User login
Richard Quinn is an award-winning journalist with 15 years’ experience. He has worked at the Asbury Park Press in New Jersey and The Virginian-Pilot in Norfolk, Va., and currently is managing editor for a leading commercial real estate publication. His freelance work has appeared in The Jewish State, The Hospitalist, The Rheumatologist, ACEP Now, and ENT Today. He lives in New Jersey with his wife and three cats.
HM17’s ‘must-see sessions’
LAS VEGAS — Not to sound like a Sin City come on, but pick a course, any course.
No, seriously.
Hospitalists and other attendees at the Hospitalist Medicine 2017 meeting next month will do well to figure out what sessions they want to attend before arriving at the Mandalay Bay Resort and Casino. This 4-day Super Bowl of hospital medicine prides itself on offering more than any attendee can find time for. This year is no exception, as the annual meeting has added five new educational tracks: High-Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
The committee does its job to fill the meeting with best-in-class educational sessions. Here are some of the group’s recommendations for this year’s meeting:
1. “The Hospitalist’s Role in the Opioid Epidemic” – Tuesday, May 2; 1:35 p.m.–2:35 p.m.
2. “Opioids for Acute Pain Management in the Seriously Ill – How to Safely Prescribe” – Wednesday, May 3; 2:50 p.m.–3:30 p.m.
3. “Non-opiate Pain Management for the Hospitalist” – Wednesday, May 3; 4:20 p.m.–5:00 p.m.
Elizabeth Cook, MD, medical director of the hospitalist division of Medical Associates of Central Virginia in Lynchburg, said, “The historical emphasis on pain control has helped contributed to the current epidemic of opioid abuse, overdoses, and deaths. Hospitalists have a need to use these medications for care of the hospitalized patient but have an important part to play in leading the way to appropriate use and patient education regarding the dangers of these medications. These sessions will provide hospitalists with some tools to use in beginning to effect a shift in pain management strategies and responsible use of narcotic pain medications.”
Miguel Angel Villagra, MD, FACP, FHM, hospitalist department program medical director at White River Medical Center in Batesville, Ark., said, “As primary front-line providers in the acute care setting, we face the everyday struggles in the management of chronic opioid users. Acquiring some general guidelines can help us tailor our approach within an ethical focus to improve the care of this population.”
Sarah Stella, MD, an academic hospitalist at Denver Health, said, “This is a crucial and timely topic. Hospitalists have had a hand in perpetuating the opioid epidemic and can play an important role in helping to end it. In this regard, there are many opportunities to do good, such as judicious prescribing and tapering medications for acute pain, starting eligible patients on Suboxone [buprenorphine] in-house, and arranging substance abuse treatment follow-up.”
4. “Focus on POCUS - Introduction to Point-of-Care Ultrasound for Pediatric Hospitalists” – Tuesday, May 2; 10:35 a.m.–11:35 a.m.
Weijen Chang, MD, SFHM, FAAP, chief of the division of pediatric hospital medicine, Baystate Medical Center/Baystate Children’s Hospital, Springfield, Mass., said, “This is the first pediatric POCUS session offered at SHM ever. And it does not require an additional cost ... the pediatric track is critically important, as a substantial number of athlete attendees are either Peds or MedPeds. I think SHM aims to create a pediatric track that discusses topics that are less covered in other meetings, such as the value equation and issues facing women leaders in HM.”
6. “Foundations of a Hospital Medicine Telemedicine Program” – Wednesday, May 3; 415 p.m.–5:20 p.m.
Dr. Villagra added, “Telemedicine is a new innovative technology with the promise of overcoming geographical barriers to health care providers. A lot of new companies and software development has made this technology more user/patient friendly.”
7. “Hot Topics in Health Policy for Hospitalists” – Thursday, May 4; 7:40 a.m.–8:35 a.m.
8. “The Impact of the New Administration on Health Care Reform” – Thursday, May 4; 8:45 a.m.–9:40 a.m.
9. “Health Care Payment Reform for Hospitalist 2017: Tips for MIPS and Beyond” – Thursday, May 4; 9:50 a.m.–10:45 a.m.
Dr. Stella said, “As a safety-net hospitalist in Colorado, a state which largely expanded Medicare under the Affordable Care Act (ACA), I am concerned about the impact repealing the ACA would have on my patients as well as on safety-net hospitals such as my own. I hope that these sessions will increase my understanding of the issues and my ability to advocate for my patients.”
Dr. Cook said, “The U.S. government is functioning in historically unprecedented ways with major shifts in health care policy expected to occur over the next 4 years. It is essential that physician leaders play an active role in shaping the discussion around these important topics ... hospitalists have an opportunity to provide leadership in this arena, and these sessions will help participants to build the knowledge about these complex issues that is crucial to being an active part of the dialogue.”
10. “Workshop: Hospitalists as Leaders in Patient Flow and Hospital Throughput” – Thursday, May 4; 10 a.m.–11:30 a.m.
Dr. Stella said, “Recently, I was appointed to a leadership role on a major initiative to improve hospital patient flow at my institution. We are concentrating on several different areas, including avoidable hospitalizations, preventable excess days, delayed discharges, and variable access to services. I was excited to see a workshop this year dedicated to how hospitalists can successfully lead such initiatives. I will definitely be attending this session as I am interested in what others are doing in their institutions to creatively overcome patient flow challenges.”
11. “Hospitalist Careers: So Many Options” – Tuesday, May 2; 10:35 a.m.–11:15 a.m.
Dr. Villagra said, “Hospital medicine has so many pathways for a full career development and is not a pit stop before fellowship. Early- and mid-career hospitalists can benefit from interactions with senior hospitalists for the understanding of what hospital medicine has to offer for their professional growth.”
Richard Quinn is a freelance writer in New Jersey.
LAS VEGAS — Not to sound like a Sin City come on, but pick a course, any course.
No, seriously.
Hospitalists and other attendees at the Hospitalist Medicine 2017 meeting next month will do well to figure out what sessions they want to attend before arriving at the Mandalay Bay Resort and Casino. This 4-day Super Bowl of hospital medicine prides itself on offering more than any attendee can find time for. This year is no exception, as the annual meeting has added five new educational tracks: High-Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
The committee does its job to fill the meeting with best-in-class educational sessions. Here are some of the group’s recommendations for this year’s meeting:
1. “The Hospitalist’s Role in the Opioid Epidemic” – Tuesday, May 2; 1:35 p.m.–2:35 p.m.
2. “Opioids for Acute Pain Management in the Seriously Ill – How to Safely Prescribe” – Wednesday, May 3; 2:50 p.m.–3:30 p.m.
3. “Non-opiate Pain Management for the Hospitalist” – Wednesday, May 3; 4:20 p.m.–5:00 p.m.
Elizabeth Cook, MD, medical director of the hospitalist division of Medical Associates of Central Virginia in Lynchburg, said, “The historical emphasis on pain control has helped contributed to the current epidemic of opioid abuse, overdoses, and deaths. Hospitalists have a need to use these medications for care of the hospitalized patient but have an important part to play in leading the way to appropriate use and patient education regarding the dangers of these medications. These sessions will provide hospitalists with some tools to use in beginning to effect a shift in pain management strategies and responsible use of narcotic pain medications.”
Miguel Angel Villagra, MD, FACP, FHM, hospitalist department program medical director at White River Medical Center in Batesville, Ark., said, “As primary front-line providers in the acute care setting, we face the everyday struggles in the management of chronic opioid users. Acquiring some general guidelines can help us tailor our approach within an ethical focus to improve the care of this population.”
Sarah Stella, MD, an academic hospitalist at Denver Health, said, “This is a crucial and timely topic. Hospitalists have had a hand in perpetuating the opioid epidemic and can play an important role in helping to end it. In this regard, there are many opportunities to do good, such as judicious prescribing and tapering medications for acute pain, starting eligible patients on Suboxone [buprenorphine] in-house, and arranging substance abuse treatment follow-up.”
4. “Focus on POCUS - Introduction to Point-of-Care Ultrasound for Pediatric Hospitalists” – Tuesday, May 2; 10:35 a.m.–11:35 a.m.
Weijen Chang, MD, SFHM, FAAP, chief of the division of pediatric hospital medicine, Baystate Medical Center/Baystate Children’s Hospital, Springfield, Mass., said, “This is the first pediatric POCUS session offered at SHM ever. And it does not require an additional cost ... the pediatric track is critically important, as a substantial number of athlete attendees are either Peds or MedPeds. I think SHM aims to create a pediatric track that discusses topics that are less covered in other meetings, such as the value equation and issues facing women leaders in HM.”
6. “Foundations of a Hospital Medicine Telemedicine Program” – Wednesday, May 3; 415 p.m.–5:20 p.m.
Dr. Villagra added, “Telemedicine is a new innovative technology with the promise of overcoming geographical barriers to health care providers. A lot of new companies and software development has made this technology more user/patient friendly.”
7. “Hot Topics in Health Policy for Hospitalists” – Thursday, May 4; 7:40 a.m.–8:35 a.m.
8. “The Impact of the New Administration on Health Care Reform” – Thursday, May 4; 8:45 a.m.–9:40 a.m.
9. “Health Care Payment Reform for Hospitalist 2017: Tips for MIPS and Beyond” – Thursday, May 4; 9:50 a.m.–10:45 a.m.
Dr. Stella said, “As a safety-net hospitalist in Colorado, a state which largely expanded Medicare under the Affordable Care Act (ACA), I am concerned about the impact repealing the ACA would have on my patients as well as on safety-net hospitals such as my own. I hope that these sessions will increase my understanding of the issues and my ability to advocate for my patients.”
Dr. Cook said, “The U.S. government is functioning in historically unprecedented ways with major shifts in health care policy expected to occur over the next 4 years. It is essential that physician leaders play an active role in shaping the discussion around these important topics ... hospitalists have an opportunity to provide leadership in this arena, and these sessions will help participants to build the knowledge about these complex issues that is crucial to being an active part of the dialogue.”
10. “Workshop: Hospitalists as Leaders in Patient Flow and Hospital Throughput” – Thursday, May 4; 10 a.m.–11:30 a.m.
Dr. Stella said, “Recently, I was appointed to a leadership role on a major initiative to improve hospital patient flow at my institution. We are concentrating on several different areas, including avoidable hospitalizations, preventable excess days, delayed discharges, and variable access to services. I was excited to see a workshop this year dedicated to how hospitalists can successfully lead such initiatives. I will definitely be attending this session as I am interested in what others are doing in their institutions to creatively overcome patient flow challenges.”
11. “Hospitalist Careers: So Many Options” – Tuesday, May 2; 10:35 a.m.–11:15 a.m.
Dr. Villagra said, “Hospital medicine has so many pathways for a full career development and is not a pit stop before fellowship. Early- and mid-career hospitalists can benefit from interactions with senior hospitalists for the understanding of what hospital medicine has to offer for their professional growth.”
Richard Quinn is a freelance writer in New Jersey.
LAS VEGAS — Not to sound like a Sin City come on, but pick a course, any course.
No, seriously.
Hospitalists and other attendees at the Hospitalist Medicine 2017 meeting next month will do well to figure out what sessions they want to attend before arriving at the Mandalay Bay Resort and Casino. This 4-day Super Bowl of hospital medicine prides itself on offering more than any attendee can find time for. This year is no exception, as the annual meeting has added five new educational tracks: High-Value Care, Clinical Updates, Health Policy, Diagnostic Reasoning, and Medical Education.
The committee does its job to fill the meeting with best-in-class educational sessions. Here are some of the group’s recommendations for this year’s meeting:
1. “The Hospitalist’s Role in the Opioid Epidemic” – Tuesday, May 2; 1:35 p.m.–2:35 p.m.
2. “Opioids for Acute Pain Management in the Seriously Ill – How to Safely Prescribe” – Wednesday, May 3; 2:50 p.m.–3:30 p.m.
3. “Non-opiate Pain Management for the Hospitalist” – Wednesday, May 3; 4:20 p.m.–5:00 p.m.
Elizabeth Cook, MD, medical director of the hospitalist division of Medical Associates of Central Virginia in Lynchburg, said, “The historical emphasis on pain control has helped contributed to the current epidemic of opioid abuse, overdoses, and deaths. Hospitalists have a need to use these medications for care of the hospitalized patient but have an important part to play in leading the way to appropriate use and patient education regarding the dangers of these medications. These sessions will provide hospitalists with some tools to use in beginning to effect a shift in pain management strategies and responsible use of narcotic pain medications.”
Miguel Angel Villagra, MD, FACP, FHM, hospitalist department program medical director at White River Medical Center in Batesville, Ark., said, “As primary front-line providers in the acute care setting, we face the everyday struggles in the management of chronic opioid users. Acquiring some general guidelines can help us tailor our approach within an ethical focus to improve the care of this population.”
Sarah Stella, MD, an academic hospitalist at Denver Health, said, “This is a crucial and timely topic. Hospitalists have had a hand in perpetuating the opioid epidemic and can play an important role in helping to end it. In this regard, there are many opportunities to do good, such as judicious prescribing and tapering medications for acute pain, starting eligible patients on Suboxone [buprenorphine] in-house, and arranging substance abuse treatment follow-up.”
4. “Focus on POCUS - Introduction to Point-of-Care Ultrasound for Pediatric Hospitalists” – Tuesday, May 2; 10:35 a.m.–11:35 a.m.
Weijen Chang, MD, SFHM, FAAP, chief of the division of pediatric hospital medicine, Baystate Medical Center/Baystate Children’s Hospital, Springfield, Mass., said, “This is the first pediatric POCUS session offered at SHM ever. And it does not require an additional cost ... the pediatric track is critically important, as a substantial number of athlete attendees are either Peds or MedPeds. I think SHM aims to create a pediatric track that discusses topics that are less covered in other meetings, such as the value equation and issues facing women leaders in HM.”
6. “Foundations of a Hospital Medicine Telemedicine Program” – Wednesday, May 3; 415 p.m.–5:20 p.m.
Dr. Villagra added, “Telemedicine is a new innovative technology with the promise of overcoming geographical barriers to health care providers. A lot of new companies and software development has made this technology more user/patient friendly.”
7. “Hot Topics in Health Policy for Hospitalists” – Thursday, May 4; 7:40 a.m.–8:35 a.m.
8. “The Impact of the New Administration on Health Care Reform” – Thursday, May 4; 8:45 a.m.–9:40 a.m.
9. “Health Care Payment Reform for Hospitalist 2017: Tips for MIPS and Beyond” – Thursday, May 4; 9:50 a.m.–10:45 a.m.
Dr. Stella said, “As a safety-net hospitalist in Colorado, a state which largely expanded Medicare under the Affordable Care Act (ACA), I am concerned about the impact repealing the ACA would have on my patients as well as on safety-net hospitals such as my own. I hope that these sessions will increase my understanding of the issues and my ability to advocate for my patients.”
Dr. Cook said, “The U.S. government is functioning in historically unprecedented ways with major shifts in health care policy expected to occur over the next 4 years. It is essential that physician leaders play an active role in shaping the discussion around these important topics ... hospitalists have an opportunity to provide leadership in this arena, and these sessions will help participants to build the knowledge about these complex issues that is crucial to being an active part of the dialogue.”
10. “Workshop: Hospitalists as Leaders in Patient Flow and Hospital Throughput” – Thursday, May 4; 10 a.m.–11:30 a.m.
Dr. Stella said, “Recently, I was appointed to a leadership role on a major initiative to improve hospital patient flow at my institution. We are concentrating on several different areas, including avoidable hospitalizations, preventable excess days, delayed discharges, and variable access to services. I was excited to see a workshop this year dedicated to how hospitalists can successfully lead such initiatives. I will definitely be attending this session as I am interested in what others are doing in their institutions to creatively overcome patient flow challenges.”
11. “Hospitalist Careers: So Many Options” – Tuesday, May 2; 10:35 a.m.–11:15 a.m.
Dr. Villagra said, “Hospital medicine has so many pathways for a full career development and is not a pit stop before fellowship. Early- and mid-career hospitalists can benefit from interactions with senior hospitalists for the understanding of what hospital medicine has to offer for their professional growth.”
Richard Quinn is a freelance writer in New Jersey.
Fellows and Awards of Excellence
Vineet Arora, MD, understands the unique value of being named one of this year’s three Masters in Hospital Medicine. It’s an honor bestowed for hospitalists, by hospitalists.
“I take a lot of pride in an honor determined by peers,” said Dr. Arora, an academic hospitalist at University of Chicago Medicine. “While peers are often the biggest support you receive in your professional career, because they are in the trenches with you, they can also be your best critics. That is especially true of the type of work that I do, which relies on the buy-in of frontline clinicians – including hospitalists and trainees – to achieve better patient care and education.”
The designation of new Masters in Hospital Medicine is a major moment at SHM’s annual meeting. The 2017 list of awardees is headlined by Dr. Arora and the other MHM designees: former SHM President Burke Kealey, MD, and Richard Slataper, MD, who was heavily involved with the National Association of Inpatient Physicians, a predecessor to SHM. The three new masters bring to 24 the number of MHMs the society has named since unveiling the honor in 2010.
