3 for ITP patients.
And patients with TTP and HIT had a significantly increased risk of in-hospital mortality. The ORs were 2.0 for TTP, 5.2 for HIT, and 1.1 for ITP patients.
Dr Goel noted that this study had several limitations. The temporality of events was not reported, there was no information on platelet thresholds for transfusion or disease severity and the effect on outcomes, and accuracy was limited by the precision of discharge coding.
Therefore, further studies are needed to assess whether platelet transfusions are directly responsible for complications or if they serve as a surrogate marker for the severity of illness.
“We propose that, until such studies or trials are indeed available, which are very hard [to conduct in] these rare disorders, platelets should continue to be considered relatively contraindicated and used only for severe or life-threatening bleeding which is refractory to other therapies,” Dr Goel concluded. ![]()
PHILADELPHIA—Results of a large study support the recommendation that patients with platelet consumptive disorders only receive platelet transfusions if they exhibit severe or life-threatening bleeding that is refractory to other therapies.
The research indicated that platelet transfusions may increase the risk of arterial thrombosis and mortality among hospitalized patients with thrombotic thrombocytopenic purpura (TTP) and those with heparin-induced thrombocytopenia (HIT).
Platelet transfusions were also associated with a greater risk of acute myocardial infarction in TTP patients.
However, transfused patients with immune thrombocytopenia (ITP) did not have an increased risk of such complications.
The study did not establish a causal link between transfusions and complications, as it was retrospective and the researchers did not know the exact timing of events.
However, the complications and the transfusions did occur during the same hospital admission, noted Ruchika Goel, MD, of Johns Hopkins University in Baltimore, Maryland. She presented these findings at the AABB Annual Meeting 2014 (abstract S41-030G).
Dr Goel and her colleagues conducted this study to assess current platelet transfusion practices in the US in hospitalized patients with TTP, HIT, and ITP. The team wanted to explore any associations between transfusions and bleeding, venous and arterial thrombotic events, acute myocardial infarction, stroke, and in-hospital mortality in these patients.
“Currently, very little data are available on the risks and benefits associated with platelet transfusions in various platelet consumptive or disruptive disorders,” Dr Goel said. “Thus, evidence-based platelet transfusion guidelines in these disorders are either non-existent or they’re based on consensus statements, with not much supportive data.”
With this in mind, the researchers analyzed data from the Nationwide Inpatient Sample, a stratified probability sample of 20% of all discharges at community hospitals in the US, which covers more than 1100 hospitals across 47 states. The team looked at 5 years of data spanning the period from 2007 through 2011.
They included patients in whom TTP and ITP were the primary admitting diagnoses and patients in whom HIT was 1 of the top 3 diagnoses. Hospitalizations in which patients had a prior history of thrombosis were excluded, as were hospitalizations with any thrombosis/thromboembolism listed as the primary admitting diagnosis (implying that it was already present at admission).
So the analysis included 10,624 patients with TTP, 6332 with HIT, and 79,980 with ITP. The median ages were 47.4, 61.8, and 47.5, respectively. And platelet transfusions were given to 10.1%, 7.1%, and 25.8% of patients, respectively.
When the researchers adjusted their analysis for age and gender, they discovered a significantly increased risk of bleeding among all transfused patients. The odds ratios (ORs) were 2.3 for TTP, 5.5 for HIT, and 5.1 for ITP patients.
“The odds of platelet transfusion were significantly higher in patients who had bleeding, thus implying that . . . that was the indication for the transfusion—an actual bleeding complication,” Dr Goel said.
The results also showed that none of the transfused patients had a significantly increased risk of venous thrombosis or stroke. The ORs for venous thrombosis were 1.1 for TTP, 0.8 for HIT, and 1.3 for ITP patients. And the ORs for stroke were 1.6, 0.5, and 1.3, respectively.
However, both TTP patients and HIT patients had a significantly increased risk of arterial thrombosis. The ORs were 5.8 for TTP, 3.4 for HIT, and 0.3 for ITP patients.
TTP patients also had a significantly increased risk of acute myocardial infarction. The ORs were 2.0 for TTP, 1.9 for HIT, and 1.3 for ITP patients.
And patients with TTP and HIT had a significantly increased risk of in-hospital mortality. The ORs were 2.0 for TTP, 5.2 for HIT, and 1.1 for ITP patients.
Dr Goel noted that this study had several limitations. The temporality of events was not reported, there was no information on platelet thresholds for transfusion or disease severity and the effect on outcomes, and accuracy was limited by the precision of discharge coding.
Therefore, further studies are needed to assess whether platelet transfusions are directly responsible for complications or if they serve as a surrogate marker for the severity of illness.
“We propose that, until such studies or trials are indeed available, which are very hard [to conduct in] these rare disorders, platelets should continue to be considered relatively contraindicated and used only for severe or life-threatening bleeding which is refractory to other therapies,” Dr Goel concluded. ![]()
Transfusions benefit adults with sickle cell disease
PHILADELPHIA—Blood transfusions can provide pain relief in adults with sickle cell disease (SCD) who have failed treatment with hydroxyurea, a pilot study suggests.
Patients had fewer visits to the emergency department (ED) and fewer hospital admissions for pain control after they received chronic transfusions for pain prophylaxis than they did prior to receiving transfusions.
Matthew S. Karafin, MD, of the Blood Center of Wisconsin in Milwaukee, presented these results at the AABB Annual Meeting 2014 (abstract S42-030G).
“Pain in adults with sickle cell disease is probably one of the most important things that we deal with in our clinics,” he began. “It is the leading cause of morbidity in this population.”
Dr Karafin also noted that adults with SCD seem to experience pain differently from children, reporting more of a constant pain, as opposed to the episodic pain observed in kids. And although previous studies have suggested that transfusions do provide pain relief in SCD, most of those studies have focused on children.
So Dr Karafin and his colleagues set out to determine the impact of prophylactic transfusions on the rate of serious pain episodes in adults with SCD. The team retrospectively analyzed a cohort of patients who received chronic transfusions at 3- to 8-week intervals from January 2009 to October 2013.
The researchers defined chronic transfusions as receiving blood—either simple transfusions or red cell exchanges—in an outpatient setting 3 days a week with the goal of controlling hemoglobin (Hb) S percentage, maintaining it at less than 30%.
Patients had to have at least 1 ED or hospital visit for severe pain per month prior to starting transfusions, they were required to have failed hydroxyurea therapy, and they had to have at least 3 months both on and off chronic transfusions. The patients could have no other reason for receiving chronic transfusions (ie, no previous stroke).
So the study included 17 patients, 12 of whom were female. Fifteen (88.1%) had Hb SS disease, and 2 had Hb SC disease. Their median age was 26 (range, 20-54).
“We were able to record 541 total ED admissions over the study period and 404 total hospital admissions,” Dr Karafin said. “The median study evaluation period pre-transfusion was about 3.5 years, and we were able to study [patients for] a median of more than a year for the post-transfusion protocol period.”
Dr Karafin also noted that most of the patients were not transfusion-naïve, but they received significantly more units after being placed on the transfusion protocol.
The median number of red cell units received per 100 days was 1.2 (range, 0-7.2) pre-transfusion and 10.2 (range, 6.7-24.3) post-transfusion (P=0.0003). Nine of the patients received simple transfusions, and 8 received red cell exchanges.
There was a significant difference in the median Hb S pre- and post-transfusion—79% (range, 26.5%-89.6%) and 30.2% (range, 10.9%-57.4%), respectively (P=0.0003).
But there was no significant difference in median ferritin levels—1128.2 ng/mL (range, 65.4-11,130) and 2632.8 ng/mL (range, 16.7-8023.6), respectively (P=0.18). Dr Karafin said this could be explained by the fact that patients were not transfusion-naïve prior to starting the protocol.
Similarly, the median new alloantibody rate per 100 units was 0 both pre- and post-transfusion. This may be due to the fact that all patients received C-, E-, and KEL-matched blood, as well as the freshest available units, Dr Karafin said.
He and his colleagues also found that the median ED admission rate was significantly lower post-transfusion compared to pre-transfusion—0.79 (range, 0-6.6) and 2 (range, 0.4-11) visits every 100 days, respectively (P=0.04).
Thirteen patients (76.5%) had a reduced ED visit rate after chronic transfusion, and there was a 60.5% reduction in the ED visit rate overall.
