User login
John Nelson: Why Spinal Epidural Abcess Poses A Particular Liability Risk for Hospitalists
Delayed diagnosis of, or treatment for, a spinal epidural abscess (SEA): that will be the case over which you are sued.
Over the last 15 years, I’ve served as an expert witness for six or seven malpractice cases. Most were related to spinal cord injuries, and in all but one of those, the etiology was epidural abscess. I’ve been asked to review about 40 or 50 additional cases, and while I’ve turned them down (I just don’t have time to do reviews), I nearly always ask about the clinical picture in every case. A significant number have been SEA-related. This experience has convinced me that SEA poses a particular liability risk for hospitalists.
Of course, it is patients who bear the real risk and unfortunate consequences of SEA. Being a defendant physician in a lawsuit is stressful, but it’s nothing compared to the distress of permanent loss of neurologic function. To prevent permanent sequelae, we need to maintain a very high index of suspicion to try to make a prompt diagnosis, and ensure immediate intervention once the diagnosis is made.
Data from Malpractice Insurers
I had the pleasure of getting to know a number of leaders at The Doctor’s Company, a large malpractice insurer that provides malpractice policies for all specialties, including a lot of hospitalists. From 2007 to 2011, they closed 28 SEA-related claims, for which they spent an average of $212,000 defending each one. Eleven of the 28 resulted in indemnity payments averaging $754,000 each (median was $455,000). These dollar amounts are roughly double what might be seen for all other claims and reflect only the payments made on behalf of the company’s insured doctors. The total award to each patient was likely much higher, because in most cases, several defendants (other doctors and a hospital) probably paid money to the patient.
The Physician Insurers Association of America (PIAA) “is the insurance industry trade association representing domestic and international medical professional liability insurance companies.” Their member malpractice insurance companies have the opportunity to report claims data that PIAA aggregates and makes available. Data from 2002 to 2011 showed 312 closed claims related to any diagnosis (not just SEA) for hospitalists, with an average indemnity payment of $272,553 (the highest hospitalist-related payment was $1.4 million). The most common allegations related to paid claims were 1) “errors in diagnosis,” 2) “failure/delay in referral or consultation,” and 3) “failure to supervise/monitor case.” Although only three of the 312 claims were related to “diseases of the spinal cord,” that was exceeded in frequency only by “diabetes.”
I think these numbers from the malpractice insurance industry support my concern that SEA is a high-risk area, but it doesn’t really support my anecdotal experience that SEA is clearly hospitalists’ highest-risk area. Maybe SEA is only one of several high-risk areas. Nevertheless, I’m going to stick to my sensationalist guns to get your attention.
Why Is Epidural Abscess a High Risk?
There likely are several reasons SEA is a treacherous liability problem. It can lead to devastating permanent disabling neurologic deficits in people who were previously healthy, and if the medical care was substandard, then significant financial compensation seems appropriate.
Delays in diagnosis of SEA are common. It can be a very sneaky illness that in the early stages is very easy to confuse with less-serious causes of back pain or fever. Even though I think about this particular diagnosis all the time, just last year I had a patient who reported an increase in his usual back pain. I felt reassured that he had no neurologic deficit or fever, and took the time to explain why there was no reason to repeat the spine MRI that had been done about two weeks prior to admission. But he was insistent that he have another MRI, and after a day or two I finally agreed to order it, assuring him it would not explain the cause of his pain. But it did. He had a significant SEA and went to emergency surgery. I was stunned, and profoundly relieved that he had no neurologic sequelae.
One of the remarkable things I’ve seen in the cases I’ve reviewed is that even when there is clear cause for concern, there is too often no action taken. In a number of cases, the nurses’ note indicates increasing back pain, loss of ability to stand, urinary retention, and other alarming signs. Yet the doctors either never learn of these issues, or they choose to attribute them to other causes.
Even when the diagnosis of SEA is clearly established, it is all too common for doctors caring for the patient not to act on this information. In several cases I reviewed, a radiologist had documented reporting the diagnosis to the hospitalist (and in one case the neurosurgeon as well), yet nothing was done for 12 hours or more. It is hard to imagine that establishing this diagnosis doesn’t reliably lead to an emergent response, but it doesn’t. (In some cases, nonsurgical management may be an option, but in these malpractices cases, there was just a failure to act on the diagnosis with any sort of plan.)
Practice Management Perspective
I usually discuss hospitalist practice operations in this space—things like work schedules and compensation. But attending to risk management is one component of effective practice operations, so I thought I’d raise the topic here. Obviously, there is a lot more to hospitalist risk management than one diagnosis, but a column on the whole universe of risk management would probably serve no purpose other than as a sleep aid. I hope that by focusing solely on SEA, there is some chance that you’ll remember it, and you’ll make sure that you disprove my first two sentences.
Lowering your risk of a malpractice lawsuit is valuable and worth spending time on. But far more important is that by keeping the diagnosis in mind, and ensuring that you act emergently when there is cause for concern, you might save someone from the devastating consequences of this disease.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Delayed diagnosis of, or treatment for, a spinal epidural abscess (SEA): that will be the case over which you are sued.
Over the last 15 years, I’ve served as an expert witness for six or seven malpractice cases. Most were related to spinal cord injuries, and in all but one of those, the etiology was epidural abscess. I’ve been asked to review about 40 or 50 additional cases, and while I’ve turned them down (I just don’t have time to do reviews), I nearly always ask about the clinical picture in every case. A significant number have been SEA-related. This experience has convinced me that SEA poses a particular liability risk for hospitalists.
Of course, it is patients who bear the real risk and unfortunate consequences of SEA. Being a defendant physician in a lawsuit is stressful, but it’s nothing compared to the distress of permanent loss of neurologic function. To prevent permanent sequelae, we need to maintain a very high index of suspicion to try to make a prompt diagnosis, and ensure immediate intervention once the diagnosis is made.
Data from Malpractice Insurers
I had the pleasure of getting to know a number of leaders at The Doctor’s Company, a large malpractice insurer that provides malpractice policies for all specialties, including a lot of hospitalists. From 2007 to 2011, they closed 28 SEA-related claims, for which they spent an average of $212,000 defending each one. Eleven of the 28 resulted in indemnity payments averaging $754,000 each (median was $455,000). These dollar amounts are roughly double what might be seen for all other claims and reflect only the payments made on behalf of the company’s insured doctors. The total award to each patient was likely much higher, because in most cases, several defendants (other doctors and a hospital) probably paid money to the patient.
The Physician Insurers Association of America (PIAA) “is the insurance industry trade association representing domestic and international medical professional liability insurance companies.” Their member malpractice insurance companies have the opportunity to report claims data that PIAA aggregates and makes available. Data from 2002 to 2011 showed 312 closed claims related to any diagnosis (not just SEA) for hospitalists, with an average indemnity payment of $272,553 (the highest hospitalist-related payment was $1.4 million). The most common allegations related to paid claims were 1) “errors in diagnosis,” 2) “failure/delay in referral or consultation,” and 3) “failure to supervise/monitor case.” Although only three of the 312 claims were related to “diseases of the spinal cord,” that was exceeded in frequency only by “diabetes.”
I think these numbers from the malpractice insurance industry support my concern that SEA is a high-risk area, but it doesn’t really support my anecdotal experience that SEA is clearly hospitalists’ highest-risk area. Maybe SEA is only one of several high-risk areas. Nevertheless, I’m going to stick to my sensationalist guns to get your attention.
Why Is Epidural Abscess a High Risk?
There likely are several reasons SEA is a treacherous liability problem. It can lead to devastating permanent disabling neurologic deficits in people who were previously healthy, and if the medical care was substandard, then significant financial compensation seems appropriate.
Delays in diagnosis of SEA are common. It can be a very sneaky illness that in the early stages is very easy to confuse with less-serious causes of back pain or fever. Even though I think about this particular diagnosis all the time, just last year I had a patient who reported an increase in his usual back pain. I felt reassured that he had no neurologic deficit or fever, and took the time to explain why there was no reason to repeat the spine MRI that had been done about two weeks prior to admission. But he was insistent that he have another MRI, and after a day or two I finally agreed to order it, assuring him it would not explain the cause of his pain. But it did. He had a significant SEA and went to emergency surgery. I was stunned, and profoundly relieved that he had no neurologic sequelae.
One of the remarkable things I’ve seen in the cases I’ve reviewed is that even when there is clear cause for concern, there is too often no action taken. In a number of cases, the nurses’ note indicates increasing back pain, loss of ability to stand, urinary retention, and other alarming signs. Yet the doctors either never learn of these issues, or they choose to attribute them to other causes.
Even when the diagnosis of SEA is clearly established, it is all too common for doctors caring for the patient not to act on this information. In several cases I reviewed, a radiologist had documented reporting the diagnosis to the hospitalist (and in one case the neurosurgeon as well), yet nothing was done for 12 hours or more. It is hard to imagine that establishing this diagnosis doesn’t reliably lead to an emergent response, but it doesn’t. (In some cases, nonsurgical management may be an option, but in these malpractices cases, there was just a failure to act on the diagnosis with any sort of plan.)
Practice Management Perspective
I usually discuss hospitalist practice operations in this space—things like work schedules and compensation. But attending to risk management is one component of effective practice operations, so I thought I’d raise the topic here. Obviously, there is a lot more to hospitalist risk management than one diagnosis, but a column on the whole universe of risk management would probably serve no purpose other than as a sleep aid. I hope that by focusing solely on SEA, there is some chance that you’ll remember it, and you’ll make sure that you disprove my first two sentences.
Lowering your risk of a malpractice lawsuit is valuable and worth spending time on. But far more important is that by keeping the diagnosis in mind, and ensuring that you act emergently when there is cause for concern, you might save someone from the devastating consequences of this disease.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Delayed diagnosis of, or treatment for, a spinal epidural abscess (SEA): that will be the case over which you are sued.
Over the last 15 years, I’ve served as an expert witness for six or seven malpractice cases. Most were related to spinal cord injuries, and in all but one of those, the etiology was epidural abscess. I’ve been asked to review about 40 or 50 additional cases, and while I’ve turned them down (I just don’t have time to do reviews), I nearly always ask about the clinical picture in every case. A significant number have been SEA-related. This experience has convinced me that SEA poses a particular liability risk for hospitalists.
Of course, it is patients who bear the real risk and unfortunate consequences of SEA. Being a defendant physician in a lawsuit is stressful, but it’s nothing compared to the distress of permanent loss of neurologic function. To prevent permanent sequelae, we need to maintain a very high index of suspicion to try to make a prompt diagnosis, and ensure immediate intervention once the diagnosis is made.
Data from Malpractice Insurers
I had the pleasure of getting to know a number of leaders at The Doctor’s Company, a large malpractice insurer that provides malpractice policies for all specialties, including a lot of hospitalists. From 2007 to 2011, they closed 28 SEA-related claims, for which they spent an average of $212,000 defending each one. Eleven of the 28 resulted in indemnity payments averaging $754,000 each (median was $455,000). These dollar amounts are roughly double what might be seen for all other claims and reflect only the payments made on behalf of the company’s insured doctors. The total award to each patient was likely much higher, because in most cases, several defendants (other doctors and a hospital) probably paid money to the patient.
The Physician Insurers Association of America (PIAA) “is the insurance industry trade association representing domestic and international medical professional liability insurance companies.” Their member malpractice insurance companies have the opportunity to report claims data that PIAA aggregates and makes available. Data from 2002 to 2011 showed 312 closed claims related to any diagnosis (not just SEA) for hospitalists, with an average indemnity payment of $272,553 (the highest hospitalist-related payment was $1.4 million). The most common allegations related to paid claims were 1) “errors in diagnosis,” 2) “failure/delay in referral or consultation,” and 3) “failure to supervise/monitor case.” Although only three of the 312 claims were related to “diseases of the spinal cord,” that was exceeded in frequency only by “diabetes.”
I think these numbers from the malpractice insurance industry support my concern that SEA is a high-risk area, but it doesn’t really support my anecdotal experience that SEA is clearly hospitalists’ highest-risk area. Maybe SEA is only one of several high-risk areas. Nevertheless, I’m going to stick to my sensationalist guns to get your attention.
Why Is Epidural Abscess a High Risk?
There likely are several reasons SEA is a treacherous liability problem. It can lead to devastating permanent disabling neurologic deficits in people who were previously healthy, and if the medical care was substandard, then significant financial compensation seems appropriate.
Delays in diagnosis of SEA are common. It can be a very sneaky illness that in the early stages is very easy to confuse with less-serious causes of back pain or fever. Even though I think about this particular diagnosis all the time, just last year I had a patient who reported an increase in his usual back pain. I felt reassured that he had no neurologic deficit or fever, and took the time to explain why there was no reason to repeat the spine MRI that had been done about two weeks prior to admission. But he was insistent that he have another MRI, and after a day or two I finally agreed to order it, assuring him it would not explain the cause of his pain. But it did. He had a significant SEA and went to emergency surgery. I was stunned, and profoundly relieved that he had no neurologic sequelae.
One of the remarkable things I’ve seen in the cases I’ve reviewed is that even when there is clear cause for concern, there is too often no action taken. In a number of cases, the nurses’ note indicates increasing back pain, loss of ability to stand, urinary retention, and other alarming signs. Yet the doctors either never learn of these issues, or they choose to attribute them to other causes.
Even when the diagnosis of SEA is clearly established, it is all too common for doctors caring for the patient not to act on this information. In several cases I reviewed, a radiologist had documented reporting the diagnosis to the hospitalist (and in one case the neurosurgeon as well), yet nothing was done for 12 hours or more. It is hard to imagine that establishing this diagnosis doesn’t reliably lead to an emergent response, but it doesn’t. (In some cases, nonsurgical management may be an option, but in these malpractices cases, there was just a failure to act on the diagnosis with any sort of plan.)
Practice Management Perspective
I usually discuss hospitalist practice operations in this space—things like work schedules and compensation. But attending to risk management is one component of effective practice operations, so I thought I’d raise the topic here. Obviously, there is a lot more to hospitalist risk management than one diagnosis, but a column on the whole universe of risk management would probably serve no purpose other than as a sleep aid. I hope that by focusing solely on SEA, there is some chance that you’ll remember it, and you’ll make sure that you disprove my first two sentences.
Lowering your risk of a malpractice lawsuit is valuable and worth spending time on. But far more important is that by keeping the diagnosis in mind, and ensuring that you act emergently when there is cause for concern, you might save someone from the devastating consequences of this disease.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
John Nelson, MD: A New Hospitalist
Ben was just accepted to med school!!! Hopefully, more acceptances will be forthcoming. We are very proud of Ben for all his hard work. Another doctor in the family.
I was delighted to find the above message from an old friend in my inbox. It got me thinking: Will Ben become a hospitalist? Will he join his dad’s hospitalist group? Will his dad encourage him to pursue a hospitalist career or something else?
Early Hospitalist Practice
The author of that email was Ben’s dad, Chuck Wilson. Chuck is the reason I’m a hospitalist. He was a year ahead of me in residency, and while still a resident, he somehow connected with a really busy family physician in town who was looking for someone to manage his hospital patients. Not one to be bound by convention, Chuck agreed to what was at the time a nearly unheard-of arrangement. He finished residency, joined the staff of the community hospital across town from our residency, and began caring for the family physician’s hospital patients. Within days, he was fielding calls from other doctors asking him to do the same for them. Within weeks of arriving, he had begun accepting essentially all unassigned medical admissions from the ED. This was in the 1980s; Chuck was among the nation’s first real hospitalists.
I don’t think Chuck spent any time worrying about how his practice was so different from the traditional internists and family physicians in the community. He was confident he was providing a valuable service to his patients and the medical community. The rapid growth in his patient census was an indicator he was on to something, and soon he and I began talking. He was looking for a partner.