Dr. Arora understands that after 20 years as a specialty, just two dozen practitioners have reached hospital medicine’s highest professional distinction.
“I think of ‘mastery’ as someone who has achieved the highest level of expertise in a field, so an honor like Master in Hospital Medicine definitely means a lot to me,” she said. “Especially given the prior recipients of this honor, and the importance of SHM in my own professional growth and development since I was a trainee.”
In addition to the top honor, HM17 will see the induction of 159 Fellows in Hospital Medicine (FHM) and 58 Senior Fellows in Hospital Medicine (SFHM). This year’s fellows join the thousands of physicians and nonphysician providers (NPPs) that have attained the distinction.
SHM also bestows its annual Awards of Excellence (past winners listed here include Dr. Arora and Dr. Kealey) that recognize practitioners across skill sets. The awards are meant to honor SHM members “whose exemplary contributions to the hospital medicine movement deserve acknowledgment and respect,” according to the society’s website.
The 2017 Award winners include:
• Excellence in Teamwork in Quality Improvement: Johnston Memorial Hospital in Abingdon, Va.
• Excellence in Research: Jeffrey Barsuk, MD, MS, SFHM.
• Excellence in Teaching: Steven Cohn, MD, FACP, SFHM.
• Excellence in Hospital Medicine for Non-Physicians: Michael McFall.
• Outstanding Service in Hospital Medicine: Jeffrey Greenwald, MD, SFHM.
• Clinical Excellence: Barbara Slawski, MD.
• Excellence in Humanitarian Services: Jonathan Crocker, MD, FHM.
Dr. Arora, who has served on the SHM committee that analyzes all nominees for the annual awards, recognizes the value of honoring these high-achieving clinicians.
“There is great value to having our specialty society recognize members in different ways,” she said “The awards of excellence serve as a wonderful reminder of the incredible impact that hospitalists have in many diverse ways … while having the distinction of a fellow or senior fellow serves as a nice benchmark to which new hospitalists can aspire and gain recognition as they emerge as leaders in the field.”
Vineet Arora, MD, understands the unique value of being named one of this year’s three Masters in Hospital Medicine. It’s an honor bestowed for hospitalists, by hospitalists.
“I take a lot of pride in an honor determined by peers,” said Dr. Arora, an academic hospitalist at University of Chicago Medicine. “While peers are often the biggest support you receive in your professional career, because they are in the trenches with you, they can also be your best critics. That is especially true of the type of work that I do, which relies on the buy-in of frontline clinicians – including hospitalists and trainees – to achieve better patient care and education.”
The designation of new Masters in Hospital Medicine is a major moment at SHM’s annual meeting. The 2017 list of awardees is headlined by Dr. Arora and the other MHM designees: former SHM President Burke Kealey, MD, and Richard Slataper, MD, who was heavily involved with the National Association of Inpatient Physicians, a predecessor to SHM. The three new masters bring to 24 the number of MHMs the society has named since unveiling the honor in 2010.
Dr. Arora understands that after 20 years as a specialty, just two dozen practitioners have reached hospital medicine’s highest professional distinction.
“I think of ‘mastery’ as someone who has achieved the highest level of expertise in a field, so an honor like Master in Hospital Medicine definitely means a lot to me,” she said. “Especially given the prior recipients of this honor, and the importance of SHM in my own professional growth and development since I was a trainee.”
In addition to the top honor, HM17 will see the induction of 159 Fellows in Hospital Medicine (FHM) and 58 Senior Fellows in Hospital Medicine (SFHM). This year’s fellows join the thousands of physicians and nonphysician providers (NPPs) that have attained the distinction.
SHM also bestows its annual Awards of Excellence (past winners listed here include Dr. Arora and Dr. Kealey) that recognize practitioners across skill sets. The awards are meant to honor SHM members “whose exemplary contributions to the hospital medicine movement deserve acknowledgment and respect,” according to the society’s website.
The 2017 Award winners include:
• Excellence in Teamwork in Quality Improvement: Johnston Memorial Hospital in Abingdon, Va.
• Excellence in Research: Jeffrey Barsuk, MD, MS, SFHM.
• Excellence in Teaching: Steven Cohn, MD, FACP, SFHM.
• Excellence in Hospital Medicine for Non-Physicians: Michael McFall.
• Outstanding Service in Hospital Medicine: Jeffrey Greenwald, MD, SFHM.
• Clinical Excellence: Barbara Slawski, MD.
• Excellence in Humanitarian Services: Jonathan Crocker, MD, FHM.
Dr. Arora, who has served on the SHM committee that analyzes all nominees for the annual awards, recognizes the value of honoring these high-achieving clinicians.
“There is great value to having our specialty society recognize members in different ways,” she said “The awards of excellence serve as a wonderful reminder of the incredible impact that hospitalists have in many diverse ways … while having the distinction of a fellow or senior fellow serves as a nice benchmark to which new hospitalists can aspire and gain recognition as they emerge as leaders in the field.”
Vineet Arora, MD, understands the unique value of being named one of this year’s three Masters in Hospital Medicine. It’s an honor bestowed for hospitalists, by hospitalists.
“I take a lot of pride in an honor determined by peers,” said Dr. Arora, an academic hospitalist at University of Chicago Medicine. “While peers are often the biggest support you receive in your professional career, because they are in the trenches with you, they can also be your best critics. That is especially true of the type of work that I do, which relies on the buy-in of frontline clinicians – including hospitalists and trainees – to achieve better patient care and education.”
The designation of new Masters in Hospital Medicine is a major moment at SHM’s annual meeting. The 2017 list of awardees is headlined by Dr. Arora and the other MHM designees: former SHM President Burke Kealey, MD, and Richard Slataper, MD, who was heavily involved with the National Association of Inpatient Physicians, a predecessor to SHM. The three new masters bring to 24 the number of MHMs the society has named since unveiling the honor in 2010.
Dr. Arora understands that after 20 years as a specialty, just two dozen practitioners have reached hospital medicine’s highest professional distinction.
“I think of ‘mastery’ as someone who has achieved the highest level of expertise in a field, so an honor like Master in Hospital Medicine definitely means a lot to me,” she said. “Especially given the prior recipients of this honor, and the importance of SHM in my own professional growth and development since I was a trainee.”
In addition to the top honor, HM17 will see the induction of 159 Fellows in Hospital Medicine (FHM) and 58 Senior Fellows in Hospital Medicine (SFHM). This year’s fellows join the thousands of physicians and nonphysician providers (NPPs) that have attained the distinction.
SHM also bestows its annual Awards of Excellence (past winners listed here include Dr. Arora and Dr. Kealey) that recognize practitioners across skill sets. The awards are meant to honor SHM members “whose exemplary contributions to the hospital medicine movement deserve acknowledgment and respect,” according to the society’s website.
The 2017 Award winners include:
• Excellence in Teamwork in Quality Improvement: Johnston Memorial Hospital in Abingdon, Va.
• Excellence in Research: Jeffrey Barsuk, MD, MS, SFHM.
• Excellence in Teaching: Steven Cohn, MD, FACP, SFHM.
• Excellence in Hospital Medicine for Non-Physicians: Michael McFall.
• Outstanding Service in Hospital Medicine: Jeffrey Greenwald, MD, SFHM.
• Clinical Excellence: Barbara Slawski, MD.
• Excellence in Humanitarian Services: Jonathan Crocker, MD, FHM.
Dr. Arora, who has served on the SHM committee that analyzes all nominees for the annual awards, recognizes the value of honoring these high-achieving clinicians.
“There is great value to having our specialty society recognize members in different ways,” she said “The awards of excellence serve as a wonderful reminder of the incredible impact that hospitalists have in many diverse ways … while having the distinction of a fellow or senior fellow serves as a nice benchmark to which new hospitalists can aspire and gain recognition as they emerge as leaders in the field.”
Networking: A skill worth learning
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Ivan Misner once spent one week on Necker Island – the tony 74-acre island in the British Virgin Islands that is entirely owned by billionaire Sir Richard Branson – because he met a guy at a convention.
And Misner is really good at networking.
“I stayed in touch with the person, and when there was an opportunity, I got invited to this incredible ethics program on Necker where I had a chance to meet Sir Richard. It all comes from building relationships with people,” said Misner, founder and chairman of BNI (Business Network International), a 32-year-old global business networking platform based in Charlotte, N.C., that has led CNN to call him “the father of modern networking.”
The why doesn’t matter most, Misner said. A person’s approach to networking, regardless of the hoped-for outcome, should always remain the same.
“The two key themes that I would address would be the mindset and the skill set,” he said.
The mindset is making sure one’s approach doesn’t “feel artificial,” Misner said.
“A lot of people, when they go to some kind of networking environment, they feel like they need to get a shower afterwards and think, ‘Ick, I don’t like that,’” Misner said. “The best way to become an effective networker is to go to networking events with the idea of being willing to help people and really believe in that and practice that. I’ve been doing this a long time and where I see it done wrong is when people use face-to-face networking as a cold-calling opportunity.”
Instead, Misner suggests, approach networking like it is “more about farming than it is about hunting.” Cultivate relationships with time and tenacity and don’t just expect them to be instant. Once the approach is set, Misner has a process he calls VCP – visibility, credibility, and profitability.
“Credibility is what takes time,” he said. “You really want to build credibility with somebody. It doesn’t happen overnight. People have to get to know, like, and trust you. It is the most time consuming portion of the VCP process... then, and only then, can you get to profitability. Where people know who you are, they know what you do, they know you’re good at it, and they’re willing to refer a business to you. They’re willing to put you in touch with other people.”
But even when a relationship gets struck early on, networking must be more than a few minutes at an SHM conference, a local chapter mixer, or a medical school reunion.
It’s the follow-up that makes all the impact. Misner calls that process 24/7/30.
Within 24 hours, send the person a note. An email, or even the seemingly lost art of a hand-written card. (If your handwriting is sloppy, Misner often recommends services that will send out legible notes on your behalf.)
Within a week, connect on social media. Focus on whatever platform that person has on their business card, or email signature. Connect where they like to connect to show the person you’re willing to make the effort.
Within a month, reach out to the person and set a time to talk, either face-to-face or via a telecommunication service like Skype.
“It’s these touch points that you make with people that build the relationship,” Misner said. “Without building a real relationship, there is almost no value in the networking effort because you basically are just waiting to stumble upon opportunities as opposed to building relationships and opportunities. It has to be more than just bumping into somebody at a meeting... otherwise you’re really wasting your time.”
Misner also notes that the point of networking is collaboration at some point. That partnership could be working on a research paper or a pilot project. Or just even getting a phone call returned to talk about something important to you.
“It’s not what you know or who you know, it’s how well you know each other that really counts,” he added. “And meeting people at events like HM17 is only the start of the process. It’s not the end of the process by any means, if you want to do this well.”
Tips for significant others
Heather Howell has gotten pretty good at making the most out of SHM’s annual meeting. It’s not that she has a system for wending through scores of educational offerings, a knack for interpersonal networking or award-winning research.
It’s that she’s the spouse of former SHM President Eric Howell, MD, MHM, and a long-time annual meeting attendee with her husband.
Welcome to HM17, family style. While thousands of hospitalists, nonphysician practitioners, and other attendees swarm the Mandalay Bay Resort and Casino for a four-day crash course on all things hospital medicine, thousands more family members tag along. Husbands and wives, like Mrs. Howell, and, in years past, children like the Howells’ 14-year-old son Mason and 12-year-old daughter Anna. The kids aren’t traveling this year, which is tip No. 1.
“It gets harder as they’re older to drag them to San Diego or Vegas in the middle of a school year, which is when [the annual meeting] is usually held,” said Mrs. Howell, whose day job is as a real estate agent.
Tip No. 2? Make friends the first time around. Maybe it’s with spouses of other physicians from your significant other’s practice. Or maybe it’s with your spouse’s old friends from past jobs. For Mrs. Howell, it’s SHM staff and the families of board members her husband has worked with for years.
“I’ve been doing it for so long that I’ve met a lot of the other [spouses] that do go,” she said. “Usually, if Eric is in meetings all day, I will connect with some of the other spouses and we will go on excursions that are in that town. There is usually so much going on.”
Las Vegas is certainly no exception. In fact, SHM has a dedicated web page recommending family activities. Recommendations include hanging out at the 11-acre Mandalay Beach, which encompasses 2,700 tons of sand, three pools and a lazy river. There’s also the popular Shark Reef Aquarium, a 1.6 million-gallon saltwater habitat with some 2,000 creatures.
Mrs. Howell says excursions further afield could include Red Rock Canyon National Conservation Area, which lies a 25-minute drive from the convention, or the Grand Canyon, which is about two hours east. But planning too much, especially with children, can become a challenge.
“When I arrive, there always seems to be a group of people that are going to do things,” Mrs. Howell said. “It’s very easy to hook up with the other spouses that aren’t involved in the meeting. We always tend to find each other.”
Heather Howell has gotten pretty good at making the most out of SHM’s annual meeting. It’s not that she has a system for wending through scores of educational offerings, a knack for interpersonal networking or award-winning research.
It’s that she’s the spouse of former SHM President Eric Howell, MD, MHM, and a long-time annual meeting attendee with her husband.
Welcome to HM17, family style. While thousands of hospitalists, nonphysician practitioners, and other attendees swarm the Mandalay Bay Resort and Casino for a four-day crash course on all things hospital medicine, thousands more family members tag along. Husbands and wives, like Mrs. Howell, and, in years past, children like the Howells’ 14-year-old son Mason and 12-year-old daughter Anna. The kids aren’t traveling this year, which is tip No. 1.
“It gets harder as they’re older to drag them to San Diego or Vegas in the middle of a school year, which is when [the annual meeting] is usually held,” said Mrs. Howell, whose day job is as a real estate agent.
Tip No. 2? Make friends the first time around. Maybe it’s with spouses of other physicians from your significant other’s practice. Or maybe it’s with your spouse’s old friends from past jobs. For Mrs. Howell, it’s SHM staff and the families of board members her husband has worked with for years.
“I’ve been doing it for so long that I’ve met a lot of the other [spouses] that do go,” she said. “Usually, if Eric is in meetings all day, I will connect with some of the other spouses and we will go on excursions that are in that town. There is usually so much going on.”
Las Vegas is certainly no exception. In fact, SHM has a dedicated web page recommending family activities. Recommendations include hanging out at the 11-acre Mandalay Beach, which encompasses 2,700 tons of sand, three pools and a lazy river. There’s also the popular Shark Reef Aquarium, a 1.6 million-gallon saltwater habitat with some 2,000 creatures.
Mrs. Howell says excursions further afield could include Red Rock Canyon National Conservation Area, which lies a 25-minute drive from the convention, or the Grand Canyon, which is about two hours east. But planning too much, especially with children, can become a challenge.
“When I arrive, there always seems to be a group of people that are going to do things,” Mrs. Howell said. “It’s very easy to hook up with the other spouses that aren’t involved in the meeting. We always tend to find each other.”
Heather Howell has gotten pretty good at making the most out of SHM’s annual meeting. It’s not that she has a system for wending through scores of educational offerings, a knack for interpersonal networking or award-winning research.
It’s that she’s the spouse of former SHM President Eric Howell, MD, MHM, and a long-time annual meeting attendee with her husband.
Welcome to HM17, family style. While thousands of hospitalists, nonphysician practitioners, and other attendees swarm the Mandalay Bay Resort and Casino for a four-day crash course on all things hospital medicine, thousands more family members tag along. Husbands and wives, like Mrs. Howell, and, in years past, children like the Howells’ 14-year-old son Mason and 12-year-old daughter Anna. The kids aren’t traveling this year, which is tip No. 1.
“It gets harder as they’re older to drag them to San Diego or Vegas in the middle of a school year, which is when [the annual meeting] is usually held,” said Mrs. Howell, whose day job is as a real estate agent.
Tip No. 2? Make friends the first time around. Maybe it’s with spouses of other physicians from your significant other’s practice. Or maybe it’s with your spouse’s old friends from past jobs. For Mrs. Howell, it’s SHM staff and the families of board members her husband has worked with for years.
“I’ve been doing it for so long that I’ve met a lot of the other [spouses] that do go,” she said. “Usually, if Eric is in meetings all day, I will connect with some of the other spouses and we will go on excursions that are in that town. There is usually so much going on.”
Las Vegas is certainly no exception. In fact, SHM has a dedicated web page recommending family activities. Recommendations include hanging out at the 11-acre Mandalay Beach, which encompasses 2,700 tons of sand, three pools and a lazy river. There’s also the popular Shark Reef Aquarium, a 1.6 million-gallon saltwater habitat with some 2,000 creatures.
Mrs. Howell says excursions further afield could include Red Rock Canyon National Conservation Area, which lies a 25-minute drive from the convention, or the Grand Canyon, which is about two hours east. But planning too much, especially with children, can become a challenge.
“When I arrive, there always seems to be a group of people that are going to do things,” Mrs. Howell said. “It’s very easy to hook up with the other spouses that aren’t involved in the meeting. We always tend to find each other.”
HM17: Plenaries – Conway and DeSalvo
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”
The first two plenary addresses at HM17 are focused on policy at a time when the dynamically evolving U.S. health care delivery system may seem daunting, opaque, and labyrinthine.
