User login
Richard Quinn is an award-winning journalist with 15 years’ experience. He has worked at the Asbury Park Press in New Jersey and The Virginian-Pilot in Norfolk, Va., and currently is managing editor for a leading commercial real estate publication. His freelance work has appeared in The Jewish State, The Hospitalist, The Rheumatologist, ACEP Now, and ENT Today. He lives in New Jersey with his wife and three cats.
From idea to abstract, RIV posters highlight novel thinking
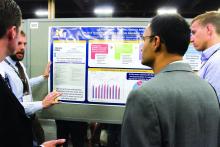
Masih Shinwa, MD, stood beside a half-circle of judges Tuesday night at SHM’s annual Research, Innovations and Clinical Vignettes (RIV) poster competition and argued why his entry, already a finalist, should win. And to think, his poster, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was born simply of a group of medical students who incredulously said they were amazed patients would be woken in the middle of the night for laboratory tests.
Eighteen months later, the poster drew hundreds of questions from passersby on how a team approach could help generate fewer labs and chemistry testing. Now, the work could serve as a potential guide for other hospitals seeking to reduce unnecessary tests, a focal point of SHM and the ABIM Foundation’s Choosing Wisely campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but unless you attend these types of national meetings, it’s hard to get that perspective across [the country].”
That level of personal and professional collaboration is the purpose of the RIV, one of the best-attended events of SHM’s annual meeting. The event has become so popular that submissions this year tallied 1,712, nearly triple the number of submissions at the 2010 event.
“One of the amazing things is everyone has their own poster. They are doing their work,” said Margaret Fang, MD, MPH, FHM, program chair for HM17’s scientific abstracts competition, the formal name for the poster contest. “But then they start up conversations with the people next to them. ... seeing the organic networking and the discussions that arise from that is really exciting. RIV really serves as a way of connecting people together who might not have known the other person was doing that kind of work.”
Dr. Shinwa said that the specialty’s focus on research is important. He said it positions the field to be leaders, not just for patient care, but for hospitals and institutions.
“We are physicians. Our role is taking care of patients,” he said. “[But] knowing that there are people who are not just focusing on taking care of specific patients, but are actually there to improve the entire system and the process, that is really gratifying.”
Masih Shinwa, MD, stood beside a half-circle of judges Tuesday night at SHM’s annual Research, Innovations and Clinical Vignettes (RIV) poster competition and argued why his entry, already a finalist, should win. And to think, his poster, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was born simply of a group of medical students who incredulously said they were amazed patients would be woken in the middle of the night for laboratory tests.
Eighteen months later, the poster drew hundreds of questions from passersby on how a team approach could help generate fewer labs and chemistry testing. Now, the work could serve as a potential guide for other hospitals seeking to reduce unnecessary tests, a focal point of SHM and the ABIM Foundation’s Choosing Wisely campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but unless you attend these types of national meetings, it’s hard to get that perspective across [the country].”
That level of personal and professional collaboration is the purpose of the RIV, one of the best-attended events of SHM’s annual meeting. The event has become so popular that submissions this year tallied 1,712, nearly triple the number of submissions at the 2010 event.
“One of the amazing things is everyone has their own poster. They are doing their work,” said Margaret Fang, MD, MPH, FHM, program chair for HM17’s scientific abstracts competition, the formal name for the poster contest. “But then they start up conversations with the people next to them. ... seeing the organic networking and the discussions that arise from that is really exciting. RIV really serves as a way of connecting people together who might not have known the other person was doing that kind of work.”
Dr. Shinwa said that the specialty’s focus on research is important. He said it positions the field to be leaders, not just for patient care, but for hospitals and institutions.
“We are physicians. Our role is taking care of patients,” he said. “[But] knowing that there are people who are not just focusing on taking care of specific patients, but are actually there to improve the entire system and the process, that is really gratifying.”
Masih Shinwa, MD, stood beside a half-circle of judges Tuesday night at SHM’s annual Research, Innovations and Clinical Vignettes (RIV) poster competition and argued why his entry, already a finalist, should win. And to think, his poster, “Please ‘THINK’ Before You Order: A Multidisciplinary Approach to Decreasing Overutilization of Daily Labs,” was born simply of a group of medical students who incredulously said they were amazed patients would be woken in the middle of the night for laboratory tests.
Eighteen months later, the poster drew hundreds of questions from passersby on how a team approach could help generate fewer labs and chemistry testing. Now, the work could serve as a potential guide for other hospitals seeking to reduce unnecessary tests, a focal point of SHM and the ABIM Foundation’s Choosing Wisely campaign.
“This is a way to make it national,” he said. “You may have affected the lives of the patients in your hospital, but unless you attend these types of national meetings, it’s hard to get that perspective across [the country].”
That level of personal and professional collaboration is the purpose of the RIV, one of the best-attended events of SHM’s annual meeting. The event has become so popular that submissions this year tallied 1,712, nearly triple the number of submissions at the 2010 event.
“One of the amazing things is everyone has their own poster. They are doing their work,” said Margaret Fang, MD, MPH, FHM, program chair for HM17’s scientific abstracts competition, the formal name for the poster contest. “But then they start up conversations with the people next to them. ... seeing the organic networking and the discussions that arise from that is really exciting. RIV really serves as a way of connecting people together who might not have known the other person was doing that kind of work.”
Dr. Shinwa said that the specialty’s focus on research is important. He said it positions the field to be leaders, not just for patient care, but for hospitals and institutions.
“We are physicians. Our role is taking care of patients,” he said. “[But] knowing that there are people who are not just focusing on taking care of specific patients, but are actually there to improve the entire system and the process, that is really gratifying.”
Systems engineering in the hospital
Systems-engineering expert James Benneyan, PhD, doesn’t want hospitalists to look at poorly working processes in their institutions and think, “I should try to tweak this process to improve it.”
Instead, he wants them to walk out of his HM17 session at 8 a.m. Thursday – appropriately titled, “Systems Engineering in the Hospital: What Is in Your Toolkit?” – thinking like engineers, which means designing a solution, analyzing how well that process works, and then optimizing it for improvements. If that means not just tweaking a process, but redesigning it from scratch, so be it.
“Systems engineering studies the performance and how to improve the performance of complex systems, particularly sociotechnical systems,” said Dr. Benneyan, who runs the Healthcare Systems Engineering Institute at Northeastern University in Boston, which encompasses four research centers. “Health care is a perfect example … systems engineering can really help to understand and improve complex processes, whether it’s patient flow, safety, on-time discharge [or] better discharge.”
Dr. Benneyan says that systems engineering is, first and foremost, a mindset. It’s an approach to problem solving that’s different, if related, to quality improvement. Both have tremendous value, but they are based on different philosophies, tools, and work styles.
For example, many hospital operating rooms measure how many days the first procedure of the day begins on time. But instead of using that as a yardstick for quality, Dr. Benneyan said a better approach would be designing a system that can adapt to situations when the first case starts late. He compared the process to a delayed flight at an airport. An airline doesn’t back up every plane’s departure when one plane is running behind. Instead, it has systems that adapt to circumstances.
“There are methods and then there are philosophies,” Dr. Benneyan said. “I don’t think people in health care realize what my field did in the airline industry. We didn’t design things that worked and clicked properly. We designed things that … react to daily events and [everything] going on and perform pretty well.”
Dr. Benneyan says that, while health care is an incredibly complex system, other fields with similar levels of technical expertise have used systems engineering much more effectively. Manufacturing, logistics, and global distribution networks are all precise industries requiring hundreds of individual processes to ensure success.
“These are really complicated processes,” he said. “The real barrier is a cultural barrier. Health care is not the most challenging environment to work in. … I think something that people in health care have to have an appreciation for is that the process of doing this work is different from doing their other work. Systems engineering is not the same as quality improvement and can achieve fundamental breakthroughs in cases where QI has not – but also tends to take more work.”
Still, Dr. Benneyan believes his field has lessons that complement quality initiatives. To wit, health care advocates – including the Institute of Medicine, the Agency for Healthcare Research and Quality, the National Institutes of Health, and the National Science Foundation – have all pushed for greater application of systems engineering in medicine with the goal of improving how well health care does its job.
