User login
When Should Antiplatelet Agents and Anticoagulants Be Restarted after Gastrointestinal Bleed?
Source: Adapted from Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
Two Cases
A 76-year-old female with a history of hypertension, diabetes, atrial fibrillation, and diverticulosis is admitted with acute onset of dizziness and several episodes of bright red blood per rectum. Her labs show a new anemia at hemoglobin level 6.9 g/dL and an international normalized ratio (INR) of 2.7. She is transfused several units of packed red blood cells and fresh frozen plasma without further bleeding. She undergoes an esophagogastroduodenoscopy (EGD) and colonoscopy, which are notable only for extensive diverticulosis. In preparing the discharge medication reconciliation, you are uncertain what to do with the patient’s anticoagulation.
An 85-year-old male with coronary artery disease status post-percutaneous coronary intervention, with placement of a drug-eluting stent several years prior, is admitted with multiple weeks of epigastric discomfort and acute onset of hematemesis. His laboratory tests are notable for a new anemia at hemoglobin level 6.5 g/dL. Urgent EGD demonstrates a bleeding ulcer, which is cauterized. He is started on a proton-pump inhibitor (PPI). He inquires as to when he can restart his home medications, including aspirin.
Overview
Gastrointestinal (GI) bleeding is a serious complication of anticoagulant and antiplatelet therapy. Risks for GI bleeding include older age, history of peptic ulcer disease, NSAID or steroid use, and the use of antiplatelet or anticoagulation therapy. The estimated incidence of GI bleeding in the general population is 48 to 160 cases (upper GI) and 21 cases (lower GI) per 1,000 adults per year, with a case-mortality rate between 5% and 14%.1
Although there is consensus on ceasing anticoagulant and antiplatelet agents during an acute GI bleed, debate remains over the appropriate approach to restarting these agents.
Anticoagulant Resumption
A recent study published in Archives of Internal Medicine supports a quick resumption of anticoagulation following a GI bleed.2 Although previous studies on restarting anticoagulants were small and demonstrated mixed results, this retrospective cohort study examined more than 442 warfarin-associated GI bleeds. After adjusting for various clinical indicators (e.g. clinical seriousness of bleeding, requirement of transfusions), the investigators found that the decision not to resume warfarin within 90 days of an initial GI hemorrhage was associated with an increased risk of thrombosis and death. Of note, in those patients restarted on warfarin, the mean time to medication initiation was four days following the initial GI bleed. In those not restarted on warfarin, the earliest incidence of thrombosis was documented at eight days following cessation of anticoagulation.2
Though its clinical implications are limited by the retrospective design, this study is helpful in guiding management decisions. Randomized control trials and society recommendations on this topic are lacking, so the decision to resume anticoagulants rests on patient-specific estimates of the risk of recurrent bleeding and the benefits of resuming anticoagulants.
In identifying those patients most likely to benefit from restarting anticoagulation, the risk of thromboembolism should be determined using an established risk stratification framework, such as Antithrombotic Therapy and Prevention of Thrombosis, 9th edition (see Table 1).3 According to the guidelines, patients at highest risk of thromboembolism (in the absence of anticoagulation) are those with:
- mitral valve prostheses;
- atrial fibrillation with a CHADS2 score of five to six or cerebrovascular accidents (CVA) within the last three months; and/or
- venous thromboembolism (VTE) within the last three months or history of severe thrombophilia.
Patients at the lowest risk of thromboembolism are those with:
- mechanical aortic prostheses with no other stroke risk factors;
- atrial fibrillation with a CHADS2 score of zero to two; and/or
- a single VTE that occurred >12 months prior.
There are several approaches to identifying patients at greatest risk for bleeding. Location-specific modeling for upper GI bleeds (e.g. Rockall score) and lower GI bleeds (e.g. BLEED score) focus on the clinical presentation and/or endoscopic findings. General hemorrhage risk scores (e.g. HAS-BLED, ATRIA) focus on medical comorbidities. While easy to use, the predictive value of such scores as part of anticoagulation resumption after a GI hemorrhage remains uncertain.
Based on the above methods of risk stratification, patients at higher risk of thromboembolism and lower risk of bleeding will likely benefit from waiting only a short time interval before restarting anticoagulation. Based on the trial conducted by Witt and colleagues, anticoagulation typically can be reinitiated within four days of obtaining hemostatic and hemodynamic stability.2 Conversely, those at highest risk of bleeding and lower risk of thromboembolism will benefit from a delayed resumption of anticoagulation. Involvement of a specialist, such as a gastroenterologist, could help further clarify the risk of rebleeding.
The ideal approach for patients with a high risk of both bleeding and thromboembolism remains uncertain. Such cases highlight the need for an informed discussion with the patient and any involved caregivers, as well as involvement of inpatient subspecialists and outpatient longitudinal providers.
There remains a lack of evidence on the best method to restart anticoagulation. Based on small and retrospective trials, we recommend restarting warfarin at the patient’s previous home dose. The duration of inpatient monitoring following warfarin initiation should be individualized, but warfarin is not expected to impair coagulation for four to six days after initiation.
Little data is available with respect to the role of novel oral anticoagulants after a GI bleed. Given the lack of reversing agents for these drugs, we recommend exercising caution in populations with a high risk of rebleeding. Theoretically, given that these agents reach peak effect faster than warfarin, waiting an additional four days after the time frame recommended for starting warfarin is a prudent resumption strategy for novel oral anticoagulants.
Source: Adapted from Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
Resumption of Antiplatelet Agents
The decision to resume antiplatelet therapy should also be highly individualized. In addition to weighing the risk of bleeding (as described in the previous section), the physician must also estimate the benefits of antiplatelet therapy in decreasing the risk of cardiovascular events.
In low-risk patients on antiplatelet therapy (i.e., for primary cardiovascular prevention) reinitiation after a bleeding episode can be reasonably delayed, because the risk of rebleeding likely outweighs the potential benefit of restarting therapy.
For patients who are at intermediate risk (i.e., those on antiplatelet agents for secondary prevention of cardiovascular disease), emerging evidence argues for early reinstitution after a GI bleed. In a trial published in Annals of Internal Medicine, Sung and colleagues randomized 156 patients to aspirin or placebo therapy immediately following endoscopically obtained hemostasis for peptic ulcer bleeding.4 All patients received PPIs. There was no significant difference in bleeding rates between the two groups, but delayed resumption of aspirin was associated with a significant increase in all-cause mortality.
Two recent meta-analyses provide further insight into the risks of withholding aspirin therapy. The first, which included 50,279 patients on aspirin for secondary prevention, found that aspirin non-adherence or withdrawal after a GI bleed was associated with a three-fold higher risk of major adverse cardiac events.5 Cardiac event rates were highest in the subgroup of patients with a history of prior percutaneous coronary stenting.
A second meta-analysis evaluated patients who had aspirin held perioperatively. In a population of patients on aspirin for secondary prevention, the mean time after withholding aspirin was 8.5 days to coronary events, 14.3 days to cerebrovascular events, and 25.8 days to peripheral arterial events.6 Events occurred as early as five days after withdrawal of aspirin.