Some might view the health care landscape as hopelessly confusing. Yet both of the keynote speakers use the same word for what they hope to leave their listeners with: optimism.
“Though it feels uncertain in the headlines, the reality is that the health care world feels pretty united in that we need to continue the progress we’ve made on moving away from the fee-for-service model and to let people practice medicine the way they want – to work better as teams and focus on patients and outcomes,” said Karen DeSalvo, MD, MPH, MSc, former acting assistant secretary for health in the U.S. Department of Health and Human Services (HHS) and former national coordinator for health information technology.
“I would view it as an opportunity as well,” said Dr. Conway, who still moonlights as a pediatric academic hospitalist on weekends in greater Washington, D.C. “I think the pieces are coming together. Everything from data, to new payment models, to the MACRA Medicare Physician payment legislation, really suggests a time of positive change.”
Dr. DeSalvo, a former political appointee, joined HHS as the national coordinator for health information technology in 2014 and soon thereafter assumed the acting assistant secretary role. Dr. Conway has attained one of the country’s highest-ranking public health care jobs since joining CMS in 2011. He retained the top post at CMS while President Donald Trump’s nominee to lead the agency, Seema Verma, awaited a confirmation hearing before the U.S. Senate. Dr. Conway’s prior title was principal deputy administrator and CMS chief medical officer.
“I don’t want people to lose sight of the fact that there’s this entire care system that everybody’s working and innovating in every day, trying to find more efficient, effective ways to get better outcomes,” she said. “Hospitalists, quite frankly, have been leading that for their entire existence. They really understand in great granular detail what it takes.”
Dr. DeSalvo believes that the progress of the past 5 years has established a path that must be followed. The public sector move away from fee-for-service has combined with emerging technology platforms to create a new age where physicians and insurers can judge, in real time, how well care is working.
“We’re now in a feedback loop where we can say – ‘When we’ve built a care system like this or when we pay this way, we are actually seeing improved outcomes’ – and change doesn’t take as long,” Dr. DeSalvo said.
Dr. Conway, whose working title for his speech is “Health care System Transformation,” said hospitalists should be encouraged by how well the field has already adapted to the proliferation of accountable care organizations (ACOs), value-based purchasing (VBP), alternative payment models (APM), and the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. He noted that, as innovations lead to better and more coordinated patient care, hospitalists, patients, and hospitals would all benefit.
“I want to leave people with the idea that value-based payment innovation and delivery system reform will continue to be critical aspects of improving our health system,” he said. “I also want hospitalists to continue to stay engaged with these new payment models, help lead them, and provide better patient care as a part of them.”
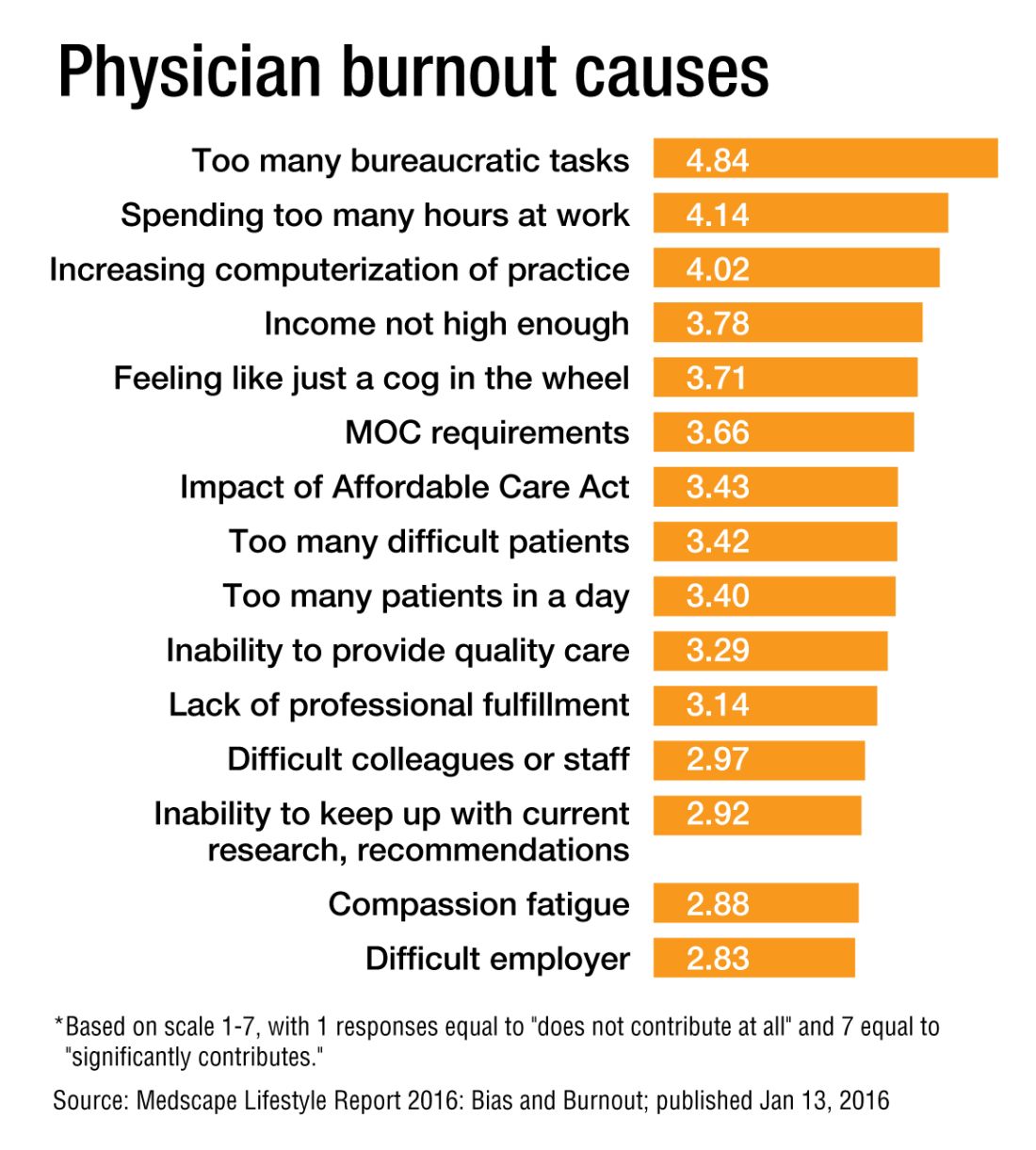
Don’t assume work is sole burnout determinant
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
Physician burnout is almost always linked to issues at work. Blame is placed on added duties piled onto a to-do list that barely makes enough time for prolonged patient interaction in the first place. Fault is laid upon the hours and hours per week – or even per day – wasted on cumbersome data entry into bulky electronic health record (EHR) systems.
But Dike Drummond, MD, a family physician and burnout coach/consultant, says burnout should not be viewed as job specific. “To say that burnout is always about work is absolutely an error,” said Dr. Drummond, whose website is www.thehappymd.com. “You can have people flame out spectacularly at work and nothing has changed about work at all. It’s because something’s going on at home that’s made it impossible to recharge on their time off. And, that list of recharge-blocking issues is huge.”
Money problems, marital problems, family problems: Dr. Drummond says any and all of those issues can eliminate the doctor’s ability to recharge at home.
“The strain of your practice continues, but now without the ability to balance your energy with some recovery when you’re away from the hospital, burnout can come on very rapidly,” he said. “So when you see a colleague flaming out at work, one of the questions you must ask is, “How is it going at home?” You may be the first to learn their spouse left them 2 weeks ago.”
Dr. Drummond’s advice is: Don’t always blame the stresses of work. Build your recharge strategy (rest, hobbies, date nights) and make sure you maintain your recharge capabilities.
“Ideally, with a hospitalist-type schedule, when you’re on you’re on and when you’re off you’re off,” he said. “It should be easier to create that boundary for hospitalists than other specialists who chart from home or are on call.
The “off switch” on your doctor programming is called a boundary ritual. Pick some activity you do on the way home from work, saying to yourself ‘with this action, I am coming all the way home.’ It can be as simple as a deep releasing breath as you step out of your car at home. Make sure you take that breath and let it all go before you walk into the house after each shift.”
Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout, refers to this phenomenon as “work-home interference.” On the bright side for hospitalists, he says, is that aspects of HM work schedules may help mitigate burnout; some work can be left at the hospital when shifts end, rather than following physicians into their home lives.
But Dr. West acknowledged that the rigors of the traditional 7-on/7-off schedule come with their own unique burnout challenges for hospitalists as well.
“A hospitalist can say ‘Well, jeez, I’m on nights for the next week, and that means during the day I’m sleeping and recovering,’” Dr. West explained. “Well, how do you maintain a family life for that period of time when you’re basically off-cycle with your family? There are those kinds of stressors. It’s a mixed bag for hospitalists there.”
Richard Quinn is a freelance writer in New Jersey.
Hot-button issue: physician burnout
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
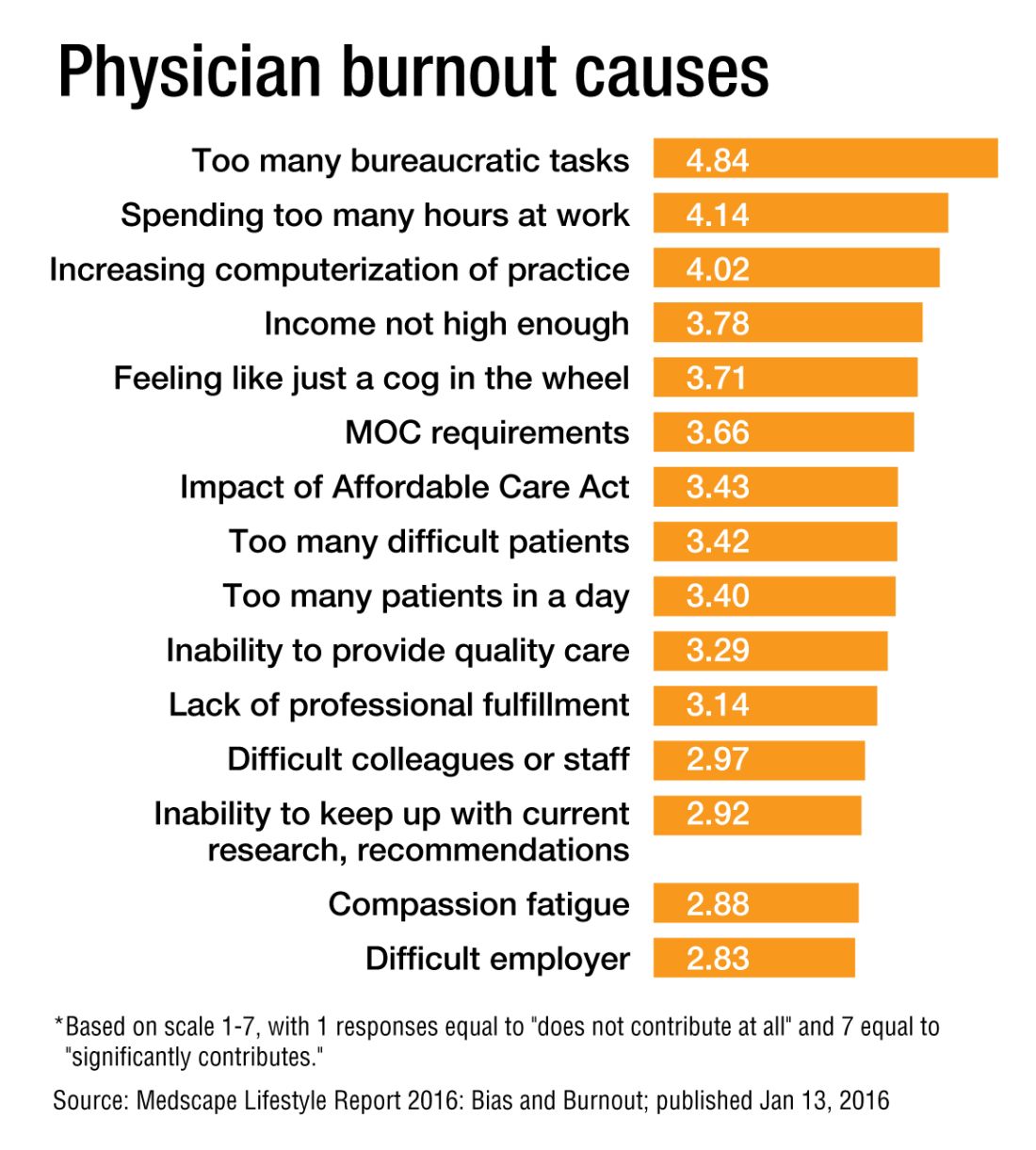
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Some 15 years ago, when Daniel Roberts, MD, FHM, decided at the end of his medical residency that his career path was going to be that of a hospitalist, he heard the same thing. A lot.
“Geesh, don’t you think you’re going to burn out?”
The reasons for such a response are well known in HM circles: the 7-on, 7-off shift structure; the constant rounding; the push-pull between clinical, administrative, and – what many would term – clerical work.
“The truth is somewhere between,” Dr. Roberts said.
Burnout is a hot topic among hospitalists and all of health care these days, as the increasing burdens of a system in seemingly constant change have fostered pressures inside and out of hospitals. Increasingly, researchers are studying and publishing about how to recognize burnout, ways to deal with, or even proactively address the issues. Some MDs – experts in physician burnout – make a living by touring the country and talking about the issue.
But what causes burnout, specifically and exactly?
“The simplistic answer is that burnout is what happens when resources do not meet demand,” said Colin West, MD, PhD, FACP, of the departments of internal medicine and health sciences research at the Mayo Clinic in Rochester, Minn., and a leading researcher on the topic of burnout. “The more complicated answer, which, at this point, is fairly solidly evidence based actually, is that there are five broad categories of drivers of physician distress and burnout.”
Dr. West’s hierarchy of stressors encompasses:
• Work effort.
• Work efficiency.
• Work-home interference.
• A sense of meaning.
• “Flexibility, control, and autonomy.”
Basically, the five drivers lead to this: Physicians who work too much and too inefficiently, with too little control and sense of purpose, end up flaming out more so than do doctors who work fewer hours, with fewer obstacles – all the while feeling satisfied with their autonomy and value.
Academic hospitalist John Yoon, MD, assistant professor of medicine at the University of Chicago, says that health care has to work harder to promote its benefits as being more important than a highly paid profession. Instead, health care should focus on giving meaning to its practitioners.
“I think it is time for leaders of HM groups to honestly discuss the intrinsic meaning and essential ‘calling’ of what it means to be a good hospitalist,” Dr. Yoon wrote in an email interview with The Hospitalist. “What can we do to make the hospitalist vocation a meaningful, long-term career, so that they do not feel like simply revenue-generating ‘pawns’ in a medical-bureaucratic system?”
A ‘meaningful’ career
The modern discussion of burnout as a phenomenon traces back to the Maslach Burnout Inventory, a three-pronged test that measures emotional exhaustion, depersonalization, and personal accomplishment.1 But why does burnout hit physicians – hospitalists, in particular – so intensely? In part, it’s because – like their predecessors in emergency medicine – hospitalists are responsible for managing the care of patients other specialties consult with, operate on, or for whom they run tests.
“Once the patients come up from the emergency room or get admitted to the hospital from the outside, the hospitalist is the one who is largely running that show,” said Dr. West, whose researchshows that HM doctors suffer burnout more than the average across medical specialties.2 “So they’re the front line of inpatient medicine.”
Another factor contributing to burnout’s impact on hospitalists is that the specialty’s rank and file (by definition) work within the walls of institutions that have a lot of contentious and complicated issues that – while outside the purview of HM – can directly or indirectly affect the field. Dr. West calls it the hassle factor.
“You want to get a test in the hospital and, even though you’re the attending on the service, you end up going through three layers of bureaucracy with an insurance company to be able to finally get what you know that patient needs,” he said. “Anything like that contributes to the burnout problem because it pulls the physician away from what they want to be doing, what is purposeful, what is meaningful for them.”
For Dr. Yoon, the exhaustion and cynicism borne out by the work of Maslach and Dr. West’s team are measures indicative of a field where physicians struggle more and more to “make sense of why their practice is worthwhile.
“In the contemporary medical literature, we have been encouraged to adopt the concepts and practices of industrial engineering and quality improvement,” Dr. Yoon added. “In other words, it seems that to the extent physicians’ aspirations to practice good medicine are confined to the narrow and unimaginative constraints of mere scientific technique (more data, higher ‘quality,’ better outcomes) physicians will struggle to recognize and respond to their practice as meaningful. There is no intrinsic meaning to simply being a ‘cog’ in a medical-industrial process or an ‘independent variable’ in an economic equation.”
Finding meaning in one’s job, of course, is less empirical an endpoint than using a reversal agent for a GI bleed. Therein lies the challenge of battling burnout, whose causes and interventions can be as varied as the people who suffer the syndrome.
Local, customized solutions
Once a group leader identifies the symptoms of burnout, the obvious question is how to address it.
Dr. West and his colleagues have identified two broad categories of interventions: individual-focused approaches and organizational solutions. Physician-centered efforts include such tacks as mindfulness, stress reduction, resilience training and small-group communication. Institutional-level changes are, typically, much harder to implement and make successful.