While he hopes hospitalists and other HM17 attendees at his session walk away with a newfound respect for and understanding of what systems engineering can do, he doesn’t want them to think it’s too easy.
“There’s a lack of appreciation of the process of engineering and how it’s different,” he said. “It’s a big challenge, partnering clinician with engineers. … We think differently even though we’re both scientifically trained.
“I hope hospitalists take away an appreciation for how this toolkit can be useful in their world.”
Systems Engineering in the Hospital: What Is in Your Toolkit?
Thursday, 8:00–9:30 a.m.
Systems-engineering expert James Benneyan, PhD, doesn’t want hospitalists to look at poorly working processes in their institutions and think, “I should try to tweak this process to improve it.”
Instead, he wants them to walk out of his HM17 session at 8 a.m. Thursday – appropriately titled, “Systems Engineering in the Hospital: What Is in Your Toolkit?” – thinking like engineers, which means designing a solution, analyzing how well that process works, and then optimizing it for improvements. If that means not just tweaking a process, but redesigning it from scratch, so be it.
“Systems engineering studies the performance and how to improve the performance of complex systems, particularly sociotechnical systems,” said Dr. Benneyan, who runs the Healthcare Systems Engineering Institute at Northeastern University in Boston, which encompasses four research centers. “Health care is a perfect example … systems engineering can really help to understand and improve complex processes, whether it’s patient flow, safety, on-time discharge [or] better discharge.”
Dr. Benneyan says that systems engineering is, first and foremost, a mindset. It’s an approach to problem solving that’s different, if related, to quality improvement. Both have tremendous value, but they are based on different philosophies, tools, and work styles.
For example, many hospital operating rooms measure how many days the first procedure of the day begins on time. But instead of using that as a yardstick for quality, Dr. Benneyan said a better approach would be designing a system that can adapt to situations when the first case starts late. He compared the process to a delayed flight at an airport. An airline doesn’t back up every plane’s departure when one plane is running behind. Instead, it has systems that adapt to circumstances.
“There are methods and then there are philosophies,” Dr. Benneyan said. “I don’t think people in health care realize what my field did in the airline industry. We didn’t design things that worked and clicked properly. We designed things that … react to daily events and [everything] going on and perform pretty well.”
Dr. Benneyan says that, while health care is an incredibly complex system, other fields with similar levels of technical expertise have used systems engineering much more effectively. Manufacturing, logistics, and global distribution networks are all precise industries requiring hundreds of individual processes to ensure success.
“These are really complicated processes,” he said. “The real barrier is a cultural barrier. Health care is not the most challenging environment to work in. … I think something that people in health care have to have an appreciation for is that the process of doing this work is different from doing their other work. Systems engineering is not the same as quality improvement and can achieve fundamental breakthroughs in cases where QI has not – but also tends to take more work.”
Still, Dr. Benneyan believes his field has lessons that complement quality initiatives. To wit, health care advocates – including the Institute of Medicine, the Agency for Healthcare Research and Quality, the National Institutes of Health, and the National Science Foundation – have all pushed for greater application of systems engineering in medicine with the goal of improving how well health care does its job.
While he hopes hospitalists and other HM17 attendees at his session walk away with a newfound respect for and understanding of what systems engineering can do, he doesn’t want them to think it’s too easy.
“There’s a lack of appreciation of the process of engineering and how it’s different,” he said. “It’s a big challenge, partnering clinician with engineers. … We think differently even though we’re both scientifically trained.
“I hope hospitalists take away an appreciation for how this toolkit can be useful in their world.”
Systems Engineering in the Hospital: What Is in Your Toolkit?
Thursday, 8:00–9:30 a.m.
Systems-engineering expert James Benneyan, PhD, doesn’t want hospitalists to look at poorly working processes in their institutions and think, “I should try to tweak this process to improve it.”
Instead, he wants them to walk out of his HM17 session at 8 a.m. Thursday – appropriately titled, “Systems Engineering in the Hospital: What Is in Your Toolkit?” – thinking like engineers, which means designing a solution, analyzing how well that process works, and then optimizing it for improvements. If that means not just tweaking a process, but redesigning it from scratch, so be it.
“Systems engineering studies the performance and how to improve the performance of complex systems, particularly sociotechnical systems,” said Dr. Benneyan, who runs the Healthcare Systems Engineering Institute at Northeastern University in Boston, which encompasses four research centers. “Health care is a perfect example … systems engineering can really help to understand and improve complex processes, whether it’s patient flow, safety, on-time discharge [or] better discharge.”
Dr. Benneyan says that systems engineering is, first and foremost, a mindset. It’s an approach to problem solving that’s different, if related, to quality improvement. Both have tremendous value, but they are based on different philosophies, tools, and work styles.
For example, many hospital operating rooms measure how many days the first procedure of the day begins on time. But instead of using that as a yardstick for quality, Dr. Benneyan said a better approach would be designing a system that can adapt to situations when the first case starts late. He compared the process to a delayed flight at an airport. An airline doesn’t back up every plane’s departure when one plane is running behind. Instead, it has systems that adapt to circumstances.
“There are methods and then there are philosophies,” Dr. Benneyan said. “I don’t think people in health care realize what my field did in the airline industry. We didn’t design things that worked and clicked properly. We designed things that … react to daily events and [everything] going on and perform pretty well.”
Dr. Benneyan says that, while health care is an incredibly complex system, other fields with similar levels of technical expertise have used systems engineering much more effectively. Manufacturing, logistics, and global distribution networks are all precise industries requiring hundreds of individual processes to ensure success.
“These are really complicated processes,” he said. “The real barrier is a cultural barrier. Health care is not the most challenging environment to work in. … I think something that people in health care have to have an appreciation for is that the process of doing this work is different from doing their other work. Systems engineering is not the same as quality improvement and can achieve fundamental breakthroughs in cases where QI has not – but also tends to take more work.”
Still, Dr. Benneyan believes his field has lessons that complement quality initiatives. To wit, health care advocates – including the Institute of Medicine, the Agency for Healthcare Research and Quality, the National Institutes of Health, and the National Science Foundation – have all pushed for greater application of systems engineering in medicine with the goal of improving how well health care does its job.
While he hopes hospitalists and other HM17 attendees at his session walk away with a newfound respect for and understanding of what systems engineering can do, he doesn’t want them to think it’s too easy.
“There’s a lack of appreciation of the process of engineering and how it’s different,” he said. “It’s a big challenge, partnering clinician with engineers. … We think differently even though we’re both scientifically trained.
“I hope hospitalists take away an appreciation for how this toolkit can be useful in their world.”
Systems Engineering in the Hospital: What Is in Your Toolkit?
Thursday, 8:00–9:30 a.m.
On Tap Wednesday
HM17 kicks off today with the presentation of the annual SHM Awards of Excellence, which honor work done in service to HM. A nod to the past, as it were. As those physicians are honored, others will be given their prizes as the winners of the Best of Research and Innovations in 2017, a nod to the present state of HM’s investigative spirit.
“We’re in the midst ... of a lot of change in the health care system,” said HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM. “To be able to hear from Dr. Conway as to how the priorities of CMS might be changing and what this all means to us in the future is an amazing opportunity. There is no better time to hear from Pat Conway. I’m really looking forward to it.”
A new highlight this year is Wednesday’s track of Repeated Sessions, something organizers added to ensure that some of the most-popular sessions – “Updates and Pearls in Infectious Diseases,” and “Non-Evidence Based Medicine: Things We Do for No Reason” – are available to as many attendees as possible.
“We’ve added that in this year because we know there are sessions that are standing room only on a regular basis,” Dr. Feldman said. “People should not have to stand.
“I’m hoping that these repeated sessions will be well received and will allow folks to be able to go to some other sessions they might not have in fear they were going to miss some of these typically ‘standing room only’ sessions.”