In November of my third year of residency, I decided I would put off my endocrinology fellowship for a year or two and join Chuck in his new practice. From our conversations, I anticipated that I would care for exactly the kinds of patients that filled nearly all of my time as a resident. I wouldn’t need to learn the new skills in ambulatory medicine, and wouldn’t need to make the long-term commitment expected to join a traditional primary-care practice. And I would earn a competitive compensation and have a flexible lifestyle. I soon realized that hospitalist practice provided me with all of these advantages, so more than two decades later, I still haven’t gotten around to completing the application for an endocrine fellowship.
A Loose Arrangement
For the first few years, Chuck and I didn’t bother to have any sort of legal agreement with each other. We shook hands and agreed to a “reap what you till” form of compensation, which meant we didn’t have to work exactly the same amount, and never had disagreements about how practice revenue was divided between us.
Because of Chuck’s influence, we had miniscule overhead expenses, most likely less than 10% of revenue. We each bought our own malpractice insurance, paid our biller a percent of collections, and rented a pager. That was about it for overhead.
We had no rigid scheduling algorithm, the only requirement being that at least one of us needed to be working every day. Both of us worked most weekdays, but we took time off whenever it suited us. Our scheduling meetings were usually held when we bumped into one another while rounding and went something like this:
“You OK if I take five days off starting tomorrow?”
“Sure. That’s fine.”
Meeting adjourned.
For years, we had no official name for our practice. This became a bigger issue when our group had grown to four doctors, so we defaulted to referring to the group by the first letter of the last name of each doctor, in order of tenure: The WNKL Group. A more formal name was to follow a few years later when the group was even larger, but I’ve taken delight in hearing that WNKL has persisted in some places and documents around the hospital years later, even though N, K, and L left the group long ago.
In the first few years, we never thought about developing clinical protocols or measuring our efficiency or clinical effectiveness. Chuck was confident that compared to the traditional primary-care model, we were providing higher-quality care at a lower cost. But I wasn’t so sure. After a few years, we began seeing hospital data showing that our cost per case tended to be lower, and what little data we could get regarding our quality of care suggested that it was about the same, and in some cases might be better.
A principal reason the practice has survived more than 25 years is that other than a small “tax” during their first 18 months (mainly to cover the cost of recruiting them), new doctors were regarded as equals in the business. Chuck and subsequent doctors never tried to gain an advantage over newer doctors by trying to claim a greater share of the practice’s revenue or decision-making authority.
Chuck is still in the same group he founded. In 2000, I was lured away by the chance to start a new group and live in a place that both my wife and I love. He and I have enjoyed watching our field grow up, and we take satisfaction in our roles in its evolution.
Lessons Learned
The hospitalist model of practice didn’t have a single inventor or place of origin, and anyone involved in starting a practice in the 1980s or before should be proud to have invented their practice when no blueprint existed. Creative thinking and openness to a new way of doing things were critical in developing the first hospitalist practices. They also are useful traits in trying to improve modern hospitalist practices or other segments of our healthcare system.
Like many new developments in medicine, the economic effects of our practice—lower hospital cost per case—became apparent, especially to Chuck, before data regarding quality surfaced. I wish we had gotten more serious early on about capturing whatever quality data might have been available—clearly less than what is available today—and those in new healthcare endeavors today should try to measure quality at the outset. Unlike the 1980s, the current marketplace will help ensure that happens.
Coda
There is one other really cool thing about Chuck’s email at the beginning of this column: those three exclamation points! Chuck is typically laconic and understated, and not given to such displays of emotion, but there are few things that generate more enthusiasm than a parent sharing news of a child’s success.
So, Ben, as you start med school next year, I wish you the best. You can be sure I’ll be asking for updates about your progress. The most important thing is that you find a life and career that engages you to do good work for others and provides satisfaction. And whatever you choose to do after med school, I know you’ll continue to make your parents proud.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Ben was just accepted to med school!!! Hopefully, more acceptances will be forthcoming. We are very proud of Ben for all his hard work. Another doctor in the family.
I was delighted to find the above message from an old friend in my inbox. It got me thinking: Will Ben become a hospitalist? Will he join his dad’s hospitalist group? Will his dad encourage him to pursue a hospitalist career or something else?
Early Hospitalist Practice
The author of that email was Ben’s dad, Chuck Wilson. Chuck is the reason I’m a hospitalist. He was a year ahead of me in residency, and while still a resident, he somehow connected with a really busy family physician in town who was looking for someone to manage his hospital patients. Not one to be bound by convention, Chuck agreed to what was at the time a nearly unheard-of arrangement. He finished residency, joined the staff of the community hospital across town from our residency, and began caring for the family physician’s hospital patients. Within days, he was fielding calls from other doctors asking him to do the same for them. Within weeks of arriving, he had begun accepting essentially all unassigned medical admissions from the ED. This was in the 1980s; Chuck was among the nation’s first real hospitalists.
I don’t think Chuck spent any time worrying about how his practice was so different from the traditional internists and family physicians in the community. He was confident he was providing a valuable service to his patients and the medical community. The rapid growth in his patient census was an indicator he was on to something, and soon he and I began talking. He was looking for a partner.
In November of my third year of residency, I decided I would put off my endocrinology fellowship for a year or two and join Chuck in his new practice. From our conversations, I anticipated that I would care for exactly the kinds of patients that filled nearly all of my time as a resident. I wouldn’t need to learn the new skills in ambulatory medicine, and wouldn’t need to make the long-term commitment expected to join a traditional primary-care practice. And I would earn a competitive compensation and have a flexible lifestyle. I soon realized that hospitalist practice provided me with all of these advantages, so more than two decades later, I still haven’t gotten around to completing the application for an endocrine fellowship.
A Loose Arrangement
For the first few years, Chuck and I didn’t bother to have any sort of legal agreement with each other. We shook hands and agreed to a “reap what you till” form of compensation, which meant we didn’t have to work exactly the same amount, and never had disagreements about how practice revenue was divided between us.
Because of Chuck’s influence, we had miniscule overhead expenses, most likely less than 10% of revenue. We each bought our own malpractice insurance, paid our biller a percent of collections, and rented a pager. That was about it for overhead.
We had no rigid scheduling algorithm, the only requirement being that at least one of us needed to be working every day. Both of us worked most weekdays, but we took time off whenever it suited us. Our scheduling meetings were usually held when we bumped into one another while rounding and went something like this:
“You OK if I take five days off starting tomorrow?”
“Sure. That’s fine.”
Meeting adjourned.
For years, we had no official name for our practice. This became a bigger issue when our group had grown to four doctors, so we defaulted to referring to the group by the first letter of the last name of each doctor, in order of tenure: The WNKL Group. A more formal name was to follow a few years later when the group was even larger, but I’ve taken delight in hearing that WNKL has persisted in some places and documents around the hospital years later, even though N, K, and L left the group long ago.
In the first few years, we never thought about developing clinical protocols or measuring our efficiency or clinical effectiveness. Chuck was confident that compared to the traditional primary-care model, we were providing higher-quality care at a lower cost. But I wasn’t so sure. After a few years, we began seeing hospital data showing that our cost per case tended to be lower, and what little data we could get regarding our quality of care suggested that it was about the same, and in some cases might be better.
A principal reason the practice has survived more than 25 years is that other than a small “tax” during their first 18 months (mainly to cover the cost of recruiting them), new doctors were regarded as equals in the business. Chuck and subsequent doctors never tried to gain an advantage over newer doctors by trying to claim a greater share of the practice’s revenue or decision-making authority.
Chuck is still in the same group he founded. In 2000, I was lured away by the chance to start a new group and live in a place that both my wife and I love. He and I have enjoyed watching our field grow up, and we take satisfaction in our roles in its evolution.
Lessons Learned
The hospitalist model of practice didn’t have a single inventor or place of origin, and anyone involved in starting a practice in the 1980s or before should be proud to have invented their practice when no blueprint existed. Creative thinking and openness to a new way of doing things were critical in developing the first hospitalist practices. They also are useful traits in trying to improve modern hospitalist practices or other segments of our healthcare system.
Like many new developments in medicine, the economic effects of our practice—lower hospital cost per case—became apparent, especially to Chuck, before data regarding quality surfaced. I wish we had gotten more serious early on about capturing whatever quality data might have been available—clearly less than what is available today—and those in new healthcare endeavors today should try to measure quality at the outset. Unlike the 1980s, the current marketplace will help ensure that happens.
Coda
There is one other really cool thing about Chuck’s email at the beginning of this column: those three exclamation points! Chuck is typically laconic and understated, and not given to such displays of emotion, but there are few things that generate more enthusiasm than a parent sharing news of a child’s success.
So, Ben, as you start med school next year, I wish you the best. You can be sure I’ll be asking for updates about your progress. The most important thing is that you find a life and career that engages you to do good work for others and provides satisfaction. And whatever you choose to do after med school, I know you’ll continue to make your parents proud.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Ben was just accepted to med school!!! Hopefully, more acceptances will be forthcoming. We are very proud of Ben for all his hard work. Another doctor in the family.
I was delighted to find the above message from an old friend in my inbox. It got me thinking: Will Ben become a hospitalist? Will he join his dad’s hospitalist group? Will his dad encourage him to pursue a hospitalist career or something else?
Early Hospitalist Practice
The author of that email was Ben’s dad, Chuck Wilson. Chuck is the reason I’m a hospitalist. He was a year ahead of me in residency, and while still a resident, he somehow connected with a really busy family physician in town who was looking for someone to manage his hospital patients. Not one to be bound by convention, Chuck agreed to what was at the time a nearly unheard-of arrangement. He finished residency, joined the staff of the community hospital across town from our residency, and began caring for the family physician’s hospital patients. Within days, he was fielding calls from other doctors asking him to do the same for them. Within weeks of arriving, he had begun accepting essentially all unassigned medical admissions from the ED. This was in the 1980s; Chuck was among the nation’s first real hospitalists.
I don’t think Chuck spent any time worrying about how his practice was so different from the traditional internists and family physicians in the community. He was confident he was providing a valuable service to his patients and the medical community. The rapid growth in his patient census was an indicator he was on to something, and soon he and I began talking. He was looking for a partner.
In November of my third year of residency, I decided I would put off my endocrinology fellowship for a year or two and join Chuck in his new practice. From our conversations, I anticipated that I would care for exactly the kinds of patients that filled nearly all of my time as a resident. I wouldn’t need to learn the new skills in ambulatory medicine, and wouldn’t need to make the long-term commitment expected to join a traditional primary-care practice. And I would earn a competitive compensation and have a flexible lifestyle. I soon realized that hospitalist practice provided me with all of these advantages, so more than two decades later, I still haven’t gotten around to completing the application for an endocrine fellowship.
A Loose Arrangement
For the first few years, Chuck and I didn’t bother to have any sort of legal agreement with each other. We shook hands and agreed to a “reap what you till” form of compensation, which meant we didn’t have to work exactly the same amount, and never had disagreements about how practice revenue was divided between us.
Because of Chuck’s influence, we had miniscule overhead expenses, most likely less than 10% of revenue. We each bought our own malpractice insurance, paid our biller a percent of collections, and rented a pager. That was about it for overhead.
We had no rigid scheduling algorithm, the only requirement being that at least one of us needed to be working every day. Both of us worked most weekdays, but we took time off whenever it suited us. Our scheduling meetings were usually held when we bumped into one another while rounding and went something like this:
“You OK if I take five days off starting tomorrow?”
“Sure. That’s fine.”
Meeting adjourned.
For years, we had no official name for our practice. This became a bigger issue when our group had grown to four doctors, so we defaulted to referring to the group by the first letter of the last name of each doctor, in order of tenure: The WNKL Group. A more formal name was to follow a few years later when the group was even larger, but I’ve taken delight in hearing that WNKL has persisted in some places and documents around the hospital years later, even though N, K, and L left the group long ago.
In the first few years, we never thought about developing clinical protocols or measuring our efficiency or clinical effectiveness. Chuck was confident that compared to the traditional primary-care model, we were providing higher-quality care at a lower cost. But I wasn’t so sure. After a few years, we began seeing hospital data showing that our cost per case tended to be lower, and what little data we could get regarding our quality of care suggested that it was about the same, and in some cases might be better.
A principal reason the practice has survived more than 25 years is that other than a small “tax” during their first 18 months (mainly to cover the cost of recruiting them), new doctors were regarded as equals in the business. Chuck and subsequent doctors never tried to gain an advantage over newer doctors by trying to claim a greater share of the practice’s revenue or decision-making authority.
Chuck is still in the same group he founded. In 2000, I was lured away by the chance to start a new group and live in a place that both my wife and I love. He and I have enjoyed watching our field grow up, and we take satisfaction in our roles in its evolution.
Lessons Learned
The hospitalist model of practice didn’t have a single inventor or place of origin, and anyone involved in starting a practice in the 1980s or before should be proud to have invented their practice when no blueprint existed. Creative thinking and openness to a new way of doing things were critical in developing the first hospitalist practices. They also are useful traits in trying to improve modern hospitalist practices or other segments of our healthcare system.
Like many new developments in medicine, the economic effects of our practice—lower hospital cost per case—became apparent, especially to Chuck, before data regarding quality surfaced. I wish we had gotten more serious early on about capturing whatever quality data might have been available—clearly less than what is available today—and those in new healthcare endeavors today should try to measure quality at the outset. Unlike the 1980s, the current marketplace will help ensure that happens.
Coda
There is one other really cool thing about Chuck’s email at the beginning of this column: those three exclamation points! Chuck is typically laconic and understated, and not given to such displays of emotion, but there are few things that generate more enthusiasm than a parent sharing news of a child’s success.
So, Ben, as you start med school next year, I wish you the best. You can be sure I’ll be asking for updates about your progress. The most important thing is that you find a life and career that engages you to do good work for others and provides satisfaction. And whatever you choose to do after med school, I know you’ll continue to make your parents proud.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
John Nelson: Peformance Key to Federal Value-Based Payment Modifier Plan
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
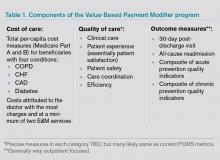
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
For years, your hospital was paid additional money by Medicare to report its performance on such things as core measures. Medicare then shared that information with the public via www.hospitalcompare.hhs.gov. Even if the hospital never gave Pneumovax when indicated, it was paid more simply for reporting that fact. (Fortunately, there were lots of reasons hospitals wanted to perform well.)
The days of hospitals being paid more simply for reporting ended a long time ago. Now performance, e.g., how often Pneumovax was given when indicated, influences payment. That is, things have transitioned from pay-for-reporting to a pay-for-performance program called hospital value-based purchasing (VBP).
I hope that at least one member of your hospitalist group is keeping up with hospital VBP. It got a lot of attention in the fall because it was the first time Medicare Part A payments to hospitals were adjusted based on performance on some core measures and patient satisfaction domains, as well as readmission rates for congestive heart failure (CHF), acute myocardial infarction (AMI), and pneumonia patients. The dollars at stake and performance metrics change will change every year, so plan to pay attention to hospital VBP on an ongoing basis.
Physicians’ Turn
Medicare payment to physicians is evolving along the same trajectory as hospitals. For several years, doctors have had the option to voluntarily participate in the Physician Quality Reporting System (PQRS). As long as a doctor reported quality performance on a sufficient portion of certain patient types, Medicare would provide a “bonus” at the end of the year. From 2012 through 2014, the “bonus” is 0.5% of that doctor’s total allowable Medicare charges. For example, if that doctor generated $150,000 of Medicare allowable charges over the calendar year, the additional payment for successful reporting PQRS would be $750 (0.5% of $150,000).