Patients with recent intracoronary stenting are at highest risk of thrombosis. In patients with a bare metal stent placed within six weeks, or a drug-eluting stent placed within six months, every effort should be made to minimize interruptions of dual antiplatelet therapy.
Based on the data presented above, for patients at intermediate and/or high risk of adverse cardiac events, we recommend reinstitution of aspirin as soon as possible following a GI hemorrhage, preferably within five days. PPI co-therapy is a mainstay for secondary prevention of upper GI bleeding in patients on antiplatelet therapy. Current research and guidelines have not addressed specifically the role of withholding and reinitiating aspirin in lower GI bleeding, non-peptic ulcer, or upper-GI bleeding, however, a similar strategy is likely appropriate. As with the decision for restarting anticoagulants, discussion with relevant specialists is essential to best define the risk of re-bleeding.
Back to the Cases
Given her CHADS2 score of three, the patient with a diverticular bleed has a 9.6% annual risk of stroke if she does not resume anticoagulation. Using the HAS-BLED and ATRIA scores, this patient has 2.6% to 5.8% annual risk of hemorrhage. We recommend resuming warfarin anticoagulation therapy within four days of achieving hemostasis.
For the patient with coronary artery disease with remote drug-eluting stent placement and upper GI bleed, evidence supports early resumption of appropriate antiplatelet therapy following endoscopic therapy and hemostasis. We recommend resuming aspirin during the current hospitalization and concomitant treatment with a PPI indefinitely.
Bottom Line
Following a GI bleed, the risks and benefits of restarting anticoagulant and antiplatelet agents need to be carefully considered. In patients on oral anticoagulants at high risk for thromboembolism and low risk for rebleeding, consider restarting anticoagulation within four to five days. Patients on antiplatelet agents for secondary prevention should have the medication restarted during hospitalization after endoscopically obtained hemostasis of a peptic ulcer.
In all cases, hospitalists should engage the patient, gastroenterologist, and outpatient provider to best determine when resumption of anticoagulant and/or antiplatelet agents should occur.
Dr. Allen-Dicker is a hospitalist and clinical instructor at Mount Sinai Medical Center in New York City. Dr. Briones is director of perioperative services in the division of hospital medicine and an assistant professor; Dr. Berman is a hospitalist and a clinical instructor, and Dr. Dunn is a professor of medicine and chief of the division of hospital medicine, all at Mount Sinai Medical Center.
References
- Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152(2):101-113.
- Witt DM, Delate T, Garcia DA, et al. Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med. 2012;172(19):1484-1491.
- Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
- Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: A randomized trial. Ann Intern Med. 2010;152(1):1-9.
- Biondi-Zoccai GG, Lotrionte M, Agostoni P, et al. A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J. 2006;27(22):2667-2674.
- Burger W, Chemnitius JM, Kneissl GD, Rücker G. Low-dose aspirin for secondary cardiovascular prevention – cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation – review and meta-analysis. J Intern Med. 2005;257(5):399-414.
Source: Adapted from Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
Two Cases
A 76-year-old female with a history of hypertension, diabetes, atrial fibrillation, and diverticulosis is admitted with acute onset of dizziness and several episodes of bright red blood per rectum. Her labs show a new anemia at hemoglobin level 6.9 g/dL and an international normalized ratio (INR) of 2.7. She is transfused several units of packed red blood cells and fresh frozen plasma without further bleeding. She undergoes an esophagogastroduodenoscopy (EGD) and colonoscopy, which are notable only for extensive diverticulosis. In preparing the discharge medication reconciliation, you are uncertain what to do with the patient’s anticoagulation.
An 85-year-old male with coronary artery disease status post-percutaneous coronary intervention, with placement of a drug-eluting stent several years prior, is admitted with multiple weeks of epigastric discomfort and acute onset of hematemesis. His laboratory tests are notable for a new anemia at hemoglobin level 6.5 g/dL. Urgent EGD demonstrates a bleeding ulcer, which is cauterized. He is started on a proton-pump inhibitor (PPI). He inquires as to when he can restart his home medications, including aspirin.
Overview
Gastrointestinal (GI) bleeding is a serious complication of anticoagulant and antiplatelet therapy. Risks for GI bleeding include older age, history of peptic ulcer disease, NSAID or steroid use, and the use of antiplatelet or anticoagulation therapy. The estimated incidence of GI bleeding in the general population is 48 to 160 cases (upper GI) and 21 cases (lower GI) per 1,000 adults per year, with a case-mortality rate between 5% and 14%.1
Although there is consensus on ceasing anticoagulant and antiplatelet agents during an acute GI bleed, debate remains over the appropriate approach to restarting these agents.
Anticoagulant Resumption
A recent study published in Archives of Internal Medicine supports a quick resumption of anticoagulation following a GI bleed.2 Although previous studies on restarting anticoagulants were small and demonstrated mixed results, this retrospective cohort study examined more than 442 warfarin-associated GI bleeds. After adjusting for various clinical indicators (e.g. clinical seriousness of bleeding, requirement of transfusions), the investigators found that the decision not to resume warfarin within 90 days of an initial GI hemorrhage was associated with an increased risk of thrombosis and death. Of note, in those patients restarted on warfarin, the mean time to medication initiation was four days following the initial GI bleed. In those not restarted on warfarin, the earliest incidence of thrombosis was documented at eight days following cessation of anticoagulation.2
Though its clinical implications are limited by the retrospective design, this study is helpful in guiding management decisions. Randomized control trials and society recommendations on this topic are lacking, so the decision to resume anticoagulants rests on patient-specific estimates of the risk of recurrent bleeding and the benefits of resuming anticoagulants.
In identifying those patients most likely to benefit from restarting anticoagulation, the risk of thromboembolism should be determined using an established risk stratification framework, such as Antithrombotic Therapy and Prevention of Thrombosis, 9th edition (see Table 1).3 According to the guidelines, patients at highest risk of thromboembolism (in the absence of anticoagulation) are those with:
- mitral valve prostheses;
- atrial fibrillation with a CHADS2 score of five to six or cerebrovascular accidents (CVA) within the last three months; and/or
- venous thromboembolism (VTE) within the last three months or history of severe thrombophilia.
Patients at the lowest risk of thromboembolism are those with:
- mechanical aortic prostheses with no other stroke risk factors;
- atrial fibrillation with a CHADS2 score of zero to two; and/or
- a single VTE that occurred >12 months prior.
There are several approaches to identifying patients at greatest risk for bleeding. Location-specific modeling for upper GI bleeds (e.g. Rockall score) and lower GI bleeds (e.g. BLEED score) focus on the clinical presentation and/or endoscopic findings. General hemorrhage risk scores (e.g. HAS-BLED, ATRIA) focus on medical comorbidities. While easy to use, the predictive value of such scores as part of anticoagulation resumption after a GI hemorrhage remains uncertain.