HM17 kicks off today with the presentation of the annual SHM Awards of Excellence, which honor work done in service to HM. A nod to the past, as it were. As those physicians are honored, others will be given their prizes as the winners of the Best of Research and Innovations in 2017, a nod to the present state of HM’s investigative spirit.
“We’re in the midst ... of a lot of change in the health care system,” said HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM. “To be able to hear from Dr. Conway as to how the priorities of CMS might be changing and what this all means to us in the future is an amazing opportunity. There is no better time to hear from Pat Conway. I’m really looking forward to it.”
A new highlight this year is Wednesday’s track of Repeated Sessions, something organizers added to ensure that some of the most-popular sessions – “Updates and Pearls in Infectious Diseases,” and “Non-Evidence Based Medicine: Things We Do for No Reason” – are available to as many attendees as possible.
“We’ve added that in this year because we know there are sessions that are standing room only on a regular basis,” Dr. Feldman said. “People should not have to stand.
“I’m hoping that these repeated sessions will be well received and will allow folks to be able to go to some other sessions they might not have in fear they were going to miss some of these typically ‘standing room only’ sessions.”
HM17 kicks off today with the presentation of the annual SHM Awards of Excellence, which honor work done in service to HM. A nod to the past, as it were. As those physicians are honored, others will be given their prizes as the winners of the Best of Research and Innovations in 2017, a nod to the present state of HM’s investigative spirit.
“We’re in the midst ... of a lot of change in the health care system,” said HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM. “To be able to hear from Dr. Conway as to how the priorities of CMS might be changing and what this all means to us in the future is an amazing opportunity. There is no better time to hear from Pat Conway. I’m really looking forward to it.”
A new highlight this year is Wednesday’s track of Repeated Sessions, something organizers added to ensure that some of the most-popular sessions – “Updates and Pearls in Infectious Diseases,” and “Non-Evidence Based Medicine: Things We Do for No Reason” – are available to as many attendees as possible.
“We’ve added that in this year because we know there are sessions that are standing room only on a regular basis,” Dr. Feldman said. “People should not have to stand.
“I’m hoping that these repeated sessions will be well received and will allow folks to be able to go to some other sessions they might not have in fear they were going to miss some of these typically ‘standing room only’ sessions.”
Telehospitalists can expand capability, capacity
The cost of health care is on the lips of everyone, from the thousands of HM17 attendees to congressional leaders to President Donald Trump. Yet, one long-promoted answer – telemedicine practiced by telehospitalists – is not as widely adopted as its proponents say it should be. After Wednesday’s session, “Foundations of a Hospital Medicine Telemedicine Program,” which begins at 4:15 p.m., at least a few more physicians will see it as an option.
“The timing is there,” said copresenter Talbot “Mac” McCormick, MD, president and chief executive officer of Eagle Telemedicine of Atlanta. “Telemedicine has come of age.”
[[{"fid":"194482","view_mode":"medstat_image_flush_left","attributes":{"alt":"Dr. Talbot \\\u0022Mac\u0022 McCormick, Eagle telemedicine, Atlanta","height":"220","width":"157","class":"media-element file-medstat-image-flush-left","data-delta":"1"},"fields":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Talbot \u0022Mac\u0022 McCormick","field_file_image_credit[und][0][value]":"","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Talbot \u0022Mac\u0022 McCormick","field_file_image_credit[und][0][value]":""}}}]]Copresenter Shannon Carpenter, BS, MBA, vice president at Charlotte, N.C.–based Carolinas Healthcare System, said telemedicine is a “relevancy issue.”
“We are hearing so much about a need for an alternative care model, [and] the virtual-care model is incredibly relevant in today’s environment,” Ms. Carpenter said. Adding to telemedicine’s basic advantage is its ability to help alleviate staffing issues.
“Telemedicine and telehospitalists can support and fill out gaps [and] can expand capability and capacity,” Dr. McCormick added. “Then, the other part is economy of scale. You can share a telehospitalist amongst a couple of small hospitals ... an advantage over each one trying to do it themselves.”
For example, individual institutions might not be able to keep a hospitalist busy 12 hours a night, but a nocturnist is still a requirement.
“When they need somebody, they sure need them,” Dr. McCormick said. “So, you get an economy of scale that several small hospitals effectively can share one physician because the space continuum – not necessarily the time continuum – but the space continuum and the geographic continuum is different engaging telemedicine versus people physically on the ground.”
Ms. Carpenter said that one of the obstacles to telemedicine is simply getting physicians to change habits.
“The biggest hurdles that we experienced were with buy-in for the care-delivery model,” she said. “Surprisingly, it’s not from the patients’ perspectives. It’s from either from the physicians who should be providing the service and/or from the staff in the hospital who aren’t used to the technology or the method of care delivery. To avoid this, it’s just like anything else: over-communication, education, and an ability to explain why and how care will be delivered.”
In addition to the difficulty of changing the culture, integration failures are another potential pitfall, according to Dr. McCormick.
“I think that communication gets to part of that,” he said. “I think [telemedicine should be viewed] ... not [as] a segmented silo of a hospitalist team – to be functional and to work well, it has to be integrated with the team so that it’s just a seamless part of the care team of the doctors, the nurses, the nurse practitioners.”
Both presenters agree that, as value-based payments and alternative payment models proliferate in the coming years, telemedicine will only grow as hospitals and hospitalist group leaders look for cost efficiencies. It will also be broader than just nocturnist services.
Ms. Carpenter said future uses could include expansion to ambulatory clinics for transitioning patients from acute care back to their medical home environment or to telehospitalists supporting paramedics on home visits.
“The use of tools and technology like this can allow care to bridge across these multiple geographic locations of care and do it in a way that provides continuity, economy of scale, consistent and high quality care,” Dr. McCormick said.
Foundations of a Hospital Medicine Telemedicine Program
Wednesday, 4:15–5:20 p.m.
Available via HM17 On Demand
The cost of health care is on the lips of everyone, from the thousands of HM17 attendees to congressional leaders to President Donald Trump. Yet, one long-promoted answer – telemedicine practiced by telehospitalists – is not as widely adopted as its proponents say it should be. After Wednesday’s session, “Foundations of a Hospital Medicine Telemedicine Program,” which begins at 4:15 p.m., at least a few more physicians will see it as an option.
“The timing is there,” said copresenter Talbot “Mac” McCormick, MD, president and chief executive officer of Eagle Telemedicine of Atlanta. “Telemedicine has come of age.”
[[{"fid":"194482","view_mode":"medstat_image_flush_left","attributes":{"alt":"Dr. Talbot \\\u0022Mac\u0022 McCormick, Eagle telemedicine, Atlanta","height":"220","width":"157","class":"media-element file-medstat-image-flush-left","data-delta":"1"},"fields":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Talbot \u0022Mac\u0022 McCormick","field_file_image_credit[und][0][value]":"","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Talbot \u0022Mac\u0022 McCormick","field_file_image_credit[und][0][value]":""}}}]]Copresenter Shannon Carpenter, BS, MBA, vice president at Charlotte, N.C.–based Carolinas Healthcare System, said telemedicine is a “relevancy issue.”
“We are hearing so much about a need for an alternative care model, [and] the virtual-care model is incredibly relevant in today’s environment,” Ms. Carpenter said. Adding to telemedicine’s basic advantage is its ability to help alleviate staffing issues.
“Telemedicine and telehospitalists can support and fill out gaps [and] can expand capability and capacity,” Dr. McCormick added. “Then, the other part is economy of scale. You can share a telehospitalist amongst a couple of small hospitals ... an advantage over each one trying to do it themselves.”
For example, individual institutions might not be able to keep a hospitalist busy 12 hours a night, but a nocturnist is still a requirement.
“When they need somebody, they sure need them,” Dr. McCormick said. “So, you get an economy of scale that several small hospitals effectively can share one physician because the space continuum – not necessarily the time continuum – but the space continuum and the geographic continuum is different engaging telemedicine versus people physically on the ground.”
Ms. Carpenter said that one of the obstacles to telemedicine is simply getting physicians to change habits.