Likewise, the median hospital admission rate decreased from 1.7 per 100 days (range, 0.05-5.8) pre-transfusion to 1.3 per 100 days (range, 0.2-3.2) post-transfusion (P=0.004).
Fifteen patients (88.2%) had reduced hospital admissions after chronic transfusion, and there was a 20.3% reduction in hospital admissions overall.
Dr Karafin noted that this study had a number of limitations, including a small number of patients, its retrospective nature, and the fact that it was conducted at a comprehensive SCD clinic.
“However, limitations aside, we found significant evidence to support that the findings observed in children seem to be similar in the adult population,” he said.
Namely, chronic transfusions can prevent serious pain episodes in adults with SCD who have failed treatment with hydroxyurea. ![]()
PHILADELPHIA—Blood transfusions can provide pain relief in adults with sickle cell disease (SCD) who have failed treatment with hydroxyurea, a pilot study suggests.
Patients had fewer visits to the emergency department (ED) and fewer hospital admissions for pain control after they received chronic transfusions for pain prophylaxis than they did prior to receiving transfusions.
Matthew S. Karafin, MD, of the Blood Center of Wisconsin in Milwaukee, presented these results at the AABB Annual Meeting 2014 (abstract S42-030G).
“Pain in adults with sickle cell disease is probably one of the most important things that we deal with in our clinics,” he began. “It is the leading cause of morbidity in this population.”
Dr Karafin also noted that adults with SCD seem to experience pain differently from children, reporting more of a constant pain, as opposed to the episodic pain observed in kids. And although previous studies have suggested that transfusions do provide pain relief in SCD, most of those studies have focused on children.
So Dr Karafin and his colleagues set out to determine the impact of prophylactic transfusions on the rate of serious pain episodes in adults with SCD. The team retrospectively analyzed a cohort of patients who received chronic transfusions at 3- to 8-week intervals from January 2009 to October 2013.
The researchers defined chronic transfusions as receiving blood—either simple transfusions or red cell exchanges—in an outpatient setting 3 days a week with the goal of controlling hemoglobin (Hb) S percentage, maintaining it at less than 30%.
Patients had to have at least 1 ED or hospital visit for severe pain per month prior to starting transfusions, they were required to have failed hydroxyurea therapy, and they had to have at least 3 months both on and off chronic transfusions. The patients could have no other reason for receiving chronic transfusions (ie, no previous stroke).
So the study included 17 patients, 12 of whom were female. Fifteen (88.1%) had Hb SS disease, and 2 had Hb SC disease. Their median age was 26 (range, 20-54).
“We were able to record 541 total ED admissions over the study period and 404 total hospital admissions,” Dr Karafin said. “The median study evaluation period pre-transfusion was about 3.5 years, and we were able to study [patients for] a median of more than a year for the post-transfusion protocol period.”
Dr Karafin also noted that most of the patients were not transfusion-naïve, but they received significantly more units after being placed on the transfusion protocol.
The median number of red cell units received per 100 days was 1.2 (range, 0-7.2) pre-transfusion and 10.2 (range, 6.7-24.3) post-transfusion (P=0.0003). Nine of the patients received simple transfusions, and 8 received red cell exchanges.
There was a significant difference in the median Hb S pre- and post-transfusion—79% (range, 26.5%-89.6%) and 30.2% (range, 10.9%-57.4%), respectively (P=0.0003).
But there was no significant difference in median ferritin levels—1128.2 ng/mL (range, 65.4-11,130) and 2632.8 ng/mL (range, 16.7-8023.6), respectively (P=0.18). Dr Karafin said this could be explained by the fact that patients were not transfusion-naïve prior to starting the protocol.
Similarly, the median new alloantibody rate per 100 units was 0 both pre- and post-transfusion. This may be due to the fact that all patients received C-, E-, and KEL-matched blood, as well as the freshest available units, Dr Karafin said.
He and his colleagues also found that the median ED admission rate was significantly lower post-transfusion compared to pre-transfusion—0.79 (range, 0-6.6) and 2 (range, 0.4-11) visits every 100 days, respectively (P=0.04).
Thirteen patients (76.5%) had a reduced ED visit rate after chronic transfusion, and there was a 60.5% reduction in the ED visit rate overall.
Likewise, the median hospital admission rate decreased from 1.7 per 100 days (range, 0.05-5.8) pre-transfusion to 1.3 per 100 days (range, 0.2-3.2) post-transfusion (P=0.004).
Fifteen patients (88.2%) had reduced hospital admissions after chronic transfusion, and there was a 20.3% reduction in hospital admissions overall.
Dr Karafin noted that this study had a number of limitations, including a small number of patients, its retrospective nature, and the fact that it was conducted at a comprehensive SCD clinic.
“However, limitations aside, we found significant evidence to support that the findings observed in children seem to be similar in the adult population,” he said.
Namely, chronic transfusions can prevent serious pain episodes in adults with SCD who have failed treatment with hydroxyurea. ![]()
PHILADELPHIA—Blood transfusions can provide pain relief in adults with sickle cell disease (SCD) who have failed treatment with hydroxyurea, a pilot study suggests.
Patients had fewer visits to the emergency department (ED) and fewer hospital admissions for pain control after they received chronic transfusions for pain prophylaxis than they did prior to receiving transfusions.
Matthew S. Karafin, MD, of the Blood Center of Wisconsin in Milwaukee, presented these results at the AABB Annual Meeting 2014 (abstract S42-030G).
“Pain in adults with sickle cell disease is probably one of the most important things that we deal with in our clinics,” he began. “It is the leading cause of morbidity in this population.”
Dr Karafin also noted that adults with SCD seem to experience pain differently from children, reporting more of a constant pain, as opposed to the episodic pain observed in kids. And although previous studies have suggested that transfusions do provide pain relief in SCD, most of those studies have focused on children.
So Dr Karafin and his colleagues set out to determine the impact of prophylactic transfusions on the rate of serious pain episodes in adults with SCD. The team retrospectively analyzed a cohort of patients who received chronic transfusions at 3- to 8-week intervals from January 2009 to October 2013.
The researchers defined chronic transfusions as receiving blood—either simple transfusions or red cell exchanges—in an outpatient setting 3 days a week with the goal of controlling hemoglobin (Hb) S percentage, maintaining it at less than 30%.
Patients had to have at least 1 ED or hospital visit for severe pain per month prior to starting transfusions, they were required to have failed hydroxyurea therapy, and they had to have at least 3 months both on and off chronic transfusions. The patients could have no other reason for receiving chronic transfusions (ie, no previous stroke).
So the study included 17 patients, 12 of whom were female. Fifteen (88.1%) had Hb SS disease, and 2 had Hb SC disease. Their median age was 26 (range, 20-54).
“We were able to record 541 total ED admissions over the study period and 404 total hospital admissions,” Dr Karafin said. “The median study evaluation period pre-transfusion was about 3.5 years, and we were able to study [patients for] a median of more than a year for the post-transfusion protocol period.”
Dr Karafin also noted that most of the patients were not transfusion-naïve, but they received significantly more units after being placed on the transfusion protocol.
The median number of red cell units received per 100 days was 1.2 (range, 0-7.2) pre-transfusion and 10.2 (range, 6.7-24.3) post-transfusion (P=0.0003). Nine of the patients received simple transfusions, and 8 received red cell exchanges.
There was a significant difference in the median Hb S pre- and post-transfusion—79% (range, 26.5%-89.6%) and 30.2% (range, 10.9%-57.4%), respectively (P=0.0003).
But there was no significant difference in median ferritin levels—1128.2 ng/mL (range, 65.4-11,130) and 2632.8 ng/mL (range, 16.7-8023.6), respectively (P=0.18). Dr Karafin said this could be explained by the fact that patients were not transfusion-naïve prior to starting the protocol.
Similarly, the median new alloantibody rate per 100 units was 0 both pre- and post-transfusion. This may be due to the fact that all patients received C-, E-, and KEL-matched blood, as well as the freshest available units, Dr Karafin said.
He and his colleagues also found that the median ED admission rate was significantly lower post-transfusion compared to pre-transfusion—0.79 (range, 0-6.6) and 2 (range, 0.4-11) visits every 100 days, respectively (P=0.04).
Thirteen patients (76.5%) had a reduced ED visit rate after chronic transfusion, and there was a 60.5% reduction in the ED visit rate overall.