Based on the above methods of risk stratification, patients at higher risk of thromboembolism and lower risk of bleeding will likely benefit from waiting only a short time interval before restarting anticoagulation. Based on the trial conducted by Witt and colleagues, anticoagulation typically can be reinitiated within four days of obtaining hemostatic and hemodynamic stability.2 Conversely, those at highest risk of bleeding and lower risk of thromboembolism will benefit from a delayed resumption of anticoagulation. Involvement of a specialist, such as a gastroenterologist, could help further clarify the risk of rebleeding.
The ideal approach for patients with a high risk of both bleeding and thromboembolism remains uncertain. Such cases highlight the need for an informed discussion with the patient and any involved caregivers, as well as involvement of inpatient subspecialists and outpatient longitudinal providers.
There remains a lack of evidence on the best method to restart anticoagulation. Based on small and retrospective trials, we recommend restarting warfarin at the patient’s previous home dose. The duration of inpatient monitoring following warfarin initiation should be individualized, but warfarin is not expected to impair coagulation for four to six days after initiation.
Little data is available with respect to the role of novel oral anticoagulants after a GI bleed. Given the lack of reversing agents for these drugs, we recommend exercising caution in populations with a high risk of rebleeding. Theoretically, given that these agents reach peak effect faster than warfarin, waiting an additional four days after the time frame recommended for starting warfarin is a prudent resumption strategy for novel oral anticoagulants.
Source: Adapted from Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
Resumption of Antiplatelet Agents
The decision to resume antiplatelet therapy should also be highly individualized. In addition to weighing the risk of bleeding (as described in the previous section), the physician must also estimate the benefits of antiplatelet therapy in decreasing the risk of cardiovascular events.
In low-risk patients on antiplatelet therapy (i.e., for primary cardiovascular prevention) reinitiation after a bleeding episode can be reasonably delayed, because the risk of rebleeding likely outweighs the potential benefit of restarting therapy.
For patients who are at intermediate risk (i.e., those on antiplatelet agents for secondary prevention of cardiovascular disease), emerging evidence argues for early reinstitution after a GI bleed. In a trial published in Annals of Internal Medicine, Sung and colleagues randomized 156 patients to aspirin or placebo therapy immediately following endoscopically obtained hemostasis for peptic ulcer bleeding.4 All patients received PPIs. There was no significant difference in bleeding rates between the two groups, but delayed resumption of aspirin was associated with a significant increase in all-cause mortality.
Two recent meta-analyses provide further insight into the risks of withholding aspirin therapy. The first, which included 50,279 patients on aspirin for secondary prevention, found that aspirin non-adherence or withdrawal after a GI bleed was associated with a three-fold higher risk of major adverse cardiac events.5 Cardiac event rates were highest in the subgroup of patients with a history of prior percutaneous coronary stenting.
A second meta-analysis evaluated patients who had aspirin held perioperatively. In a population of patients on aspirin for secondary prevention, the mean time after withholding aspirin was 8.5 days to coronary events, 14.3 days to cerebrovascular events, and 25.8 days to peripheral arterial events.6 Events occurred as early as five days after withdrawal of aspirin.
Patients with recent intracoronary stenting are at highest risk of thrombosis. In patients with a bare metal stent placed within six weeks, or a drug-eluting stent placed within six months, every effort should be made to minimize interruptions of dual antiplatelet therapy.
Based on the data presented above, for patients at intermediate and/or high risk of adverse cardiac events, we recommend reinstitution of aspirin as soon as possible following a GI hemorrhage, preferably within five days. PPI co-therapy is a mainstay for secondary prevention of upper GI bleeding in patients on antiplatelet therapy. Current research and guidelines have not addressed specifically the role of withholding and reinitiating aspirin in lower GI bleeding, non-peptic ulcer, or upper-GI bleeding, however, a similar strategy is likely appropriate. As with the decision for restarting anticoagulants, discussion with relevant specialists is essential to best define the risk of re-bleeding.
Back to the Cases
Given her CHADS2 score of three, the patient with a diverticular bleed has a 9.6% annual risk of stroke if she does not resume anticoagulation. Using the HAS-BLED and ATRIA scores, this patient has 2.6% to 5.8% annual risk of hemorrhage. We recommend resuming warfarin anticoagulation therapy within four days of achieving hemostasis.
For the patient with coronary artery disease with remote drug-eluting stent placement and upper GI bleed, evidence supports early resumption of appropriate antiplatelet therapy following endoscopic therapy and hemostasis. We recommend resuming aspirin during the current hospitalization and concomitant treatment with a PPI indefinitely.
Bottom Line
Following a GI bleed, the risks and benefits of restarting anticoagulant and antiplatelet agents need to be carefully considered. In patients on oral anticoagulants at high risk for thromboembolism and low risk for rebleeding, consider restarting anticoagulation within four to five days. Patients on antiplatelet agents for secondary prevention should have the medication restarted during hospitalization after endoscopically obtained hemostasis of a peptic ulcer.
In all cases, hospitalists should engage the patient, gastroenterologist, and outpatient provider to best determine when resumption of anticoagulant and/or antiplatelet agents should occur.
Dr. Allen-Dicker is a hospitalist and clinical instructor at Mount Sinai Medical Center in New York City. Dr. Briones is director of perioperative services in the division of hospital medicine and an assistant professor; Dr. Berman is a hospitalist and a clinical instructor, and Dr. Dunn is a professor of medicine and chief of the division of hospital medicine, all at Mount Sinai Medical Center.
References
- Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152(2):101-113.
- Witt DM, Delate T, Garcia DA, et al. Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med. 2012;172(19):1484-1491.
- Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
- Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: A randomized trial. Ann Intern Med. 2010;152(1):1-9.
- Biondi-Zoccai GG, Lotrionte M, Agostoni P, et al. A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J. 2006;27(22):2667-2674.
- Burger W, Chemnitius JM, Kneissl GD, Rücker G. Low-dose aspirin for secondary cardiovascular prevention – cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation – review and meta-analysis. J Intern Med. 2005;257(5):399-414.
Source: Adapted from Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
Two Cases
A 76-year-old female with a history of hypertension, diabetes, atrial fibrillation, and diverticulosis is admitted with acute onset of dizziness and several episodes of bright red blood per rectum. Her labs show a new anemia at hemoglobin level 6.9 g/dL and an international normalized ratio (INR) of 2.7. She is transfused several units of packed red blood cells and fresh frozen plasma without further bleeding. She undergoes an esophagogastroduodenoscopy (EGD) and colonoscopy, which are notable only for extensive diverticulosis. In preparing the discharge medication reconciliation, you are uncertain what to do with the patient’s anticoagulation.
An 85-year-old male with coronary artery disease status post-percutaneous coronary intervention, with placement of a drug-eluting stent several years prior, is admitted with multiple weeks of epigastric discomfort and acute onset of hematemesis. His laboratory tests are notable for a new anemia at hemoglobin level 6.5 g/dL. Urgent EGD demonstrates a bleeding ulcer, which is cauterized. He is started on a proton-pump inhibitor (PPI). He inquires as to when he can restart his home medications, including aspirin.