“It doesn’t make sense to ... simply send physicians to stress-management training so that they’re better equipped to deal with a system that is not working to improve itself,” Dr. West said. “The system and the leadership in that system needs to take responsibility from an organizational standpoint.”
Health care as a whole has worked to address the systems-level issue. Duty-hour regulations have been reined in for trainees to be proactive in addressing both fatigue and its inevitable endpoint: burnout.
In a report, “Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-Analysis,”3 published online Dec. 5 in JAMA Internal Medicine, researchers concluded that interventions associated with small benefits “may be boosted by adoption of organization-directed approaches.
“This finding provides support for the view that burnout is a problem of the whole health care organization, rather than individuals,” they wrote.
But the issue typically remains a local one, as group leaders need to realize that what could cause or contribute to burnout in one employee might be enjoyable to another.
“The prospect of doing that was daunting,” Dr. Roberts recalled. “I didn’t know much about EHRs and it was going to be a lot of meetings ... and [it] was going to take me away from patient care. It really ended up being rewarding, despite all the time and frustration, because I got to help represent the interests of my hospitalist colleagues, the physician assistants, and nurses that I work with in trying to avoid some real problems that could have arisen in the EHR.”
Doing that work appealed to Dr. Roberts, so he embraced it. That approach is one championed by Thom Mayer, MD, FACEP, FAAP, executive vice president of EmCare, founder and CEO of BestPractices Inc., medical director for the NFL Players Association, and clinical professor of emergency medicine at George Washington University, Washington, and University of Virginia, Charlottesville. Dr. Mayer travels the country talking about burnout and suggests a three-pronged approach.
First, find what you like about your job and maximize those duties.
Second, label those tasks that are tolerable and don’t allow them to become issues leading to burnout.
Third, and perhaps most difficult, “take the things [you] hate and eliminate them to the best extent possible from [your] job.”
“I’ll give you an example,” he said. “What I hear from emergency physicians and hospitalists is: ‘What do I hate? Well, I hate chronic pain patients.’ Well, does that mean you’re going to be able to eliminate the fact that there are chronic pain patients? No. But, what you can do is ... really drill down on it, and say ‘Why do you hate that?’ The answer is, “Well, I don’t have a strategy for it.” No one likes doing things when they don’t know what they’re doing.
“Now you take the chronic pain patient and the problem is, most of us just haven’t really thought that out. Most of us haven’t sat down with our colleagues and said, “What are you doing that’s working? How are you handling these people? What are the scripts that I can use, the evidence-based language that I can use? What alternatives can I give them?” Instead of just assuming that the only answer to the problem of chronic pain is opioids.”
The silent epidemic
So if there are measurements for burnout, and even best practices on how to address it, why is the issue one that Dr. Mayer calls a silent epidemic? One word: stigma.
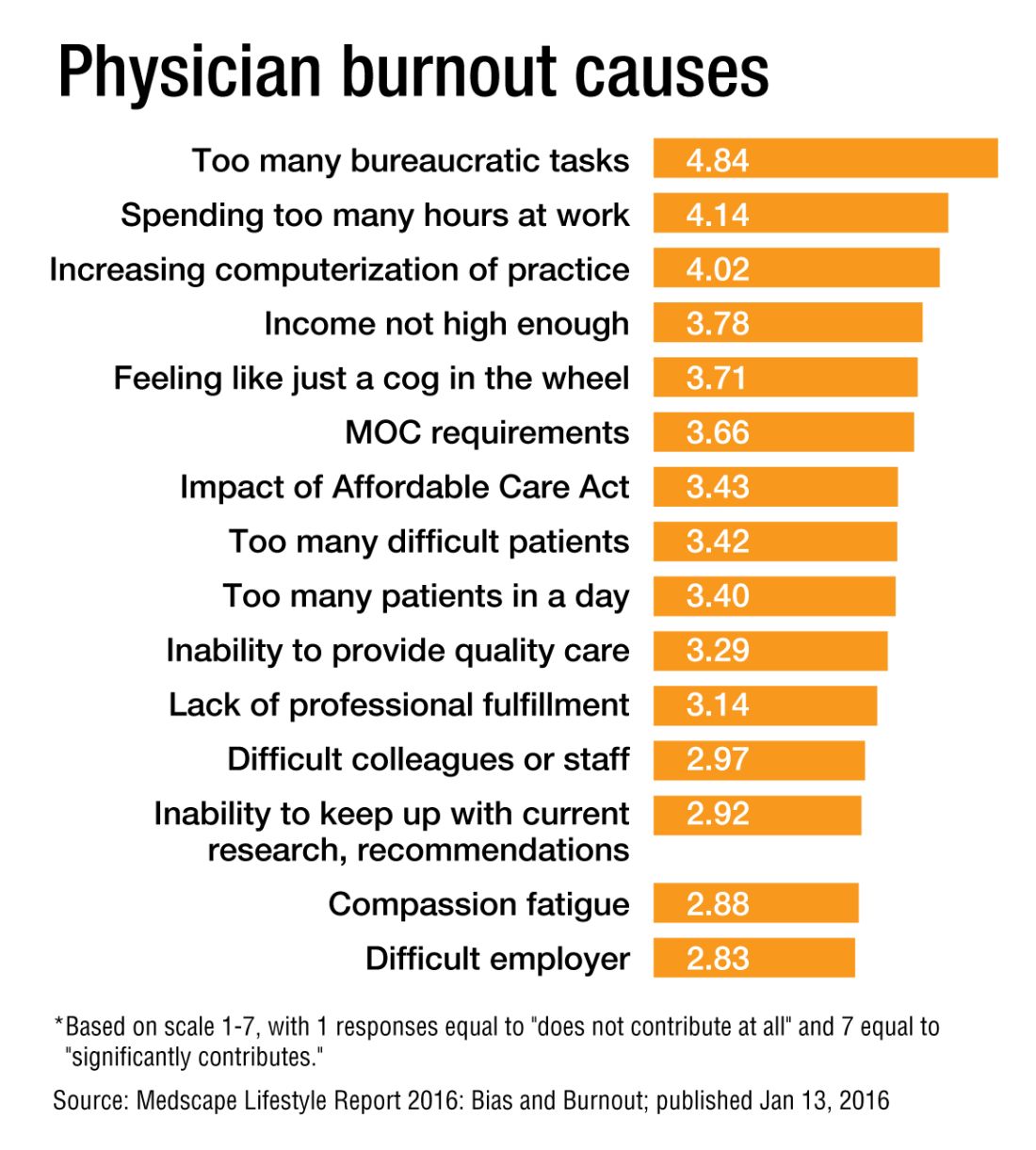
“We as physicians can’t afford to propagate that stigma any further,” Dr. Roberts said. “People who have even tougher jobs than we have, involving combat and hostage negotiation and things like that, have found a way to have honest conversations about the impact of their work on their lives. There is no reason physicians shouldn’t be able to slowly change the culture of medicine to be able to do that, so that there isn’t a stigma around saying, ‘I need some time away before this begins to impact the safety of our patients.’ ”
Dr. West said that when data show that as many as half of all physicians show symptoms of burnout, there is no need to stigmatize a group that large.
Dike Drummond, MD, a family physician, coach, and consultant on burnout prevention, said that the No. 1 mistake physicians and leaders make about burnout is labeling it a “problem.”
“Burnout does not have a single solution because it is not a problem to begin with,” he added. “Burnout is a classic dilemma – a never-ending balancing act. Think of the balancing act of burnout as a teeter-totter, like the one you see in a children’s playground. On one side is the energy you put into your practice and larger life … and on the other side your ability to recharge your energy levels.
“To prevent burnout you must keep your energy expenditure and your recharge activities in balance to keep this teeter-totter in a relatively horizontal position. And the way you address the dilemma is with a strategy: three to five individual tools you use to lower your stress levels or recharge your energy balance.”
And a strategy is a long-term approach to a long-term problem, he said.
“Burnout is not necessarily a terminal condition,” Dr. Roberts said. “If we can structure their work and the balance in their life in such a way that they don’t experience it, or that when they do experience it, they can recognize it and make the changes they need to avoid it getting worse, I think we’d be better off as a profession.”
Richard Quinn is a freelance writer in New Jersey.
References
1. Maslach C, Jackson S. The measurement of experienced burnout. J Occup Behavior. 1981;2:99-113
2. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176-81.
3. Panagioti M, Panagopoulou E, Brower P. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis [published online Dec. 5, 2016 ahead of print]. JAMA Intern Med. doi: 10.1001/jamainternmed.2016.7674.
Miguel Angel Villagra Brings Management Skills to The Hospitalist's Volunteer Editorial Advisory Board
Some have called this the “Year of the Hospitalist,” as it’s the 20th anniversary of the New England Journal of Medicine paper by Dr. Robert Wachter and Dr. Lee Goldman that first used the term “hospitalist” to describe physicians who care for hospitalized patients.
But the paper was more than just that to Miguel Angel Villagra, MD.
He saw it four years ago while training in internal medicine at Texas Tech University Health Sciences Center in El Paso, Texas.
“I was very intrigued,” Dr. Villagra says. “I asked a few of my mentors. They were very skeptical on following a hospitalist career, [but] I saw opportunities for improvement and professional growth in the field, so I decided to jump in. And after four years, I don’t regret my decision of becoming a full-time hospitalist.”
The field doesn’t regret it either. Dr. Villagra was promoted last fall to hospitalist department program medical director at White River Medical Center in Batesville, Ark. And this year, he was named one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Why did you choose a career in medicine?
Answer: At age 11 and after an emergent appendectomy, I decided that I wanted to become a physician. That was one of the best decisions of my life. It is a great combination of art and science, and you get to help people in difficult moments of their life.
Q: Tell us more about your background.
A: I went to medical school in my country of origin at Universidad Autonóma de Nicaragua of Managua, and I did an internal medicine residency at Hospital Militar Escuela Dr. Alejandro Dávila Bolaños. I came to the U.S. for internal medicine residency training at Texas Tech of El Paso. I enjoy learning new skills and this power of knowledge that can help your patients in desperate moments. Most of my challenges during my training involved how to manage stress and sleep deprivation.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were most important lessons you learned from them?
A: Dr. Jorge Cuadra [from Hospital Militar in Nicaragua] and Dr. Manuel Rivera [from Texas Tech], both pulmonologists. They taught me that medicine is a changing field that requires everyday reading. You never end learning new things and approaches. Taking full advantage of your interaction with your patients always improves your clinical skills.
Q: What do you like most about working as a hospitalist?
A: It is an evolving field; we are still trying to “figure it out.” That creates challenges but also opportunities for growth and career development, [for example], how to tackle the readmission problem, how to improve quality at lower cost while keeping patient satisfaction, how to face the burnout challenge and improve physician engagement, just to name a few.
Q: What do you dislike most?
A: In the beginning of my career as a hospitalist, I was exposed constantly to high patient loads that were more than I should have. I also dislike the difficulties at times of electronic medical records. You have to spend excessive time sitting in front of a monitor.
Q: You note the challenges the field of HM is facing. How exciting is it to hopefully be part of the solutions?
A: I feel pumped having been part of this amazing movement of hospital medicine. I think we are leading the change from the acute-care setting front line, helping to take better care of our patients. The current healthcare changes create multiple challenges and, along with that, endless opportunities for professional growth and career development.
Q: You’ve said you see being a chief quality officer in the future. Why? What appeals about those C-suite positions?
A: I think that physicians as leaders are in a great position to drive the change within a healthcare organization toward high-value care. We are at the front line, at the bedside taking care of patients. That gives us firsthand information on what needs to be done. With appropriate training, we can be the executives the institution needs. When I started my role as medical director, initially I focused mainly on managing the group, but rapidly I was involved in several quality projects and academic activities. And soon I realized that I can have a broader impact on what I was doing, going beyond the bedside where you try to offer the best care possible for your patients to an organizational level of change.
Q: How has your journey from Nicaragua to the U.S. shaped you, and how has it shaped the way you practice medicine?
A: Certainly it shaped what I am today, coming from a country that struggles with poverty. During medical school, you lack advances in technology and depend mainly on your desire to excel and be better for the benefit of your patients. You build strong clinical skills from history to physical exam. When you move to the U.S. and have access to so many technological advances, from new diagnostic tests to top-of the-line imaging studies, you combine the best of both worlds, and [that] makes you a better physician. I am very proud of my heritage, and definitely I wouldn’t change anything on my path thus far. I believe the more you overcome difficulties and adversities, the more you appreciate what you accomplished.
Q: As a group leader, why is it important for you to continue seeing patients?
A: We lead our teams by example, and that requires treating patients. I am also a clinician, and I love my profession, so I don’t foresee myself only in an administrative role. Finding the sweet spot of clinician-administrative time is very difficult, and I am still working on it.
Q: What’s the best advice you ever received?
A: Read and learn every day, be good to people, and also dream big.
Q: What’s the worst advice you ever received?
A: Never get married. I didn’t listen.
Richard Quinn is a freelance writer in New Jersey.
Some have called this the “Year of the Hospitalist,” as it’s the 20th anniversary of the New England Journal of Medicine paper by Dr. Robert Wachter and Dr. Lee Goldman that first used the term “hospitalist” to describe physicians who care for hospitalized patients.
But the paper was more than just that to Miguel Angel Villagra, MD.
He saw it four years ago while training in internal medicine at Texas Tech University Health Sciences Center in El Paso, Texas.
“I was very intrigued,” Dr. Villagra says. “I asked a few of my mentors. They were very skeptical on following a hospitalist career, [but] I saw opportunities for improvement and professional growth in the field, so I decided to jump in. And after four years, I don’t regret my decision of becoming a full-time hospitalist.”
The field doesn’t regret it either. Dr. Villagra was promoted last fall to hospitalist department program medical director at White River Medical Center in Batesville, Ark. And this year, he was named one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Why did you choose a career in medicine?
Answer: At age 11 and after an emergent appendectomy, I decided that I wanted to become a physician. That was one of the best decisions of my life. It is a great combination of art and science, and you get to help people in difficult moments of their life.
Q: Tell us more about your background.
A: I went to medical school in my country of origin at Universidad Autonóma de Nicaragua of Managua, and I did an internal medicine residency at Hospital Militar Escuela Dr. Alejandro Dávila Bolaños. I came to the U.S. for internal medicine residency training at Texas Tech of El Paso. I enjoy learning new skills and this power of knowledge that can help your patients in desperate moments. Most of my challenges during my training involved how to manage stress and sleep deprivation.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were most important lessons you learned from them?
A: Dr. Jorge Cuadra [from Hospital Militar in Nicaragua] and Dr. Manuel Rivera [from Texas Tech], both pulmonologists. They taught me that medicine is a changing field that requires everyday reading. You never end learning new things and approaches. Taking full advantage of your interaction with your patients always improves your clinical skills.
Q: What do you like most about working as a hospitalist?
A: It is an evolving field; we are still trying to “figure it out.” That creates challenges but also opportunities for growth and career development, [for example], how to tackle the readmission problem, how to improve quality at lower cost while keeping patient satisfaction, how to face the burnout challenge and improve physician engagement, just to name a few.
Q: What do you dislike most?
A: In the beginning of my career as a hospitalist, I was exposed constantly to high patient loads that were more than I should have. I also dislike the difficulties at times of electronic medical records. You have to spend excessive time sitting in front of a monitor.
Q: You note the challenges the field of HM is facing. How exciting is it to hopefully be part of the solutions?
A: I feel pumped having been part of this amazing movement of hospital medicine. I think we are leading the change from the acute-care setting front line, helping to take better care of our patients. The current healthcare changes create multiple challenges and, along with that, endless opportunities for professional growth and career development.
Q: You’ve said you see being a chief quality officer in the future. Why? What appeals about those C-suite positions?
A: I think that physicians as leaders are in a great position to drive the change within a healthcare organization toward high-value care. We are at the front line, at the bedside taking care of patients. That gives us firsthand information on what needs to be done. With appropriate training, we can be the executives the institution needs. When I started my role as medical director, initially I focused mainly on managing the group, but rapidly I was involved in several quality projects and academic activities. And soon I realized that I can have a broader impact on what I was doing, going beyond the bedside where you try to offer the best care possible for your patients to an organizational level of change.
Q: How has your journey from Nicaragua to the U.S. shaped you, and how has it shaped the way you practice medicine?
A: Certainly it shaped what I am today, coming from a country that struggles with poverty. During medical school, you lack advances in technology and depend mainly on your desire to excel and be better for the benefit of your patients. You build strong clinical skills from history to physical exam. When you move to the U.S. and have access to so many technological advances, from new diagnostic tests to top-of the-line imaging studies, you combine the best of both worlds, and [that] makes you a better physician. I am very proud of my heritage, and definitely I wouldn’t change anything on my path thus far. I believe the more you overcome difficulties and adversities, the more you appreciate what you accomplished.
Q: As a group leader, why is it important for you to continue seeing patients?
A: We lead our teams by example, and that requires treating patients. I am also a clinician, and I love my profession, so I don’t foresee myself only in an administrative role. Finding the sweet spot of clinician-administrative time is very difficult, and I am still working on it.