Although $750 is only a tiny fraction of collections, the right charge-capture system can make it pretty easy to achieve. And an extra payment of $750 sure is better than the 1.5% penalty for not participating; that program starts in 2015 and increases to a 2% penalty in 2016. If you are still not participating successfully in PQRS in 2015, the reimbursement for that $150,000 in charges will be reduced by $2,250 (1.5% of $150,000). So I strongly recommend that you begin reporting in 2013 so that you have time to work out the kinks well ahead of 2015. Don’t delay, but don’t panic, either, because you can still succeed in 2013 even if you don’t start capturing or reporting PQRS data until late winter or early spring.
At some point in the next year or so, data from as early as January 2013 for doctors reporting through PQRS will be made public on the Centers for Medicare & Medicaid’s (CMS) physician compare website: www.medicare.gov/find-a-doctor/provider-search.aspx. For example, should you choose to report the portion of stroke patients for whom you prescribed DVT prophylaxis, the public will be able to see your data.
The Next Wave of Physician Pay for Performance
As the name implies, PQRS is a program based on reporting. Now CMS is adding the Value-Based Payment Modifier (VBPM) program, in which performance determines payments (see Table 1). It incorporates quality measures from PQRS, but is for now a separate program. It is very similar in name and structure to the hospital VBP program mentioned above, but incorporates cost of care data as well as quality performance. So it is really about value and not just quality performance (hence the name).
For providers in groups of more than 100 that bill under the same tax ID number (they don’t have to be in the same specialty), VBPM will first influence Part B Medicare reimbursement for physician services in 2015. It will expand to include all providers in 2017.
But don’t think you have until 2015 or 2017 to learn about all of this. There is a two-year lag, so payments in 2015 are based on performance in 2013 and 2017 payments presumably will be based on 2015 performance. In the fall of 2013, CMS plans to provide group-level (not individual) performance reports to all doctors in groups of 100 or more under the same tax ID number. These performance reports are known as quality resource use reports (QRURs). QRURs were trialed on physicians in a few states who received reports in 2012 based on 2011 performance, but in 2013, reports based on 2012 performance will be distributed to all doctors who practice in groups of 100 or more.
The calculation to determine whether a doctor is due additional payment for good performance (more accurately, good value) is awfully complicated. But providers have a choice to make. They can choose to:
- Not report data and accept a 1% penalty (likely to increase in successive years and in addition to the penalty for not reporting PQRS data, for a total penalty of 2.5%);
- Report data but not compete for financial upside or downside; or
- Compete for additional payments (amount to be determined) and risk a penalty of 0.5% or 1% for poor performance.
Look for more details about the VBPM program in future columns and other articles in The Hospitalist. There are a number of good online resources, including a CMS presentation titled “CMS Proposals for the Physician Value-Based Payment Modifier under the Medicare Physician Fee Schedule.” Type “Value-Based Payment Modifier” and “CMS” into any search engine to locate the video.
Parting Recommendations
Just about every hospitalist group should:
- Designate someone in your group to keep up with evolving pay-for-performance programs. It doesn’t have to be an MD, but you do need someone local that can guide your group through it. Consider becoming the most expert physician at your hospital on this topic.
- Start reporting through PQRS in 2013 if you haven’t already.
- Support SHM’s efforts to provide feedback to CMS to ensure that the metrics are meaningful for the type of care we provide.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Author’s note: For helping to explain all this pay-for-performance stuff, I once again owe thanks to Dr. Pat Torcson, a hospitalist in Covington, La., and member of SHM’s Public Policy Committee. He does an amazing job of keeping up with the evolving pay-for-performance programs, advocating on behalf of hospitalists and the patients we serve, and graciously answers my tedious questions with thoughtful and informative replies. He is a really pleasant guy and a terrific asset to SHM and hospital medicine.
John Nelson: Learning CPT Coding and Documentation Tricky for Hospitalists
There is a lot to learn when it comes to proper coding and the documentation requirements that go with it. It can even be tricky for a new residency grad to keep the difference in CPT and ICD-9 coding straight, to say nothing of the difference between documentation requirements for physician reimbursement versus hospital reimbursement. This column addresses only physician CPT coding (I’ll save documentation to support hospital billing for another column).
Although I believe that devoting the large number of brain cells required to keep this stuff straight gets in the way of maintaining necessary clinical knowledge, physicians have no real choice but to do it. (One could argue that having a professional coder read charts to determine proper CPT codes relieves a doctor of the burden of documentation and coding headaches. But this is only partially true. The doctor still needs to ensure that the documentation accurately reflects what was done for the coder to be able to select the appropriate codes, so he still needs to know a lot about this topic.)
All providers have a duty to reasonably ensure that submitted claims (bills) are true and accurate. Failing to document and code correctly risks anything from you or your employer having to return money, potentially with a penalty and interest, to being accused of criminal fraud.
Medicare and other payors generally categorize inaccurate claims as follows:
- Erroneous claims include inadvertent mistakes, innocent errors, or even negligence but still require payments associated with the error to be returned.
- Fraudulent claims are ones judged to be intentionally or recklessly false, and are subject to administrative or civil penalties, such as fines.
- Claims associated with criminal intent to defraud are subject to criminal penalties, which could include jail time.
While I haven’t heard of any hospitalists being accused of fraud, I know of several who have undergone audits and been required to return money. Whether your employer would refund the money or you would have to write a personal check to refund the money depends on your employment situation. For example, in most cases, the hospital would be liable to make the repayment for hospitalists it employs. If you’re an independent contractor, there is a good chance you could be stuck making the repayment yourself.
Trend: Increased Use of Higher-Level Codes
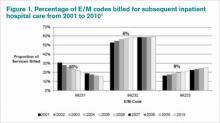
You might have missed it, but there was a recent study of Medicare Part B claims data from 2001 to 2010 showing that “physicians increased their billing of higher-level E/M codes in all types of E/M services.”1 For example, the report showed a steady decrease in use of the 99231 code, the lowest of the three subsequent inpatient hospital care codes, and an increase in the highest level code, 99233 (see Figure 1, below).
I can think of two reasons hospitalists might be increasing the use of higher codes. One, less-sick patients just aren’t seen in the hospital as often as they used to be, so the remaining patients require more intensive services, which could lead to the appropriate use of higher-level codes. Two, doctors have over the past 10 to 15 years invested more energy in learning appropriate documentation and coding, which might have led to correcting historical overuse of lower-level codes.
Did I tell you who conducted the study showing increased use of higher-level codes? It was the federal Office of Inspector General (OIG), which is responsible for preventing and detecting fraud and waste. Although the OIG might agree that the sicker patients and correction of historical undercoding might explain some of the trend, it’s a pretty safe bet they’re also concerned that a significant portion is inappropriate or fraudulent. Some portion of it probably is.
“CMS concurred with [OIG’s] recommendations to (1) continue to educate physicians on proper billing for E/M services and (2) encourage its contractor to review physicians’ billing for E/M services. CMS partially concurred with [OIG’s] third recommendation, to review physicians who bill higher-level E/M codes for appropriate action,” the OIG report noted.1
Plan for Education, Compliance
My sense is that most hospitalists employed by a large entity, such as a hospital or large medical group, have access to a certified coder to perform documentation and coding audits, as well as educational feedback when needed. If your practice doesn’t have access to a certified coder, you should consider photocopying some chart notes (e.g. 10 notes from each of your docs) and send them to an outside coder for an audit. Though they are very valuable, audits usually are not enough to ensure good performance.
In my March 2007 column, I described a reasonably simple chart audit allowing each doctor to compare his or her CPT coding pattern to everyone else in the group. You can compare your own coding to national coding patterns via SHM’s 2012 State of Hospital Medicine Report (www.hospitalmedicine.org/survey) or data from the CMS website, and the Medical Group Management Association (MGMA) will have data in future surveys. Such comparisons might help uncover unusual patterns that are worthy of a closer look.
Other strategies to promote proper documentation and coding include online educational programs, such as:
- SHM’s CODE-H webinars (www.hospitalmedicine.org/codeh), which are available on demand for a fee;
- American Association of Professional Coders Evaluation and Management Online Training (http://www.aapc.com/training/evaluation-management-coding-training.aspx); and
- The American Health Information Management Association’s (AHIMA) Coding Basics Program (www.ahima.org/continuinged/campus/courseinfo/cb.aspx).
If you prefer, an Internet search can turn up in-person courses to learn documentation and coding. Additionally, your in-house or external coding auditors can provide training.
To address tricky issues that come up only occasionally, several in our practice have compiled a “coding manual” by distilling guidance from our certified coders and compliance people on issues as they came up. Some issues would stump all of us, and we’d have to go to the Internet for help. All hospitalists are provided with a copy of the manual during orientation, and an electronic copy is available on the hospital’s Intranet. Topics addressed in the manual include things like how to bill the first inpatient day when a patient has changed from observation status, how to bill initial consult visits for various payors (an issue since Medicare eliminated consult codes a few years ago), how to bill when a patient is seen and discharged from the ED, etc.
Lastly, I suggest someone in your group talk with your hospital’s compliance department about its own coding and billing compliance plan. This could lead to ideas or help develop a compliance plan for your group.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Reference
There is a lot to learn when it comes to proper coding and the documentation requirements that go with it. It can even be tricky for a new residency grad to keep the difference in CPT and ICD-9 coding straight, to say nothing of the difference between documentation requirements for physician reimbursement versus hospital reimbursement. This column addresses only physician CPT coding (I’ll save documentation to support hospital billing for another column).
Although I believe that devoting the large number of brain cells required to keep this stuff straight gets in the way of maintaining necessary clinical knowledge, physicians have no real choice but to do it. (One could argue that having a professional coder read charts to determine proper CPT codes relieves a doctor of the burden of documentation and coding headaches. But this is only partially true. The doctor still needs to ensure that the documentation accurately reflects what was done for the coder to be able to select the appropriate codes, so he still needs to know a lot about this topic.)
All providers have a duty to reasonably ensure that submitted claims (bills) are true and accurate. Failing to document and code correctly risks anything from you or your employer having to return money, potentially with a penalty and interest, to being accused of criminal fraud.
Medicare and other payors generally categorize inaccurate claims as follows:
- Erroneous claims include inadvertent mistakes, innocent errors, or even negligence but still require payments associated with the error to be returned.
- Fraudulent claims are ones judged to be intentionally or recklessly false, and are subject to administrative or civil penalties, such as fines.
- Claims associated with criminal intent to defraud are subject to criminal penalties, which could include jail time.
While I haven’t heard of any hospitalists being accused of fraud, I know of several who have undergone audits and been required to return money. Whether your employer would refund the money or you would have to write a personal check to refund the money depends on your employment situation. For example, in most cases, the hospital would be liable to make the repayment for hospitalists it employs. If you’re an independent contractor, there is a good chance you could be stuck making the repayment yourself.
Trend: Increased Use of Higher-Level Codes
You might have missed it, but there was a recent study of Medicare Part B claims data from 2001 to 2010 showing that “physicians increased their billing of higher-level E/M codes in all types of E/M services.”1 For example, the report showed a steady decrease in use of the 99231 code, the lowest of the three subsequent inpatient hospital care codes, and an increase in the highest level code, 99233 (see Figure 1, below).
I can think of two reasons hospitalists might be increasing the use of higher codes. One, less-sick patients just aren’t seen in the hospital as often as they used to be, so the remaining patients require more intensive services, which could lead to the appropriate use of higher-level codes. Two, doctors have over the past 10 to 15 years invested more energy in learning appropriate documentation and coding, which might have led to correcting historical overuse of lower-level codes.
Did I tell you who conducted the study showing increased use of higher-level codes? It was the federal Office of Inspector General (OIG), which is responsible for preventing and detecting fraud and waste. Although the OIG might agree that the sicker patients and correction of historical undercoding might explain some of the trend, it’s a pretty safe bet they’re also concerned that a significant portion is inappropriate or fraudulent. Some portion of it probably is.
“CMS concurred with [OIG’s] recommendations to (1) continue to educate physicians on proper billing for E/M services and (2) encourage its contractor to review physicians’ billing for E/M services. CMS partially concurred with [OIG’s] third recommendation, to review physicians who bill higher-level E/M codes for appropriate action,” the OIG report noted.1
Plan for Education, Compliance
My sense is that most hospitalists employed by a large entity, such as a hospital or large medical group, have access to a certified coder to perform documentation and coding audits, as well as educational feedback when needed. If your practice doesn’t have access to a certified coder, you should consider photocopying some chart notes (e.g. 10 notes from each of your docs) and send them to an outside coder for an audit. Though they are very valuable, audits usually are not enough to ensure good performance.
In my March 2007 column, I described a reasonably simple chart audit allowing each doctor to compare his or her CPT coding pattern to everyone else in the group. You can compare your own coding to national coding patterns via SHM’s 2012 State of Hospital Medicine Report (www.hospitalmedicine.org/survey) or data from the CMS website, and the Medical Group Management Association (MGMA) will have data in future surveys. Such comparisons might help uncover unusual patterns that are worthy of a closer look.
Other strategies to promote proper documentation and coding include online educational programs, such as:
- SHM’s CODE-H webinars (www.hospitalmedicine.org/codeh), which are available on demand for a fee;
- American Association of Professional Coders Evaluation and Management Online Training (http://www.aapc.com/training/evaluation-management-coding-training.aspx); and
- The American Health Information Management Association’s (AHIMA) Coding Basics Program (www.ahima.org/continuinged/campus/courseinfo/cb.aspx).
If you prefer, an Internet search can turn up in-person courses to learn documentation and coding. Additionally, your in-house or external coding auditors can provide training.
To address tricky issues that come up only occasionally, several in our practice have compiled a “coding manual” by distilling guidance from our certified coders and compliance people on issues as they came up. Some issues would stump all of us, and we’d have to go to the Internet for help. All hospitalists are provided with a copy of the manual during orientation, and an electronic copy is available on the hospital’s Intranet. Topics addressed in the manual include things like how to bill the first inpatient day when a patient has changed from observation status, how to bill initial consult visits for various payors (an issue since Medicare eliminated consult codes a few years ago), how to bill when a patient is seen and discharged from the ED, etc.
Lastly, I suggest someone in your group talk with your hospital’s compliance department about its own coding and billing compliance plan. This could lead to ideas or help develop a compliance plan for your group.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Reference
There is a lot to learn when it comes to proper coding and the documentation requirements that go with it. It can even be tricky for a new residency grad to keep the difference in CPT and ICD-9 coding straight, to say nothing of the difference between documentation requirements for physician reimbursement versus hospital reimbursement. This column addresses only physician CPT coding (I’ll save documentation to support hospital billing for another column).
Although I believe that devoting the large number of brain cells required to keep this stuff straight gets in the way of maintaining necessary clinical knowledge, physicians have no real choice but to do it. (One could argue that having a professional coder read charts to determine proper CPT codes relieves a doctor of the burden of documentation and coding headaches. But this is only partially true. The doctor still needs to ensure that the documentation accurately reflects what was done for the coder to be able to select the appropriate codes, so he still needs to know a lot about this topic.)
All providers have a duty to reasonably ensure that submitted claims (bills) are true and accurate. Failing to document and code correctly risks anything from you or your employer having to return money, potentially with a penalty and interest, to being accused of criminal fraud.
Medicare and other payors generally categorize inaccurate claims as follows:
- Erroneous claims include inadvertent mistakes, innocent errors, or even negligence but still require payments associated with the error to be returned.
- Fraudulent claims are ones judged to be intentionally or recklessly false, and are subject to administrative or civil penalties, such as fines.
- Claims associated with criminal intent to defraud are subject to criminal penalties, which could include jail time.
While I haven’t heard of any hospitalists being accused of fraud, I know of several who have undergone audits and been required to return money. Whether your employer would refund the money or you would have to write a personal check to refund the money depends on your employment situation. For example, in most cases, the hospital would be liable to make the repayment for hospitalists it employs. If you’re an independent contractor, there is a good chance you could be stuck making the repayment yourself.