Overview
Gastrointestinal (GI) bleeding is a serious complication of anticoagulant and antiplatelet therapy. Risks for GI bleeding include older age, history of peptic ulcer disease, NSAID or steroid use, and the use of antiplatelet or anticoagulation therapy. The estimated incidence of GI bleeding in the general population is 48 to 160 cases (upper GI) and 21 cases (lower GI) per 1,000 adults per year, with a case-mortality rate between 5% and 14%.1
Although there is consensus on ceasing anticoagulant and antiplatelet agents during an acute GI bleed, debate remains over the appropriate approach to restarting these agents.
Anticoagulant Resumption
A recent study published in Archives of Internal Medicine supports a quick resumption of anticoagulation following a GI bleed.2 Although previous studies on restarting anticoagulants were small and demonstrated mixed results, this retrospective cohort study examined more than 442 warfarin-associated GI bleeds. After adjusting for various clinical indicators (e.g. clinical seriousness of bleeding, requirement of transfusions), the investigators found that the decision not to resume warfarin within 90 days of an initial GI hemorrhage was associated with an increased risk of thrombosis and death. Of note, in those patients restarted on warfarin, the mean time to medication initiation was four days following the initial GI bleed. In those not restarted on warfarin, the earliest incidence of thrombosis was documented at eight days following cessation of anticoagulation.2
Though its clinical implications are limited by the retrospective design, this study is helpful in guiding management decisions. Randomized control trials and society recommendations on this topic are lacking, so the decision to resume anticoagulants rests on patient-specific estimates of the risk of recurrent bleeding and the benefits of resuming anticoagulants.
In identifying those patients most likely to benefit from restarting anticoagulation, the risk of thromboembolism should be determined using an established risk stratification framework, such as Antithrombotic Therapy and Prevention of Thrombosis, 9th edition (see Table 1).3 According to the guidelines, patients at highest risk of thromboembolism (in the absence of anticoagulation) are those with:
- mitral valve prostheses;
- atrial fibrillation with a CHADS2 score of five to six or cerebrovascular accidents (CVA) within the last three months; and/or
- venous thromboembolism (VTE) within the last three months or history of severe thrombophilia.
Patients at the lowest risk of thromboembolism are those with:
- mechanical aortic prostheses with no other stroke risk factors;
- atrial fibrillation with a CHADS2 score of zero to two; and/or
- a single VTE that occurred >12 months prior.
There are several approaches to identifying patients at greatest risk for bleeding. Location-specific modeling for upper GI bleeds (e.g. Rockall score) and lower GI bleeds (e.g. BLEED score) focus on the clinical presentation and/or endoscopic findings. General hemorrhage risk scores (e.g. HAS-BLED, ATRIA) focus on medical comorbidities. While easy to use, the predictive value of such scores as part of anticoagulation resumption after a GI hemorrhage remains uncertain.
Based on the above methods of risk stratification, patients at higher risk of thromboembolism and lower risk of bleeding will likely benefit from waiting only a short time interval before restarting anticoagulation. Based on the trial conducted by Witt and colleagues, anticoagulation typically can be reinitiated within four days of obtaining hemostatic and hemodynamic stability.2 Conversely, those at highest risk of bleeding and lower risk of thromboembolism will benefit from a delayed resumption of anticoagulation. Involvement of a specialist, such as a gastroenterologist, could help further clarify the risk of rebleeding.
The ideal approach for patients with a high risk of both bleeding and thromboembolism remains uncertain. Such cases highlight the need for an informed discussion with the patient and any involved caregivers, as well as involvement of inpatient subspecialists and outpatient longitudinal providers.
There remains a lack of evidence on the best method to restart anticoagulation. Based on small and retrospective trials, we recommend restarting warfarin at the patient’s previous home dose. The duration of inpatient monitoring following warfarin initiation should be individualized, but warfarin is not expected to impair coagulation for four to six days after initiation.
Little data is available with respect to the role of novel oral anticoagulants after a GI bleed. Given the lack of reversing agents for these drugs, we recommend exercising caution in populations with a high risk of rebleeding. Theoretically, given that these agents reach peak effect faster than warfarin, waiting an additional four days after the time frame recommended for starting warfarin is a prudent resumption strategy for novel oral anticoagulants.
Source: Adapted from Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
Resumption of Antiplatelet Agents
The decision to resume antiplatelet therapy should also be highly individualized. In addition to weighing the risk of bleeding (as described in the previous section), the physician must also estimate the benefits of antiplatelet therapy in decreasing the risk of cardiovascular events.
In low-risk patients on antiplatelet therapy (i.e., for primary cardiovascular prevention) reinitiation after a bleeding episode can be reasonably delayed, because the risk of rebleeding likely outweighs the potential benefit of restarting therapy.
For patients who are at intermediate risk (i.e., those on antiplatelet agents for secondary prevention of cardiovascular disease), emerging evidence argues for early reinstitution after a GI bleed. In a trial published in Annals of Internal Medicine, Sung and colleagues randomized 156 patients to aspirin or placebo therapy immediately following endoscopically obtained hemostasis for peptic ulcer bleeding.4 All patients received PPIs. There was no significant difference in bleeding rates between the two groups, but delayed resumption of aspirin was associated with a significant increase in all-cause mortality.
Two recent meta-analyses provide further insight into the risks of withholding aspirin therapy. The first, which included 50,279 patients on aspirin for secondary prevention, found that aspirin non-adherence or withdrawal after a GI bleed was associated with a three-fold higher risk of major adverse cardiac events.5 Cardiac event rates were highest in the subgroup of patients with a history of prior percutaneous coronary stenting.
A second meta-analysis evaluated patients who had aspirin held perioperatively. In a population of patients on aspirin for secondary prevention, the mean time after withholding aspirin was 8.5 days to coronary events, 14.3 days to cerebrovascular events, and 25.8 days to peripheral arterial events.6 Events occurred as early as five days after withdrawal of aspirin.
Patients with recent intracoronary stenting are at highest risk of thrombosis. In patients with a bare metal stent placed within six weeks, or a drug-eluting stent placed within six months, every effort should be made to minimize interruptions of dual antiplatelet therapy.
Based on the data presented above, for patients at intermediate and/or high risk of adverse cardiac events, we recommend reinstitution of aspirin as soon as possible following a GI hemorrhage, preferably within five days. PPI co-therapy is a mainstay for secondary prevention of upper GI bleeding in patients on antiplatelet therapy. Current research and guidelines have not addressed specifically the role of withholding and reinitiating aspirin in lower GI bleeding, non-peptic ulcer, or upper-GI bleeding, however, a similar strategy is likely appropriate. As with the decision for restarting anticoagulants, discussion with relevant specialists is essential to best define the risk of re-bleeding.
Back to the Cases
Given her CHADS2 score of three, the patient with a diverticular bleed has a 9.6% annual risk of stroke if she does not resume anticoagulation. Using the HAS-BLED and ATRIA scores, this patient has 2.6% to 5.8% annual risk of hemorrhage. We recommend resuming warfarin anticoagulation therapy within four days of achieving hemostasis.