“The biggest hurdles that we experienced were with buy-in for the care-delivery model,” she said. “Surprisingly, it’s not from the patients’ perspectives. It’s from either from the physicians who should be providing the service and/or from the staff in the hospital who aren’t used to the technology or the method of care delivery. To avoid this, it’s just like anything else: over-communication, education, and an ability to explain why and how care will be delivered.”
In addition to the difficulty of changing the culture, integration failures are another potential pitfall, according to Dr. McCormick.
“I think that communication gets to part of that,” he said. “I think [telemedicine should be viewed] ... not [as] a segmented silo of a hospitalist team – to be functional and to work well, it has to be integrated with the team so that it’s just a seamless part of the care team of the doctors, the nurses, the nurse practitioners.”
Both presenters agree that, as value-based payments and alternative payment models proliferate in the coming years, telemedicine will only grow as hospitals and hospitalist group leaders look for cost efficiencies. It will also be broader than just nocturnist services.
Ms. Carpenter said future uses could include expansion to ambulatory clinics for transitioning patients from acute care back to their medical home environment or to telehospitalists supporting paramedics on home visits.
“The use of tools and technology like this can allow care to bridge across these multiple geographic locations of care and do it in a way that provides continuity, economy of scale, consistent and high quality care,” Dr. McCormick said.
Foundations of a Hospital Medicine Telemedicine Program
Wednesday, 4:15–5:20 p.m.
Available via HM17 On Demand
The cost of health care is on the lips of everyone, from the thousands of HM17 attendees to congressional leaders to President Donald Trump. Yet, one long-promoted answer – telemedicine practiced by telehospitalists – is not as widely adopted as its proponents say it should be. After Wednesday’s session, “Foundations of a Hospital Medicine Telemedicine Program,” which begins at 4:15 p.m., at least a few more physicians will see it as an option.
“The timing is there,” said copresenter Talbot “Mac” McCormick, MD, president and chief executive officer of Eagle Telemedicine of Atlanta. “Telemedicine has come of age.”
[[{"fid":"194482","view_mode":"medstat_image_flush_left","attributes":{"alt":"Dr. Talbot \\\u0022Mac\u0022 McCormick, Eagle telemedicine, Atlanta","height":"220","width":"157","class":"media-element file-medstat-image-flush-left","data-delta":"1"},"fields":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Talbot \u0022Mac\u0022 McCormick","field_file_image_credit[und][0][value]":"","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Talbot \u0022Mac\u0022 McCormick","field_file_image_credit[und][0][value]":""}}}]]Copresenter Shannon Carpenter, BS, MBA, vice president at Charlotte, N.C.–based Carolinas Healthcare System, said telemedicine is a “relevancy issue.”
“We are hearing so much about a need for an alternative care model, [and] the virtual-care model is incredibly relevant in today’s environment,” Ms. Carpenter said. Adding to telemedicine’s basic advantage is its ability to help alleviate staffing issues.
“Telemedicine and telehospitalists can support and fill out gaps [and] can expand capability and capacity,” Dr. McCormick added. “Then, the other part is economy of scale. You can share a telehospitalist amongst a couple of small hospitals ... an advantage over each one trying to do it themselves.”
For example, individual institutions might not be able to keep a hospitalist busy 12 hours a night, but a nocturnist is still a requirement.
“When they need somebody, they sure need them,” Dr. McCormick said. “So, you get an economy of scale that several small hospitals effectively can share one physician because the space continuum – not necessarily the time continuum – but the space continuum and the geographic continuum is different engaging telemedicine versus people physically on the ground.”
Ms. Carpenter said that one of the obstacles to telemedicine is simply getting physicians to change habits.
“The biggest hurdles that we experienced were with buy-in for the care-delivery model,” she said. “Surprisingly, it’s not from the patients’ perspectives. It’s from either from the physicians who should be providing the service and/or from the staff in the hospital who aren’t used to the technology or the method of care delivery. To avoid this, it’s just like anything else: over-communication, education, and an ability to explain why and how care will be delivered.”
In addition to the difficulty of changing the culture, integration failures are another potential pitfall, according to Dr. McCormick.
“I think that communication gets to part of that,” he said. “I think [telemedicine should be viewed] ... not [as] a segmented silo of a hospitalist team – to be functional and to work well, it has to be integrated with the team so that it’s just a seamless part of the care team of the doctors, the nurses, the nurse practitioners.”
Both presenters agree that, as value-based payments and alternative payment models proliferate in the coming years, telemedicine will only grow as hospitals and hospitalist group leaders look for cost efficiencies. It will also be broader than just nocturnist services.
Ms. Carpenter said future uses could include expansion to ambulatory clinics for transitioning patients from acute care back to their medical home environment or to telehospitalists supporting paramedics on home visits.
“The use of tools and technology like this can allow care to bridge across these multiple geographic locations of care and do it in a way that provides continuity, economy of scale, consistent and high quality care,” Dr. McCormick said.
Foundations of a Hospital Medicine Telemedicine Program
Wednesday, 4:15–5:20 p.m.
Available via HM17 On Demand
DeSalvo: HM needs holistic approach to health care
LAS VEGAS – To deliver her message of inclusion Tuesday morning, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) Karen DeSalvo, MD, MPH, MSc, could think of “no finer group” than those assembled before her at HM17.
The thousands of hospitalists gathered to hear her keynote address, “Rethinking Health: The Vital Role of Hospitals and the Hospitalist,” listened as she talked about including more than just the best medical care in HM’s scope of practice. The job must evolve to include a focus on such social issues as economic stability, neighborhood and physical environment, education, and access to healthy options for food.
In other words, Dr. DeSalvo wondered aloud, what good is treating a grandmother’s heart failure over and over if she’s always going to return to the hospital because her home, her neighborhood, or her finances mean she is unable to prevent recurring health issues? [[{"fid":"195561","view_mode":"medstat_image_flush_left","attributes":{"alt":"Dr. Brian Harte conducts an interveiw with Dr. Karen DeSalvo duing the opening plenary Tuesday at HM17.","height":"147","width":"220","class":"media-element file-medstat-image-flush-left","data-delta":"1"},"fields":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Brian Harte conducts an interview with Dr. Karen DeSalvo during the opening plenary Tuesday at HM17.","field_file_image_credit[und][0][value]":"Darnell Scott","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Brian Harte conducts an interview with Dr. Karen DeSalvo during the opening plenary Tuesday at HM17.","field_file_image_credit[und][0][value]":"Darnell Scott"}}}]]
Hospitalists “have been at the center of change, not only in building a new field and showing us that medicine doesn’t have to always be the way it always was,” she said. “You have been at the forefront of seeing that we’re getting better value out of our health care system and, though that work must continue, you must also begin to broaden our thinking and understand that the drivers of health are much more than [just] health care. There are social determinants, social factors.”
Dr. DeSalvo, an internist by training, understands that dealing with social issues may seem like a role for others, but she said that the implications of those factors directly impact hospitalists and their institutions via issues such as readmissions.
“These things … don’t just matter conceptually,” she said. “They [have] direct relationships with mortality and morbidity and cost. They are literally affecting people’s lives in this country every day. When we begin to adjust them, to impact them, you can see that it also affects the health care system.”
On the front lines, Dr. DeSalvo said that hospitalists and others can work to take advantage of their hospital’s existing tools to link their patients to available resources, partner with local public health offices, and push to make their hospitals “anchor institutions to build community capacity to address these social determinants.”
Dr. DeSalvo also praised HM as a field that has already embraced value-based payment (VBP) models. She said that ability to anticipate and adapt to health care’s changing needs positions the field well as the Medicare Access and CHIP Reauthorization Act (MACRA) moves health care from fee-for-service to payment models that seek to manage risk and penalize mistakes.
LAS VEGAS – To deliver her message of inclusion Tuesday morning, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) Karen DeSalvo, MD, MPH, MSc, could think of “no finer group” than those assembled before her at HM17.
The thousands of hospitalists gathered to hear her keynote address, “Rethinking Health: The Vital Role of Hospitals and the Hospitalist,” listened as she talked about including more than just the best medical care in HM’s scope of practice. The job must evolve to include a focus on such social issues as economic stability, neighborhood and physical environment, education, and access to healthy options for food.
