User login
The Cruise With No Snooze
ANSWER
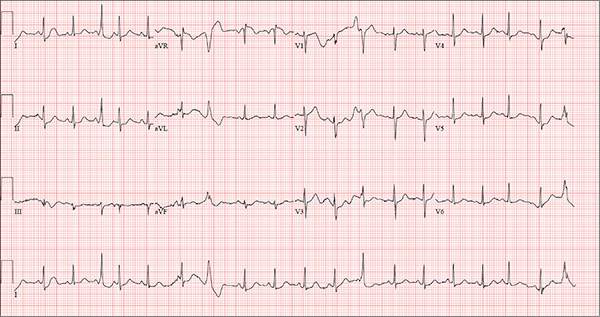
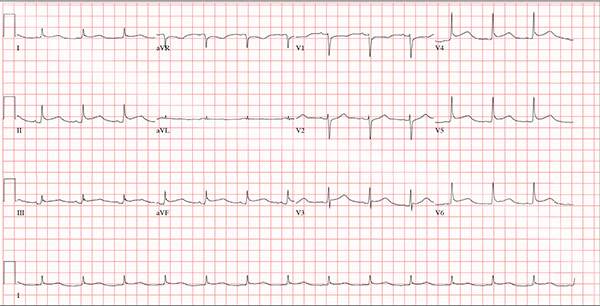
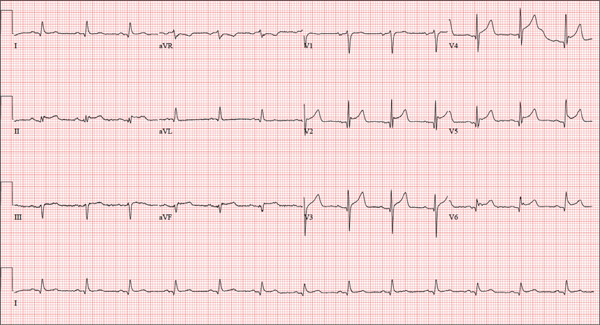
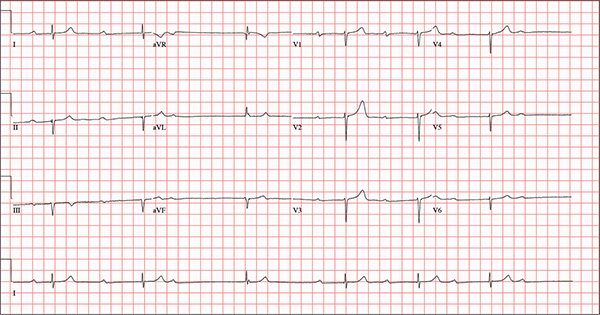
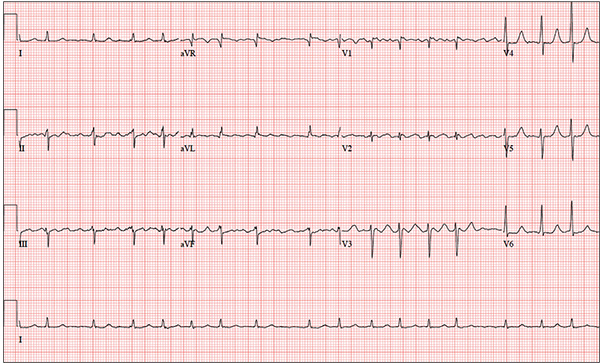
The correct interpretation of this ECG includes sinus tachycardia with premature supraventricular complexes, some with aberrant conduction.
The first, third, fourth, and 17th beats on lead I at the bottom of the rhythm strip are consistent with premature atrial contractions (PACs), while the sixth, seventh, 12th, and 19th beats represent PACs with aberrancy. The change in the QRS complex in the latter is due to the delay through the conduction system.
This patient was treated with low-dose ß-blockers and instructed to discontinue use of his holistic medication. His symptoms resolved, and follow-up ECGs have shown no evidence of sinus tachycardia or PACs.
ANSWER
The correct interpretation of this ECG includes sinus tachycardia with premature supraventricular complexes, some with aberrant conduction.
The first, third, fourth, and 17th beats on lead I at the bottom of the rhythm strip are consistent with premature atrial contractions (PACs), while the sixth, seventh, 12th, and 19th beats represent PACs with aberrancy. The change in the QRS complex in the latter is due to the delay through the conduction system.
This patient was treated with low-dose ß-blockers and instructed to discontinue use of his holistic medication. His symptoms resolved, and follow-up ECGs have shown no evidence of sinus tachycardia or PACs.
ANSWER
The correct interpretation of this ECG includes sinus tachycardia with premature supraventricular complexes, some with aberrant conduction.
The first, third, fourth, and 17th beats on lead I at the bottom of the rhythm strip are consistent with premature atrial contractions (PACs), while the sixth, seventh, 12th, and 19th beats represent PACs with aberrancy. The change in the QRS complex in the latter is due to the delay through the conduction system.
This patient was treated with low-dose ß-blockers and instructed to discontinue use of his holistic medication. His symptoms resolved, and follow-up ECGs have shown no evidence of sinus tachycardia or PACs.
Three weeks ago, while on a Caribbean cruise with his family, a 55-year-old man started experiencing an irregular heart rate, fluttering in his chest, and fullness in his throat. At the time, he was eating to excess, drinking heavily, and consuming three to five cups of coffee each morning to shake off the effects of the previous night. The palpitations were not noticeable during the day but were prevalent at night, when he tried to sleep. On more than one occasion, they woke him.
Since his return home, the symptoms have persisted; they now occur nightly. The patient is so concerned about them that he dreads going to bed. He has lost the 13 lb he gained on vacation and has abstained from alcohol, but he continues to drink four to six cups of coffee per day.
He denies syncope, near-syncope, chest pain, shortness of breath, and exertional dyspnea. On presentation, he is anxious to determine the cause of his symptoms and alleviate them.
The patient describes himself as active; he says he watches his diet, exercises regularly, and has never smoked. His medical history is unremarkable. He has never had surgery, and aside from sprained ankles, has had no medical treatment. His alcohol consumption, which tends to be limited to weekends, consists of four or five highballs at a time.
He is not currently taking any prescription medications, but he does admit to taking a proprietary herbal supplement that he purchases from a local Asian market. He says it “increases energy and libido.” He denies illicit drug use, now or ever.
The patient is married with three teenaged children who are all in the gifted program in high school. He and his wife are both accountants. His parents have no known medical problems; however, he is uncertain about the medical history of his grandparents.
A review of systems is unremarkable and reveals no complaints. The physical exam reveals an anxious male in no distress. His weight is 179 lb and his height, 74 in. Vital signs include a blood pressure of 140/86 mm Hg; pulse, 120 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.2°F.
The HEENT exam is remarkable for contacts but is otherwise normal. There is no thyromegaly or jugular venous distention. His lungs are clear in all fields, and there are no wheezes.
His cardiac exam reveals an irregular rhythm at a rate of 120 beats/min. There are no appreciable murmurs or rubs, given his heart rate.
The abdomen is soft and nontender, with no palpable masses. The peripheral pulses are strong bilaterally in the upper and lower extremities, and the neurologic exam is normal.