For the patient with coronary artery disease with remote drug-eluting stent placement and upper GI bleed, evidence supports early resumption of appropriate antiplatelet therapy following endoscopic therapy and hemostasis. We recommend resuming aspirin during the current hospitalization and concomitant treatment with a PPI indefinitely.
Bottom Line
Following a GI bleed, the risks and benefits of restarting anticoagulant and antiplatelet agents need to be carefully considered. In patients on oral anticoagulants at high risk for thromboembolism and low risk for rebleeding, consider restarting anticoagulation within four to five days. Patients on antiplatelet agents for secondary prevention should have the medication restarted during hospitalization after endoscopically obtained hemostasis of a peptic ulcer.
In all cases, hospitalists should engage the patient, gastroenterologist, and outpatient provider to best determine when resumption of anticoagulant and/or antiplatelet agents should occur.
Dr. Allen-Dicker is a hospitalist and clinical instructor at Mount Sinai Medical Center in New York City. Dr. Briones is director of perioperative services in the division of hospital medicine and an assistant professor; Dr. Berman is a hospitalist and a clinical instructor, and Dr. Dunn is a professor of medicine and chief of the division of hospital medicine, all at Mount Sinai Medical Center.
References
- Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152(2):101-113.
- Witt DM, Delate T, Garcia DA, et al. Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med. 2012;172(19):1484-1491.
- Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S-350S.
- Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: A randomized trial. Ann Intern Med. 2010;152(1):1-9.
- Biondi-Zoccai GG, Lotrionte M, Agostoni P, et al. A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J. 2006;27(22):2667-2674.
- Burger W, Chemnitius JM, Kneissl GD, Rücker G. Low-dose aspirin for secondary cardiovascular prevention – cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation – review and meta-analysis. J Intern Med. 2005;257(5):399-414.
What Are the Indications for a Blood Transfusion?
Case
A 65-year-old man with a history of coronary artery disease (CAD) presents to the ED after a mechanical fall. He was found to have a hip fracture, admitted to orthopedic service, and underwent an uneventful hip repair. His post-operative course was uncomplicated, except for his hemoglobin level of 7.5 g/dL, which had decreased from his pre-operative hemoglobin of 11.2 g/dL. The patient was without cardiac symptoms, was ambulating with assistance, had normal vital signs, and was otherwise having an unremarkable recovery. The orthopedic surgeon, who recently heard that you do not have to transfuse patients unless their hemoglobin is less than 7 g/dL, consulted the hospitalist to help make the decision. What would your recommendation be?
Overview
Blood transfusions are a common medical procedure routinely given in the hospital.1 An estimated 15 million red blood cell (RBC) units are transfused each year in the United States.2 Despite its common use, the clinical indications for transfusion continue to be the subject of considerable debate. Most clinicians would agree that treating a patient with a low hemoglobin level and symptoms of anemia is reasonable.1,3 However, in the absence of overt symptoms, there is debate about when transfusions are appropriate.2,3
Because tissue oxygen delivery is dependent on hemoglobin and cardiac output, past medical practice has supported the use of the “golden 10/30 rule,” by which patients are transfused to a hemoglobin concentration of 10 g/dL or a hematocrit of 30%, regardless of symptoms. The rationale for this approach is based on physiologic evidence that cardiac output increases when hemoglobin falls below 7 g/dl. In patients with cardiac disease, the ability to increase cardiac output is compromised. Therefore, in order to reduce strain on the heart, hemoglobin levels historically have been kept higher than this threshold.
However, several studies have forced us to re-evaluate this old paradigm, including increasing concern for the infectious and noninfectious complications associated with blood transfusions and the need for cost containment (see Table 1).1,2,4 Due to improved blood screening, infectious complications from transfusions have been greatly reduced; noninfectious complications are 1,000 times more likely than infectious ones.
Review of Data
Although a number of studies have been performed on the indications for blood transfusions, many of the trials conducted in the past were too small to substantiate a certain practice. However, three trials with a large number of participants have allowed for a more evidence-based approach to blood transfusions. The studies address different patient populations to help broaden the restrictive transfusion approach to a larger range of patients.
TRICC trial: critically ill patients5. The TRICC trial was the first major study that compared a liberal transfusion strategy (transfuse when Hb <10 g/dL) to a more conservative approach (transfuse when Hb <7 g/dL). In this multicenter, randomized controlled trial, Hébert et al enrolled 418 critically ill patients and found that there was no significant difference in 30-day all-cause mortality between the restrictive-strategy group (18.7%) and the liberal-strategy group (23.3%).
However, in the pre-determined subgroup analysis, patients who were less severely ill (APACHE II scores of <20) had 30-day all-cause mortality of 8.7%, compared with 16.1% in the liberal-strategy group. Interestingly, there were more cardiac complications (pulmonary edema, angina, MI, and cardiac arrest) in the liberal-strategy group (21%) compared with the restrictive-strategy group (13%). Despite this finding, 30-day mortality was not significantly different in patients with clinically significant cardiac disease (primary or secondary diagnosis of cardiac disease [20.5% restrictive versus 22.9% liberal]).
An average of 2.6 units of RBCs per patient were given in the restrictive group, while 5.6 units were given to patients in the liberal group. This reflects a 54% decrease in the number of transfusions used in the conservative group. All the patients in the liberal group received transfusions, while 33% of the restrictive group’s patients received no blood at all.
The results of this trial suggested that there is no clinical advantage in transfusing ICU patients to Hb values above 9 g/dL, even if they have a history of cardiac disease. In fact, it may be harmful to practice a liberal transfusion strategy in critically ill younger patients (<55 years old) and those who are less severely ill (APACHE II <20).5
FOCUS trial: hip surgery and history of cardiac disease6. The FOCUS trial is a recent study that looked at the optimal hemoglobin level at which an RBC transfusion is beneficial for patients undergoing hip surgery. This study enrolled patients aged 50 or older who had a history or risk factors for cardiovascular disease (clinical evidence of cardiovascular disease: h/o ischemic heart disease, EKG evidence of previous MI, h/o CHF/PVD, h/o stroke/TIA, h/o HTN, DM, hyperlipidemia (TC >200/LDL >130), current tobacco use, or Cr>2.0), who were undergoing primary surgical repair of a hip fracture, and who had Hb <10g/dL within three days after surgery.
More than 2,000 patients were assigned randomly to a liberal-strategy group (transfuse to maintain a Hb >10g/dL) or a restrictive strategy group (transfuse to maintain Hg >8g/dl or for symptoms or signs of anemia). These signs/symptoms included chest pain that was possibly cardiac-related, congestive heart failure, tachycardia, and unresponsive hypotension. The primary outcomes were mortality or inability to walk 10 feet without assistance at 60-day follow-up.