Q: What’s the best advice you ever received?
A: Read and learn every day, be good to people, and also dream big.
Q: What’s the worst advice you ever received?
A: Never get married. I didn’t listen.
Richard Quinn is a freelance writer in New Jersey.
Some have called this the “Year of the Hospitalist,” as it’s the 20th anniversary of the New England Journal of Medicine paper by Dr. Robert Wachter and Dr. Lee Goldman that first used the term “hospitalist” to describe physicians who care for hospitalized patients.
But the paper was more than just that to Miguel Angel Villagra, MD.
He saw it four years ago while training in internal medicine at Texas Tech University Health Sciences Center in El Paso, Texas.
“I was very intrigued,” Dr. Villagra says. “I asked a few of my mentors. They were very skeptical on following a hospitalist career, [but] I saw opportunities for improvement and professional growth in the field, so I decided to jump in. And after four years, I don’t regret my decision of becoming a full-time hospitalist.”
The field doesn’t regret it either. Dr. Villagra was promoted last fall to hospitalist department program medical director at White River Medical Center in Batesville, Ark. And this year, he was named one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Why did you choose a career in medicine?
Answer: At age 11 and after an emergent appendectomy, I decided that I wanted to become a physician. That was one of the best decisions of my life. It is a great combination of art and science, and you get to help people in difficult moments of their life.
Q: Tell us more about your background.
A: I went to medical school in my country of origin at Universidad Autonóma de Nicaragua of Managua, and I did an internal medicine residency at Hospital Militar Escuela Dr. Alejandro Dávila Bolaños. I came to the U.S. for internal medicine residency training at Texas Tech of El Paso. I enjoy learning new skills and this power of knowledge that can help your patients in desperate moments. Most of my challenges during my training involved how to manage stress and sleep deprivation.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were most important lessons you learned from them?
A: Dr. Jorge Cuadra [from Hospital Militar in Nicaragua] and Dr. Manuel Rivera [from Texas Tech], both pulmonologists. They taught me that medicine is a changing field that requires everyday reading. You never end learning new things and approaches. Taking full advantage of your interaction with your patients always improves your clinical skills.
Q: What do you like most about working as a hospitalist?
A: It is an evolving field; we are still trying to “figure it out.” That creates challenges but also opportunities for growth and career development, [for example], how to tackle the readmission problem, how to improve quality at lower cost while keeping patient satisfaction, how to face the burnout challenge and improve physician engagement, just to name a few.
Q: What do you dislike most?
A: In the beginning of my career as a hospitalist, I was exposed constantly to high patient loads that were more than I should have. I also dislike the difficulties at times of electronic medical records. You have to spend excessive time sitting in front of a monitor.
Q: You note the challenges the field of HM is facing. How exciting is it to hopefully be part of the solutions?
A: I feel pumped having been part of this amazing movement of hospital medicine. I think we are leading the change from the acute-care setting front line, helping to take better care of our patients. The current healthcare changes create multiple challenges and, along with that, endless opportunities for professional growth and career development.
Q: You’ve said you see being a chief quality officer in the future. Why? What appeals about those C-suite positions?
A: I think that physicians as leaders are in a great position to drive the change within a healthcare organization toward high-value care. We are at the front line, at the bedside taking care of patients. That gives us firsthand information on what needs to be done. With appropriate training, we can be the executives the institution needs. When I started my role as medical director, initially I focused mainly on managing the group, but rapidly I was involved in several quality projects and academic activities. And soon I realized that I can have a broader impact on what I was doing, going beyond the bedside where you try to offer the best care possible for your patients to an organizational level of change.
Q: How has your journey from Nicaragua to the U.S. shaped you, and how has it shaped the way you practice medicine?
A: Certainly it shaped what I am today, coming from a country that struggles with poverty. During medical school, you lack advances in technology and depend mainly on your desire to excel and be better for the benefit of your patients. You build strong clinical skills from history to physical exam. When you move to the U.S. and have access to so many technological advances, from new diagnostic tests to top-of the-line imaging studies, you combine the best of both worlds, and [that] makes you a better physician. I am very proud of my heritage, and definitely I wouldn’t change anything on my path thus far. I believe the more you overcome difficulties and adversities, the more you appreciate what you accomplished.
Q: As a group leader, why is it important for you to continue seeing patients?
A: We lead our teams by example, and that requires treating patients. I am also a clinician, and I love my profession, so I don’t foresee myself only in an administrative role. Finding the sweet spot of clinician-administrative time is very difficult, and I am still working on it.
Q: What’s the best advice you ever received?
A: Read and learn every day, be good to people, and also dream big.
Q: What’s the worst advice you ever received?
A: Never get married. I didn’t listen.
Richard Quinn is a freelance writer in New Jersey.
HM 2016: A Year in Review
From celebrating the 20th anniversary of hospital medicine’s arrival to rapid reimbursement reform to sought-after clarity for observation rules, the past 12 months have been eventful. The Hospitalist asked more than a dozen industry leaders what they thought were the biggest highlights of 2016. Here is what they said:
1. Happy Birthday, HM
August 15 marked the 20th anniversary of “The Emerging Role of ‘Hospitalists’ in the American Health Care System,”1 a New England Journal of Medicine paper authored by Lee Goldman, MD, and Robert Wachter, MD, MHM.2 It was the first time anyone defined what a hospitalist was, putting a sobriquet to an inpatient care model that had organically and independently started happening nationwide.
The paper laid the groundwork for a specialty that spread like a proverbial wildfire over the next 20 years. The model overcame early opposition from residents fearful they’d lose the ability to learn and critical-care specialists who wanted to maintain the caseloads they’d fought to build. The field has now swelled to an estimated 52,000 practitioners.
“I reflect back … and think today about what the hospitalist model brings to us,” James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division, told The Hospitalist. “It is an amazing transformation on how the hospitalist model really delivers.”1
2. Its Own Specialty Code
Hospitalist medicine received federal approval for its first dedicated specialty code3 in a decision hailed by many. The code, approved by the Centers for Medicare & Medicaid Services (CMS), should allow hospitalist-specific billing in 2017.
SHM leaders have long pushed for the code, particularly as healthcare transitions from fee-for-service (FFS) to quality-based payment models. Public Policy Committee Chair Ron Greeno, MD, MHM, says that a dedicated code is necessary to ensure that hospitalists are properly reimbursed for their work.
Historically, hospitalists have used codes more in line with the workload of general internal medicine, family medicine, and other specialties. But those codes don’t account for the complexity of what hospitalists deal with on a daily basis.
“We as hospitalists face unique challenges and work with patients from all demographics, often with severe illnesses, making it nearly impossible to rely on benchmarks used for these other specialties,” Dr. Greeno said.3
SHM pushed for the change and has said it is committed to educating members about how best to use it. Scott Sears, MD, FHM, CPE, MBA, chief clinical officer for Sound Physicians of Tacoma, Wash., said the move is great for HM but that more needs to be done to tailor billing and coding to the specialty’s actual workflow.
“A pediatric hospitalist may not want to be compared to an adult hospitalist. A critical-access hospitalist doesn’t want to be compared to a hospitalist in a tertiary academic medical center,” Dr. Sears said. “I don’t think it’s an end-all, be-all, but it’s a place to start.”3
3. Down with SGR, Long Live MACRA
While it’s unlikely hospitalists have that printed on bumper stickers, 2016 brought the end of the oft-maligned Sustainable Growth Rate (SGR) formula. This was the first year under the Medicare Access and CHIP Reauthorization Act of 2015, better known as MACRA.4
MACRA changes the ways hospitalists and other physicians are reimbursed by Medicare by continuing the broader trend of moving from volume-based reimbursements toward a value-based payment (VBP) system. Its two tracks for physicians to change how they get paid are the Merit-Based Incentive Payment System (MIPS) and the Alternative Payments Model (APM).
MIPS probably looks familiar because it is similar to the traditional FFS model. But to make value a more important factor in the reimbursement formula, MIPS will account for both volume and quality. APM allows physicians to opt out of MIPS by participating in other approved programs where providers take on “more than nominal” financial risk, report on their quality measures, and use certified electronic health record (EHR) technology.
4. The Surgeon General Is a Hospitalist
Any specialty’s annual meeting would be lucky to get the U.S. Surgeon General as a plenary speaker, but HM16 featured one of its own in hospitalist and U.S. Surgeon General Vivek Murthy, MD, MBA.
Dr. Murthy kicked off the confab in San Diego, and some 4,000 hospitalists listened to one of their own talk about ascending the highest perch a physician can attain in the federal government.7 Dr. Murthy, previously a hospitalist at Brigham and Women’s Hospital in Boston, was confirmed as the 19th Surgeon General in December 2014.
In an address titled “Bringing Health to America,” Dr. Murthy inspired with tales of hope and encouraged hospitalists to make the pursuit of healthy appealing while improving the safety of our communities. In particular, he suggested hospitalists look to leverage their leadership to improve systems and to be a powerful force of change both inside the walls of their institution and in their communities.
“In the end, the world gets better when people choose to come together to make it better,” he said.8
5. Nurse Practitioner Joins SHM Board of Directors
At HM16, Tracy Cardin, ACNP-BC, SFHM, was the first nurse practitioner (NP) or physician assistant (PA) given voting privileges on the society’s oversight panel.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin said. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”9
With Cardin’s ascension, it has added the voice of another constituency to its board. She was previously chair of SHM’s Nurse Practitioner/Physician Assistant Committee and in 2015 received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has been at the University of Chicago for about 10 years.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” immediate past president Robert Harrington Jr., MD, SFHM said.10
6. The State of Hospital Medicine Is Strong
According to the biennial 2016 State of Hospital Medicine Report6 from SHM and partially populated by data from the Medical Group Management Association (MGMA), median compensation for adult hospitalists rose 10% to $278,746 from 2013 to 2015. The double-digit increase continues the steady climb of hospitalist pay, which is up 30% since 2010. At the same time, productivity is flattening.
And nearly all HM groups (HMGs)—96%—are still getting financial support, mostly from their host hospitals, in addition to their professional fee revenue. However, that median support, $157,535 per full-time employee (FTE), increased just 1%.
The slowing growth in that contribution is a harbinger that the level of financial support can no longer grow unabated, said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
“We’re pretty close to that breaking point,” she said. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”6
7. Pay Cut for ‘Two-Midnight’ Rule for Observations Is No More
CMS announced a proposed rule in April that would have Medicare stop imposing an inpatient payment cut to hospitals under the “two-midnight” rule, according to a report in Modern Healthcare.10 The final rule went into effect in October.
The rule, which continues to be a contentious issue for hospitalists even with the pay cut being eliminated, was put in place in October 2013 to define which Medicare beneficiary hospital stays are appropriate for Medicare Part A payment by stating that if the physician expected the patient to stay for fewer than two midnights, then the services should be billed as outpatient (Medicare Part B) and not inpatient.
For two years, the only exception to the pay withhold was for those diagnoses that CMS designated as “inpatient only.” An overhaul of the rule in October 2015 stated that exceptions could be determined by the physician (or other practitioner) on a “case-by-case basis.”
But a legal challenge and withering criticism from SHM and other professional organizations prompted CMS to undo the withheld payments associated rule.11–13 In fact, hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates of the last three years. SHM has said it will continue to advocate for further changes to the rule.
8. Medicaid Expansion Takes Hold
Thirty-one states and the District of Columbia, under the auspices of the Affordable Care Act, have expanded Medicaid. One 2014 study in states including Minnesota, Kentucky, and Arizona showed a dramatic decrease in uninsured hospital stays and a significant increase in Medicaid stays. Meanwhile, in six states that did not expand, including Florida, Georgia, and Missouri, there was no significant change in payor mix.14
“What a lot of these early studies are saying is that when you expand Medicaid, people get on Medicaid, and that’s exactly what you hope will happen when you do a major public coverage expansion,” said Sayeh Nikpay, PhD, MPH, assistant professor of health policy at Vanderbilt University School of Medicine in Nashville, Tenn., and a lead author of the 2014 Health Affairs study. “Physicians are grappling with payment issues, and it should be quite a relief that people are coming in the door with some kind of insurance rather than uninsured.”15
While expansion from 2015 to 2016 was the main story for Medicaid, many observers are now watching to see what President-elect Donald Trump will do. As a candidate, he campaigned to repeal Obamacare, and that may have significant impacts on the expansion of Medicaid.
9. Antimicrobial Stewardship Rules Upgrade
In July, The Joint Commission announced a new Medication Management (MM) standard for hospitals, critical-access hospitals, and nursing care centers that goes into effect in 2017.16,17 Its stated purpose is to improve quality and patient safety. The Joint Commission move came a year after President Barack Obama made combatting antibiotic-resistant bacteria a national issue.
“If you review the scientific literature, it will indicate that we’re in crisis mode right now because of this,” said Kelly Podgorny, DNP, MS, CPHQ, RN, project director at The Joint Commission. 16
The standard encourages the prioritization of establishing antimicrobial stewardship programs. It suggests staff members at institutions receive training and education on dispensing, administering, and monitoring antimicrobial resistance and antimicrobial stewardship practice. And, in turn, those staffers should look to educate patients and caregivers on appropriate use of antimicrobial medications.
Lastly, when possible, an antimicrobial team should take a multidisciplinary approach and include an infectious disease physician, a pharmacist, and a practitioner.
10. Febrile-Infant Care Draws a Crowd
One of the most well-attended sessions at 2016 Pediatric Hospital Medicine in Chicago was an update on the anticipated American Academy of Pediatricians (AAP) guidelines for febrile infants.18
The guidelines, for infants 7–90 days old, are aimed at providing pediatric hospitalists and others evidence-based guidelines, not rules, from the most recent literature available. The PHM16 session, presented by Kenneth Roberts, MD, highlighted the need to separate individual components of serious bacterial infections such as urinary tract infections (UTIs), bacteremia, and meningitis. Dr. Roberts noted that the incidence and clinical course can vary greatly for the different diagnoses.
The new criteria would be for full-term infants (37–43 weeks’ gestation) who are well-appearing and present with a temperature of 38°C. Exclusion criteria would include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
In particular, the new guidelines will look to risk-stratify management by age groups of 7–28 days, 29–60 days, and 61–90 days. The criteria are expected to be released in the next year.
Richard Quinn is a freelance writer in New Jersey.
References
- Quinn R. HM turns 20: a look at the evolution of hospitalist medicine. The Hospitalist website. Accessed November 14, 2016.
- Wachter M, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-517.
- Tyrrell KA. New hospitalist billing code should benefit hospitalists, patients. The Hospitalist website. Accessed November 14, 2016.
- Doctoroff L, Dutta S. MACRA provides new direction for U.S. healthcare. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. Everything you need to know about the Bundled Payments for Care Improvement Initiative. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. The state of hospital medicine is strong. The Hospitalist website. Accessed November 14, 2016.
- Scheurer D. U.S. surgeon general encourages hospitalists to remain hopeful, motivated. The Hospitalist website. Accessed November 14, 2016.
- Collins TR. HM16 speakers focus on public health, leadership, future of hospital medicine. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. SHM seats its first non-physician board member. The Hospitalist website. Accessed at November 14, 2016.
- Carris J. Centers for Medicare & Medicaid Services (CMS) eliminates two-midnight rule’s inpatient payment cuts: report. The Hospitalist website. Accessed November 14, 2016.
- Schencker L. Judge tells HHS to revisit two-midnight rule’s inpatient pay cut. Healh Affairs website. Accessed November 14, 2016.
- Tyrrell KA. Physicians critical of proposed changes to Medicare’s two-midnight rule. The Hospitalist website. Accessed November 14, 2016.
- Tyrrell KA. Ann Sheehy, MD, MS, FHM, outlines to lawmakers hospitalist concerns about two-midnight rule, Medicare policies. The Hospitalist website. Accessed November 14, 2016.
- Nikpay S, Buchmueller T, Levy HG. Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Aff (Millwood). 2016;35(1):106-110.
- Tyrrell KA. Benefits of Medicaid expansion for hospitalists. The Hospitalist website. Accessed November 14, 2016.
- Bopp S. New standard announced for antimicrobial stewardship. The Hospitalist website. Accessed November 14, 2016.
- Prepublication standards – new antimicrobial stewardship standard. The Joint Commission website. Accessed November 14, 2016.
- 18. DeZure C. PHM16: the new AAP clinical practice guideline on evaluating, managing febrile infants. The Hospitalist website. Accessed November 14, 2016.
From celebrating the 20th anniversary of hospital medicine’s arrival to rapid reimbursement reform to sought-after clarity for observation rules, the past 12 months have been eventful. The Hospitalist asked more than a dozen industry leaders what they thought were the biggest highlights of 2016. Here is what they said:
1. Happy Birthday, HM
August 15 marked the 20th anniversary of “The Emerging Role of ‘Hospitalists’ in the American Health Care System,”1 a New England Journal of Medicine paper authored by Lee Goldman, MD, and Robert Wachter, MD, MHM.2 It was the first time anyone defined what a hospitalist was, putting a sobriquet to an inpatient care model that had organically and independently started happening nationwide.