Bloodwork is performed to assess blood chemistries, complete blood count, and thyroid and liver function. All results are within normal limits. An ECG shows a ventricular rate of 123 beats/min; PR interval, 128 ms; QRS duration, 72 ms; QT/QTc interval, 308/440 ms; P axis, 43°; R axis, –2°; and T axis, 46°.
What is your interpretation of this ECG?
Persistent Cough, Peculiar Heart Sound
ANSWER
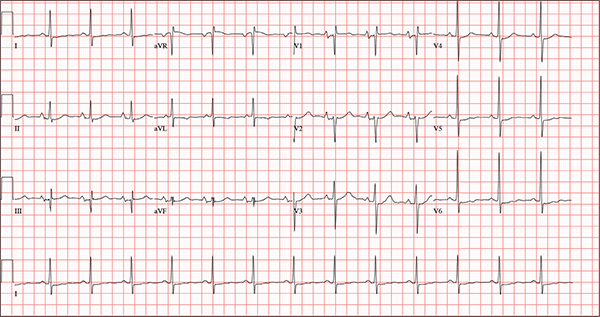
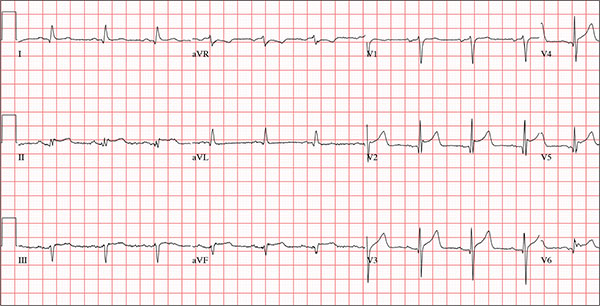
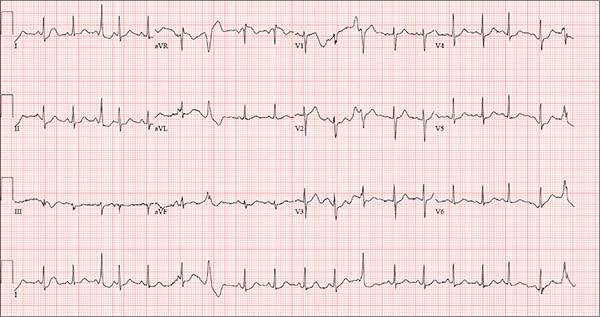
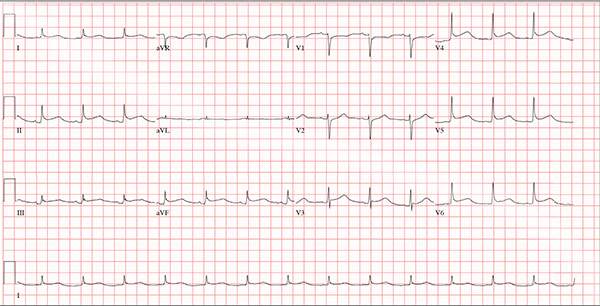
The correct interpretation of this ECG includes normal sinus rhythm, biatrial enlargement, nonspecific ST-T wave abnormality, and an RSR’ or QR pattern in V1, suggestive of right ventricular conduction delay.
Biatrial enlargement by definition encompasses right atrial enlargement (criteria include P waves in leads II, III, and aVF measuring 2.5 mm or more) and left atrial enlargement (evidenced by P waves in lead I ≥ 110 ms, and a biphasic, or “notched,” P wave with terminal negativity in lead V1).
Lead V1 may be interpreted as either an RSR’ or a QR pattern. However, the QRS duration of < 120 ms precludes this from meeting criteria for a right bundle branch block.
Finally, nonspecific ST-T wave changes were present in the precordial leads. These may be consistent with pulmonary disease.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm, biatrial enlargement, nonspecific ST-T wave abnormality, and an RSR’ or QR pattern in V1, suggestive of right ventricular conduction delay.
Biatrial enlargement by definition encompasses right atrial enlargement (criteria include P waves in leads II, III, and aVF measuring 2.5 mm or more) and left atrial enlargement (evidenced by P waves in lead I ≥ 110 ms, and a biphasic, or “notched,” P wave with terminal negativity in lead V1).
Lead V1 may be interpreted as either an RSR’ or a QR pattern. However, the QRS duration of < 120 ms precludes this from meeting criteria for a right bundle branch block.
Finally, nonspecific ST-T wave changes were present in the precordial leads. These may be consistent with pulmonary disease.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm, biatrial enlargement, nonspecific ST-T wave abnormality, and an RSR’ or QR pattern in V1, suggestive of right ventricular conduction delay.
Biatrial enlargement by definition encompasses right atrial enlargement (criteria include P waves in leads II, III, and aVF measuring 2.5 mm or more) and left atrial enlargement (evidenced by P waves in lead I ≥ 110 ms, and a biphasic, or “notched,” P wave with terminal negativity in lead V1).
Lead V1 may be interpreted as either an RSR’ or a QR pattern. However, the QRS duration of < 120 ms precludes this from meeting criteria for a right bundle branch block.
Finally, nonspecific ST-T wave changes were present in the precordial leads. These may be consistent with pulmonary disease.
A 54-year-old man presents with a four-day history of productive cough, low-grade fever, and malaise. The patient, a long-haul trucker, has been on the road for the past 30 days, traveling from Florida to California, and then to New Jersey. He first noticed a change in his cough after leaving Chicago. He says he’s tried OTC cough syrups to no avail, and he wants you to prescribe antibiotics so he can get back to work. He denies blood in his sputum; the specimen he provides on request is yellow, mucoid, and malodorous. You know this patient well: He has been in your patient panel for the past five years. His active problem list includes chronic obstructive pulmonary disease, hypertension, type 2 diabetes, obesity, and heavy tobacco use. He is rarely compliant with any of the treatment regimens you prescribe, and he frequently misses scheduled appointments due to his job. The patient is divorced, with no children, and spends most of his time on the road. His family history is remarkable for diabetes and hypertension in both parents. He had a history of binge drinking in his early 20s but has never had a citation for driving under the influence. He denies current recreational drug use, but he admits to using amphetamines prior to his employer’s mandatory drug monitoring. He smokes 2 to 2.5 packs of cigarettes per day and always has one in his mouth. His surgical history includes appendectomy and cholecystectomy, as well as two laparoscopic procedures for abdominal adhesions. His current medication list includes an albuterol inhaler, hydrochlorothiazide, metoprolol, and metformin; however, he states he rarely takes any of them on a daily basis. He is allergic to tetracycline, which produces urticaria and a rash. Vital signs include a blood pressure of 168/114 mm Hg; pulse, 80 beats/min; respiratory rate, 14 breaths/min-1; O2 saturation, 92% on room air; and temperature, 101°F. The review of systems is positive for headaches, toothache in numbers 13 and 14, and bleeding hemorrhoids. The remainder of the review is noncontributory. The physical exam reveals a disheveled male who appears uncomfortable and diaphoretic. His weight is 314 lb and his height, 70 in. Pertinent physical findings include consolidation in the right lower chest that does not change with coughing. He has coarse respiratory sounds in all other lung fields. There are no murmurs or rubs; however, there is a fixed, split-second heart sound that you haven’t heard in previous exams. The patient’s abdomen is rotund and nontender, with wellhealed surgical scars. Two large, inflamed hemorrhoids are present, and a stool guaiac test is positive for blood. The peripheral exam reveals 2+ bilateral pitting edema. All pulses are full, and there are no focal neurologic abnormalities. Given your concern about the unfamiliar heart sound, you order an ECG in addition to laboratory bloodwork and chest x-ray. The white blood cell count measures 12.4 x 1,000 μL, and the chest xray is consistent with right lower lobe pneumonia. The ECG reveals a ventricular rate of 82 beats/min; PR interval, 148 ms; QRS duration, 82 ms; QT/QTc interval, 378/441 ms; P axis, 42°; R wave axis, 20°; and T axis, 96°. What is your interpretation of this ECG?