The FOCUS trial found no statistically significant difference in mortality rate (7.6% in the liberal group versus 6.6% in the restrictive group) or in the ability to walk at 60 days (35.2% in the liberal group versus 34.7% in the restrictive group). There were no significant differences in the rates of in-hospital acute MI, unstable angina, or death between the two groups.
Patients in the restrictive-strategy group received 65% fewer units of blood than the liberal group, with 59% receiving no blood after surgery compared with 3% of the liberal group. Overall, the liberal group received 1,866 units of blood, compared with 652 units in the restrictive group.
This trial helps support the findings in previous trials, such as TRICC, by showing that a restrictive transfusion strategy using a trigger point of 8 g/dl does not increase mortality or cardiovascular complications and does not decrease functional ability after orthopedic surgery.
TRAC trial: patients after cardiac surgery7. The TRAC trial was a prospective randomized trial in 502 patients undergoing cardiac surgery that assigned 253 patients to the liberal-transfusion-strategy group (Hb >10g/dl) and 249 to the restrictive-strategy group (Hb >8 g/dl). In this study, the primary endpoint of all-cause 30-day mortality occurred in 10% of the liberal group and 11% of the restrictive group. This difference was not significant.
Subanalysis showed that blood transfusion in both groups was an independent risk factor for the occurrence of respiratory, cardiac, renal, and infectious complications, in addition to the composite end point of 30-day mortality—again highlighting the risk involved in of blood transfusions.
These results support the other trial conclusions that a restrictive transfusion strategy of maintaining a hematocrit of 24% (Hb 8 g/dL) is as safe as a more liberal strategy with a hematocrit of 30% (Hb 10 g/dL). It also offers further evidence of the risks of blood transfusions and supports the view that blood transfusions should never be given simply to correct low hemoglobin levels.
Cochrane Review. A recent Cochrane Review that comprised 19 trials with a combined total of 6,264 patients also supported a restrictive-strategy approach.8 In this review, no difference in mortality was established between the restrictive and liberal transfusion groups, with a trend toward decreased hospital mortality in the restrictive-transfusion group. The authors of the study felt that for most patients, blood transfusion is not necessary until hemoglobin levels drop below 7-8 g/dL but emphasized that this criteria should not be generalized to patients with an acute cardiac issue.
Back to the Case
In this case, the patient is doing well post-operatively and has no cardiac symptoms or hypotension. However, based on the new available data from the FOCUS trial, given the patient’s history of CAD, and the threshold of 8 g/dL used in the study, it was recommended that the patient be transfused.
Bottom Line
Current practice guidelines clearly support clinical judgment as the primary determinant in the decision to transfuse.2 However, current evidence is growing that our threshold for blood transfusions should be a hemoglobin level of 7-8 g/dl.
Dr. Chang is a hospitalist and assistant professor at Mount Sinai Medical Center in New York City, and is co-director of the medicine-geriatrics clerkship at the Icahn School of Medicine at Mount Sinai. Dr. Torgalkar is a hospitalist and assistant professor at Mount Sinai Medical Center.
References
- Sharma S, Sharma P, Tyler L. Transfusion of blood and blood products: indications and complications. Am Fam Physician. 2011;83:719-724.
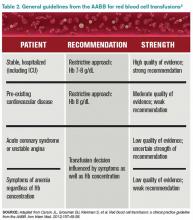
- Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2012;157:49-58.
- Valeri CR, Crowley JP, Loscalzo J. The red cell transfusion trigger: has a sin of commission now become a sin of omission? Transfusion. 1998;38:602-610.
- Klein HG, Spahn DR, Carson JL. Red blood cell transfusion in clinical practice. Lancet. 2007;370(9585):415-426.
- Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340:409-17.
- Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453-2462.
- Hajjar LA, Vincent JL, Galas FR, et al. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010;304:1559-1567.
- Carson JL, Carless PA, Hébert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012; 4:CD002042.
Case
A 65-year-old man with a history of coronary artery disease (CAD) presents to the ED after a mechanical fall. He was found to have a hip fracture, admitted to orthopedic service, and underwent an uneventful hip repair. His post-operative course was uncomplicated, except for his hemoglobin level of 7.5 g/dL, which had decreased from his pre-operative hemoglobin of 11.2 g/dL. The patient was without cardiac symptoms, was ambulating with assistance, had normal vital signs, and was otherwise having an unremarkable recovery. The orthopedic surgeon, who recently heard that you do not have to transfuse patients unless their hemoglobin is less than 7 g/dL, consulted the hospitalist to help make the decision. What would your recommendation be?
Overview
Blood transfusions are a common medical procedure routinely given in the hospital.1 An estimated 15 million red blood cell (RBC) units are transfused each year in the United States.2 Despite its common use, the clinical indications for transfusion continue to be the subject of considerable debate. Most clinicians would agree that treating a patient with a low hemoglobin level and symptoms of anemia is reasonable.1,3 However, in the absence of overt symptoms, there is debate about when transfusions are appropriate.2,3
Because tissue oxygen delivery is dependent on hemoglobin and cardiac output, past medical practice has supported the use of the “golden 10/30 rule,” by which patients are transfused to a hemoglobin concentration of 10 g/dL or a hematocrit of 30%, regardless of symptoms. The rationale for this approach is based on physiologic evidence that cardiac output increases when hemoglobin falls below 7 g/dl. In patients with cardiac disease, the ability to increase cardiac output is compromised. Therefore, in order to reduce strain on the heart, hemoglobin levels historically have been kept higher than this threshold.
However, several studies have forced us to re-evaluate this old paradigm, including increasing concern for the infectious and noninfectious complications associated with blood transfusions and the need for cost containment (see Table 1).1,2,4 Due to improved blood screening, infectious complications from transfusions have been greatly reduced; noninfectious complications are 1,000 times more likely than infectious ones.
Review of Data
Although a number of studies have been performed on the indications for blood transfusions, many of the trials conducted in the past were too small to substantiate a certain practice. However, three trials with a large number of participants have allowed for a more evidence-based approach to blood transfusions. The studies address different patient populations to help broaden the restrictive transfusion approach to a larger range of patients.
TRICC trial: critically ill patients5. The TRICC trial was the first major study that compared a liberal transfusion strategy (transfuse when Hb <10 g/dL) to a more conservative approach (transfuse when Hb <7 g/dL). In this multicenter, randomized controlled trial, Hébert et al enrolled 418 critically ill patients and found that there was no significant difference in 30-day all-cause mortality between the restrictive-strategy group (18.7%) and the liberal-strategy group (23.3%).
However, in the pre-determined subgroup analysis, patients who were less severely ill (APACHE II scores of <20) had 30-day all-cause mortality of 8.7%, compared with 16.1% in the liberal-strategy group. Interestingly, there were more cardiac complications (pulmonary edema, angina, MI, and cardiac arrest) in the liberal-strategy group (21%) compared with the restrictive-strategy group (13%). Despite this finding, 30-day mortality was not significantly different in patients with clinically significant cardiac disease (primary or secondary diagnosis of cardiac disease [20.5% restrictive versus 22.9% liberal]).