Likewise, the median hospital admission rate decreased from 1.7 per 100 days (range, 0.05-5.8) pre-transfusion to 1.3 per 100 days (range, 0.2-3.2) post-transfusion (P=0.004).
Fifteen patients (88.2%) had reduced hospital admissions after chronic transfusion, and there was a 20.3% reduction in hospital admissions overall.
Dr Karafin noted that this study had a number of limitations, including a small number of patients, its retrospective nature, and the fact that it was conducted at a comprehensive SCD clinic.
“However, limitations aside, we found significant evidence to support that the findings observed in children seem to be similar in the adult population,” he said.
Namely, chronic transfusions can prevent serious pain episodes in adults with SCD who have failed treatment with hydroxyurea. ![]()
RECESS suggests RBC age doesn’t affect outcomes

Credit: UAB Hospital
PHILADELPHIA—As the medical community continues to debate whether transfusing older blood has a negative outcome on patients, results of the RECESS trial add fuel to the fire.
The study showed no significant differences in clinical outcomes between cardiac surgery patients who received newer red blood cells (RBCs) and those who received older RBCs.
There were no differences in multi-organ dysfunction scores (MODS), mortality rates, or the incidence of serious adverse events.
Marie E. Stein, MD, of the University of Minnesota in Minneapolis, presented the results of RECESS at the AABB Annual Meeting 2014 (abstract P2-020A).
The findings contradict results from another recent study presented at the Canadian Cardiovascular Congress.
“There are many studies of the effects of red blood cell storage duration on clinical outcomes, most of which are observational and include only a few randomized trials to date,” Dr Stein noted. “When studying cardiac surgery patients, some studies have found significant adverse outcomes of subjects who are transfused with red cells stored for a longer duration compared to shorter duration, and other studies have not.”
“Based on this equipoise, the primary hypothesis for RECESS was that there would be an important difference between the effect of transfusing shorter-storage-age-duration red cells compared to transfusing longer-storage-age-duration red cells on clinical outcomes in cardiac surgery patients.”
Patient characteristics
Dr Stein and her colleagues enrolled 1481 patients who were 12 years of age and older, weighed 40 kg or more, were undergoing complex cardiac surgery, and were considered “highly likely” to be transfused. They had to have a TRUST score of 3 or greater if they were older than 18 years of age, but this was not required for children.
Patients were split into two groups: those set to receive RBCs stored for 10 days or fewer and those set to receive RBCs stored for 21 days or more. Patients were stratified by age (those 12 to 17 years vs patients 18 and older) and according to whether they were in the intensive care unit prior to surgery. They were balanced by site as well.
In all, there were 538 subjects evaluable for the newer RBC arm and 560 subjects evaluable for the older RBC arm. (Subjects were evaluable if they underwent surgery and received at least 1 RBC unit.) The median patient age was 73 and 72 years, respectively, and males made up 42% and 44% of the patients, respectively.
The same percentage of patients in each arm—96%—underwent cardiopulmonary bypass, and 23% of patients in each arm underwent coronary artery bypass grafting. Seventeen percent of patients in the newer RBC arm and 14% in the older RBC arm underwent valve surgery only.
“Red cells were leukoreduced, stored in additive solution, and provided according to storage duration arm assignment for all pre-op, post-op, and intra-operative transfusions through day 28, discharge, or death, whichever occurred first,” Dr Stein noted.
The number of RBC units did not differ significantly between the two arms (P=0.80), and there was a comparable number of highly transfused subjects in each arm (P=0.81).
Eighty-seven percent of patients in the newer RBC arm and 89% in the older RBC arm received all their RBC units as assigned (P=0.35).
Six percent and 8%, respectively, received 1 or more unit aged 11 to 20 days but none belonging to the opposite arm to which they were assigned. Five percent and 4%, respectively, received 1 or more RBC unit from the opposite arm to which they were assigned.
“There was a 20-day difference in the mean storage duration between the two arms: 8 vs 28 days,” Dr Stein pointed out.
Outcomes
The study’s primary outcome was the change in multi-organ dysfunction score (ΔMODS) at 7 days. The MODS system includes assessments of respiratory, renal, hepatic, cardiovascular, hematologic, and neurologic function.
“The MODS system was chosen as the primary endpoint because the data elements are objective and readily available,” Dr Stein said. “MODS also incorporates organ dysfunction and not just frank organ failure. It correlates with mortality, with length of stay, and does incorporate death. MODS has been validated in other studies and has been used in other transfusion trials, including TRICC.”
To calculate 7-day ΔMODS, the researchers identified the worst score for each organ system through day 7 after surgery, discharge, or death. The 7-day MODS was the sum of the worst score for each organ system, and the 7-day ΔMODS was the pre-surgery MODS subtracted from the 7-day MODS.
Secondary outcomes were the 28-day ΔMODS, 28-day mortality, and the incidence of serious adverse events.
There was no significant difference between the arms with regard to 7-day or 28-day ΔMODS.
For the 7-day ΔMODS, the mean was 8.5±3.6 in the newer RBC arm and 8.7±3.6 in the older RBC arm. The unadjusted difference and the difference adjusted for baseline MODS were both -0.02.
For the 28-day ΔMODS, the mean was 8.7±4.0 in the newer RBC arm and 9.1±4.2 in the older RBC arm. The unadjusted difference and the difference adjusted for baseline MODS were both -0.3.
There was no significant difference between the arms in time to death (P=0.50), 7-day mortality (P=0.43), or 28-day mortality (P=0.57). The rate of 7-day mortality was 2.8% in the newer RBC arm and 2.0% in the older RBC arm. The 28-day mortality was 4.4% and 5.3%, respectively.
There was no significant difference in the percentage of subjects with 1 or more serious adverse events. The rate was 53% in the newer RBC arm and 51% in the older RBC arm (P=0.72).
Taking these results together, Dr Stein concluded that differences in the storage duration of RBCs did not translate to significant differences in “key clinical outcomes.” ![]()

Credit: UAB Hospital
PHILADELPHIA—As the medical community continues to debate whether transfusing older blood has a negative outcome on patients, results of the RECESS trial add fuel to the fire.
The study showed no significant differences in clinical outcomes between cardiac surgery patients who received newer red blood cells (RBCs) and those who received older RBCs.
There were no differences in multi-organ dysfunction scores (MODS), mortality rates, or the incidence of serious adverse events.
Marie E. Stein, MD, of the University of Minnesota in Minneapolis, presented the results of RECESS at the AABB Annual Meeting 2014 (abstract P2-020A).
The findings contradict results from another recent study presented at the Canadian Cardiovascular Congress.
“There are many studies of the effects of red blood cell storage duration on clinical outcomes, most of which are observational and include only a few randomized trials to date,” Dr Stein noted. “When studying cardiac surgery patients, some studies have found significant adverse outcomes of subjects who are transfused with red cells stored for a longer duration compared to shorter duration, and other studies have not.”
“Based on this equipoise, the primary hypothesis for RECESS was that there would be an important difference between the effect of transfusing shorter-storage-age-duration red cells compared to transfusing longer-storage-age-duration red cells on clinical outcomes in cardiac surgery patients.”
Patient characteristics
Dr Stein and her colleagues enrolled 1481 patients who were 12 years of age and older, weighed 40 kg or more, were undergoing complex cardiac surgery, and were considered “highly likely” to be transfused. They had to have a TRUST score of 3 or greater if they were older than 18 years of age, but this was not required for children.
Patients were split into two groups: those set to receive RBCs stored for 10 days or fewer and those set to receive RBCs stored for 21 days or more. Patients were stratified by age (those 12 to 17 years vs patients 18 and older) and according to whether they were in the intensive care unit prior to surgery. They were balanced by site as well.
In all, there were 538 subjects evaluable for the newer RBC arm and 560 subjects evaluable for the older RBC arm. (Subjects were evaluable if they underwent surgery and received at least 1 RBC unit.) The median patient age was 73 and 72 years, respectively, and males made up 42% and 44% of the patients, respectively.
The same percentage of patients in each arm—96%—underwent cardiopulmonary bypass, and 23% of patients in each arm underwent coronary artery bypass grafting. Seventeen percent of patients in the newer RBC arm and 14% in the older RBC arm underwent valve surgery only.
“Red cells were leukoreduced, stored in additive solution, and provided according to storage duration arm assignment for all pre-op, post-op, and intra-operative transfusions through day 28, discharge, or death, whichever occurred first,” Dr Stein noted.