In other words, Dr. DeSalvo wondered aloud, what good is treating a grandmother’s heart failure over and over if she’s always going to return to the hospital because her home, her neighborhood, or her finances mean she is unable to prevent recurring health issues? [[{"fid":"195561","view_mode":"medstat_image_flush_left","attributes":{"alt":"Dr. Brian Harte conducts an interveiw with Dr. Karen DeSalvo duing the opening plenary Tuesday at HM17.","height":"147","width":"220","class":"media-element file-medstat-image-flush-left","data-delta":"1"},"fields":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Brian Harte conducts an interview with Dr. Karen DeSalvo during the opening plenary Tuesday at HM17.","field_file_image_credit[und][0][value]":"Darnell Scott","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Brian Harte conducts an interview with Dr. Karen DeSalvo during the opening plenary Tuesday at HM17.","field_file_image_credit[und][0][value]":"Darnell Scott"}}}]]
Hospitalists “have been at the center of change, not only in building a new field and showing us that medicine doesn’t have to always be the way it always was,” she said. “You have been at the forefront of seeing that we’re getting better value out of our health care system and, though that work must continue, you must also begin to broaden our thinking and understand that the drivers of health are much more than [just] health care. There are social determinants, social factors.”
Dr. DeSalvo, an internist by training, understands that dealing with social issues may seem like a role for others, but she said that the implications of those factors directly impact hospitalists and their institutions via issues such as readmissions.
“These things … don’t just matter conceptually,” she said. “They [have] direct relationships with mortality and morbidity and cost. They are literally affecting people’s lives in this country every day. When we begin to adjust them, to impact them, you can see that it also affects the health care system.”
On the front lines, Dr. DeSalvo said that hospitalists and others can work to take advantage of their hospital’s existing tools to link their patients to available resources, partner with local public health offices, and push to make their hospitals “anchor institutions to build community capacity to address these social determinants.”
Dr. DeSalvo also praised HM as a field that has already embraced value-based payment (VBP) models. She said that ability to anticipate and adapt to health care’s changing needs positions the field well as the Medicare Access and CHIP Reauthorization Act (MACRA) moves health care from fee-for-service to payment models that seek to manage risk and penalize mistakes.
LAS VEGAS – To deliver her message of inclusion Tuesday morning, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) Karen DeSalvo, MD, MPH, MSc, could think of “no finer group” than those assembled before her at HM17.
The thousands of hospitalists gathered to hear her keynote address, “Rethinking Health: The Vital Role of Hospitals and the Hospitalist,” listened as she talked about including more than just the best medical care in HM’s scope of practice. The job must evolve to include a focus on such social issues as economic stability, neighborhood and physical environment, education, and access to healthy options for food.
In other words, Dr. DeSalvo wondered aloud, what good is treating a grandmother’s heart failure over and over if she’s always going to return to the hospital because her home, her neighborhood, or her finances mean she is unable to prevent recurring health issues? [[{"fid":"195561","view_mode":"medstat_image_flush_left","attributes":{"alt":"Dr. Brian Harte conducts an interveiw with Dr. Karen DeSalvo duing the opening plenary Tuesday at HM17.","height":"147","width":"220","class":"media-element file-medstat-image-flush-left","data-delta":"1"},"fields":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Brian Harte conducts an interview with Dr. Karen DeSalvo during the opening plenary Tuesday at HM17.","field_file_image_credit[und][0][value]":"Darnell Scott","field_file_image_caption[und][0][format]":"plain_text","field_file_image_credit[und][0][format]":"plain_text"},"type":"media","field_deltas":{"1":{"format":"medstat_image_flush_left","field_file_image_caption[und][0][value]":"Dr. Brian Harte conducts an interview with Dr. Karen DeSalvo during the opening plenary Tuesday at HM17.","field_file_image_credit[und][0][value]":"Darnell Scott"}}}]]
Hospitalists “have been at the center of change, not only in building a new field and showing us that medicine doesn’t have to always be the way it always was,” she said. “You have been at the forefront of seeing that we’re getting better value out of our health care system and, though that work must continue, you must also begin to broaden our thinking and understand that the drivers of health are much more than [just] health care. There are social determinants, social factors.”
Dr. DeSalvo, an internist by training, understands that dealing with social issues may seem like a role for others, but she said that the implications of those factors directly impact hospitalists and their institutions via issues such as readmissions.
“These things … don’t just matter conceptually,” she said. “They [have] direct relationships with mortality and morbidity and cost. They are literally affecting people’s lives in this country every day. When we begin to adjust them, to impact them, you can see that it also affects the health care system.”
On the front lines, Dr. DeSalvo said that hospitalists and others can work to take advantage of their hospital’s existing tools to link their patients to available resources, partner with local public health offices, and push to make their hospitals “anchor institutions to build community capacity to address these social determinants.”
Dr. DeSalvo also praised HM as a field that has already embraced value-based payment (VBP) models. She said that ability to anticipate and adapt to health care’s changing needs positions the field well as the Medicare Access and CHIP Reauthorization Act (MACRA) moves health care from fee-for-service to payment models that seek to manage risk and penalize mistakes.
Optimism in the face of change
The first HM17 plenary is focused on health policy at a time when a dynamically evolving health care delivery system may seem daunting, opaque, and labyrinthine.
“Though it feels uncertain in some ways, the health care world is pretty united that we need to continue the progress we’ve made on moving away from the old fee-for-service model, toward one that lets people practice medicine the way they want and focus on patients and outcomes,” said HM17 keynote speaker Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS).
“That’s just the way that we finance or pay for care,” she said. “There’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes. Hospitalists, quite frankly, have been in the lead for 20 years and really understand in granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has already laid the path that must now be followed. The public sector’s move away from fee for service, toward payment for episodic care, has combined with emerging technology platforms to create a new age in which physicians and insurers can judge, in real-time, how well care is working.
Add to this the growth of accountable care organizations, other alternative payment models, value-based purchasing, and the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and it is clear the direction in which the industry is headed.
Of course, Dr. DeSalvo understands the fears of those wondering where the next wave of change will carry them. She’s heard the political debate over the past 8 years and the rancorous discussions in just the first few months of 2017. But she believes the path for health care delivery continues to be “toward the natural place as opposed to the unnatural place.”
“That gives me a lot of optimism,” she said. “One of the most important things for hospitalists to be doing right now is to keep standing up and speaking on behalf of patients and saying that the right thing is for us not to regress but to continue moving forward so that we can all have the kind of system we want for our patients.
The first HM17 plenary is focused on health policy at a time when a dynamically evolving health care delivery system may seem daunting, opaque, and labyrinthine.
“Though it feels uncertain in some ways, the health care world is pretty united that we need to continue the progress we’ve made on moving away from the old fee-for-service model, toward one that lets people practice medicine the way they want and focus on patients and outcomes,” said HM17 keynote speaker Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS).
“That’s just the way that we finance or pay for care,” she said. “There’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes. Hospitalists, quite frankly, have been in the lead for 20 years and really understand in granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has already laid the path that must now be followed. The public sector’s move away from fee for service, toward payment for episodic care, has combined with emerging technology platforms to create a new age in which physicians and insurers can judge, in real-time, how well care is working.
Add to this the growth of accountable care organizations, other alternative payment models, value-based purchasing, and the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and it is clear the direction in which the industry is headed.
Of course, Dr. DeSalvo understands the fears of those wondering where the next wave of change will carry them. She’s heard the political debate over the past 8 years and the rancorous discussions in just the first few months of 2017. But she believes the path for health care delivery continues to be “toward the natural place as opposed to the unnatural place.”
“That gives me a lot of optimism,” she said. “One of the most important things for hospitalists to be doing right now is to keep standing up and speaking on behalf of patients and saying that the right thing is for us not to regress but to continue moving forward so that we can all have the kind of system we want for our patients.
The first HM17 plenary is focused on health policy at a time when a dynamically evolving health care delivery system may seem daunting, opaque, and labyrinthine.