The paper laid the groundwork for a specialty that spread like a proverbial wildfire over the next 20 years. The model overcame early opposition from residents fearful they’d lose the ability to learn and critical-care specialists who wanted to maintain the caseloads they’d fought to build. The field has now swelled to an estimated 52,000 practitioners.
“I reflect back … and think today about what the hospitalist model brings to us,” James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division, told The Hospitalist. “It is an amazing transformation on how the hospitalist model really delivers.”1
2. Its Own Specialty Code
Hospitalist medicine received federal approval for its first dedicated specialty code3 in a decision hailed by many. The code, approved by the Centers for Medicare & Medicaid Services (CMS), should allow hospitalist-specific billing in 2017.
SHM leaders have long pushed for the code, particularly as healthcare transitions from fee-for-service (FFS) to quality-based payment models. Public Policy Committee Chair Ron Greeno, MD, MHM, says that a dedicated code is necessary to ensure that hospitalists are properly reimbursed for their work.
Historically, hospitalists have used codes more in line with the workload of general internal medicine, family medicine, and other specialties. But those codes don’t account for the complexity of what hospitalists deal with on a daily basis.
“We as hospitalists face unique challenges and work with patients from all demographics, often with severe illnesses, making it nearly impossible to rely on benchmarks used for these other specialties,” Dr. Greeno said.3
SHM pushed for the change and has said it is committed to educating members about how best to use it. Scott Sears, MD, FHM, CPE, MBA, chief clinical officer for Sound Physicians of Tacoma, Wash., said the move is great for HM but that more needs to be done to tailor billing and coding to the specialty’s actual workflow.
“A pediatric hospitalist may not want to be compared to an adult hospitalist. A critical-access hospitalist doesn’t want to be compared to a hospitalist in a tertiary academic medical center,” Dr. Sears said. “I don’t think it’s an end-all, be-all, but it’s a place to start.”3
3. Down with SGR, Long Live MACRA
While it’s unlikely hospitalists have that printed on bumper stickers, 2016 brought the end of the oft-maligned Sustainable Growth Rate (SGR) formula. This was the first year under the Medicare Access and CHIP Reauthorization Act of 2015, better known as MACRA.4
MACRA changes the ways hospitalists and other physicians are reimbursed by Medicare by continuing the broader trend of moving from volume-based reimbursements toward a value-based payment (VBP) system. Its two tracks for physicians to change how they get paid are the Merit-Based Incentive Payment System (MIPS) and the Alternative Payments Model (APM).
MIPS probably looks familiar because it is similar to the traditional FFS model. But to make value a more important factor in the reimbursement formula, MIPS will account for both volume and quality. APM allows physicians to opt out of MIPS by participating in other approved programs where providers take on “more than nominal” financial risk, report on their quality measures, and use certified electronic health record (EHR) technology.
4. The Surgeon General Is a Hospitalist
Any specialty’s annual meeting would be lucky to get the U.S. Surgeon General as a plenary speaker, but HM16 featured one of its own in hospitalist and U.S. Surgeon General Vivek Murthy, MD, MBA.
Dr. Murthy kicked off the confab in San Diego, and some 4,000 hospitalists listened to one of their own talk about ascending the highest perch a physician can attain in the federal government.7 Dr. Murthy, previously a hospitalist at Brigham and Women’s Hospital in Boston, was confirmed as the 19th Surgeon General in December 2014.
In an address titled “Bringing Health to America,” Dr. Murthy inspired with tales of hope and encouraged hospitalists to make the pursuit of healthy appealing while improving the safety of our communities. In particular, he suggested hospitalists look to leverage their leadership to improve systems and to be a powerful force of change both inside the walls of their institution and in their communities.
“In the end, the world gets better when people choose to come together to make it better,” he said.8
5. Nurse Practitioner Joins SHM Board of Directors
At HM16, Tracy Cardin, ACNP-BC, SFHM, was the first nurse practitioner (NP) or physician assistant (PA) given voting privileges on the society’s oversight panel.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin said. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”9
With Cardin’s ascension, it has added the voice of another constituency to its board. She was previously chair of SHM’s Nurse Practitioner/Physician Assistant Committee and in 2015 received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has been at the University of Chicago for about 10 years.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” immediate past president Robert Harrington Jr., MD, SFHM said.10
6. The State of Hospital Medicine Is Strong
According to the biennial 2016 State of Hospital Medicine Report6 from SHM and partially populated by data from the Medical Group Management Association (MGMA), median compensation for adult hospitalists rose 10% to $278,746 from 2013 to 2015. The double-digit increase continues the steady climb of hospitalist pay, which is up 30% since 2010. At the same time, productivity is flattening.
And nearly all HM groups (HMGs)—96%—are still getting financial support, mostly from their host hospitals, in addition to their professional fee revenue. However, that median support, $157,535 per full-time employee (FTE), increased just 1%.
The slowing growth in that contribution is a harbinger that the level of financial support can no longer grow unabated, said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
“We’re pretty close to that breaking point,” she said. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”6
7. Pay Cut for ‘Two-Midnight’ Rule for Observations Is No More
CMS announced a proposed rule in April that would have Medicare stop imposing an inpatient payment cut to hospitals under the “two-midnight” rule, according to a report in Modern Healthcare.10 The final rule went into effect in October.
The rule, which continues to be a contentious issue for hospitalists even with the pay cut being eliminated, was put in place in October 2013 to define which Medicare beneficiary hospital stays are appropriate for Medicare Part A payment by stating that if the physician expected the patient to stay for fewer than two midnights, then the services should be billed as outpatient (Medicare Part B) and not inpatient.
For two years, the only exception to the pay withhold was for those diagnoses that CMS designated as “inpatient only.” An overhaul of the rule in October 2015 stated that exceptions could be determined by the physician (or other practitioner) on a “case-by-case basis.”
But a legal challenge and withering criticism from SHM and other professional organizations prompted CMS to undo the withheld payments associated rule.11–13 In fact, hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates of the last three years. SHM has said it will continue to advocate for further changes to the rule.
8. Medicaid Expansion Takes Hold
Thirty-one states and the District of Columbia, under the auspices of the Affordable Care Act, have expanded Medicaid. One 2014 study in states including Minnesota, Kentucky, and Arizona showed a dramatic decrease in uninsured hospital stays and a significant increase in Medicaid stays. Meanwhile, in six states that did not expand, including Florida, Georgia, and Missouri, there was no significant change in payor mix.14
“What a lot of these early studies are saying is that when you expand Medicaid, people get on Medicaid, and that’s exactly what you hope will happen when you do a major public coverage expansion,” said Sayeh Nikpay, PhD, MPH, assistant professor of health policy at Vanderbilt University School of Medicine in Nashville, Tenn., and a lead author of the 2014 Health Affairs study. “Physicians are grappling with payment issues, and it should be quite a relief that people are coming in the door with some kind of insurance rather than uninsured.”15
While expansion from 2015 to 2016 was the main story for Medicaid, many observers are now watching to see what President-elect Donald Trump will do. As a candidate, he campaigned to repeal Obamacare, and that may have significant impacts on the expansion of Medicaid.
9. Antimicrobial Stewardship Rules Upgrade
In July, The Joint Commission announced a new Medication Management (MM) standard for hospitals, critical-access hospitals, and nursing care centers that goes into effect in 2017.16,17 Its stated purpose is to improve quality and patient safety. The Joint Commission move came a year after President Barack Obama made combatting antibiotic-resistant bacteria a national issue.
“If you review the scientific literature, it will indicate that we’re in crisis mode right now because of this,” said Kelly Podgorny, DNP, MS, CPHQ, RN, project director at The Joint Commission. 16
The standard encourages the prioritization of establishing antimicrobial stewardship programs. It suggests staff members at institutions receive training and education on dispensing, administering, and monitoring antimicrobial resistance and antimicrobial stewardship practice. And, in turn, those staffers should look to educate patients and caregivers on appropriate use of antimicrobial medications.
Lastly, when possible, an antimicrobial team should take a multidisciplinary approach and include an infectious disease physician, a pharmacist, and a practitioner.
10. Febrile-Infant Care Draws a Crowd
One of the most well-attended sessions at 2016 Pediatric Hospital Medicine in Chicago was an update on the anticipated American Academy of Pediatricians (AAP) guidelines for febrile infants.18
The guidelines, for infants 7–90 days old, are aimed at providing pediatric hospitalists and others evidence-based guidelines, not rules, from the most recent literature available. The PHM16 session, presented by Kenneth Roberts, MD, highlighted the need to separate individual components of serious bacterial infections such as urinary tract infections (UTIs), bacteremia, and meningitis. Dr. Roberts noted that the incidence and clinical course can vary greatly for the different diagnoses.
The new criteria would be for full-term infants (37–43 weeks’ gestation) who are well-appearing and present with a temperature of 38°C. Exclusion criteria would include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
In particular, the new guidelines will look to risk-stratify management by age groups of 7–28 days, 29–60 days, and 61–90 days. The criteria are expected to be released in the next year.
Richard Quinn is a freelance writer in New Jersey.
References
- Quinn R. HM turns 20: a look at the evolution of hospitalist medicine. The Hospitalist website. Accessed November 14, 2016.
- Wachter M, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-517.
- Tyrrell KA. New hospitalist billing code should benefit hospitalists, patients. The Hospitalist website. Accessed November 14, 2016.
- Doctoroff L, Dutta S. MACRA provides new direction for U.S. healthcare. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. Everything you need to know about the Bundled Payments for Care Improvement Initiative. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. The state of hospital medicine is strong. The Hospitalist website. Accessed November 14, 2016.
- Scheurer D. U.S. surgeon general encourages hospitalists to remain hopeful, motivated. The Hospitalist website. Accessed November 14, 2016.
- Collins TR. HM16 speakers focus on public health, leadership, future of hospital medicine. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. SHM seats its first non-physician board member. The Hospitalist website. Accessed at November 14, 2016.
- Carris J. Centers for Medicare & Medicaid Services (CMS) eliminates two-midnight rule’s inpatient payment cuts: report. The Hospitalist website. Accessed November 14, 2016.
- Schencker L. Judge tells HHS to revisit two-midnight rule’s inpatient pay cut. Healh Affairs website. Accessed November 14, 2016.
- Tyrrell KA. Physicians critical of proposed changes to Medicare’s two-midnight rule. The Hospitalist website. Accessed November 14, 2016.
- Tyrrell KA. Ann Sheehy, MD, MS, FHM, outlines to lawmakers hospitalist concerns about two-midnight rule, Medicare policies. The Hospitalist website. Accessed November 14, 2016.
- Nikpay S, Buchmueller T, Levy HG. Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Aff (Millwood). 2016;35(1):106-110.
- Tyrrell KA. Benefits of Medicaid expansion for hospitalists. The Hospitalist website. Accessed November 14, 2016.
- Bopp S. New standard announced for antimicrobial stewardship. The Hospitalist website. Accessed November 14, 2016.
- Prepublication standards – new antimicrobial stewardship standard. The Joint Commission website. Accessed November 14, 2016.
- 18. DeZure C. PHM16: the new AAP clinical practice guideline on evaluating, managing febrile infants. The Hospitalist website. Accessed November 14, 2016.
From celebrating the 20th anniversary of hospital medicine’s arrival to rapid reimbursement reform to sought-after clarity for observation rules, the past 12 months have been eventful. The Hospitalist asked more than a dozen industry leaders what they thought were the biggest highlights of 2016. Here is what they said:
1. Happy Birthday, HM
August 15 marked the 20th anniversary of “The Emerging Role of ‘Hospitalists’ in the American Health Care System,”1 a New England Journal of Medicine paper authored by Lee Goldman, MD, and Robert Wachter, MD, MHM.2 It was the first time anyone defined what a hospitalist was, putting a sobriquet to an inpatient care model that had organically and independently started happening nationwide.
The paper laid the groundwork for a specialty that spread like a proverbial wildfire over the next 20 years. The model overcame early opposition from residents fearful they’d lose the ability to learn and critical-care specialists who wanted to maintain the caseloads they’d fought to build. The field has now swelled to an estimated 52,000 practitioners.
“I reflect back … and think today about what the hospitalist model brings to us,” James Merlino, MD, president and chief medical officer of Press Ganey’s strategic consulting division, told The Hospitalist. “It is an amazing transformation on how the hospitalist model really delivers.”1
2. Its Own Specialty Code
Hospitalist medicine received federal approval for its first dedicated specialty code3 in a decision hailed by many. The code, approved by the Centers for Medicare & Medicaid Services (CMS), should allow hospitalist-specific billing in 2017.
SHM leaders have long pushed for the code, particularly as healthcare transitions from fee-for-service (FFS) to quality-based payment models. Public Policy Committee Chair Ron Greeno, MD, MHM, says that a dedicated code is necessary to ensure that hospitalists are properly reimbursed for their work.
Historically, hospitalists have used codes more in line with the workload of general internal medicine, family medicine, and other specialties. But those codes don’t account for the complexity of what hospitalists deal with on a daily basis.
“We as hospitalists face unique challenges and work with patients from all demographics, often with severe illnesses, making it nearly impossible to rely on benchmarks used for these other specialties,” Dr. Greeno said.3
SHM pushed for the change and has said it is committed to educating members about how best to use it. Scott Sears, MD, FHM, CPE, MBA, chief clinical officer for Sound Physicians of Tacoma, Wash., said the move is great for HM but that more needs to be done to tailor billing and coding to the specialty’s actual workflow.
“A pediatric hospitalist may not want to be compared to an adult hospitalist. A critical-access hospitalist doesn’t want to be compared to a hospitalist in a tertiary academic medical center,” Dr. Sears said. “I don’t think it’s an end-all, be-all, but it’s a place to start.”3
3. Down with SGR, Long Live MACRA
While it’s unlikely hospitalists have that printed on bumper stickers, 2016 brought the end of the oft-maligned Sustainable Growth Rate (SGR) formula. This was the first year under the Medicare Access and CHIP Reauthorization Act of 2015, better known as MACRA.4
MACRA changes the ways hospitalists and other physicians are reimbursed by Medicare by continuing the broader trend of moving from volume-based reimbursements toward a value-based payment (VBP) system. Its two tracks for physicians to change how they get paid are the Merit-Based Incentive Payment System (MIPS) and the Alternative Payments Model (APM).
MIPS probably looks familiar because it is similar to the traditional FFS model. But to make value a more important factor in the reimbursement formula, MIPS will account for both volume and quality. APM allows physicians to opt out of MIPS by participating in other approved programs where providers take on “more than nominal” financial risk, report on their quality measures, and use certified electronic health record (EHR) technology.
4. The Surgeon General Is a Hospitalist
Any specialty’s annual meeting would be lucky to get the U.S. Surgeon General as a plenary speaker, but HM16 featured one of its own in hospitalist and U.S. Surgeon General Vivek Murthy, MD, MBA.
Dr. Murthy kicked off the confab in San Diego, and some 4,000 hospitalists listened to one of their own talk about ascending the highest perch a physician can attain in the federal government.7 Dr. Murthy, previously a hospitalist at Brigham and Women’s Hospital in Boston, was confirmed as the 19th Surgeon General in December 2014.
In an address titled “Bringing Health to America,” Dr. Murthy inspired with tales of hope and encouraged hospitalists to make the pursuit of healthy appealing while improving the safety of our communities. In particular, he suggested hospitalists look to leverage their leadership to improve systems and to be a powerful force of change both inside the walls of their institution and in their communities.
“In the end, the world gets better when people choose to come together to make it better,” he said.8
5. Nurse Practitioner Joins SHM Board of Directors
At HM16, Tracy Cardin, ACNP-BC, SFHM, was the first nurse practitioner (NP) or physician assistant (PA) given voting privileges on the society’s oversight panel.
“I can’t describe to you how passionately I believe that [NPs and PAs] have a huge role moving forward,” Cardin said. “I think our representation, our visibility, has sort of been flabby and kind of under the wire for a long time. We can really impact the design of care models at the bedside in a way that’s innovative and more efficient and in a way that’s really huge. I think there’s a transformation that’s going to be coming, and we’re going to be a huge part of it.”9
With Cardin’s ascension, it has added the voice of another constituency to its board. She was previously chair of SHM’s Nurse Practitioner/Physician Assistant Committee and in 2015 received the society’s Award in Excellence in Hospital Medicine for NPs and PAs. She has been at the University of Chicago for about 10 years.
“It does send a message to the rest of our membership that SHM values those other constituencies and that this is not a physician membership organization but rather a membership organization comprised of people who are interested in improving healthcare for our hospitalized patients,” immediate past president Robert Harrington Jr., MD, SFHM said.10
6. The State of Hospital Medicine Is Strong
According to the biennial 2016 State of Hospital Medicine Report6 from SHM and partially populated by data from the Medical Group Management Association (MGMA), median compensation for adult hospitalists rose 10% to $278,746 from 2013 to 2015. The double-digit increase continues the steady climb of hospitalist pay, which is up 30% since 2010. At the same time, productivity is flattening.
And nearly all HM groups (HMGs)—96%—are still getting financial support, mostly from their host hospitals, in addition to their professional fee revenue. However, that median support, $157,535 per full-time employee (FTE), increased just 1%.