Trend: Increased Use of Higher-Level Codes
You might have missed it, but there was a recent study of Medicare Part B claims data from 2001 to 2010 showing that “physicians increased their billing of higher-level E/M codes in all types of E/M services.”1 For example, the report showed a steady decrease in use of the 99231 code, the lowest of the three subsequent inpatient hospital care codes, and an increase in the highest level code, 99233 (see Figure 1, below).
I can think of two reasons hospitalists might be increasing the use of higher codes. One, less-sick patients just aren’t seen in the hospital as often as they used to be, so the remaining patients require more intensive services, which could lead to the appropriate use of higher-level codes. Two, doctors have over the past 10 to 15 years invested more energy in learning appropriate documentation and coding, which might have led to correcting historical overuse of lower-level codes.
Did I tell you who conducted the study showing increased use of higher-level codes? It was the federal Office of Inspector General (OIG), which is responsible for preventing and detecting fraud and waste. Although the OIG might agree that the sicker patients and correction of historical undercoding might explain some of the trend, it’s a pretty safe bet they’re also concerned that a significant portion is inappropriate or fraudulent. Some portion of it probably is.
“CMS concurred with [OIG’s] recommendations to (1) continue to educate physicians on proper billing for E/M services and (2) encourage its contractor to review physicians’ billing for E/M services. CMS partially concurred with [OIG’s] third recommendation, to review physicians who bill higher-level E/M codes for appropriate action,” the OIG report noted.1
Plan for Education, Compliance
My sense is that most hospitalists employed by a large entity, such as a hospital or large medical group, have access to a certified coder to perform documentation and coding audits, as well as educational feedback when needed. If your practice doesn’t have access to a certified coder, you should consider photocopying some chart notes (e.g. 10 notes from each of your docs) and send them to an outside coder for an audit. Though they are very valuable, audits usually are not enough to ensure good performance.
In my March 2007 column, I described a reasonably simple chart audit allowing each doctor to compare his or her CPT coding pattern to everyone else in the group. You can compare your own coding to national coding patterns via SHM’s 2012 State of Hospital Medicine Report (www.hospitalmedicine.org/survey) or data from the CMS website, and the Medical Group Management Association (MGMA) will have data in future surveys. Such comparisons might help uncover unusual patterns that are worthy of a closer look.
Other strategies to promote proper documentation and coding include online educational programs, such as:
- SHM’s CODE-H webinars (www.hospitalmedicine.org/codeh), which are available on demand for a fee;
- American Association of Professional Coders Evaluation and Management Online Training (http://www.aapc.com/training/evaluation-management-coding-training.aspx); and
- The American Health Information Management Association’s (AHIMA) Coding Basics Program (www.ahima.org/continuinged/campus/courseinfo/cb.aspx).
If you prefer, an Internet search can turn up in-person courses to learn documentation and coding. Additionally, your in-house or external coding auditors can provide training.
To address tricky issues that come up only occasionally, several in our practice have compiled a “coding manual” by distilling guidance from our certified coders and compliance people on issues as they came up. Some issues would stump all of us, and we’d have to go to the Internet for help. All hospitalists are provided with a copy of the manual during orientation, and an electronic copy is available on the hospital’s Intranet. Topics addressed in the manual include things like how to bill the first inpatient day when a patient has changed from observation status, how to bill initial consult visits for various payors (an issue since Medicare eliminated consult codes a few years ago), how to bill when a patient is seen and discharged from the ED, etc.
Lastly, I suggest someone in your group talk with your hospital’s compliance department about its own coding and billing compliance plan. This could lead to ideas or help develop a compliance plan for your group.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Reference
John Nelson: Post-Discharge Calls
There are lots of places to learn methods to improve patient satisfaction, including my thoughts from the January 2009 issue. Run an Internet search on “improve patient satisfaction” to get a huge number of articles, many of which have useful information and inspiration.
If you’re in a high-functioning hospitalist group, you’ve already read a lot on the topic, listened to presentations by someone at your hospital and elsewhere, and reliably reported and analyzed satisfaction survey results including HCAHPS questions and others. Maybe you’ve even engaged a consultant to help.
You might already have in place a number of strategies, such as reliably providing a business card with your photo, always sitting down in the patient’s room, asking “Is there anything else I can do?” before ending your time with a patient, etc. You’re doing all these things and more, but perhaps you’ve barely moved the needle on your satisfaction scores.
Despite your efforts, I bet your hospitalist group’s aggregate score is among the lowest of any physician group at your hospital.
You’re not alone.
What can you do about this?
High-Value Strategy: Phoning Patients after Discharge
I’m lucky enough to practice with some of the smartest, most professional, and most personable hospitalists you could ever meet. Yet our satisfaction scores are among the lowest for physicians at our hospital. Despite all of the improvement strategies we put in place over the last few years, our scores have barely budged. But that all changed once we instituted a formal program of phoning patients after discharge. That produced the largest uptick in our scores we’ve ever seen.
I can’t guarantee that our results are generalizable. But I have all the anecdotal information I need to be willing to invest the resources to make the calls. They improve scores. Likely more than any other single strategy. And they seem to have a positive effect on all survey questions, from how well the doctor explained things (nearly always the lowest of the HCAHPS scores for hospitalists) to the patient’s opinion of the hospital food.
Though initially resistant to expending the time and energy to make the calls, most in our group have said that they regularly feel really gratified by the response they get from patients or families. I think it is much better if a hospitalist who cared for the patient makes the calls, and I suspect (I have no proof) that calls made by a nurse or clerk are much less effective at improving patient satisfaction. And the call can serve as a valuable clinical encounter to briefly troubleshoot a problem or review a test result that was pending at discharge.
Simple Strategies
- More than 80% of these calls should last less than three minutes. Most patients or family members will report things are going OK and thank you profusely for the call. “No doctor has ever called before,” many will say. “Can we get you the next time Mom is hospitalized?”
- You could reduce the number of calls needed if you limit them to patients eligible for a survey; this typically is only about half of a hospitalist’s patient census. For example, patients on observation status and those discharged somewhere other than to home (e.g. to a skilled-nursing facility) are not eligible for a survey.
- It’s usually best not to tell a patient or family to expect the call. Surprising them makes them more delighted when you do call, and a patient told to expect a call but doesn’t get one will be less satisfied than if never told to expect it. Best if no one at the hospital knows you’re making the calls, because someone might brag about you and tell the patient to expect the call.
- For patients seen by several hospitalists, decide ahead of time which doctor makes the call. The doctor who discharged the patient is probably the simplest protocol.
- Develop a system to track patients who have been discharged. Every morning, we get a printout of all patients discharged the prior day. We try to call all patients the day after discharge to ensure that we reach them before they’ve had a chance to complete a satisfaction survey and before the discharging doctor rotates off.
- Develop a protocol to document the calls. Calls that lead to any new advice or therapies (e.g. see your primary-care physician sooner than planned) must be documented in the medical record, e.g., by dictating an addendum to the discharge summary. Don’t let the system get too complicated or keep you from making the calls.
- Use your judgment about whether to call the patient or just call a family member directly; it’s often better to do the latter.
- If you reach a voicemail (about 50% of the calls I make), leave a message and don’t keep calling back to reach a person.
Sample Scripts
Here are some simple scripts to use for post-discharge calls. If you reach the patient or family member:
- “This is Dr. X from Superior Hospital. I was just thinking about you/your mother/your father and wanted to know how things have gone since you/she/he left the hospital.”
- Ask about something related to the reason for their stay. “How is your appetite?” or “You haven’t had any more fever, have you?” or “Have you made your appointment with Dr. PCP yet?”
- “I hope things go really well for you, but if you ever need the hospital again, we’d be happy to care for you at Superior Hospital.”
If you get a voicemail:
- “This is Dr. X from Superior Hospital. I’ve been thinking about you/your mother/father since you/she/he left the hospital, and I am calling just to check on how things are going.” (For HIPPA reasons, don’t use the patient’s name when leaving a voicemail.)
- Mention some medical concern specific to the patient, e.g., “Your culture test turned out OK and I hope you’ve been able to get the antibiotic I prescribed.”
- “You don’t need to call me back, but if you have questions or want to provide an update, I can be reached at 555-123-4567.” (It’s very important to include this last sentence and a number where you can be reached. If omitted, many patients/families will think you must have called to convey something really important and will be distressed until able to reach you.)
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
There are lots of places to learn methods to improve patient satisfaction, including my thoughts from the January 2009 issue. Run an Internet search on “improve patient satisfaction” to get a huge number of articles, many of which have useful information and inspiration.
If you’re in a high-functioning hospitalist group, you’ve already read a lot on the topic, listened to presentations by someone at your hospital and elsewhere, and reliably reported and analyzed satisfaction survey results including HCAHPS questions and others. Maybe you’ve even engaged a consultant to help.
You might already have in place a number of strategies, such as reliably providing a business card with your photo, always sitting down in the patient’s room, asking “Is there anything else I can do?” before ending your time with a patient, etc. You’re doing all these things and more, but perhaps you’ve barely moved the needle on your satisfaction scores.
Despite your efforts, I bet your hospitalist group’s aggregate score is among the lowest of any physician group at your hospital.
You’re not alone.
What can you do about this?
High-Value Strategy: Phoning Patients after Discharge
I’m lucky enough to practice with some of the smartest, most professional, and most personable hospitalists you could ever meet. Yet our satisfaction scores are among the lowest for physicians at our hospital. Despite all of the improvement strategies we put in place over the last few years, our scores have barely budged. But that all changed once we instituted a formal program of phoning patients after discharge. That produced the largest uptick in our scores we’ve ever seen.
I can’t guarantee that our results are generalizable. But I have all the anecdotal information I need to be willing to invest the resources to make the calls. They improve scores. Likely more than any other single strategy. And they seem to have a positive effect on all survey questions, from how well the doctor explained things (nearly always the lowest of the HCAHPS scores for hospitalists) to the patient’s opinion of the hospital food.
Though initially resistant to expending the time and energy to make the calls, most in our group have said that they regularly feel really gratified by the response they get from patients or families. I think it is much better if a hospitalist who cared for the patient makes the calls, and I suspect (I have no proof) that calls made by a nurse or clerk are much less effective at improving patient satisfaction. And the call can serve as a valuable clinical encounter to briefly troubleshoot a problem or review a test result that was pending at discharge.
Simple Strategies
- More than 80% of these calls should last less than three minutes. Most patients or family members will report things are going OK and thank you profusely for the call. “No doctor has ever called before,” many will say. “Can we get you the next time Mom is hospitalized?”
- You could reduce the number of calls needed if you limit them to patients eligible for a survey; this typically is only about half of a hospitalist’s patient census. For example, patients on observation status and those discharged somewhere other than to home (e.g. to a skilled-nursing facility) are not eligible for a survey.
- It’s usually best not to tell a patient or family to expect the call. Surprising them makes them more delighted when you do call, and a patient told to expect a call but doesn’t get one will be less satisfied than if never told to expect it. Best if no one at the hospital knows you’re making the calls, because someone might brag about you and tell the patient to expect the call.
- For patients seen by several hospitalists, decide ahead of time which doctor makes the call. The doctor who discharged the patient is probably the simplest protocol.
- Develop a system to track patients who have been discharged. Every morning, we get a printout of all patients discharged the prior day. We try to call all patients the day after discharge to ensure that we reach them before they’ve had a chance to complete a satisfaction survey and before the discharging doctor rotates off.
- Develop a protocol to document the calls. Calls that lead to any new advice or therapies (e.g. see your primary-care physician sooner than planned) must be documented in the medical record, e.g., by dictating an addendum to the discharge summary. Don’t let the system get too complicated or keep you from making the calls.
- Use your judgment about whether to call the patient or just call a family member directly; it’s often better to do the latter.
- If you reach a voicemail (about 50% of the calls I make), leave a message and don’t keep calling back to reach a person.
Sample Scripts
Here are some simple scripts to use for post-discharge calls. If you reach the patient or family member:
- “This is Dr. X from Superior Hospital. I was just thinking about you/your mother/your father and wanted to know how things have gone since you/she/he left the hospital.”
- Ask about something related to the reason for their stay. “How is your appetite?” or “You haven’t had any more fever, have you?” or “Have you made your appointment with Dr. PCP yet?”
- “I hope things go really well for you, but if you ever need the hospital again, we’d be happy to care for you at Superior Hospital.”
If you get a voicemail:
- “This is Dr. X from Superior Hospital. I’ve been thinking about you/your mother/father since you/she/he left the hospital, and I am calling just to check on how things are going.” (For HIPPA reasons, don’t use the patient’s name when leaving a voicemail.)
- Mention some medical concern specific to the patient, e.g., “Your culture test turned out OK and I hope you’ve been able to get the antibiotic I prescribed.”
- “You don’t need to call me back, but if you have questions or want to provide an update, I can be reached at 555-123-4567.” (It’s very important to include this last sentence and a number where you can be reached. If omitted, many patients/families will think you must have called to convey something really important and will be distressed until able to reach you.)
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
There are lots of places to learn methods to improve patient satisfaction, including my thoughts from the January 2009 issue. Run an Internet search on “improve patient satisfaction” to get a huge number of articles, many of which have useful information and inspiration.
If you’re in a high-functioning hospitalist group, you’ve already read a lot on the topic, listened to presentations by someone at your hospital and elsewhere, and reliably reported and analyzed satisfaction survey results including HCAHPS questions and others. Maybe you’ve even engaged a consultant to help.
You might already have in place a number of strategies, such as reliably providing a business card with your photo, always sitting down in the patient’s room, asking “Is there anything else I can do?” before ending your time with a patient, etc. You’re doing all these things and more, but perhaps you’ve barely moved the needle on your satisfaction scores.
Despite your efforts, I bet your hospitalist group’s aggregate score is among the lowest of any physician group at your hospital.
You’re not alone.
What can you do about this?
High-Value Strategy: Phoning Patients after Discharge
I’m lucky enough to practice with some of the smartest, most professional, and most personable hospitalists you could ever meet. Yet our satisfaction scores are among the lowest for physicians at our hospital. Despite all of the improvement strategies we put in place over the last few years, our scores have barely budged. But that all changed once we instituted a formal program of phoning patients after discharge. That produced the largest uptick in our scores we’ve ever seen.
I can’t guarantee that our results are generalizable. But I have all the anecdotal information I need to be willing to invest the resources to make the calls. They improve scores. Likely more than any other single strategy. And they seem to have a positive effect on all survey questions, from how well the doctor explained things (nearly always the lowest of the HCAHPS scores for hospitalists) to the patient’s opinion of the hospital food.
Though initially resistant to expending the time and energy to make the calls, most in our group have said that they regularly feel really gratified by the response they get from patients or families. I think it is much better if a hospitalist who cared for the patient makes the calls, and I suspect (I have no proof) that calls made by a nurse or clerk are much less effective at improving patient satisfaction. And the call can serve as a valuable clinical encounter to briefly troubleshoot a problem or review a test result that was pending at discharge.
Simple Strategies
- More than 80% of these calls should last less than three minutes. Most patients or family members will report things are going OK and thank you profusely for the call. “No doctor has ever called before,” many will say. “Can we get you the next time Mom is hospitalized?”
- You could reduce the number of calls needed if you limit them to patients eligible for a survey; this typically is only about half of a hospitalist’s patient census. For example, patients on observation status and those discharged somewhere other than to home (e.g. to a skilled-nursing facility) are not eligible for a survey.
- It’s usually best not to tell a patient or family to expect the call. Surprising them makes them more delighted when you do call, and a patient told to expect a call but doesn’t get one will be less satisfied than if never told to expect it. Best if no one at the hospital knows you’re making the calls, because someone might brag about you and tell the patient to expect the call.
- For patients seen by several hospitalists, decide ahead of time which doctor makes the call. The doctor who discharged the patient is probably the simplest protocol.
- Develop a system to track patients who have been discharged. Every morning, we get a printout of all patients discharged the prior day. We try to call all patients the day after discharge to ensure that we reach them before they’ve had a chance to complete a satisfaction survey and before the discharging doctor rotates off.