“Though it feels uncertain in some ways, the health care world is pretty united that we need to continue the progress we’ve made on moving away from the old fee-for-service model, toward one that lets people practice medicine the way they want and focus on patients and outcomes,” said HM17 keynote speaker Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS).
“That’s just the way that we finance or pay for care,” she said. “There’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes. Hospitalists, quite frankly, have been in the lead for 20 years and really understand in granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has already laid the path that must now be followed. The public sector’s move away from fee for service, toward payment for episodic care, has combined with emerging technology platforms to create a new age in which physicians and insurers can judge, in real-time, how well care is working.
Add to this the growth of accountable care organizations, other alternative payment models, value-based purchasing, and the implementation of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and it is clear the direction in which the industry is headed.
Of course, Dr. DeSalvo understands the fears of those wondering where the next wave of change will carry them. She’s heard the political debate over the past 8 years and the rancorous discussions in just the first few months of 2017. But she believes the path for health care delivery continues to be “toward the natural place as opposed to the unnatural place.”
“That gives me a lot of optimism,” she said. “One of the most important things for hospitalists to be doing right now is to keep standing up and speaking on behalf of patients and saying that the right thing is for us not to regress but to continue moving forward so that we can all have the kind of system we want for our patients.
Conway: HM well positioned for ‘system transformation’
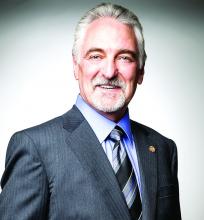
Patrick Conway, MD, MSc, MHM, may have had a lot of job titles recently, but his work address hasn’t changed in 6 years.
Dr. Conway, deputy administrator for innovation and quality for the Centers for Medicare & Medicaid Services and director of its Center for Medicare and Medicaid Innovation, has been at the intersection of policy and practice in Washington, since joining CMS in 2011. The still-practicing hospitalist was acting CMS administrator for several months earlier this year, holding the top post while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited U.S. Senate confirmation. His title before that was principal deputy administrator and CMS chief medical officer.
Dr. Conway said he believes that at a “macro legislation” level, Washington is committed to health care reform that improves patient care and incentivizes physicians to join alternative payment models (APMs). He said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable-care organizations, value-based purchasing, and the Medicare Access and CHIP Reauthorization Act of 2015, or MACRA. He said that as innovations lead to better patient care and more coordinated care, that’s good for hospitalists, patients, and the hospitals that bring them together.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged in these new payment models and help lead them and provide better patient care as part of them.”
Dr. Conway said that focusing on innovations is essential to hospitalists to ensure the specialty remains at the forefront of improved patient care, decreased readmissions, decreased infections and other quality improvements. He notes that by still practicing on an academic medical service with faculty, residents and medical students, he’s encouraged and excited that “people get it.”
“Every doctor wants better care for their patients,” Dr. Conway said. “The reality of … new payment systems and new fields of innovation we’re entering into is it unleashes hospitalists and aligns incentives with what they want for their patients.”
Take bundled payments around episodic care. With innovations in payment models, hospitalists are increasingly being paid for how good their care is, not how much care there is.
“That’s exciting,” Dr. Conway said. “Very different than 10 years ago where you had a lot of groups where it was about how much volume can we churn through. Now I think hospitals and HM groups [realize] value is going to continue to increasingly be based on the quality of care and the efficiency of care delivery.”
Patrick Conway, MD, MSc, MHM, may have had a lot of job titles recently, but his work address hasn’t changed in 6 years.
Dr. Conway, deputy administrator for innovation and quality for the Centers for Medicare & Medicaid Services and director of its Center for Medicare and Medicaid Innovation, has been at the intersection of policy and practice in Washington, since joining CMS in 2011. The still-practicing hospitalist was acting CMS administrator for several months earlier this year, holding the top post while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited U.S. Senate confirmation. His title before that was principal deputy administrator and CMS chief medical officer.
Dr. Conway said he believes that at a “macro legislation” level, Washington is committed to health care reform that improves patient care and incentivizes physicians to join alternative payment models (APMs). He said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable-care organizations, value-based purchasing, and the Medicare Access and CHIP Reauthorization Act of 2015, or MACRA. He said that as innovations lead to better patient care and more coordinated care, that’s good for hospitalists, patients, and the hospitals that bring them together.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged in these new payment models and help lead them and provide better patient care as part of them.”
Dr. Conway said that focusing on innovations is essential to hospitalists to ensure the specialty remains at the forefront of improved patient care, decreased readmissions, decreased infections and other quality improvements. He notes that by still practicing on an academic medical service with faculty, residents and medical students, he’s encouraged and excited that “people get it.”
“Every doctor wants better care for their patients,” Dr. Conway said. “The reality of … new payment systems and new fields of innovation we’re entering into is it unleashes hospitalists and aligns incentives with what they want for their patients.”
Take bundled payments around episodic care. With innovations in payment models, hospitalists are increasingly being paid for how good their care is, not how much care there is.
“That’s exciting,” Dr. Conway said. “Very different than 10 years ago where you had a lot of groups where it was about how much volume can we churn through. Now I think hospitals and HM groups [realize] value is going to continue to increasingly be based on the quality of care and the efficiency of care delivery.”
Patrick Conway, MD, MSc, MHM, may have had a lot of job titles recently, but his work address hasn’t changed in 6 years.
Dr. Conway, deputy administrator for innovation and quality for the Centers for Medicare & Medicaid Services and director of its Center for Medicare and Medicaid Innovation, has been at the intersection of policy and practice in Washington, since joining CMS in 2011. The still-practicing hospitalist was acting CMS administrator for several months earlier this year, holding the top post while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited U.S. Senate confirmation. His title before that was principal deputy administrator and CMS chief medical officer.
Dr. Conway said he believes that at a “macro legislation” level, Washington is committed to health care reform that improves patient care and incentivizes physicians to join alternative payment models (APMs). He said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable-care organizations, value-based purchasing, and the Medicare Access and CHIP Reauthorization Act of 2015, or MACRA. He said that as innovations lead to better patient care and more coordinated care, that’s good for hospitalists, patients, and the hospitals that bring them together.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged in these new payment models and help lead them and provide better patient care as part of them.”
Dr. Conway said that focusing on innovations is essential to hospitalists to ensure the specialty remains at the forefront of improved patient care, decreased readmissions, decreased infections and other quality improvements. He notes that by still practicing on an academic medical service with faculty, residents and medical students, he’s encouraged and excited that “people get it.”
“Every doctor wants better care for their patients,” Dr. Conway said. “The reality of … new payment systems and new fields of innovation we’re entering into is it unleashes hospitalists and aligns incentives with what they want for their patients.”
Take bundled payments around episodic care. With innovations in payment models, hospitalists are increasingly being paid for how good their care is, not how much care there is.
“That’s exciting,” Dr. Conway said. “Very different than 10 years ago where you had a lot of groups where it was about how much volume can we churn through. Now I think hospitals and HM groups [realize] value is going to continue to increasingly be based on the quality of care and the efficiency of care delivery.”