An average of 2.6 units of RBCs per patient were given in the restrictive group, while 5.6 units were given to patients in the liberal group. This reflects a 54% decrease in the number of transfusions used in the conservative group. All the patients in the liberal group received transfusions, while 33% of the restrictive group’s patients received no blood at all.
The results of this trial suggested that there is no clinical advantage in transfusing ICU patients to Hb values above 9 g/dL, even if they have a history of cardiac disease. In fact, it may be harmful to practice a liberal transfusion strategy in critically ill younger patients (<55 years old) and those who are less severely ill (APACHE II <20).5
FOCUS trial: hip surgery and history of cardiac disease6. The FOCUS trial is a recent study that looked at the optimal hemoglobin level at which an RBC transfusion is beneficial for patients undergoing hip surgery. This study enrolled patients aged 50 or older who had a history or risk factors for cardiovascular disease (clinical evidence of cardiovascular disease: h/o ischemic heart disease, EKG evidence of previous MI, h/o CHF/PVD, h/o stroke/TIA, h/o HTN, DM, hyperlipidemia (TC >200/LDL >130), current tobacco use, or Cr>2.0), who were undergoing primary surgical repair of a hip fracture, and who had Hb <10g/dL within three days after surgery.
More than 2,000 patients were assigned randomly to a liberal-strategy group (transfuse to maintain a Hb >10g/dL) or a restrictive strategy group (transfuse to maintain Hg >8g/dl or for symptoms or signs of anemia). These signs/symptoms included chest pain that was possibly cardiac-related, congestive heart failure, tachycardia, and unresponsive hypotension. The primary outcomes were mortality or inability to walk 10 feet without assistance at 60-day follow-up.
The FOCUS trial found no statistically significant difference in mortality rate (7.6% in the liberal group versus 6.6% in the restrictive group) or in the ability to walk at 60 days (35.2% in the liberal group versus 34.7% in the restrictive group). There were no significant differences in the rates of in-hospital acute MI, unstable angina, or death between the two groups.
Patients in the restrictive-strategy group received 65% fewer units of blood than the liberal group, with 59% receiving no blood after surgery compared with 3% of the liberal group. Overall, the liberal group received 1,866 units of blood, compared with 652 units in the restrictive group.
This trial helps support the findings in previous trials, such as TRICC, by showing that a restrictive transfusion strategy using a trigger point of 8 g/dl does not increase mortality or cardiovascular complications and does not decrease functional ability after orthopedic surgery.
TRAC trial: patients after cardiac surgery7. The TRAC trial was a prospective randomized trial in 502 patients undergoing cardiac surgery that assigned 253 patients to the liberal-transfusion-strategy group (Hb >10g/dl) and 249 to the restrictive-strategy group (Hb >8 g/dl). In this study, the primary endpoint of all-cause 30-day mortality occurred in 10% of the liberal group and 11% of the restrictive group. This difference was not significant.
Subanalysis showed that blood transfusion in both groups was an independent risk factor for the occurrence of respiratory, cardiac, renal, and infectious complications, in addition to the composite end point of 30-day mortality—again highlighting the risk involved in of blood transfusions.
These results support the other trial conclusions that a restrictive transfusion strategy of maintaining a hematocrit of 24% (Hb 8 g/dL) is as safe as a more liberal strategy with a hematocrit of 30% (Hb 10 g/dL). It also offers further evidence of the risks of blood transfusions and supports the view that blood transfusions should never be given simply to correct low hemoglobin levels.
Cochrane Review. A recent Cochrane Review that comprised 19 trials with a combined total of 6,264 patients also supported a restrictive-strategy approach.8 In this review, no difference in mortality was established between the restrictive and liberal transfusion groups, with a trend toward decreased hospital mortality in the restrictive-transfusion group. The authors of the study felt that for most patients, blood transfusion is not necessary until hemoglobin levels drop below 7-8 g/dL but emphasized that this criteria should not be generalized to patients with an acute cardiac issue.
Back to the Case
In this case, the patient is doing well post-operatively and has no cardiac symptoms or hypotension. However, based on the new available data from the FOCUS trial, given the patient’s history of CAD, and the threshold of 8 g/dL used in the study, it was recommended that the patient be transfused.
Bottom Line
Current practice guidelines clearly support clinical judgment as the primary determinant in the decision to transfuse.2 However, current evidence is growing that our threshold for blood transfusions should be a hemoglobin level of 7-8 g/dl.
Dr. Chang is a hospitalist and assistant professor at Mount Sinai Medical Center in New York City, and is co-director of the medicine-geriatrics clerkship at the Icahn School of Medicine at Mount Sinai. Dr. Torgalkar is a hospitalist and assistant professor at Mount Sinai Medical Center.
References
- Sharma S, Sharma P, Tyler L. Transfusion of blood and blood products: indications and complications. Am Fam Physician. 2011;83:719-724.
- Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2012;157:49-58.
- Valeri CR, Crowley JP, Loscalzo J. The red cell transfusion trigger: has a sin of commission now become a sin of omission? Transfusion. 1998;38:602-610.
- Klein HG, Spahn DR, Carson JL. Red blood cell transfusion in clinical practice. Lancet. 2007;370(9585):415-426.
- Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340:409-17.
- Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453-2462.
- Hajjar LA, Vincent JL, Galas FR, et al. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010;304:1559-1567.
- Carson JL, Carless PA, Hébert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012; 4:CD002042.
Case
A 65-year-old man with a history of coronary artery disease (CAD) presents to the ED after a mechanical fall. He was found to have a hip fracture, admitted to orthopedic service, and underwent an uneventful hip repair. His post-operative course was uncomplicated, except for his hemoglobin level of 7.5 g/dL, which had decreased from his pre-operative hemoglobin of 11.2 g/dL. The patient was without cardiac symptoms, was ambulating with assistance, had normal vital signs, and was otherwise having an unremarkable recovery. The orthopedic surgeon, who recently heard that you do not have to transfuse patients unless their hemoglobin is less than 7 g/dL, consulted the hospitalist to help make the decision. What would your recommendation be?
Overview
Blood transfusions are a common medical procedure routinely given in the hospital.1 An estimated 15 million red blood cell (RBC) units are transfused each year in the United States.2 Despite its common use, the clinical indications for transfusion continue to be the subject of considerable debate. Most clinicians would agree that treating a patient with a low hemoglobin level and symptoms of anemia is reasonable.1,3 However, in the absence of overt symptoms, there is debate about when transfusions are appropriate.2,3
Because tissue oxygen delivery is dependent on hemoglobin and cardiac output, past medical practice has supported the use of the “golden 10/30 rule,” by which patients are transfused to a hemoglobin concentration of 10 g/dL or a hematocrit of 30%, regardless of symptoms. The rationale for this approach is based on physiologic evidence that cardiac output increases when hemoglobin falls below 7 g/dl. In patients with cardiac disease, the ability to increase cardiac output is compromised. Therefore, in order to reduce strain on the heart, hemoglobin levels historically have been kept higher than this threshold.