The slowing growth in that contribution is a harbinger that the level of financial support can no longer grow unabated, said Leslie Flores, MHA, a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
“We’re pretty close to that breaking point,” she said. “When we go around the country and do consulting work, we are hearing many more hospital leaders telling us, ‘We’re concerned about how much money this program is costing us, and we are getting to the point where we can’t afford it.’”6
7. Pay Cut for ‘Two-Midnight’ Rule for Observations Is No More
CMS announced a proposed rule in April that would have Medicare stop imposing an inpatient payment cut to hospitals under the “two-midnight” rule, according to a report in Modern Healthcare.10 The final rule went into effect in October.
The rule, which continues to be a contentious issue for hospitalists even with the pay cut being eliminated, was put in place in October 2013 to define which Medicare beneficiary hospital stays are appropriate for Medicare Part A payment by stating that if the physician expected the patient to stay for fewer than two midnights, then the services should be billed as outpatient (Medicare Part B) and not inpatient.
For two years, the only exception to the pay withhold was for those diagnoses that CMS designated as “inpatient only.” An overhaul of the rule in October 2015 stated that exceptions could be determined by the physician (or other practitioner) on a “case-by-case basis.”
But a legal challenge and withering criticism from SHM and other professional organizations prompted CMS to undo the withheld payments associated rule.11–13 In fact, hospitals also will see a one-time increase of 0.6% in fiscal 2017, making up for the 0.2% reduction to the rates of the last three years. SHM has said it will continue to advocate for further changes to the rule.
8. Medicaid Expansion Takes Hold
Thirty-one states and the District of Columbia, under the auspices of the Affordable Care Act, have expanded Medicaid. One 2014 study in states including Minnesota, Kentucky, and Arizona showed a dramatic decrease in uninsured hospital stays and a significant increase in Medicaid stays. Meanwhile, in six states that did not expand, including Florida, Georgia, and Missouri, there was no significant change in payor mix.14
“What a lot of these early studies are saying is that when you expand Medicaid, people get on Medicaid, and that’s exactly what you hope will happen when you do a major public coverage expansion,” said Sayeh Nikpay, PhD, MPH, assistant professor of health policy at Vanderbilt University School of Medicine in Nashville, Tenn., and a lead author of the 2014 Health Affairs study. “Physicians are grappling with payment issues, and it should be quite a relief that people are coming in the door with some kind of insurance rather than uninsured.”15
While expansion from 2015 to 2016 was the main story for Medicaid, many observers are now watching to see what President-elect Donald Trump will do. As a candidate, he campaigned to repeal Obamacare, and that may have significant impacts on the expansion of Medicaid.
9. Antimicrobial Stewardship Rules Upgrade
In July, The Joint Commission announced a new Medication Management (MM) standard for hospitals, critical-access hospitals, and nursing care centers that goes into effect in 2017.16,17 Its stated purpose is to improve quality and patient safety. The Joint Commission move came a year after President Barack Obama made combatting antibiotic-resistant bacteria a national issue.
“If you review the scientific literature, it will indicate that we’re in crisis mode right now because of this,” said Kelly Podgorny, DNP, MS, CPHQ, RN, project director at The Joint Commission. 16
The standard encourages the prioritization of establishing antimicrobial stewardship programs. It suggests staff members at institutions receive training and education on dispensing, administering, and monitoring antimicrobial resistance and antimicrobial stewardship practice. And, in turn, those staffers should look to educate patients and caregivers on appropriate use of antimicrobial medications.
Lastly, when possible, an antimicrobial team should take a multidisciplinary approach and include an infectious disease physician, a pharmacist, and a practitioner.
10. Febrile-Infant Care Draws a Crowd
One of the most well-attended sessions at 2016 Pediatric Hospital Medicine in Chicago was an update on the anticipated American Academy of Pediatricians (AAP) guidelines for febrile infants.18
The guidelines, for infants 7–90 days old, are aimed at providing pediatric hospitalists and others evidence-based guidelines, not rules, from the most recent literature available. The PHM16 session, presented by Kenneth Roberts, MD, highlighted the need to separate individual components of serious bacterial infections such as urinary tract infections (UTIs), bacteremia, and meningitis. Dr. Roberts noted that the incidence and clinical course can vary greatly for the different diagnoses.
The new criteria would be for full-term infants (37–43 weeks’ gestation) who are well-appearing and present with a temperature of 38°C. Exclusion criteria would include perinatal/prenatal/neonatal maternal fever, infection, or antimicrobial treatment; the presence of any evident infection; being technology-dependent; and the presence of congenital anomalies.
In particular, the new guidelines will look to risk-stratify management by age groups of 7–28 days, 29–60 days, and 61–90 days. The criteria are expected to be released in the next year.
Richard Quinn is a freelance writer in New Jersey.
References
- Quinn R. HM turns 20: a look at the evolution of hospitalist medicine. The Hospitalist website. Accessed November 14, 2016.
- Wachter M, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-517.
- Tyrrell KA. New hospitalist billing code should benefit hospitalists, patients. The Hospitalist website. Accessed November 14, 2016.
- Doctoroff L, Dutta S. MACRA provides new direction for U.S. healthcare. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. Everything you need to know about the Bundled Payments for Care Improvement Initiative. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. The state of hospital medicine is strong. The Hospitalist website. Accessed November 14, 2016.
- Scheurer D. U.S. surgeon general encourages hospitalists to remain hopeful, motivated. The Hospitalist website. Accessed November 14, 2016.
- Collins TR. HM16 speakers focus on public health, leadership, future of hospital medicine. The Hospitalist website. Accessed November 14, 2016.
- Quinn R. SHM seats its first non-physician board member. The Hospitalist website. Accessed at November 14, 2016.
- Carris J. Centers for Medicare & Medicaid Services (CMS) eliminates two-midnight rule’s inpatient payment cuts: report. The Hospitalist website. Accessed November 14, 2016.
- Schencker L. Judge tells HHS to revisit two-midnight rule’s inpatient pay cut. Healh Affairs website. Accessed November 14, 2016.
- Tyrrell KA. Physicians critical of proposed changes to Medicare’s two-midnight rule. The Hospitalist website. Accessed November 14, 2016.
- Tyrrell KA. Ann Sheehy, MD, MS, FHM, outlines to lawmakers hospitalist concerns about two-midnight rule, Medicare policies. The Hospitalist website. Accessed November 14, 2016.
- Nikpay S, Buchmueller T, Levy HG. Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Aff (Millwood). 2016;35(1):106-110.
- Tyrrell KA. Benefits of Medicaid expansion for hospitalists. The Hospitalist website. Accessed November 14, 2016.
- Bopp S. New standard announced for antimicrobial stewardship. The Hospitalist website. Accessed November 14, 2016.
- Prepublication standards – new antimicrobial stewardship standard. The Joint Commission website. Accessed November 14, 2016.
- 18. DeZure C. PHM16: the new AAP clinical practice guideline on evaluating, managing febrile infants. The Hospitalist website. Accessed November 14, 2016.
Everything You Need to Know About the Bundled Payments for Care Improvement Initiative
As far back as 1983 —13 years before the birth of HM—Medicare created what was then called an “inpatient prospective payment system,” which essentially let Medicare pay a fixed amount for the entirety of a hospital stay, based on diagnosis. Then in 1991, the Centers for Medicare & Medicaid Services (CMS) introduced one payment for coronary artery bypass graft surgery, and even included 90-day readmission in the check.
Fast forward to the past 10 years when accountable care organizations (ACOs) and value-based purchasing (VBP) have been the focus of HM executives looking to take the lead in how to make bundled payments work for them.
The Bundled Payments for Care Improvement (BPCI) initiative was introduced by CMS’s Center for Medicare & Medicaid Innovation (CMMI) in 2011 and is now compiling its first data sets for the next frontier of payments for episodic care.
For rank-and-file hospitalists who have felt inundated by the regulations and promised payment reforms from ACOs and VBPs, why is this program so important?
“The reason this is so special is that it is one of the few CMS programs that allows providers to be in the driver’s seat,” says Kerry Weiner, MD, chief medical officer of acute and post-acute services at TeamHealth-IPC The Hospitalist Company. “They have the opportunity to be accountable and to actually be the designers of reengineering care. The other programs that you just mentioned, like value-based purchasing, largely originate from health systems or the federal government and dictate the principles and the metrics that as a provider you’re going to be evaluated upon.
“This model, the bundled model, gives us the flexibility, scale and brackets of risk that we want to accept and thereby gives us a lot more control over what physicians and physician groups can manage successfully.”
BPCI might be a game-changer for HM because it’s the first of the bundled-payment initiatives that truly falls direct to the care provided by hospitalists. In short, the plan covers 48 defined episodes of care and would parse out payments for those episodes in a holistic—and some say more appropriate—way. Currently, a hospitalist would get paid for a patient’s stay in the hospital and a primary-care physician (PCP) could be paid for some follow-up. If the patient ends up back in the hospital quickly, the hospitalist could get paid again and, upon discharge, a PCP could, too.
But under BPCI, pay would be determined based on the episode of care. The details of who gets paid what and the rules that apply are all likely to evolve, of course, but it’s hoped the basic premise of bundled payments would lower the overall cost of healthcare.
How It Works
Under the Patient Protection and Affordable Care Act (ACA) of 2009, it was mandated that the government establish a five-year pilot program by 2013 that bundled payments for inpatient care, according to the American Hospital Association.
The program has now ramped up to include more than 650 participating organization, not including thousands of physicians that then partner with those groups, over four models. The initiative covers defined episodes of care, both medical and surgical, that begin at the time of inpatient admission and stretch 30, 60 or 90 days post-discharge.
And hospitalists are poised to take the lead on how payment models, especially bundled payments, are shaped over the next few years, says John Nelson, MD, MHM, a co-founder and past president of SHM and and principal in Nelson Flores Hospital Medicine Consultants in Bellevue, Wash. Nelson says his consulting firm has seen an uptick in calls over the past two years dealing with alternative payment models (APMs).
“Hospitalists find themselves at a vitally important nexus of performance and success on new payment models,” he adds.
Win Whitcomb, MD, MHM, chief medical officer of Remedy Partners in Darien, Conn., agrees that BPCI and future iterations of bundled payment programs “are likely to be a potent driver of an evolving hospitalist specialty.” His hypothesis is that APMs such as BPCI are an important way for Medicare to reach its stated goal of having 50% of its fee-for-service payments running through APMs by the end of 2018. To further entice that process, physicians who document at least 25% of their revenue as coming through APMs will get a 5% bonus.
“The stakes are high now,” says Dr. Whitcomb, a past SHM president whose employer is an Awardee Convener in the BPCI initiative, meaning it administers the program. “Medicare [has] laid out the
course for the next two and a half, three years and beyond… It will be crucial for hospitalists to have a path to participate broadly in APMs..”
Dr. Whitcomb says BPCI is the program that should excite hospitalists most because it is more applicable to them moving forward than ACOs, heralded by many healthcare executives several years ago as the future of payment reform.
“With a focus on ambulatory care, ACOs have not broadly involved hospitalists,” he says. “If you look at the State of Hospital Medicine surveys, you look at how many hospitalists are meaningfully working at a system level on ACOs and committees and so forth to improve the performance of the ACO, and it’s very low.”
In fact, just 13.9% of HM groups serving adults only had formed or were participating in a functioning ACO, according to SHM’s 2014 State of Hospital Medicine report. Another 6% were in the process of forming or participating, the paper reported.
“ACOs have not yet widely worked alongside hospitalist teams to optimize where patients go after hospitalization, which is arguably the most important way to deal with post-acute-care utilization” Dr. Whitcomb adds. “whereas nearly all hospitalists working in bundle payments are focusing on a ‘high-value’ transition out of the hospital.”
Improving Care
While BPCI is focused on payment structure, the program could breed process improvements as well as improve care, says hospitalist Patrick Conway, MD, MHM, MSc, CMS’s chief medical officer and deputy administrator for innovation and quality.
“In addition to assessing the quality of patient outcomes and patient experience, CMS is also monitoring for unintended consequences, including whether there is an increase in the number of specific clinical episodes [such as specific elective surgeries] that would not have been expected in the absence of BPCI,” Dr. Conway says. “CMS can audit and intervene if it detects unintended negative consequences for beneficiaries.”
Dr. Whitcomb says two main ways that hospitalists can use BPCI to calculate value is by having better metrics on post-acute facility utilization and reduced readmission.
Immediate past SHM President Robert Harrington Jr., MD, SFHM, says that BPCI is a major stepping stone to merging quality and payment, along the lines of using Physician Quality Reporting System (PQRS) data in the value-based payment modifier.
“CMS is saying to all of us in the provider world, ‘We want to get out of the business of unit economics, and we want to start paying for episodes of care and providers should be at risk for quality outcomes,” he says. “BPCI, to me, is one of the rungs in the ladder.”
Dr. Harrington, chief medical officer at Reliant Post-Acute Care Solutions in Atlanta, says that the program’s inclusion of acute-care hospitals, skilled nursing facilities (SNFs), physician group practices, long-term care hospitals, inpatient rehabilitation facilities, and home health agencies working together is what differentiates it from past attempts at payment reform.
“Population health is sort of where this is headed,” he adds. “You sit in a CFO seat at a hospital or healthcare system right now, and five years ago, they’d buy an MRI machine and they wanted throughput through that MRI machine and they wanted as many people run through that MRI machine in the fee-for-service world as they could get to go through that machine. Nowadays, you start to look at it from a population health standpoint and the CFO is going to say to you, ‘I don’t want anybody going through that MRI machine unless they have to.’
“So it’s a total reversal of perspective when hospitals either become joined at the hip with the payors or become the payors and they start taking risk on population health and I think BPCI is one way that Medicare has allowed all of us to test the waters and get comfortable with that.”
Getting Involved
Dr. Weiner is aware that some hospitalists are nervous about bundled payments because their reimbursement is, in part based on care provided outside of their control. Take a surgical procedure where a hospitalist managing the post-surgery care is left to deal with any potential mistakes made. Or the process works fine until there is poor management by ambulatory care once the patient is discharged.
“That is the reason this program exists,” he says. “It poses the question, who is going to be accountable for the care outside of the traditional site of care that providers have been practicing in, your traditional boundaries? I would argue that physicians are more or are just as valuable as any other segment of the healthcare system in managing the transitions of care and in managing the gaps in the system.”
Given how HM has moved into post-discharge care via SNFs and other post-acute care facilities in recent years, Dr. Weiner says that while hospitalists can’t actually deliver all of the care in an “episode,” they can shepherd that process.
Hospitalists “have control over where the patient goes after they leave the acute-care facility, for example,” he says. “They write the orders on what level of care is needed, and they should have the intimate knowledge about what’s available in their community to ensure the patient gets the best care possible. As long as they have the accountability and the power to direct care, then they have the ability to negotiate and recommend care that is best for the patient, so they can select the better facilities in the community, the better agencies in the community, the better resources in the community to ensure that there is better care once the patient leaves the hospital.”
Dr. Conway suggests HM practitioners view BPCI as a model based on “quality and value.” He says early participants helped define clinical episodes, length of episode, and risk track, making the program better suited to address the actual needs of hospitalists.
“I would encourage hospital medicine physicians and care teams to view bundled payment models as an opportunity for them and their patients for better care and smarter spending,” he adds. “CMS continues to explore ways to pay for value and not just volume. Many of the organizations that are participating in BPCI have partnered with their physician communities and established gainsharing agreement. …Most importantly, this model focuses on care coordination for patients across episodes of care.
And that’s the key for Dr. Weiner.
Hospitalists who embrace BPCI can shape it as the predominant inpatient funding model for hospitals over the next five or 10 years. HM administrators and practitioners who don’t seize the opportunity to flesh out the program tacitly cede control to people outside the hospital who may not tailor the program nearly as well, he says.
“Those who have accountability in the end, the systems, the people, the entities, the providers that have the ability, the accountability for it will ultimately design it,” Dr. Weiner adds. “I think physicians, especially hospitalists, should be at that table. We should play an active role in designing the system.” TH
Richard Quinn is a freelance writer in New Jersey.
As far back as 1983 —13 years before the birth of HM—Medicare created what was then called an “inpatient prospective payment system,” which essentially let Medicare pay a fixed amount for the entirety of a hospital stay, based on diagnosis. Then in 1991, the Centers for Medicare & Medicaid Services (CMS) introduced one payment for coronary artery bypass graft surgery, and even included 90-day readmission in the check.
Fast forward to the past 10 years when accountable care organizations (ACOs) and value-based purchasing (VBP) have been the focus of HM executives looking to take the lead in how to make bundled payments work for them.
The Bundled Payments for Care Improvement (BPCI) initiative was introduced by CMS’s Center for Medicare & Medicaid Innovation (CMMI) in 2011 and is now compiling its first data sets for the next frontier of payments for episodic care.
For rank-and-file hospitalists who have felt inundated by the regulations and promised payment reforms from ACOs and VBPs, why is this program so important?