RIV poster contest a meeting highlight
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
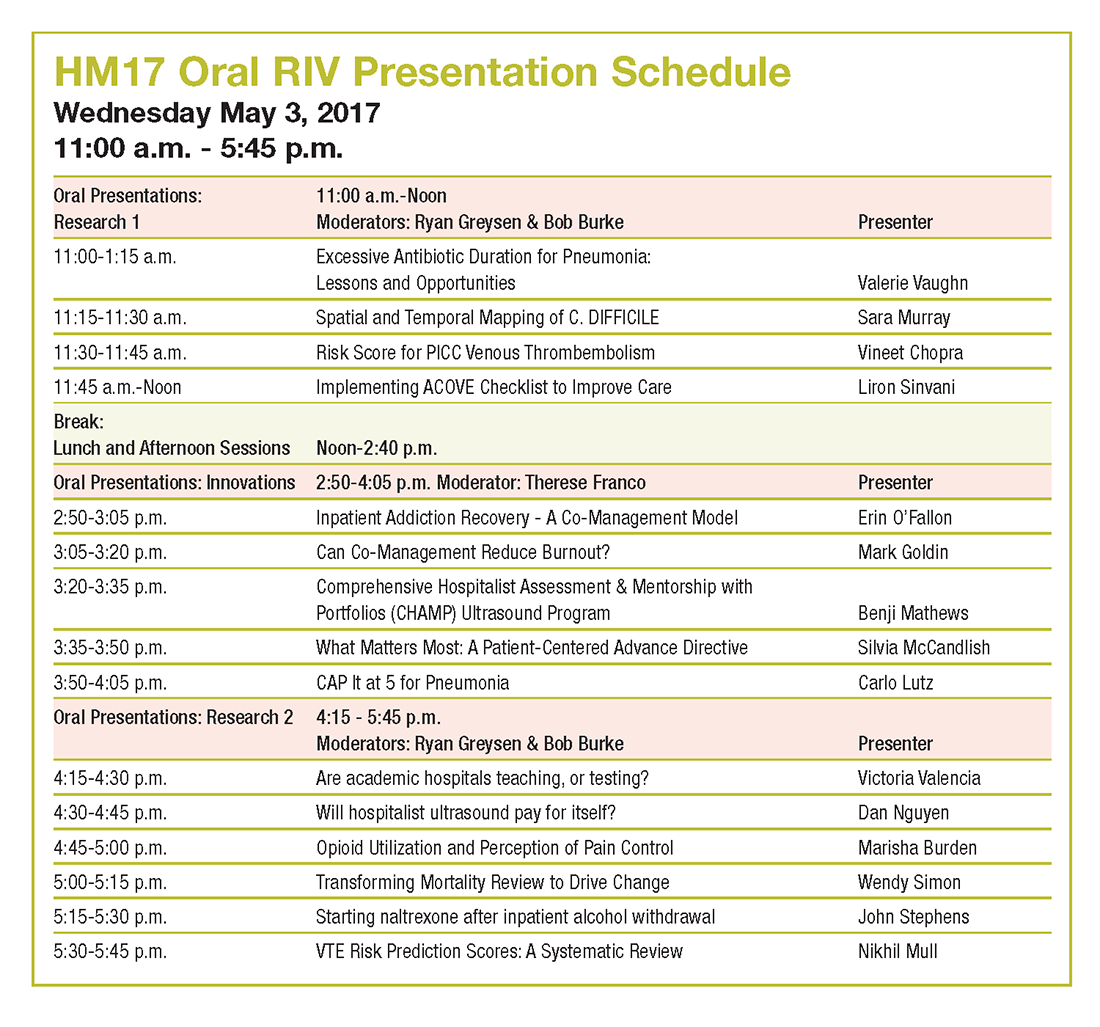
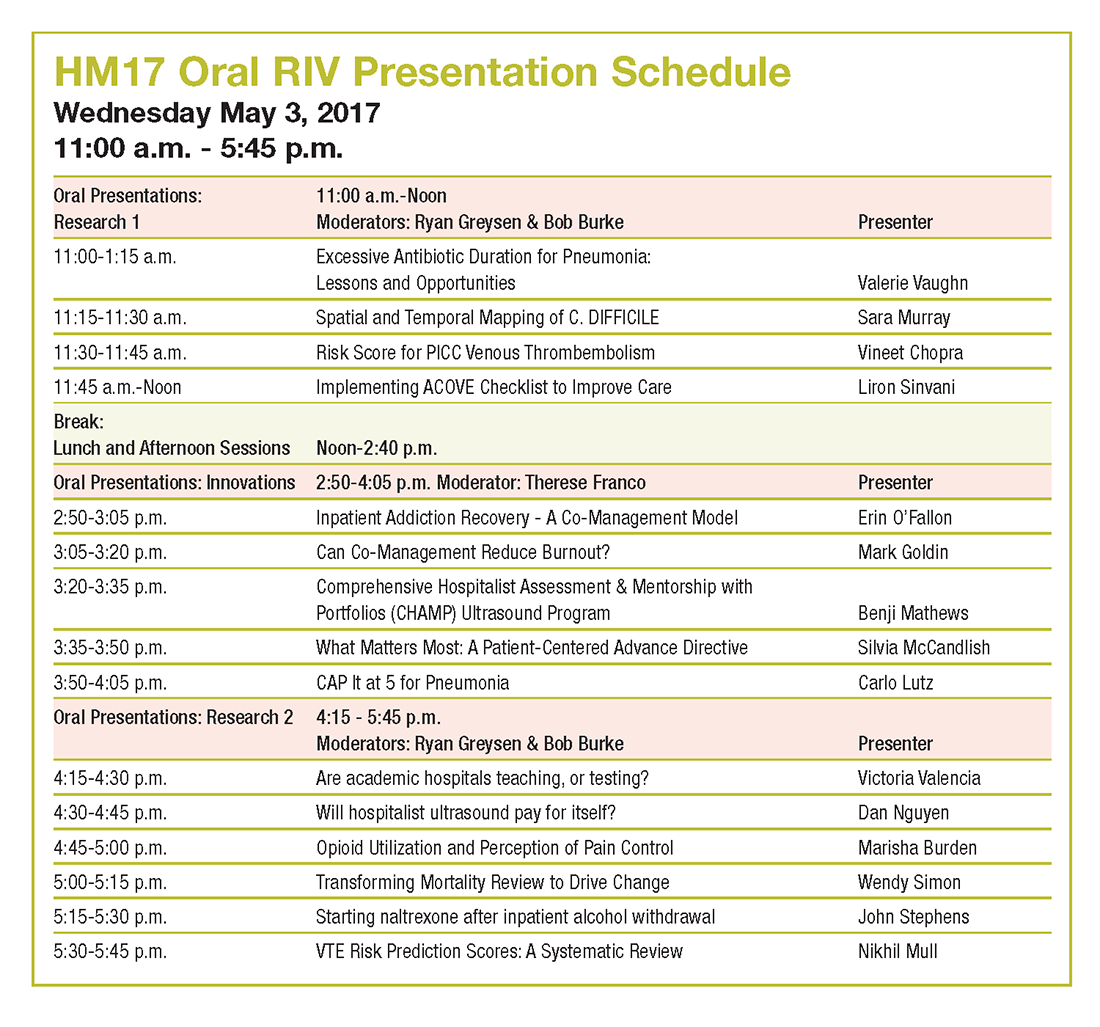
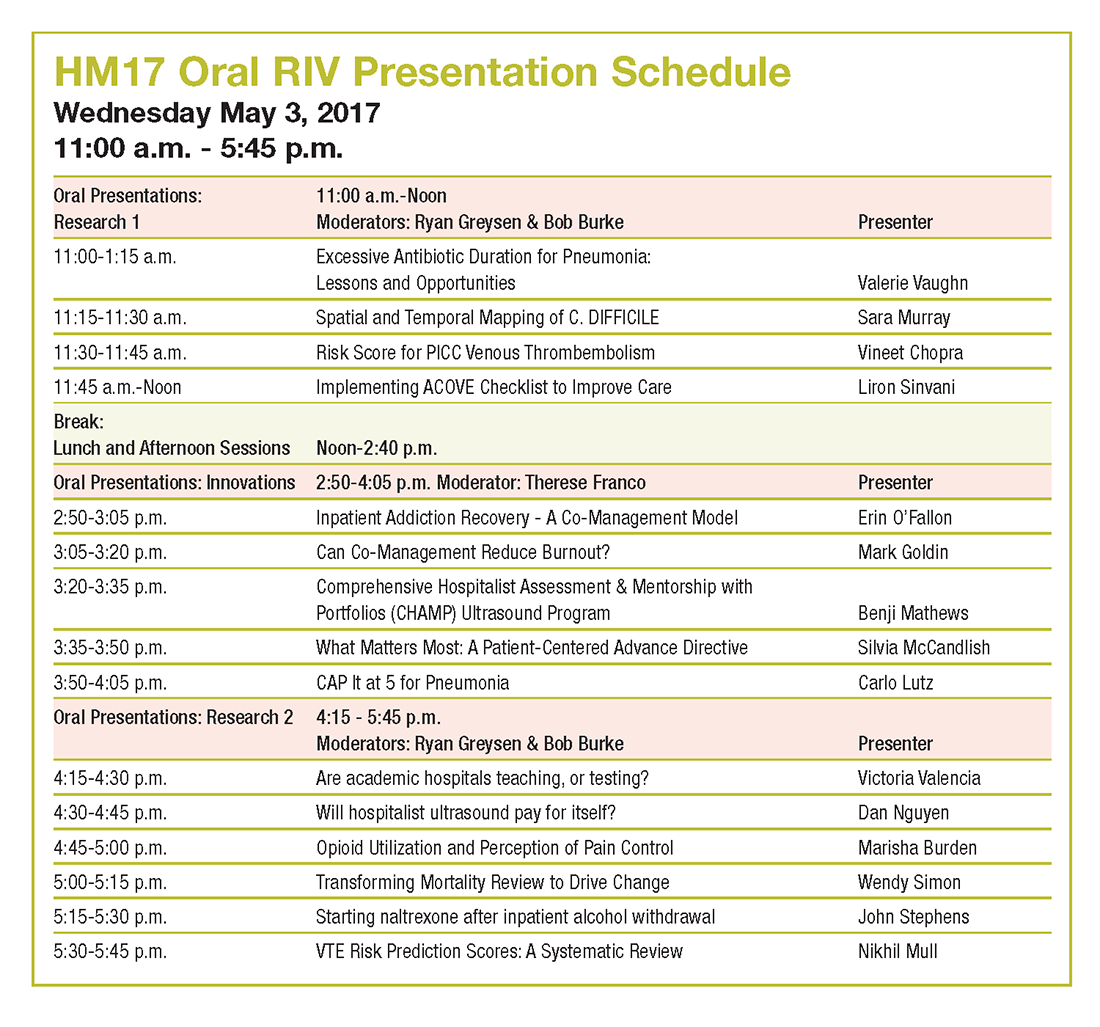
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
Tips from 'the father of modern networking'
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
What’s new at HM17
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”
There is only one annual meeting dedicated to hospitalists, designed by hospitalists, and focusing purely on issues important to hospitalists. But even that isn’t enough to make sure more hospitalists show up every year.