- Develop a protocol to document the calls. Calls that lead to any new advice or therapies (e.g. see your primary-care physician sooner than planned) must be documented in the medical record, e.g., by dictating an addendum to the discharge summary. Don’t let the system get too complicated or keep you from making the calls.
- Use your judgment about whether to call the patient or just call a family member directly; it’s often better to do the latter.
- If you reach a voicemail (about 50% of the calls I make), leave a message and don’t keep calling back to reach a person.
Sample Scripts
Here are some simple scripts to use for post-discharge calls. If you reach the patient or family member:
- “This is Dr. X from Superior Hospital. I was just thinking about you/your mother/your father and wanted to know how things have gone since you/she/he left the hospital.”
- Ask about something related to the reason for their stay. “How is your appetite?” or “You haven’t had any more fever, have you?” or “Have you made your appointment with Dr. PCP yet?”
- “I hope things go really well for you, but if you ever need the hospital again, we’d be happy to care for you at Superior Hospital.”
If you get a voicemail:
- “This is Dr. X from Superior Hospital. I’ve been thinking about you/your mother/father since you/she/he left the hospital, and I am calling just to check on how things are going.” (For HIPPA reasons, don’t use the patient’s name when leaving a voicemail.)
- Mention some medical concern specific to the patient, e.g., “Your culture test turned out OK and I hope you’ve been able to get the antibiotic I prescribed.”
- “You don’t need to call me back, but if you have questions or want to provide an update, I can be reached at 555-123-4567.” (It’s very important to include this last sentence and a number where you can be reached. If omitted, many patients/families will think you must have called to convey something really important and will be distressed until able to reach you.)
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
John Nelson: Admit Resolution
Editor’s note: Second in a two-part series.
I used last month’s column to frame the issue of disagreement between doctors over who should admit a particular patient, as well as discuss the value of good social connections to reduce the chance that divergent opinions lead to outright conflict. This month, I’ll review another worthwhile strategy—one that could be a definitive solution to these disagreements but often falls short of that goal in practice.
Service Agreements, or “Compacts,” between Physician Groups
If, at your hospital, there are reasonably frequent cases of divergent opinions regarding whether an ED admission or transfer from elsewhere should be admitted by a hospitalist or doctor in another specialty, why not meet in advance to decide this? Many hospitalist groups have held meetings with doctors in other specialties and now have a collection of agreements outlining scenarios, such as:
- ESRD patients: Hospitalist admits for non-dialysis issues (pneumonia, diabetic issues, etc.); nephrologist admits for urgent dialysis issues (K+>6.3, pH<7.3, etc.).
- Cardiology: Hospitalist admits CHF and non-ST elevation chest pain; cardiologist admits STEMI.
- General surgery: Hospitalist admits ileus, pseudo obstruction, and SBO due to adhesions; general surgery admits bowel obstruction in “virgin abdomen,” volvulus, and any obstruction thought to require urgent surgery.
To be clear, I’m not suggesting the above guidelines are evidence-based or are the right ones for your institution. I just made these up, so yours might differ significantly. I just want to provide a sense of the kinds of issues these agreements typically cover. The comanagement section of the SHM website has several documents regarding hospitalist-orthopedic service agreements.
The Negotiation Process
It’s tempting for the lead hospitalist to just have a hallway chat with a spokesperson from the other specialty, then email a draft agreement, exchange a few messages until both parties are satisfied, then email a copy of the final document to all the doctors in both groups. This might work for some simple service agreements, but for any area with significant ambiguity or disagreements (or potential for disagreements), one or more in-person meetings are usually necessary. Ideally, several doctors in both groups will attend these meetings.
Much work could be done in advance of the first meeting, including surveying other practices to see how they decide which group admits the same kinds of patents, gathering any relevant published research, and possibly drafting a “straw man” proposed agreement. When meeting in person, the doctors will have a chance to explain their points of view, needs, and concerns, and gain a greater appreciation of the way “the other guy” sees things. An important purpose of the in-person meeting is to “look the other guy in the eye” to know if he or she really is committed to following through.
Remember that written agreements like these might become an issue in malpractice suits, so you might want to have them reviewed first by risk managers. You might also write them as guidelines rather than rigid protocols that don’t allow variations.
Maximize Effectiveness
Ideally, every doctor involved in the agreement should document their approval with a signature and date. My experience is that this doesn’t happen at most places, but if there is concern about whether everyone will comply, signing the document will probably help at least a little.
The completed agreements should be provided to all doctors in both groups, the ED, affected hospital nursing units, and others. Any new doctor should get a copy of all such agreements that might be relevant. And, most important, it should be made available electronically so that it is easy to find at any time. Some agreements cover uncommon events, and the doctors on duty might not remember what the agreement said and will need ready access to it.
Most service agreements should be reviewed and updated every two or three years or as needed. If there is confusion or controversy around a particular agreement, or if disagreements about which doctor does the admission are common despite the agreement, then an in-person meeting between the physician groups should be scheduled to revise or update it.
Keep Your Fingers Crossed
If it sounds like a lot of work to develop and maintain these agreements, it is. But they’re worth every bit of that work if they reduce confusion or discord. Sadly, for several reasons, they rarely prove so effective.
One doctor might think the agreement applies, but the other doctor says this patient is an exception and the agreement doesn’t apply. It is impossible to write an agreement that addresses all possible scenarios, so a doctor can argue that any particular patient falls outside the agreement because of things like comorbidities, which service admitted the patient last time (many agreements will have defined “bounce back” intervals), which primary-care physician (PCP) the patient sees, etc.
Even if there is no dispute about whether the agreement covers a particular patient, many doctors simply don’t feel obligated to uphold the agreement. Such a doctor might tell the ED doctor: “Yep, I signed the agreement, but only as a way to get the meeting over with. I was never in favor of it and just can’t admit the patient. Call the other guy to admit.” So in spite of all the work done to create a reasonable agreement, some doctors might feel entitled to ignore it when it suits them.
Compliance Is Critical
Sadly, my take is that despite the tremendous hoped-for benefits that service agreements might provide, poor compliance means they rarely achieve their potential. Even so, they are usually worth the time and effort to create them if it leads doctors in the two specialties to schedule time away from patient care to listen to the other group’s point of view and discuss how best to handle particular types of patients. In some cases, it will be the first time the two groups of doctors have set aside time to talk about the work they do together; that alone can have significant value.
Tom Lorence, MD, a Kaiser hospitalist in Portland, Ore., who is chief of hospital medicine for Northwest Permanente, developed more than 20 service agreements with many different specialties at his institution. He has found that they are worth the effort, and that they helped allay hospitalists’ feeling of being “dumped on.”
He also told me a rule that probably applies to all such agreements in any setting: The tie goes to the hospitalist—that is, when there is reasonable uncertainty or disagreement about which group should admit a patient, it is nearly always the hospitalist who will do so.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Editor’s note: Second in a two-part series.
I used last month’s column to frame the issue of disagreement between doctors over who should admit a particular patient, as well as discuss the value of good social connections to reduce the chance that divergent opinions lead to outright conflict. This month, I’ll review another worthwhile strategy—one that could be a definitive solution to these disagreements but often falls short of that goal in practice.
Service Agreements, or “Compacts,” between Physician Groups
If, at your hospital, there are reasonably frequent cases of divergent opinions regarding whether an ED admission or transfer from elsewhere should be admitted by a hospitalist or doctor in another specialty, why not meet in advance to decide this? Many hospitalist groups have held meetings with doctors in other specialties and now have a collection of agreements outlining scenarios, such as:
- ESRD patients: Hospitalist admits for non-dialysis issues (pneumonia, diabetic issues, etc.); nephrologist admits for urgent dialysis issues (K+>6.3, pH<7.3, etc.).
- Cardiology: Hospitalist admits CHF and non-ST elevation chest pain; cardiologist admits STEMI.
- General surgery: Hospitalist admits ileus, pseudo obstruction, and SBO due to adhesions; general surgery admits bowel obstruction in “virgin abdomen,” volvulus, and any obstruction thought to require urgent surgery.
To be clear, I’m not suggesting the above guidelines are evidence-based or are the right ones for your institution. I just made these up, so yours might differ significantly. I just want to provide a sense of the kinds of issues these agreements typically cover. The comanagement section of the SHM website has several documents regarding hospitalist-orthopedic service agreements.
The Negotiation Process
It’s tempting for the lead hospitalist to just have a hallway chat with a spokesperson from the other specialty, then email a draft agreement, exchange a few messages until both parties are satisfied, then email a copy of the final document to all the doctors in both groups. This might work for some simple service agreements, but for any area with significant ambiguity or disagreements (or potential for disagreements), one or more in-person meetings are usually necessary. Ideally, several doctors in both groups will attend these meetings.
Much work could be done in advance of the first meeting, including surveying other practices to see how they decide which group admits the same kinds of patents, gathering any relevant published research, and possibly drafting a “straw man” proposed agreement. When meeting in person, the doctors will have a chance to explain their points of view, needs, and concerns, and gain a greater appreciation of the way “the other guy” sees things. An important purpose of the in-person meeting is to “look the other guy in the eye” to know if he or she really is committed to following through.
Remember that written agreements like these might become an issue in malpractice suits, so you might want to have them reviewed first by risk managers. You might also write them as guidelines rather than rigid protocols that don’t allow variations.
Maximize Effectiveness
Ideally, every doctor involved in the agreement should document their approval with a signature and date. My experience is that this doesn’t happen at most places, but if there is concern about whether everyone will comply, signing the document will probably help at least a little.
The completed agreements should be provided to all doctors in both groups, the ED, affected hospital nursing units, and others. Any new doctor should get a copy of all such agreements that might be relevant. And, most important, it should be made available electronically so that it is easy to find at any time. Some agreements cover uncommon events, and the doctors on duty might not remember what the agreement said and will need ready access to it.
Most service agreements should be reviewed and updated every two or three years or as needed. If there is confusion or controversy around a particular agreement, or if disagreements about which doctor does the admission are common despite the agreement, then an in-person meeting between the physician groups should be scheduled to revise or update it.
Keep Your Fingers Crossed
If it sounds like a lot of work to develop and maintain these agreements, it is. But they’re worth every bit of that work if they reduce confusion or discord. Sadly, for several reasons, they rarely prove so effective.
One doctor might think the agreement applies, but the other doctor says this patient is an exception and the agreement doesn’t apply. It is impossible to write an agreement that addresses all possible scenarios, so a doctor can argue that any particular patient falls outside the agreement because of things like comorbidities, which service admitted the patient last time (many agreements will have defined “bounce back” intervals), which primary-care physician (PCP) the patient sees, etc.
Even if there is no dispute about whether the agreement covers a particular patient, many doctors simply don’t feel obligated to uphold the agreement. Such a doctor might tell the ED doctor: “Yep, I signed the agreement, but only as a way to get the meeting over with. I was never in favor of it and just can’t admit the patient. Call the other guy to admit.” So in spite of all the work done to create a reasonable agreement, some doctors might feel entitled to ignore it when it suits them.
Compliance Is Critical
Sadly, my take is that despite the tremendous hoped-for benefits that service agreements might provide, poor compliance means they rarely achieve their potential. Even so, they are usually worth the time and effort to create them if it leads doctors in the two specialties to schedule time away from patient care to listen to the other group’s point of view and discuss how best to handle particular types of patients. In some cases, it will be the first time the two groups of doctors have set aside time to talk about the work they do together; that alone can have significant value.
Tom Lorence, MD, a Kaiser hospitalist in Portland, Ore., who is chief of hospital medicine for Northwest Permanente, developed more than 20 service agreements with many different specialties at his institution. He has found that they are worth the effort, and that they helped allay hospitalists’ feeling of being “dumped on.”
He also told me a rule that probably applies to all such agreements in any setting: The tie goes to the hospitalist—that is, when there is reasonable uncertainty or disagreement about which group should admit a patient, it is nearly always the hospitalist who will do so.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Editor’s note: Second in a two-part series.
I used last month’s column to frame the issue of disagreement between doctors over who should admit a particular patient, as well as discuss the value of good social connections to reduce the chance that divergent opinions lead to outright conflict. This month, I’ll review another worthwhile strategy—one that could be a definitive solution to these disagreements but often falls short of that goal in practice.
Service Agreements, or “Compacts,” between Physician Groups
If, at your hospital, there are reasonably frequent cases of divergent opinions regarding whether an ED admission or transfer from elsewhere should be admitted by a hospitalist or doctor in another specialty, why not meet in advance to decide this? Many hospitalist groups have held meetings with doctors in other specialties and now have a collection of agreements outlining scenarios, such as:
- ESRD patients: Hospitalist admits for non-dialysis issues (pneumonia, diabetic issues, etc.); nephrologist admits for urgent dialysis issues (K+>6.3, pH<7.3, etc.).
- Cardiology: Hospitalist admits CHF and non-ST elevation chest pain; cardiologist admits STEMI.
- General surgery: Hospitalist admits ileus, pseudo obstruction, and SBO due to adhesions; general surgery admits bowel obstruction in “virgin abdomen,” volvulus, and any obstruction thought to require urgent surgery.
To be clear, I’m not suggesting the above guidelines are evidence-based or are the right ones for your institution. I just made these up, so yours might differ significantly. I just want to provide a sense of the kinds of issues these agreements typically cover. The comanagement section of the SHM website has several documents regarding hospitalist-orthopedic service agreements.
The Negotiation Process
It’s tempting for the lead hospitalist to just have a hallway chat with a spokesperson from the other specialty, then email a draft agreement, exchange a few messages until both parties are satisfied, then email a copy of the final document to all the doctors in both groups. This might work for some simple service agreements, but for any area with significant ambiguity or disagreements (or potential for disagreements), one or more in-person meetings are usually necessary. Ideally, several doctors in both groups will attend these meetings.
Much work could be done in advance of the first meeting, including surveying other practices to see how they decide which group admits the same kinds of patents, gathering any relevant published research, and possibly drafting a “straw man” proposed agreement. When meeting in person, the doctors will have a chance to explain their points of view, needs, and concerns, and gain a greater appreciation of the way “the other guy” sees things. An important purpose of the in-person meeting is to “look the other guy in the eye” to know if he or she really is committed to following through.
Remember that written agreements like these might become an issue in malpractice suits, so you might want to have them reviewed first by risk managers. You might also write them as guidelines rather than rigid protocols that don’t allow variations.
Maximize Effectiveness
Ideally, every doctor involved in the agreement should document their approval with a signature and date. My experience is that this doesn’t happen at most places, but if there is concern about whether everyone will comply, signing the document will probably help at least a little.
The completed agreements should be provided to all doctors in both groups, the ED, affected hospital nursing units, and others. Any new doctor should get a copy of all such agreements that might be relevant. And, most important, it should be made available electronically so that it is easy to find at any time. Some agreements cover uncommon events, and the doctors on duty might not remember what the agreement said and will need ready access to it.
Most service agreements should be reviewed and updated every two or three years or as needed. If there is confusion or controversy around a particular agreement, or if disagreements about which doctor does the admission are common despite the agreement, then an in-person meeting between the physician groups should be scheduled to revise or update it.
Keep Your Fingers Crossed
If it sounds like a lot of work to develop and maintain these agreements, it is. But they’re worth every bit of that work if they reduce confusion or discord. Sadly, for several reasons, they rarely prove so effective.
One doctor might think the agreement applies, but the other doctor says this patient is an exception and the agreement doesn’t apply. It is impossible to write an agreement that addresses all possible scenarios, so a doctor can argue that any particular patient falls outside the agreement because of things like comorbidities, which service admitted the patient last time (many agreements will have defined “bounce back” intervals), which primary-care physician (PCP) the patient sees, etc.