The number of RBC units did not differ significantly between the two arms (P=0.80), and there was a comparable number of highly transfused subjects in each arm (P=0.81).
Eighty-seven percent of patients in the newer RBC arm and 89% in the older RBC arm received all their RBC units as assigned (P=0.35).
Six percent and 8%, respectively, received 1 or more unit aged 11 to 20 days but none belonging to the opposite arm to which they were assigned. Five percent and 4%, respectively, received 1 or more RBC unit from the opposite arm to which they were assigned.
“There was a 20-day difference in the mean storage duration between the two arms: 8 vs 28 days,” Dr Stein pointed out.
Outcomes
The study’s primary outcome was the change in multi-organ dysfunction score (ΔMODS) at 7 days. The MODS system includes assessments of respiratory, renal, hepatic, cardiovascular, hematologic, and neurologic function.
“The MODS system was chosen as the primary endpoint because the data elements are objective and readily available,” Dr Stein said. “MODS also incorporates organ dysfunction and not just frank organ failure. It correlates with mortality, with length of stay, and does incorporate death. MODS has been validated in other studies and has been used in other transfusion trials, including TRICC.”
To calculate 7-day ΔMODS, the researchers identified the worst score for each organ system through day 7 after surgery, discharge, or death. The 7-day MODS was the sum of the worst score for each organ system, and the 7-day ΔMODS was the pre-surgery MODS subtracted from the 7-day MODS.
Secondary outcomes were the 28-day ΔMODS, 28-day mortality, and the incidence of serious adverse events.
There was no significant difference between the arms with regard to 7-day or 28-day ΔMODS.
For the 7-day ΔMODS, the mean was 8.5±3.6 in the newer RBC arm and 8.7±3.6 in the older RBC arm. The unadjusted difference and the difference adjusted for baseline MODS were both -0.02.
For the 28-day ΔMODS, the mean was 8.7±4.0 in the newer RBC arm and 9.1±4.2 in the older RBC arm. The unadjusted difference and the difference adjusted for baseline MODS were both -0.3.
There was no significant difference between the arms in time to death (P=0.50), 7-day mortality (P=0.43), or 28-day mortality (P=0.57). The rate of 7-day mortality was 2.8% in the newer RBC arm and 2.0% in the older RBC arm. The 28-day mortality was 4.4% and 5.3%, respectively.
There was no significant difference in the percentage of subjects with 1 or more serious adverse events. The rate was 53% in the newer RBC arm and 51% in the older RBC arm (P=0.72).
Taking these results together, Dr Stein concluded that differences in the storage duration of RBCs did not translate to significant differences in “key clinical outcomes.” ![]()

Credit: UAB Hospital
PHILADELPHIA—As the medical community continues to debate whether transfusing older blood has a negative outcome on patients, results of the RECESS trial add fuel to the fire.
The study showed no significant differences in clinical outcomes between cardiac surgery patients who received newer red blood cells (RBCs) and those who received older RBCs.
There were no differences in multi-organ dysfunction scores (MODS), mortality rates, or the incidence of serious adverse events.
Marie E. Stein, MD, of the University of Minnesota in Minneapolis, presented the results of RECESS at the AABB Annual Meeting 2014 (abstract P2-020A).
The findings contradict results from another recent study presented at the Canadian Cardiovascular Congress.
“There are many studies of the effects of red blood cell storage duration on clinical outcomes, most of which are observational and include only a few randomized trials to date,” Dr Stein noted. “When studying cardiac surgery patients, some studies have found significant adverse outcomes of subjects who are transfused with red cells stored for a longer duration compared to shorter duration, and other studies have not.”
“Based on this equipoise, the primary hypothesis for RECESS was that there would be an important difference between the effect of transfusing shorter-storage-age-duration red cells compared to transfusing longer-storage-age-duration red cells on clinical outcomes in cardiac surgery patients.”
Patient characteristics
Dr Stein and her colleagues enrolled 1481 patients who were 12 years of age and older, weighed 40 kg or more, were undergoing complex cardiac surgery, and were considered “highly likely” to be transfused. They had to have a TRUST score of 3 or greater if they were older than 18 years of age, but this was not required for children.
Patients were split into two groups: those set to receive RBCs stored for 10 days or fewer and those set to receive RBCs stored for 21 days or more. Patients were stratified by age (those 12 to 17 years vs patients 18 and older) and according to whether they were in the intensive care unit prior to surgery. They were balanced by site as well.
In all, there were 538 subjects evaluable for the newer RBC arm and 560 subjects evaluable for the older RBC arm. (Subjects were evaluable if they underwent surgery and received at least 1 RBC unit.) The median patient age was 73 and 72 years, respectively, and males made up 42% and 44% of the patients, respectively.
The same percentage of patients in each arm—96%—underwent cardiopulmonary bypass, and 23% of patients in each arm underwent coronary artery bypass grafting. Seventeen percent of patients in the newer RBC arm and 14% in the older RBC arm underwent valve surgery only.
“Red cells were leukoreduced, stored in additive solution, and provided according to storage duration arm assignment for all pre-op, post-op, and intra-operative transfusions through day 28, discharge, or death, whichever occurred first,” Dr Stein noted.
The number of RBC units did not differ significantly between the two arms (P=0.80), and there was a comparable number of highly transfused subjects in each arm (P=0.81).
Eighty-seven percent of patients in the newer RBC arm and 89% in the older RBC arm received all their RBC units as assigned (P=0.35).
Six percent and 8%, respectively, received 1 or more unit aged 11 to 20 days but none belonging to the opposite arm to which they were assigned. Five percent and 4%, respectively, received 1 or more RBC unit from the opposite arm to which they were assigned.
“There was a 20-day difference in the mean storage duration between the two arms: 8 vs 28 days,” Dr Stein pointed out.
Outcomes
The study’s primary outcome was the change in multi-organ dysfunction score (ΔMODS) at 7 days. The MODS system includes assessments of respiratory, renal, hepatic, cardiovascular, hematologic, and neurologic function.
“The MODS system was chosen as the primary endpoint because the data elements are objective and readily available,” Dr Stein said. “MODS also incorporates organ dysfunction and not just frank organ failure. It correlates with mortality, with length of stay, and does incorporate death. MODS has been validated in other studies and has been used in other transfusion trials, including TRICC.”
To calculate 7-day ΔMODS, the researchers identified the worst score for each organ system through day 7 after surgery, discharge, or death. The 7-day MODS was the sum of the worst score for each organ system, and the 7-day ΔMODS was the pre-surgery MODS subtracted from the 7-day MODS.
Secondary outcomes were the 28-day ΔMODS, 28-day mortality, and the incidence of serious adverse events.
There was no significant difference between the arms with regard to 7-day or 28-day ΔMODS.
For the 7-day ΔMODS, the mean was 8.5±3.6 in the newer RBC arm and 8.7±3.6 in the older RBC arm. The unadjusted difference and the difference adjusted for baseline MODS were both -0.02.
For the 28-day ΔMODS, the mean was 8.7±4.0 in the newer RBC arm and 9.1±4.2 in the older RBC arm. The unadjusted difference and the difference adjusted for baseline MODS were both -0.3.
There was no significant difference between the arms in time to death (P=0.50), 7-day mortality (P=0.43), or 28-day mortality (P=0.57). The rate of 7-day mortality was 2.8% in the newer RBC arm and 2.0% in the older RBC arm. The 28-day mortality was 4.4% and 5.3%, respectively.
There was no significant difference in the percentage of subjects with 1 or more serious adverse events. The rate was 53% in the newer RBC arm and 51% in the older RBC arm (P=0.72).
Taking these results together, Dr Stein concluded that differences in the storage duration of RBCs did not translate to significant differences in “key clinical outcomes.” ![]()
Study supports 2:1 ratio for transfusion in pregnancy
PHILADELPHIA—Results of a single-center study suggest that, when it comes to massive transfusion in pregnancy, a 1:1 ratio of red blood cells (RBCs) to plasma is not needed to maintain adequate hemostasis.
A 2:1 ratio produces prothrombin times (PTs), activated partial thromboplastin times (PTTs), and fibrinogen levels within references ranges.
Vanessa Plasencia, MLS (ASCP)CM, of Texas Children’s Hospital in Houston, presented these findings at the AABB Annual Meeting 2014 (abstract S43-030G).