That’s because a yearly conference can’t just be a rehash of the last one.
A valuable conference, certainly one worth spending the bulk of a continuing medical budget on, offers something new every year. Or, to look at the schedule for HM17, a lot of new every year.
That’s an unlikely complaint this year. The annual meeting schedule for May 1-4 at Mandalay Bay Resort and Casino includes five new educational tracks: High Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
“We’re really excited to be able to offer more clinical content,” said HM17 course director Lenny Feldman, MD, FAAP, FACP, SFHM.
Dr. Feldman sees each of the new tracks as filling separate and specific needs of HM attendees who vary from nonphysician providers to hospitalists to medical students.
Take, for instance, the High Value Care, Clinical Updates, and Diagnostic Reasoning sessions that are debuting.
“We wanted to make sure that we had as many clinically oriented sessions as possible,” Dr. Feldman said. “Which meant we needed to increase the amount of clinical content we have offered compared to the past few years. The new clinical track allows us to add probably 12 or so different sessions that will fill the needs of our attendees.”
The Diagnostic Reasoning and High Value Care tracks, in particular, highlight the annual meeting’s continued evolution toward a focus on evidence-based care, as that mantra becomes a bedrock of clinical treatment.
“Training our hospitalists to use the best dialogistic reasoning in their approach to their patients is a big push in hospital medicine right now,” Dr. Feldman said, “Hopefully, a track on that topic will excite people who love thinking about medicine, who got into medicine because of the mystery and want a renewed focus on how to be a great diagnostician.”
Dr. Feldman also noted that the High Value Care track should be a hot topic, as hospitalists want to learn how to provide high quality and high value care to patients at the same time. The new tracks should appeal to different groups and make the annual meeting more appealing to a variety of attendees, not just rank-and-file doctors.
The mini Medical Education track, for instance, is a subset of a half-dozen sessions tailored directly to medical educators in academic settings who face different challenges than their counterparts in community settings. The same goes for the Health Policy track, which will offer a handful of sessions suitable for novices looking to learn more in an age of reform, or policy wonks hoping to expand their knowledge.
Meeting evolving needs
New offerings aren’t limited to the main conference schedule. The 2017 roster of pre-courses includes one titled, “Bugs, Drugs and You: Infectious Diseases ‘Boot Camp’ for Hospitalists.” This daylong session hasn’t been held since 2013, and copresenter Jennifer Hanrahan, DO, associate professor of medicine at Case Western Reserve University in Cleveland, says the timing is good.
“I don’t know that the percentage of people hospitalized for infection has increased,” she said. “Because we are doing things more quickly than we did in the past, length of stays are shorter and there is a lot of pressure to get patients out of the hospital. There is a lot of consultation with Infectious Disease.”
Dr. Hanrahan, who also serves as medical director of infection prevention at Cleveland’s MetroHealth Medical Center, says that with so many patients hospitalized for infections, the value of updating one’s knowledge every few years is critical.
“I’ve been an infectious disease physician for 18 years and I’m also a hospitalist,” she said. “The types of questions I get vary a great deal depending on the experience of the hospitalist. My hope would be that we would be able to provide a basic level of understanding so that people would be more confident in approaching these problems.”
Another new feature this year is offer some of the most popular sessions at multiple times. In years past, popular sessions – such as “Update and Pearls in Infectious Diseases” and “Non–Evidence-Based Medicine: Things We Do for No Reason” – are standing room only events with attendees sitting on floors or gathered to eavesdrop from doorways.
“That says something about the content that’s being delivered, but that’s not very comfortable for folks who want to sit through a session,” Dr. Feldman said. “We’ve decided to add repeat sessions of popular presentations. We want everyone to be comfortable while they’re learning the important clinical content that’s being delivered at these sessions.”
The 2017 focus on healthcare policy is also new. Educational sessions on the policy landscape will be formally buttressed by plenary presentations from Patrick Conway, MD, MSc, MHM, deputy administrator for Innovation and Quality at the Centers for Medicare & Medicaid Services and director of the Center for Medicare and Medicaid Innovation, and Karen DeSalvo, MD, MPH, MSc, a former acting assistant secretary for health at the U.S. Department of Health and Human Services and national coordinator for health information technology.
“There’s a thirst for (policy news) among members of the Society of Hospital Medicine,” Dr. Feldman said. “It is easy to get lost in the day-to-day work that we do, but I think most of us really enjoy hearing about the bigger picture, especially when the bigger picture is in flux.”
“Right now, this is critical,” added Dr. Finn. “Health insurance coverage has a huge impact on hospitals. I think all practicing hospitalists will need to engage with the hospital C-suite if insurance and coverage changes. Since we are hospital based, we are directly tied to anything that the federal government does in terms of health care changes. It’s important for hospitalists to be knowledgeable about health policy.”
One major highlight of the meeting calendar – less new and more historically under-appreciated, in Dr. Feldman’s view – should be the 18 workshop presentations, which are essentially 90-minute dissertations, whittled down from roughly 150 submissions.
“These are the best submissions that we received,” Dr. Feldman said. “We worked hard to make sure that the workshops encompass the breadth and depth of hospital medicine. It is not just one area that’s covered in every workshop. We’ll have workshops ranging from clinical reasoning and communication with patients, to quality improvement issues and high value care discussions, as well as a case-based approach to inpatient dermatology.”
While annual meetings’ new offerings are always an important draw, Dr. Feldman says that the annual “standbys,” such as practice management and pediatrics, are necessary to keep attendees up to date on best practices in changing times.
“It’s pretty self-evident that if we’re going to be an important specialty, we need to serve those who are caring for patients day in and day out, as well as folks who are researching how we can do it better,” he said. “Then we must make sure that data is disseminated to all of us who are taking care of patients. That’s one of the really important parts of this meeting: dissemination of the important work.”