It Reminds Him of When His Heart “Got Very Sick”
ANSWER
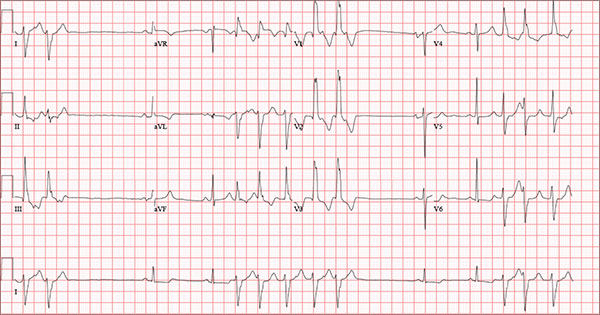
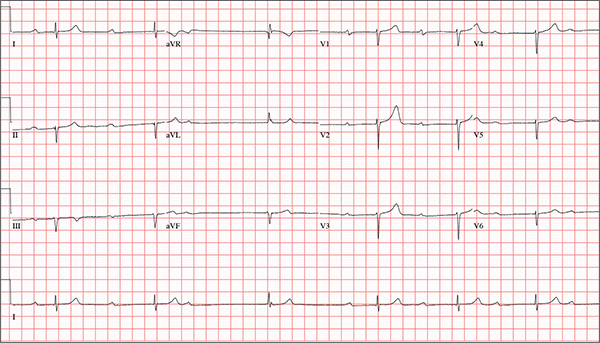
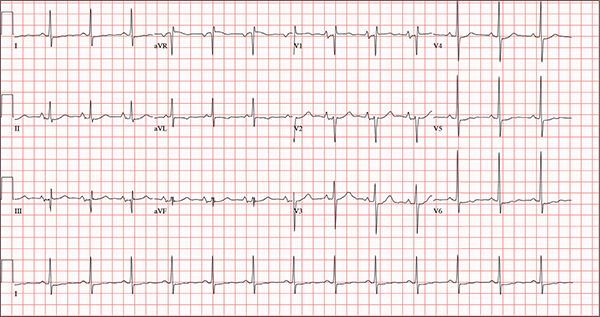
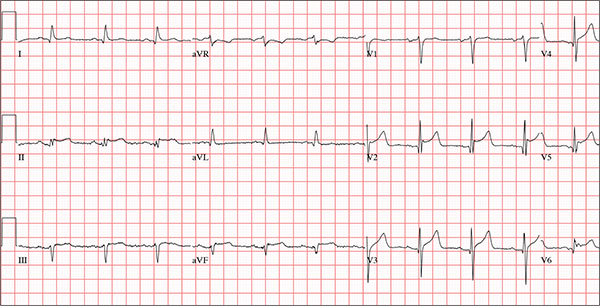
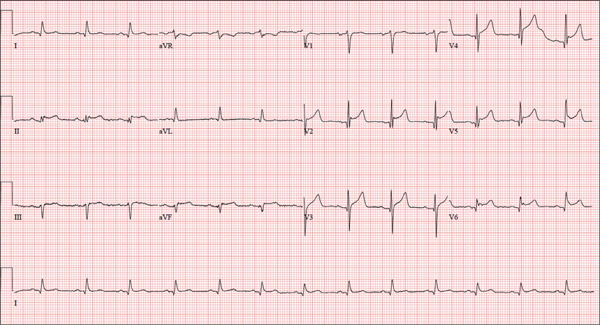
Findings on this ECG include sinus rhythm with frequent, consecutive premature ventricular complexes (PVCs) consistent with nonsustained ventricular tachycardia (NSVT). There is also evidence of a probable left atrial enlargement.
The key to interpreting this ECG is to first locate normal-appearing complexes. These are illustrated by the third, fourth, 10th, and 11th complexes on the rhythm strip (lead I) at the bottom of the ECG. Notice that there is a normal-appearing PQRST complex for each of these beats.
The rate of 82 beats/min is calculated from a sum average of all beats on the 12-lead ECG; however, the R-R interval between the third and fourth and the 10th and 11th beats is roughly 60 beats/min, signifying a normal sinus rhythm. All other beats are PVCs arising from the left ventricle (as evidenced by a right bundle branch pattern in lead V1).
Careful inspection will reveal retrograde P waves located in the terminal upstroke of the S wave. NSVT is defined as three or more consecutive PVCs at a rate greater than 100 beats/min with a duration of less than 30 seconds. The pauses seen between a PVC and a normally conducting P wave are caused by retrograde conduction from the ventricle to the atrium, with subsequent block within the atrium.
Finally, left atrial enlargement is evidenced by a biphasic P wave in the normally conducting beat seen in lead V1.
ANSWER
Findings on this ECG include sinus rhythm with frequent, consecutive premature ventricular complexes (PVCs) consistent with nonsustained ventricular tachycardia (NSVT). There is also evidence of a probable left atrial enlargement.
The key to interpreting this ECG is to first locate normal-appearing complexes. These are illustrated by the third, fourth, 10th, and 11th complexes on the rhythm strip (lead I) at the bottom of the ECG. Notice that there is a normal-appearing PQRST complex for each of these beats.
The rate of 82 beats/min is calculated from a sum average of all beats on the 12-lead ECG; however, the R-R interval between the third and fourth and the 10th and 11th beats is roughly 60 beats/min, signifying a normal sinus rhythm. All other beats are PVCs arising from the left ventricle (as evidenced by a right bundle branch pattern in lead V1).
Careful inspection will reveal retrograde P waves located in the terminal upstroke of the S wave. NSVT is defined as three or more consecutive PVCs at a rate greater than 100 beats/min with a duration of less than 30 seconds. The pauses seen between a PVC and a normally conducting P wave are caused by retrograde conduction from the ventricle to the atrium, with subsequent block within the atrium.
Finally, left atrial enlargement is evidenced by a biphasic P wave in the normally conducting beat seen in lead V1.
ANSWER
Findings on this ECG include sinus rhythm with frequent, consecutive premature ventricular complexes (PVCs) consistent with nonsustained ventricular tachycardia (NSVT). There is also evidence of a probable left atrial enlargement.
The key to interpreting this ECG is to first locate normal-appearing complexes. These are illustrated by the third, fourth, 10th, and 11th complexes on the rhythm strip (lead I) at the bottom of the ECG. Notice that there is a normal-appearing PQRST complex for each of these beats.