However, several studies have forced us to re-evaluate this old paradigm, including increasing concern for the infectious and noninfectious complications associated with blood transfusions and the need for cost containment (see Table 1).1,2,4 Due to improved blood screening, infectious complications from transfusions have been greatly reduced; noninfectious complications are 1,000 times more likely than infectious ones.
Review of Data
Although a number of studies have been performed on the indications for blood transfusions, many of the trials conducted in the past were too small to substantiate a certain practice. However, three trials with a large number of participants have allowed for a more evidence-based approach to blood transfusions. The studies address different patient populations to help broaden the restrictive transfusion approach to a larger range of patients.
TRICC trial: critically ill patients5. The TRICC trial was the first major study that compared a liberal transfusion strategy (transfuse when Hb <10 g/dL) to a more conservative approach (transfuse when Hb <7 g/dL). In this multicenter, randomized controlled trial, Hébert et al enrolled 418 critically ill patients and found that there was no significant difference in 30-day all-cause mortality between the restrictive-strategy group (18.7%) and the liberal-strategy group (23.3%).
However, in the pre-determined subgroup analysis, patients who were less severely ill (APACHE II scores of <20) had 30-day all-cause mortality of 8.7%, compared with 16.1% in the liberal-strategy group. Interestingly, there were more cardiac complications (pulmonary edema, angina, MI, and cardiac arrest) in the liberal-strategy group (21%) compared with the restrictive-strategy group (13%). Despite this finding, 30-day mortality was not significantly different in patients with clinically significant cardiac disease (primary or secondary diagnosis of cardiac disease [20.5% restrictive versus 22.9% liberal]).
An average of 2.6 units of RBCs per patient were given in the restrictive group, while 5.6 units were given to patients in the liberal group. This reflects a 54% decrease in the number of transfusions used in the conservative group. All the patients in the liberal group received transfusions, while 33% of the restrictive group’s patients received no blood at all.
The results of this trial suggested that there is no clinical advantage in transfusing ICU patients to Hb values above 9 g/dL, even if they have a history of cardiac disease. In fact, it may be harmful to practice a liberal transfusion strategy in critically ill younger patients (<55 years old) and those who are less severely ill (APACHE II <20).5
FOCUS trial: hip surgery and history of cardiac disease6. The FOCUS trial is a recent study that looked at the optimal hemoglobin level at which an RBC transfusion is beneficial for patients undergoing hip surgery. This study enrolled patients aged 50 or older who had a history or risk factors for cardiovascular disease (clinical evidence of cardiovascular disease: h/o ischemic heart disease, EKG evidence of previous MI, h/o CHF/PVD, h/o stroke/TIA, h/o HTN, DM, hyperlipidemia (TC >200/LDL >130), current tobacco use, or Cr>2.0), who were undergoing primary surgical repair of a hip fracture, and who had Hb <10g/dL within three days after surgery.
More than 2,000 patients were assigned randomly to a liberal-strategy group (transfuse to maintain a Hb >10g/dL) or a restrictive strategy group (transfuse to maintain Hg >8g/dl or for symptoms or signs of anemia). These signs/symptoms included chest pain that was possibly cardiac-related, congestive heart failure, tachycardia, and unresponsive hypotension. The primary outcomes were mortality or inability to walk 10 feet without assistance at 60-day follow-up.
The FOCUS trial found no statistically significant difference in mortality rate (7.6% in the liberal group versus 6.6% in the restrictive group) or in the ability to walk at 60 days (35.2% in the liberal group versus 34.7% in the restrictive group). There were no significant differences in the rates of in-hospital acute MI, unstable angina, or death between the two groups.
Patients in the restrictive-strategy group received 65% fewer units of blood than the liberal group, with 59% receiving no blood after surgery compared with 3% of the liberal group. Overall, the liberal group received 1,866 units of blood, compared with 652 units in the restrictive group.
This trial helps support the findings in previous trials, such as TRICC, by showing that a restrictive transfusion strategy using a trigger point of 8 g/dl does not increase mortality or cardiovascular complications and does not decrease functional ability after orthopedic surgery.
TRAC trial: patients after cardiac surgery7. The TRAC trial was a prospective randomized trial in 502 patients undergoing cardiac surgery that assigned 253 patients to the liberal-transfusion-strategy group (Hb >10g/dl) and 249 to the restrictive-strategy group (Hb >8 g/dl). In this study, the primary endpoint of all-cause 30-day mortality occurred in 10% of the liberal group and 11% of the restrictive group. This difference was not significant.
Subanalysis showed that blood transfusion in both groups was an independent risk factor for the occurrence of respiratory, cardiac, renal, and infectious complications, in addition to the composite end point of 30-day mortality—again highlighting the risk involved in of blood transfusions.
These results support the other trial conclusions that a restrictive transfusion strategy of maintaining a hematocrit of 24% (Hb 8 g/dL) is as safe as a more liberal strategy with a hematocrit of 30% (Hb 10 g/dL). It also offers further evidence of the risks of blood transfusions and supports the view that blood transfusions should never be given simply to correct low hemoglobin levels.
Cochrane Review. A recent Cochrane Review that comprised 19 trials with a combined total of 6,264 patients also supported a restrictive-strategy approach.8 In this review, no difference in mortality was established between the restrictive and liberal transfusion groups, with a trend toward decreased hospital mortality in the restrictive-transfusion group. The authors of the study felt that for most patients, blood transfusion is not necessary until hemoglobin levels drop below 7-8 g/dL but emphasized that this criteria should not be generalized to patients with an acute cardiac issue.
Back to the Case
In this case, the patient is doing well post-operatively and has no cardiac symptoms or hypotension. However, based on the new available data from the FOCUS trial, given the patient’s history of CAD, and the threshold of 8 g/dL used in the study, it was recommended that the patient be transfused.
Bottom Line
Current practice guidelines clearly support clinical judgment as the primary determinant in the decision to transfuse.2 However, current evidence is growing that our threshold for blood transfusions should be a hemoglobin level of 7-8 g/dl.
Dr. Chang is a hospitalist and assistant professor at Mount Sinai Medical Center in New York City, and is co-director of the medicine-geriatrics clerkship at the Icahn School of Medicine at Mount Sinai. Dr. Torgalkar is a hospitalist and assistant professor at Mount Sinai Medical Center.
References
- Sharma S, Sharma P, Tyler L. Transfusion of blood and blood products: indications and complications. Am Fam Physician. 2011;83:719-724.
- Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2012;157:49-58.
- Valeri CR, Crowley JP, Loscalzo J. The red cell transfusion trigger: has a sin of commission now become a sin of omission? Transfusion. 1998;38:602-610.
- Klein HG, Spahn DR, Carson JL. Red blood cell transfusion in clinical practice. Lancet. 2007;370(9585):415-426.
- Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340:409-17.
- Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453-2462.
- Hajjar LA, Vincent JL, Galas FR, et al. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010;304:1559-1567.
- Carson JL, Carless PA, Hébert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012; 4:CD002042.