She noted that hospital staff perform approximately 4500 to 5000 deliveries per year, and they define massive transfusion as 4 or more RBC units in 1 hour or 10 or more RBC units in 24 hours.
The hospital’s initial obstetric massive transfusion protocol was 4 units of RBCs and 4 units of plasma to be issued in a cooler. Four units of group AB thawed plasma or liquid plasma were always available.
To determine if this protocol is optimal, Plasencia and her colleagues conducted a retrospective review of patient records from April 2012 to June 2014. During this time, there were 28 cases of massive transfusion.
Two of these patients died and were excluded from the study. One, who had placental abruption, received 131 RBC units and 48 plasma units (ratio=2.7:1). The other, who had placenta percreta, received 90 RBC units and 52 plasma units (ratio=1.7:1).
The median age of the remaining 26 patients was 34 years (range, 24-44). Four of these patients had placenta accreta, 2 had placenta increta, 14 had placenta percreta, and 6 had other complications (such as placental abruption, diabetes, and risks due to advanced-age pregnancy).
A median of 12 RBC units (range, 9-20) and 9 plasma units (range, 5-19) were issued. And a median of 8 RBC units (range, 6-12) and 5 plasma units (range, 4-8) were actually transfused. That translates to RBC-to-plasma ratios of 1.4:1 (range, 1.0-2.0) and 1.7:1 (1.3-2.5), respectively.
So despite the hospital’s protocol of a 1:1 RBC-to-plasma ratio, the actual ratio of transfusion in practice was approximately 2:1, Plasencia noted. And the patients had PT, PTT, and fibrinogen values within reference ranges.
Coagulation data were collected after transfusions took place, once patients were stable. The median PT was 14.8 seconds (range, 14.1-15.2), the median PTT was 29.9 seconds (range, 27.6-33.3), and the median fibrinogen was 283 mg/dL (range, 225-325).
Because of these results, Texas Children’s Hospital decided to change its massive transfusion protocol for obstetrics to a 2:1 RBC-to-plasma ratio. Now, the hospital issues 4 units of RBCs and 2 units of plasma in its initial blood package.
PHILADELPHIA—Results of a single-center study suggest that, when it comes to massive transfusion in pregnancy, a 1:1 ratio of red blood cells (RBCs) to plasma is not needed to maintain adequate hemostasis.
A 2:1 ratio produces prothrombin times (PTs), activated partial thromboplastin times (PTTs), and fibrinogen levels within references ranges.
Vanessa Plasencia, MLS (ASCP)CM, of Texas Children’s Hospital in Houston, presented these findings at the AABB Annual Meeting 2014 (abstract S43-030G).
She noted that hospital staff perform approximately 4500 to 5000 deliveries per year, and they define massive transfusion as 4 or more RBC units in 1 hour or 10 or more RBC units in 24 hours.
The hospital’s initial obstetric massive transfusion protocol was 4 units of RBCs and 4 units of plasma to be issued in a cooler. Four units of group AB thawed plasma or liquid plasma were always available.
To determine if this protocol is optimal, Plasencia and her colleagues conducted a retrospective review of patient records from April 2012 to June 2014. During this time, there were 28 cases of massive transfusion.
Two of these patients died and were excluded from the study. One, who had placental abruption, received 131 RBC units and 48 plasma units (ratio=2.7:1). The other, who had placenta percreta, received 90 RBC units and 52 plasma units (ratio=1.7:1).
The median age of the remaining 26 patients was 34 years (range, 24-44). Four of these patients had placenta accreta, 2 had placenta increta, 14 had placenta percreta, and 6 had other complications (such as placental abruption, diabetes, and risks due to advanced-age pregnancy).
A median of 12 RBC units (range, 9-20) and 9 plasma units (range, 5-19) were issued. And a median of 8 RBC units (range, 6-12) and 5 plasma units (range, 4-8) were actually transfused. That translates to RBC-to-plasma ratios of 1.4:1 (range, 1.0-2.0) and 1.7:1 (1.3-2.5), respectively.
So despite the hospital’s protocol of a 1:1 RBC-to-plasma ratio, the actual ratio of transfusion in practice was approximately 2:1, Plasencia noted. And the patients had PT, PTT, and fibrinogen values within reference ranges.
Coagulation data were collected after transfusions took place, once patients were stable. The median PT was 14.8 seconds (range, 14.1-15.2), the median PTT was 29.9 seconds (range, 27.6-33.3), and the median fibrinogen was 283 mg/dL (range, 225-325).
Because of these results, Texas Children’s Hospital decided to change its massive transfusion protocol for obstetrics to a 2:1 RBC-to-plasma ratio. Now, the hospital issues 4 units of RBCs and 2 units of plasma in its initial blood package.
PHILADELPHIA—Results of a single-center study suggest that, when it comes to massive transfusion in pregnancy, a 1:1 ratio of red blood cells (RBCs) to plasma is not needed to maintain adequate hemostasis.
A 2:1 ratio produces prothrombin times (PTs), activated partial thromboplastin times (PTTs), and fibrinogen levels within references ranges.
Vanessa Plasencia, MLS (ASCP)CM, of Texas Children’s Hospital in Houston, presented these findings at the AABB Annual Meeting 2014 (abstract S43-030G).
She noted that hospital staff perform approximately 4500 to 5000 deliveries per year, and they define massive transfusion as 4 or more RBC units in 1 hour or 10 or more RBC units in 24 hours.
The hospital’s initial obstetric massive transfusion protocol was 4 units of RBCs and 4 units of plasma to be issued in a cooler. Four units of group AB thawed plasma or liquid plasma were always available.
To determine if this protocol is optimal, Plasencia and her colleagues conducted a retrospective review of patient records from April 2012 to June 2014. During this time, there were 28 cases of massive transfusion.
Two of these patients died and were excluded from the study. One, who had placental abruption, received 131 RBC units and 48 plasma units (ratio=2.7:1). The other, who had placenta percreta, received 90 RBC units and 52 plasma units (ratio=1.7:1).
The median age of the remaining 26 patients was 34 years (range, 24-44). Four of these patients had placenta accreta, 2 had placenta increta, 14 had placenta percreta, and 6 had other complications (such as placental abruption, diabetes, and risks due to advanced-age pregnancy).
A median of 12 RBC units (range, 9-20) and 9 plasma units (range, 5-19) were issued. And a median of 8 RBC units (range, 6-12) and 5 plasma units (range, 4-8) were actually transfused. That translates to RBC-to-plasma ratios of 1.4:1 (range, 1.0-2.0) and 1.7:1 (1.3-2.5), respectively.
So despite the hospital’s protocol of a 1:1 RBC-to-plasma ratio, the actual ratio of transfusion in practice was approximately 2:1, Plasencia noted. And the patients had PT, PTT, and fibrinogen values within reference ranges.
Coagulation data were collected after transfusions took place, once patients were stable. The median PT was 14.8 seconds (range, 14.1-15.2), the median PTT was 29.9 seconds (range, 27.6-33.3), and the median fibrinogen was 283 mg/dL (range, 225-325).
Because of these results, Texas Children’s Hospital decided to change its massive transfusion protocol for obstetrics to a 2:1 RBC-to-plasma ratio. Now, the hospital issues 4 units of RBCs and 2 units of plasma in its initial blood package.
Residents arrange transfusions despite poor knowledge
PHILADELPHIA—Internal medicine residents are obtaining transfusion consent from patients despite having poor knowledge of transfusion medicine, according to a study of nearly 500 residents in 9 countries.
On an exam assessing transfusion knowledge, the residents’ mean score was 45.7%.
And in a survey, an overwhelming majority of residents said they had “beginner” or “intermediate” transfusion knowledge.
Still, 89% said they had obtained patient consent for a transfusion.
Richard Haspel, MD, PhD, of Beth Israel Deacon Medical Center and Harvard Medical School in Boston, presented these data at the AABB Annual Meeting 2014 (abstract S45-030G).
“We all know there’s a problem with clinicians not knowing how to transfuse blood,” Dr Haspel began. “I would argue, though, that there are a lot of questions we don’t know the answer to. How prevalent is this problem? Are there some places that do it better than others? What areas need improvement?”
With these questions in mind, Dr Haspel and his colleagues used a 23-question survey and a 20-question exam (validated by the BEST Collaborative) to assess 474 internal medicine residents from 23 sites in 9 countries: Australia, Canada, England, Ireland, Italy, Germany, The Netherlands, Spain, and the US.