The rate of 82 beats/min is calculated from a sum average of all beats on the 12-lead ECG; however, the R-R interval between the third and fourth and the 10th and 11th beats is roughly 60 beats/min, signifying a normal sinus rhythm. All other beats are PVCs arising from the left ventricle (as evidenced by a right bundle branch pattern in lead V1).
Careful inspection will reveal retrograde P waves located in the terminal upstroke of the S wave. NSVT is defined as three or more consecutive PVCs at a rate greater than 100 beats/min with a duration of less than 30 seconds. The pauses seen between a PVC and a normally conducting P wave are caused by retrograde conduction from the ventricle to the atrium, with subsequent block within the atrium.
Finally, left atrial enlargement is evidenced by a biphasic P wave in the normally conducting beat seen in lead V1.
An 84-year-old man is transferred to your facility from a skilled nursing facility (SNF). During the routine morning vital signs check, the medical assistant (MA) at the SNF noted that the patient had a normal blood pressure but an irregular heart rate that she hadn’t observed before. The MA asked the nursing supervisor to verify her findings. The nursing supervisor noticed not only an irregular heart rate, but also pauses of up to 3 seconds. The patient denied chest pain, shortness of breath, or syncope, but he did say that twice overnight he had become lightheaded while walking from his bed to the bathroom. Upon further questioning, he informed the staff that this had happened once before: right before his “heart became very sick” and he spent a long time in the hospital “getting it fixed.” Given this history and the physical findings, the nursing supervisor called 911 to have him further evaluated. Your first impression of the patient is that he is comfortable, pleasant, and in no distress. His medical history is remarkable for a nonischemic cardiomyopathy with acute onset chronic heart failure. A year ago, he had an echocardiogram at another facility that showed aortic sclerosis, mild mitral regurgitation, and a left ventricular ejection fraction of 35%. He also has a history of hypertension, COPD, hypothyroidism, and osteoarthritis. His surgical history is remarkable for bilateral knee replacements, left hip replacement, and appendectomy. Family history is significant for heart failure in both parents and in his maternal grandparents. His father died in World War I, and his mother died of complications from abdominal surgery. The patient, a retired contract painter, became a widower five years ago, when his wife died of a hemorrhagic stroke. He has no children. Before voluntarily moving to the SNF after his wife’s death, he smoked one pack of cigarettes and drank one six-pack of beer per day. He now abstains from both substances. His medication list includes metoprolol, furosemide, potassium, lisinopril, and levothyroxine. He is allergic to tetracycline antibiotics.The review of systems is remarkable for hearing loss requiring bilateral hearing aids, corrective lenses, and use of a cane for ambulation. Physical examination reveals a frail, elderly male with a weight of 148 lb and a height of 68 in. His blood pressure is 104/52 mm Hg; pulse, irregularly irregular with pauses at an average rate of 80 beats/min; and O2 saturation, 94% on room air. He is afebrile. Pertinent physical findings include corrective lenses and bilateral hearing aids. A cataract is visible on the left eye. The lungs are clear bilaterally. The cardiac exam reveals an irregular rate, a grade II/VI early systolic murmur at the left upper sternal border with radiation into the neck, a grade II/VI early diastolic murmur heard during periods of a regular heart rate, and no rubs or gallops. The abdomen is protuberant but soft, with an old right lower quadrant surgical scar. The extremities show no evidence of peripheral edema; however, there are advanced changes related to osteoarthritis in both hands, and surgical scars over both knees and the lateral aspect of his left hip. Bloodwork is obtained for analysis, and an ECG is performed. The latter reveals a ventricular rate of 82 beats/min; PR interval, 146 ms; QRS duration, 76 ms; QT/QTc interval, 438/511 ms; P axis, 73°; R axis, 62°; and T axis, 92°. What is your interpretation of this ECG?
A Double Dose of Trouble
ANSWER
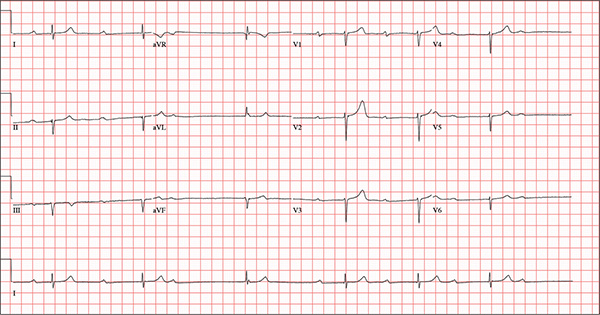
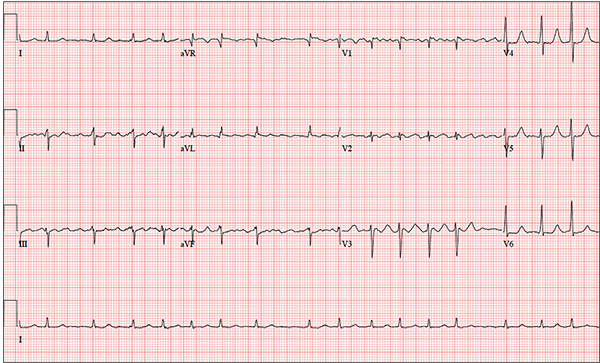
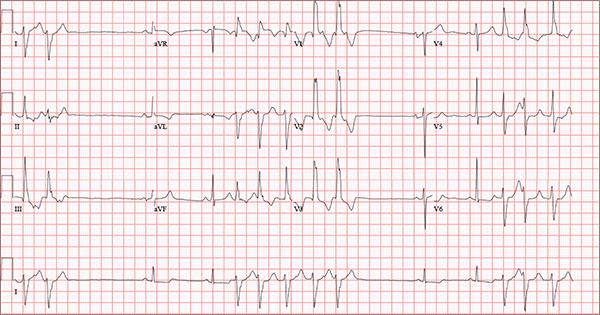
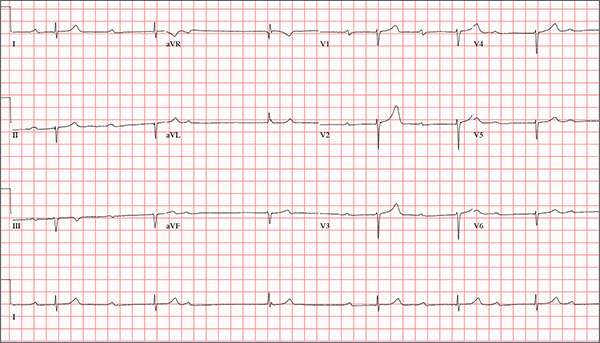
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
ANSWER
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
ANSWER
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
An 82-year-old man is referred from a nearby Alzheimer care facility following an episode of postural hypotension. While trying to get out of bed, he experienced near-syncope, which was observed by a nurse caring for another patient in the same room. The patient was helped back into bed, and the resident care provider was summoned. A careful examination ruled out any injury sustained when the patient’s knees buckled and he fell to the ground. However, he was found to have profound bradycardia with a pulse of 30 beats/min. Emergency medical services were called, and the patient was transported to your facility for further evaluation. You find the patient to be pleasant but mildly confused. He is in no distress. A review of the limited available records shows that he has had Alzheimer disease for four years; it has been relatively stable, with no recent changes in cognition. His history includes an inferior myocardial infarction (MI) at age 68 and hypertension. The latter has been treated with diuretics and ß-blockers, although the doses have not been changed since his MI. Other remarkable items in the history include hypothyroidism, type 2 diabetes, cholecystectomy, and appendectomy. He has significant osteoarthritis in both knees but does not require a cane or other device to ambulate. The patient is a retired iron worker from the local foundry. He is a widower with two adult children who live remotely and do not visit. He was a heavy drinker in his younger years and smoked one to two packs of cigarettes per day until his MI. He has abstained from alcohol and tobacco since his wife’s death six years ago. His medication list includes a daily aspirin, furosemide, potassium chloride, propranolol, and levothyroxine. He is said to be allergic to penicillin, but there is no record of him ever receiving it. The review of systems is difficult to obtain due to the patient’s confusion. He has not had any recent infectious illnesses, according to the accompanying nurse from the Alzheimer facility. Physical exam reveals a disheveled but otherwise pleasant man. He can remember only one out of three words when asked to recite immediately after hearing them. Vital signs include a blood pressure of 86/48 mm Hg; pulse, 40 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. His weight is 163 lb and his height, 66 in. The patient wears corrective lenses and hearing aids, but the batteries in the latter are dead. Regardless, he can hear you if you speak loudly. Pertinent physical findings include scattered crackles in both lung bases, a regularly irregular slow heart rate, a grade III/VI systolic murmur that radiates to the neck, and well-healed surgical scars on the abdomen consistent with the surgeries described in the history. There appear to be no gross focal neurologic findings. An ECG reveals a ventricular rate of 38 beats/min; PR interval, not measured; QRS duration, 78 ms; QT/QTc interval, 434/345 ms; P axis, 25°; R axis, –78°; and T axis, 13°. What is your interpretation of this ECG?