Even if there is no dispute about whether the agreement covers a particular patient, many doctors simply don’t feel obligated to uphold the agreement. Such a doctor might tell the ED doctor: “Yep, I signed the agreement, but only as a way to get the meeting over with. I was never in favor of it and just can’t admit the patient. Call the other guy to admit.” So in spite of all the work done to create a reasonable agreement, some doctors might feel entitled to ignore it when it suits them.
Compliance Is Critical
Sadly, my take is that despite the tremendous hoped-for benefits that service agreements might provide, poor compliance means they rarely achieve their potential. Even so, they are usually worth the time and effort to create them if it leads doctors in the two specialties to schedule time away from patient care to listen to the other group’s point of view and discuss how best to handle particular types of patients. In some cases, it will be the first time the two groups of doctors have set aside time to talk about the work they do together; that alone can have significant value.
Tom Lorence, MD, a Kaiser hospitalist in Portland, Ore., who is chief of hospital medicine for Northwest Permanente, developed more than 20 service agreements with many different specialties at his institution. He has found that they are worth the effort, and that they helped allay hospitalists’ feeling of being “dumped on.”
He also told me a rule that probably applies to all such agreements in any setting: The tie goes to the hospitalist—that is, when there is reasonable uncertainty or disagreement about which group should admit a patient, it is nearly always the hospitalist who will do so.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
John Nelson: Conflict Resolution
Editor’s note: First of a two-part series.
Think about the last time you found yourself in the middle of a contentious conversation with another doctor about whether a patient should be admitted by you, the hospitalist, or by a doctor in another specialty. Such conversations can sometimes move quickly from respectful disagreement to posturing, drawing lines in the sand, or worse.
Respectful conversations between doctors with differing opinions about the best plan of care for patients are valuable. But disagreements that lead doctors to talk at rather than with each other risk creating quality-of-care issues for the patient, demoralize other hospital staff, and can result in lasting harm to the relationship between the doctors involved. I’d bet the frequency of such disputes could serve as a reliable predictor of overall quality of care, and might correlate with cost of care. Doctors in all specialties should work diligently to reduce the chance that such conversations lead to conflict and stress.
Middle Manager
This conflict arises most often when an ED doctor is calling about a patient needing admission; the way communication between ED doctors and other physicians happens nearly everywhere is one reason the problem is so difficult to eradicate. (To be clear, I’m not faulting ED doctors for causing this problem; I think they usually try very hard to prevent it.)
Because the ED doctor is often in the middle of the chain of communication (disagreement), those whom the ED doctor is asking to admit the patient often are emboldened to take more unreasonable or extreme positions. It is a lot easier for Dr. Perry to make a case to the ED doctors that Dr. Mercury should admit a patient than to present the same rationale to Dr. Mercury himself. In many cases, the ED doctors can make the problem go away, or at least extricate themselves from the disagreement, by insisting that Dr. Perry and Dr. Mercury speak directly to each other.
Of course, things can sometimes go so badly that they refuse to speak directly with one another and force the ED doctor to settle the dispute a power given to the ED doctor by the medical staff bylaws at nearly every hospital. Or maybe they do speak directly and that leads to greater conflict (i.e. shouting or an abrupt hang-up).
Improved Social Connections
Most hospitals I’ve worked with seem to feature harmonious and collegial relationships between the ED doctors, hospitalists, and other specialties. But for some, divisive conflict crops up frequently. A first step for those hospitals laden with conflict could be to deliberately work to improve the social connections between the physician groups that often disagree. I’m not Pollyannaish; sometimes relationships are beyond repair, or one of the doctors involved might have a character disorder that requires more significant interventions.
A few years ago, I visited a place where years of conflict between ED doctors and hospitalists had led to remarkably adversarial relationships. Both of the lead physicians for the ED doctors and hospitalists were pleasant, professional, and highly regarded by others. Nonetheless, they both were fed up with the ongoing conflict and found themselves in such an adversarial relationship that I worried the next nighttime dispute could come to blows (literally). With a combination of support and pressure from hospital leaders and physician peers, they committed to a series of dinner meetings, just the two of them. They agreed to meet monthly, away from the hospital, and for the first few meetings avoid any conversation about work-related issues. The point was for them to build social connections so that they could find new ways of communicating, thus regain respect for the character of the other.
Some months later, I heard from the lead hospitalist, who said that the meetings had proven very valuable and things had improved dramatically between the department heads. He also said they were working together to improve the way their whole groups interacted. This wouldn’t work so well everywhere, and would have failed if not for the good character of both the doctors. But I’m struck by how infrequently the formation of social ties is included in any plan to reduce physician conflict. It is valuable, regardless of which specialties the doctors work in.
Hospitals have figured this out. Most provide a doctor’s lounge where meals might be served to provide a place for socialization. Some arrange periodic retreats for physician and hospital leaders to spend a weekend in a nice setting (with some time devoted to business and ample time for recreation and socialization). Expensive “perks” like these probably pay dividends in improving culture and reducing conflict. They also might soon be a thing of the past due to cost pressures. If so, we should all think deliberately about other ways hospitals can preserve and enhance the social fabric of what is becoming a more segregated medical staff as doctors narrow their sites of care and specialty focus.
The Universal Admitter
The most effective way to eliminate disagreements in admission decisions is to have the hospitalist admit all of them—that is, make the hospitalist a universal admitter.
Some hospitalist groups are nearly universal admitters already. No, they aren’t admitting all patients, including women in labor and some others. But they do admit and serve as attending for patients with hip fractures and other trauma and surgical issues, scheduled chemotherapy patients, etc.
I’ll save of my comments about the appropriateness of hospitalists as universal admitters for a future column. But I think that it is overkill to move to that model solely to address disagreements regarding which group admits a patient.
Service Agreements
Another way to reduce conflict over which physician group will serve as admitting/attending physician is to develop service agreements, or “compacts,” between different specialties. The idea is to create a set of clear, written guidelines or rules that determine which group admits the patient. For example, should the hospitalist or the surgeon admit?
ED doctors usually are delighted when the hospitalists and surgeons have met to create such an agreement. It could mean the end of disputes about who admits the patient. But does it?
I’ll discuss these agreements further in next month’s column, including elements that should be addressed, how to maximize compliance with them, and why they almost always fall short of realizing their hoped-for potential.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Editor’s note: First of a two-part series.
Think about the last time you found yourself in the middle of a contentious conversation with another doctor about whether a patient should be admitted by you, the hospitalist, or by a doctor in another specialty. Such conversations can sometimes move quickly from respectful disagreement to posturing, drawing lines in the sand, or worse.
Respectful conversations between doctors with differing opinions about the best plan of care for patients are valuable. But disagreements that lead doctors to talk at rather than with each other risk creating quality-of-care issues for the patient, demoralize other hospital staff, and can result in lasting harm to the relationship between the doctors involved. I’d bet the frequency of such disputes could serve as a reliable predictor of overall quality of care, and might correlate with cost of care. Doctors in all specialties should work diligently to reduce the chance that such conversations lead to conflict and stress.
Middle Manager
This conflict arises most often when an ED doctor is calling about a patient needing admission; the way communication between ED doctors and other physicians happens nearly everywhere is one reason the problem is so difficult to eradicate. (To be clear, I’m not faulting ED doctors for causing this problem; I think they usually try very hard to prevent it.)
Because the ED doctor is often in the middle of the chain of communication (disagreement), those whom the ED doctor is asking to admit the patient often are emboldened to take more unreasonable or extreme positions. It is a lot easier for Dr. Perry to make a case to the ED doctors that Dr. Mercury should admit a patient than to present the same rationale to Dr. Mercury himself. In many cases, the ED doctors can make the problem go away, or at least extricate themselves from the disagreement, by insisting that Dr. Perry and Dr. Mercury speak directly to each other.
Of course, things can sometimes go so badly that they refuse to speak directly with one another and force the ED doctor to settle the dispute a power given to the ED doctor by the medical staff bylaws at nearly every hospital. Or maybe they do speak directly and that leads to greater conflict (i.e. shouting or an abrupt hang-up).
Improved Social Connections
Most hospitals I’ve worked with seem to feature harmonious and collegial relationships between the ED doctors, hospitalists, and other specialties. But for some, divisive conflict crops up frequently. A first step for those hospitals laden with conflict could be to deliberately work to improve the social connections between the physician groups that often disagree. I’m not Pollyannaish; sometimes relationships are beyond repair, or one of the doctors involved might have a character disorder that requires more significant interventions.
A few years ago, I visited a place where years of conflict between ED doctors and hospitalists had led to remarkably adversarial relationships. Both of the lead physicians for the ED doctors and hospitalists were pleasant, professional, and highly regarded by others. Nonetheless, they both were fed up with the ongoing conflict and found themselves in such an adversarial relationship that I worried the next nighttime dispute could come to blows (literally). With a combination of support and pressure from hospital leaders and physician peers, they committed to a series of dinner meetings, just the two of them. They agreed to meet monthly, away from the hospital, and for the first few meetings avoid any conversation about work-related issues. The point was for them to build social connections so that they could find new ways of communicating, thus regain respect for the character of the other.
Some months later, I heard from the lead hospitalist, who said that the meetings had proven very valuable and things had improved dramatically between the department heads. He also said they were working together to improve the way their whole groups interacted. This wouldn’t work so well everywhere, and would have failed if not for the good character of both the doctors. But I’m struck by how infrequently the formation of social ties is included in any plan to reduce physician conflict. It is valuable, regardless of which specialties the doctors work in.
Hospitals have figured this out. Most provide a doctor’s lounge where meals might be served to provide a place for socialization. Some arrange periodic retreats for physician and hospital leaders to spend a weekend in a nice setting (with some time devoted to business and ample time for recreation and socialization). Expensive “perks” like these probably pay dividends in improving culture and reducing conflict. They also might soon be a thing of the past due to cost pressures. If so, we should all think deliberately about other ways hospitals can preserve and enhance the social fabric of what is becoming a more segregated medical staff as doctors narrow their sites of care and specialty focus.
The Universal Admitter
The most effective way to eliminate disagreements in admission decisions is to have the hospitalist admit all of them—that is, make the hospitalist a universal admitter.
Some hospitalist groups are nearly universal admitters already. No, they aren’t admitting all patients, including women in labor and some others. But they do admit and serve as attending for patients with hip fractures and other trauma and surgical issues, scheduled chemotherapy patients, etc.
I’ll save of my comments about the appropriateness of hospitalists as universal admitters for a future column. But I think that it is overkill to move to that model solely to address disagreements regarding which group admits a patient.
Service Agreements
Another way to reduce conflict over which physician group will serve as admitting/attending physician is to develop service agreements, or “compacts,” between different specialties. The idea is to create a set of clear, written guidelines or rules that determine which group admits the patient. For example, should the hospitalist or the surgeon admit?
ED doctors usually are delighted when the hospitalists and surgeons have met to create such an agreement. It could mean the end of disputes about who admits the patient. But does it?
I’ll discuss these agreements further in next month’s column, including elements that should be addressed, how to maximize compliance with them, and why they almost always fall short of realizing their hoped-for potential.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Editor’s note: First of a two-part series.
Think about the last time you found yourself in the middle of a contentious conversation with another doctor about whether a patient should be admitted by you, the hospitalist, or by a doctor in another specialty. Such conversations can sometimes move quickly from respectful disagreement to posturing, drawing lines in the sand, or worse.
Respectful conversations between doctors with differing opinions about the best plan of care for patients are valuable. But disagreements that lead doctors to talk at rather than with each other risk creating quality-of-care issues for the patient, demoralize other hospital staff, and can result in lasting harm to the relationship between the doctors involved. I’d bet the frequency of such disputes could serve as a reliable predictor of overall quality of care, and might correlate with cost of care. Doctors in all specialties should work diligently to reduce the chance that such conversations lead to conflict and stress.
Middle Manager
This conflict arises most often when an ED doctor is calling about a patient needing admission; the way communication between ED doctors and other physicians happens nearly everywhere is one reason the problem is so difficult to eradicate. (To be clear, I’m not faulting ED doctors for causing this problem; I think they usually try very hard to prevent it.)
Because the ED doctor is often in the middle of the chain of communication (disagreement), those whom the ED doctor is asking to admit the patient often are emboldened to take more unreasonable or extreme positions. It is a lot easier for Dr. Perry to make a case to the ED doctors that Dr. Mercury should admit a patient than to present the same rationale to Dr. Mercury himself. In many cases, the ED doctors can make the problem go away, or at least extricate themselves from the disagreement, by insisting that Dr. Perry and Dr. Mercury speak directly to each other.
Of course, things can sometimes go so badly that they refuse to speak directly with one another and force the ED doctor to settle the dispute a power given to the ED doctor by the medical staff bylaws at nearly every hospital. Or maybe they do speak directly and that leads to greater conflict (i.e. shouting or an abrupt hang-up).
Improved Social Connections
Most hospitals I’ve worked with seem to feature harmonious and collegial relationships between the ED doctors, hospitalists, and other specialties. But for some, divisive conflict crops up frequently. A first step for those hospitals laden with conflict could be to deliberately work to improve the social connections between the physician groups that often disagree. I’m not Pollyannaish; sometimes relationships are beyond repair, or one of the doctors involved might have a character disorder that requires more significant interventions.
A few years ago, I visited a place where years of conflict between ED doctors and hospitalists had led to remarkably adversarial relationships. Both of the lead physicians for the ED doctors and hospitalists were pleasant, professional, and highly regarded by others. Nonetheless, they both were fed up with the ongoing conflict and found themselves in such an adversarial relationship that I worried the next nighttime dispute could come to blows (literally). With a combination of support and pressure from hospital leaders and physician peers, they committed to a series of dinner meetings, just the two of them. They agreed to meet monthly, away from the hospital, and for the first few meetings avoid any conversation about work-related issues. The point was for them to build social connections so that they could find new ways of communicating, thus regain respect for the character of the other.
Some months later, I heard from the lead hospitalist, who said that the meetings had proven very valuable and things had improved dramatically between the department heads. He also said they were working together to improve the way their whole groups interacted. This wouldn’t work so well everywhere, and would have failed if not for the good character of both the doctors. But I’m struck by how infrequently the formation of social ties is included in any plan to reduce physician conflict. It is valuable, regardless of which specialties the doctors work in.
Hospitals have figured this out. Most provide a doctor’s lounge where meals might be served to provide a place for socialization. Some arrange periodic retreats for physician and hospital leaders to spend a weekend in a nice setting (with some time devoted to business and ample time for recreation and socialization). Expensive “perks” like these probably pay dividends in improving culture and reducing conflict. They also might soon be a thing of the past due to cost pressures. If so, we should all think deliberately about other ways hospitals can preserve and enhance the social fabric of what is becoming a more segregated medical staff as doctors narrow their sites of care and specialty focus.
The Universal Admitter
The most effective way to eliminate disagreements in admission decisions is to have the hospitalist admit all of them—that is, make the hospitalist a universal admitter.
Some hospitalist groups are nearly universal admitters already. No, they aren’t admitting all patients, including women in labor and some others. But they do admit and serve as attending for patients with hip fractures and other trauma and surgical issues, scheduled chemotherapy patients, etc.
I’ll save of my comments about the appropriateness of hospitalists as universal admitters for a future column. But I think that it is overkill to move to that model solely to address disagreements regarding which group admits a patient.
Service Agreements
Another way to reduce conflict over which physician group will serve as admitting/attending physician is to develop service agreements, or “compacts,” between different specialties. The idea is to create a set of clear, written guidelines or rules that determine which group admits the patient. For example, should the hospitalist or the surgeon admit?
ED doctors usually are delighted when the hospitalists and surgeons have met to create such an agreement. It could mean the end of disputes about who admits the patient. But does it?