The mean score of correct responses in the exam was 45.7%. The mean score was significantly lower for first-year residents (43.9%) than for third- (47.1%; P=0.02) and fourth-year residents (50.6%, P=0.002).
However, as 50.6% was the highest mean score, exam scores were poor regardless of a resident’s time served, Dr Haspel noted. Scores were poor across the different study sites as well, ranging from about 32% to 55%.
The exam included questions on red cells, platelets, plasma, allergic reactions, transfusion-related acute lung injury (TRALI), and transfusion-associated circulatory overload (TACO), among other topics.
As an example, Dr Haspel pointed out that, for the 3 questions on TRALI, the percentage of correct responses did not exceed 15%. This was the topic about which residents seemed the least informed.
Dr Haspel noted that, in general, residents with more medical school hours spent learning about transfusion medicine and those with better perceived quality of their training tended to score higher on the exam. Still, there wasn’t much of a difference in exam scores between residents who said they had beginner, intermediate, or advanced knowledge of transfusion medicine.
Twelve percent of residents said they did not receive any transfusion medicine training in medical school, and 28% said they didn’t receive any training during their residency. About 35% said they received more than 2 hours of training in medical school, and 18% said they received more than 2 hours of training during their residency.
“In terms of the quality of the training, most rated it ‘slightly’ or ‘moderately’ effective,” Dr Haspel said. “In terms of attitudes and perceptions, most of them considered themselves a beginner [48%] or intermediate [48%] in regard to transfusion medicine knowledge.”
Ninety-seven percent of residents said they know how to contact the blood bank, and 72% said they know how to contact a transfusion medicine doctor. But 14% percent of residents did not know if their hospital had transfusion guidelines, and 1% wrongly said their hospital did not have guidelines.
Yet 89% of residents said they had obtained consent for a transfusion from a patient.
On the other hand, most residents (77%) said knowledge of transfusion medicine is “very” or “extremely” important in providing appropriate patient care. And 65% said they would find additional training “very” or “extremely” helpful. ![]()
PHILADELPHIA—Internal medicine residents are obtaining transfusion consent from patients despite having poor knowledge of transfusion medicine, according to a study of nearly 500 residents in 9 countries.
On an exam assessing transfusion knowledge, the residents’ mean score was 45.7%.
And in a survey, an overwhelming majority of residents said they had “beginner” or “intermediate” transfusion knowledge.
Still, 89% said they had obtained patient consent for a transfusion.
Richard Haspel, MD, PhD, of Beth Israel Deacon Medical Center and Harvard Medical School in Boston, presented these data at the AABB Annual Meeting 2014 (abstract S45-030G).
“We all know there’s a problem with clinicians not knowing how to transfuse blood,” Dr Haspel began. “I would argue, though, that there are a lot of questions we don’t know the answer to. How prevalent is this problem? Are there some places that do it better than others? What areas need improvement?”
With these questions in mind, Dr Haspel and his colleagues used a 23-question survey and a 20-question exam (validated by the BEST Collaborative) to assess 474 internal medicine residents from 23 sites in 9 countries: Australia, Canada, England, Ireland, Italy, Germany, The Netherlands, Spain, and the US.
The mean score of correct responses in the exam was 45.7%. The mean score was significantly lower for first-year residents (43.9%) than for third- (47.1%; P=0.02) and fourth-year residents (50.6%, P=0.002).
However, as 50.6% was the highest mean score, exam scores were poor regardless of a resident’s time served, Dr Haspel noted. Scores were poor across the different study sites as well, ranging from about 32% to 55%.
The exam included questions on red cells, platelets, plasma, allergic reactions, transfusion-related acute lung injury (TRALI), and transfusion-associated circulatory overload (TACO), among other topics.
As an example, Dr Haspel pointed out that, for the 3 questions on TRALI, the percentage of correct responses did not exceed 15%. This was the topic about which residents seemed the least informed.
Dr Haspel noted that, in general, residents with more medical school hours spent learning about transfusion medicine and those with better perceived quality of their training tended to score higher on the exam. Still, there wasn’t much of a difference in exam scores between residents who said they had beginner, intermediate, or advanced knowledge of transfusion medicine.
Twelve percent of residents said they did not receive any transfusion medicine training in medical school, and 28% said they didn’t receive any training during their residency. About 35% said they received more than 2 hours of training in medical school, and 18% said they received more than 2 hours of training during their residency.
“In terms of the quality of the training, most rated it ‘slightly’ or ‘moderately’ effective,” Dr Haspel said. “In terms of attitudes and perceptions, most of them considered themselves a beginner [48%] or intermediate [48%] in regard to transfusion medicine knowledge.”
Ninety-seven percent of residents said they know how to contact the blood bank, and 72% said they know how to contact a transfusion medicine doctor. But 14% percent of residents did not know if their hospital had transfusion guidelines, and 1% wrongly said their hospital did not have guidelines.
Yet 89% of residents said they had obtained consent for a transfusion from a patient.
On the other hand, most residents (77%) said knowledge of transfusion medicine is “very” or “extremely” important in providing appropriate patient care. And 65% said they would find additional training “very” or “extremely” helpful. ![]()
PHILADELPHIA—Internal medicine residents are obtaining transfusion consent from patients despite having poor knowledge of transfusion medicine, according to a study of nearly 500 residents in 9 countries.
On an exam assessing transfusion knowledge, the residents’ mean score was 45.7%.
And in a survey, an overwhelming majority of residents said they had “beginner” or “intermediate” transfusion knowledge.
Still, 89% said they had obtained patient consent for a transfusion.
Richard Haspel, MD, PhD, of Beth Israel Deacon Medical Center and Harvard Medical School in Boston, presented these data at the AABB Annual Meeting 2014 (abstract S45-030G).
“We all know there’s a problem with clinicians not knowing how to transfuse blood,” Dr Haspel began. “I would argue, though, that there are a lot of questions we don’t know the answer to. How prevalent is this problem? Are there some places that do it better than others? What areas need improvement?”
With these questions in mind, Dr Haspel and his colleagues used a 23-question survey and a 20-question exam (validated by the BEST Collaborative) to assess 474 internal medicine residents from 23 sites in 9 countries: Australia, Canada, England, Ireland, Italy, Germany, The Netherlands, Spain, and the US.
The mean score of correct responses in the exam was 45.7%. The mean score was significantly lower for first-year residents (43.9%) than for third- (47.1%; P=0.02) and fourth-year residents (50.6%, P=0.002).
However, as 50.6% was the highest mean score, exam scores were poor regardless of a resident’s time served, Dr Haspel noted. Scores were poor across the different study sites as well, ranging from about 32% to 55%.
The exam included questions on red cells, platelets, plasma, allergic reactions, transfusion-related acute lung injury (TRALI), and transfusion-associated circulatory overload (TACO), among other topics.
As an example, Dr Haspel pointed out that, for the 3 questions on TRALI, the percentage of correct responses did not exceed 15%. This was the topic about which residents seemed the least informed.
Dr Haspel noted that, in general, residents with more medical school hours spent learning about transfusion medicine and those with better perceived quality of their training tended to score higher on the exam. Still, there wasn’t much of a difference in exam scores between residents who said they had beginner, intermediate, or advanced knowledge of transfusion medicine.
Twelve percent of residents said they did not receive any transfusion medicine training in medical school, and 28% said they didn’t receive any training during their residency. About 35% said they received more than 2 hours of training in medical school, and 18% said they received more than 2 hours of training during their residency.
“In terms of the quality of the training, most rated it ‘slightly’ or ‘moderately’ effective,” Dr Haspel said. “In terms of attitudes and perceptions, most of them considered themselves a beginner [48%] or intermediate [48%] in regard to transfusion medicine knowledge.”
Ninety-seven percent of residents said they know how to contact the blood bank, and 72% said they know how to contact a transfusion medicine doctor. But 14% percent of residents did not know if their hospital had transfusion guidelines, and 1% wrongly said their hospital did not have guidelines.
Yet 89% of residents said they had obtained consent for a transfusion from a patient.