Cold and Fever Followed by Chest Discomfort
ANSWER
This ECG demonstrates normal sinus rhythm and diffuse ST elevations consistent with a diagnosis of pericarditis.
Although the QTc interval is long, it is due to the ST changes of pericarditis. Comparison with previous ECGs documented normal QTc intervals.
The patient’s pericarditis is most likely related to his recent viral illness. Following treatment with indomethacin, his symptoms resolved and his ECG normalized. Also, his abscess was managed by the surgical service and has since resolved.
ANSWER
This ECG demonstrates normal sinus rhythm and diffuse ST elevations consistent with a diagnosis of pericarditis.
Although the QTc interval is long, it is due to the ST changes of pericarditis. Comparison with previous ECGs documented normal QTc intervals.
The patient’s pericarditis is most likely related to his recent viral illness. Following treatment with indomethacin, his symptoms resolved and his ECG normalized. Also, his abscess was managed by the surgical service and has since resolved.
ANSWER
This ECG demonstrates normal sinus rhythm and diffuse ST elevations consistent with a diagnosis of pericarditis.
Although the QTc interval is long, it is due to the ST changes of pericarditis. Comparison with previous ECGs documented normal QTc intervals.
The patient’s pericarditis is most likely related to his recent viral illness. Following treatment with indomethacin, his symptoms resolved and his ECG normalized. Also, his abscess was managed by the surgical service and has since resolved.
A 47-year-old man presents with a five-day history of chest discomfort that he describes as vague and achy but not painful. The discomfort does not radiate to his arm or neck and is not affected by activity. About six weeks ago, the patient says, he developed a severe viral cold that had him bedridden for several days. During his illness, his temperature reached 102°F for three or four days, and he developed a rash that subsided around the time his fever did. He had shortness of breath then, but not now. He adds, however, that if he takes a deep breath, coughs, or sneezes, he feels a shooting pain beneath his sternum. Medical history is remarkable for hypertension, type 2 diabetes, and Wolff-Parkinson-White syndrome. Surgical history includes a left inguinal hernia repair at age 6, an appendectomy for acute appendicitis at age 13, and a successful catheter ablation at age 24. The patient, a long-haul trucker, is on the road five days a week and home on weekends. He is married and has four teenage children. He does not smoke or use recreational drugs; the company he works for performs weekly drug checks and offers financial incentives to employees who do not smoke. Family history reveals that his father died at age 68 of complications of diabetes. His 64-year-old mother is alive and well and has no health issues of which he is aware. His grandparents are deceased, and he has no information on their medical history. His medication list includes metoprolol, glyburide, and metformin. He has no known drug allergies. Review of systems reveals that he has recently developed an abscess on his left buttock that he says he needs to get fixed. He wears glasses and has several teeth with dental caries. He denies any symptoms suggestive of diabetic neuropathy. The remainder of the review is normal. Physical exam reveals that he weighs 228 lb and stands 76 in tall. Vital signs include a blood pressure of 138/84 mm Hg; pulse, 80 beats/min and regular; respiratory rate, 14 breaths/min-1; temperature, 99°F; and O2 saturation, 97% on room air. Pertinent physical findings include clear lungs bilaterally and a friction rub over the entire precordium. The abdomen is soft and nontender. There is a 1-cm abscess located 2 cm left of the sacrum that is fluctuant and tender to palpation. There is no peripheral edema. All pulses are present and strong bilaterally, and there are no focal neurologic findings. Laboratory tests reveal a normal blood chemistry panel. The complete blood count is remarkable for a white blood cell count of 12,000 cells/µL. In light of the friction rub, an ECG is obtained. It shows a ventricular rate of 82 beats/min; PR interval, 130 ms; QRS duration, 90 ms; QT/QTc interval, 442/516 ms; P axis, 78°; R axis, 59°; and T axis, 73°. What is your interpretation of this ECG?
Man Finds Worst Way to Get Out of Shoveling Snow
ANSWER
The correct answer is normal sinus rhythm, acute anterior myocardial infarction, and inferolateral injury.
A P wave for every QRS and a QRS for every P wave at a rate between 60 and 100 beats/min are indicative of normal sinus rhythm.
Acute anterior myocardial infarction is evidenced by the significant Q waves and ST elevations in leads I and V2 to V4 and inferolateral injury by ST elevations in limb leads II, III, and aVF and precordial leads V5 and V6.
Subsequent cardiac catheterization revealed an occlusion of the proximal left anterior descending coronary artery, as well as significant lesions in the posterior descending artery and a marginal branch of the circumflex coronary artery.
ANSWER
The correct answer is normal sinus rhythm, acute anterior myocardial infarction, and inferolateral injury.
A P wave for every QRS and a QRS for every P wave at a rate between 60 and 100 beats/min are indicative of normal sinus rhythm.
Acute anterior myocardial infarction is evidenced by the significant Q waves and ST elevations in leads I and V2 to V4 and inferolateral injury by ST elevations in limb leads II, III, and aVF and precordial leads V5 and V6.
Subsequent cardiac catheterization revealed an occlusion of the proximal left anterior descending coronary artery, as well as significant lesions in the posterior descending artery and a marginal branch of the circumflex coronary artery.
ANSWER
The correct answer is normal sinus rhythm, acute anterior myocardial infarction, and inferolateral injury.