I’ll discuss these agreements further in next month’s column, including elements that should be addressed, how to maximize compliance with them, and why they almost always fall short of realizing their hoped-for potential.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
John Nelson: Recognition, Promotion, Development Critical to Group Success
Well-designed forms of non-monetary compensation can have a greater impact on a hospitalist than providing a reward in dollars. This is true for any employee in any enterprise. It can have a greater impact than dollars in making a doctor feel appreciated and committed to the work of the organization. For example, a $100 gift certificate at a nice local restaurant can have a lot more impact and value than adding an extra $100 to the next paycheck.
A hospitalist’s salary and typical benefits (e.g. health insurance and retirement plan) must be attractive and competitive in the marketplace (obviously), but they are typically seen as entitlements, so they aren’t very effective at improving retention or motivating a doctor to perform well. Various forms of non-monetary compensation can be an effective way to achieve these things.
I should say that as I’m using the term here, non-monetary compensation includes things provided in some form other than dollars. But many forms—such as a restaurant gift certificate or tickets to a baseball game—likely will cost the practice something to provide. They also could be taxable to the doctor (i.e. should be reported on a W-2 statement), and Stark laws apply.
When discussing a citizenship bonus in my November 2011 column (see “Good Citizenship,” p. 53), I mentioned Daniel Pink’s book Drive: The Surprising Truth About What Motivates Us. In it, he argues that “Carrots and sticks are so last-century. We need to upgrade to autonomy, mastery, and purpose.” I’ll discuss forms of non-monetary compensation that fall into a modified version of Pink’s three upgrade categories.
Recognition
When is the last time a hospitalist leader or hospital executive sent a handwritten note of thanks and recognition to a hospitalist? It costs nothing, and it can be brief. Variations on this theme include awarding a plaque or trophy at a group meeting, or having an annual social event, such as a holiday party, that includes expressions of praise and gratitude for accomplishments in front of all the hospitalists and their significant others.
SHM past president Joseph Ming Wah Li, MD, SFHM, presides over his group’s annual “Hospy Awards,” a name inspired by ESPN’s ESPY Awards. Nurses, case managers, and residents vote for different awards and are asked to provide written comments about the doctor they’re voting for. Joe reads comments about both the winners and other hospitalists. The group has several additional social events each year, and photos from these are posted on the Internet.
Some hospital CEOs or other leaders periodically invite hospitalists to their homes for a dinner as a way of recognizing their work, as well as to build relationships and connectedness.
I was co-presenter in a session at HM12 in San Diego. Attendees had several terrific suggestions, including:
- Sending a note to the hospitalist’s significant other, rather than the hospitalist herself, expressing thanks for sharing her with us. Doing so is a way of acknowledging the good work of the hospitalist and the potential sacrifice of his or her family behind it. A short note of thanks with a restaurant gift certificate, so that hospitalist and a significant other can have dinner out paid for by the practice, seems like a great idea.
- Another idea that on the surface seems pretty silly, but likely has real value, is to identify a “superhero hospitalist” at some or all monthly group meetings. The group leader who brought it up does this by superimposing a photo of the doctor’s head onto a picture of a superhero like Superman and projects it during the meeting while saying something about the good work done to earn it. While silly, it has created some interest within the group regarding who the next winner will be and which superhero the honoree will be.
Promotion
Promoting a doctor into a position with greater responsibility, and perhaps a little (OK, maybe very little) prestige can be a valuable form of non-monetary compensation. A promotion could be as small as electing a doctor to serve on the hospitalist group’s own advisory committee, or representing the group at the hospital’s medical executive committee or other leadership group. More significant promotions could be having the hospitalist serve as medical director for case management or a clinical activity, such as palliative care; these positions often include additional monetary compensation.
SHM offers recognition in the form of fellowship and the opportunity for promotion to Senior Fellow in Hospital Medicine and Master of Hospital Medicine status. This can be seen as a promotion.
Professional Development
I think it is pretty tough to work an entire career devoted solely to patient care in any field, not just hospitalist practice. In June 2011 (see “Good Advice, Bad Advice,” p. 46), I wrote about the value of every hospitalist having at least a few additional professional interests and activities. A practice can encourage development of new interests and career roles, and make some available as a reward and recognition for good performance. Examples include sending your superstar doctors to SHM’s Leadership Academy, or even enroll them in a course to expand their clinical skill set, such as a procedures course or one that teaches interpretation of carotid ultrasounds or echocardiograms. An institution might find it worthwhile to reward the right doctor by paying their tuition at an executive MHA or MBA program.
It is all too easy to think that salary and benefits are the only rewards—i.e., compensation—that matter. Yet, in addition to money, all of us seek rewards in recognition, promotion, and professional development, and every practice should think deliberately about whether there are valuable opportunities in these categories.
I’d love to hear from anyone who has put in place novel and effective non-monetary compensation.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Well-designed forms of non-monetary compensation can have a greater impact on a hospitalist than providing a reward in dollars. This is true for any employee in any enterprise. It can have a greater impact than dollars in making a doctor feel appreciated and committed to the work of the organization. For example, a $100 gift certificate at a nice local restaurant can have a lot more impact and value than adding an extra $100 to the next paycheck.
A hospitalist’s salary and typical benefits (e.g. health insurance and retirement plan) must be attractive and competitive in the marketplace (obviously), but they are typically seen as entitlements, so they aren’t very effective at improving retention or motivating a doctor to perform well. Various forms of non-monetary compensation can be an effective way to achieve these things.
I should say that as I’m using the term here, non-monetary compensation includes things provided in some form other than dollars. But many forms—such as a restaurant gift certificate or tickets to a baseball game—likely will cost the practice something to provide. They also could be taxable to the doctor (i.e. should be reported on a W-2 statement), and Stark laws apply.
When discussing a citizenship bonus in my November 2011 column (see “Good Citizenship,” p. 53), I mentioned Daniel Pink’s book Drive: The Surprising Truth About What Motivates Us. In it, he argues that “Carrots and sticks are so last-century. We need to upgrade to autonomy, mastery, and purpose.” I’ll discuss forms of non-monetary compensation that fall into a modified version of Pink’s three upgrade categories.
Recognition
When is the last time a hospitalist leader or hospital executive sent a handwritten note of thanks and recognition to a hospitalist? It costs nothing, and it can be brief. Variations on this theme include awarding a plaque or trophy at a group meeting, or having an annual social event, such as a holiday party, that includes expressions of praise and gratitude for accomplishments in front of all the hospitalists and their significant others.
SHM past president Joseph Ming Wah Li, MD, SFHM, presides over his group’s annual “Hospy Awards,” a name inspired by ESPN’s ESPY Awards. Nurses, case managers, and residents vote for different awards and are asked to provide written comments about the doctor they’re voting for. Joe reads comments about both the winners and other hospitalists. The group has several additional social events each year, and photos from these are posted on the Internet.
Some hospital CEOs or other leaders periodically invite hospitalists to their homes for a dinner as a way of recognizing their work, as well as to build relationships and connectedness.
I was co-presenter in a session at HM12 in San Diego. Attendees had several terrific suggestions, including:
- Sending a note to the hospitalist’s significant other, rather than the hospitalist herself, expressing thanks for sharing her with us. Doing so is a way of acknowledging the good work of the hospitalist and the potential sacrifice of his or her family behind it. A short note of thanks with a restaurant gift certificate, so that hospitalist and a significant other can have dinner out paid for by the practice, seems like a great idea.
- Another idea that on the surface seems pretty silly, but likely has real value, is to identify a “superhero hospitalist” at some or all monthly group meetings. The group leader who brought it up does this by superimposing a photo of the doctor’s head onto a picture of a superhero like Superman and projects it during the meeting while saying something about the good work done to earn it. While silly, it has created some interest within the group regarding who the next winner will be and which superhero the honoree will be.
Promotion
Promoting a doctor into a position with greater responsibility, and perhaps a little (OK, maybe very little) prestige can be a valuable form of non-monetary compensation. A promotion could be as small as electing a doctor to serve on the hospitalist group’s own advisory committee, or representing the group at the hospital’s medical executive committee or other leadership group. More significant promotions could be having the hospitalist serve as medical director for case management or a clinical activity, such as palliative care; these positions often include additional monetary compensation.
SHM offers recognition in the form of fellowship and the opportunity for promotion to Senior Fellow in Hospital Medicine and Master of Hospital Medicine status. This can be seen as a promotion.
Professional Development
I think it is pretty tough to work an entire career devoted solely to patient care in any field, not just hospitalist practice. In June 2011 (see “Good Advice, Bad Advice,” p. 46), I wrote about the value of every hospitalist having at least a few additional professional interests and activities. A practice can encourage development of new interests and career roles, and make some available as a reward and recognition for good performance. Examples include sending your superstar doctors to SHM’s Leadership Academy, or even enroll them in a course to expand their clinical skill set, such as a procedures course or one that teaches interpretation of carotid ultrasounds or echocardiograms. An institution might find it worthwhile to reward the right doctor by paying their tuition at an executive MHA or MBA program.
It is all too easy to think that salary and benefits are the only rewards—i.e., compensation—that matter. Yet, in addition to money, all of us seek rewards in recognition, promotion, and professional development, and every practice should think deliberately about whether there are valuable opportunities in these categories.
I’d love to hear from anyone who has put in place novel and effective non-monetary compensation.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Well-designed forms of non-monetary compensation can have a greater impact on a hospitalist than providing a reward in dollars. This is true for any employee in any enterprise. It can have a greater impact than dollars in making a doctor feel appreciated and committed to the work of the organization. For example, a $100 gift certificate at a nice local restaurant can have a lot more impact and value than adding an extra $100 to the next paycheck.
A hospitalist’s salary and typical benefits (e.g. health insurance and retirement plan) must be attractive and competitive in the marketplace (obviously), but they are typically seen as entitlements, so they aren’t very effective at improving retention or motivating a doctor to perform well. Various forms of non-monetary compensation can be an effective way to achieve these things.
I should say that as I’m using the term here, non-monetary compensation includes things provided in some form other than dollars. But many forms—such as a restaurant gift certificate or tickets to a baseball game—likely will cost the practice something to provide. They also could be taxable to the doctor (i.e. should be reported on a W-2 statement), and Stark laws apply.
When discussing a citizenship bonus in my November 2011 column (see “Good Citizenship,” p. 53), I mentioned Daniel Pink’s book Drive: The Surprising Truth About What Motivates Us. In it, he argues that “Carrots and sticks are so last-century. We need to upgrade to autonomy, mastery, and purpose.” I’ll discuss forms of non-monetary compensation that fall into a modified version of Pink’s three upgrade categories.
Recognition
When is the last time a hospitalist leader or hospital executive sent a handwritten note of thanks and recognition to a hospitalist? It costs nothing, and it can be brief. Variations on this theme include awarding a plaque or trophy at a group meeting, or having an annual social event, such as a holiday party, that includes expressions of praise and gratitude for accomplishments in front of all the hospitalists and their significant others.
SHM past president Joseph Ming Wah Li, MD, SFHM, presides over his group’s annual “Hospy Awards,” a name inspired by ESPN’s ESPY Awards. Nurses, case managers, and residents vote for different awards and are asked to provide written comments about the doctor they’re voting for. Joe reads comments about both the winners and other hospitalists. The group has several additional social events each year, and photos from these are posted on the Internet.
Some hospital CEOs or other leaders periodically invite hospitalists to their homes for a dinner as a way of recognizing their work, as well as to build relationships and connectedness.
I was co-presenter in a session at HM12 in San Diego. Attendees had several terrific suggestions, including:
- Sending a note to the hospitalist’s significant other, rather than the hospitalist herself, expressing thanks for sharing her with us. Doing so is a way of acknowledging the good work of the hospitalist and the potential sacrifice of his or her family behind it. A short note of thanks with a restaurant gift certificate, so that hospitalist and a significant other can have dinner out paid for by the practice, seems like a great idea.
- Another idea that on the surface seems pretty silly, but likely has real value, is to identify a “superhero hospitalist” at some or all monthly group meetings. The group leader who brought it up does this by superimposing a photo of the doctor’s head onto a picture of a superhero like Superman and projects it during the meeting while saying something about the good work done to earn it. While silly, it has created some interest within the group regarding who the next winner will be and which superhero the honoree will be.
Promotion
Promoting a doctor into a position with greater responsibility, and perhaps a little (OK, maybe very little) prestige can be a valuable form of non-monetary compensation. A promotion could be as small as electing a doctor to serve on the hospitalist group’s own advisory committee, or representing the group at the hospital’s medical executive committee or other leadership group. More significant promotions could be having the hospitalist serve as medical director for case management or a clinical activity, such as palliative care; these positions often include additional monetary compensation.
SHM offers recognition in the form of fellowship and the opportunity for promotion to Senior Fellow in Hospital Medicine and Master of Hospital Medicine status. This can be seen as a promotion.
Professional Development
I think it is pretty tough to work an entire career devoted solely to patient care in any field, not just hospitalist practice. In June 2011 (see “Good Advice, Bad Advice,” p. 46), I wrote about the value of every hospitalist having at least a few additional professional interests and activities. A practice can encourage development of new interests and career roles, and make some available as a reward and recognition for good performance. Examples include sending your superstar doctors to SHM’s Leadership Academy, or even enroll them in a course to expand their clinical skill set, such as a procedures course or one that teaches interpretation of carotid ultrasounds or echocardiograms. An institution might find it worthwhile to reward the right doctor by paying their tuition at an executive MHA or MBA program.
It is all too easy to think that salary and benefits are the only rewards—i.e., compensation—that matter. Yet, in addition to money, all of us seek rewards in recognition, promotion, and professional development, and every practice should think deliberately about whether there are valuable opportunities in these categories.
I’d love to hear from anyone who has put in place novel and effective non-monetary compensation.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
John Nelson: Your Hospital Should Use Scripts to Describe Hospitalists to Patients
My anecdotal experience (no scientific research data) has convinced me that nearly every patient has some or all of the following questions or concerns when admitted by a hospitalist for the first time:
- Why is my usual doctor (PCP) not going to be in charge of my hospital care?
- Is the hospitalist a “real” doctor or someone in training, and whatdoes my regular doctor think of the hospitalist?
- Does the arrival of the hospitalist mean my long-term relationship with my PCP has been severed and I’ll see the hospitalist for all care (inpatient and outpatient) from now on?
- How will the hospitalist know my medical history, and will she communicate with my PCP?
Ideally, all communication about the hospitalist as an individual and the whole system of hospitalist care should help answer these questions and reassure the patient. Sadly, many people at the hospital unwittingly do the opposite.
Unintentional Undermining of Patient Confidence
Despite good intentions, doctors and nurses at the hospital often describe hospitalists to patients in a way that undermines the patients’ satisfaction and confidence in the hospitalist. They may say something like: Your doctor (PCP) doesn’t come to the hospital anymore and we have these doctors who are here all the time called hospitalists. I’ll ask one of them to see you.
To a patient, this might sound like he’s getting just any old doctor who happens to be around with nothing to do, rather than someone who specializes in the care of hospital patients and comes highly recommended by his PCP. The patient is left wondering why their “regular doctor” isn’t in charge of the hospital care, and often suspects the PCP has terminated their relationship or has been forced to refer by an insurance company when, in fact, the PCP chose to refer. Misunderstandings like these are a recipe for less satisfied and less confident patients.
Most hospitalist groups have a brochure explaining their practice, which addresses all of these points. (A simple Internet search for “hospitalist brochure patient information” or similar terms will reveal a number of good samples.) However, some patients never get a copy, and many won’t read it. So just having a brochure isn’t enough; there needs to be a way to ensure that all verbal communication serves to enlighten and reassure the patient.
Scripts for Nurses and Non-Hospitalist Physicians
Nurses and non-hospitalist doctors might not realize they’re sowing seeds of unhappiness in how they describe the hospitalist. Targeted education usually is necessary and can provide them with a new way of talking about the hospitalist. In most cases, it will be most effective to provide them with a script to use. For example, they could say: Your doctor has decided to focus her practice on the office to be more available to you there. As a result, she has decided to refer you to Dr. Bonamassa, a doctor who specializes in the care of hospitalized patients with problems like yours. Dr. Bonamassa will communicate with your primary doctor, and you should plan to follow up with her when you are discharged.