“The reason this is so special is that it is one of the few CMS programs that allows providers to be in the driver’s seat,” says Kerry Weiner, MD, chief medical officer of acute and post-acute services at TeamHealth-IPC The Hospitalist Company. “They have the opportunity to be accountable and to actually be the designers of reengineering care. The other programs that you just mentioned, like value-based purchasing, largely originate from health systems or the federal government and dictate the principles and the metrics that as a provider you’re going to be evaluated upon.
“This model, the bundled model, gives us the flexibility, scale and brackets of risk that we want to accept and thereby gives us a lot more control over what physicians and physician groups can manage successfully.”
BPCI might be a game-changer for HM because it’s the first of the bundled-payment initiatives that truly falls direct to the care provided by hospitalists. In short, the plan covers 48 defined episodes of care and would parse out payments for those episodes in a holistic—and some say more appropriate—way. Currently, a hospitalist would get paid for a patient’s stay in the hospital and a primary-care physician (PCP) could be paid for some follow-up. If the patient ends up back in the hospital quickly, the hospitalist could get paid again and, upon discharge, a PCP could, too.
But under BPCI, pay would be determined based on the episode of care. The details of who gets paid what and the rules that apply are all likely to evolve, of course, but it’s hoped the basic premise of bundled payments would lower the overall cost of healthcare.
How It Works
Under the Patient Protection and Affordable Care Act (ACA) of 2009, it was mandated that the government establish a five-year pilot program by 2013 that bundled payments for inpatient care, according to the American Hospital Association.
The program has now ramped up to include more than 650 participating organization, not including thousands of physicians that then partner with those groups, over four models. The initiative covers defined episodes of care, both medical and surgical, that begin at the time of inpatient admission and stretch 30, 60 or 90 days post-discharge.
And hospitalists are poised to take the lead on how payment models, especially bundled payments, are shaped over the next few years, says John Nelson, MD, MHM, a co-founder and past president of SHM and and principal in Nelson Flores Hospital Medicine Consultants in Bellevue, Wash. Nelson says his consulting firm has seen an uptick in calls over the past two years dealing with alternative payment models (APMs).
“Hospitalists find themselves at a vitally important nexus of performance and success on new payment models,” he adds.
Win Whitcomb, MD, MHM, chief medical officer of Remedy Partners in Darien, Conn., agrees that BPCI and future iterations of bundled payment programs “are likely to be a potent driver of an evolving hospitalist specialty.” His hypothesis is that APMs such as BPCI are an important way for Medicare to reach its stated goal of having 50% of its fee-for-service payments running through APMs by the end of 2018. To further entice that process, physicians who document at least 25% of their revenue as coming through APMs will get a 5% bonus.
“The stakes are high now,” says Dr. Whitcomb, a past SHM president whose employer is an Awardee Convener in the BPCI initiative, meaning it administers the program. “Medicare [has] laid out the
course for the next two and a half, three years and beyond… It will be crucial for hospitalists to have a path to participate broadly in APMs..”
Dr. Whitcomb says BPCI is the program that should excite hospitalists most because it is more applicable to them moving forward than ACOs, heralded by many healthcare executives several years ago as the future of payment reform.
“With a focus on ambulatory care, ACOs have not broadly involved hospitalists,” he says. “If you look at the State of Hospital Medicine surveys, you look at how many hospitalists are meaningfully working at a system level on ACOs and committees and so forth to improve the performance of the ACO, and it’s very low.”
In fact, just 13.9% of HM groups serving adults only had formed or were participating in a functioning ACO, according to SHM’s 2014 State of Hospital Medicine report. Another 6% were in the process of forming or participating, the paper reported.
“ACOs have not yet widely worked alongside hospitalist teams to optimize where patients go after hospitalization, which is arguably the most important way to deal with post-acute-care utilization” Dr. Whitcomb adds. “whereas nearly all hospitalists working in bundle payments are focusing on a ‘high-value’ transition out of the hospital.”
Improving Care
While BPCI is focused on payment structure, the program could breed process improvements as well as improve care, says hospitalist Patrick Conway, MD, MHM, MSc, CMS’s chief medical officer and deputy administrator for innovation and quality.
“In addition to assessing the quality of patient outcomes and patient experience, CMS is also monitoring for unintended consequences, including whether there is an increase in the number of specific clinical episodes [such as specific elective surgeries] that would not have been expected in the absence of BPCI,” Dr. Conway says. “CMS can audit and intervene if it detects unintended negative consequences for beneficiaries.”
Dr. Whitcomb says two main ways that hospitalists can use BPCI to calculate value is by having better metrics on post-acute facility utilization and reduced readmission.
Immediate past SHM President Robert Harrington Jr., MD, SFHM, says that BPCI is a major stepping stone to merging quality and payment, along the lines of using Physician Quality Reporting System (PQRS) data in the value-based payment modifier.
“CMS is saying to all of us in the provider world, ‘We want to get out of the business of unit economics, and we want to start paying for episodes of care and providers should be at risk for quality outcomes,” he says. “BPCI, to me, is one of the rungs in the ladder.”
Dr. Harrington, chief medical officer at Reliant Post-Acute Care Solutions in Atlanta, says that the program’s inclusion of acute-care hospitals, skilled nursing facilities (SNFs), physician group practices, long-term care hospitals, inpatient rehabilitation facilities, and home health agencies working together is what differentiates it from past attempts at payment reform.
“Population health is sort of where this is headed,” he adds. “You sit in a CFO seat at a hospital or healthcare system right now, and five years ago, they’d buy an MRI machine and they wanted throughput through that MRI machine and they wanted as many people run through that MRI machine in the fee-for-service world as they could get to go through that machine. Nowadays, you start to look at it from a population health standpoint and the CFO is going to say to you, ‘I don’t want anybody going through that MRI machine unless they have to.’
“So it’s a total reversal of perspective when hospitals either become joined at the hip with the payors or become the payors and they start taking risk on population health and I think BPCI is one way that Medicare has allowed all of us to test the waters and get comfortable with that.”
Getting Involved
Dr. Weiner is aware that some hospitalists are nervous about bundled payments because their reimbursement is, in part based on care provided outside of their control. Take a surgical procedure where a hospitalist managing the post-surgery care is left to deal with any potential mistakes made. Or the process works fine until there is poor management by ambulatory care once the patient is discharged.
“That is the reason this program exists,” he says. “It poses the question, who is going to be accountable for the care outside of the traditional site of care that providers have been practicing in, your traditional boundaries? I would argue that physicians are more or are just as valuable as any other segment of the healthcare system in managing the transitions of care and in managing the gaps in the system.”
Given how HM has moved into post-discharge care via SNFs and other post-acute care facilities in recent years, Dr. Weiner says that while hospitalists can’t actually deliver all of the care in an “episode,” they can shepherd that process.
Hospitalists “have control over where the patient goes after they leave the acute-care facility, for example,” he says. “They write the orders on what level of care is needed, and they should have the intimate knowledge about what’s available in their community to ensure the patient gets the best care possible. As long as they have the accountability and the power to direct care, then they have the ability to negotiate and recommend care that is best for the patient, so they can select the better facilities in the community, the better agencies in the community, the better resources in the community to ensure that there is better care once the patient leaves the hospital.”
Dr. Conway suggests HM practitioners view BPCI as a model based on “quality and value.” He says early participants helped define clinical episodes, length of episode, and risk track, making the program better suited to address the actual needs of hospitalists.
“I would encourage hospital medicine physicians and care teams to view bundled payment models as an opportunity for them and their patients for better care and smarter spending,” he adds. “CMS continues to explore ways to pay for value and not just volume. Many of the organizations that are participating in BPCI have partnered with their physician communities and established gainsharing agreement. …Most importantly, this model focuses on care coordination for patients across episodes of care.
And that’s the key for Dr. Weiner.
Hospitalists who embrace BPCI can shape it as the predominant inpatient funding model for hospitals over the next five or 10 years. HM administrators and practitioners who don’t seize the opportunity to flesh out the program tacitly cede control to people outside the hospital who may not tailor the program nearly as well, he says.
“Those who have accountability in the end, the systems, the people, the entities, the providers that have the ability, the accountability for it will ultimately design it,” Dr. Weiner adds. “I think physicians, especially hospitalists, should be at that table. We should play an active role in designing the system.” TH
Richard Quinn is a freelance writer in New Jersey.
As far back as 1983 —13 years before the birth of HM—Medicare created what was then called an “inpatient prospective payment system,” which essentially let Medicare pay a fixed amount for the entirety of a hospital stay, based on diagnosis. Then in 1991, the Centers for Medicare & Medicaid Services (CMS) introduced one payment for coronary artery bypass graft surgery, and even included 90-day readmission in the check.
Fast forward to the past 10 years when accountable care organizations (ACOs) and value-based purchasing (VBP) have been the focus of HM executives looking to take the lead in how to make bundled payments work for them.
The Bundled Payments for Care Improvement (BPCI) initiative was introduced by CMS’s Center for Medicare & Medicaid Innovation (CMMI) in 2011 and is now compiling its first data sets for the next frontier of payments for episodic care.
For rank-and-file hospitalists who have felt inundated by the regulations and promised payment reforms from ACOs and VBPs, why is this program so important?
“The reason this is so special is that it is one of the few CMS programs that allows providers to be in the driver’s seat,” says Kerry Weiner, MD, chief medical officer of acute and post-acute services at TeamHealth-IPC The Hospitalist Company. “They have the opportunity to be accountable and to actually be the designers of reengineering care. The other programs that you just mentioned, like value-based purchasing, largely originate from health systems or the federal government and dictate the principles and the metrics that as a provider you’re going to be evaluated upon.
“This model, the bundled model, gives us the flexibility, scale and brackets of risk that we want to accept and thereby gives us a lot more control over what physicians and physician groups can manage successfully.”
BPCI might be a game-changer for HM because it’s the first of the bundled-payment initiatives that truly falls direct to the care provided by hospitalists. In short, the plan covers 48 defined episodes of care and would parse out payments for those episodes in a holistic—and some say more appropriate—way. Currently, a hospitalist would get paid for a patient’s stay in the hospital and a primary-care physician (PCP) could be paid for some follow-up. If the patient ends up back in the hospital quickly, the hospitalist could get paid again and, upon discharge, a PCP could, too.
But under BPCI, pay would be determined based on the episode of care. The details of who gets paid what and the rules that apply are all likely to evolve, of course, but it’s hoped the basic premise of bundled payments would lower the overall cost of healthcare.
How It Works
Under the Patient Protection and Affordable Care Act (ACA) of 2009, it was mandated that the government establish a five-year pilot program by 2013 that bundled payments for inpatient care, according to the American Hospital Association.
The program has now ramped up to include more than 650 participating organization, not including thousands of physicians that then partner with those groups, over four models. The initiative covers defined episodes of care, both medical and surgical, that begin at the time of inpatient admission and stretch 30, 60 or 90 days post-discharge.
And hospitalists are poised to take the lead on how payment models, especially bundled payments, are shaped over the next few years, says John Nelson, MD, MHM, a co-founder and past president of SHM and and principal in Nelson Flores Hospital Medicine Consultants in Bellevue, Wash. Nelson says his consulting firm has seen an uptick in calls over the past two years dealing with alternative payment models (APMs).
“Hospitalists find themselves at a vitally important nexus of performance and success on new payment models,” he adds.
Win Whitcomb, MD, MHM, chief medical officer of Remedy Partners in Darien, Conn., agrees that BPCI and future iterations of bundled payment programs “are likely to be a potent driver of an evolving hospitalist specialty.” His hypothesis is that APMs such as BPCI are an important way for Medicare to reach its stated goal of having 50% of its fee-for-service payments running through APMs by the end of 2018. To further entice that process, physicians who document at least 25% of their revenue as coming through APMs will get a 5% bonus.
“The stakes are high now,” says Dr. Whitcomb, a past SHM president whose employer is an Awardee Convener in the BPCI initiative, meaning it administers the program. “Medicare [has] laid out the
course for the next two and a half, three years and beyond… It will be crucial for hospitalists to have a path to participate broadly in APMs..”
Dr. Whitcomb says BPCI is the program that should excite hospitalists most because it is more applicable to them moving forward than ACOs, heralded by many healthcare executives several years ago as the future of payment reform.
“With a focus on ambulatory care, ACOs have not broadly involved hospitalists,” he says. “If you look at the State of Hospital Medicine surveys, you look at how many hospitalists are meaningfully working at a system level on ACOs and committees and so forth to improve the performance of the ACO, and it’s very low.”
In fact, just 13.9% of HM groups serving adults only had formed or were participating in a functioning ACO, according to SHM’s 2014 State of Hospital Medicine report. Another 6% were in the process of forming or participating, the paper reported.
“ACOs have not yet widely worked alongside hospitalist teams to optimize where patients go after hospitalization, which is arguably the most important way to deal with post-acute-care utilization” Dr. Whitcomb adds. “whereas nearly all hospitalists working in bundle payments are focusing on a ‘high-value’ transition out of the hospital.”
Improving Care
While BPCI is focused on payment structure, the program could breed process improvements as well as improve care, says hospitalist Patrick Conway, MD, MHM, MSc, CMS’s chief medical officer and deputy administrator for innovation and quality.
“In addition to assessing the quality of patient outcomes and patient experience, CMS is also monitoring for unintended consequences, including whether there is an increase in the number of specific clinical episodes [such as specific elective surgeries] that would not have been expected in the absence of BPCI,” Dr. Conway says. “CMS can audit and intervene if it detects unintended negative consequences for beneficiaries.”
Dr. Whitcomb says two main ways that hospitalists can use BPCI to calculate value is by having better metrics on post-acute facility utilization and reduced readmission.
Immediate past SHM President Robert Harrington Jr., MD, SFHM, says that BPCI is a major stepping stone to merging quality and payment, along the lines of using Physician Quality Reporting System (PQRS) data in the value-based payment modifier.
“CMS is saying to all of us in the provider world, ‘We want to get out of the business of unit economics, and we want to start paying for episodes of care and providers should be at risk for quality outcomes,” he says. “BPCI, to me, is one of the rungs in the ladder.”
Dr. Harrington, chief medical officer at Reliant Post-Acute Care Solutions in Atlanta, says that the program’s inclusion of acute-care hospitals, skilled nursing facilities (SNFs), physician group practices, long-term care hospitals, inpatient rehabilitation facilities, and home health agencies working together is what differentiates it from past attempts at payment reform.
“Population health is sort of where this is headed,” he adds. “You sit in a CFO seat at a hospital or healthcare system right now, and five years ago, they’d buy an MRI machine and they wanted throughput through that MRI machine and they wanted as many people run through that MRI machine in the fee-for-service world as they could get to go through that machine. Nowadays, you start to look at it from a population health standpoint and the CFO is going to say to you, ‘I don’t want anybody going through that MRI machine unless they have to.’
“So it’s a total reversal of perspective when hospitals either become joined at the hip with the payors or become the payors and they start taking risk on population health and I think BPCI is one way that Medicare has allowed all of us to test the waters and get comfortable with that.”
Getting Involved
Dr. Weiner is aware that some hospitalists are nervous about bundled payments because their reimbursement is, in part based on care provided outside of their control. Take a surgical procedure where a hospitalist managing the post-surgery care is left to deal with any potential mistakes made. Or the process works fine until there is poor management by ambulatory care once the patient is discharged.
“That is the reason this program exists,” he says. “It poses the question, who is going to be accountable for the care outside of the traditional site of care that providers have been practicing in, your traditional boundaries? I would argue that physicians are more or are just as valuable as any other segment of the healthcare system in managing the transitions of care and in managing the gaps in the system.”
Given how HM has moved into post-discharge care via SNFs and other post-acute care facilities in recent years, Dr. Weiner says that while hospitalists can’t actually deliver all of the care in an “episode,” they can shepherd that process.
Hospitalists “have control over where the patient goes after they leave the acute-care facility, for example,” he says. “They write the orders on what level of care is needed, and they should have the intimate knowledge about what’s available in their community to ensure the patient gets the best care possible. As long as they have the accountability and the power to direct care, then they have the ability to negotiate and recommend care that is best for the patient, so they can select the better facilities in the community, the better agencies in the community, the better resources in the community to ensure that there is better care once the patient leaves the hospital.”
Dr. Conway suggests HM practitioners view BPCI as a model based on “quality and value.” He says early participants helped define clinical episodes, length of episode, and risk track, making the program better suited to address the actual needs of hospitalists.
“I would encourage hospital medicine physicians and care teams to view bundled payment models as an opportunity for them and their patients for better care and smarter spending,” he adds. “CMS continues to explore ways to pay for value and not just volume. Many of the organizations that are participating in BPCI have partnered with their physician communities and established gainsharing agreement. …Most importantly, this model focuses on care coordination for patients across episodes of care.
And that’s the key for Dr. Weiner.
Hospitalists who embrace BPCI can shape it as the predominant inpatient funding model for hospitals over the next five or 10 years. HM administrators and practitioners who don’t seize the opportunity to flesh out the program tacitly cede control to people outside the hospital who may not tailor the program nearly as well, he says.
“Those who have accountability in the end, the systems, the people, the entities, the providers that have the ability, the accountability for it will ultimately design it,” Dr. Weiner adds. “I think physicians, especially hospitalists, should be at that table. We should play an active role in designing the system.” TH
Richard Quinn is a freelance writer in New Jersey.