A P wave for every QRS and a QRS for every P wave at a rate between 60 and 100 beats/min are indicative of normal sinus rhythm.
Acute anterior myocardial infarction is evidenced by the significant Q waves and ST elevations in leads I and V2 to V4 and inferolateral injury by ST elevations in limb leads II, III, and aVF and precordial leads V5 and V6.
Subsequent cardiac catheterization revealed an occlusion of the proximal left anterior descending coronary artery, as well as significant lesions in the posterior descending artery and a marginal branch of the circumflex coronary artery.
A 66-year-old man presents with ongoing chest pain of 45 minutes’ duration followed by ventricular fibrillation. He was outside shoveling snow for about 30 minutes before his wife noticed that the sound of shoveling had ceased and her husband was nowhere to be seen. Upon investigation, she found him sitting on the porch, holding his chest and moaning, and she immediately called 911. Paramedics arrived within 10 minutes. When the ambulance pulled into the driveway, the patient stood up and collapsed. The paramedics identified ventricular fibrillation and resuscitated him with a single shock from the automatic external defibrillator. The patient quickly regained consciousness and did not require further intervention. According to the paramedics, the patient was in ventricular fibrillation for less than one minute. Oxygen and anti-angina therapy, started in the field, provided prompt relief of his chest pain. Upon arrival to the emergency department, the patient is awake, stable, and fully cognizant of what happened and where he is. History taking reveals that he has experienced chest pain with exertion for several weeks, beginning around Thanksgiving, but did not want to worry his family during the holiday season. All prior episodes stopped as soon as he ceased physical activity, unlike the one he experienced today. The patient has a history of hypertension but no other cardiac problems. Surgical history is remarkable for a right rotator cuff repair and removal of a melanoma from his nose. Family history is positive for myocardial infarction (both parents and paternal grandfather) and type 1 diabetes (mother). The patient, an only child, has two adult sons, both of whom are in good health. The patient is a retired attorney. He drinks approximately one bottle of wine per week, does not drink beer or hard liquor, and has never smoked. He has been quite active and runs 10K races three or four times per year. He denies recreational or herbal drug use. He currently takes no medications—not even the hydrochlorothiazide and metoprolol prescribed for his hypertension, neither of which he has taken for the past year. He says he occasionally takes ibuprofen for “typical muscle aches and pains.” He has no known drug allergies. The review of systems is unremarkable. The patient denies palpitations, shortness of breath, recent weight gain, and headaches. Physical exam reveals a well-nourished, well-groomed man with a blood pressure of 160/98 mm Hg; pulse, 80 beats/min; respiratory rate, 18 breaths/min-1; O2 saturation, 100% on 2 L of oxygen via nasal cannula; and temperature, 98.2°F. He reports his weight to be 189 lb and his height, 6 ft 2 in. There are no unusual findings: His lungs are clear; his cardiac exam reveals no murmurs, rubs, gallops, or arrhythmia; the abdomen is soft and not tender; there is no peripheral edema; and he is neurologically intact. An ECG, laboratory tests, and an echocardiogram are ordered. You review the ECG while the other tests are pending and note a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 390/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of this ECG?
Holiday Trip Marred by Illness
ANSWER
This ECG is representative of marked sinus bradycardia with second-degree atrioventricular block (Mobitz I) with an occasional junctional escape, left-axis deviation, and poor R-wave progression in the precordial leads.
Marked sinus bradycardia is evidenced by P waves that are regular except where expected, prior to the third QRS complex on the rhythm strip (lead 1).
Second-degree Mobitz I (Wenckebach) block is indicated by a gradual prolonging of the PR interval until there is loss of conduction from the atria to the ventricle (following the third P wave). Careful inspection of the third QRS complex shows a slight difference in the normally conducted sinus beat, indicative of a junctional escape beat. Left-axis deviation entails an R-wave axis of –78°.
Finally, there is poor R-wave progression in the precordial leads, including the lateral leads.
Although Mobitz I block is not an indication for pacemaker placement, symptomatic bradycardia is. The patient underwent implantation of a dual-chamber permanent pacemaker, with complete resolution of symptoms.
ANSWER
This ECG is representative of marked sinus bradycardia with second-degree atrioventricular block (Mobitz I) with an occasional junctional escape, left-axis deviation, and poor R-wave progression in the precordial leads.
Marked sinus bradycardia is evidenced by P waves that are regular except where expected, prior to the third QRS complex on the rhythm strip (lead 1).
Second-degree Mobitz I (Wenckebach) block is indicated by a gradual prolonging of the PR interval until there is loss of conduction from the atria to the ventricle (following the third P wave). Careful inspection of the third QRS complex shows a slight difference in the normally conducted sinus beat, indicative of a junctional escape beat. Left-axis deviation entails an R-wave axis of –78°.
Finally, there is poor R-wave progression in the precordial leads, including the lateral leads.
Although Mobitz I block is not an indication for pacemaker placement, symptomatic bradycardia is. The patient underwent implantation of a dual-chamber permanent pacemaker, with complete resolution of symptoms.
ANSWER
This ECG is representative of marked sinus bradycardia with second-degree atrioventricular block (Mobitz I) with an occasional junctional escape, left-axis deviation, and poor R-wave progression in the precordial leads.
Marked sinus bradycardia is evidenced by P waves that are regular except where expected, prior to the third QRS complex on the rhythm strip (lead 1).
Second-degree Mobitz I (Wenckebach) block is indicated by a gradual prolonging of the PR interval until there is loss of conduction from the atria to the ventricle (following the third P wave). Careful inspection of the third QRS complex shows a slight difference in the normally conducted sinus beat, indicative of a junctional escape beat. Left-axis deviation entails an R-wave axis of –78°.
Finally, there is poor R-wave progression in the precordial leads, including the lateral leads.
Although Mobitz I block is not an indication for pacemaker placement, symptomatic bradycardia is. The patient underwent implantation of a dual-chamber permanent pacemaker, with complete resolution of symptoms.