On the other hand, most residents (77%) said knowledge of transfusion medicine is “very” or “extremely” important in providing appropriate patient care. And 65% said they would find additional training “very” or “extremely” helpful. ![]()
Method can detect drivers of AML
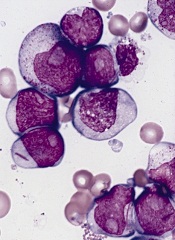
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.” ![]()
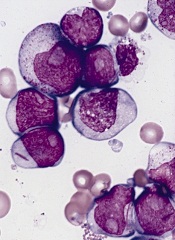
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.” ![]()
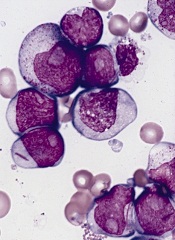
PHILADELPHIA—Super-enhancer profiling can unearth biomarkers and therapeutic targets for acute myeloid leukemia (AML), according to research presented at the AACR conference Hematologic Malignancies: Translating Discoveries to Novel Therapies.
Researchers used high-throughput ChIP sequencing to identify super-enhancer domains in a cohort of AML patients.
And this revealed both known and previously unknown genes that are important for AML disease biology.
Eric Olson, PhD, and his colleagues from Syros Pharmaceuticals in Watertown, Massachusetts, presented this research during one of the meeting’s poster sessions.
The investigators explained that super-enhancers are a class of densely clustered cis-regulatory elements that are key to initiating and maintaining cell-type-specific gene expression in cancer and other settings. Tumor cells acquire super-enhancers at key oncogenes and at genes that participate in the acquisition of hallmark capabilities in cancer.
So the researchers set out to identify and characterize super-enhancer domains in a cohort of AML patients.
The team collected primary AML samples and performed chromatin fragmentation, chromatin immunoprecipitation, and DNA purification and sequencing.
They then mapped enhancer regions and characterized enhancer profiles. This revealed AML-specific super-enhancers and associated genes.
For example, in one patient, the investigators identified 392 AML-specific super-enhancers, which were associated with 11 genes important for AML disease biology: HOXA7, LMO2, HLX, MYADM, ETV6, AFF1, RUNX1, GFI1, SPI1, MEIS1, and MYB.
In another patient, the team identified 279 AML-specific super-enhancers that were associated with 9 genes: MLLT10, AKT3, FLT3, ETV6, KLF13, RELA, FOSB, BMI1, and RUNX1.
The researchers said these findings suggest that super-enhancer profiling provides a new option for identifying biomarkers and therapeutic targets in AML and other malignancies.
“Syros’s gene control platform can systematically and efficiently identify known and previously unrecognized tumor biomarkers and cancer dependencies directly from patient tissue,” Dr Olson said. “Our data demonstrate unique gene control elements in AML patient subsets that hold promise in the classification and treatment of AML.” ![]()
Antibody gets orphan status for CTCL in Europe
The European Commission has granted orphan drug designation to IPH4102 for the treatment of cutaneous T-cell lymphoma (CTCL).
IPH4102 is a cytotoxic anti-KIR3DL2 monoclonal antibody (mAb) that targets CTCL cells.
Orphan status provides Innate Pharma, the company developing IPH4102, with benefits such as tax incentives, market exclusivity for 10 years, possibilities for additional research funding, and additional guidance from the European Medicines Agency during clinical development.
Preclinical results with IPH4102 were presented in a poster at the 2014 T-cell Lymphoma Forum. The research was conducted by investigators from Innate Pharma and INSERM at Hôpital Saint Louis in Paris.
The researchers generated 3 mAbs that bind selectively to KIR3DL2 and evaluated their efficacy against KIR3DL2-expressing tumors and Sézary cell lines.
IPH4102 was among the 3 mAbs and emerged as the most promising drug candidate.
Experiments revealed that anti-KIR3DL2 mAbs can kill KIR3DL2+ cell lines through allo-antibody-dependent cell cytotoxicity, even at low tumor antigen density.
The mAbs also improved survival in KIR3DL2+ xenograft models. Survival in mAb-treated mice ranged from 30.5 days to 54.5 days, compared to 19 days in controls.
Finally, the mAbs mediated killing of primary Sézary cells with autologous natural killer cells nearly as efficiently as alemtuzumab.
The investigators said these results suggest anti-KIR3DL2 mAbs are a feasible treatment option for CTCL patients. They plan to prove this hypothesis with a phase 1 trial of IPH4102, which is expected to begin in 2015. ![]()
The European Commission has granted orphan drug designation to IPH4102 for the treatment of cutaneous T-cell lymphoma (CTCL).
IPH4102 is a cytotoxic anti-KIR3DL2 monoclonal antibody (mAb) that targets CTCL cells.
Orphan status provides Innate Pharma, the company developing IPH4102, with benefits such as tax incentives, market exclusivity for 10 years, possibilities for additional research funding, and additional guidance from the European Medicines Agency during clinical development.
Preclinical results with IPH4102 were presented in a poster at the 2014 T-cell Lymphoma Forum. The research was conducted by investigators from Innate Pharma and INSERM at Hôpital Saint Louis in Paris.
The researchers generated 3 mAbs that bind selectively to KIR3DL2 and evaluated their efficacy against KIR3DL2-expressing tumors and Sézary cell lines.
IPH4102 was among the 3 mAbs and emerged as the most promising drug candidate.
Experiments revealed that anti-KIR3DL2 mAbs can kill KIR3DL2+ cell lines through allo-antibody-dependent cell cytotoxicity, even at low tumor antigen density.
The mAbs also improved survival in KIR3DL2+ xenograft models. Survival in mAb-treated mice ranged from 30.5 days to 54.5 days, compared to 19 days in controls.
Finally, the mAbs mediated killing of primary Sézary cells with autologous natural killer cells nearly as efficiently as alemtuzumab.
The investigators said these results suggest anti-KIR3DL2 mAbs are a feasible treatment option for CTCL patients. They plan to prove this hypothesis with a phase 1 trial of IPH4102, which is expected to begin in 2015. ![]()
The European Commission has granted orphan drug designation to IPH4102 for the treatment of cutaneous T-cell lymphoma (CTCL).
IPH4102 is a cytotoxic anti-KIR3DL2 monoclonal antibody (mAb) that targets CTCL cells.
Orphan status provides Innate Pharma, the company developing IPH4102, with benefits such as tax incentives, market exclusivity for 10 years, possibilities for additional research funding, and additional guidance from the European Medicines Agency during clinical development.
Preclinical results with IPH4102 were presented in a poster at the 2014 T-cell Lymphoma Forum. The research was conducted by investigators from Innate Pharma and INSERM at Hôpital Saint Louis in Paris.
The researchers generated 3 mAbs that bind selectively to KIR3DL2 and evaluated their efficacy against KIR3DL2-expressing tumors and Sézary cell lines.
IPH4102 was among the 3 mAbs and emerged as the most promising drug candidate.
Experiments revealed that anti-KIR3DL2 mAbs can kill KIR3DL2+ cell lines through allo-antibody-dependent cell cytotoxicity, even at low tumor antigen density.
The mAbs also improved survival in KIR3DL2+ xenograft models. Survival in mAb-treated mice ranged from 30.5 days to 54.5 days, compared to 19 days in controls.
Finally, the mAbs mediated killing of primary Sézary cells with autologous natural killer cells nearly as efficiently as alemtuzumab.
The investigators said these results suggest anti-KIR3DL2 mAbs are a feasible treatment option for CTCL patients. They plan to prove this hypothesis with a phase 1 trial of IPH4102, which is expected to begin in 2015.
Study validates drug’s efficacy in CLL/SLL
MILAN—Results of the phase 3 RESONATE trial suggest ibrutinib can improve response and survival rates in patients with relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), when compared to ofatumumab.
Ibrutinib conferred these benefits irrespective of baseline clinical characteristics or molecular features, including 17p deletion.
Atrial fibrillation and bleeding-related events were more common with ibrutinib. But the rate of serious adverse events was similar between the treatment arms.
About 86% of patients remained on ibrutinib at last analysis, and roughly 29% of patients initially randomized to ofatumumab crossed over to the ibrutinib arm after disease progression.
“This study undoubtedly confirms that ibrutinib is a very effective agent—as a single-agent—in relapsed CLL patients,” said investigator Peter Hillmen, MD, PhD, of The Leeds Teaching Hospitals in the UK.
Dr Hillmen presented these results at the 19th Congress of the European Hematology Association (EHA) as abstract S693. The RESONATE trial was sponsored by Pharmacyclics and Janssen, the companies developing ibrutinib.
The trial included 391 patients with relapsed or refractory CLL/SLL. They were randomized to receive oral ibrutinib at 420 mg once daily until progression or unacceptable toxicity (n=195) or intravenous ofatumumab at an initial dose of 300 mg, followed by 11 doses of 2000 mg (n=196). Patients in the ofatumumab arm were allowed to cross over to ibrutinib if they progressed (n=57).