Or:
Your doctor has asked Dr. Trucks to take care of you while you are in the hospital. He is a specialist in the care of hospitalized patients and works with a team of doctors who are in the hospital 24 hours a day. Dr. Trucks will be your main doctor while you are in the hospital.
The Two Most Valuable Things For A Patient To Hear Are...
- That their PCP is in favor of the referral to a hospitalist, and that the patient’s relationship with the PCP will remain intact. Many patients worry that the arrival of the hospitalist means they won’t see their PCP ever again. Hence, the value in mentioning the patient will follow up with their usual PCP after discharge.
- That the hospitalist is a doctor devoted to the care of hospitalized patients, or a specialist in hospital care, rather than just a doctor who happens to be available.
My experience is that some PCPs worry that their patients might think less of them if they don’t provide hospital care. So despite good intentions, these PCPs’ words, demeanor, or body language could communicate unhappiness in, or something other than enthusiasm for, the hospitalist. The PCP may tell the patient something like, “I’m sending you to the hospital where you’ll be seen by a hospitalist, but I’ll be involved or overseeing everything.” This might be said with the intention of reassuring the patient, but it has the effect of undermining the patient’s confidence in the hospitalist. Such PCPs would benefit from adopting a better script.
It takes a reasonable amount of encouragement and cajoling to get others to adopt a script like I’ve suggested above, and requires periodic remedial education to ensure it isn’t abandoned in favor of old habits. But it is worth the effort.
Ensure Others Know the Hospitalist’s Name
Using the above scripts will have limited value if others don’t have a way of knowing the name of the hospitalist who will actually see the patient. If a worried family walks out of a room and asks the nurse, “Who is taking care of my father?” it is a lot better for the nurse to respond with the hospitalist’s name rather than “Your father is on the gold service, and the gold team doctor will be around later. I’m not sure which doctor has the gold service today.”
Try to ensure that everyone at the hospital knows which hospitalist is caring for every patient every day.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course
.
My anecdotal experience (no scientific research data) has convinced me that nearly every patient has some or all of the following questions or concerns when admitted by a hospitalist for the first time:
- Why is my usual doctor (PCP) not going to be in charge of my hospital care?
- Is the hospitalist a “real” doctor or someone in training, and whatdoes my regular doctor think of the hospitalist?
- Does the arrival of the hospitalist mean my long-term relationship with my PCP has been severed and I’ll see the hospitalist for all care (inpatient and outpatient) from now on?
- How will the hospitalist know my medical history, and will she communicate with my PCP?
Ideally, all communication about the hospitalist as an individual and the whole system of hospitalist care should help answer these questions and reassure the patient. Sadly, many people at the hospital unwittingly do the opposite.
Unintentional Undermining of Patient Confidence
Despite good intentions, doctors and nurses at the hospital often describe hospitalists to patients in a way that undermines the patients’ satisfaction and confidence in the hospitalist. They may say something like: Your doctor (PCP) doesn’t come to the hospital anymore and we have these doctors who are here all the time called hospitalists. I’ll ask one of them to see you.
To a patient, this might sound like he’s getting just any old doctor who happens to be around with nothing to do, rather than someone who specializes in the care of hospital patients and comes highly recommended by his PCP. The patient is left wondering why their “regular doctor” isn’t in charge of the hospital care, and often suspects the PCP has terminated their relationship or has been forced to refer by an insurance company when, in fact, the PCP chose to refer. Misunderstandings like these are a recipe for less satisfied and less confident patients.
Most hospitalist groups have a brochure explaining their practice, which addresses all of these points. (A simple Internet search for “hospitalist brochure patient information” or similar terms will reveal a number of good samples.) However, some patients never get a copy, and many won’t read it. So just having a brochure isn’t enough; there needs to be a way to ensure that all verbal communication serves to enlighten and reassure the patient.
Scripts for Nurses and Non-Hospitalist Physicians
Nurses and non-hospitalist doctors might not realize they’re sowing seeds of unhappiness in how they describe the hospitalist. Targeted education usually is necessary and can provide them with a new way of talking about the hospitalist. In most cases, it will be most effective to provide them with a script to use. For example, they could say: Your doctor has decided to focus her practice on the office to be more available to you there. As a result, she has decided to refer you to Dr. Bonamassa, a doctor who specializes in the care of hospitalized patients with problems like yours. Dr. Bonamassa will communicate with your primary doctor, and you should plan to follow up with her when you are discharged.
Or:
Your doctor has asked Dr. Trucks to take care of you while you are in the hospital. He is a specialist in the care of hospitalized patients and works with a team of doctors who are in the hospital 24 hours a day. Dr. Trucks will be your main doctor while you are in the hospital.
The Two Most Valuable Things For A Patient To Hear Are...
- That their PCP is in favor of the referral to a hospitalist, and that the patient’s relationship with the PCP will remain intact. Many patients worry that the arrival of the hospitalist means they won’t see their PCP ever again. Hence, the value in mentioning the patient will follow up with their usual PCP after discharge.
- That the hospitalist is a doctor devoted to the care of hospitalized patients, or a specialist in hospital care, rather than just a doctor who happens to be available.
My experience is that some PCPs worry that their patients might think less of them if they don’t provide hospital care. So despite good intentions, these PCPs’ words, demeanor, or body language could communicate unhappiness in, or something other than enthusiasm for, the hospitalist. The PCP may tell the patient something like, “I’m sending you to the hospital where you’ll be seen by a hospitalist, but I’ll be involved or overseeing everything.” This might be said with the intention of reassuring the patient, but it has the effect of undermining the patient’s confidence in the hospitalist. Such PCPs would benefit from adopting a better script.
It takes a reasonable amount of encouragement and cajoling to get others to adopt a script like I’ve suggested above, and requires periodic remedial education to ensure it isn’t abandoned in favor of old habits. But it is worth the effort.
Ensure Others Know the Hospitalist’s Name
Using the above scripts will have limited value if others don’t have a way of knowing the name of the hospitalist who will actually see the patient. If a worried family walks out of a room and asks the nurse, “Who is taking care of my father?” it is a lot better for the nurse to respond with the hospitalist’s name rather than “Your father is on the gold service, and the gold team doctor will be around later. I’m not sure which doctor has the gold service today.”
Try to ensure that everyone at the hospital knows which hospitalist is caring for every patient every day.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course
.
My anecdotal experience (no scientific research data) has convinced me that nearly every patient has some or all of the following questions or concerns when admitted by a hospitalist for the first time:
- Why is my usual doctor (PCP) not going to be in charge of my hospital care?
- Is the hospitalist a “real” doctor or someone in training, and whatdoes my regular doctor think of the hospitalist?
- Does the arrival of the hospitalist mean my long-term relationship with my PCP has been severed and I’ll see the hospitalist for all care (inpatient and outpatient) from now on?
- How will the hospitalist know my medical history, and will she communicate with my PCP?
Ideally, all communication about the hospitalist as an individual and the whole system of hospitalist care should help answer these questions and reassure the patient. Sadly, many people at the hospital unwittingly do the opposite.
Unintentional Undermining of Patient Confidence
Despite good intentions, doctors and nurses at the hospital often describe hospitalists to patients in a way that undermines the patients’ satisfaction and confidence in the hospitalist. They may say something like: Your doctor (PCP) doesn’t come to the hospital anymore and we have these doctors who are here all the time called hospitalists. I’ll ask one of them to see you.
To a patient, this might sound like he’s getting just any old doctor who happens to be around with nothing to do, rather than someone who specializes in the care of hospital patients and comes highly recommended by his PCP. The patient is left wondering why their “regular doctor” isn’t in charge of the hospital care, and often suspects the PCP has terminated their relationship or has been forced to refer by an insurance company when, in fact, the PCP chose to refer. Misunderstandings like these are a recipe for less satisfied and less confident patients.
Most hospitalist groups have a brochure explaining their practice, which addresses all of these points. (A simple Internet search for “hospitalist brochure patient information” or similar terms will reveal a number of good samples.) However, some patients never get a copy, and many won’t read it. So just having a brochure isn’t enough; there needs to be a way to ensure that all verbal communication serves to enlighten and reassure the patient.
Scripts for Nurses and Non-Hospitalist Physicians
Nurses and non-hospitalist doctors might not realize they’re sowing seeds of unhappiness in how they describe the hospitalist. Targeted education usually is necessary and can provide them with a new way of talking about the hospitalist. In most cases, it will be most effective to provide them with a script to use. For example, they could say: Your doctor has decided to focus her practice on the office to be more available to you there. As a result, she has decided to refer you to Dr. Bonamassa, a doctor who specializes in the care of hospitalized patients with problems like yours. Dr. Bonamassa will communicate with your primary doctor, and you should plan to follow up with her when you are discharged.
Or:
Your doctor has asked Dr. Trucks to take care of you while you are in the hospital. He is a specialist in the care of hospitalized patients and works with a team of doctors who are in the hospital 24 hours a day. Dr. Trucks will be your main doctor while you are in the hospital.
The Two Most Valuable Things For A Patient To Hear Are...
- That their PCP is in favor of the referral to a hospitalist, and that the patient’s relationship with the PCP will remain intact. Many patients worry that the arrival of the hospitalist means they won’t see their PCP ever again. Hence, the value in mentioning the patient will follow up with their usual PCP after discharge.
- That the hospitalist is a doctor devoted to the care of hospitalized patients, or a specialist in hospital care, rather than just a doctor who happens to be available.
My experience is that some PCPs worry that their patients might think less of them if they don’t provide hospital care. So despite good intentions, these PCPs’ words, demeanor, or body language could communicate unhappiness in, or something other than enthusiasm for, the hospitalist. The PCP may tell the patient something like, “I’m sending you to the hospital where you’ll be seen by a hospitalist, but I’ll be involved or overseeing everything.” This might be said with the intention of reassuring the patient, but it has the effect of undermining the patient’s confidence in the hospitalist. Such PCPs would benefit from adopting a better script.
It takes a reasonable amount of encouragement and cajoling to get others to adopt a script like I’ve suggested above, and requires periodic remedial education to ensure it isn’t abandoned in favor of old habits. But it is worth the effort.
Ensure Others Know the Hospitalist’s Name
Using the above scripts will have limited value if others don’t have a way of knowing the name of the hospitalist who will actually see the patient. If a worried family walks out of a room and asks the nurse, “Who is taking care of my father?” it is a lot better for the nurse to respond with the hospitalist’s name rather than “Your father is on the gold service, and the gold team doctor will be around later. I’m not sure which doctor has the gold service today.”
Try to ensure that everyone at the hospital knows which hospitalist is caring for every patient every day.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is course co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course
.
HM12 Pre-course Analysis: How to Improve Performance in CMS Valued Based Purchasing Program
As part of the Affordable Care Act, the value-based purchasing program (VBP) is being rolled out this year. Beginning in October, VBP will put hospitals at financial risk for a defined set of clinical and patient satisfaction metrics. Because of the significant impact that this will have on hospitals and HM, SHM had a pre-course focused on this topic at HM12.
Pat Torscon and Joe Miller led the pre-course, which focused on VBP's key components. Through a series of vignettes and studies, the faculty provided nearly 100 attendess a better understanding of the impact.
Key Takeaways
1. VBP is budget neutral. Some Hospitals will receive bonuses, some will not. This will depend on where hospitals fall in the performance score. To receive a bonus, a hospital will have to exceed the 50% threshold. If below, then no opportunity for performance bonus. The model is based on a floor, a threshold (50%), and benchmark, which is presently a bell-shaped curve.
2. The performance score will be 70% clinical process domain and 30% patient experience domain. Hospitalists will have a major role in the perfromance measures around AMI, CHF, pneumonia, SCIP, and patient experience.
3. Hospitalists will need to understand the data and where it comes from. When you combine VBP, Inpatient Quality Reporting, readmissions, hospital-acquired conditions, and meaningful use, the actual amount of payment at risk is 7%. With most hospital profit margins around 1-3% this amount will be significant. Of those hospitals that have been studied, 10% in high performance, and 74% were inconsistent performance across four clinical measures.
4. Concurrent patient management will be important. Hospitalists will become the drivers and champions of this. To move either your HCAHPS score or Press Ganey performance scores will take time. It is important to convey that to the C-suite. An example of the impact of VBP for a 146-bed hospital over five years could be more than $5 million at stake; a 541-bed hospital would be $40 million.
As part of the Affordable Care Act, the value-based purchasing program (VBP) is being rolled out this year. Beginning in October, VBP will put hospitals at financial risk for a defined set of clinical and patient satisfaction metrics. Because of the significant impact that this will have on hospitals and HM, SHM had a pre-course focused on this topic at HM12.
Pat Torscon and Joe Miller led the pre-course, which focused on VBP's key components. Through a series of vignettes and studies, the faculty provided nearly 100 attendess a better understanding of the impact.
Key Takeaways
1. VBP is budget neutral. Some Hospitals will receive bonuses, some will not. This will depend on where hospitals fall in the performance score. To receive a bonus, a hospital will have to exceed the 50% threshold. If below, then no opportunity for performance bonus. The model is based on a floor, a threshold (50%), and benchmark, which is presently a bell-shaped curve.
2. The performance score will be 70% clinical process domain and 30% patient experience domain. Hospitalists will have a major role in the perfromance measures around AMI, CHF, pneumonia, SCIP, and patient experience.
3. Hospitalists will need to understand the data and where it comes from. When you combine VBP, Inpatient Quality Reporting, readmissions, hospital-acquired conditions, and meaningful use, the actual amount of payment at risk is 7%. With most hospital profit margins around 1-3% this amount will be significant. Of those hospitals that have been studied, 10% in high performance, and 74% were inconsistent performance across four clinical measures.
4. Concurrent patient management will be important. Hospitalists will become the drivers and champions of this. To move either your HCAHPS score or Press Ganey performance scores will take time. It is important to convey that to the C-suite. An example of the impact of VBP for a 146-bed hospital over five years could be more than $5 million at stake; a 541-bed hospital would be $40 million.
As part of the Affordable Care Act, the value-based purchasing program (VBP) is being rolled out this year. Beginning in October, VBP will put hospitals at financial risk for a defined set of clinical and patient satisfaction metrics. Because of the significant impact that this will have on hospitals and HM, SHM had a pre-course focused on this topic at HM12.
Pat Torscon and Joe Miller led the pre-course, which focused on VBP's key components. Through a series of vignettes and studies, the faculty provided nearly 100 attendess a better understanding of the impact.
Key Takeaways
1. VBP is budget neutral. Some Hospitals will receive bonuses, some will not. This will depend on where hospitals fall in the performance score. To receive a bonus, a hospital will have to exceed the 50% threshold. If below, then no opportunity for performance bonus. The model is based on a floor, a threshold (50%), and benchmark, which is presently a bell-shaped curve.
2. The performance score will be 70% clinical process domain and 30% patient experience domain. Hospitalists will have a major role in the perfromance measures around AMI, CHF, pneumonia, SCIP, and patient experience.
3. Hospitalists will need to understand the data and where it comes from. When you combine VBP, Inpatient Quality Reporting, readmissions, hospital-acquired conditions, and meaningful use, the actual amount of payment at risk is 7%. With most hospital profit margins around 1-3% this amount will be significant. Of those hospitals that have been studied, 10% in high performance, and 74% were inconsistent performance across four clinical measures.
4. Concurrent patient management will be important. Hospitalists will become the drivers and champions of this. To move either your HCAHPS score or Press Ganey performance scores will take time. It is important to convey that to the C-suite. An example of the impact of VBP for a 146-bed hospital over five years could be more than $5 million at stake; a 541-bed hospital would be $40 million.