While visiting family over the holidays, an 84-year-old man is (plaintively) informed by his wife that he appears unwell; she suspects he has the flu. The patient’s son, whom they are visiting, learns through conversation that his father has been feeling very tired and lethargic and becomes dizzy if he stands too quickly. The son, concerned for his father’s well-being, brings him to your clinic in the hope of obtaining a prescription for antibiotics. According to the patient, his symptoms, which have waxed and waned for several weeks, have become constant in the past week. He denies fever, cough, nausea, and vomiting, as well as chest pain, shortness of breath, palpitations, and lower extremity swelling. He reports that he has not recently changed his medication regimen and, aside from this current visit, has not traveled anywhere; he reiterates that his symptoms started prior to this trip. Medical history is remarkable for hypertension, peripheral atherosclerosis, osteoarthritis, gout, and pneumonia. Surgical history is remarkable for appendectomy, cholecystectomy, and removal of multiple lipomas from the patient’s upper extremities. Via the family history, you learn that the man’s father had a myocardial infarction and died of complications from a stroke at age 92 and his mother died of complications of diabetes at age 87. The patient is married, with three sons and one daughter, all of whom are in good health. He is a retired owner of a hardware store. He has never smoked or used recreational drugs and says he rarely drinks alcohol. The patient’s medication list includes metoprolol, atorvastatin, furosemide, and a daily baby aspirin. He is allergic to sulfa, which causes shortness of breath and wheezing. Review of systems reveals that he wears corrective lenses and hearing aids. He walks with a cane due to pain in both knees but is not dependent on it. He denies constitutional symptoms. A review of cardiovascular, respiratory, gastrointestinal, urologic, neurologic, and integumentary systems is noncontributory. Chest x-ray and laboratory testing, including complete blood count and chemistry panel, yield normal results. Vital signs include a blood pressure of 162/92 mm Hg; pulse, 40 beats/min; respiratory rate, 14 breaths/min; temperature, 99.2°F; and O2 saturation, 97% on room air. Pertinent physical findings include clear lung fields bilaterally, no evidence of jugular venous distention, and a heart rate of 40 beats/min that is regular and without evidence of a murmur or rub. There are well-healed scars on the abdomen and no evidence of organomegaly. Peripheral pulses are diminished but present bilaterally in both lower extremities. The neurologic exam is grossly intact, and the patient is alert, cooperative, and cognizant. Your concern about the patient’s heart rate prompts you to order an ECG. It reveals a ventricular rate of 38 beats/min; no measurable PR interval; QRS duration, 78 ms; QT/QTc interval, 434/345 ms; P axis, 25°; R axis, –78°; and T axis, 13°. What is your interpretation of this ECG?
Friendly Advice Goes Awry
ANSWER
The correct interpretation is coarse atrial fibrillation with a rapid ventricular response and left-axis deviation.
Coarse atrial fibrillation is evidenced by the irregularly irregular rhythm with a normal QRS duration and flutter/fibrillation waves arising from the atria. Rapid ventricular response is defined as a ventricular response > 100 beats/min (seen in this case). Finally, an R-wave axis between –30° and –90° is indicative of left-axis deviation.
Correcting the patient’s hypokalemia and hypomagnesemia resulted in a return to normal sinus rhythm. At one-year follow-up, he had had no further episodes of atrial fibrillation.
ANSWER
The correct interpretation is coarse atrial fibrillation with a rapid ventricular response and left-axis deviation.
Coarse atrial fibrillation is evidenced by the irregularly irregular rhythm with a normal QRS duration and flutter/fibrillation waves arising from the atria. Rapid ventricular response is defined as a ventricular response > 100 beats/min (seen in this case). Finally, an R-wave axis between –30° and –90° is indicative of left-axis deviation.
Correcting the patient’s hypokalemia and hypomagnesemia resulted in a return to normal sinus rhythm. At one-year follow-up, he had had no further episodes of atrial fibrillation.
ANSWER
The correct interpretation is coarse atrial fibrillation with a rapid ventricular response and left-axis deviation.
Coarse atrial fibrillation is evidenced by the irregularly irregular rhythm with a normal QRS duration and flutter/fibrillation waves arising from the atria. Rapid ventricular response is defined as a ventricular response > 100 beats/min (seen in this case). Finally, an R-wave axis between –30° and –90° is indicative of left-axis deviation.
Correcting the patient’s hypokalemia and hypomagnesemia resulted in a return to normal sinus rhythm. At one-year follow-up, he had had no further episodes of atrial fibrillation.
You have been following a 57-year-old man for gastroesophageal reflux disease (GERD). He presents for routine follow-up stating that his reflux has subsided; you presume this is a result of the 14-day course of a proton pump inhibitor that you prescribed. However, the patient confesses that, for about three months, he’s taken his omeprazole at twice the dose—because a friend told him that OTC medications are half the dose of the prescription versions. His primary concern today is that his heart has started flip-flopping in his chest for brief periods at bedtime. The symptoms typically last for 30 to 60 minutes and recur when he wakes in the morning—particularly if he is startled by his alarm clock. They began approximately a week ago, and he reports that they start and stop abruptly. The patient denies chest pain, dyspnea, and syncope or near-syncope, but he does note that it feels like something is “sticking in his throat.” His active medical problems include GERD, hypertension, and obesity. Surgical history is remarkable for repair of bilateral ankle fractures and a left femur fracture sustained in a motorcycle accident six years ago. Current medications include omeprazole, metoprolol, furosemide, and potassium chloride. He says he ran out of his potassium about a month ago and hasn’t refilled it yet. He also reports that he hasn’t taken his metoprolol in more than six months, because it makes him lethargic. He has no known drug allergies. The patient, who works as a welder, is married and has one son. He drinks approximately one six-pack of beer per week and smokes half a pack of cigarettes per day. He uses marijuana recreationally once or twice a month but denies use of any other illicit or naturopathic drugs. Review of systems is remarkable for a smoker’s cough, which clears with coughing. He also states his right eye twitches uncontrollably, and he feels weak and washed out. He denies nausea, vomiting, diarrhea, and constipation. While you are conducting the review, he states, “It just started again.” You immediately check the patient’s pulse; it is 110 beats/min and irregular. Additional vital statistics include a blood pressure of 124/74 mm Hg; respiratory rate, 14 breaths/min; O2 saturation, 96% on room air; and temperature, 98.4°F. His weight is 245 lb and his height, 72 in. Pertinent physical findings include inspiratory and expiratory crackles that change with coughing, an irregularly irregular rhythm without evidence of a murmur or rub, a soft abdomen, and no evidence of jugular venous distention or peripheral edema. Laboratory values are within normal limits, with the exception of the potassium (2.8 mmol/L; normal range, 3.6-5.2 mmol/L) and magnesium (0.9 mg/dL; normal range, 1.8-2.6 mg/dL). An ECG reveals a ventricular rate of 108 beats/min; PR interval, not measured; QRS duration, 78 ms; QT/QTc interval, 352/471 ms; no P axis; R axis, –64°; and T axis, –58°. What is your interpretation of this ECG?
“Spry” Woman Reports Rapid Heart Rate
ANSWER
The correct interpretation includes atrial fibrillation with a rapid ventricular response and aberrantly conducted complexes, left axis deviation, and a left bundle branch block.
Atrial fibrillation is evidenced by the irregularly irregular heart rhythm without a measurable PR interval, and the rapid ventricular response is indicated by a ventricular rate > 100 beats/min.
Aberrant conduction, caused by conduction delay down the His-Purkinje system, is evidenced by the wide QRS complexes with a normally conducted beat (see first beat in leads V1-V3). Criteria for left axis deviation include an R axis between –30° and –90°, and left bundle branch block criteria include a QRS duration > 120 ms, a dominant S wave in V1, and broad monophasic R waves in leads I, aVL, and V5-V6.
ANSWER
The correct interpretation includes atrial fibrillation with a rapid ventricular response and aberrantly conducted complexes, left axis deviation, and a left bundle branch block.
Atrial fibrillation is evidenced by the irregularly irregular heart rhythm without a measurable PR interval, and the rapid ventricular response is indicated by a ventricular rate > 100 beats/min.
Aberrant conduction, caused by conduction delay down the His-Purkinje system, is evidenced by the wide QRS complexes with a normally conducted beat (see first beat in leads V1-V3). Criteria for left axis deviation include an R axis between –30° and –90°, and left bundle branch block criteria include a QRS duration > 120 ms, a dominant S wave in V1, and broad monophasic R waves in leads I, aVL, and V5-V6.