The median age in both treatment arms was 67. Overall, roughly 50% of patients had received 3 or more prior therapies, including purine analogs, alkylating agents, and anti-CD20 antibodies. The proportion of patients with del17p was similar between the treatment arms—32% in the ibrutinib arm and 33% in the ofatumumab arm.
Response and survival
At the time of interim analysis, patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm, according to an independent review committee.
In addition, ibrutinib significantly prolonged progression-free survival (PFS). The median PFS was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The improvement in PFS represents a 78% reduction in the risk of progression or death.
Dr Hillmen noted that PFS favored ibrutinib regardless of baseline characteristics such as refractoriness to purine analogs, del17p, age, gender, Rai stage, bulky disease, number of prior treatments, del11q, B2 microglobulin, and IgVH mutation status.
Ibrutinib significantly prolonged overall survival (OS) as well. The median OS was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049). The improvement in OS represents a 56% reduction in the risk of death in patients treated with ibrutinib.
Adverse events
Dr Hillmen pointed out that the median treatment duration was 8.6 months for ibrutinib and 5.3 months for ofatumumab, and this difference confounds the assessment of side effects.
Nevertheless, nearly all patients in both treatment arms experienced adverse events—99% in the ibrutinib arm and 98% in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39% of patients, respectively.
Atrial fibrillation of any grade was more common in the ibrutinib arm (n=10) than in the ofatumumab arm (n=1), but 5 of the ibrutinib-treated patients had a prior history of atrial fibrillation. Bleeding-related events were also more common with ibrutinib (44% vs 12%), as were diarrhea (48% vs 18%) and arthralgia (17% vs 7%).
Events more common in the ofatumumab arm included infusion-related reactions (28% vs 0%), peripheral sensory neuropathy (13% vs 4%), urticaria (6% vs 1%), night sweats (13% vs 5%), and pruritus (9% vs 4%).
MILAN—Results of the phase 3 RESONATE trial suggest ibrutinib can improve response and survival rates in patients with relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), when compared to ofatumumab.
Ibrutinib conferred these benefits irrespective of baseline clinical characteristics or molecular features, including 17p deletion.
Atrial fibrillation and bleeding-related events were more common with ibrutinib. But the rate of serious adverse events was similar between the treatment arms.
About 86% of patients remained on ibrutinib at last analysis, and roughly 29% of patients initially randomized to ofatumumab crossed over to the ibrutinib arm after disease progression.
“This study undoubtedly confirms that ibrutinib is a very effective agent—as a single-agent—in relapsed CLL patients,” said investigator Peter Hillmen, MD, PhD, of The Leeds Teaching Hospitals in the UK.
Dr Hillmen presented these results at the 19th Congress of the European Hematology Association (EHA) as abstract S693. The RESONATE trial was sponsored by Pharmacyclics and Janssen, the companies developing ibrutinib.
The trial included 391 patients with relapsed or refractory CLL/SLL. They were randomized to receive oral ibrutinib at 420 mg once daily until progression or unacceptable toxicity (n=195) or intravenous ofatumumab at an initial dose of 300 mg, followed by 11 doses of 2000 mg (n=196). Patients in the ofatumumab arm were allowed to cross over to ibrutinib if they progressed (n=57).
The median age in both treatment arms was 67. Overall, roughly 50% of patients had received 3 or more prior therapies, including purine analogs, alkylating agents, and anti-CD20 antibodies. The proportion of patients with del17p was similar between the treatment arms—32% in the ibrutinib arm and 33% in the ofatumumab arm.
Response and survival
At the time of interim analysis, patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm, according to an independent review committee.
In addition, ibrutinib significantly prolonged progression-free survival (PFS). The median PFS was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The improvement in PFS represents a 78% reduction in the risk of progression or death.
Dr Hillmen noted that PFS favored ibrutinib regardless of baseline characteristics such as refractoriness to purine analogs, del17p, age, gender, Rai stage, bulky disease, number of prior treatments, del11q, B2 microglobulin, and IgVH mutation status.
Ibrutinib significantly prolonged overall survival (OS) as well. The median OS was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049). The improvement in OS represents a 56% reduction in the risk of death in patients treated with ibrutinib.
Adverse events
Dr Hillmen pointed out that the median treatment duration was 8.6 months for ibrutinib and 5.3 months for ofatumumab, and this difference confounds the assessment of side effects.
Nevertheless, nearly all patients in both treatment arms experienced adverse events—99% in the ibrutinib arm and 98% in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39% of patients, respectively.
Atrial fibrillation of any grade was more common in the ibrutinib arm (n=10) than in the ofatumumab arm (n=1), but 5 of the ibrutinib-treated patients had a prior history of atrial fibrillation. Bleeding-related events were also more common with ibrutinib (44% vs 12%), as were diarrhea (48% vs 18%) and arthralgia (17% vs 7%).
Events more common in the ofatumumab arm included infusion-related reactions (28% vs 0%), peripheral sensory neuropathy (13% vs 4%), urticaria (6% vs 1%), night sweats (13% vs 5%), and pruritus (9% vs 4%).
MILAN—Results of the phase 3 RESONATE trial suggest ibrutinib can improve response and survival rates in patients with relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), when compared to ofatumumab.
Ibrutinib conferred these benefits irrespective of baseline clinical characteristics or molecular features, including 17p deletion.
Atrial fibrillation and bleeding-related events were more common with ibrutinib. But the rate of serious adverse events was similar between the treatment arms.
About 86% of patients remained on ibrutinib at last analysis, and roughly 29% of patients initially randomized to ofatumumab crossed over to the ibrutinib arm after disease progression.
“This study undoubtedly confirms that ibrutinib is a very effective agent—as a single-agent—in relapsed CLL patients,” said investigator Peter Hillmen, MD, PhD, of The Leeds Teaching Hospitals in the UK.
Dr Hillmen presented these results at the 19th Congress of the European Hematology Association (EHA) as abstract S693. The RESONATE trial was sponsored by Pharmacyclics and Janssen, the companies developing ibrutinib.
The trial included 391 patients with relapsed or refractory CLL/SLL. They were randomized to receive oral ibrutinib at 420 mg once daily until progression or unacceptable toxicity (n=195) or intravenous ofatumumab at an initial dose of 300 mg, followed by 11 doses of 2000 mg (n=196). Patients in the ofatumumab arm were allowed to cross over to ibrutinib if they progressed (n=57).
The median age in both treatment arms was 67. Overall, roughly 50% of patients had received 3 or more prior therapies, including purine analogs, alkylating agents, and anti-CD20 antibodies. The proportion of patients with del17p was similar between the treatment arms—32% in the ibrutinib arm and 33% in the ofatumumab arm.
Response and survival
At the time of interim analysis, patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm, according to an independent review committee.
In addition, ibrutinib significantly prolonged progression-free survival (PFS). The median PFS was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The improvement in PFS represents a 78% reduction in the risk of progression or death.
Dr Hillmen noted that PFS favored ibrutinib regardless of baseline characteristics such as refractoriness to purine analogs, del17p, age, gender, Rai stage, bulky disease, number of prior treatments, del11q, B2 microglobulin, and IgVH mutation status.
Ibrutinib significantly prolonged overall survival (OS) as well. The median OS was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049). The improvement in OS represents a 56% reduction in the risk of death in patients treated with ibrutinib.
Adverse events
Dr Hillmen pointed out that the median treatment duration was 8.6 months for ibrutinib and 5.3 months for ofatumumab, and this difference confounds the assessment of side effects.
Nevertheless, nearly all patients in both treatment arms experienced adverse events—99% in the ibrutinib arm and 98% in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39% of patients, respectively.
Atrial fibrillation of any grade was more common in the ibrutinib arm (n=10) than in the ofatumumab arm (n=1), but 5 of the ibrutinib-treated patients had a prior history of atrial fibrillation. Bleeding-related events were also more common with ibrutinib (44% vs 12%), as were diarrhea (48% vs 18%) and arthralgia (17% vs 7%).
Events more common in the ofatumumab arm included infusion-related reactions (28% vs 0%), peripheral sensory neuropathy (13% vs 4%), urticaria (6% vs 1%), night sweats (13% vs 5%), and pruritus (9% vs 4%).