ANSWER
The correct interpretation includes atrial fibrillation with a rapid ventricular response and aberrantly conducted complexes, left axis deviation, and a left bundle branch block.
Atrial fibrillation is evidenced by the irregularly irregular heart rhythm without a measurable PR interval, and the rapid ventricular response is indicated by a ventricular rate > 100 beats/min.
Aberrant conduction, caused by conduction delay down the His-Purkinje system, is evidenced by the wide QRS complexes with a normally conducted beat (see first beat in leads V1-V3). Criteria for left axis deviation include an R axis between –30° and –90°, and left bundle branch block criteria include a QRS duration > 120 ms, a dominant S wave in V1, and broad monophasic R waves in leads I, aVL, and V5-V6.

An 84-year-old woman who recently relocated to be closer to her children presents to your practice as a new patient. She is a resident of an assisted living facility near your office, and although she has no specific complaints, she does report that her home health nurse observed a rapid heart rate and recommended she get it checked. A comprehensive medical history—provided by the patient, her daughter, and the aforementioned nurse—includes hypertension, paroxysmal atrial fibrillation, hypothyroidism, and type 2 diabetes. She has taken medication for these diagnoses for more than 30 years. Surgical history is remarkable for cholecystectomy, appendectomy, and abdominal hysterectomy and oophorectomy, all of which were performed in the 1970s. Her current medication list—confirmed by the assisted living facility—includes furosemide, glyburide, metoprolol, potassium, and levothyroxine. She has not missed any doses. She is allergic to sulfa. The patient, a retired teacher, has never smoked, but she does “enjoy” one martini at dinner on a regular basis. She is widowed; her two daughters and four sons are all alive and well. The review of systems is remarkable for corrective lenses, bilateral hearing aids, and chronic joint pain. The patient does not routinely weigh herself but thinks, based on the fit of her clothes, that she may have gained some weight. She denies constitutional symptoms and shortness of breath. She thinks she may have a urinary tract infection, as she’s had burning with urination for several days, but says this is beginning to improve. Physical exam reveals a blood pressure of 168/90 mm Hg; pulse, 106 beats/min; temperature, 98.4° F; and O2 saturation, 94% on room air. Her weight is 132 lb and her height, 60 in. She is alert and quite spry, with a lot of energy. She wears glasses and bilateral hearing aids. Jugular distention is present to the angle of the jaw. There is no thyromegaly. The pulmonary exam is remarkable for crackles in both lung bases. The heart rhythm is irregularly irregular at a rate of 110 beats/min, and a grade II/VI murmur of mitral regurgitation is heard at the left lower sternal border. The abdomen is soft and nontender, with multiple surgical scars. The lower extremities are remarkable for 2+ pitting edema bilaterally to the level of the mid-calf. Osteoarthritic changes are present in both hands. The neurologic exam is grossly intact. An ECG reveals a ventricular rate of 110 beats/min; PR interval, not measured; QRS duration, 144 ms; QT/QTc interval, 298/403 ms; no P axis; R axis, –36°; and T axis, 169°. What is your interpretation of this ECG?
Man Collapses While Playing Basketball
ANSWER
The correct interpretation is normal sinus rhythm with an acute anterior MI (STEMI) and inferolateral injury. In the absence of left ventricular hypertrophy and left bundle-branch block, an acute anterior MI manifests with new ST elevations ≥ 0.1 mV, measured at the J point in leads V2-V3. Inferolateral injury is indicated by ST elevations in leads II, III, and aVF, as well as ST elevations in leads V4-V6.
Laboratory findings confirmed the diagnosis of a new infarction, and cardiac catheterization revealed significant blockage in the proximal left anterior descending and circumflex coronary arteries. These were treated percutaneously, and the patient recovered without sequelae.
ANSWER
The correct interpretation is normal sinus rhythm with an acute anterior MI (STEMI) and inferolateral injury. In the absence of left ventricular hypertrophy and left bundle-branch block, an acute anterior MI manifests with new ST elevations ≥ 0.1 mV, measured at the J point in leads V2-V3. Inferolateral injury is indicated by ST elevations in leads II, III, and aVF, as well as ST elevations in leads V4-V6.
Laboratory findings confirmed the diagnosis of a new infarction, and cardiac catheterization revealed significant blockage in the proximal left anterior descending and circumflex coronary arteries. These were treated percutaneously, and the patient recovered without sequelae.
ANSWER
The correct interpretation is normal sinus rhythm with an acute anterior MI (STEMI) and inferolateral injury. In the absence of left ventricular hypertrophy and left bundle-branch block, an acute anterior MI manifests with new ST elevations ≥ 0.1 mV, measured at the J point in leads V2-V3. Inferolateral injury is indicated by ST elevations in leads II, III, and aVF, as well as ST elevations in leads V4-V6.
Laboratory findings confirmed the diagnosis of a new infarction, and cardiac catheterization revealed significant blockage in the proximal left anterior descending and circumflex coronary arteries. These were treated percutaneously, and the patient recovered without sequelae.
A 46-year-old man is playing intramural basketball when he suddenly collapses on the court. Bystander CPR is begun; the patient is revived immediately without need for cardioversion or defibrillation. He regains consciousness before EMS arrives and, although he does not recall collapsing, he is able to tell them that he has been experiencing chest discomfort all morning (but didn’t mention it to anyone). The patient is transported in stable condition to the emergency department (ED) via BLS ambulance. The total time from his collapse to hospital arrival is 77 minutes, due to the rural location of the high school where he was playing. When you see the patient in the ED, you learn that he has no prior history of cardiac symptoms. He specifically denies chest pain, shortness of breath, dyspnea on exertion, or peripheral edema, although with additional questioning, he admits to having ongoing substernal pressure. There is no history of hypertension, diabetes, hyperlipidemia, or thyroid disorder. Surgical history is remarkable for a left anterior cruciate repair that he underwent while in high school. He is employed as an assistant principal at a local high school, is married with two children, and is active in his community—a fact borne out by the volume of well-wishers in the waiting area, inquiring about his status. He does not smoke, drinks two or three beers on the weekend, and does not use recreational drugs, although he admits he tried marijuana in college and didn’t care for it. He is not taking any routine prescription or holistic medications and has no known drug allergies. He reports taking ibuprofen on occasion but adds that he hasn’t taken any in the past three weeks. Review of systems is remarkable for a recent cold. He says he has a residual cough and runny nose but does not feel like he’s currently sick. He considers himself to be very healthy and a role model for the students and faculty at his school. Physical exam reveals a blood pressure of 142/84 mm Hg; pulse, 84 beats/min; respiratory rate, 18 breaths/min; and O2 saturation, 99% on 2 L of oxygen. His weight is 189 lb and his height, 74 in. He appears anxious and apprehensive but is alert and cooperative. Pertinent physical findings include a regular rate and rhythm, clear lungs, a soft, nontender abdomen, and no peripheral edema or jugular venous distention. The neurologic exam is intact. Specimens are drawn and sent to the lab for processing. While awaiting the results, you review the ECG taken at the time of arrival. It shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of this ECG?